RT-qPCR in Liquid Biopsy: A Comprehensive Guide for Cancer Detection and Monitoring
This article provides a detailed examination of Reverse Transcription Quantitative PCR (RT-qPCR) for liquid biopsy applications in oncology, tailored for researchers and drug development professionals.
RT-qPCR in Liquid Biopsy: A Comprehensive Guide for Cancer Detection and Monitoring
Abstract
This article provides a detailed examination of Reverse Transcription Quantitative PCR (RT-qPCR) for liquid biopsy applications in oncology, tailored for researchers and drug development professionals. It explores the foundational principles of detecting circulating biomarkers like mRNA and microRNA in blood and bone marrow. The content delves into advanced methodological workflows, from sample collection to data analysis, and addresses key troubleshooting and optimization challenges for sensitive minimal residual disease (MRD) detection. Finally, it critically validates RT-qPCR performance against other technologies and through large-scale clinical studies, offering a roadmap for its integration into precision medicine and future cancer diagnostics.
The Foundation of RT-qPCR in Liquid Biopsy: Principles and Biomarker Discovery
Liquid biopsy has emerged as a transformative approach in oncology, providing a minimally invasive alternative to traditional tissue biopsies for cancer detection, monitoring, and treatment selection. This technical guide explores the core components of liquid biopsy—including circulating tumor cells (CTCs), circulating tumor DNA (ctDNA), and extracellular vesicles (EVs)—and their applications within cancer research and clinical practice. By enabling real-time monitoring of tumor dynamics and overcoming the limitations of tissue biopsy, liquid biopsy represents a paradigm shift in cancer management. Particular emphasis is placed on the role of RT-qPCR methodologies in advancing liquid biopsy applications, with detailed experimental protocols and reagent solutions provided for research implementation.
Liquid biopsy represents a minimally invasive approach for analyzing tumor-derived components from peripheral blood or other bodily fluids. Unlike traditional tissue biopsy, which remains the gold standard for tumor diagnosis due to high laboratory standardization and accuracy, liquid biopsy provides distinct advantages including non-invasive sampling, capability for repeated monitoring, and comprehensive representation of tumor heterogeneity [1]. The concept has evolved through four distinct developmental phases: the period of scientific exploration (before the 1990s), scientific development (1990s), industrial growth (2000-2010), and industrial outbreak (2010-present) [1].
The foundational discoveries underlying liquid biopsy date back to 1869 when Australian physician Thomas Ashworth first observed cells resembling tumor cells in the blood of a deceased cancer patient [1]. In 1948, Mandel and Metais made the groundbreaking discovery of cell-free nucleic acids in plasma, followed by Leon et al.'s 1977 observation that plasma-free DNA levels were significantly elevated in cancer patients compared to healthy individuals [1]. The modern era of liquid biopsy began with the first isolation of CTCs from blood in 1998, demonstrating correlation with pathological staging, and the 1994 identification of KRAS mutations in pancreatic cancer patients' blood cfDNA that matched tumor tissue findings [1]. The field has since accelerated rapidly, with regulatory approvals including the 2014 EMA authorization of ctDNA for EGFR mutation detection in non-small cell lung cancer and the 2018 incorporation of CTC testing into AJCC guidelines for breast cancer prognostic assessment [1].
Key Biomarkers in Liquid Biopsy
Circulating Tumor Cells (CTCs)
CTCs are cells released from primary and metastatic tumors that enter the bloodstream or lymphatic circulation [1]. Although extremely rare in peripheral blood (approximately 1 CTC per 1 million leukocytes), with most surviving only 1-2.5 hours in circulation, CTCs provide vital information about cancer biology and metastatic potential [1]. The detection and analysis of CTCs face significant technical challenges due to their scarcity, requiring highly sensitive capture methodologies including density gradient centrifugation, immunomagnetic separation (such as the FDA-approved CellSearch system), and microfluidic devices targeting surface markers like epithelial cell adhesion molecule (EpCAM), vimentin, and N-cadherin [1]. Clinically, CTC enumeration has demonstrated prognostic value, with higher counts correlating with reduced progression-free survival and overall survival in multiple cancer types [1].
Circulating Tumor DNA (ctDNA)
CtDNA comprises tumor-derived fragmented DNA circulating in bloodstream, typically representing 0.1-1.0% of total cell-free DNA (cfDNA) [1]. Unlike cfDNA from normal leukocytes and stromal cells, ctDNA fragments are shorter (approximately 20-50 base pairs) and exhibit a shorter half-life, enabling real-time monitoring of tumor dynamics [1]. CtDNA can be isolated from various sources including blood, ascites, pleural fluid, urine, and cerebrospinal fluid, providing flexibility in sampling approaches [1]. The detection of tumor-specific genetic alterations in ctDNA, such as mutations in APC, KRAS, TP53, and PIK3CA genes, allows for monitoring of treatment response and disease progression, as demonstrated in studies of colorectal cancer patients where ctDNA mutation rates correlated with therapeutic response [1].
Extracellular Vesicles (EVs) and Other Biomarkers
Extracellular vesicles, including exosomes, represent membrane-bound particles released by cells that carry molecular cargo including proteins, lipids, and nucleic acids [1]. First observed in 1967 and characterized as exosomes in 1983, EVs have demonstrated biological activity including antigen presentation capabilities [1]. Beyond CTCs, ctDNA, and EVs, the liquid biopsy biomarker landscape includes microRNAs, circulating free RNA (cfRNA), tumor-educated platelets (TEPs), and tumor endothelial cells, creating a multi-parametric approach to cancer detection and monitoring [2]. Each biomarker class offers complementary information, with integrated approaches demonstrating enhanced sensitivity and specificity for disease monitoring [2].
Table 1: Comparison of Major Liquid Biopsy Biomarkers
| Biomarker | Composition | Primary Sources | Key Features | Research Applications |
|---|---|---|---|---|
| CTCs | Intact tumor cells | Peripheral blood | Rare population (1 per 10^6 WBCs), short half-life (1-2.5 hours) | Prognostic assessment, metastasis research, drug response monitoring |
| ctDNA | Tumor-derived DNA fragments | Blood, urine, CSF, ascites | Short fragments (20-50 bp), 0.1-1.0% of total cfDNA | Mutation detection, treatment response monitoring, MRD assessment |
| EVs/Exosomes | Membrane-bound vesicles with molecular cargo | Blood, urine | Stable in circulation, carry proteins, RNA, DNA | Biomarker discovery, intercellular communication studies |
| cfRNA | Cell-free RNA including mRNA, miRNA | Blood, urine | Reflects gene expression patterns | Gene expression profiling, treatment response biomarkers |
Current Applications and Recent Advances
Liquid biopsy applications span the cancer care continuum, from early detection to monitoring treatment response and disease recurrence. Recent research presented at the AACR Annual Meeting 2025 highlights significant advancements in three primary areas: screening/detection, minimal residual disease (MRD) monitoring, and prediction/prognostication [3].
Screening, Detection, and Diagnosis
Multi-cancer early detection (MCED) platforms represent one of the most promising applications of liquid biopsy. The Vanguard Study, part of the NCI Cancer Screening Research Network, demonstrated feasibility of implementing MCED tests in real-world settings, enrolling over 6,200 participants with high adherence across diverse populations [3]. Technological advances include methylation-based approaches, with one hybrid-capture methylation assay demonstrating 98.5% specificity and 59.7% overall sensitivity (increasing to 84.2% in late-stage tumors) [3]. Fragmentomics approaches using low-coverage whole genomic sequencing have shown remarkable accuracy in detecting liver conditions, distinguishing cirrhosis and hepatocellular carcinoma from healthy states with an AUC of 0.92 in a 724-person cohort [3]. Additionally, proteomic analyses within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort identified 19 circulating plasma proteins associated with premenopausal breast cancer risk and three proteins (LEG1, CST6, SAR1B) with postmenopausal risk, enabling improved risk stratification [3].
Minimal Residual Disease (MRD) Monitoring
MRD detection through liquid biopsy provides critical insights into treatment efficacy and early recurrence detection. In colorectal cancer, the VICTORI study demonstrated that 87% of recurrences were preceded by ctDNA positivity, while no ctDNA-negative patients relapsed [3]. In bladder cancer, the TOMBOLA trial compared ddPCR and whole-genome sequencing for ctDNA detection in 1,282 paired plasma samples, revealing 82.9% concordance between methods, with ddPCR showing higher sensitivity in low tumor fraction samples [3]. Novel technologies such as MUTE-Seq (Mutation tagging by CRISPR-based Ultra-precise Targeted Elimination in Sequencing) enable ultrasensitive detection of low-frequency mutations in cfDNA through engineered advanced-fidelity FnCas9, significantly improving sensitivity for MRD evaluation in NSCLC and pancreatic cancer [3].
Prediction and Prognostication
Liquid biopsy biomarkers demonstrate significant utility for predicting treatment response and patient prognosis. In metastatic prostate cancer, morphological evaluation of chromosomal instability in CTCs (CTC-CIN) from the CARD trial showed that high baseline CTC-CIN counts were significantly associated with worse overall survival, while low CTC-CIN predicted greater benefit from cabazitaxel treatment [3]. Combined tissue and liquid biopsy approaches have demonstrated improved outcomes, with an exploratory analysis of the ROME trial showing that despite only 49% concordance between modalities, combining both significantly increased detection of actionable alterations and improved survival outcomes in patients receiving tailored therapy [3]. In NSCLC, baseline detection of EGFR mutations in plasma, particularly at variant allele frequency >0.5%, was prognostic for significantly shorter PFS and OS in patients treated with osimertinib [3].
Table 2: Recent Advancements in Liquid Biopsy Applications (AACR 2025 Highlights)
| Application Area | Study/Technology | Cancer Type | Key Findings |
|---|---|---|---|
| Early Detection | Vanguard Study | Multi-cancer | Established feasibility in 6,200 participants; high adherence across diverse populations |
| Early Detection | MCED Methylation Assay | Multi-cancer | 98.5% specificity, 59.7% overall sensitivity (84.2% in late-stage tumors) |
| MRD Monitoring | VICTORI Study | Colorectal Cancer | 87% of recurrences preceded by ctDNA positivity; no ctDNA-negative patients relapsed |
| MRD Monitoring | MUTE-Seq | NSCLC, Pancreatic | Ultrasensitive detection of low-frequency mutations via engineered FnCas9 |
| Prediction/Prognosis | CTC-CIN Analysis | Metastatic Prostate | High CTC chromosomal instability associated with worse OS; predicts taxane benefit |
| Prediction/Prognosis | ROME Trial Analysis | Advanced Solid Tumors | Combined tissue/liquid biopsy increased actionable alterations detection and improved survival |
RT-qPCR Methodologies in Liquid Biopsy Analysis
Experimental Workflow for Multi-Parametric Liquid Biopsy Analysis
Reverse transcription quantitative PCR (RT-qPCR) represents a cornerstone technology for analyzing gene expression patterns in liquid biopsy components, particularly CTCs and EVs. A comprehensive protocol for longitudinal multi-parametric liquid biopsy analysis involves blood collection, component separation, nucleic acid isolation, and molecular analysis [2].
Sample Collection and Processing: Approximately 18mL of blood is collected in EDTA tubes and stored briefly at 4°C before processing. CTCs are isolated via positive immunomagnetic selection targeting surface markers including EpCAM, EGFR, and HER2. The remaining blood undergoes centrifugation at 1841× g for 8 minutes to obtain plasma, which is stored at -80°C. EVs are isolated from 4mL of prefiltered (0.8µm pore size) plasma using affinity-based binding to spin columns. Cell-free DNA is isolated from plasma using affinity-based binding to magnetic beads, with quantification performed via chip-based systems assessing fragments between 100-700bp [2].
RNA Isolation and cDNA Synthesis: Total RNA is isolated from EVs using commercial kits, while mRNA is isolated from CTC lysates and vesicular RNA eluates using Oligo(dT)25 beads followed by reverse transcription to generate cDNA [2].
RT-qPCR Analysis: Multi-marker RT-qPCR is performed using customized panels targeting cancer-relevant transcripts (e.g., AKT2, ALK, AR, AURKA, BRCA1, EGFR, ERCC1, ERBB2, ERBB3, KIT, KRT5, MET, MTOR, NOTCH1, PARP1, PIK3CA, SRC). The process involves transcript-specific multiplex pre-amplification followed by SYBR green-based qPCR in single-plex reactions. Melting curve analysis ensures amplicon specificity, with controls for PCR inhibition and contamination. Data evaluation normalizes transcripts not exclusively expressed in CTCs to the leukocyte-specific CD45 transcript, with expression data normalized to healthy donor controls and analyzed binarily (overexpression yes/no) [2].
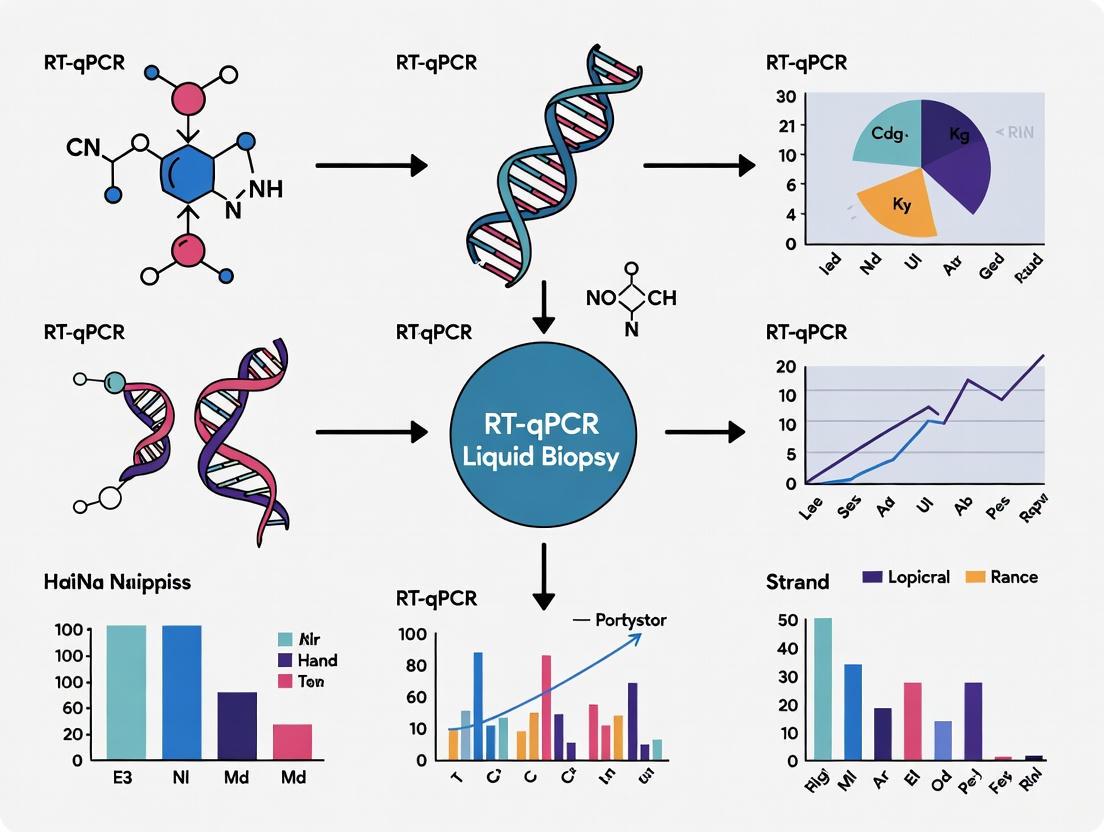
Diagram 1: Multi-Parametric Liquid Biopsy Workflow
Key Research Reagent Solutions
Table 3: Essential Research Reagents for Liquid Biopsy RT-qPCR Analysis
| Reagent/Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Blood Collection Tubes | EDTA tubes | Prevents coagulation and preserves blood components | Process within 4 hours of collection; store at 4°C |
| CTC Isolation Kits | AdnaTest EMT-2/StemCell Select | Immunomagnetic selection targeting EpCAM, EGFR, HER2 | Enriches tumor cells while depleting hematopoietic cells |
| EV Isolation Kits | exoRNeasy Kit | Affinity-based binding to spin columns | Prefiltration (0.8µm) removes larger particles; preserves EV integrity |
| RNA Extraction Kits | exoRNeasy Kit, QIAamp MinElute | Isolation and purification of nucleic acids | Oligo(dT)25 beads for mRNA selection from CTCs and EVs |
| Reverse Transcription Kits | AdnaTest EMT-2/StemCell Detect | cDNA synthesis from mRNA templates | Includes necessary controls for reaction efficiency |
| qPCR Master Mixes | SYBR green-based systems | Amplification and detection of target sequences | Enables melting curve analysis for amplicon verification |
| Gene Expression Panels | AdnaTest TNBC Panel prototype | Multi-marker analysis of cancer-relevant transcripts | Analyzes 17+ transcripts including AKT2, ALK, AR, AURKA, BRCA1, EGFR |
| Quality Controls | Artificial RNA spikes, negative controls | Monitoring PCR inhibition and contamination | Essential for validating assay performance and specificity |
Data Analysis and Interpretation
For CTC and EV mRNA profiling, data evaluation follows established protocols where transcripts not exclusively expressed in CTCs are normalized to the leukocyte-specific CD45 transcript. Patient expression data is normalized to matched healthy donor controls, with signals analyzed binarily (overexpression present/absent) [2]. In cfDNA analysis, targeted next-generation sequencing panels assess mutational status in key cancer genes, with variant allele frequency (VAF) dynamics providing insights into treatment response and resistance mechanisms [2]. A longitudinal study in metastatic breast cancer demonstrated that fluctuations in EV ERCC1 signals correlated with progressive disease (97% specificity), while allele frequency developments of ESR1 and PIK3CA variants predicted therapy success and could guide treatment decisions [2].
Diagram 2: Liquid Biopsy Data Analysis Pathway
Liquid biopsy has fundamentally expanded the diagnostic and monitoring capabilities in oncology, offering solutions to longstanding limitations of tissue biopsy. The multi-analyte approach—encompassing CTCs, ctDNA, EVs, and other biomarkers—provides complementary information that enables comprehensive assessment of tumor dynamics. RT-qPCR methodologies represent robust, accessible tools for implementing liquid biopsy analyses in research settings, particularly for gene expression profiling in CTCs and EVs. As technological innovations continue to enhance the sensitivity and specificity of liquid biopsy platforms, and as standardized protocols emerge for clinical implementation, these approaches promise to further transform cancer management through personalized, dynamic monitoring of disease progression and treatment response.
Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) is a cornerstone molecular technique that enables the sensitive, specific, and quantitative detection of RNA targets. This guide details the core principles of RT-qPCR, from its fundamental workflow and chemistry to its critical data analysis methods. Framed within the context of liquid biopsy for cancer research, we explore how this powerful technique is employed to detect and quantify minute amounts of tumor-derived nucleic acids, such as circulating tumor RNA, facilitating advancements in cancer diagnosis, monitoring, and personalized therapy.
Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) is a powerful molecular technique that combines the reverse transcription of RNA into complementary DNA (cDNA) with the simultaneous amplification and quantification of a specific DNA target [4] [5]. It has become an indispensable tool in molecular biology and clinical diagnostics, particularly in the field of cancer research using liquid biopsies.
The process begins with RNA extracted from a biological sample, such as blood plasma in a liquid biopsy. This RNA, which may include circulating tumor RNA or other cancer-associated transcripts, is first converted into stable cDNA using the enzyme reverse transcriptase [4]. The cDNA then serves as the template for the qPCR step, where a target sequence is amplified exponentially and monitored in real-time using fluorescent reporter molecules [6]. The ability to focus on the exponential phase of the PCR reaction, where amplification is most efficient and consistent, is a key reason for the technique's precision and wide dynamic range [6].
In liquid biopsy-based cancer research, RT-qPCR's exceptional sensitivity allows for the detection of rare RNA biomarkers present in complex biological fluids at low concentrations. Its specificity enables the discrimination of closely related transcripts, such as different splice variants or mutant alleles, while its quantitative nature permits researchers to monitor changes in gene expression or pathogen load over time, providing critical insights into tumor dynamics and treatment response [5] [6].
Core Principles and Workflow
The sensitivity of RT-qPCR stems from the synergistic combination of its two core components: reverse transcription and quantitative PCR. The entire process converts a single RNA molecule into a measurable fluorescent signal.
The Reverse Transcription (RT) Step
The foundational first step is the conversion of RNA into complementary DNA (cDNA). This process requires several key reagents [5]:
- Reverse Transcriptase: The enzyme that synthesizes a DNA strand from an RNA template.
- Primers: Short DNA oligonucleotides that provide a starting point for synthesis. The choice of primer dictates which RNA populations are converted to cDNA and can influence sensitivity and specificity [4].
- dNTPs: The building blocks (deoxynucleoside triphosphates) for the nascent cDNA strand.
- MgCl₂: Provides magnesium ions, an essential cofactor for reverse transcriptase activity.
- RNase Inhibitors: Protect the often scarce and fragile RNA templates from degradation.
The RT reaction involves a defined series of steps to ensure complete and accurate cDNA synthesis, outlined in the diagram below.
Priming Strategies for cDNA Synthesis
The method used to prime the reverse transcription reaction is a critical factor influencing the scope and specificity of the resulting cDNA pool, which is especially important when analyzing diverse RNA populations from liquid biopsies [4]. The common priming strategies are:
- Oligo(dT) Primers: These primers, consisting of a stretch of thymine residues, anneal to the poly(A) tail of messenger RNAs (mRNAs). They are ideal for generating a cDNA library enriched for full-length protein-coding transcripts, making them suitable for gene expression studies of mRNA biomarkers [4] [5].
- Random Primers: These are short (6-9 base) oligonucleotides that anneal at multiple points along any RNA transcript. This allows for the reverse transcription of a broad range of RNAs, including non-coding RNAs, degraded RNA, and transcripts without a poly(A) tail, thereby capturing a more comprehensive snapshot of the transcriptome from a liquid biopsy sample [4] [5].
- Gene-Specific Primers: These custom-designed primers target a specific mRNA sequence of interest. This method provides the highest sensitivity and specificity for the target gene and is often used in one-step RT-qPCR protocols. However, it is limited to pre-selected targets [4] [5].
The Quantitative PCR (qPCR) Step
Following cDNA synthesis, the qPCR step amplifies a specific target sequence and monitors its accumulation in real-time. The reaction mixture contains cDNA template, DNA polymerase, sequence-specific primers, dNTPs, and a fluorescent detection system [5]. The process involves thermal cycling, typically consisting of three steps per cycle: denaturation (to separate DNA strands), annealing (to allow primers to bind), and extension (where DNA polymerase synthesizes new strands) [5]. Fluorescence is measured during each cycle, generating an amplification curve.
The core quantitative output of RT-qPCR is the Cycle Threshold (Ct) value. The Ct is the PCR cycle number at which the fluorescent signal crosses a predefined threshold, which is set above the baseline background fluorescence but within the exponential phase of amplification [7] [6]. The Ct value is inversely proportional to the starting quantity of the target: a low Ct value indicates a high initial amount of target RNA, while a high Ct value indicates a low initial amount [5] [7].
One-Step vs. Two-Step RT-qPCR
RT-qPCR can be performed using either a one-step or a two-step approach, each with distinct advantages and applications, particularly in a diagnostic or high-throughput setting.
- One-Step RT-qPCR: The reverse transcription and qPCR reactions are performed sequentially in a single tube. This approach is faster, reduces pipetting steps and the associated risk of contamination, and is ideal for processing large numbers of samples for a limited number of targets [4] [6].
- Two-Step RT-qPCR: The RT and qPCR reactions are performed in separate tubes with individually optimized reaction buffers. The key advantage is flexibility; the stable cDNA product generated in the first step can be stored and used to analyze multiple different targets over time [4] [6]. This is beneficial when studying the expression of many genes from a single, precious liquid biopsy sample.
Table 1: Comparison of One-Step and Two-Step RT-qPCR Methods
| Feature | One-Step RT-qPCR | Two-Step RT-qPCR |
|---|---|---|
| Workflow | RT and qPCR in a single tube | RT and qPCR in separate tubes |
| Throughput | Suitable for high-throughput | Less suitable for high-throughput |
| Flexibility | Low; cDNA cannot be stored/re-used | High; cDNA can be used for multiple assays |
| Risk of Contamination | Lower | Higher |
| Optimization | Compromise conditions for both steps | Individual optimization for each step |
| Ideal For | Screening a few targets in many samples | Analyzing many targets from a single sample |
Detection Chemistries and Their Mechanisms
The real-time quantification in qPCR relies on fluorescent chemistries that report the accumulation of amplified DNA. The choice of chemistry involves a trade-off between specificity, cost, and multiplexing capability.
DNA-Binding Dyes
The simplest and most cost-effective chemistry involves fluorescent dyes that bind non-specifically to double-stranded DNA (dsDNA). SYBR Green is the most common example; it emits minimal fluorescence when free in solution but exhibits a strong fluorescent signal upon binding to the minor groove of dsDNA [5] [6]. The fluorescence increases as the amount of PCR product increases with each cycle.
- Advantage: Inexpensive and easy to use; no need for a specific probe.
- Disadvantage: Lack of inherent specificity; the dye will bind to any dsDNA, including non-specific amplification products and primer-dimers, which can lead to false-positive signals [6]. This necessitates the use of a melt curve analysis post-amplification to verify the identity of the PCR product.
Sequence-Specific Probes
These chemistries provide a higher level of specificity by using an oligonucleotide probe that is complementary to the target sequence. The TaqMan Probe system is the gold standard.
- Mechanism: A TaqMan probe is labeled with a fluorescent reporter dye at one end and a quencher molecule at the other. When intact, the quencher suppresses the reporter's fluorescence via Fluorescence Resonance Energy Transfer (FRET). During the PCR extension phase, the DNA polymerase's 5' to 3' exonuclease activity cleaves the probe, separating the reporter from the quencher and resulting in a permanent increase in fluorescence that is proportional to the target amplification [8] [6].
- Advantage: High specificity, as fluorescence requires both correct primer binding and probe hybridization. Enables multiplexing—the detection of multiple targets in a single reaction by using probes labeled with different colored fluorophores [6].
Table 2: Key Detection Chemistries for qPCR
| Chemistry | Mechanism of Action | Specificity | Multiplexing Potential |
|---|---|---|---|
| SYBR Green | Binds non-specifically to dsDNA | Low | None |
| TaqMan Probe | Relies on probe hydrolysis by DNA polymerase | High | High (with different dyes) |
Achieving Sensitivity: Key Experimental Considerations
The renowned sensitivity of RT-qPCR is not automatic; it is achieved through meticulous optimization of several experimental parameters.
Primer and Probe Design
Proper design of primers and probes is paramount for specific and efficient amplification. Key principles include [4] [5]:
- Exon-Exon Spanning: Primers should be designed to span an exon-exon junction. This ensures that the cDNA amplicon is shorter than any potential genomic DNA contaminant, preventing false positives from gDNA [4].
- Amplicon Length: Optimal amplicon length is typically between 70-200 base pairs. Shorter amplicons amplify with higher efficiency, which is critical for detecting low-abundance targets [5].
- GC Content and Secondary Structure: Primers should have a GC content of 40-60% and be checked to avoid self-complementarity or stable secondary structures that can hinder annealing and reduce efficiency [5].
- PCR Efficiency: This is a measure of how perfectly the reaction proceeds, with 100% efficiency representing a perfect doubling every cycle. The efficiency of an assay should ideally be between 90-110% [7] [6]. Efficiency can be calculated from a standard curve generated using a dilution series, using the formula: Efficiency (%) = (10^(-1/slope) - 1) x 100 [7].
Controls and Normalization
Robust experimental design requires appropriate controls to ensure data integrity.
- No-RT Control: A control reaction that includes all components except the reverse transcriptase. This is essential for identifying false-positive signals caused by contaminating genomic DNA in the RNA sample [4].
- Normalization with Reference Genes: To account for variations in RNA input, quality, and cDNA synthesis efficiency, the expression of the target gene must be normalized to that of stable, constitutively expressed reference genes (e.g., GAPDH, ACTB). This allows for meaningful comparisons between different samples [7] [6].
Application in Liquid Biopsy for Cancer Research
Liquid biopsy—the analysis of tumor-derived components in bodily fluids like blood—has emerged as a transformative, non-invasive approach in oncology. RT-qPCR plays a vital role in detecting and quantifying RNA-based biomarkers in these samples.
Liquid biopsies encompass a range of analytes, including circulating tumor cells (CTCs), circulating tumor DNA (ctDNA), and extracellular vesicles (EVs), which carry nucleic acids including RNA [1] [9]. RT-qPCR is exquisitely suited to analyze the RNA content from these sources. For example, it can be used to:
- Detect circulating microRNAs (miRNAs) that are dysregulated in cancer [1].
- Quantify the expression of drug target genes or resistance markers from circulating EVs or CTCs [9].
- Monitor minimal Residual Disease (MRD) by detecting transcripts specific to a particular cancer type after treatment [10].
The following diagram illustrates how RT-qPCR is integrated into a typical liquid biopsy research workflow for cancer biomarker analysis.
The technique's high sensitivity is crucial here, as it allows for the detection of extremely rare RNA molecules shed by tumors into the bloodstream against a high background of normal cellular RNA. Furthermore, the quantitative nature of RT-qPCR enables researchers to track dynamic changes in these biomarker levels over time, providing a real-time view of tumor response to therapy or the emergence of resistance [1] [9].
Advanced Multiplexing Strategies
The need to analyze multiple biomarkers simultaneously from a limited liquid biopsy sample has driven the development of advanced multiplexing strategies. While traditional multiplex qPCR is limited by the number of distinct fluorescent channels available on the instrument, novel approaches are pushing these boundaries.
One innovative method is Amplitude Modulation. This technique allows for the detection of multiple targets in a single fluorescent channel by assigning each target a unique concentration of its respective TaqMan probe. Because the final fluorescent intensity is proportional to the probe concentration, each combination of present targets generates a distinct endpoint fluorescence "signature." This method has been demonstrated to accurately detect up to nine different targets across three color channels, significantly expanding the multiplexing capacity of standard RT-qPCR instruments without requiring new hardware or chemistry [8].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for RT-qPCR in Liquid Biopsy Research
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| Reverse Transcriptase | Enzyme that synthesizes cDNA from an RNA template. | Choose enzymes with high thermal stability for GC-rich transcripts or those with secondary structure [4]. |
| DNA Polymerase | Enzyme that amplifies the cDNA target during qPCR. | Hot-start enzymes are preferred to reduce non-specific amplification [5]. |
| Fluorescent Probes (TaqMan) | Provide sequence-specific detection of the amplified target. | Essential for multiplexing; requires individual optimization of probe concentrations [8] [6]. |
| Fluorescent Dyes (SYBR Green) | Bind non-specifically to double-stranded DNA. | Cost-effective; requires post-amplification melt curve analysis to verify specificity [6]. |
| Sequence-Specific Primers | Define the region of the cDNA to be amplified. | Must be designed for high specificity and efficiency (90-110%); should span exon-exon junctions where possible [4] [5]. |
| dNTPs | Nucleotide building blocks for cDNA and new DNA strands. | |
| RNase Inhibitors | Protect RNA templates from degradation during the RT reaction. | Critical for working with low-input or degraded samples from liquid biopsies [5]. |
| Reference Gene Assays | Used to normalize target gene expression to a stably expressed gene. | Vital for accurate quantification; stability of reference genes must be validated for the sample type under investigation [6]. |
Liquid biopsy has emerged as a revolutionary, non-invasive approach for cancer detection and monitoring, presenting a compelling alternative to traditional tissue biopsies. By analyzing tumor-derived components circulating in various bodily fluids such as blood, this technique provides a dynamic window into tumor biology and heterogeneity [1] [11]. Among these components, RNA biomarkers—particularly messenger RNA (mRNA), microRNA (miRNA), and other forms of circulating RNA—have gained significant prominence due to their stability in extracellular environments and the rich biological information they encode [12] [13]. Their detection and quantification via Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) offer a highly sensitive, specific, and accessible method for researchers and clinicians engaged in cancer diagnostics and therapeutic monitoring.
The application of RT-qPCR in profiling these RNA biomarkers facilitates early cancer detection, real-time monitoring of treatment efficacy, assessment of emerging drug resistance, and detection of minimal residual disease [14] [15] [12]. This technical guide provides an in-depth examination of the core RNA biomarkers used in RT-qPCR-based liquid biopsy analyses, detailing their characteristics, methodological protocols, and practical applications within oncological research and drug development.
microRNA (miRNA) as Biomarkers
Biology and Significance
MicroRNAs (miRNAs) are short, non-coding RNA molecules typically 18–25 nucleotides in length that play a fundamental role in the post-transcriptional regulation of gene expression [14] [13]. They function by binding to complementary sequences in the 3' or 5' untranslated regions (UTRs) of target messenger RNAs (mRNAs), leading to mRNA degradation or translational repression [14]. The discovery of the first miRNA, Lin-4, in Caenorhabditis elegans in 1993 by Victor Ambros and colleagues reshaped the scientific understanding of gene regulation [14]. This was followed by the identification of Let-7, which is evolutionarily conserved across species, including humans [14]. The significance of miRNAs in cancer biology was firmly established by a pioneering study revealing that miR-15a and miR-16-1 are often deleted or down-regulated in chronic lymphocytic leukaemia (CLL), leading to increased expression of the anti-apoptotic protein BCL-2 [14].
The exceptional stability of circulating miRNAs in biofluids, despite the presence of endogenous RNases, makes them particularly attractive as biomarkers [14] [12]. This stability is conferred through their association with various carriers that protect them from degradation. These carriers include extracellular vesicles (EVs) such as exosomes and microvesicles; protein complexes with Argonaute 2 (AGO2) or nucleophosmin 1 (NPM1); and lipoproteins such as high-density lipoprotein (HDL) [12] [13]. This robust stability, coupled with their disease-specific expression patterns, underpins their utility as sensitive and reliable biomarkers in liquid biopsy [12].
Experimental Protocol for miRNA Analysis
Workflow: RT-qPCR Analysis of Circulating miRNA
The analysis of circulating miRNAs via RT-qPCR requires meticulous sample handling and specialized reagents to accurately quantify these small RNA molecules. The protocol begins with sample collection and stabilization. Blood samples should be collected in EDTA or citrate tubes (heparin is avoided as it can inhibit PCR) and processed within 2 hours of collection to minimize cellular RNA contamination and miRNA degradation [12]. Plasma or serum is obtained via centrifugation, typically at 1,500-2,000 × g for 10 minutes to remove cells, followed by a higher-speed centrifugation (e.g., 12,000-16,000 × g for 15 minutes) to eliminate residual platelets and cell debris [12]. The resulting supernatant (plasma/serum) should be aliquoted and stored at -80°C. The inclusion of RNase inhibitors at this stage is recommended to preserve RNA integrity.
RNA extraction is most commonly performed using phenol-chloroform-based methods (e.g., TRIzol LS) followed by purification with silica-based columns specifically designed for small RNA isolation. These columns typically have pore sizes that retain small RNAs below 200 nucleotides. Commercially available kits such as the miRNeasy Serum/Plasma Kit (Qiagen) or the miRCURY RNA Isolation Kit (Bio-Rad) are optimized for this purpose. To account for extraction efficiency variations, the introduction of a non-human synthetic spike-in control (e.g., C. elegans miR-39) is essential and should be added to the lysis buffer at the beginning of the extraction process [12].
For the reverse transcription step, stem-loop RT primers are the gold standard for miRNA analysis. These primers have a short region that binds to the 3' end of the mature miRNA and a universal stem-loop structure. This design creates a longer, extended cDNA product that provides a more specific template for the subsequent qPCR, overcoming the challenge posed by the short length of mature miRNAs. The reaction utilizes reverse transcriptase enzymes with high processivity and the ability to reverse transcribe structured RNA.
The qPCR amplification can be performed using specific TaqMan miRNA assays, which employ a miRNA-specific forward primer, a universal reverse primer, and a TaqMan probe with a fluorophore and quencher. Alternatively, SYBR Green-based systems with specifically designed primers can be used, though they may require meticulous optimization to ensure specificity. The quantification cycle (Cq) values are obtained, and relative quantification is performed using the comparative ΔΔCt method. Normalization is critical and can be achieved using the spiked-in synthetic controls (e.g., cel-miR-39) or a combination of endogenous stable miRNAs identified in the specific sample matrix (e.g., miR-16-5p, miR-484) [12]. The selection of appropriate reference genes must be empirically validated for the specific sample set and cancer type under investigation.
Table 1: Key miRNA Biomarkers in Cancer Detection and Monitoring
| miRNA | Cancer Type | Expression Change | Potential Clinical Utility | Supporting Evidence |
|---|---|---|---|---|
| miR-21 | Breast Cancer, Lung Cancer, Melanoma | Upregulated | Diagnosis, Prognosis, Therapeutic Resistance | Prevalent in multiple cancer types; acts as an "oncomiR" [12] |
| miR-145 | Breast Cancer, Lung Cancer | Downregulated | Tumor Suppressor, Early Detection | Frequently downregulated in carcinomas [12] |
| miR-205-5p | Pancreatic Cancer | Upregulated | Early Detection (vs. chronic pancreatitis) | 91.5% accuracy distinguishing cancer from pancreatitis [14] |
| miR-1247-5p, miR-301b-3p, miR-105-5p | Non-Small Cell Lung Cancer (NSCLC) | Upregulated | Diagnostic Panel | AUCs of 0.769, 0.761, and 0.777, respectively [14] |
| miR-29c | Melanoma | Downregulated | Diagnostic (vs. other cancers) | Distinguishes melanoma from metastatic colon/renal cancer [13] |
| MEL38 Signature | Melanoma | Specific Signature | Diagnostic and Prognostic Panel | 93% sensitivity, 98% specificity for invasive melanoma [13] |
Messenger RNA (mRNA) as Biomarkers
Biology and Significance
Messenger RNA (mRNA) serves as the intermediary template for protein synthesis, carrying genetic information from DNA in the nucleus to the ribosomes in the cytoplasm. In the context of liquid biopsy, the presence of circulating mRNA fragments, often encapsulated within extracellular vesicles or bound to protective proteins, provides a snapshot of the active gene expression profile of tumor cells [11]. The analysis of tumor-specific mRNAs in circulation, such as those related to hormone receptors, growth factors, or epithelial-mesenchymal transition (EMT) markers, can offer invaluable insights into tumor subtype, aggressiveness, and potential therapeutic vulnerabilities [15].
A key application in breast cancer research, for instance, involves detecting mRNAs for the estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) from circulating tumor cells (CTCs) or exosomes [15]. This can help monitor dynamic changes in receptor status, a phenomenon known as receptor conversion, which may underlie acquired resistance to targeted therapies [15]. Similarly, the detection of PD-L1 mRNA in EVs or CTCs presents a non-invasive strategy to identify patients who might respond to immunotherapy [15]. However, a significant technical challenge is the inherent instability of cell-free mRNA in plasma due to its susceptibility to ribonucleases, making robust pre-analytical protocols paramount [15].
Experimental Protocol for mRNA Analysis
Workflow: RT-qPCR Analysis of Circulating mRNA
The protocol for mRNA analysis from liquid biopsy samples often requires an initial enrichment step for the mRNA source, such as Circulating Tumor Cells (CTCs) or extracellular vesicles (EVs). CTCs can be isolated from whole blood using platforms like the FDA-cleared CellSearch system (based on EpCAM immunomagnetic enrichment) or microfluidic devices [1]. EVs, including exosomes, can be harvested from plasma or serum via differential ultracentrifugation, density gradient centrifugation, or commercial polymer-based precipitation kits [11].
Following isolation, the RNA extraction process is critical. Due to the fragmented nature of circulating mRNA, total RNA is typically extracted. However, for CTC-derived mRNA, a higher-quality RNA may be obtained. The use of oligo(dT) magnetic beads is highly recommended as they selectively enrich for polyadenylated mRNA, thereby reducing background from non-polyadenylated RNA (like miRNA and ribosomal RNA) and improving the detection sensitivity for protein-coding transcripts.
A DNase treatment step is imperative to remove any contaminating genomic DNA that could lead to false-positive amplification signals. This is typically performed on the column or in solution after RNA extraction.
The reverse transcription reaction should utilize a mix of oligo(dT) primers and random hexamers. Oligo(dT) primers bind to the poly-A tail of eukaryotic mRNAs, ensuring the reverse transcription of full-length or near-full-length transcripts, while random hexamers can prime from any point on the RNA molecule, which is useful for degraded RNA or transcripts that may lack a complete poly-A tail.
For qPCR amplification, TaqMan probe-based chemistry is generally preferred over SYBR Green for its superior specificity, especially when dealing with complex backgrounds and closely related gene family members. The assays must be designed to span exon-exon junctions to prevent amplification from any residual genomic DNA. The amplicon size should be kept relatively short (80-150 bp) to accommodate the typically fragmented nature of circulating RNA.
Data analysis requires careful normalization. When analyzing RNA from isolated CTCs or EVs, classic endogenous housekeeping genes (e.g., GAPDH, ACTB, HPRT1) can be used, but their stability must be rigorously validated in the specific sample context. For cell-free mRNA in plasma, the use of spiked-in synthetic external RNA controls or globally identified stable mRNA references is necessary for reliable relative quantification using the ΔΔCt method.
Table 2: Key mRNA Biomarkers and Their Applications in Liquid Biopsy
| mRNA Target | Cancer Type | Source in Liquid Biopsy | Clinical/Research Application |
|---|---|---|---|
| ER/PR/HER2 | Breast Cancer | CTCs, Exosomes | Monitoring receptor status and therapy resistance [15] |
| PD-L1 | Triple-Negative Breast Cancer (TNBC), Melanoma | CTCs, Exosomes, Plasma | Predicting response to immunotherapy [15] |
| EMT Markers (e.g., Vimentin, N-cadherin) | Various Carcinomas | CTCs | Assessing metastatic potential and aggressiveness [1] |
| TMPRSS2-ERG | Prostate Cancer | CTCs | Subtyping and prognostic stratification |
| B-cell lymphoma 2 (BCL-2) | Chronic Lymphocytic Leukaemia (CLL) | Blood | Linked to apoptotic resistance [14] |
Other Circulating RNA Biomarkers
Beyond miRNA and mRNA, the circulatory landscape contains other RNA species with biomarker potential. Long non-coding RNAs (lncRNAs) and circular RNAs (circRNAs) are gaining attention for their roles in cancer biology and their notable stability in biofluids, often attributed to their circular structure or association with EVs [11]. Furthermore, the total pool of circulating cell-free RNA (cfRNA) can be interrogated for global transcriptomic changes, mutation detection, or fusion transcripts, providing a comprehensive view of the tumor's genetic activity [11]. The protocols for analyzing these molecules often overlap with those for mRNA but may require specific enzymatic treatments or library preparation strategies to capture their unique features (e.g., backsplicing junctions for circRNAs).
The Scientist's Toolkit: Essential Research Reagents
Successful RT-qPCR analysis of RNA biomarkers in liquid biopsy relies on a suite of specialized reagents and tools. The following table details key solutions and their critical functions in the experimental workflow.
Table 3: Essential Research Reagent Solutions for RT-qPCR in Liquid Biopsy
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Blood Collection & Stabilization | EDTA or Citrate Tubes; Cell-Free DNA/RNA Blood Collection Tubes (e.g., Streck, PAXgene) | Prevents coagulation and preserves RNA integrity by stabilizing nucleated blood cells, preventing gene expression changes post-phlebotomy. |
| RNA Extraction | miRNeasy Serum/Plasma Kit (Qiagen); miRCURY RNA Isolation Kit (Bio-Rad); TRIzol LS Reagent | Efficiently isolates high-quality total RNA, including the small RNA fraction (<200 nucleotides), from complex biofluids like plasma and serum. |
| Spike-In Controls | Synthetic C. elegans miRNAs (e.g., cel-miR-39, cel-miR-54, cel-miR-238); External RNA Controls Consortium (ERCC) RNA Spike-Ins | Monitors and corrects for variations in RNA extraction efficiency and reverse transcription efficacy, enabling reliable relative quantification. |
| Reverse Transcription | Stem-Loop RT Primers (for miRNA); Oligo(dT) Primers (for mRNA); Random Hexamers; High-Efficiency Reverse Transcriptase (e.g., MultiScribe) | Generates complementary DNA (cDNA) from RNA templates. Stem-loop primers provide superior specificity and efficiency for short miRNA targets. |
| qPCR Amplification | TaqMan MicroRNA Assays; TaqMan Gene Expression Assays; SYBR Green Master Mix | Enables specific and sensitive quantification of target sequences. TaqMan probes offer higher specificity, crucial for discriminating between homologous sequences. |
| Reference Genes | Endogenous miRNAs (e.g., miR-16-5p, miR-484); Housekeeping mRNAs (e.g., GAPDH, ACTB); Spiked Synthetic RNAs | Used for data normalization to correct for technical variations, ensuring accurate interpretation of target RNA expression levels. |
The integration of mRNA, miRNA, and circulating RNA biomarkers with RT-qPCR technology represents a powerful paradigm in liquid biopsy research. This combination offers a minimally invasive means to obtain critical diagnostic, prognostic, and predictive information, enabling a shift towards personalized cancer management. While challenges remain in standardizing pre-analytical variables, normalizing data, and validating biomarkers across diverse populations, the trajectory of research is clear. As isolation techniques become more refined, detection technologies more sensitive, and bioinformatic analyses more sophisticated, the routine clinical application of RT-qPCR-based RNA biomarker detection is poised to revolutionize cancer care, from early detection to the monitoring of advanced disease. For researchers and drug development professionals, mastering these protocols and understanding the biological context of these biomarkers is essential for driving this transformative field forward.
Quantitative Reverse Transcription PCR (RT-qPCR) stands as a cornerstone technology in molecular diagnostics, offering an unparalleled combination of analytical sensitivity, robust standardization, and cost-efficiency. This technical guide delineates the core advantages of RT-qPCR, with a specific focus on its application in liquid biopsy for cancer detection research. We detail experimental protocols that underpin its performance, provide structured quantitative data comparisons, and visualize key workflows. For the research scientist, this whitepaper serves as a foundational resource, affirming the critical role of RT-qPCR in advancing precision oncology through reliable, scalable, and accessible biomarker analysis.
Liquid biopsy, the analysis of tumor-derived markers in biofluids like blood, has emerged as a transformative approach for cancer diagnosis, prognosis, and therapy monitoring. Within this field, RNA biomarkers—including microRNAs (miRNAs), messenger RNAs (mRNAs), and other non-coding RNAs—offer profound insights into the tumor's molecular state [16] [17]. The detection of these biomarkers, however, is technically challenging due to their low abundance and the complex background of clinical samples. RT-qPCR has established itself as a preeminent method for this task. Its unique value proposition lies in its ability to deliver a gold-standard level of performance for the sensitive, specific, and quantitative detection of RNA targets, making it indispensable for both foundational research and clinical assay development in oncology [18]. This document elucidates the technical foundations of RT-qPCR's key advantages, framing them within the critical needs of liquid biopsy research.
Core Technical Advantages
The utility of RT-qPCR in liquid biopsy applications is anchored on three principal advantages: exceptional sensitivity, a high degree of standardization, and significant cost-effectiveness.
Superior Sensitivity and Specificity
The ability of RT-qPCR to detect minute quantities of nucleic acid is paramount for liquid biopsies, where targets like cell-free RNA can be present at extremely low concentrations.
- Wide Dynamic Range and Low Limit of Detection (LOD): Advanced one-pot RT-qPCR methods have demonstrated a wide linear dynamic range from 7.5 × 10¹ to 7.5 × 10⁸ copies/reaction, enabling the accurate quantification of target RNA across a vast concentration span, which is essential for monitoring disease progression [16]. The LOD can reach femtomolar concentrations, allowing for the detection of rare RNA transcripts [16].
- Specificity for Sequence Variants: The combination of sequence-specific priming and fluorescent probe systems (e.g., TaqMan hydrolysis probes) allows RT-qPCR to distinguish between closely related miRNA family members or single-nucleotide polymorphisms, which is critical for identifying specific cancer-associated mutations or isoforms [16] [19].
- Performance in Complex Matrices: RT-qPCR reagents have been engineered for robust performance in inhibitory clinical matrices such as plasma, serum, and samples derived from formalin-fixed paraffin-embedded (FFPE) tissue. Next-generation polymerases and optimized buffers mitigate the effects of PCR inhibitors commonly found in these samples, ensuring reliable results [18].
Table 1: Sensitivity and Dynamic Range of RT-qPCR in Biomarker Detection
| Target Type | Reported Linear Dynamic Range (copies/reaction) | Key Application in Liquid Biopsy | Citation |
|---|---|---|---|
| miRNA | 7.5 x 10¹ to 7.5 x 10⁸ | Multiplex detection of cancer biomarkers in serum | [16] |
| mRNA (e.g., PIK3CA) | Comparable performance in diluted blood lysates | SNP analysis and deletion detection from whole blood | [20] |
| SARS-CoV-2 RNA | Detection in direct (no extraction) protocols | Model for rapid, sensitive viral RNA detection | [21] |
Robust Standardization and Reproducibility
The quantitative nature of RT-qPCR demands rigorous standardization to minimize measurement uncertainty and ensure data reproducibility across experiments and laboratories.
- Standardized Data Analysis: Statistical methods have been developed to objectively handle outliers and compare calibration curves, moving beyond subjective visual assessments. The implementation of guidelines for accepting or rejecting statistical outliers, such as those based on ISO 17025, is critical for generating reliable and comparable quantitative data [22].
- Reference Gene Validation: Accurate normalization is the cornerstone of reliable gene expression data. Studies emphasize that the expression of commonly used "housekeeping" genes (e.g., ACTB, GAPDH, RPL13A) can vary significantly under different experimental conditions, such as in dormant cancer cells. It is therefore mandatory to validate reference genes for each specific biological context to prevent significant distortion of gene expression profiles [23].
- Multiplexing Capability: RT-qPCR's strong multiplexing capability allows for the simultaneous detection of multiple clinically relevant RNA targets in a single reaction. This not only conserves precious sample but also ensures that all targets are amplified under identical conditions, improving the internal consistency and reliability of the data. For example, multiplex panels can simultaneously assess alterations in several genes (e.g., EGFR, KRAS, BRAF) from limited liquid biopsy material [18] [24].
Unmatched Cost-Effectiveness and Workflow Efficiency
In an environment of constrained research budgets and the need for scalable testing, the economic and practical advantages of RT-qPCR are significant.
- Low per-Reaction Cost: The cost of RT-qPCR testing is substantially lower than next-generation sequencing (NGS), typically ranging from $50 to $200 per test compared to $300 to $3,000 for NGS. This affordability makes RT-qPCR ideal for large-scale screening initiatives and routine diagnostics [18].
- Rapid Turnaround Time: Unlike sequencing platforms that can take days to generate data, RT-qPCR delivers clinically actionable results within a few hours. This rapid turnaround is crucial for time-sensitive scenarios in research and potential clinical decision-making [18] [21].
- Protocol Simplification and Resource Savings: Recent methodological advances enable further cost and time savings. For instance, the GG-RT PCR method allows for real-time PCR amplification directly from diluted and heat-treated whole blood lysates, eliminating the need for DNA/RNA extraction kits and reducing both cost and processing time [20]. Similarly, direct RT-PCR assays for SARS-CoV-2 that omit the RNA extraction step have maintained high sensitivity (93.9%) while reducing turnaround time and reagent costs [21].
Table 2: Cost and Workflow Comparison of RNA Detection Technologies
| Parameter | RT-qPCR | Next-Generation Sequencing (NGS) | Microarray |
|---|---|---|---|
| Approximate Cost per Test | $50 - $200 | $300 - $3,000 | $100 - $500 |
| Typical Turnaround Time | 2 - 4 hours | 1 - 5 days | 1 - 2 days |
| Sample Throughput | High (96/384-well formats) | High (multiplexed) | Medium to High |
| Ease of Data Analysis | Relatively Simple | Complex, requires bioinformatics | Moderate |
| Best Suited For | Targeted, quantitative analysis of known biomarkers | Discovery, comprehensive transcriptome profiling | Profiling of known, pre-defined transcripts |
Experimental Protocols for Liquid Biopsy Research
The following section outlines detailed protocols that leverage the advantages of RT-qPCR for cancer biomarker detection.
Protocol 1: One-Pot, One-Step Multiplex miRNA RT-qPCR
This novel protocol, mediated by a reverse transcription-hairpin occlusion system (RT-HOS), enables highly specific, one-pot detection of multiple miRNAs, ideal for profiling serum or plasma samples [16].
- Sample Preparation and Lysis: Extract total RNA, including small RNAs, from serum or plasma using a phenol-guanidine-based lysis reagent. Include a spike-in synthetic RNA for normalization to control for extraction efficiency.
- Primer and Reaction Setup: Design and synthesize RT-HOS primers. Each primer functions as a reverse transcription primer, a fluorescent probe (labeled with a 5' fluorophore), and a reverse PCR primer. Combine with a complementary hairpin quencher oligonucleotide.
- Prepare a master mix containing: High-Fidelity or Taq DNA polymerase, dNTPs, reaction buffer, and the RT-HOS primer/hairpin quencher complexes.
- Aliquot the master mix into a qPCR plate and add the RNA template.
- Reverse Transcription and Amplification: Run the one-step reaction on a real-time PCR instrument with the following cycling conditions:
- Reverse Transcription: 50°C for 15-30 minutes (higher temperature enhances specificity).
- Initial Denaturation: 95°C for 2 minutes.
- Amplification (40-50 cycles): Denature at 95°C for 15 seconds, then anneal/extend at 60-65°C for 30-60 seconds (with fluorescence acquisition).
- Data Analysis: Determine Cycle Threshold (Ct) values using the instrument's software. Use a standard curve of synthetic miRNA for absolute quantification or the ΔΔCt method for relative quantification to a validated reference gene.
Protocol 2: Direct RT-qPCR from Whole Blood (GG-RT PCR)
This cost-effective protocol bypasses the nucleic acid extraction step, saving time and resources while being suitable for applications like SNP analysis from blood [20].
- Blood Lysate Preparation:
- Mix 400 µL of EDTA-treated whole blood with 1.6 mL of distilled water (to achieve an ~80% dilution, facilitating cell lysis via osmotic pressure).
- Incubate the mixture at 95°C for 20 minutes, vortexing 2-3 times during incubation.
- Centrifuge at 14,000 rpm for 5 minutes to pellet debris.
- Collect the clear supernatant (lysate) and use it directly as a template, or prepare 1:5 and 1:10 dilutions in water.
- qPCR Reaction Setup:
- Use a SYBR Green I Master Mix.
- In each reaction, combine 2.5 µL of blood lysate (or dilution) with 5 pmol of each sequence-specific primer.
- Ensure amplicons are designed to be small (80-150 bp) for efficient amplification from the complex lysate.
- qPCR Amplification:
- Initial Denaturation: 95°C for 10 minutes.
- Amplification (40 cycles): 95°C for 15 seconds, 60-61°C for 30 seconds (with fluorescence acquisition).
- Post-Amplification Analysis:
- Perform melt curve analysis by incrementally heating the products from 65°C to 95°C while monitoring fluorescence. A single sharp peak confirms specific amplification.
- Compare Ct values to a standard curve generated from samples with known DNA concentrations to determine PCR efficiency.
Visualizing Workflows and Reagent Systems
RT-qPCR Workflow for Liquid Biopsy
The following diagram illustrates the streamlined workflow of RT-qPCR for liquid biopsy analysis, from sample collection to data interpretation.
RT-HOS Primer System for miRNA Detection
This diagram details the mechanism of the RT-HOS primer system, a key innovation for specific, one-pot miRNA detection.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for RT-qPCR in Oncology Research
| Reagent / Material | Critical Function | Technical Notes for Liquid Biopsy |
|---|---|---|
| High-Sensitivity Master Mix | Provides DNA polymerase, dNTPs, buffers, and fluorescence dye/probe system. | Select mixes engineered for inhibitor resistance (e.g., tolerant to heparin, heme) and compatible with multiplexing [18]. |
| RT-HOS Primers & Quenchers | Enable one-pot, one-step multiplex miRNA detection. | HPLC-purified primers are essential for specificity. The system allows reverse transcription at higher temperatures, improving accuracy for short RNA targets [16]. |
| Validated Reference Genes | Serve as endogenous controls for data normalization. | Crucially validate stability in your specific sample type (e.g., plasma, serum) and cancer model. Do not assume standard genes (e.g., ACTB) are stable [23]. |
| RNA Stabilization Reagents | Preserve RNA integrity in blood samples pre-processing. | Prevents degradation of labile RNA biomarkers, ensuring an accurate representation of the in vivo profile. |
| Synthetic RNA Standards | Generate standard curves for absolute quantification. | Allows precise determination of miRNA/mRNA copy numbers per volume of biofluid, critical for longitudinal monitoring [16]. |
RT-qPCR remains an indispensable technology in the arsenal of cancer researchers, particularly in the rapidly advancing field of liquid biopsy. Its trifecta of advantages—exceptional sensitivity capable of detecting low-abundance RNA biomarkers, a highly standardized framework that ensures reproducible and reliable data, and superior cost-effectiveness that enables scalable application—solidifies its status as a gold standard. As innovations in reagent engineering, assay design, and protocol simplification continue to emerge, the utility of RT-qPCR will only expand, further accelerating its role in the discovery, validation, and ultimately, the clinical translation of novel RNA biomarkers for precision oncology.
Liquid biopsy represents a transformative, minimally invasive approach for cancer management, enabling the detection of tumor-derived biomarkers from biofluids such as blood, urine, and cerebrospinal fluid [1]. Unlike traditional tissue biopsies, which provide a snapshot from a single anatomical site, liquid biopsies capture the molecular heterogeneity of tumors and allow for real-time monitoring of disease progression and treatment response [25] [26]. Reverse transcription quantitative polymerase chain reaction (RT-qPCR) has emerged as a cornerstone technology for analyzing RNA biomarkers from liquid biopsies due to its exceptional sensitivity, specificity, quantitative capabilities, and cost-effectiveness [5] [18]. This technical guide provides a comprehensive workflow for implementing RT-qPCR in liquid biopsy cancer detection research, framed within the context of advancing precision oncology.
The application of RT-qPCR in liquid biopsy spans multiple critical areas in cancer research, including the detection of circulating tumor cells (CTCs), analysis of circulating tumor DNA (ctDNA), and profiling of various RNA species such as messenger RNA (mRNA), microRNA (miRNA), and circular RNA (circRNA) [1]. Among these, circRNAs have gained significant attention as promising biomarkers due to their remarkable stability in bodily fluids, a characteristic conferred by their covalently closed-loop structure that confers resistance to exonuclease degradation [25]. This structural stability makes circRNAs exceptionally suitable for the liquid biopsy context, where biomarkers are often present at low concentrations and must withstand variable conditions before analysis.
Liquid Biopsy Sample Collection and Processing
Sample Source Selection
The initial critical step in the liquid biopsy workflow involves selecting the appropriate biofluid source, which significantly impacts biomarker yield and analytical sensitivity. Blood remains the most commonly used source, with plasma being preferred over serum for ctDNA and RNA analyses due to less contamination from genomic DNA released during the clotting process [27] [26]. For cancers located in specific anatomical sites, local biofluids often offer superior biomarker concentration and reduced background noise. Cerebrospinal fluid (CSF) demonstrates enhanced sensitivity for central nervous system tumors, while urine is particularly effective for urological cancers such as bladder cancer, where studies have reported mutation detection sensitivity of 87% in urine versus only 7% in plasma [26]. Saliva and sputum serve as valuable sources for head and neck cancers and lung adenocarcinoma, with studies showing high concordance (93%) in ctDNA detection between saliva and blood samples [27].
Sample Collection and Pre-analytical Processing
Proper sample collection and processing are paramount for preserving nucleic acid integrity and ensuring reliable RT-qPCR results. Blood samples should be collected in specialized tubes containing stabilizers to prevent nucleic acid degradation and processed within a narrow time window to maintain biomarker stability [1]. Plasma separation through centrifugation must be performed carefully to avoid contamination with cellular components. For RNA biomarkers like circRNAs, the exceptional stability conferred by their closed-loop structure provides some protection against degradation, but proper handling remains essential [25]. The following table summarizes key considerations for sample collection from different biofluids:
Table 1: Liquid Biopsy Sample Collection Guidelines for RT-qPCR Analysis
| Biofluid Source | Recommended Collection Tubes | Processing Timeline | Centrifugation Conditions | Primary RNA Biomarkers |
|---|---|---|---|---|
| Blood Plasma | EDTA or specialized cfDNA/RNA tubes | Within 2-4 hours of draw | Dual-centrifugation: 1,600-2,000 × g followed by 10,000-16,000 × g | circRNA, miRNA, mRNA |
| Cerebrospinal Fluid | Sterile collection tubes | Immediate processing preferred | 2,000-3,000 × g for 10 minutes | circRNA, miRNA |
| Urine | Sterile containers with RNA stabilizers | Within 4 hours | 2,000-3,000 × g for 10 minutes | circRNA, mRNA |
| Saliva/Sputum | Containers with RNA stabilizers | Within 2 hours | 2,000-3,000 × g for 10 minutes | circRNA, mRNA |
After processing, samples are typically aliquoted to avoid freeze-thaw cycles and stored at -80°C until nucleic acid extraction. Maintaining a consistent cold chain throughout transportation and storage is critical for preserving RNA integrity, particularly for less stable linear RNA species.
Nucleic Acid Isolation and Quality Control
Extraction Methods for Liquid Biopsy Samples
Nucleic acid extraction from liquid biopsy samples requires specialized protocols optimized for low-abundance targets and challenging sample matrices. For RNA isolation, methods incorporating guanidinium thiocyanate-phenol-chloroform extraction combined with silica membrane-based purification consistently yield high-quality RNA suitable for sensitive RT-qPCR applications [5]. The closed-loop structure of circRNAs provides natural resistance to degradation during extraction, but proper handling remains essential to preserve other RNA species. For comprehensive biomarker analysis, parallel extraction of DNA and RNA from the same sample aliquot enables correlative studies of DNA mutations and RNA expression patterns from a single liquid biopsy specimen.
The extraction process must address several challenges unique to liquid biopsies, including low nucleic acid concentrations, the presence of PCR inhibitors (hemoglobin in blood, mucins in saliva), and the need for high recovery efficiency. Incorporating carrier RNA during extraction can improve yields when working with low-input samples, but may interfere with accurate quantification. For circRNA analysis, protocols often include RNase R treatment to digest linear RNAs and enrich for circular forms, thereby enhancing detection sensitivity for these biomarkers [25].
Quality Assessment and Quantification
Rigorous quality assessment of extracted nucleic acids is essential before proceeding to RT-qPCR analysis. For RNA samples, integrity is typically evaluated using microfluidic capillary electrophoresis systems, which generate RNA Integrity Numbers (RIN) that correlate with amplification efficiency. While circRNAs remain stable despite partial RNA degradation, high-quality total RNA (RIN >7) is recommended for accurate gene expression analysis. Spectrophotometric methods provide concentration measurements but cannot distinguish between intact and degraded RNA or differentiate circRNAs from their linear counterparts.
For liquid biopsy samples with limited material, droplet digital PCR (ddPCR) offers an alternative quantification approach that provides absolute copy number measurements without requiring standard curves. This method is particularly valuable for establishing input amounts for rare biomarker detection. The following table outlines quality control parameters and thresholds for liquid biopsy nucleic acids:
Table 2: Quality Control Standards for Liquid Biopsy Nucleic Acids
| Parameter | Assessment Method | Acceptance Criteria for RT-qPCR | Notes |
|---|---|---|---|
| RNA Concentration | Fluorometric quantification | ≥0.5 ng/μL | Spectrophotometry may overestimate due to contaminants |
| RNA Purity | Spectrophotometry (A260/A280) | 1.8-2.1 | Deviations suggest protein or chemical contamination |
| RNA Integrity | Microfluidic electrophoresis (RIN) | ≥7.0 | circRNAs may be detectable in partially degraded samples |
| circRNA Enrichment | RT-qPCR with divergent primers | ΔCt >5 vs non-enriched | Confirm enrichment after RNase R treatment |
| Genomic DNA Contamination | No-RT control | Ct >35 or undetectable | Indicates need for DNase treatment |
RT-qPCR Experimental Workflow
Reverse Transcription: Converting RNA to cDNA
The reverse transcription (RT) reaction represents a critical first step in RT-qPCR, converting RNA templates into more stable complementary DNA (cDNA) suitable for PCR amplification. This process requires several key reagents: primers to initiate synthesis, reverse transcriptase enzyme, dNTPs as building blocks, MgCl₂ as a cofactor, and RNase inhibitors to protect template RNA [5]. Three primer strategies are commonly employed, each with distinct advantages for liquid biopsy applications. Oligo(dT) primers target the poly(A) tails of mRNAs, generating full-length transcripts but excluding non-polyadenylated RNAs such as some circRNAs. Random primers provide comprehensive coverage of all RNA species by annealing at multiple points along RNA transcripts, making them particularly suitable for detecting diverse RNA biomarkers. Gene-specific primers offer the highest sensitivity for predetermined targets and are ideal when focusing on specific circRNAs or mutations [4].
The RT reaction follows a defined four-step process: (1) denaturation of RNA secondary structures at 65-70°C for 5-10 minutes; (2) primer annealing at optimal temperature; (3) cDNA synthesis at 37-50°C for 30-60 minutes; and (4) reaction termination by enzyme inactivation at 70-85°C [5]. For circRNA analysis, additional considerations include the potential need for specialized reverse transcriptases that can handle highly structured RNA elements and the possible incorporation of RNase R treatment to enrich circular transcripts before reverse transcription.
Quantitative PCR: Amplification and Detection
The qPCR phase amplifies and quantifies specific cDNA targets using sequence-specific primers, DNA polymerase, dNTPs, and fluorescent detection systems [5]. Two primary detection chemistries are employed: intercalating dyes like SYBR Green that bind nonspecifically to double-stranded DNA, and fluorescent probes such as TaqMan probes that provide target-specific detection through fluorescence resonance energy transfer (FRET) mechanisms [5] [4]. Probe-based systems offer superior specificity for liquid biopsy applications where distinguishing closely related sequences or detecting single-nucleotide variants is essential.
Primer design represents perhaps the most critical factor in successful qPCR assay development. For mRNA targets, primers should ideally span exon-exon junctions to prevent amplification of contaminating genomic DNA [4]. For circRNA detection, "divergent" primers that target the unique back-splice junction are essential to specifically amplify circular transcripts while excluding linear isoforms [25]. Optimal primers are typically 18-25 nucleotides in length with GC content of 40-60%, and should be validated for specificity and efficiency using dilution series [5]. The thermal cycling profile consists of initial denaturation (95°C), followed by 30-40 cycles of denaturation (95°C), primer annealing (55-65°C), and extension (72°C), with fluorescence measurement occurring during each cycle [5].
One-Step vs. Two-Step RT-qPCR Protocols
Researchers must choose between one-step and two-step RT-qPCR protocols based on their specific application requirements. In one-step protocols, reverse transcription and qPCR occur in the same tube with a unified buffer system, minimizing pipetting steps and reducing contamination risk [4]. This approach is ideal for high-throughput applications and when analyzing multiple samples for a limited number of targets. Two-step protocols separate the reverse transcription and qPCR reactions, allowing for optimized conditions in each step and enabling the generated cDNA to be used for multiple qPCR assays [4]. This flexibility makes two-step approaches preferable for longitudinal studies or when analyzing each sample for numerous targets.
For liquid biopsy applications, one-step protocols offer advantages in minimizing sample loss during transfer steps, while two-step protocols provide more flexibility for assay optimization and multiple analyses from precious samples. The decision between these approaches should consider sample quantity, number of targets, throughput requirements, and need for assay optimization.
Table 3: Comparison of One-Step vs. Two-Step RT-qPCR Approaches
| Parameter | One-Step RT-qPCR | Two-Step RT-qPCR |
|---|---|---|
| Workflow Efficiency | Combined reaction in single tube | Separate reactions in different tubes |
| Hands-on Time | Minimal pipetting steps | Additional transfer steps required |
| Sample Consumption | Lower - single reaction uses less sample | Higher - multiple reactions from same cDNA |
| Optimization Flexibility | Limited - compromised conditions for both reactions | High - independent optimization of RT and qPCR |
| Contamination Risk | Reduced - closed tube system | Increased - multiple open tube steps |
| cDNA Archive | Not possible - immediate amplification | Stable cDNA bank for future analyses |
| Ideal Application | High-throughput targeted screening | Multiple targets from limited samples |
Data Analysis and Interpretation
Quantification Methods and Normalization
RT-qPCR data analysis centers on the cycle threshold (Ct) value, which represents the amplification cycle at which the fluorescence signal exceeds a defined threshold [5]. Low Ct values indicate high target abundance, while high Ct values reflect low abundance. Two primary quantification approaches are employed: absolute quantification, which determines exact copy numbers using a standard curve of known concentrations, and relative quantification, which compares expression levels between samples using reference genes for normalization [5]. For most liquid biopsy applications, relative quantification is preferred due to challenges in creating accurate standards for rare biomarkers.
Proper normalization is essential for meaningful RT-qPCR results, particularly in liquid biopsy where sample input may vary. Reference genes (often called housekeeping genes) should be carefully selected based on stable expression across sample types and experimental conditions. For circRNA analysis, normalization approaches may include using stable linear RNAs as references or spike-in synthetic circRNAs to control for extraction efficiency. The ΔΔCt method is widely used for relative quantification, calculating expression fold changes based on differences in Ct values between target and reference genes [5].
Quality Control and Validation
Robust quality control measures are essential for generating reliable liquid biopsy data. Each RT-qPCR experiment should include multiple controls: no-template controls to detect contamination, no-reverse transcription controls to assess genomic DNA contamination, and positive controls to verify reaction efficiency [4]. Amplification efficiency should be calculated from standard curves and fall within 90-110% for optimal results, with correlation coefficients (R²) >0.98 indicating a strong linear relationship [5].
For circRNA detection, additional validation is crucial to confirm circular nature rather than linear isoforms. This may include RNase R treatment resistance assays, Sanger sequencing of back-splice junctions, or comparison with linear transcript detection using convergent primers. In cancer biomarker applications, establishing clinical thresholds is particularly important, often requiring receiver operating characteristic (ROC) curve analysis to determine Ct values that optimally distinguish patient groups [25].
Applications in Cancer Research and Biomarker Development
circRNA Biomarkers in Drug Resistance Monitoring
Circular RNAs have emerged as particularly promising biomarkers for monitoring therapy response and detecting emergent drug resistance in cancer. Their stability, abundance in body fluids, and functional involvement in gene regulation make them ideal candidates for liquid biopsy approaches [25]. Several circRNAs have been implicated in mediating resistance to targeted therapies through diverse mechanisms including microRNA sponging, regulation of autophagy, inhibition of apoptosis, and modulation of drug efflux pumps [25].
In non-small cell lung cancer (NSCLC), circRNA_102231 overexpression is associated with resistance to gefitinib, an EGFR-tyrosine kinase inhibitor, through sponging of miR-130a-3p [25]. Similarly, in breast cancer, CDR1as correlates with tamoxifen resistance via modulation of the miR-7/EGFR pathway [25]. The following table highlights key circRNAs implicated in therapy resistance:
Table 4: circRNA Biomarkers in Cancer Drug Resistance
| circRNA | Cancer Type | Therapeutic Context | Resistance Mechanism | Clinical Utility |
|---|---|---|---|---|
| circHIPK3 | Colorectal, lung, bladder | 5-FU, cisplatin | Sponges miR-124 and miR-558 | Chemoresistance biomarker |
| circFOXO3 | Breast, lung | Chemotherapy | Binds CDK2 and p21, affecting cell cycle | Prognostic marker |
| circRNA_100290 | Oral squamous cell carcinoma | Cisplatin | Modulates miR-29 family | Diagnostic and response predictor |
| circ_0001946 | NSCLC | Gefitinib | Activates STAT6/PI3K/AKT pathway | EGFR-TKI resistance monitoring |
| circ-PVT1 | Gastric | Paclitaxel | Sponges miR-124-3p, regulates ZEB1 | Chemoresistance biomarker |
Integration with Artificial Intelligence and Multi-analyte Approaches
The future of RT-qPCR in liquid biopsy lies in integration with artificial intelligence (AI) and multi-analyte profiling approaches. AI and machine learning algorithms can enhance the diagnostic and prognostic value of RT-qPCR data by identifying subtle patterns in expression profiles that may not be apparent through conventional analysis [17]. Support vector machines and neural networks have been successfully trained using circulating RNA data to accurately differentiate between benign and malignant conditions [17].
Combining RT-qPCR analysis of RNA biomarkers with other liquid biopsy components, such as ctDNA mutation analysis and protein markers, provides a more comprehensive view of tumor biology and heterogeneity. This integrated approach can capture complementary information about genetic alterations, transcriptional regulation, and functional pathway activities, enabling more robust cancer detection and monitoring [17] [26].
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of RT-qPCR for liquid biopsy applications requires careful selection of reagents and materials optimized for sensitive detection of low-abundance targets. The following table outlines key components and their functions in the workflow:
Table 5: Essential Research Reagents for RT-qPCR Liquid Biopsy Analysis
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Reverse Transcriptase | Moloney murine leukemia virus RT, Avian myeloblastosis virus RT | Synthesizes cDNA from RNA template | High thermal stability enhances cDNA yield from structured RNAs |
| RNA Stabilization Reagents | RNAlater, specialized cfRNA tubes | Preserve RNA integrity during collection | Critical for clinical sampling and transport |
| qPCR Polymerase Master Mixes | Hot-start, inhibitor-resistant formulations | Amplifies target cDNA with high fidelity | Enable detection of rare targets in complex biofluids |
| Fluorescent Detection Systems | SYBR Green, TaqMan probes, molecular beacons | Enable real-time quantification | Probe-based systems preferred for variant discrimination |
| Reference RNAs | Synthetic circRNAs, in vitro transcribed RNAs | Normalization controls | Account for extraction and reverse transcription efficiency |
| Nucleic Acid Extraction Kits | silica membrane-based, magnetic bead systems | Isolate high-quality RNA from biofluids | Optimized for low-concentration samples |
RT-qPCR continues to serve as a foundational technology in liquid biopsy-based cancer research, offering an optimal balance of sensitivity, specificity, throughput, and cost-effectiveness [18]. The complete workflow—from appropriate sample collection through rigorous data interpretation—requires careful attention to technical details at each step to ensure reliable detection of low-abundance cancer biomarkers. As our understanding of molecular biomarkers such as circRNAs expands, and as AI-based analytical approaches become more sophisticated, RT-qPCR remains positioned as an accessible, robust platform for advancing cancer detection, therapy selection, and resistance monitoring through liquid biopsy. The standardization of protocols across laboratories and the validation of biomarkers in large, multi-center studies will be essential for translating these research applications into clinical practice, ultimately enabling more personalized and adaptive cancer management strategies.
Methodology and Clinical Application: From Bench to Bedside
The reliability of liquid biopsy research, particularly in cancer detection using reverse transcription quantitative polymerase chain reaction (RT-qPCR), is fundamentally dependent on the integrity of the pre-analytical phase. This technical guide details standardized protocols for collecting and handling blood and bone marrow samples, which are critical for ensuring the stability of molecular targets such as circulating tumor DNA (ctDNA), cell-free RNA (cfRNA), and circulating tumor cells (CTCs). Inconsistent pre-analytical procedures can introduce significant variability, compromising the accuracy of RT-qPCR results and the validity of downstream clinical interpretations [28] [29]. Adherence to the meticulously outlined protocols in this document is therefore essential for generating robust, reproducible, and clinically actionable data in liquid biopsy research for drug development.
Blood Collection Tube Selection and Handling
The choice of blood collection tube and its subsequent handling directly influences the quality of the sample for liquid biopsy analysis.
Common Blood Collection Tubes for Research
Table 1: Characteristics of Common Blood Collection Tubes for Liquid Biopsy Research
| Tube Type (Color) | Additive | Sample Type Produced | Primary Uses in Liquid Biopsy | Key Pre-analytical Considerations |
|---|---|---|---|---|
| EDTA (Lavender) | Ethylenediaminetetraacetic acid (EDTA) | Plasma | Genomic analyses (ctDNA, cfDNA); a study showed good results for ctDNA if processed within 4h at room temperature or 24h at 4°C [28]. | Inhibits coagulation by chelating calcium; requires prompt mixing and processing to prevent cell lysis and genomic degradation [30]. |
| Citrate (Light Blue) | Sodium Citrate | Plasma | Coagulation studies; can be used for specialized liquid biopsy workflows [30]. | Binds calcium to prevent clotting; requires gentle inversion for mixing [30]. |
| Heparin (Green) | Lithium/Sodium Heparin | Plasma | Some chemistry and molecular testing; not ideal for PCR due to potential inhibition [30] [29]. | Inhibits thrombin formation; heparin can interfere with enzymatic reactions in PCR [30] [29]. |
| Serum (Red) | Clot Activator (No anticoagulant) | Serum | Proteomic analyses, detection of some protein biomarkers [29] [31]. | Blood must clot for 30+ minutes before centrifugation; yields lower volume vs. plasma; clotting removes fibrinogen and some proteins [30] [29]. |
| Stabilizing Tubes | Preservatives to prevent cell lysis and nucleic acid degradation | Cell-free DNA Plasma | Specialized ctDNA and cfDNA preservation; allows extended room temperature storage [28]. | Essential for multi-center trials with long transport times; requires validation with downstream assays [28]. |
Detailed Protocol: Blood Collection and Plasma Processing for RT-qPCR
This protocol is optimized for the isolation of high-quality cell-free nucleic acids (cfDNA and cfRNA) for RT-qPCR analysis from EDTA tubes.
Materials:
- EDTA Blood Collection Tubes (Lavender top)
- Tourniquet, alcohol swabs, 21-gauge needles, and venipuncture kit
- Personal protective equipment (PPE)
- Centrifuge capable of refrigeration
- Sterile pipettes and aerosol-resistant filter tips
- Nuclease-free microcentrifuge tubes
- Research Reagent Solutions: PBS (Dulbecco's Phosphate-Buffered Saline), RNase and DNase inhibitors, cryopreservation medium (e.g., containing 10% DMSO)
Procedure:
- Patient Preparation and Phlebotomy: Perform venipuncture using standard aseptic technique. Draw blood into EDTA tubes according to the recommended "order of draw" to avoid cross-contamination of additives [30].
- Immediate Inversion and Temporary Storage: Gently invert the EDTA tubes 8-10 times immediately after collection to ensure proper mixing with the anticoagulant. If processing cannot occur immediately, store tubes at 4°C. Process EDTA tubes within a maximum of 4 hours for optimal ctDNA recovery [28].
- Centrifugation for Plasma Separation:
- Centrifuge the blood tubes at 1,600 - 2,000 × g for 10 minutes at 4°C. This step separates plasma from blood cells.
- Carefully aspirate the supernatant (plasma) without disturbing the buffy coat (layer containing white blood cells and CTCs) or the red blood cell pellet, and transfer it to a nuclease-free tube.
- Second Centrifugation for Platelet Removal:
- Centrifuge the collected plasma a second time at 16,000 × g for 10 minutes at 4°C.
- Transfer the clarified plasma to a new nuclease-free tube. This step removes any remaining platelets or cell debris, which can be a source of contaminating genomic DNA.
- Aliquoting and Storage:
- Aliquot the processed plasma into nuclease-free tubes to avoid repeated freeze-thaw cycles.
- Flash-freeze aliquots in liquid nitrogen and store at -80°C until nucleic acid extraction.
Diagram: Blood Plasma Processing Workflow for Liquid Biopsy
Bone Marrow Aspirate Collection and Processing
Bone marrow aspirates are a vital source for measuring residual disease in hematological malignancies, requiring specialized handling to preserve cell viability and nucleic acid integrity.
Detailed Protocol: Bone Marrow Aspiration and Mononuclear Cell Isolation
This protocol describes the procedure for obtaining and processing bone marrow aspirates for subsequent RNA/DNA extraction or viable cell cryopreservation for RT-qPCR and other assays [32] [33].
Materials:
- Bone marrow aspiration needles (15-16 gauge)
- Sterile syringes (10mL, 20mL)
- Bone marrow collection tubes containing anticoagulant (Heparin or EDTA)
- Research Reagent Solutions: Ficoll-Paque PLUS (or equivalent density gradient medium), PBS (without Ca2+/Mg2+), Trypan Blue solution, cryopreservation medium (e.g., 90% FBS with 10% DMSO)
Procedure:
- Patient Positioning and Site Preparation: Position the patient in the lateral decubitus position. Locate the posterior superior iliac spine. Disinfect the skin thoroughly using chlorhexidine (0.5-1%) in ethanol [32].
- Anesthesia and Needle Insertion: Anesthetize the skin, subcutaneous tissue, and periosteum with 1% lidocaine. Using a rotating motion, introduce the aspiration needle until a loss of resistance indicates entry into the marrow cavity [32].
- Aspiration: Remove the stylet and attach a 10-20 mL syringe. Apply negative pressure to aspirate 1-2 mL of marrow. Crucially, limit the volume aspirated from a single site to 1-2 mL to minimize peripheral blood dilution, which can confound subsequent measurable residual disease (MRD) analysis [32].
- Sample Transfer and Initial Handling: Immediately expel the marrow into a watch glass containing a small amount of anticoagulant (e.g., EDTA) to prevent clotting, then transfer it to a heparin or EDTA-coated tube. Invert the tube several times to ensure adequate mixing with the anticoagulant [32].
- Bone Marrow Mononuclear Cell (BMMNC) Isolation:
- Dilute the bone marrow aspirate 1:1 with PBS.
- Carefully layer the diluted sample over Ficoll-Paque density gradient medium in a centrifuge tube.
- Centrifuge at 400 × g for 30-40 minutes at room temperature with the brake disengaged.
- After centrifugation, carefully aspirate the upper plasma layer. Harvest the mononuclear cell layer (BMMNCs) at the interface using a sterile pipette and transfer it to a new tube.
- Wash the BMMNCs three times with a large volume (e.g., 45 mL) of PBS by centrifuging at 800 × g for 10 minutes [33].
- Cell Counting and Cryopreservation:
- Resuspend the cell pellet in a small volume of PBS. Mix a small aliquot with Trypan Blue and count viable cells using a hemocytometer.
- For cryopreservation, centrifuge the cells and resuspend them in cold cryopreservation medium at a concentration of 5-10 x 10^6 cells/mL.
- Transfer 1 mL aliquots to cryovials. Freeze the cells in a controlled-rate freezer or place vials in an isopropanol freezing container at -80°C overnight before transferring to liquid nitrogen for long-term storage [33].
Diagram: Bone Marrow Mononuclear Cell Isolation Workflow
Sample Stabilization for RT-qPCR Analysis
The lability of RNA targets makes stabilization the most critical factor for successful RT-qPCR in liquid biopsy.
Stabilization Guidelines for Key Biomarkers
Table 2: Stabilization Protocols for Liquid Biopsy Biomarkers in RT-qPCR
| Biomarker | Stability Concern | Recommended Stabilization Protocol | Impact on RT-qPCR |
|---|---|---|---|
| Cell-free RNA (cfRNA) | Extremely labile; degraded rapidly by ubiquitous RNases. Half-life in plasma is ~15 seconds [31]. | Immediate plasma separation (within 30 mins of draw) is critical. Add RNase inhibitors to isolated plasma or use blood collection tubes with specific RNA stabilizers. Aliquot and freeze at -80°C [31]. | Degraded RNA results in failed reverse transcription, low yield, and unreliable Cq values, compromising gene expression analysis. |
| Circulating Tumor Cells (CTCs) | Fragile; short half-life (1-2.5 hours). Prone to apoptosis and loss of marker expression [1] [34]. | Process blood samples within 4-6 hours of collection. Store at room temperature and avoid refrigeration. Use specialized preservative tubes if processing delays are anticipated [1]. | Compromised cell integrity reduces RNA yield and quality from isolated CTCs, introducing bias in tumor transcript detection. |
| Cell-free DNA (cfDNA)/ ctDNA | More stable than RNA, but fragmentation occurs over time. | Process EDTA tubes within 4 hours (RT) or 24 hours (4°C). For longer delays, use specialized cfDNA/ctDNA stabilizing tubes that prevent white blood cell lysis and nuclease activity [28]. | White blood cell lysis contaminates plasma with genomic DNA, altering mutant allele frequency quantification in RT-qPCR/ddPCR assays. |
Ribonucleic acid (RNA) isolation is a foundational step in molecular biology, serving as the critical gateway for downstream analyses such as reverse transcription quantitative polymerase chain reaction (RT-qPCR), next-generation sequencing, and microarray studies [35] [36]. The purity, integrity, and yield of isolated RNA directly determine the reliability and accuracy of subsequent experimental results. Within the rapidly advancing field of liquid biopsy for cancer detection, where analytes like circulating tumor RNA are often scarce and highly labile, the choice of RNA extraction method becomes paramount for successful biomarker quantification and clinical interpretation [25] [37].
Two predominant methodologies have emerged as standards for RNA isolation: organic phase separation (often called liquid-liquid extraction) and spin column-based purification (a solid-phase extraction technique). Each approach possesses distinct biochemical principles, advantages, and limitations that render them uniquely suited to specific research contexts. This technical guide provides an in-depth comparison of these core methodologies, with particular emphasis on their application in liquid biopsy workflows for cancer research, including detailed protocols, performance metrics, and practical implementation guidelines for research scientists and drug development professionals.
Core Principles and Methodological Comparison
Organic Phase Separation
Historical Foundation and Biochemical Mechanism
Organic extraction, historically regarded as the "gold standard" for RNA isolation, relies on the differential solubility of cellular components in immiscible aqueous and organic solvents [35] [38]. The technique typically employs a mono-phasic mixture of phenol and guanidine isothiocyanate (commercially available as TRIzol or TRI Reagent) to simultaneously lyse cells and inhibit ribonucleases (RNases) [39] [38]. Subsequent addition of chloroform and centrifugation creates a bi-phasic system where denatured proteins partition to the lower organic phase and interface, while nucleic acids remain in the upper aqueous phase [35].
A critical aspect of this separation is pH dependence. Under acidic conditions (pH < 7.0), DNA denatures and precipitates into the organic phase and interphase, while RNA remains in the aqueous phase [35] [39]. The RNA is then recovered from the aqueous phase through precipitation with isopropanol or ethanol, followed by washing with ethanol to remove residual salts, and finally rehydration in nuclease-free water or buffer [36] [39].
Advantages and Limitations in Liquid Biopsy Context
The organic method offers several key benefits for liquid biopsy applications: rapid protein denaturation that immediately stabilizes labile RNA transcripts; applicability to diverse sample types from large tissues to small cell culture pellets; and well-established, straightforward protocols that require no specialized equipment beyond a centrifuge [35]. However, significant limitations include: limited amenability to high-throughput processing and automation; labor-intensive manual processing; management of hazardous chemical waste; and potential for phase contamination during aqueous layer collection [35] [39].
Spin Column-Based Purification
Solid-Phase Extraction Mechanism
Spin column purification represents a more recent technological advancement based on the principle of solid-phase nucleic acid binding. Samples are lysed in a buffered solution containing RNase inhibitors and high concentrations of chaotropic salts (such as guanidinium thiocyanate), which disrupt hydrogen bonding, denature proteins, and facilitate RNA binding to the silica-based membrane in the column [35] [36]. Under specific pH and salt conditions, RNA adsorbs to the silica matrix while contaminants pass through during centrifugation.
The membrane-bound RNA undergoes successive wash steps with ethanol-based buffers to remove impurities, proteins, and salts. Finally, purified RNA is eluted in a low-salt buffer or nuclease-free water, which disrupts the RNA-silica interaction and releases the nucleic acid into solution [35] [36]. This method is frequently commercialized in convenient kit formats that standardize the procedure across users and laboratories.
Advantages and Limitations in Liquid Biopsy Context
Spin column systems offer distinct operational advantages: simple, straightforward procedures amenable to novice researchers; compatibility with high-throughput processing and automation; reduced exposure to hazardous chemicals; and convenient kit formats [35]. However, researchers must be aware of limitations including: membrane clogging with excessive sample input or incomplete homogenization; potential contamination with proteins or genomic DNA; incomplete cellular lysis leading to low yields; and relatively high costs, particularly for automated systems [35] [36].
Comparative Performance Analysis
Table 1: Direct Comparison of RNA Extraction Methods for Liquid Biopsy Applications
| Parameter | Organic Phase Separation | Spin Column Purification |
|---|---|---|
| RNA Quality/Purity | High quality, effective protein removal [35] | High purity, but potential gDNA contamination without DNase treatment [35] |
| Yield | High recovery, even from challenging samples [35] | Variable; dependent on complete lysis and avoidance of membrane clogging [35] |
| Hands-on Time | High (labor-intensive) [35] | Low to moderate [35] |
| Throughput Potential | Low, difficult to automate [35] | High, easily automated [35] |
| Cost Considerations | Lower reagent cost, higher labor cost [35] | Higher reagent cost (kit-based), lower labor cost [35] |
| Hazard Exposure | High (toxic chemicals: phenol, chloroform) [35] [36] | Low (minimal organic solvent exposure) [35] |
| Sample Flexibility | Excellent for diverse samples (tissues, cells) [35] | Good, but may require optimization for difficult tissues [35] |
| Technical Skill Required | Moderate (phase separation expertise needed) [39] | Low (standardized protocols) [35] |
| Suitability for Liquid Biopsy | Excellent for challenging biofluids with inhibitors [40] | Ideal for plasma/serum with low input volumes [37] |
| Downstream Compatibility | Excellent for sensitive applications like RT-qPCR [37] | Excellent, though potential carrier alcohol contamination may inhibit reactions [36] |
Table 2: Troubleshooting Common Issues in RNA Extraction
| Problem | Organic Extraction Solutions | Spin Column Solutions |
|---|---|---|
| Low Yield | Ensure complete homogenization; add carrier (glycogen) during precipitation [39] | Verify lysis efficiency; avoid overloading column; ensure proper elution [35] |
| Protein Contamination | Avoid interphase during aqueous collection; re-extract with chloroform [39] | Add additional wash steps; ensure correct ethanol concentration in wash buffers [35] |
| DNA Contamination | Optimize pH for RNA separation; include DNase treatment step [39] | Use on-column DNase digestion [36] |
| RNA Degradation | Immediately process samples in TRIzol; use RNase-free techniques [39] | Process samples quickly; use fresh RNase inhibitors [36] |
| Inhibitors in Downstream Applications | Ensure complete ethanol removal; additional precipitation/wash steps [39] | Increase wash volumes; ensure complete drying of membrane; use recommended elution buffers [36] |
| Phase Separation Issues | Centrifuge at recommended speeds/times; ensure proper TRIzol:sample ratio (10:1) [39] | Not applicable |
| Column Clogging | Not applicable | Pre-centrifuge lysates; reduce sample input; improve homogenization [35] |
Special Considerations for Liquid Biopsy and Cancer Research
Circulating RNA Biomarkers in Cancer Detection
Liquid biopsy approaches for cancer detection increasingly rely on various RNA species as biomarkers, including messenger RNAs (mRNAs), microRNAs (miRNAs), and circular RNAs (circRNAs) [25] [37]. These circulating nucleic acids offer unique opportunities for non-invasive cancer monitoring but present distinct challenges for isolation due to their low abundance in biofluids and association with different carrier complexes (exosomes, ribonucleoproteins, lipoproteins) [25] [40].
Circular RNAs have garnered significant attention as promising biomarkers because their covalently closed-loop structure confers exceptional stability in bodily fluids, making them particularly suitable for liquid biopsy applications [25]. Studies have identified specific circRNAs associated with drug resistance in various cancers, including circHIPK3 in colorectal, lung, and bladder cancers; circFOXO3 in breast and lung cancers; and circRNA_100290 in oral squamous cell carcinoma [25].
Pre-analytical Variables in Liquid Biopsy
The reliability of RNA-based liquid biopsy tests depends heavily on standardized pre-analytical procedures, as circulating RNA biomarkers are susceptible to degradation and contamination from blood cellular components [37] [40]. Key considerations include:
- Blood Collection Tubes: The use of specialized stabilization tubes (e.g., Streck Cell-Free DNA BCT) is crucial for preserving RNA integrity during sample transport and storage [37].
- Centrifugation Protocols: Double-centrifugation protocols are essential to obtain platelet-poor plasma. Research demonstrates that plasma prepared with a second centrifugation at 160 × g preserves mRNA levels significantly better than high-speed centrifugation (16,000 × g) typically used for cell-free DNA analysis [37].
- Sample Input and Carrier Molecules: For low-abundance targets in plasma or serum, the addition of carrier molecules (e.g., glycogen) during precipitation can significantly improve RNA recovery, though this may interfere with downstream applications for some spin column systems [40].
Integrated Workflow for Liquid Biopsy RNA Isolation
The following diagram illustrates a generalized workflow for RNA isolation from blood samples, integrating optimal pre-analytical steps with the core extraction methodologies:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents for RNA Isolation in Liquid Biopsy
| Reagent/Material | Function/Purpose | Method Compatibility |
|---|---|---|
| TRIzol LS Reagent | Monophasic solution of phenol and guanidine isothiocyanate for cell lysis and RNase inhibition; LS formulation optimized for liquid samples [39] [40] | Organic extraction |
| Silica Spin Columns | Microporous membrane that selectively binds RNA under high-salt conditions [35] [36] | Spin column purification |
| DNase I (RNase-free) | Enzyme that degrades genomic DNA contamination without damaging RNA [36] | Both methods |
| RNase Inhibitors | Proteins that bind to and inhibit RNases, preventing RNA degradation [35] [36] | Both methods |
| Glycogen (Molecular Grade) | Carrier molecule that co-precipitates with RNA to improve visualization and recovery from dilute solutions [39] [40] | Primarily organic extraction |
| Chaotropic Salts | (e.g., guanidinium thiocyanate) Denature proteins, inactivate RNases, and promote RNA binding to silica [35] [38] | Both methods |
| Streck Cell-Free DNA BCT Tubes | Blood collection tubes with preservatives that stabilize nucleic acids and prevent cell lysis during storage/transport [37] | Pre-analytical (both methods) |
| Agencourt RNAdvance Blood Kit | Specialized system optimized for RNA extraction from blood and plasma samples [40] | Spin column purification |
The selection between organic phase separation and spin column purification for RNA isolation in liquid biopsy cancer research involves careful consideration of research priorities, sample characteristics, and practical laboratory constraints. Organic extraction remains a powerful method for challenging samples where maximum RNA integrity and yield are paramount, despite its limitations in throughput and safety. Spin column methods offer clear advantages in convenience, scalability, and compatibility with automated platforms, making them ideal for high-throughput clinical applications and standardized biomarker assays.
For liquid biopsy applications specifically focused on detecting low-abundance circulating RNA biomarkers for cancer detection, spin column systems optimized for biofluids generally provide the best balance of practicality, consistency, and performance. However, researchers working with particularly challenging sample matrices or novel biomarker classes may find that organic extraction offers superior recovery. As the field advances toward clinical implementation, standardization of pre-analytical variables and RNA isolation protocols will be equally critical as the choice of extraction methodology itself to ensure reproducible, clinically actionable results.
MicroRNAs (miRNAs) are short, non-coding RNA molecules, typically 18–25 nucleotides in length, that have emerged as powerful regulatory molecules and promising biomarkers for cancer detection [41] [14]. Their remarkable stability in bodily fluids such as blood, urine, and saliva, coupled with their tissue-specific expression patterns, makes them exceptionally suitable for liquid biopsy applications in cancer diagnostics and monitoring [16] [41]. The 2024 Nobel Prize in Physiology or Medicine recognized the fundamental role of miRNAs in gene regulation, further underscoring their biological and clinical significance [16] [42].
However, the unique characteristics of miRNAs—including their short length, low abundance, and high sequence similarity among family members—present significant analytical challenges for their precise detection and quantification [16] [42]. Reverse transcription quantitative polymerase chain reaction (RT-qPCR) has become the gold standard method for miRNA detection due to its robustness, sensitivity, and clinical accessibility [16] [41]. Among RT-qPCR strategies, stem-loop and poly(A)-tailing have emerged as the two predominant approaches, each with distinct advantages and limitations for liquid biopsy cancer detection research [41] [43] [44]. This technical guide provides an in-depth comparison of these methodologies, focusing on their application in cancer biomarker detection.
Technical Principles and Mechanisms
Stem-Loop RT-qPCR Methodology
The stem-loop RT-qPCR method employs specially designed reverse transcription primers featuring a hairpin structure that enhances both specificity and sensitivity [45] [43]. This approach addresses the fundamental challenge of miRNA shortness, as standard PCR requires templates at least twice the length of typical primers (~20 nt each), making conventional methods unsuitable for miRNAs (17-24 nt) [45].
The process begins with a stem-loop RT primer that hybridizes to the 3' end of the mature miRNA target. This primer contains a highly stable stem-loop structure that extends the cDNA product, effectively creating a longer template for subsequent PCR amplification [45]. The forward PCR primer is designed with two distinct regions: a 3' portion that binds specifically to the miRNA sequence and a 5' extension that optimizes melting temperature and enhances assay specificity. The reverse primer targets the stem-loop region of the RT primer, while the probe (often with a minor groove binder moiety) is positioned over much of the original miRNA sequence to maximize specificity [45].
A key advantage of this method is its exceptional specificity in distinguishing between closely related miRNA family members. Research has demonstrated that properly designed stem-loop RT-qPCR can differentiate let-7 family members differing by as little as a single nucleotide [43]. This precision is particularly valuable in cancer research, where specific miRNA isoforms may have distinct clinical implications.
Poly(A)-Tailing RT-qPCR Methodology
The poly(A)-tailing method employs a different strategy, beginning with the enzymatic addition of a poly(A) tail to the 3' end of miRNAs using poly(A) polymerase [41]. This approach exploits the fact that miRNAs naturally lack poly(A) tails, unlike mRNAs. Following tailing, reverse transcription is performed using an oligo-dT adapter primer that binds to the newly added poly(A) sequence, creating cDNA suitable for PCR amplification [41].
The universal nature of this approach—where the same adapter primer can be used for all miRNAs—simplifies experimental design and enables profiling of multiple miRNAs from limited sample material [41]. However, this method faces challenges including variable extension efficiency depending on the miRNA sequence, potential sequence-specific bias, and reduced sensitivity for low-abundance miRNAs [16]. The requirement for high-quality RNA and precise experimental conditions can also introduce significant variability in miRNA detection and quantification [16].
A notable limitation of the poly(A)-tailing method is its incompatibility with 3'-terminal 2'-O-methylated small RNAs. The 2'-O-methylation modification at the RNA 3'-terminus inhibits the activity of polyadenylate polymerase, making stem-loop RT-qPCR the only suitable approach for quantifying these modified RNAs [44].
Figure 1: Comparative Workflows of Stem-Loop and Poly(A)-Tailing RT-qPCR Methods
Performance Comparison and Technical Considerations
Quantitative Comparison of Method Performance
The selection between stem-loop and poly(A)-tailing methodologies requires careful consideration of multiple performance parameters, each with implications for liquid biopsy applications.
Table 1: Comprehensive Performance Comparison of Stem-Loop vs. Poly(A)-Tailing RT-qPCR
| Performance Parameter | Stem-Loop RT-qPCR | Poly(A)-Tailing RT-qPCR |
|---|---|---|
| Theoretical Amplification Efficiency | ~100% [43] | Variable, typically lower |
| Specificity | High (can distinguish single-nucleotide differences) [43] | Moderate (may cross-detect similar family members) [43] |
| Detection Limit | ~10 miRNA molecules [41] | Higher than stem-loop (reduced sensitivity) [16] |
| Dynamic Range | Wide (from 7.5×101 to 7.5×108 copies/reaction in optimized systems) [16] | Narrower compared to stem-loop |
| Compatibility with 3'-terminal 2'-O-methylated RNAs | Yes (superior performance) [44] | No (methylation inhibits polyadenylation) [44] |
| Discrimination of Mature vs. Precursor miRNAs | Excellent (specific to mature miRNAs) | Poorer (may detect both forms) |
| Multiplexing Capability | Limited in conventional format | Better (universal reverse transcription) |
| Experimental Time | Longer (two-step process) [16] | Shorter |
Specificity and Discrimination Capability
The ability to distinguish between highly similar miRNA sequences is particularly crucial in cancer research, where specific miRNA isoforms may serve as distinct biomarkers. Stem-loop RT-qPCR demonstrates superior performance in this regard, with research showing it can effectively discriminate between let-7 family members that differ by as little as a single nucleotide [43]. This high specificity stems from the positioning of the stem-loop RT primer, which binds to a short sequence (6-8 nucleotides) at the 3' end of the miRNA, and the strategic placement of the detection probe over much of the original miRNA sequence [45] [43].
In contrast, the poly(A)-tailing method shows lower discrimination capability for closely related miRNA family members [43]. This limitation was clearly demonstrated in a study comparing the two methods for quantification of distinct let-7 microRNA family members, where the poly(A)-tailing approach showed reduced ability to differentiate between isoforms with high sequence similarity [43].
Melting curve analysis provides further evidence of the specificity advantage of stem-loop RT-qPCR. When compared to the poly(A)-tailing method, stem-loop assays produce sharper, single-peak melting curves, indicating more specific amplification without primer dimers or non-specific products [43].
Sensitivity and Detection Limits
Sensitivity is a critical parameter in liquid biopsy applications, where miRNA biomarkers often exist at low concentrations in complex biological matrices. Stem-loop RT-qPCR generally offers superior sensitivity, with detection limits as low as approximately 10 miRNA molecules per reaction under optimal conditions [41]. This exceptional sensitivity makes it particularly suitable for quantifying low-abundance miRNAs in clinical samples such as plasma, serum, or urine [41].
The enhanced sensitivity of the stem-loop method derives from several factors: the extended cDNA product provides a better template for PCR amplification, the stem-loop structure improves RT primer binding efficiency, and the overall design reduces non-specific amplification [45]. These features collectively enable reliable detection of miRNAs present at minute concentrations in liquid biopsy samples.
While the poly(A)-tailing method also provides good sensitivity, it typically demonstrates higher detection limits and reduced sensitivity for low-abundance miRNAs compared to the stem-loop approach [16]. This limitation becomes particularly significant when analyzing miRNAs that are present in very low copies in circulation.
Experimental Design and Protocol Optimization
Stem-Loop RT-qPCR Protocol
The successful implementation of stem-loop RT-qPCR requires careful attention to protocol details and optimization steps. Below is a detailed methodology based on established protocols with specific modifications for liquid biopsy samples [45] [43].
Sample Preparation and RNA Isolation
- Input Material: Use 1-10 µL of plasma or serum from liquid biopsy samples. Consider sample volume limitations in clinical settings.
- RNA Isolation: Employ small RNA enrichment kits specifically designed for biofluids (e.g., miRNeasy Serum/Plasma Kit) [41]. These kits optimize recovery of small RNAs while removing PCR inhibitors.
- Quality Assessment: Verify RNA integrity and quantify using spectrophotometry (A260/A280 ratio of 1.8-2.0 is acceptable). For low-concentration samples, proceed directly to reverse transcription without quantification.
Stem-Loop Reverse Transcription
- RT Primer Design: Design stem-loop primers with:
- 6-8 nucleotide 3' extension complementary to target miRNA
- Stem region with complementary sequences forming stable hairpin (ΔG ≈ -23 to -25 kcal/mol)
- Universal sequence in the loop for reverse primer binding
- Reaction Setup:
- Thermal Cycling:
- 16°C for 30 min (primer annealing)
- 42°C for 30 min (reverse transcription)
- 85°C for 5 min (enzyme inactivation)
Quantitative PCR Amplification
- Primer Design:
- Forward primer: 5' portion with universal sequence, 3' portion with miRNA-specific sequence (8-10 nt)
- Reverse primer: Universal sequence complementary to stem-loop region
- Reaction Setup:
- Thermal Cycling (40-45 cycles):
- 95°C for 10 min (initial denaturation)
- 95°C for 15 sec (denaturation)
- 60°C for 1 min (annealing/extension) - optimize temperature
Validation and Controls
- Include synthetic miRNA spikes (e.g., cel-miR-39) for process control
- Use no-template controls (NTC) and no-reverse-transcription controls
- Normalize to stable endogenous controls (e.g., U6 snRNA, miR-16-5p)
Critical Optimization Parameters
Several parameters require special attention during assay optimization for liquid biopsy applications:
Annealing Temperature Optimization Systematically test annealing temperatures from 55°C to 65°C to identify the optimal temperature that provides the lowest Cq values without compromising specificity. Stem-loop primers typically have optimal annealing temperatures around 40-45°C for the reverse transcription step, while PCR annealing temperatures are generally higher (55-65°C) [46].
Primer and Probe Concentration Titration Test primer concentrations from 50 nM to 400 nM and probe concentrations from 50 nM to 200 nM to identify optimal concentrations that maximize signal-to-noise ratio. Higher concentrations may increase sensitivity but also risk non-specific amplification.
Dynamic Range Assessment Perform serial dilutions of synthetic miRNA standards (from 108 to 101 copies/reaction) to establish the linear dynamic range of the assay [16]. Ensure clinical sample concentrations fall within the linear range of the standard curve.
Research Reagent Solutions
Successful implementation of miRNA detection assays requires appropriate selection of reagents and kits. The following table summarizes key solutions for liquid biopsy research.
Table 2: Essential Research Reagent Solutions for miRNA RT-qPCR
| Reagent Category | Specific Examples | Function and Application Notes |
|---|---|---|
| RNA Isolation Kits | miRNeasy Serum/Plasma Kit (Qiagen) [41], miRNeasy Serum/Plasma Advanced Kit [41] | Small RNA enrichment from biofluids; critical for efficient miRNA recovery |
| Stem-Loop RT-qPCR Kits | TaqMan MicroRNA Assays (Applied Biosystems) [41], miRCURY LNA RT Kit (Qiagen) [41] | Pre-designed assays for specific miRNAs; include optimized stem-loop primers |
| Poly(A)-Tailing Kits | miRNA First-Strand cDNA Synthesis Kit (ComWin Biotech) [43], TaqMan Advanced miRNA Assays [41] | Poly(A) tailing and cDNA synthesis in optimized buffer systems |
| qPCR Master Mixes | SYBR Premix Ex Taq (Takara) [43], TaqMan Universal PCR Master Mix [41] | Enzymes and reagents optimized for miRNA detection assays |
| Quality Control Reagents | Synthetic miRNA spikes (e.g., cel-miR-39) [41], RNA Integrity Number (RIN) standards | Process control and quality assessment |
| Stem-Loop Primers | Custom-designed with ~-23.40 kcal/mol ΔG [46] | Target-specific reverse transcription; requires careful in silico design |
Emerging Methodologies and Future Directions
Novel One-Pot RT-qPCR Methods
Recent advancements have addressed several limitations of conventional two-step RT-qPCR methods. Novel one-pot, one-step approaches such as High-Fidelity DNA polymerase-driven one-pot miRNA multiplex RT-qPCR (HOM-qPCR) and Taq DNA polymerase-driven one-pot miRNA multiplex RT-qPCR (TOM-qPCR) offer significant improvements [16].
These methods utilize a reverse transcription-hairpin occlusion system (RT-HOS) that integrates three functions: reverse transcription primer, fluorescent probe, and reverse primer in a single system [16]. This innovation enables true one-pot, one-step multiplex miRNA detection with a wide linear dynamic range from 7.5 × 108 to 7.5 × 101 copies/reaction while maintaining high specificity for distinguishing closely related miRNA sequences [16].
The key advantages of these emerging methods include:
- Reduced experimental time and minimized risk of cross-contamination
- Compatibility with both High-Fidelity and Taq DNA polymerases
- Higher temperature reverse transcription, enhancing specificity
- Elimination of RNA extraction and purification steps in some configurations
Amplification-Free and Isothermal Approaches
While RT-qPCR remains the gold standard, emerging technologies show promise for future applications:
Amplification-Free Methods Novel amplification-free approaches aim to overcome limitations of PCR-based methods by enabling direct miRNA detection without reverse transcription or amplification [42]. These methods offer streamlined workflows, reduced error rates, and enhanced compatibility with various clinical sample types, potentially enabling absolute quantification without preprocessing steps [42].
Isothermal Amplification Techniques Isothermal methods such as rolling circle amplification (RCA), catalytic hairpin assembly (CHA), and loop-mediated isothermal amplification (LAMP) eliminate the need for thermal cycling, reducing equipment requirements and operational complexity [47]. When combined with CRISPR/Cas systems, these techniques can achieve exceptional sensitivity down to attomolar levels [47].
Despite their promise, these emerging technologies currently face challenges including complex probe design, potential non-specific amplification, and limited multiplexing capability compared to established RT-qPCR methods [47].
Figure 2: Method Selection Framework for Liquid Biopsy Applications
Application in Liquid Biopsy Cancer Detection
The selection between stem-loop and poly(A)-tailing methodologies has direct implications for cancer detection and monitoring applications. Specific miRNA signatures have demonstrated clinical utility for various challenging cancers:
Pancreatic Cancer Detection Serum-derived miR-205-5p has been identified as a promising predictor that can distinguish between patients with pancreatitis and pancreatic cancer with reported accuracy rates of 91.5% [14]. High expression levels correlate with poorer prognosis and positive resection margins [14].
Non-Small Cell Lung Cancer (NSCLC) Diagnostics Plasma-based miRNA profiling has identified miR-1247-5p, miR-301b-3p and miR-105-5p as accurate discriminators between NSCLC patients and healthy individuals, with AUC values of 0.769, 0.761, and 0.777, respectively [14].
Renal Cell Carcinoma Urinary miRNAs including miR-135b-5p, miR-196b-5p, miR-200c-3p, and miR-203a-3p show promise for early-stage detection, demonstrating the utility of alternative biofluids beyond blood [41].
For these clinical applications, stem-loop RT-qPCR generally provides superior performance due to its enhanced specificity and sensitivity, particularly important when analyzing low-abundance biomarkers in complex matrices. However, the poly(A)-tailing approach may be preferable in discovery-phase studies where simultaneous profiling of multiple miRNAs is required.
The selection between stem-loop and poly(A)-tailing RT-qPCR methodologies represents a critical decision point in liquid biopsy assay design for cancer detection. Stem-loop RT-qPCR offers distinct advantages in specificity, sensitivity, and ability to discriminate closely related miRNA family members, making it particularly suitable for validation studies and clinical applications where precision is paramount. The method's compatibility with 3'-terminal 2'-O-methylated RNAs further extends its utility for comprehensive small RNA profiling.
Poly(A)-tailing RT-qPCR provides a more universal approach that simplifies experimental design and enables efficient profiling of multiple miRNAs, making it valuable for discovery-phase studies. However, its limitations in specificity and sensitivity relative to stem-loop methods must be carefully considered in the context of liquid biopsy applications where analyte concentrations are typically low.
Emerging technologies including one-pot RT-qPCR methods, amplification-free approaches, and isothermal amplification techniques show promise for addressing current limitations, though RT-qPCR remains the gold standard for sensitivity, specificity, and clinical applicability. As liquid biopsy continues to evolve as a non-invasive approach for cancer detection and monitoring, optimal assay selection and implementation will play increasingly important roles in translating miRNA biomarkers into clinical practice.
Real-time quantitative polymerase chain reaction (qPCR) and its derivative, reverse transcription qPCR (RT-qPCR), represent cornerstone technologies in molecular diagnostics and life science research. Within the rapidly evolving field of liquid biopsy for cancer detection, these amplification methods provide the sensitivity required to detect rare circulating biomarkers. The performance of any qPCR-based assay is fundamentally governed by its detection chemistry, with SYBR Green and TaqMan probe-based methods representing the two predominant approaches. The selection between these chemistries involves critical trade-offs between specificity, cost, multiplexing capability, and experimental workflow complexity. For researchers focusing on oncological applications such as detecting circular RNAs (circRNAs)—noted for their exceptional stability in bodily fluids and growing importance as cancer biomarkers—this choice is particularly consequential. This technical guide provides an in-depth comparison of SYBR Green and TaqMan chemistries, framed within the context of liquid biopsy development for cancer research and drug development.
Fundamental Principles of Detection
SYBR Green Chemistry
SYBR Green is a fluorescent dye that belongs to the class of DNA intercalating agents. Its mechanism of action is relatively straightforward:
- The dye exhibits minimal fluorescence when free in solution.
- Upon binding to the minor groove of double-stranded DNA (dsDNA), its fluorescence increases by over 1000-fold [48] [49].
- During qPCR, SYBR Green intercalates into the dsDNA amplification products as they are generated, resulting in a fluorescent signal that is proportional to the total mass of dsDNA present at the end of each cycle [50] [49].
A key characteristic of this chemistry is that the signal depends on the mass of the amplified product. Consequently, longer amplicons can potentially bind more dye molecules and generate a stronger fluorescent signal than shorter ones, assuming equivalent amplification efficiency [50].
TaqMan Probe-Based Chemistry
The TaqMan method, also known as fluorogenic 5' nuclease chemistry, employs a sequence-specific, dual-labeled oligonucleotide probe to generate a fluorescent signal. The process involves several precise steps:
- An oligonucleotide probe is constructed with a fluorescent reporter dye on the 5' end and a quencher dye on the 3' end [50].
- When the probe is intact, the proximity of the quencher to the reporter dye causes fluorescence resonance energy transfer (FRET), greatly reducing the fluorescence emitted by the reporter [50].
- If the target sequence is present, the probe anneals to its complementary sequence downstream from one of the primer sites.
- During the extension phase, the 5' nuclease activity of Taq DNA polymerase cleaves the annealed probe, separating the reporter dye from the quencher [50].
- This separation prevents FRET, resulting in a detectable increase in the reporter's fluorescence intensity, which is proportional to the accumulation of the specific target amplicon [50] [49].
Unlike SYBR Green, the TaqMan method generates a single fluorescent molecule for each amplified target molecule synthesized, independent of the amplicon length [50].
Table 1: Core Principles and Mechanism of Action
| Characteristic | SYBR Green | TaqMan Probes |
|---|---|---|
| Core Principle | Intercalating dye binding dsDNA | Fluorogenic, sequence-specific probe hydrolysis |
| Signal Generation | Binding to all dsDNA | Probe cleavage by Taq polymerase's 5' nuclease activity |
| Key Components | SYBR Green I dye, primers | Primers, dual-labeled probe (Reporter/Quencher) |
| Fluorescence Output | Proportional to dsDNA mass | Proportional to specific target amplification |
Molecular Detection Workflows
The fundamental difference in how these two chemistries detect and report amplification is illustrated in the following workflow diagrams.
Diagram 1: Comparative qPCR Workflows.
Critical Performance Comparison in a Research Context
The choice between SYBR Green and TaqMan chemistry significantly impacts assay performance, influencing experimental outcomes, data reliability, and resource allocation.
Specificity and Sensitivity
- TaqMan demonstrates higher inherent specificity because fluorescence generation requires the specific hybridization and cleavage of a target-specific probe. This minimizes the detection of non-specific amplification products or primer-dimers [50]. Its sensitivity is consistently high, reliably detecting down to 1-10 copies of the target sequence [50].
- SYBR Green has lower inherent specificity since the dye binds to any dsDNA present in the reaction, including non-specific PCR products and primer-dimers [50] [49]. This can lead to false positive signals. Its sensitivity is more variable and is highly dependent on template quality and the optimization of primer design [50]. However, with well-designed primers and proper validation, SYBR Green can achieve performance comparable to TaqMan, as demonstrated in SARS-CoV-2 detection studies where, with suitable primer sets, its performance was "comparable or better" [51].
The specificity of a SYBR Green assay can be verified post-amplification through melting curve analysis. This analysis involves gradually denaturing the amplified DNA products after the final PCR cycle while monitoring fluorescence. A single, sharp peak in the melting curve indicates a single, specific amplification product, whereas multiple peaks suggest the presence of non-specific products or primer-dimers [50] [49].
Multiplexing and Throughput
- TaqMan supports multiplexing—the simultaneous detection of multiple targets in a single reaction. This is achieved by using different probes, each labeled with a distinguishable reporter dye that fluoresces at a unique wavelength [50]. This is particularly valuable in liquid biopsy for co-detecting different cancer biomarkers or for including an internal control in the same well.
- SYBR Green is not suitable for multiplexing because the dye binds non-specifically to all dsDNA, making it impossible to distinguish between different amplicons in a single reaction [50].
Cost, Time, and Accessibility
- SYBR Green is markedly more cost-effective. It eliminates the need for expensive, fluorophore-labeled probes, reducing setup and running costs significantly [50] [52]. This makes it accessible for labs with budget constraints or for high-throughput screening where cost per reaction is a major factor.
- TaqMan is more expensive due to the cost of synthesizing the target-specific, dual-labeled probes [50]. However, this is often balanced by reduced optimization time and the availability of a vast catalog of predesigned assays for many human genes, which can accelerate research [50].
Table 2: Performance and Practical Application Comparison
| Parameter | SYBR Green | TaqMan Probes |
|---|---|---|
| Specificity | Lower (requires careful optimization & melt curve) [50] [49] | Higher (inherent in probe design) [50] |
| Sensitivity | Variable (can detect 1-10 copies with optimization) [50] [51] | High (consistently detects 1-10 copies) [50] |
| Reproducibility | Medium (depends on optimization) [50] | High [50] |
| Multiplexing | No [50] | Yes [50] |
| Cost | Lower (no probe cost) [50] [52] | Higher (costly probe synthesis) [50] |
| Ease of Design/Use | Requires primer design and assay optimization [50] | Easier; many predesigned assays available [50] |
| Optimal Applications | - Assay development- miRNA target validation- High-throughput, single-target screening | - Multiplex detection- High-fidelity quantification (e.g., gene expression)- SNP genotyping [50] |
Application in Liquid Biopsy for Cancer Detection
Liquid biopsy—the analysis of circulating tumor biomarkers in bodily fluids like blood—is transforming oncology research and clinical practice. RT-qPCR is a key enabling technology for detecting RNA biomarkers in these samples, where analyte abundance is typically very low.
The Role of circRNAs as Stable Biomarkers
Circular RNAs (circRNAs) are a promising class of non-coding RNA biomarkers for liquid biopsy. Their covalently closed-loop structure confers exceptional stability in bodily fluids (e.g., plasma, saliva), making them ideal for robust detection [25]. They are functionally involved in key oncological processes, including the development of drug resistance through mechanisms like miRNA sponging, regulation of apoptosis, and induction of epithelial-mesenchymal transition (EMT) [25]. For example:
- circHIPK3 is implicated in chemoresistance in colorectal, lung, and bladder cancers by sponging tumor-suppressive miRNAs like miR-124 [25].
- circFOXO3 can influence cell cycle regulation and apoptosis, with dysregulation linked to chemoresistance in breast and lung cancer [25].
- circ_0001946 is associated with resistance to gefitinib (an EGFR-TKI) in non-small cell lung cancer (NSCLC) [25].
Detecting these and other circRNAs via liquid biopsy offers a dynamic, non-invasive strategy for monitoring tumor evolution and therapy response [25].
Chemistry Selection for circRNA Detection
The choice between SYBR Green and TaqMan for circRNA detection involves strategic considerations:
- TaqMan Probes are often superior for the high-specificity detection of known circRNAs. Their ability to distinguish between closely related sequences is crucial because a defining feature of most circRNAs is the "back-splice" junction—a sequence not present in the linear RNA transcript. TaqMan probes can be designed to span this unique junction, ensuring that only the circular, and not the linear, isoform is detected [25].
- SYBR Green can be a valuable tool in the discovery and initial validation phase. Its lower cost and flexibility are beneficial when screening multiple candidate circRNAs across many patient samples. However, careful primer design to span the back-splice junction and rigorous melting curve analysis are mandatory to confirm amplification specificity [25].
Diagram 2: Detection Chemistry Selection for circRNA Analysis.
Experimental Protocols and Validation
Adherence to robust experimental protocols and validation is critical for generating publication-quality data, especially in a challenging field like liquid biopsy.
Essential Research Reagent Solutions
Table 3: Key Reagents for RT-qPCR in Liquid Biopsy Research
| Reagent / Solution | Critical Function | Technical Notes |
|---|---|---|
| Nucleic Acid Extraction Kit | Ishes total RNA (including circRNAs) from biofluids like plasma. | Select kits optimized for low-abundance RNA and small volumes. |
| Reverse Transcriptase | Synthesizes complementary DNA (cDNA) from RNA templates. | Critical for detecting RNA biomarkers. Use enzymes with high processivity and fidelity. |
| SYBR Green Master Mix | Contains optimized buffer, Taq polymerase, dNTPs, and SYBR Green dye. | Enables dye-based detection. Simplifies reaction setup. |
| TaqMan Master Mix | Contains buffer, Taq polymerase, dNTPs, and other components for probe-based assays. | Optimized for probe chemistry. Often includes UNG to prevent carryover contamination. |
| Sequence-Specific Primers | Amplify the target region. | For circRNAs, one primer should span the back-splice junction. |
| TaqMan Probes | Provide sequence-specific detection via fluorogenic reporting. | Must be designed for the specific target. Dual-labeled (FAM/BHQ-1 are common). |
Detailed Protocol: SYBR Green-based circRNA Detection
The following protocol is adapted from methodologies successfully used in recent studies [52].
Step 1: RNA Extraction and Qualification
- Extract total RNA from 200-300 µL of plasma or serum using a commercial kit designed for low-concentration samples.
- Quantify RNA concentration using a sensitive method like a fluorometric assay.
- Assess RNA quality if possible, though this can be challenging with liquid biopsy samples due to heavily fragmented RNA.
Step 2: Reverse Transcription (RT)
- Use 1 µg of total RNA (or the maximum available volume if concentration is low) for cDNA synthesis.
- Perform RT using a reverse transcriptase enzyme and random hexamers or gene-specific primers, following the manufacturer's protocol.
- Dilute the resulting cDNA as needed for the qPCR reaction.
Step 3: qPCR Reaction Setup
- Prepare a 20 µL reaction mixture containing:
- 10 µL of 2X SYBR Green Master Mix
- 0.6 µL of forward and reverse primer mix (final concentration 0.25 µM each)
- 3.8 µL of Nuclease-Free Water
- 5 µL of cDNA template
- Include negative controls (no-template control, NTC) in every run.
Step 4: Thermal Cycling
- Perform amplification on a real-time PCR instrument with the following cycling conditions:
- Initial Denaturation: 95°C for 2 minutes (1 cycle)
- Amplification: 95°C for 5 seconds (denaturation) and 60°C for 20 seconds (annealing/extension) for 40-45 cycles)
- Melting Curve Analysis: 65°C to 95°C, with continuous fluorescence measurement (e.g., increment of 0.5°C every 5 seconds) [52].
Detailed Protocol: TaqMan-based circRNA Detection
Step 1 & 2: RNA Extraction and Reverse Transcription
- These initial steps are identical to the SYBR Green protocol. Consistency in sample preparation is key for comparative studies.
Step 3: qPCR Reaction Setup
- Prepare a 20 µL reaction mixture containing:
- 9 µL of TaqMan Master Mix (e.g., enzyme mix and buffer)
- 1 µL of the specific TaqMan Assay (containing primers and probe) or 1 µL of a custom primer-probe mix
- 5 µL of Nuclease-Free Water
- 5 µL of cDNA template
- Include necessary controls.
Step 4: Thermal Cycling
- Perform amplification with the following conditions:
- Reverse Transcription (if one-step): 50°C for 20 minutes (1 cycle)
- Enzyme Activation/Initial Denaturation: 95°C for 3 minutes (1 cycle)
- Amplification: 94°C for 10 seconds (denaturation) and 55°C for 30 seconds (annealing/extension) for 40 cycles [52].
- A melting curve step is typically omitted as specificity is conferred by the probe.
Assay Validation and Data Analysis
Regardless of the chemistry used, rigorous validation is mandatory.
- Reaction Efficiency: Determine by creating a standard curve with a serial dilution (e.g., 5-fold or 10-fold) of a template with known concentration. Plot the log of the starting quantity against the Ct value. The slope of the linear regression is used to calculate efficiency: Efficiency = (10^(-1/slope) - 1) x 100. Efficiencies between 90-110% are considered acceptable [49].
- Specificity: For SYBR Green, a single peak in the melting curve confirms specificity. For both chemistries, run agarose gel electrophoresis to confirm a single amplicon of the expected size.
- Data Normalization (Relative Quantification): Use the ΔΔCt method (if efficiencies are near 100% and similar for target and reference genes) or the Pfaffl method (if efficiencies differ) [49]. Normalize the target circRNA Ct values to a stable reference gene (e.g., GAPDH, β-actin) or global mean.
The decision between SYBR Green and TaqMan detection chemistries is fundamental to designing robust RT-qPCR assays for liquid biopsy-based cancer research. TaqMan probes offer a premium solution for applications demanding the highest specificity, multiplexing capability, and reliability for validated targets, such as quantifying specific drug resistance-associated circRNAs like circHIPK3 or circFOXO3. SYBR Green provides a flexible and cost-effective alternative ideal for initial biomarker screening and assay development, where budget and throughput are primary concerns, provided that researchers invest the necessary effort in rigorous primer design and validation. As the field of liquid biopsy continues to advance, the strategic selection and meticulous implementation of these core detection technologies will remain vital for unlocking the clinical potential of circulating biomarkers like circRNAs, ultimately driving forward personalized cancer medicine.
The shift towards minimally invasive diagnostic techniques has positioned liquid biopsy as a transformative approach in clinical oncology. Within this field, Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) has emerged as a particularly powerful and accessible technology for detecting tumor-derived biomarkers in various body fluids. This technical guide details the sophisticated application of RT-qPCR across three distinct cancer types—neuroblastoma, lung cancer, and ovarian cancer—framed within the broader context of advancing liquid biopsy research. By enabling sensitive detection of minimal residual disease (MRD), circulating microRNAs (miRNAs), and cancer-specific gene expression profiles, RT-qPCR provides researchers and drug development professionals with a versatile platform for early cancer detection, therapy monitoring, and prognostic assessment. The following sections explore specific technical implementations, experimental protocols, and clinical validations that demonstrate how RT-qPCR is addressing critical challenges in molecular oncology through standardized, reproducible, and increasingly multiplexed assay systems.
Neuroblastoma: Multiplex RT-qPCR for Minimal Residual Disease Detection
Technical Rationale and Marker Selection
In high-risk neuroblastoma, bone marrow dissemination is present at diagnosis in more than half of patients and is predictive of poor outcome [53]. Detection of minimal residual disease (MRD) during and after treatment provides critical prognostic information, but standard cytomorphological assessment lacks sensitivity, missing the MRD that eventually leads to relapse in approximately 60% of patients [54]. RT-qPCR has emerged as a highly sensitive solution, capable of detecting one tumor cell in one million normal nucleated bone marrow cells [54].
A significant challenge in neuroblastoma MRD detection is tumor heterogeneity, which has been addressed through the development of multipanel mRNA marker approaches. Neuroblastoma tumors exhibit two distinct phenotypes—adrenergic (ADRN) and mesenchymal (MES)—each characterized by unique gene expression profiles [53]. The ADRN phenotype expresses markers such as paired-like homeobox 2b (PHOX2B), tyrosine hydroxylase (TH), cholinergic receptor nicotinic alpha 3 (CHRNA3), and growth-associated protein 43 (GAP43). In contrast, the MES phenotype expresses periostin (POSTN) and paired related homeobox 1 (PRRX1) but lacks expression of traditional ADRN markers [53] [54]. This phenotypic plasticity necessitates comprehensive marker panels for reliable MRD detection, as MES cells have been implicated in therapy resistance and are enriched in post-treatment and relapsed tumors [53].
Table 1: Neuroblastoma MRD Marker Panels for RT-qPCR Detection
| Marker Panel | Specific Markers | Biological Significance | Optimal Sample Source |
|---|---|---|---|
| ADRN Panel | PHOX2B, TH, CHRNA3, GAP43 | Characterizes adrenergic phenotype; high expression in primary tumors | Bone Marrow, Peripheral Blood |
| MES Panel | POSTN, PRRX1 | Identifies mesenchymal phenotype associated with therapy resistance | Bone Marrow, Peripheral Blood |
| Specificity Control | FMO3 | Expressed in mesenchymal stromal cells but not MES tumor cells | Bone Marrow |
| Reference Gene | GUSB | Housekeeping gene for normalization | Bone Marrow, Peripheral Blood |
Advanced Multiplex Assay Development
To overcome limitations of sample volume in pediatric patients and streamline clinical implementation, researchers have developed multiplex RT-qPCR assays capable of simultaneously testing seven different mRNA markers while reducing required sample volume [53]. Technical optimization has involved careful primer and probe redesign with fluorophores (FAM, Yakima Yellow, Dragonfly Orange) matched to available channels and paired with appropriate Black Hole Quenchers [53]. Critical reagent adjustments included replacing reverse transcriptase mixes containing dithiothreitol (DTT)—which caused fluorescence quenching with Mustang Purple—with the High-Capacity RNA-to-cDNA Kit for more efficient cDNA synthesis [53].
Validation studies comparing multiplex and singleplex RT-qPCR results from 21 blood and 24 bone marrow samples demonstrated comparable sensitivity, with the multiplex assay maintaining detection capability even in samples of low RNA quantity [53]. This technical advancement represents a significant step toward clinical implementation, conserving precious patient samples while reducing processing time and resource requirements.
Clinical Workflow and Interpretation Guidelines
The clinical workflow for neuroblastoma MRD detection begins with bone marrow aspirate collection from both iliac crests, processed within 24 hours for RNA preservation [54]. Following RNA extraction, the multiplex RT-qPCR assay simultaneously evaluates ADRN and MES markers alongside reference genes.
Thresholds for positivity have been established using control bone marrow (n=54) and peripheral blood (n=50) samples, with patient samples scored positive when Ctsample <40 and mean ΔCtsample is <3.0 Ct than median ΔCtcontrol tissue [53]. PHOX2B demonstrates ideal characteristics as a specific marker, showing no expression in any control samples [53]. Researchers must remain vigilant for potential genomic DNA amplification, particularly with the TH assay, where specific amplification plot characteristics and confidence scores (AMPSCORE, CQCONF) help distinguish true from false amplifications [53].
Diagram 1: Neuroblastoma MRD detection workflow showing bone marrow processing, multiplex RT-qPCR analysis, and comprehensive result interpretation.
Lung Cancer: miRNA Expression Profiling for Diagnostic Classification
miRNA Biomarker Discovery and Validation
MicroRNA (miRNA) expression profiling has revolutionized molecular classification of non-small cell lung cancer (NSCLC), with RT-qPCR serving as the gold standard for validation and clinical implementation. Lung adenocarcinoma (LUAD) and squamous cell carcinoma (LUSC) exhibit distinct miRNA expression signatures that can be detected in both tissue and blood plasma, offering significant potential for diagnostic and prognostic applications [55].
Comprehensive miRNA profiling using microarray technology in 12 LUAD and 12 LUSC samples identified 107 significantly deregulated miRNAs in LUAD and 235 in LUSC, with 26 miRNAs common between subtypes [55]. Through rigorous validation via RT-qPCR in independent sample sets (50 LUAD and 50 LUSC patients with adjacent normal tissues), researchers established verified miRNA panels specific to each subtype. In LUAD, three miRNAs were consistently upregulated (miR-7-5p, miR-375-5p, miR-6785-3p) while five were downregulated (miR-101-3p, miR-139-5p, miR-140-3p, miR-144-3p, miR-195-5p) [55]. The LUSC signature comprised three upregulated (miR-7-5p, miR-21-3p, miR-650) and seven downregulated miRNAs (miR-95-5p, miR-140-3p, miR-144-3p, miR-195-5p, miR-375, miR-744-3p, miR-4689-3p) [55].
Table 2: Validated miRNA Signatures in Non-Small Cell Lung Cancer Subtypes
| Cancer Subtype | Upregulated miRNAs | Downregulated miRNAs | Key Regulatory Pathways |
|---|---|---|---|
| Lung Adenocarcinoma (LUAD) | miR-7-5p, miR-375-5p, miR-6785-3p | miR-101-3p, miR-139-5p, miR-140-3p, miR-144-3p, miR-195-5p | Cell Cycle, Membrane Trafficking, EGFR Signaling |
| Squamous Cell Carcinoma (LUSC) | miR-7-5p, miR-21-3p, miR-650 | miR-95-5p, miR-140-3p, miR-144-3p, miR-195-5p, miR-375, miR-744-3p, miR-4689-3p | Immune System, Transcriptional Regulation by TP53, FGFR Signaling |
Plasma-Based Detection and Diagnostic Algorithms
Circulating miRNAs in blood plasma represent particularly promising biomarkers due to their remarkable stability, protected from degradation by membrane vesicles and biopolymer complexes [56]. Profiling of 179 miRNAs in blood plasma of lung cancer patients using miRCURY LNA miRNA qPCR Serum/Plasma Panel identified distinct expression patterns that differentiated cancer patients from healthy individuals and those with non-cancerous lung diseases [56].
To address normalization challenges in circulating miRNA quantification, researchers employed innovative ratio-based statistical analyses, generating 9,729 miRNA ratios from profiling data [56]. This approach identified 241 ratios (comprising 98 individual miRNAs) with significantly different expression between healthy individuals and the combined lung cancer group. Using LASSO-penalized logistic regression modeling, a diagnostic algorithm incorporating 10 miRNA ratios (comprising 14 individual miRNAs) achieved exceptional discrimination between lung cancer patients and control groups with an AUC of 0.979 [56].
Technical Considerations for miRNA RT-qPCR
Robust miRNA profiling requires meticulous attention to technical details throughout the workflow. Total RNA isolation from fresh-frozen tissues should utilize kits specifically designed for small RNA preservation (e.g., miRNeasy mini kit), with quality assessment through NanoDrop quantification and RNA Integrity Number (RIN) evaluation using Agilent TapeStation systems [55]. Only non-degraded samples with RIN >7.0 should proceed to analysis.
For RT-qPCR validation, the miScript SYBR Green PCR Kit with miScript Primer Assays on fast real-time PCR systems enables high-throughput profiling. RNU6B serves as an appropriate endogenous control for tissue samples, while plasma-based assays may require alternative normalization strategies due to the lack of consistently expressed reference miRNAs in circulation [55] [56]. All reactions should be performed in technical triplicate with rigorous inclusion of no-template controls to ensure assay specificity.
Ovarian Cancer: mRNA Profiling for Biomarker Discovery
Multi-Gene Expression Signatures
Ovarian cancer detection and prognosis have been enhanced through RT-qPCR-based profiling of cancer-related genes in tumor tissues. A comprehensive analysis of 60 ovarian carcinoma tumors compared to 30 normal ovaries evaluated expression of suppressor genes (ATM, BRCA1, BRCA2), proto-oncogenes (KRAS, c-JUN, c-FOS), pro-apoptotic genes (NOXA, PUMA), and genes related to chromatin remodeling (MEN1) and carcinogenesis (NOD2, CHEK2, EGFR) [57].
This systematic approach identified significant overexpression of KRAS, c-FOS, PUMA, and EGFR at both mRNA and protein levels in ovarian cancer patients compared to controls [57]. Notably, BRCA1, BRCA2, NOD2, and CHEK2 showed no significant transcriptional changes, highlighting the importance of multi-marker panels rather than single-gene biomarkers. The study further suggested that KRAS, NOXA, PUMA, c-FOS, and c-JUN may be associated with poor prognosis in ovarian cancer, providing potential targets for therapeutic intervention [57].
Innovative Platelet RNA Profiling Approach
Beyond traditional tissue analysis, liquid biopsy approaches using blood-based biomarkers have emerged as promising tools for ovarian cancer detection. A novel qPCR-based algorithm leveraging tumor-educated platelets has demonstrated exceptional diagnostic performance, detecting ovarian cancer with 94.1% sensitivity and 94.4% specificity (AUC=0.933) [58].
This innovative methodology utilizes intron-spanning read (ISR) counts rather than conventional gene expression levels, enhancing detection of cancer-specific splicing events while reducing genomic DNA interference [58]. The approach specifically captures alternative splicing events in platelet RNA that occur in response to tumor signals, providing a unique molecular signature of malignancy. From initial RNA sequencing data, researchers selected a final panel of 10 splice-junction biomarkers with minimal expression in benign samples but elevated levels in ovarian cancer, validating them via RT-qPCR to create a clinically accessible diagnostic tool [58].
Diagram 2: Platelet RNA profiling workflow for ovarian cancer detection, showing from blood collection through diagnostic algorithm development.
Technical Protocol for Ovarian Cancer Gene Expression Analysis
For tissue-based ovarian cancer profiling, RNA isolation is optimally performed using TriPure Isolation Reagent according to manufacturer protocols [57]. cDNA synthesis from total RNA utilizes the Transcriptor First Strand Synthesis Kit, with subsequent RT-qPCR analysis conducted on LightCycler480 systems using LightCycler480 Probes Master kit.
Primer design follows established sequences with GAPDH and β-ACTIN as dual housekeeping genes for normalization [57]. The PCR program initiates with activation at 95°C for 10 minutes, followed by cycles of denaturation (95°C), annealing at primer-specific temperatures, and extension (72°C). Fluorescence acquisition and data analysis using the 2^(-ΔΔCt) method provide quantitative expression values for target genes relative to controls [57].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for RT-qPCR-Based Cancer Detection
| Reagent Category | Specific Products | Application Note | Reference |
|---|---|---|---|
| RNA Isolation | miRNeasy Mini Kit (Qiagen), TriPure Isolation Reagent (Roche), PAXgene Blood RNA Tubes | Platform-specific optimization for blood, tissue, or bone marrow samples | [55] [57] [54] |
| cDNA Synthesis | High-Capacity RNA-to-cDNA Kit (Applied Biosystems), Transcriptor First Strand Synthesis Kit (Roche) | Critical for eliminating fluorescence quenching in multiplex assays | [53] [57] |
| qPCR Master Mixes | LightCycler480 Probes Master (Roche), miScript SYBR Green PCR Kit (Qiagen) | Fluorophore compatibility essential for multiplex detection | [53] [57] |
| miRNA Profiling | miRCURY LNA miRNA qPCR Serum/Plasma Panel (Exiqon) | Optimized for circulating miRNA detection in blood plasma | [56] |
| Reference Genes | GUSB, PHOX2B (negative control), RNU6B, GAPDH, β-ACTIN | Tissue-specific and application-specific validation required | [53] [55] [57] |
| Automated Platforms | CellSearch (CTCs), AIPF (DTCs), Liquid Bead Array Technology | Integration with RT-qPCR for multimodal analysis | [1] [54] |
The expanding clinical applications of RT-qPCR in neuroblastoma MRD detection, lung cancer miRNA profiling, and ovarian cancer biomarker validation demonstrate the remarkable versatility of this technology in advancing liquid biopsy approaches. The development of multiplex assays, standardized workflows, and sophisticated analytical algorithms has transformed RT-qPCR from a basic research tool into an indispensable platform for molecular diagnostics. Future directions will likely focus on increased multiplexing capabilities, integration with other liquid biopsy modalities (ctDNA, CTCs, exosomes), and implementation of artificial intelligence for data interpretation. As standardization improves and clinical validation expands, RT-qPCR-based liquid biopsy approaches promise to revolutionize cancer detection, monitoring, and personalized treatment selection across the oncologic spectrum. The techniques and applications detailed in this technical guide provide researchers and drug development professionals with both the theoretical foundation and practical methodologies to advance this rapidly evolving field.
Liquid biopsy represents a transformative approach for less burdensome disease monitoring in oncology. In neuroblastoma, the detection of minimal residual disease (MRD) and circulating tumor cells via bone marrow (BM) and peripheral blood (PB) sampling is crucial for risk stratification and therapy guidance. This technical guide elucidates the development, validation, and application of a multi-marker RT-qPCR panel targeting PHOX2B, TH, and DDC for sensitive molecular detection. We detail the core methodologies, analytical performance, and clinical prognostic significance of this panel, framing it within the broader context of RT-qPCR for liquid biopsy in cancer detection. Supported by prospective international validation studies, the implementation of this multi-marker assay correlates powerfully with event-free and overall survival, establishing a new standard for MRD testing in neuroblastoma.
Neuroblastoma (NB), a pediatric solid tumor originating from the sympathetic nervous system, is characterized by extreme clinical heterogeneity. While non-high-risk patients exhibit survival rates exceeding 90%, high-risk (HR) patients face a dismal prognosis, with long-term survival below 50% despite intensive multimodal therapy [59] [60]. Metastatic disease is the principal cause of death, and the persistence of minimal residual disease after initial treatment is a major mechanism of relapse [59]. This clinical reality underscores the critical need for highly sensitive and specific methods to detect disseminated tumor cells for accurate risk stratification, therapy response monitoring, and early relapse detection.
Liquid biopsy, through the sampling of BM and PB, offers a less invasive means for sensitive disease monitoring compared to traditional solid tumor biopsies. The core challenge lies in identifying molecular markers that are highly expressed in tumor cells but absent in normal hematopoietic cells. Single-marker assays have historically faced limitations in sensitivity and specificity. The solution, validated in recent large-scale studies, is the implementation of multi-marker panels. By simultaneously targeting several neuroblastoma-associated mRNAs (NB-mRNAs), these panels overcome tumor heterogeneity and significantly enhance the sensitivity of detecting disseminated tumor cells and circulating tumor cells, providing a powerful tool for clinical management and research [59] [61].
Molecular Foundations of the Core Marker Panel
The selection of PHOX2B, TH, and DDC is grounded in their fundamental roles in neuroblastoma biology and their specific expression patterns.
PHOX2B (Paired-like Homeobox 2B)
PHOX2B is a homeodomain transcription factor that is essential for the development and differentiation of sympathetic neurons. It acts as a master regulator of the noradrenergic phenotype in neuroblastoma cells [62]. Its expression is exquisitely restricted to neural crest-derived tissues, resulting in undetectable expression in normal bone marrow and peripheral blood [63]. This high degree of specificity makes it an ideal marker for MRD detection, as it eliminates background noise from healthy blood cells, a common limitation of other markers like TH and GD2 synthase [63].
TH (Tyrosine Hydroxylase)
TH is the rate-limiting enzyme in the catecholamine biosynthesis pathway, converting tyrosine to L-DOPA. It is a well-established tissue-specific marker for neuroblastoma and has been used for MRD detection for decades [62]. However, a key limitation of TH is its low-level expression in normal hematopoietic cells, which can lead to false-positive results or inconclusive data if appropriate, stringent cut-off thresholds are not applied [63].
DDC (Dopa Decarboxylase or Aromatic L-Amino Acid Decarboxylase)
DDC is another enzyme in the catecholamine pathway, responsible for converting L-DOPA to dopamine. Like TH and PHOX2B, it is a member of the adrenergic (ADRN) gene signature that defines a major cell state in neuroblastoma [60]. Its inclusion in multi-marker panels adds another layer of sensitivity, capturing tumor cells that might express a complementary but not identical profile of NB-mRNAs.
The logical relationship between these markers, their biological pathway, and their role in detection is summarized in the diagram below.
Assay Configuration and Experimental Protocol
The establishment of a robust RT-qPCR-based multi-marker panel requires meticulous optimization at each step, from sample collection to data analysis.
Sample Collection and Pre-processing
- Bone Marrow and Peripheral Blood: Collect 2-8 mL of BM or PB in appropriate anticoagulant tubes (e.g., EDTA or CPT tubes) [64] [61].
- Processing Time: Process samples within 2-4 hours of collection to preserve RNA integrity [61].
- Mononuclear Cell Enrichment: Isolate mononuclear cells (including any tumor cells) using density gradient centrifugation (e.g., Ficoll-Hypaque or commercial kits like OncoQuick) [64] [61]. This step reduces the sample volume and removes granulocytes and red blood cells.
RNA Isolation and cDNA Synthesis
- RNA Extraction: Isolve total RNA from the mononuclear cell fraction using commercial kits (e.g., Qiagen RNA Isolation Kit). For low cell numbers, carrier RNA can be added to improve yield.
- cDNA Synthesis: Synthesize complementary DNA (cDNA) using reverse transcriptase with oligo(dT) and/or random hexamer primers. Using oligo(dT)-coated magnetic beads (e.g., μMACS One-step cDNA kit) during this step can simultaneously purify mRNA and synthesize cDNA, improving assay sensitivity [64].
Quantitative Real-Time PCR (RT-qPCR)
- Primer and Probe Design: Design TaqMan hydrolysis probes and primers that are intron-spanning to preclude amplification of genomic DNA [64].
- Multiplex Reaction: Perform multiplex RT-qPCR reactions. A typical reaction mixture includes:
- cDNA template
- TaqMan Universal PCR Master Mix
- Primers and FAM-labeled probes for PHOX2B, TH, DDC, and other panel genes (e.g., CHRNA3, GAP43)
- Primer and probe for a reference housekeeping gene (e.g., GAPDH, β-actin) for normalization.
- Thermal Cycling: Standard TaqMan cycling conditions are used: 50°C for 2 min, 95°C for 10 min, followed by 45-50 cycles of 95°C for 15 sec and 60°C for 1 min.
- Pre-amplification (Optional): For samples with very low RNA content, a target-specific pre-amplification PCR step can be incorporated prior to the main qPCR to increase the signal [61].
Data Analysis and Interpretation
- Cycle Threshold (Ct): The Ct value for each marker is determined.
- Normalization: Normalize the Ct values of target genes to the housekeeping gene (ΔCt).
- Cut-off Threshold: Establish a validated cut-off Ct or ΔCt value for each marker to define positivity. This is critical for specificity and is typically derived from the mean expression + 2-3 standard deviations in a large set of healthy control samples [64] [61]. A sample is considered positive for NB if the expression level of any marker in the panel exceeds its specific cut-off.
The following diagram illustrates the complete workflow from sample to result.
Key Validation Data and Clinical Performance
The clinical utility of the PHOX2B/TH/DDC panel has been rigorously validated in large, prospective, international cohorts.
Table 1: Key Prognostic Findings from the GPOH-DCOG HR-NB Validation Study (n=345) [59]
| Timepoint & Metric | Finding | Statistical Significance |
|---|---|---|
| At Diagnosis | BM infiltration >10% by RT-qPCR | aHR for EFS: 1.82 (95% CI: 1.25-2.63)aHR for OS: 2.04 (95% CI: 1.33-3.14) |
| Post-Induction | Any RT-qPCR positivity in BM | 5-year EFS: 26.6% vs 60.4% (negative)5-year OS: 43.8% vs 65.7% (negative) |
| Post-Induction | Association with EFS | Hazard Ratio (HR): 2.10 (95% CI: 1.27-3.49) |
| Post-Induction | Association with OS | Hazard Ratio (HR): 1.76 (95% CI: 1.01-3.08) |
Table 2: Comparison of Marker Specificity in Normal Tissues [63]
| Marker | Expression in Normal BM (n=51) | Expression in Normal PB (n=37) | Expression in PBSC (n=24) |
|---|---|---|---|
| PHOX2B | 0% (0/51) | 0% (0/37) | 0% (0/24) |
| TH | Low-level expression detected | Low-level expression detected | Low-level expression detected |
| GD2 Synthase | Low-level expression detected | Low-level expression detected | Low-level expression detected |
The data in Table 1 demonstrates the powerful prognostic value of the multi-marker RT-qPCR assay, particularly after induction therapy. The failure to clear BM metastases, as detected by this sensitive method, is strongly correlated with very poor outcomes. Table 2 highlights the superior specificity of PHOX2B compared to other historical markers, which is fundamental for reducing false-positive results in MRD testing.
The Scientist's Toolkit: Essential Research Reagents
The table below details key reagents and materials utilized in the establishment and execution of the multi-marker RT-qPCR assay, as cited in the literature.
Table 3: Key Research Reagent Solutions for Multi-Marker RT-qPCR Assays
| Reagent / Material | Function / Description | Example Use-Case / Citation |
|---|---|---|
| TaqMan Probes & Primers | Sequence-specific detection of PHOX2B, TH, DDC, and other panel genes via hydrolysis probes. | Custom designed, intron-spanning primers and FAM-labeled probes [64]. |
| Mono-Poly Resolving Medium | Density gradient medium for the separation of mononuclear cells from whole blood or bone marrow. | Used for PB and BM sample preparation in NB studies [60]. |
| μMACS cDNA Synthesis Kit | mRNA purification and cDNA synthesis using oligo(dT) MicroBeads on a magnetic column. | Used for cDNA synthesis following tumor cell enrichment [64]. |
| AdnaTest EMT-2/StemCell Select | Immunomagnetic enrichment of CTCs using antibodies against EPCAM and ERBB2. | Used for CTC enrichment in metastatic breast cancer studies prior to multi-marker qPCR [65]. |
| OncoQuick System | A commercial tube system with a porous barrier for the enrichment of circulating tumor cells from blood. | Used for CTC enrichment in female cancer patients prior to RNA isolation and RT-qPCR [61]. |
| qPCR Master Mix | Optimized buffer, enzymes, and dNTPs for efficient and robust qPCR amplification. | "Oncology-ready" master mixes are engineered for sensitivity and inhibitor tolerance in clinical samples [18]. |
Advanced Applications and Emerging Directions
Integration with Droplet Digital PCR (ddPCR)
While RT-qPCR is the current validated standard, droplet digital PCR (ddPCR) is an emerging technology that offers absolute quantification of nucleic acid molecules without the need for a standard curve. A recent study developed a ddPCR-based assay measuring seven NB-mRNAs (CRMP1, DBH, DDC, GAP43, ISL1, PHOX2B, and TH) and found that the expression profiles and predominant mRNA species differed significantly between non-high-risk and high-risk cases [60]. This suggests that ddPCR may provide even more precise prognostic stratification and could be a future direction for assay evolution.
Guiding Maintenance Therapy and Clinical Decision-Making
The prognostic power of the multi-marker panel, especially at the end of therapy, is being leveraged to stratify patients for novel maintenance therapies. Detection of MRD at the end of therapy is an independent predictor of worse event-free survival, even in patients who are in complete remission by standard imaging criteria [66]. This "molecular relapse" identifies a patient population with a high risk of clinical relapse, creating an opportunity for intervention with targeted immunotherapies or other novel agents to eradicate persistent disease and improve long-term outcomes [59] [66].
The multi-marker RT-qPCR panel incorporating PHOX2B, TH, and DDC represents a significant advancement in the molecular diagnosis and monitoring of neuroblastoma. Its enhanced sensitivity and specificity over single-marker assays and traditional immunocytology have been conclusively demonstrated in large, prospective, international studies. The strong correlation between post-therapy MRD detection and poor clinical outcome provides a compelling evidence base for the implementation of this panel in clinical trials and eventually in routine practice. As the field moves forward, the integration of even more sensitive technologies like ddPCR and the application of these liquid biopsy panels to guide personalized maintenance therapy will be critical steps toward improving the survival of high-risk neuroblastoma patients.
Troubleshooting and Optimization: Maximizing Assay Sensitivity and Reproducibility
The reliability of liquid biopsy data, particularly in RT-qPCR-based cancer detection, is fundamentally dependent on pre-analytical sample quality. Hemolysis and sample instability introduce significant analytical bias by altering the molecular composition of biofluids, potentially leading to false positives or negatives. This technical guide examines the impact of these variables within the context of circulating tumor DNA (ctDNA) and cell-free RNA (cfRNA) analysis, providing evidence-based protocols to standardize liquid biopsy workflows for oncological research and drug development.
The Impact of Hemolysis on Liquid Biopsy Biomarkers
Mechanisms of Hemolysis-Induced Bias
Hemolysis, the rupture of red blood cells (RBCs) during blood collection or processing, releases intracellular components that contaminate cell-free plasma or serum. This process substantially alters the detectable profile of circulating biomarkers because RBCs contain high concentrations of endogenous miRNAs and other nucleic acids that are not derived from tumors [67]. The release of these components dilutes or masks tumor-specific signals, compromising the integrity of data obtained from plasma or serum samples.
The electrical conductivity of blood increases during hemolysis because the insulating lipid bilayers of intact RBCs are ruptured, releasing conductive intracellular hemoglobin and electrolytes into the plasma. This property enables real-time monitoring of hemolysis through resistance measurements, providing researchers with a rapid quality assessment tool [68].
Effects on microRNA Biomarkers
Hemolysis disproportionately affects microRNA biomarkers due to the abundant and specific miRNA content within red blood cells. Research profiling miRNA content in hemolyzed versus non-hemolyzed plasma has identified a substantial proportion of detectable miRNAs that are susceptible to hemolysis interference [67].
Table 1: Hemolysis-Susceptible microRNAs with Proposed Cancer Biomarker Potential
| microRNA | Reported Cancer Association | Fold Increase in Hemolyzed Plasma |
|---|---|---|
| miR-16 | Chronic lymphocytic leukemia, prostate cancer | Significantly elevated [67] |
| miR-451 | Various cancers | Highly elevated (RBC-enriched) [67] |
| miR-92a | Ischemic heart disease, various cancers | Affected by hemolysis [67] |
| miR-21 | Breast, lung, colorectal cancers | Elevated in hemolysis [67] |
| miR-106a | Proposed cancer biomarker | Susceptible to hemolysis [67] |
| miR-17 | Proposed cancer biomarker | Susceptible to hemolysis [67] |
The data indicate that low-level hemolysis, frequently occurring during plasma/serum collection, substantially impacts many candidate circulating miRNAs. Rigorous quality control is therefore critical for the accurate measurement of any candidate circulating miRNA biomarker [67].
Hemolysis Assessment Methods
Spectrophotometric Analysis
The most accurate method for quantifying hemolysis involves spectrophotometric measurement of free hemoglobin concentration. Hemoglobin exhibits characteristic absorbance peaks at 414 nm (primary peak), with secondary peaks at 541 and 576 nm indicating very high hemolysis levels [67]. Samples with A414 readings exceeding 0.2 demonstrate significantly increased variability in RBC-enriched miRNAs like miR-16 and miR-451. Non-hemolyzed samples typically present with A414 readings between 0.14-0.18 [67].
Real-Time Conductivity Monitoring
Emerging methodologies enable real-time hemolysis monitoring through conductivity measurements. As RBCs rupture, they release hemoglobin and intracellular electrolytes, increasing plasma conductivity. This approach provides continuous assessment during procedures but currently detects relative changes rather than absolute hemolysis percentages, as baseline conductivity varies between patients [68].
Sample Stability Under Different Pre-analytical Conditions
Sample Collection and Transport Media
The choice of transport medium significantly impacts RNA stability in liquid biopsy samples. Comparative studies of Viral Transport Medium (VTM), normal saline, and dry swabs demonstrate substantial differences in nucleic acid recovery under varying temperature conditions [69].
Table 2: Sample Media Performance for RNA Stabilization
| Transport Media | Composition | Stability Performance | Recommended Use |
|---|---|---|---|
| Viral Transport Medium (VTM) | Balanced salt solution with stabilizers and antibiotics | Superior stability; <1.34 Ct increase after 5 days at 40°C [69] | Gold standard for RNA preservation |
| Normal Saline (0.9% NaCl) | Sodium chloride solution | Substantial sensitivity loss; up to 7.8 Ct increase after 120h [69] | Limited use, requires cold chain |
| Dry Samples | No stabilization media | Significant RNA degradation; undetectable in some cases after 120h [69] | Not recommended for RNA analysis |
VTM outperforms saline and dry conditions across all temperature ranges, maintaining RNA stability for up to 5 days without refrigeration. In contrast, samples in normal saline demonstrate a time- and temperature-dependent loss of sensitivity, with some samples becoming undetectable after 120 hours [69].
Temperature and Time Considerations
Temperature control during sample transport and storage represents a critical factor in nucleic acid preservation. Research indicates that VTM-stabilized samples maintain stability across a broad temperature range (20-40°C) for extended periods, enabling flexibility in logistics for multi-center trials [69]. However, samples stabilized in suboptimal media like saline demonstrate marked degradation at elevated temperatures, with false-negative results occurring after 96 hours at elevated temperatures [69].
For urine samples in bladder cancer detection, specific stabilization protocols enable RNA stability for over 10 days at unchilled temperatures during shipping, facilitating centralized testing facilities [70].
Tissue Stabilization Methods for Control Samples
While liquid biopsy focuses on biofluids, tissue samples often serve as reference materials. Comparison of stabilization methods for human lung tissue demonstrates significant differences in RNA integrity:
- RNAlater and Snap-Freezing with OCT compound: Highest RNA Integrity Numbers (RIN 7.6-8.1), suitable for long amplicon PCR [71]
- Snap-Freezing alone: Moderate RNA integrity (RIN 5.2), showing degradation [71]
- Formalin-Fixed Paraffin-Embedded (FFPE): Lowest RNA integrity (RIN 1.4), severely fragmented [71]
These findings highlight the importance of matched stabilization protocols when using tissue controls to validate liquid biopsy findings.
Experimental Protocols for Pre-analytical Validation
Hemolysis Assessment Protocol
Principle: Quantify hemolysis through spectrophotometric measurement of free hemoglobin at 414 nm absorbance [67].
Procedure:
- Centrifuge collected blood samples at 2,500 × g for 20 minutes at room temperature to separate plasma
- Transfer 200 μL plasma to spectrophotometer cuvette
- Measure absorbance from 350-650 nm, noting peak values at 414 nm, 541 nm, and 576 nm
- Calculate degree of hemolysis relative to non-hemolyzed control (A414 0.14-0.18)
- Exclusion criterion: Reject samples with A414 > 0.2 for miRNA analysis
Quality Control: Include a known non-hemolyzed sample as reference. Establish acceptable ranges for specific analyte classes (e.g., stricter thresholds for miRNA than for DNA biomarkers).
Sample Stability Validation Protocol
Principle: Evaluate the impact of pre-analytical variables on target analyte integrity using RT-qPCR [69].
Procedure:
- Spike synthetic RNA or DNA controls into sample collection tubes
- Aliquot samples into different transport media (VTM, saline, dry)
- Incubate under varying temperature conditions (4°C, 20°C, 30°C, 40°C)
- Collect subsets at multiple timepoints (0h, 8h, 24h, 72h, 120h)
- Extract nucleic acids using standardized protocols
- Perform RT-qPCR targeting multiple amplicon lengths (e.g., 73bp, 436bp)
- Record Cycle quantification (Cq) values and calculate ΔCq relative to time zero
Interpretation: Acceptable stability is defined as <2.0 Cq increase over baseline. Media and conditions maintaining this threshold qualify for operational use.
Visualizing Pre-analytical Workflows and Impacts
Diagram 1: Pre-analytical Variables Impact Pathway. This workflow illustrates how pre-analytical decisions and risk factors lead to specific analytical impacts in liquid biopsy testing.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Pre-analytical Control in Liquid Biopsy
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Viral Transport Medium (VTM) | Stabilizes RNA in biofluids during transport | Superior to saline for extended storage; maintains stability for 5 days without cold chain [69] |
| RNAlater Stabilization Solution | Preserves RNA in tissue and cell samples | Provides high RNA Integrity Numbers (RIN 7.6); superior to snap-freezing alone [71] |
| Cell-Free DNA BCT Tubes | Preserves blood ctDNA profile | Prevents genomic DNA contamination and ctDNA degradation |
| Drabkin's Reagent | Quantifies free hemoglobin for hemolysis assessment | Converts hemoglobin to cyanmethemoglobin for spectrophotometric measurement at 540nm [68] |
| Histopaque Density Gradient Medium | Enriches mononuclear cell fraction | Isolates white blood cells and CTCs from whole blood; used prior to RNA extraction [72] |
| TaqMan Hydrolysis Probes | Target-specific detection in RT-qPCR | Enable multiplexed detection of epithelial markers (CK8, CK18, CK19) for CTC detection [72] |
Standardization of pre-analytical protocols is not merely a quality control measure but a fundamental requirement for generating reliable, reproducible liquid biopsy data in cancer research. The implementation of rigorous hemolysis screening, appropriate stabilization media selection, and controlled transport conditions significantly reduces technical variance, enabling more accurate detection of biologically significant changes in circulating biomarkers. As liquid biopsy technologies evolve toward earlier cancer detection and minimal residual disease monitoring, controlling these pre-analytical variables becomes increasingly critical for meaningful clinical translation.
The analysis of circulating biomarkers for early cancer detection represents a paradigm shift in molecular diagnostics; however, the extreme scarcity of these markers in bodily fluids presents a formidable analytical challenge. In liquid biopsies, tumor-derived materials such as circulating tumor DNA (ctDNA), microRNAs (miRNAs), and other nucleic acids are highly diluted within the total biological sample, often constituting less than 0.01% of the total cell-free DNA in early-stage disease [73] [26]. This low abundance creates a critical detection barrier for conventional molecular techniques, potentially leading to false negatives and impeding early intervention. The rapid clearance of circulating cell-free DNA, with half-lives ranging from minutes to a few hours, further intensifies this challenge by narrowing the diagnostic window [26]. Overcoming these limitations requires technological innovations that push the boundaries of detection sensitivity while maintaining specificity and practical applicability in clinical settings.
Within this context, reverse transcription quantitative PCR (RT-qPCR) remains a cornerstone technology due to its robustness, cost-effectiveness, and widespread availability in clinical laboratories [16] [73]. The technique's inherent compatibility with liquid biopsy workflows and its proven track record in molecular diagnostics make it an essential platform for enhancement. Recent methodological refinements have significantly advanced RT-qPCR capabilities, enabling researchers to detect biomarker concentrations previously considered undetectable. This technical guide examines these cutting-edge approaches, providing researchers with actionable methodologies to enhance detection sensitivity for low-abundance targets in cancer research.
Advanced Techniques for Enhanced Sensitivity
Novel PCR Methodologies
Digital PCR (dPCR) represents a fundamental departure from conventional qPCR principles, enabling absolute quantification of nucleic acids without requiring standard curves. This third-generation PCR technology partitions a single PCR reaction into thousands to millions of parallel nanoliter-scale reactions, so that each partition contains either zero, one, or a few target molecules according to a Poisson distribution. Following end-point amplification, the fraction of positive partitions is counted, and the target concentration is calculated using Poisson statistics [74]. This approach provides several critical advantages for detecting rare biomarkers: it eliminates amplification efficiency biases, reduces background noise from competing reactions, and enables detection of single molecules. dPCR demonstrates particular utility in liquid biopsy applications for detecting rare mutations within a background of wild-type DNA, monitoring treatment response through ctDNA quantification, and detecting minimal residual disease with a sensitivity that often exceeds conventional qPCR [74].
The RT-Hairpin Occlusion System (RT-HOS) is an innovative one-pot, one-step multiplex miRNA detection method that simultaneously utilizes both High-Fidelity DNA polymerase and Taq DNA polymerase. This system integrates three functions into a single platform: reverse transcription primer, fluorescent probe, and reverse primer. The RT-HOS consists of an RT fluorescent primer labeled with a fluorescent group at its 5' end and a hairpin quencher labeled with a quencher group at its 3' end. This configuration enables reverse transcription at higher temperatures, significantly enhancing specificity and accelerating the reaction process. Compared to traditional two-step stem-loop RT-qPCR, this method demonstrates a wide linear dynamic range from 7.5 × 10¹ to 7.5 × 10⁸ copies/reaction while maintaining excellent specificity for distinguishing closely related miRNA sequences [16].
Emerging Amplification-Free Technologies
CRISPR-CasΦ-based detection (TCC method) represents a revolutionary approach that achieves ultrasensitive detection without target amplification. This method leverages a dual-stem-loop DNA amplifier to enhance non-specific collateral enzymatic cleavage by CRISPR-CasΦ. When target pathogen DNA binds to its complementary gRNA in the CRISPR-CasΦ complex, it activates collateral DNA-cleavage capability, enabling CasΦ to cleave stem-loops in the amplifier. The cleavage product then binds complementary gRNA in another CRISPR-CasΦ complex, activating more CasΦ molecules in a cascading amplification effect. The activated CasΦ collaterally cleaves an oligonucleotide linker between a fluorophore and quencher, releasing the fluorophore to generate a fluorescent signal. This cycle of stem-loop cleavage, CasΦ activation, and fluorescence recovery exponentially amplifies the detection signal, achieving a remarkable detection limit of 0.11 copies/μL – superior to conventional qPCR – within just 40 minutes [75].
Table 1: Comparison of Ultra-Sensitive Detection Techniques
| Technique | Principle | Detection Limit | Time Required | Key Advantages |
|---|---|---|---|---|
| Digital PCR | Partitioning & Poisson statistics | Varies by target; single-molecule sensitivity | 2-4 hours | Absolute quantification, high precision, resistant to inhibitors |
| RT-HOS Multiplex qPCR | Integrated reverse transcription & detection | 7.5 × 10¹ copies/reaction | ~1 hour | One-pot protocol, high specificity, multiplexing capability |
| CRISPR-CasΦ (TCC) | Collateral cleavage amplification | 0.11 copies/μL | 40 minutes | Amplification-free, rapid, ultra-sensitive |
| Standard RT-qPCR | Fluorescence monitoring during amplification | ~10³ copies/reaction | 1-2 hours | Established protocols, cost-effective, high throughput |
Experimental Protocols for Implementation
RT-HOS Multiplex qPCR for miRNA Detection
Protocol Overview: This protocol enables simultaneous detection of multiple miRNA targets in a single reaction vessel, significantly reducing processing time and potential contamination compared to traditional two-step methods [16].
Materials and Reagents:
- High-Fidelity DNA polymerase OR Taq DNA polymerase (commercial preparations)
- HPLC-purified RT fluorescent primers (Sangon Biological Corporation)
- Hairpin quenchers with complementary regions (~20 bp)
- Target miRNAs and miRNA precursors
- dNTP mixture
- Appropriate buffer systems
Procedure:
- Reaction Setup: Prepare a master mix containing either High-Fidelity DNA polymerase or Taq DNA polymerase, dNTPs, and reaction buffer according to manufacturer specifications.
- Primer System Addition: Add RT fluorescent primers and hairpin quenchers at optimized concentrations (typically 100-400 nM each). The RT fluorescent primer is labeled with a fluorescent group at its 5' end, while the hairpin quencher is labeled with a quencher group at its 3' end.
- Sample Introduction: Add extracted RNA samples (serum, plasma, or tissue extracts) to the reaction mixture.
- Reverse Transcription: Incubate at 50-60°C for 15-30 minutes to allow reverse transcription to proceed. The RT-HOS system permits higher temperature reverse transcription than conventional methods, enhancing specificity.
- Amplification: Perform 40-45 cycles of PCR with optimized annealing temperatures specific to your target miRNAs.
- Detection: Monitor fluorescence in real-time during the amplification phase. The mechanism relies on the separation of fluorophore and quencher during amplification, generating a detectable signal.
Critical Optimization Parameters:
- Primer and quencher concentrations require empirical optimization for each miRNA target
- Annealing temperature should be determined through gradient PCR
- Magnesium concentration significantly impacts reaction efficiency and specificity
- The complementary region between RT fluorescent primer and hairpin quencher should be approximately 20 bp for stable hybridization
Digital PCR Setup for Rare Mutation Detection
Protocol Overview: This protocol details the droplet digital PCR (ddPCR) workflow for detecting low-frequency mutations in ctDNA from liquid biopsies, enabling absolute quantification without standard curves [74].
Materials and Reagents:
- ddPCR system (commercial platform such as Bio-Rad QX200)
- Supermix for probes (without dUTP)
- Target-specific primer-probe sets (FAM and HEX/VIC labeled)
- Droplet generation oil
- DG8 cartridges and gaskets
- ctDNA extracted from plasma samples
Procedure:
- Reaction Preparation: Prepare a 20μL reaction mix containing ddPCR Supermix, primers, probes, and template DNA (typically 1-10 ng of ctDNA).
- Droplet Generation: Assemble the DG8 cartridge with the reaction mixture and droplet generation oil. Place in the droplet generator to create approximately 20,000 nanoliter-sized droplets.
- PCR Amplification: Transfer the emulsified samples to a 96-well PCR plate and perform endpoint PCR amplification using the following cycling conditions: 95°C for 10 minutes (enzyme activation), followed by 40 cycles of 94°C for 30 seconds and 60°C for 60 seconds (annealing/extension), with a final 98°C incubation for 10 minutes (enzyme deactivation). Use a ramp rate of 2°C/second.
- Droplet Reading: Place the amplified plate in the droplet reader, which measures fluorescence in each droplet individually.
- Data Analysis: Use companion software to analyze the fluorescence data and apply Poisson statistics to determine the absolute concentration of the target molecule in the original sample.
Critical Optimization Parameters:
- Template quantity must be optimized to avoid saturation (ideal: 1,000-10,000 copies per reaction)
- Annealing temperature should be optimized through gradient experiments
- Probe concentrations typically range from 250-500 nM
- Partition number directly impacts sensitivity (more partitions = higher sensitivity)
Diagram 1: Digital PCR workflow for absolute quantification of nucleic acid targets, demonstrating the partitioning process that enables single-molecule sensitivity.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Ultra-Sensitive Detection
| Reagent/Category | Specific Examples | Function & Importance | Technical Notes |
|---|---|---|---|
| Specialized Polymerases | High-Fidelity DNA polymerase, Taq DNA polymerase | DNA amplification with proofreading (High-Fidelity) or probe compatibility (Taq) | High-Fidelity offers 3'-5' exonuclease activity; Taq is compatible with hydrolysis probes [16] |
| Engineered Primer Systems | RT-HOS primers, Stem-loop primers | Enable specific reverse transcription and detection of short targets like miRNAs | RT-HOS integrates three functions: RT primer, fluorescent probe, and reverse primer [16] |
| CRISPR Components | CasΦ protein, gRNA, TCC amplifier | Target recognition and signal amplification without target pre-amplification | CasΦ is a compact Cas12 variant (∼80 kDa) with trans-cleavage activity [75] |
| Fluorescent Reporters | TaqMan probes, Molecular beacons | Generate quantifiable signal during amplification | Dual-labeled probes (fluorophore-quencher) provide specific detection |
| Reference Genes | IbACT, IbARF, IbCYC (validated in studies) | Normalization of RT-qPCR data for accurate quantification | Stability across tissues/conditions is critical; must be empirically validated [76] |
| Partitioning Media | Droplet generation oil, Microchamber arrays | Create nanoreactors for digital PCR | Water-in-oil emulsions require proper surfactant stabilization [74] |
The evolving landscape of ultra-sensitive detection technologies is increasingly intersecting with artificial intelligence (AI) approaches, creating powerful synergies for liquid biopsy applications. AI and machine learning algorithms can analyze complex RNA expression patterns from high-throughput sequencing data, identifying subtle yet clinically significant signatures that conventional analysis might miss [77]. These computational approaches enhance the discriminatory power of molecular diagnostics, enabling more accurate cancer subtype classification, prognosis prediction, and treatment response monitoring. The integration of multi-omics data through AI-driven platforms represents a promising frontier for developing comprehensive diagnostic signatures that improve early detection rates while minimizing false positives.
The selection of appropriate liquid biopsy sources presents another critical consideration for optimizing detection sensitivity. While blood remains the most common source, local fluids such as urine, bile, and cerebrospinal fluid often offer higher biomarker concentrations for cancers in proximity to these fluids [26]. For example, urine-based tests for bladder cancer detection demonstrate significantly higher sensitivity (87%) compared to plasma-based approaches (7%) for TERT mutation detection [26]. This principle of source selection emphasizes the importance of anatomical proximity when designing detection strategies for specific cancer types.
In conclusion, overcoming the challenge of low biomarker abundance requires a multifaceted approach combining technological innovations in PCR methodologies, novel detection systems like CRISPR-CasΦ, appropriate reagent selection, and strategic experimental design. The techniques outlined in this guide provide researchers with powerful tools to push detection boundaries, enabling the sensitive and specific identification of rare molecular targets in liquid biopsies. As these technologies continue to evolve and integrate with computational approaches, they hold immense promise for transforming cancer diagnostics through earlier detection, improved monitoring, and more personalized treatment strategies.
Reverse transcription quantitative polymerase chain reaction (RT-qPCR) is considered the gold standard for accurate, sensitive, and rapid measurements of gene expression, playing a crucial role in liquid biopsy cancer detection research [78] [79]. This technique enables quantitative measurement of RNA levels, including mRNAs, small RNAs, and other noncoding RNAs, which is fundamental for understanding gene expression regulation and for diagnosing and monitoring diseases [5]. The accuracy and efficiency of RT-qPCR depend heavily on proper experimental design and data analysis, with normalization standing as an absolute necessity to achieve reliable results [79].
Normalization controls for technical variations inherent to the RT-qPCR process, including differences in RNA extraction efficiency, cDNA synthesis yield, and PCR amplification efficiency. Among various normalization methods, the use of reference genes—also termed endogenous control genes—is considered one of the most effective strategies [79]. These genes serve as internal reaction controls and must be unaffected by experimental conditions while showing minimal variability between tissues and physiological states of the organism [79]. For liquid biopsy applications in oncology, where sample quantity is often limited and analyte concentrations can be extremely low, selecting appropriate endogenous controls becomes particularly critical for obtaining meaningful data that can inform clinical decisions.
The Critical Importance of Reference Gene Validation
The misconception that so-called "housekeeping genes" maintain constant expression across all conditions has been decisively refuted by numerous studies. It is now well-established that the expression levels of commonly used reference genes vary significantly across different tissue types, between experimental treatments, in various disease states including cancer, and even across different cell types [78] [79]. This variability is especially pronounced in oncological research, where different cancer types exhibit distinct physiologies and involve complex genetic and external factors [79].
Gene expression can be influenced by numerous factors including tissue type, developmental stage, abiotic stress, diseases, infections, and particularly tumors [79]. Therefore, experimental confirmation of reference gene stability has become a standard requirement in rigorous molecular studies [79]. This is especially true for liquid biopsy research, where blood-based biomarkers may originate from diverse tissue sources and exist at low concentrations, potentially affecting the stability of commonly used reference genes.
Without proper validation, normalization using inappropriate reference genes can lead to misinterpretation of results and incorrect conclusions—a particularly dangerous scenario in cancer detection research where clinical decisions may hinge on accurate gene expression data. The literature contains examples of validated reference genes for specific cancer types, including MRPL19 and PPIA for breast cancer, and RPL30, MT-ATP6, and ACTB for endometrial cancer [79]. However, the suitability of these genes cannot be extrapolated to liquid biopsy applications without empirical validation.
Table 1: Consequences of Improper Normalization in Liquid Biopsy Research
| Error Type | Impact on Data Interpretation | Clinical Implications |
|---|---|---|
| False Positives | Overestimation of biomarker expression | Incorrect disease detection |
| False Negatives | Underestimation of biomarker expression | Missed early cancer detection |
| Reduced Statistical Power | Inability to distinguish true biological differences | Unreliable clinical validation |
| Poor Reproducibility | Inconsistent results across studies | Failed translation to clinic |
Candidate Endogenous Control Genes
Commonly Used Reference Genes
Research studies have evaluated numerous candidate reference genes for their stability in various cancer contexts. These genes typically participate in basic cellular maintenance functions and are selected based on their presumed stable expression across biological conditions. Among the most frequently studied genes are GUSB (glucuronidase β), ACTB (β-actin), GAPDH (glyceraldehyde-3-phosphate dehydrogenase), B2M (β-2-microglobulin), PPIA (peptidylprolyl isomerase A), RPL29 (ribosomal protein L29), HPRT1 (hypoxanthine phosphoribosyltransferase 1), ALAS1 (5′-aminolevulinate synthase 1), HMBS (hydroxymethylbilane synthase), TBP (TATA-box binding protein), PUM1 (pumilio RNA binding family member 1), and 18S rRNA (18S ribosomal RNA) [78].
Each of these genes plays fundamental roles in cellular function: GUSB is involved in glycosaminoglycan degradation; ACTB is a cytoskeletal structural protein; GAPDH participates in glycolysis; B2M is a component of major histocompatibility complex class I molecules; PPIA facilitates protein folding; RPL29 is a ribosomal component; HPRT1 is involved in purine salvage; ALAS1 catalyzes the first step in heme synthesis; HMBS participates in heme biosynthesis; TBP is a general transcription factor; PUM1 regulates mRNA stability and translation; and 18S rRNA is a component of the small ribosomal subunit.
Performance in Cancer Studies
The expression stability of these candidate genes varies significantly across different cancer types and sample sources. In a comprehensive study on human tongue carcinoma, researchers evaluated 12 common reference genes in Tca-8113 and CAL-27 cell lines along with 8 tongue carcinoma tissue samples [78]. The stability of candidate genes was determined using three statistical algorithms—geNorm, NormFinder, and BestKeeper—with results demonstrating considerable variability between the different software programs [78].
For the combined cell line and tissue group, the recommended combination was ALAS1 + GUSB + RPL29 [78]. In the cell line group specifically, B2M + RPL29 showed optimal stability, while for the tissue group alone, PPIA + HMBS + RPL29 constituted the best combination [78]. This study notably found that GUSB performed well enough to be included in the optimal combination for mixed sample types, supporting its potential utility in liquid biopsy research where multiple sample types may be analyzed.
In acute leukemia gene expression studies, researchers validated a different panel of endogenous controls in peripheral blood and bone marrow samples [79]. Their analysis identified that the endogenous set composed of ACTB, ABL, TBP, and RPLP0 demonstrated good performances and stable expressions between the analyzed groups [79]. Conversely, GAPDH and HPRT could not be classified as good reference genes as they presented high standard deviation and great variability between groups, indicating low stability [79].
Table 2: Reference Gene Performance Across Cancer Types
| Cancer Type | Most Stable Genes | Least Stable Genes | Sample Type |
|---|---|---|---|
| Tongue Carcinoma [78] | ALAS1, GUSB, RPL29, B2M, PPIA, HMBS | Not specified | Cell lines, Tissue |
| Acute Leukemia [79] | ACTB, ABL, TBP, RPLP0 | GAPDH, HPRT | Peripheral blood, Bone marrow |
Experimental Design for Validation
Sample Selection and Preparation
Proper experimental design begins with thoughtful sample selection that represents the biological variability expected in the actual study. For liquid biopsy cancer detection research, this should include samples from multiple individuals across different disease stages, and if possible, various cancer types. Appropriate control samples (e.g., healthy donors) should also be included to ensure the candidate reference genes show minimal variation across both normal and disease states.
In the tongue carcinoma study, researchers used two human tongue carcinoma cell lines (Tca-8113 and CAL-27) and 8 tongue carcinoma tissue samples with a mean age of 56.75±4.06 years, including 6 males and 2 females with various TNM stages [78]. The acute leukemia study analyzed samples from 24 AML patients, 25 ALL adults, 25 pediatric ALL patients, and 15 controls, including both peripheral blood and bone marrow samples [78]. This diverse sampling strategy provides confidence that the validated reference genes will perform consistently across different biological conditions.
For RNA extraction, the TRIzol reagent method has been successfully employed in multiple reference gene validation studies [78] [79]. After extraction, RNA concentration and purity should be measured using spectrophotometry (e.g., NanoDrop 2000), and RNA integrity should be verified before proceeding to cDNA synthesis [78]. The cDNA synthesis reaction is typically performed using random primers, oligo(dT) primers, or gene-specific primers with reverse transcriptase and reaction components including dNTPs, RNase inhibitors, and MgCl2 [5].
Primer Design and Validation
Proper primer design is crucial for ensuring precise detection and quantification of target sequences in RT-qPCR reactions [5]. Key considerations for optimal primer design include:
- Target Sequence: Primers should be designed to span exon-exon junctions where possible to avoid amplification of genomic DNA [5].
- Length and GC Content: The optimal length of primers is 18-25 nucleotides, with GC content of 40-60% for stable binding [5].
- Amplicon Length: The preferable distance between forward and reverse primers is 70-200 base pairs to ensure efficient qPCR [5].
- Secondary Structures: Primers should be designed to avoid sequences that form secondary structures which interfere with amplification [5].
Several bioinformatics tools are available to assist with primer design, including NCBI's Basic Local Alignment Search Tool for ensuring primer specificity, Integrated Genome Browser for visualization of genomic landscape, OligoAnalyzer for calculating melting temperature and GC content, and Primer3PLUS for predicting secondary structures [5].
After primer design, validation should include checking amplification efficiency through standard curves, verifying single amplification products through melt curve analysis, and confirming expected amplicon size through gel electrophoresis [78].
Diagram 1: Experimental Workflow for Reference Gene Validation. This flowchart outlines the key steps in validating endogenous control genes for RT-qPCR studies.
Data Analysis Methods
Statistical Algorithms for Stability Assessment
A robust reference gene validation study employs multiple statistical algorithms to comprehensively evaluate gene expression stability. Three widely used software programs include:
geNorm: This algorithm calculates a gene expression stability measure (M) for each candidate reference gene based on the average pairwise variation between all genes tested. Genes with lower M values have more stable expression. geNorm also determines the optimal number of reference genes needed for accurate normalization by calculating pairwise variation (V) between sequential normalization factors [78] [79].
NormFinder: This method evaluates the expression stability of candidate reference genes by considering both intra-group and inter-group variation. It provides a stability value for each gene, with lower values indicating greater stability. NormFinder is particularly valuable for identifying the best single reference gene when multiple sample groups are included in the study [78] [79].
BestKeeper: This algorithm determines the most stable reference genes based on the coefficient of variance (CV) and standard deviation (SD) of the Ct values. Genes with lower CV and SD values are considered more stable. BestKeeper can also calculate an index based on the geometric mean of the best-performing genes [78].
Each algorithm has distinct strengths, and using multiple approaches provides a more comprehensive assessment of gene stability. The tongue carcinoma study found that results from the three software programs were variable following comparison, highlighting the importance of using complementary methods [78].
Technical and Biological Replication
The question of technical replication in RT-qPCR has been systematically evaluated in a comprehensive study analyzing 71,142 Ct values from 1,113 RT-qPCR runs [80]. This research revealed several important findings challenging conventional assumptions:
- No correlation was found between Ct values (indicating template concentration) and the coefficient of variation, contradicting the common assumption that low template concentration inflates technical variability [80].
- Inexperienced operators exhibited only slightly higher technical variability than experienced operators, with both groups producing replicates within widely accepted precision limits [80].
- Dye-based detection (SYBR Green) showed greater variability than probe-based detection (TaqMan) [80].
- Instrument calibration had negligible effects on replicate consistency [80].
Most significantly, the study demonstrated that duplicate or single replicates sufficiently approximated triplicate means, suggesting that moving from technical triplicates to duplicates or singles can reduce reagent use, instrument time, and labor by 33-66% without substantially affecting precision [80]. However, the authors emphasize that biological replication remains indispensable for capturing true biological variability and enabling valid statistical inference [80].
Table 3: Comparison of Reference Gene Validation Algorithms
| Algorithm | Statistical Approach | Primary Output | Key Strength |
|---|---|---|---|
| geNorm [78] | Pairwise comparison | Stability measure (M) | Determines optimal number of reference genes |
| NormFinder [78] | Model-based approach | Stability value | Considers sample subgroup variations |
| BestKeeper [78] | Correlation analysis | Coefficient of variation | Based on raw Ct values without transformation |
Implementation in Liquid Biopsy Research
Application to Cancer Detection
Liquid biopsy represents a promising minimally invasive approach for cancer detection and monitoring, with RT-qPCR serving as a key analytical tool for measuring circulating RNA biomarkers. Implementing proper normalization strategies is particularly challenging in liquid biopsy due to the low concentration of circulating nucleic acids, the heterogeneous nature of blood samples, and the potential lack of appropriate reference genes with consistent expression between tissue and blood.
For gene expression analysis in peripheral blood and bone marrow samples from acute leukemia patients, the recommended endogenous gene set includes ACTB, ABL, TBP, and RPLP0 [79]. Researchers may choose two to three of these housekeeping genes to perform data normalization, following the geNorm recommendation that the optimal number of reference genes is determined by the pairwise variation V value [79].
The finding that GUSB was included in the optimal reference gene combination for tongue carcinoma (across cell lines and tissues) suggests it may have broader utility in cancer detection studies [78]. However, this must be empirically validated for each specific liquid biopsy application, as gene expression stability can vary significantly between different biological matrices.
Practical Implementation Framework
Based on the reviewed literature, we propose the following framework for implementing normalization strategies in liquid biopsy cancer detection research:
Select Candidate Genes: Choose 4-8 candidate reference genes from the literature, including both traditional housekeeping genes and genes previously validated in similar sample types. GUSB, ACTB, TBP, and RPLP0 represent promising starting points based on current evidence [78] [79].
Include Diverse Samples: Validate candidate genes across the full range of sample types expected in the actual study, including different disease stages, treatment statuses, and appropriate controls.
Use Multiple Algorithms: Assess expression stability using at least two different statistical algorithms (e.g., geNorm and NormFinder) to obtain a comprehensive evaluation.
Determine Optimal Number: Calculate the pairwise variation V value using geNorm to determine the optimal number of reference genes for normalization. While multiple genes are typically recommended, practical constraints may influence the final choice.
Validate Normalization Strategy: Confirm that the selected reference genes remain stable under the specific experimental conditions by testing their performance with known positive and negative controls.
Diagram 2: Reference Gene Selection and Validation Process. This workflow illustrates the multi-step process for identifying and validating appropriate endogenous control genes for RT-qPCR normalization.
Research Reagent Solutions
Table 4: Essential Reagents for Reference Gene Validation Studies
| Reagent/Category | Specific Examples | Function in RT-qPCR | Considerations for Liquid Biopsy |
|---|---|---|---|
| RNA Extraction | TRIzol Reagent [78] [79] | Isolation of total RNA from biological samples | Efficiency with low-input samples critical |
| Reverse Transcriptase | M-MuLV Reverse Transcriptase [78] | Converts RNA to complementary DNA (cDNA) | High efficiency needed for degraded samples |
| qPCR Master Mix | SYBR Green, TaqMan Master Mix [5] [80] | Provides enzymes and reagents for amplification | Probe-based offers higher specificity |
| Reference Gene Assays | Pre-designed primer/probe sets [78] | Target-specific amplification | Should span exon-exon junctions |
| Quality Control Tools | NanoDrop spectrophotometer [78] | Assess RNA concentration and purity | Essential for sample qualification |
Proper normalization using validated endogenous controls represents a critical methodological foundation for reliable RT-qPCR data in liquid biopsy cancer detection research. The selection of appropriate reference genes must be empirically determined for each specific experimental system, as expression stability varies significantly across different biological matrices and disease states. Based on current evidence, GUSB demonstrates promise as a component of multi-gene normalization panels in oncology applications, but should be validated alongside other candidates such as ACTB, TBP, and RPLP0 in the context of liquid biopsy samples.
The implementation of a systematic validation framework incorporating multiple statistical algorithms and representative sample types will enhance the accuracy and reproducibility of gene expression measurements in circulating biomarkers. As liquid biopsy technologies continue to evolve toward clinical application, rigorous normalization strategies will play an increasingly important role in ensuring the reliability of molecular diagnostics for cancer detection and monitoring.
Limit of Detection (LOD) and Standardization Challenges
Liquid biopsy, the analysis of tumor-derived material in body fluids, represents a paradigm shift in oncology, enabling non-invasive diagnosis and monitoring of cancer. Limit of Detection (LOD) defines the lowest concentration of an analyte that can be reliably distinguished from zero and is particularly challenging in liquid biopsy due to the extremely low abundance of circulating tumor DNA (ctDNA) in early-stage cancer. For context, the ctDNA fraction can be less than 0.1% in early-stage disease, creating significant technical hurdles for detection technologies [26]. The standardization of pre-analytical, analytical, and post-analytical processes is essential to ensure reliability and reproducibility of liquid biopsy results across laboratories [81]. Within this field, RT-qPCR (Reverse Transcription Quantitative Polymerase Chain Reaction) maintains relevance due to its accessibility, cost-effectiveness, and rapid turnaround time, making it suitable for targeted mutation detection and minimal residual disease monitoring [82] [83]. This review examines the LOD challenges and standardization efforts specifically within the context of RT-qPCR-based liquid biopsy applications for cancer detection.
LOD Performance of Detection Technologies
The sensitivity required for liquid biopsy applications varies significantly depending on the clinical context. While monitoring tumor burden in advanced cancer may require detection of variant allele frequencies (VAF) of 1-5%, early detection and minimal residual disease monitoring may need sensitivity down to 0.01% VAF or even lower [84] [82]. Different technologies offer varying levels of sensitivity, as summarized in Table 1.
Table 1: LOD Performance of Key Liquid Biopsy Detection Technologies
| Technology | Theoretical LOD | Reported LOD in Studies | Key Applications |
|---|---|---|---|
| RT-qPCR | ~0.1-1% VAF | 0.32% VAF in colorectal cancer [83] | Targeted mutation detection, gene expression analysis |
| Digital PCR (dPCR) | ~0.001-0.1% VAF | 1 in 180,000 (∼0.0006%) for EGFR L858R [84] | Low frequency mutation detection, target quantification |
| Next-Generation Sequencing (NGS) | ~0.1-5% VAF (varies with coverage) | 0.15% VAF for SNV/Indels in validated CGP assay [85] | Comprehensive genomic profiling, multi-cancer detection |
| Advanced qPCR Methods (PNB-qPCR) | ~0.003% VAF | 0.003% for KRAS mutations in colorectal cancer [83] | Ultra-sensitive detection of specific mutations |
The relationship between sequencing coverage depth and detection sensitivity is particularly important for NGS methods. As illustrated in Figure 1, achieving a LOD of 3% VAF with a false positive probability of 0.001 requires a minimum coverage depth of 1,650 reads [86]. This coverage ensures sufficient statistical power for reliable mutation detection at specific variant allele frequencies.
Figure 1: The relationship between NGS coverage depth and Limit of Detection (LOD). This diagram shows how deeper sequencing coverage enables detection of lower variant allele frequencies (VAF).
RT-qPCR demonstrates particular utility in specific clinical contexts despite generally higher LOD compared to digital methods. In neuroblastoma, RT-qPCR detection of bone marrow infiltration >10% at diagnosis was prognostic for survival, with adjusted hazard ratios of 1.82 for event-free survival and 2.04 for overall survival [82]. Furthermore, any post-induction RT-qPCR positivity correlated with poor outcomes, demonstrating the clinical relevance of this technology even with its sensitivity limitations [82].
Key Standardization Challenges in Liquid Biopsy
Pre-analytical Variables
Pre-analytical factors introduce significant variability in liquid biopsy analysis. Sample collection procedures must be standardized, as the choice of blood collection tubes, time-to-processing, and centrifugation protocols can dramatically affect ctDNA yield and quality [81]. Sample type selection is equally critical; while plasma is generally preferred for ctDNA analysis due to lower genomic DNA contamination, serum may yield higher total cell-free DNA concentrations [26]. The time-to-processing is particularly important for ctDNA, which has a short half-life ranging from minutes to a few hours, necessitating rapid and standardized processing protocols [26].
Analytical Challenges
During the analytical phase, several factors challenge standardization. Input DNA quality and quantity significantly impact assay performance, with recommendations for minimum input amounts often lacking in laboratory-developed tests [86]. The selection of appropriate controls is essential for both discovery and validation phases, yet control materials are not consistently implemented across laboratories [26]. Assay-specific errors occurring during DNA processing and library preparation add to the intrinsic sequencing errors, creating composite error rates that differ between laboratories and platforms [86]. This variability complicates inter-laboratory comparisons and multicenter trial interpretations.
Post-analytical and Data Interpretation Hurdles
Data analysis and interpretation present substantial standardization challenges. Variant calling thresholds must balance sensitivity and specificity, with insufficiently standardized parameters leading to both false positives and false negatives [86]. Reporting standards for key parameters like coverage depth, DNA input quality, and limit of detection are inconsistently applied, hindering comparative analysis across studies [86]. The clinical interpretation of low VAF variants remains challenging, particularly for subclonal mutations that may have clinical significance but appear at frequencies near the assay's LOD [86].
Experimental Protocols for LOD Determination
Digital PCR LOD Validation Protocol
Determining the LOD for dPCR assays requires a rigorous approach as demonstrated for EGFR mutation detection [84]. The process begins with sample preparation, creating a mutation titration series by spiking mutant plasmid DNA (e.g., EGFR T790M or L858R) into wild-type genomic DNA at varying ratios (e.g., 0.5-1.0%, 0.05-0.1%, 0.005-0.01%, and 0.0005-0.001%) [84]. The PCR reaction setup follows with 50μl reactions containing approximately 20,000 copies/μl of genomic DNA, 1× TaqMan Genotyping Master Mix, 0.2μM hydrolysis probes, and 0.9μM primers [84]. For data analysis, the false-positive rate is determined using wild-type-only samples, while the titration series establishes linearity and sensitivity. The LOD is statistically calculated with 95% confidence limits, considering both the false-positive rate and the amount of amplifiable DNA analyzed [84].
Advanced qPCR Method: PNB-qPCR Protocol
The PNB-qPCR (Pooled, Nested, WT-Blocking qPCR) protocol exemplifies how methodological innovations can dramatically improve LOD [83]. This protocol employs first-round PCR with wild-type specific blocking primers to enrich mutant fragments, significantly reducing background noise [83]. The pooling strategy then distributes the sample into five separate first-round PCRs, with products pooled for second-round analysis, reducing variance and improving quantification accuracy [83]. The second-round qPCR uses mutation-specific ARMS primers and short LNA probes to amplify short amplicons, enhancing detection of fragmented ctDNA [83]. This comprehensive approach improved the limit of quantification (LOQ) to a median of 6.25 copies, ranging from 3.1 to 12.5 copies, substantially enhancing sensitivity over standard qPCR methods [83].
Figure 2: PNB-qPCR Workflow. This diagram illustrates the multi-step process of Pooled, Nested, Blocking qPCR for ultra-sensitive mutation detection.
NGS Coverage Depth Determination Protocol
For NGS assays, determining appropriate coverage depth is essential for achieving the desired LOD [86]. The process begins with defining requirements, including the intended LOD, tolerance for false positives/false negatives, and the assay's error rate [86]. Binomial distribution calculations determine the probability of false positives and false negatives for given error rates and intended LOD, establishing thresholds for variant calling [86]. Coverage validation through dilution experiments confirms theoretical calculations, as demonstrated by TP53 mutation detection experiments that revealed 30% false negatives at 100x coverage for 10% VAF detection [86]. Finally, threshold adjustment ensures that the minimum number of variant-supporting reads provides sufficient statistical confidence for mutation calling at the desired LOD [86].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Liquid Biopsy Assays
| Reagent/Category | Function | Example Applications |
|---|---|---|
| Blood Collection Tubes with Stabilizers | Preserves cell-free DNA by preventing white blood cell lysis and nuclease degradation | Standardized plasma collection for ctDNA analysis [81] [26] |
| Wild-Type Blocking Primers | Enriches mutant alleles during PCR amplification by suppressing wild-type amplification | PNB-qPCR protocols for ultra-sensitive mutation detection [83] |
| Hydrolysis Probes (TaqMan, LNA) | Enables specific detection and quantification of amplified targets during qPCR | EGFR L858R and T790M mutation detection [84] |
| Reference Standard Materials | Provides known mutation status and abundance for assay validation and quality control | Linearized plasmid controls with specific mutations [84] |
| NGS Library Preparation Kits | Facilitates target enrichment and adapter ligation for next-generation sequencing | Comprehensive genomic profiling assays [85] |
The field of liquid biopsy continues to evolve with emerging technologies pushing detection limits to unprecedented levels. Multi-cancer early detection (MCED) tests represent the next frontier, though none have yet received full regulatory approval due to challenges in achieving optimal sensitivity for early-stage cancers while minimizing false positives [87]. DNA methylation biomarkers offer particular promise due to their early emergence in tumorigenesis and stability, with several blood-based tests achieving FDA Breakthrough Device designation [26]. The International Society of Liquid Biopsy (ISLB) has initiated global efforts to establish minimal requirements for ctDNA testing, focusing on standardizing pre-analytical, analytical, and post-analytical phases [81]. As these efforts mature and technologies continue to advance, liquid biopsy promises to revolutionize cancer detection and monitoring, potentially enabling population-level screening through sufficiently sensitive, specific, and cost-effective assays.
Optimizing Primer/Probe Design for Specificity and Efficiency
In liquid biopsy cancer detection research, Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) serves as a powerful tool for identifying tumor-specific biomarkers, such as circulating tumor cells (CTCs) and cell-free nucleic acids, in patient blood samples [88] [89]. The success of these assays hinges critically on the specificity and efficiency of primer and probe design. Optimal design minimizes off-target amplification and maximizes reliable detection of low-abundance targets, which is paramount given the fragmented nature of circulating tumor DNA (cfDNA) and the low concentrations of analytes in body fluids [88]. This guide synthesizes foundational principles and advanced strategies to equip researchers with the knowledge to develop robust RT-qPCR assays for sensitive liquid biopsy applications.
Core Principles of Primer and Probe Design
Adherence to established design parameters is the first defense against inefficient amplification and non-specific detection, which are major pitfalls in liquid biopsy where target material is often scarce [90] [91] [92].
Primer Design Specifications
Table 1: Key Design Parameters for PCR Primers
| Parameter | Ideal Specification | Rationale |
|---|---|---|
| Length | 18–30 bases [90] | Balances specificity with practical synthesis. |
| Melting Temperature (Tm) | 60–64°C; ideal 62°C [90] | Ensures efficient annealing under standard cycling conditions. |
| Tm Difference (Forward vs. Reverse) | ≤ 2–3°C [90] [91] | Allows both primers to bind simultaneously and efficiently. |
| GC Content | 40–60%; ideal ~50% [91] [92] | Provides sufficient sequence complexity while avoiding stable secondary structures. |
| 3' End Stability | Avoid 3+ G/C residues (GC clamp) [92] | Prevents mis-priming at non-target sites; a single C or G is acceptable. |
| Self-Complementarity | ΔG > -9.0 kcal/mol [90] | Minimizes hairpin formation and primer-dimer artifacts. |
Hydrolysis (TaqMan) Probe Design Specifications
Table 2: Key Design Parameters for Hydrolysis Probes
| Parameter | Ideal Specification | Rationale |
|---|---|---|
| Length | 15–30 nucleotides [90] [91] | Ensures sufficient quenching of the fluorophore. |
| Melting Temperature (Tm) | 5–10°C higher than primers [90] [91] | Guarantees probe binds before primers, ensuring all amplicons are probed. |
| Location | Close to, but not overlapping, a primer-binding site [90] | Maximizes fluorescence signal from probe cleavage. |
| GC Content | 40–60% [91] | Similar rationale as for primers. |
| 5' End Base | Avoid Guanine (G) [90] [91] | Prevents quenching of the 5' fluorophore. |
| Quenching Strategy | Double-quenched probes recommended [90] | Lowers background fluorescence and increases signal-to-noise ratio. |
Advanced Strategies for Liquid Biopsy Applications
Liquid biopsy presents unique challenges, including high background of wild-type DNA and ultra-low target frequency. Advanced design and validation strategies are required to address these.
Ensuring Specificity and Preventing Genomic DNA Amplification
A primary concern in RT-qPCR is the amplification of contaminating genomic DNA (gDNA), which can lead to false positives. Two key strategies mitigate this risk:
- Design Across Exon-Exon Junctions: Designing primers so that the primer binding sites are located on different exons forces the amplification of cDNA but not gDNA [90] [92]. This is because the intronic sequence in gDNA is too large to be efficiently amplified under standard qPCR conditions.
- DNase Treatment: Treating RNA samples with DNase I before reverse transcription provides a biochemical method to remove residual gDNA [91].
Assay Validation and Performance Metrics
Once a candidate assay is designed, rigorous validation is essential. The following protocol and metrics ensure the assay is fit for purpose, especially for detecting minimal residual disease (MRD) [89].
Experimental Protocol: Assay Validation for Liquid Biopsy
- RNA Extraction & cDNA Synthesis: Use high-quality, purified RNA. Treat samples with DNase I. Synthesize cDNA using random hexamers and MMLV transcriptase [89].
- Standard Curve Generation: Serially dilute (e.g., 1:10 dilutions) a sample with known target concentration. Run the qPCR assay with these dilutions in triplicate [91].
- Efficiency and Linearity Calculation: The slope of the log-linear plot of the standard curve (Cq vs. log template concentration) is used to calculate PCR efficiency (E) using the formula: ( E = (10^{-1/slope} - 1) \times 100\% ). The correlation coefficient (R²) indicates linearity [91].
- Specificity Confirmation: Verify amplicon size via gel electrophoresis or perform melt-curve analysis for dye-based assays [91].
- Sensitivity (Limit of Detection) Determination: Test a series of low-concentration samples to establish the lowest concentration at which the target can be reliably detected.
Table 3: Key Performance Metrics for a Validated qPCR Assay
| Metric | Target Value | Importance in Liquid Biopsy |
|---|---|---|
| PCR Efficiency (E) | 90–110% [91] | Indicates robust, exponential amplification; efficiencies outside this range suggest poor primer/probe design or reaction optimization. |
| Linearity (R²) | ≥ 0.99 [91] | Demonstrates accurate quantification across a wide dynamic range, crucial for measuring varying tumor burden. |
| Dynamic Range | 5–8 orders of magnitude [91] | Essential for detecting both high and ultra-low abundance targets in liquid biopsy. |
Multiplexing and Novel Methodologies
For comprehensive cancer profiling, multiplexing—detecting multiple targets in a single reaction—is highly desirable. The USE-PCR (Universal Signal Encoding PCR) platform represents a transformative approach. It uses allele-specific primers with 5' synthetic tails ("color-coded tags") that are complementary to a standardized set of universal hydrolysis probes. This decouples the detection chemistry from the specific target, enabling highly multiplexed detection of up to 32 targets simultaneously with high accuracy (up to 97.6%) and a dynamic range of four orders of magnitude, as demonstrated in cancer cell lines [93]. Key considerations for multiplexing include:
- Using non-overlapping fluorophores with distinct emission spectra [91].
- Carefully balancing primer and probe concentrations to ensure equal amplification efficiency for all targets [91].
- Validating each primer/probe set individually before combining them [91].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents and Tools for RT-qPCR Assay Development
| Item | Function/Description | Example Use Case |
|---|---|---|
| One-Step RT-qPCR Kits | Integrates reverse transcription and qPCR in a single master mix. | Simplified workflow for high-throughput gene expression analysis in liquid biopsy samples [91]. |
| Double-Quenched Probes | Hydrolysis probes with an internal quencher (e.g., ZEN/TAO) for lower background. | Essential for achieving high signal-to-noise ratios when detecting low-VAF mutations in ctDNA [90]. |
| Universal Probe Systems (e.g., USE-PCR) | Pre-optimized universal probe mix used with target-specific tailed primers. | Enables rapid development of highly multiplexed panels for detecting multiple SNVs without custom probes [93]. |
| Reference Standards | Commercially available cfDNA/ctDNA with known mutations and variant allele frequencies. | Critical for validating assay sensitivity, accuracy, and for spike-in/recovery experiments [94]. |
| Magnetic Bead-based cfDNA Kits | High-throughput, automated extraction of cfDNA from plasma. | Standardized pre-analytical workflow for obtaining high-quality, gDNA-free cfDNA for downstream qPCR [94]. |
| Primer Design Tools | Software for designing and analyzing oligonucleotides (e.g., Primer-BLAST, PrimerQuest). | In-silico checks for specificity, secondary structure, and Tm calculation during assay design [90] [95] [92]. |
The path to reliable and meaningful results in liquid biopsy research using RT-qPCR is paved by meticulous primer and probe design. By adhering to the core principles of length, Tm, and specificity, and by embracing advanced strategies like exon-junction design and novel multiplexing platforms, researchers can develop powerful assays. These assays are capable of detecting and quantifying rare cancer biomarkers with the sensitivity and precision required to guide diagnosis, monitor therapeutic response, and ultimately, improve patient outcomes.
Experimental Workflow and Strategy Diagrams
In the realm of liquid biopsy cancer detection research, establishing clinically relevant thresholds is the critical bridge between raw molecular data and actionable diagnostic, prognostic, or predictive information. Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) enables the sensitive detection of RNA biomarkers—such as circulating tumor cells (CTCs), specific mRNA signatures, or non-coding RNAs—from minimally invasive blood samples [96] [5]. However, the quantitative data generated, primarily the Cycle threshold (Ct), only gains clinical meaning when interpreted against a rigorously defined cutoff that distinguishes biological states, for instance, the presence or absence of lymph node metastasis [97]. This guide details the experimental and analytical methodologies for establishing these vital thresholds, framed within the rigorous context of clinical translation for cancer research and drug development.
Core Principles of RT-qPCR Data Analysis
Fundamental Output: The Cycle Threshold (Ct)
The cornerstone of RT-qPCR data analysis is the Cycle threshold (Ct) value, also known as quantification cycle (Cq) [98] [5]. The Ct is defined as the number of PCR cycles required for the fluorescent signal to cross a predetermined threshold level, signifying the point where amplification is first detected above the background baseline. This value is inversely proportional to the starting quantity of the target nucleic acid in the sample; a low Ct value indicates a high initial concentration of the target RNA, while a high Ct suggests a low abundance [5].
Ensuring Assay Quality: Efficiency and Validation
A clinically robust threshold cannot be established without a validated and efficient assay. PCR Efficiency measures how perfectly the amplification process doubles the target DNA each cycle. It is calculated using a standard curve generated from serial dilutions of a known template [98]. The slope of the line plotting the log of the dilution factor against the Ct value is used in the formula: Efficiency (%) = [10^(-1/slope) - 1] x 100. An efficiency between 90% and 105% is generally considered acceptable, with 100% representing perfect doubling [98]. Assays with low efficiency produce inaccurate Ct values, compromising downstream threshold analysis.
Validation is essential and includes:
- Specificity Checks: Using melt curve analysis to ensure a single, specific amplification product [99].
- Controls: Including a "no reverse transcription" control (-RT) to check for genomic DNA contamination and a no-template control (NTC) to detect reagent contamination [4].
Quantification Methods: Absolute vs. Relative
The choice of quantification method depends on the clinical question.
- Absolute Quantification: Determines the exact copy number of the target RNA by comparing Ct values to a standard curve with known concentrations. This is often used in viral load testing [98] [5].
- Relative Quantification (RQ): More common in gene expression studies, RQ compares the expression level of a target gene between test and control groups relative to one or more stably expressed reference genes (e.g., GAPDH, ACTB) [98] [5]. This is calculated using the ΔΔCt method, which normalizes data to correct for variations in RNA input and reverse transcription efficiency [98].
Table 1: Key qPCR Analysis Metrics and Their Interpretation
| Metric | Definition | Ideal Range/Value | Clinical Impact of Deviation |
|---|---|---|---|
| Cycle Threshold (Ct) | Cycle where amplification crosses fluorescence threshold | Sample-dependent; very high Ct (>35) may indicate low abundance | High Ct in a positive sample can lead to false negatives if threshold is set too low |
| PCR Efficiency | The rate of target amplification per cycle | 90% - 105% | Low efficiency inflates Ct values, reducing quantitative accuracy and threshold reliability |
| Correlation Coefficient (R²) | Fit of the standard curve in absolute quantification | >0.98 | Low R² indicates poor reproducibility, making standard curve and copy number unreliable |
| ΔCt (in RQ) | Difference in Ct between target and reference gene | Stable across control samples | High variability indicates unstable reference gene, invalidating relative expression results |
Methodologies for Establishing Clinical Thresholds
Cohort Selection and Study Design
The foundation of a clinically relevant threshold is a well-characterized patient cohort. The cohort must include sufficient numbers of patients with and without the clinical condition of interest (e.g., with lymph node metastasis (LNM) vs. without LNM) [97]. Cohort design should account for potential confounders such as cancer stage, histology, and patient demographics to ensure the threshold's generalizability.
Analytical Techniques for Threshold Determination
Once high-quality ΔCt, ΔΔCt, or absolute copy number data is obtained for a defined cohort, statistical methods are employed to define the optimal cutoff.
- Receiver Operating Characteristic (ROC) Curve Analysis: This is the most common method. The ROC curve plots the sensitivity (true positive rate) against 1-specificity (false positive rate) for every possible cutoff value of the biomarker [97]. The Youden's Index (J) is a single statistic that identifies the cutoff that maximizes (Sensitivity + Specificity - 1). The Area Under the Curve (AUC) quantifies the overall predictive power of the biomarker, where 1.0 is a perfect test and 0.5 is no better than chance [97].
- Reference Range Establishment: For prognostic monitoring, thresholds can be set based on the distribution of values in a healthy control population or a patient group with a known good outcome. A common approach is to set the threshold at the mean ± 2 standard deviations of the reference group.
Table 2: Clinical Threshold Examples from Gastric Cancer Liquid Biopsy Studies
| Biomarker / Panel | Clinical Context | Established Threshold | Performance Metrics | Citation |
|---|---|---|---|---|
| Circulating Tumor Cells (CTCs) | Discriminating GC patients from healthy controls | ≥2 CTCs / 7.5 mL blood | Sensitivity: 85.3%, Specificity: 90.3%, AUC: 0.928 | [96] |
| CTC Count | Prognosis in progressive GC | ≥5 CTCs / 7.5 mL blood | Associated with significantly lower Overall Survival | [96] |
| 4-mRNA Panel (SDS, TESMIN, NEB, GRB14) | Predicting LNM in T1 Gastric Cancer (Liquid Biopsy) | Risk Stratification Assessment (RSA) Model | Validation AUC: 0.852, Reduced overtreatment from 84.4% to 56.0% | [97] |
| 4-mRNA Panel | Predicting LNM in T1 Gastric Cancer (Tissue Biopsy) | Same RSA Model | Validation AUC: 0.878, Reduced overtreatment from 83.9% to 44.1% | [97] |
Establishing a Clinical Threshold: This workflow outlines the key steps from initial data acquisition to a validated clinical cutoff.
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of a threshold-setting RT-qPCR study requires carefully selected reagents and controls.
Table 3: Research Reagent Solutions for RT-qPCR in Liquid Biopsy
| Reagent / Material | Function / Role | Key Considerations and Examples |
|---|---|---|
| RNA Isolation Kit | Purifies total RNA from liquid biopsy samples (e.g., plasma). | Choose kits designed for low-abundance targets in biofluids (e.g., PAXgene Blood RNA Kit [97]). Assess yield and purity (A260/280). |
| Reverse Transcriptase | Synthesizes complementary DNA (cDNA) from RNA templates. | Select enzymes with high thermal stability for GC-rich transcripts. Consider RNase H activity for better qPCR efficiency [4] [5]. |
| qPCR Master Mix | Provides core components for amplification (polymerase, dNTPs, buffer). | Contains DNA polymerase, dNTPs, and MgCl2. Select based on dye chemistry (SYBR Green vs. TaqMan probes) [5]. |
| Sequence-Specific Primers | Amplifies the target cDNA sequence. | Must be designed to span exon-exon junctions to avoid genomic DNA amplification. Optimal length: 18-25 bp; GC content: 40-60% [4] [5]. |
| Reference Gene Assays | Used for normalization in relative quantification. | Gene must be stably expressed across all sample types (e.g., GAPDH). Requires validation in the specific liquid biopsy matrix [98] [99]. |
| Positive Control RNA | Assesses reverse transcription and qPCR efficiency. | A synthetic or pooled RNA sample with known expression of the target and reference genes. |
| No-RT Control | Detects contamination from genomic DNA. | Sample is processed without reverse transcriptase. Amplification indicates gDNA contamination [4]. |
Experimental Protocol: A Step-by-Step Guide
This protocol outlines the key steps for validating a biomarker panel and establishing a clinical threshold, as exemplified by the 4-mRNA panel for lymph node metastasis in T1 gastric cancer [97].
Sample Collection and RNA Extraction
- Collection: Collect peripheral blood from a defined cohort of T1 GC patients (e.g., training cohort, n=147). Process samples to isolate plasma within a set time frame to prevent RNA degradation [97].
- RNA Extraction: Isolate total RNA from plasma using a specialized kit (e.g., PAXgene Blood RNA Kit). Document RNA concentration and purity (A260/280 ratio). Assess RNA integrity if possible [97] [99].
Reverse Transcription and qPCR
- cDNA Synthesis: Convert equal amounts of total RNA (e.g., 500 ng) to cDNA using a reverse transcription kit. A mixture of random hexamers and oligo(dT) primers is often used to ensure comprehensive cDNA coverage [4] [5]. Include a no-RT control.
- qPCR Setup: Perform qPCR reactions in triplicate for each sample. The reaction mix should contain:
- Thermal Cycling: Run the plate with a standard protocol: initial denaturation (95°C for 10 min), followed by 40 cycles of denaturation (95°C for 15 sec), and annealing/extension (60°C for 1 min) with fluorescence acquisition [5].
Data Analysis and Threshold Derivation
- Data Preprocessing: Calculate the average Ct for each triplicate. Use the 2^(-ΔΔCt) method to calculate the relative expression of each target gene, normalized to the reference gene [98].
- Model Building (Training Phase): In the training cohort, use statistical methods (e.g., logistic regression) to combine the expression values of the 4-mRNA panel, along with key clinical features, into a single Risk Stratification Assessment (RSA) score [97].
- ROC Analysis: Perform ROC curve analysis using the RSA score to predict LNM status (determined by histopathology). Calculate the AUC and use the Youden's Index to determine the optimal RSA score cutoff that best discriminates between patients with and without LNM [97].
- Validation: Apply the exact same RSA model and cutoff to an independent, blinded validation cohort (e.g., n=168 from multiple institutions) to confirm its predictive accuracy and clinical utility [97].
RT-qPCR Threshold Validation Workflow: This diagram visualizes the end-to-end experimental process for developing and validating a clinically relevant threshold.
Validation and Comparative Analysis: Establishing Clinical Utility
Liquid biopsy, particularly through the analysis of bone marrow (BM) and peripheral blood (PB), presents a less burdensome method for sensitive disease monitoring in oncology. In neuroblastoma, the most common extracranial solid tumor in children, the detection of minimal residual disease (MRD) is critical as bone marrow is a primary site of metastasis and relapse [89]. Despite intensive multimodal treatment, approximately 50% of children with newly diagnosed high-risk neuroblastoma are cured of their disease, underscoring the urgent need for more sensitive disease monitoring techniques to guide therapy [100]. Reverse transcription quantitative polymerase chain reaction (RT-qPCR) has emerged as a powerful tool for MRD detection, offering superior sensitivity compared to traditional morphological examinations or immunocytology [89] [101]. This technical guide examines the neuroblastoma model as a paradigm for the clinical validation of RT-qPCR-based liquid biopsy approaches in prospective studies, framing the discussion within broader cancer detection research.
Prospectively Validated mRNA Marker Panels
The clinical validation of RT-qPCR for neuroblastoma has progressed through several prospective studies that established the prognostic significance of specific mRNA marker panels. The core principle involves detecting neuroblastoma-associated mRNAs that are highly expressed in tumor cells but show minimal or no expression in normal bone marrow and peripheral blood.
Table 1: Prospectively Validated mRNA Marker Panels for Neuroblastoma MRD Detection
| Study/Marker Panel | Key mRNA Targets | Sample Types | Clinical Validation | Prognostic Significance |
|---|---|---|---|---|
| International GPOH-DCOG Validation Study [89] | PHOX2B, TH, DDC, CHRNA3, GAP43 | Bone marrow, Peripheral blood | Prospective multicenter study (n=345 high-risk patients) | BM infiltration >10% at diagnosis: adjusted HR 1.82 for EFS, 2.04 for OS; Any post-induction positivity: HR 2.10 for EFS, 1.76 for OS |
| NB5 Assay [101] | CHGA, DCX, DDC, PHOX2B, TH | Bone marrow, Peripheral blood, Cerebrospinal fluid | Multicenter analysis (71 patients, 113 detections) | PFS significantly lower in NB5-positive MRD-negative patients (27.4 vs 36.0 months, P=0.034); Independent prognostic factor (HR=3.046, P=0.046) |
| 7-Marker Panel [102] | CRMP1, DBH, DDC, GAP43, ISL1, PHOX2B, TH | Bone marrow, Peripheral blood | Retrospective analysis (20 high-risk patients) | Level of 7NB-mRNAs varied with disease status; Significantly higher in relapsed/regrown samples |
The international GPOH-DCOG prospective study validated a five-marker panel (PHOX2B, TH, DDC, CHRNA3, and GAP43) in 345 high-risk neuroblastoma patients treated in trials NB2004 (GPOH) or NBL2009 (DCOG) [89]. This study demonstrated that BM infiltration >10% by RT-qPCR at diagnosis was independently prognostic for survival, with adjusted hazard ratios of 1.82 for event-free survival (EFS) and 2.04 for overall survival (OS). Critically, any post-induction RT-qPCR positivity correlated with poor EFS and OS, with 5-year EFS of 26.6% for RT-qPCR-positive patients versus 60.4% for negative patients [89].
The NB5 assay (CHGA, DCX, DDC, PHOX2B, and TH) was evaluated across six research centers with 71 patients, demonstrating 100% sensitivity and specificity in assessing tumor relapse or residual disease [101]. This assay showed significantly higher sensitivity compared to flow cytometric MRD detection, with BM specimens exhibiting an additional 45.5% positive results compared to PB specimens. Notably, NB5 positivity provided prognostic value even in patients classified as MRD-negative by other methods [101].
Table 2: Comparison of Detection Method Performance Characteristics
| Method | Sensitivity | Specificity | Sample Volume Efficiency | Implementation Complexity |
|---|---|---|---|---|
| RT-qPCR | High (detects 1-10 tumor cells per 10^5 normal cells) | High with multi-marker panels | Moderate (requires separate reactions for multiple markers) | Moderate (requires optimization of primer/probe sets) |
| Multiplex RT-qPCR [53] | Comparable to singleplex | Comparable to singleplex | High (multiple markers in single reaction) | High (requires extensive optimization to prevent interference) |
| Droplet Digital PCR [101] [102] | Very High (absolute quantification without standard curves) | Very High (reduced false positives) | Moderate | High (specialized equipment required) |
| Flow Cytometric MRD [101] | Lower than RT-qPCR (17.0% positive in same samples) | High with appropriate antibody panels | High (multiple parameters simultaneously) | Low to Moderate |
Signaling Pathways and Biological Context
The mRNA markers used in neuroblastoma liquid biopsy assays are not arbitrary but reflect the fundamental biology of neuroblastoma cells and their origins in the sympathetic nervous system. The signaling pathways and biological processes represented by these markers provide insights into neuroblastoma pathogenesis and tumor heterogeneity.
Diagram 1: Neuroblastoma MRD Marker Biology (82 characters)
The diagram above illustrates the biological context of neuroblastoma MRD markers. Key transcriptional regulator PHOX2B controls sympathetic neuron differentiation from neural crest precursors [89] [53]. The adrenergic (ADRN) phenotype markers include catecholamine synthesis enzymes (TH, DDC, DBH) and neuronal function proteins (GAP43, CHGA, DCX) [53] [101]. Neuroblastoma tumors exhibit heterogeneity between ADRN and mesenchymal (MES) phenotypes, with MES cells lacking expression of traditional markers like PHOX2B but expressing POSTN and PRRX1 instead [53]. This biological understanding informs comprehensive marker panel design to overcome tumor heterogeneity in MRD detection.
Experimental Protocols and Workflows
Prospective Study Design for Clinical Validation
The international GPOH-DCOG validation study exemplifies a robust prospective design for validating liquid biopsy assays [89]. The study enrolled 345 high-risk neuroblastoma patients across multiple centers, with BM aspirates collected from 2-4 sites at diagnosis and dedicated time points during induction chemotherapy: after the first two therapy courses and at the intended end of induction. This longitudinal sampling strategy enabled assessment of BM clearance dynamics and correlation with clinical outcomes. The primary endpoints were event-free survival (EFS) and overall survival (OS), with statistical analysis using Cox regression models and Kaplan-Meier methodology with log-rank tests [89].
Sample Processing and RNA Extraction
Sample processing follows standardized protocols to ensure reproducible results. BM samples are transferred to PAXgene blood RNA tubes within 24 hours and stored at -20°C [89]. RNA extraction uses the PAXgene Blood RNA Kit (QIAGEN), with cDNA synthesis from 2-3 µg of RNA using random hexamers, dNTPs, and MMLV reverse transcriptase incubated at 42°C for 45 minutes [89]. For multiplex RT-qPCR approaches, the reverse transcription method may be optimized using the High-Capacity RNA-to-cDNA Kit (Applied Biosystems) to improve efficiency and compatibility with multiplex reactions [53].
RT-qPCR and Multiplex Assay Methodology
The standard RT-qPCR protocol utilizes TaqMan chemistry with reactions performed in 20 µL volumes containing 10 µL TaqMan Fast Universal PCR Master Mix, 300 nM forward and reverse primers, 200 nM probe, and 5 µL cDNA [89]. Thermal cycling conditions include initial heating at 95°C for 20 seconds, followed by 40 cycles of denaturation at 95°C and annealing/extension at 60°C. For the five-marker panel, reactions are typically performed as singleplex assays [89].
Multiplex RT-qPCR requires additional optimization to detect multiple targets in a single reaction. Primers and probes are redesigned with compatible fluorophores (FAM, Yakima Yellow, Dragonfly Orange) matched to available detection channels, with corresponding Black Hole Quenchers [53]. Master mix composition must be optimized to prevent fluorescence quenching, which may involve replacing standard mixes with alternatives that use Mustang Purple as a reference control instead of ROX [53]. The development process includes validation of primer compatibility, efficiency testing in both singleplex and multiplex formats, and establishment of new thresholds for positivity specific to the multiplex format.
Diagram 2: MRD Detection Workflow (65 characters)
Threshold Determination and Data Analysis
Thresholds for positivity are established based on expression levels in control BM and PB samples from individuals without neuroblastoma. For the multiplex RT-qPCR approach, a sample is considered positive when Ctsample < 40 cycles and mean ΔCtsample is at least 3.0 Ct lower than the median ΔCt of control tissue [53]. This threshold provides optimal specificity while maintaining high sensitivity for MRD detection. For the NB5 assay, positivity is determined based on expression levels significantly above those observed in control samples, with careful normalization to reference genes such as GUSB [101].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Neuroblastoma Liquid Biopsy Studies
| Reagent/Category | Specific Examples | Function & Application | Technical Notes |
|---|---|---|---|
| Sample Collection & Stabilization | PAXgene Blood RNA Tubes (QIAGEN) | Stabilizes RNA in BM/PB samples during transport | Enables processing within 24 hours; storage at -20°C |
| RNA Extraction | PAXgene Blood RNA Kit (QIAGEN) | Isales high-quality RNA from small volume samples | Includes DNase treatment to remove genomic DNA contamination |
| Reverse Transcription | High-Capacity RNA-to-cDNA Kit (Applied Biosystems) | Converts RNA to cDNA with high efficiency | Preferred for multiplex RT-qPCR; reduces DTT-related quenching |
| qPCR Master Mix | TaqMan Fast Universal PCR Master Mix (Applied Biosystems) | Provides enzymes, dNTPs, buffers for qPCR | Compatible with fast cycling protocols; contains UDG for carryover prevention |
| Primers & Probes | Custom TaqMan assays for PHOX2B, TH, DDC, etc. | Target-specific detection of neuroblastoma mRNAs | Fluorophores: FAM, YY, DFO with corresponding BHQ quenchers |
| Reference Genes | GUSB, B2M | Normalizes for RNA input and cDNA synthesis efficiency | Stable expression across BM and PB samples essential |
| Positive Controls | Neuroblastoma cell lines (IMR32, SH-SY5Y, 691-MES/ADRN) | Assay validation and sensitivity determination | Covers adrenergic and mesenchymal phenotypes |
| Digital PCR Systems | Droplet Digital PCR (Bio-Rad) | Absolute quantification without standard curves | Higher sensitivity for low-abundance targets; 72.2% positive in BM vs 40.0% in PB [101] |
Clinical Implications and Future Directions
The prospective validation of RT-qPCR for neuroblastoma MRD detection has significant clinical implications. The international GPOH-DCOG study concluded that implementation of RT-qPCR for minimal residual disease testing in neuroblastoma should be used to guide therapy [89]. This recommendation is based on their finding that post-induction RT-qPCR positivity correlated with markedly poor outcomes (5-year EFS 26.6% vs 60.4% for negative patients), whereas post-induction immunocytology positivity showed no significant association with survival [89].
Future developments in the field include addressing tumor heterogeneity more comprehensively through expanded marker panels that encompass both adrenergic and mesenchymal phenotypes [53]. The transition to more practical and efficient testing formats, such as multiplex RT-qPCR, will facilitate clinical implementation by reducing required sample volumes, processing time, and costs [53]. Additionally, emerging technologies like droplet digital PCR offer potentially simpler and more reproducible detection of low-level mRNAs, with studies showing higher prognostic value compared to qPCR in post-treatment BM samples [102].
Beyond MRD detection, liquid biopsy approaches are expanding to encompass other biomarkers and applications in neuroblastoma. Recent research has identified ultra-high-risk subsets of patients based on TERT promoter mutations (TERT-PM) and TERT rearrangements (TERT-RA), with median progression-free survival of only nine months despite risk-appropriate therapy [103]. Routine testing for these mutations may refine risk stratification and identify patients who may benefit from treatment escalation or novel TERT-targeted therapies [103].
The neuroblastoma model demonstrates a successful pathway for clinical validation of liquid biopsy technologies, from initial marker identification through prospective multicenter validation. This framework provides a template for developing similar approaches in other solid tumors, with potential to significantly impact patient stratification, therapy guidance, and outcome prediction in oncology.
Within the broader thesis on the advancing role of liquid biopsy in oncology, the detection of bone marrow (BM) infiltration represents a critical application for prognosis and therapy guidance. This whitepaper details how sensitive molecular monitoring of BM, particularly via RT-qPCR, provides a powerful correlation with patient survival outcomes. The move towards liquid biopsies addresses a significant clinical need across various cancers, including neuroblastoma and malignant lymphoma, where BM is a common site for metastatic disease and is associated with poor prognosis [104] [105]. Traditional methods for assessing BM status, such as histology, immunocytology, and imaging, often lack the sensitivity to detect minimal residual disease (MRD), leading to an underestimation of disease burden and inaccurate prognostication in a substantial number of patients [104] [106]. This document serves as a technical guide for researchers and drug development professionals, summarizing the compelling clinical evidence, detailing standardized experimental protocols, and providing resources to implement these assays in translational research settings.
BM Infiltration as a Prognostic Indicator
The presence of tumor cells in the bone marrow is a recognized indicator of disseminated disease and is consistently correlated with inferior survival rates across multiple cancer types. In neuroblastoma, BM is the most common site of metastatic disease at diagnosis and a frequent site of relapse [104]. Studies have shown that despite initial response to treatment, the majority of high-risk neuroblastoma patients relapse, culminating in only 40% long-term survivors, underscoring the limitations of conventional response assessment and the urgent need for more sensitive disease monitoring [104]. Similarly, in malignant lymphoma (ML), bone marrow infiltration (BMI) is a key factor in disease staging and is a clear marker of disseminated disease, with studies reporting a poor prognosis for patients with BMI [106]. The quantitative assessment of tumor burden in BM, therefore, offers a critical window into a patient's disease status and likelihood of treatment success.
Table 1: Key mRNA Biomarkers for BM Infiltration Detection in Different Cancers
| Cancer Type | Key mRNA Biomarkers | Detection Method | Clinical Utility |
|---|---|---|---|
| Neuroblastoma | PHOX2B, TH, DDC, CHRNA3, GAP43 [104] | RT-qPCR | Diagnosis, MRD monitoring, prognosis [104] [105] |
| Anaplastic Large Cell Lymphoma (ALCL) | NPM/ALK fusion gene, CD30 [107] | Quantitative RT-PCR | MRD monitoring, correlation with disease status [107] |
| Rhabdomyosarcoma | MYOD1, MYOG, PDLIM3, ACTC1 [105] | RT-qPCR | Determination of metastatic status, prognostication [105] |
Quantitative Data: BM Infiltration Levels and Survival Outcomes
Recent prospective studies have validated the strong association between BM infiltration levels detected by RT-qPCR and patient event-free survival (EFS) and overall survival (OS). The data consistently demonstrates that both the magnitude of infiltration at diagnosis and the persistence of disease after induction therapy are prognostically significant.
A landmark prospective study of 345 high-risk neuroblastoma patients treated in international trials (NB2004 and NBL2009) revealed striking results. BM infiltration greater than 10% as quantified by RT-qPCR at diagnosis was a significant prognostic factor for survival, with adjusted hazard ratios (HR) of 1.82 for EFS and 2.04 for OS [104]. Even more notably, the failure to clear BM metastases after induction therapy was a powerful predictor of very poor outcomes. Any post-induction RT-qPCR positivity was associated with a 5-year EFS of only 26.6% compared to 60.4% for RT-qPCR-negative patients, and a 5-year OS of 43.8% versus 65.7% [104]. The hazard ratio for an event in post-induction positive patients was 2.10 [104]. In contrast, post-induction immunocytology positivity was not significantly associated with EFS or OS, highlighting the superior prognostic value of the more sensitive molecular technique [104].
Table 2: Survival Outcomes Based on BM Infiltration Status in Neuroblastoma
| Parameter | Patient Group | 5-Year EFS (SE%) | 5-Year OS (SE%) | Hazard Ratio (HR) [95% CI] |
|---|---|---|---|---|
| Infiltration at Diagnosis | RT-qPCR >10% | - | - | EFS: 1.82 [1.25-2.63]; OS: 2.04 [1.33-3.14] [104] |
| Status Post-Induction Therapy | RT-qPCR Positive | 26.6% (5.2) | 43.8% (5.9) | EFS: 2.10 [1.27-3.49]; OS: 1.76 [1.01-3.08] [104] |
| Status Post-Induction Therapy | RT-qPCR Negative | 60.4% (6.7) | 65.7% (6.6) | Reference group [104] |
Similar approaches in lymphoma demonstrate the utility of quantitative PCR. In Anaplastic Large Cell Lymphoma (ALCL), monitoring the NPM/ALK fusion gene and CD30 expression via quantitative real-time RT-PCR allowed for residual disease detection and showed correlation with the clinical disease status [107]. Furthermore, machine learning models are being developed to predict BMI in ML using routine laboratory indicators, achieving area under the curve (AUC) values of 0.844, offering a potential complementary approach to direct molecular detection [106].
Experimental Protocols for BM Infiltration Detection
Sample Collection and Processing
For optimal RNA preservation, bone marrow aspirates from two to four sites should be collected in EDTA tubes and transferred to PAXgene blood RNA tubes within 24 hours of collection [104]. Samples should be stored at -20°C until RNA extraction. For cell-free DNA (cfDNA) analysis from blood plasma, centrifugation steps are required to separate plasma from cellular components before cfDNA extraction [105].
RNA Extraction and cDNA Synthesis
RNA is isolated using standardized kits such as the PAXgene Blood RNA Kit. For cDNA synthesis, 2-3 µg of RNA is typically reverse-transcribed using random hexamers, dNTPs, and MMLV transcriptase. The reaction is incubated at 42°C for 45 minutes before enzyme inactivation, and the final volume is diluted to 100 µl [104].
Reverse Transcription Quantitative PCR (RT-qPCR)
RT-qPCR is performed using TaqMan chemistry on a real-time PCR system. Reactions are carried out in a 20 µL volume containing TaqMan Fast Universal PCR Master Mix, forward and reverse primers, and probes [104]. Expression of target mRNA markers (e.g., PHOX2B, TH) is normalized to a reference gene, typically beta-glucoronidase (GUSB) [104]. Positivity is scored according to validated thresholds, and the level of infiltration can be calculated by relating expression levels in the patient sample to expression in a relevant tumor cell line (e.g., IMR32 for neuroblastoma) [105].
Droplet Digital PCR (ddPCR) for Genetic Alterations
For absolute quantification of specific genetic alterations, such as MYCN amplification in neuroblastoma, ddPCR can be employed. This involves a duplex PCR reaction with a primer-probe set for the target (MYCN) and a reference gene (NAGK). The MYCN copy number is determined by calculating the ratio of MYCN to the reference gene [105]. For methylation analysis, methods like cfRRBS (cell-free reduced representation bisulfite sequencing) can be applied to cfDNA to establish a diagnosis based on tumor-specific methylation patterns [105].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for BM Infiltration Studies
| Item | Function/Application | Example Products/Catalog Numbers |
|---|---|---|
| PAXgene Blood RNA Tubes | Stabilizes intracellular RNA in whole blood and bone marrow aspirates for transport and storage [104]. | QIAGEN PAXgene Blood RNA Tubes |
| RNA Isolation Kit | Purifies high-quality total RNA from PAXgene samples. | PAXgene Blood RNA Kit (QIAGEN) [104] |
| Reverse Transcriptase | Synthesizes cDNA from purified RNA templates. | MMLV Transcriptase (Invitrogen) [104] |
| TaqMan Master Mix | Provides all components (except primers/probes) for probe-based qPCR reactions. | TaqMan Fast Universal PCR Master Mix (Applied Biosystems) [104] |
| Primers & Probes | Sequence-specific oligonucleotides for amplification and detection of target mRNA markers (e.g., PHOX2B, TH) and reference genes (e.g., GUSB) [104]. | Custom synthesized (e.g., Eurogentec) |
| Methylation-Sensitive Restriction Enzymes (MSRE) | Digests unmethylated DNA in ddPCR assays to specifically detect methylated alleles like RASSF1A-M [105]. | Commercially available MSREs |
Signaling Pathways and Molecular Logic
The molecular detection of BM infiltration relies on identifying genes that are highly and specifically expressed in the tumor cells of origin. In neuroblastoma, which arises from neural crest cells, the targeted mRNA markers are part of core neurodevelopmental pathways. PHOX2B is a transcription factor critical for autonomic nervous system development, while TH and DDC are enzymes in the catecholamine synthesis pathway [104]. Their aberrant expression in BM indicates the presence of neuroblastoma cells. In lymphomas, detection may focus on fusion oncogenes like NPM/ALK, which drives oncogenic signaling through constitutive ALK kinase activity, or on surface receptors like CD30 [107]. The logical relationship is that the persistent presence of these tumor-specific molecular signals after therapy indicates MRD, which is the precursor to clinical relapse.
The correlation between BM infiltration and patient survival is unequivocal, and the adoption of sensitive RT-qPCR-based liquid biopsy methods provides a robust and clinically actionable means of quantifying this risk. The data demonstrates that molecular BM status, particularly after induction therapy, is a superior prognostic factor compared to conventional methods. The standardized protocols and tools outlined in this guide provide a framework for researchers to incorporate these assays into clinical trials and drug development programs. As the field advances, the integration of multi-analyte liquid biopsy approaches—combining mRNA markers, cfDNA genotyping, and methylation analysis—will further refine risk stratification. This will ultimately pave the way for MRD-directed therapy, enabling treatment intensification for high-risk patients and de-escalation for those with confirmed disease eradication, thereby improving survival outcomes and quality of life.
Within the evolving landscape of cancer diagnostics, the detection of minimal residual disease (MRD) and disseminated tumor cells is paramount for accurate prognosis and treatment adjustment. Liquid biopsies, particularly those utilizing bone marrow aspirates, have emerged as a less invasive method for this monitoring. This technical guide provides an in-depth comparison of two principal laboratory techniques—Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) and Immunocytology (ICC)—framed within broader research on liquid biopsy for cancer detection. Focusing on sensitivity, this review synthesizes current data to inform researchers, scientists, and drug development professionals about the optimal application of these methodologies.
Core Principles and Workflows
Immunocytology (ICC) is a cytological technique that involves the use of antibodies to visually detect specific protein antigens (e.g., GD2, NCAM) on the surface of disseminated tumor cells (DTCs) in bone marrow samples. The process entails preparing cytospins from mononuclear cells, staining with fluorescent or chromogenic antibodies, and manually enumerating positive cells via microscopy [108] [109] [110]. Its effectiveness is dependent on antibody specificity and investigator experience.
RT-qPCR is a molecular technique that detects and quantifies specific mRNA transcripts (e.g., PHOX2B, TH, CK-19) expressed by tumor cells. The workflow involves RNA extraction from samples, reverse transcription to cDNA, and quantitative PCR amplification. The cycle threshold (Ct) value determines transcript quantity, offering a highly sensitive, quantitative measure of tumor cell presence that is less observer-dependent [108] [109] [89].
Table 1: Core Technical Characteristics of ICC and RT-qPCR
| Feature | Immunocytology (ICC) | RT-qPCR |
|---|---|---|
| Analytical Target | Protein antigens (e.g., GD2, NCAM) [108] [110] | mRNA transcripts (e.g., PHOX2B, TH, CK-19) [108] [109] [89] |
| Detection Method | Microscopy-based cell counting [109] | Fluorescence-based cycle threshold (Ct) measurement [109] |
| Result Output | Number of stained cells per million mononuclear cells [109] | Relative gene expression or transcript quantity [109] |
| Key Advantage | Direct visualization and morphological confirmation of cells [109] | High sensitivity, automation potential, and quantitative output [108] [109] |
| Key Limitation | Observer-dependent, time-consuming, lower sensitivity [109] [89] | Does not provide cell morphology, potential for false positives from illegitimate transcription [109] |
Direct Comparison of Analytical and Clinical Sensitivity
Extensive studies across cancer types, including neuroblastoma and breast cancer, consistently demonstrate the superior sensitivity of RT-qPCR over ICC. In neuroblastoma, RT-qPCR reliably detects tumor cells with a sensitivity of up to one tumor cell in one million normal bone marrow cells, a threshold that challenges ICC [110]. A direct comparative study showed ICC and RT-qPCR had high concordance (85%), but RT-qPCR detected a higher number of positive bone marrow samples in patients with metastatic breast cancer [109].
This analytical advantage translates into significant clinical value, particularly in monitoring Minimal Residual Disease (MRD). In a prospective international validation study on high-risk neuroblastoma, any post-induction therapy positivity detected by RT-qPCR was a strong prognostic indicator of poor event-free and overall survival, whereas post-induction immunocytology positivity showed no significant association with patient outcome [89]. This underscores RT-qPCR's critical role in predicting relapse and guiding therapeutic decisions.
Table 2: Clinical Performance and Prognostic Value in Cancer Monitoring
| Cancer Type / Context | ICC Findings | RT-qPCR Findings | Clinical Correlation & Prognostic Power |
|---|---|---|---|
| Metastatic Breast Cancer [109] | 62% (15/24) of patient samples were positive. | 80% (20/25) were positive for CK-19; 40% (10/25) for hMAM. | A strong correlation was observed between CK-19 RT-qPCR and ICC (r=0.9, p<0.0001). |
| Neuroblastoma (MRD Post-Induction) [89] | Positivity not significantly associated with survival (HR 1.22 for EFS). | Any positivity correlated with poor EFS (HR 2.10) and OS (HR 1.76). | RT-qPCR is a superior prognostic tool for predicting relapse and survival after initial therapy. |
| Neuroblastoma (General Detection) [108] | Sensitivity was 1-2 logs lower than RT-qPCR. All controls tested negative. | High sensitivity; 1-2 logs more sensitive than flow cytometry. 6% of controls were false positive. | Correlation between tumor cell levels by RT-qPCR and ICC was high (r=0.78, p<0.001). |
Experimental Protocols for Sensitivity Comparison
To ensure valid and reproducible comparisons between RT-qPCR and ICC, a standardized experimental approach using paired patient samples is essential. The following protocol outlines a robust methodology for a head-to-head sensitivity assessment.
Sample Collection and Processing
- Patient Cohort and Sample Type: The study should include bone marrow aspirates from patients with cancers known to disseminate to the bone marrow (e.g., neuroblastoma, breast cancer) and control patients with non-malignant conditions [109] [89]. Bilateral aspirates from the iliac crest are recommended to account for potential heterogeneous infiltration [110].
- Informed Consent: Obtain written informed consent from all patients or guardians, with approval from the institutional Medical Research Ethics Committee, following the Declaration of Helsinki [110] [89].
- Mononuclear Cell (MNC) Isolation: Within 24 hours of collection, process the bone marrow aspirates. Isolate MNCs using density-gradient centrifugation with Ficoll-Paque. Wash the cells twice with phosphate-buffered saline (PBS) [109].
- Sample Division: Divide the MNC pellet into two aliquots after isolation. One aliquot is resuspended in PBS for immediate use in ICC. The other aliquot should be preserved in a nucleic acid-stabilizing buffer, such as TRIzol or PAXgene blood RNA tubes, and stored at -80°C (for TRIzol) or -20°C (for PAXgene) until RNA extraction for RT-qPCR [109] [89].
Immunocytology (ICC) Protocol
- Cell Preparation: Cytocentrifuge the MNC suspension onto glass slides at a density of approximately 5 x 10^5 cells per spot [109].
- Staining: Perform immunostaining using validated primary antibodies. For neuroblastoma, anti-GD2 (e.g., 14.G2a) and anti-NCAM (e.g., 5.1H11) are commonly used [108]. For breast cancer, pan-cytokeratin antibodies (e.g., A45-B/B3) are standard [109]. Use appropriate fluorescent or chromogenic detection kits according to manufacturer instructions.
- Microscopy and Enumeration: Screen at least 2 million cells per patient sample microscopically. Cells should be identified as tumor cells based on standard criteria (e.g., those defined by the ISHAGE working group) [109]. To minimize bias, have two independent, experienced observers evaluate the slides. Express results as the number of positive cells per million MNCs.
RT-qPCR Protocol
- RNA Extraction and QC: Extract total RNA from the stabilized MNC pellet using a commercial kit (e.g., RNeasy Kit, PAXgene Blood RNA Kit) [109] [89]. Quantify RNA concentration and assess purity spectrophotometrically, accepting 260/280 nm ratios between 1.8 and 2.0. RNA integrity can be further verified using an instrument like the Agilent Bioanalyzer [109].
- cDNA Synthesis: Synthesize cDNA from 2-3 µg of total RNA using random hexamers, dNTPs, and MMLV reverse transcriptase in a recommended reaction volume. After synthesis, inactivate the enzyme and dilute the cDNA to a standardized volume [89].
- Quantitative PCR: Perform multiplex RT-qPCR on a platform such as the ABI Prism 7700 or Step-One-Plus. Each reaction should include TaqMan Universal PCR Master Mix, sequence-specific primers and probes, and the cDNA template. Key cancer-specific mRNA markers include:
- Neuroblastoma: PHOX2B, TH, DDC, CHRNA3, GAP43 [89].
- Breast Cancer: CK-19, hMAM [109]. Normalize target gene expression against a reference gene, such as β-actin, GAPDH, or GUSB [109] [89]. Calculate relative gene expression using the comparative Ct method (2^-ΔΔCt) relative to a calibrator sample [109].
Data and Sensitivity Analysis
- Sensitivity Determination: Test the limit of detection (LoD) for each method by spiking known numbers of cultured tumor cells (e.g., MCF-7 for breast cancer) into healthy donor MNCs. The LoD is the lowest concentration at which the tumor cells are consistently detected [109].
- Statistical Correlation: Compare the quantitative results from ICC and RT-qPCR for patient samples using statistical tests like Spearman's rank correlation to calculate the correlation coefficient (r) and determine significance (p-value) [109]. Analyze the concordance rate between the two methods for categorical (positive/negative) results.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these protocols requires specific, validated reagents. The following table details essential solutions for comparing RT-qPCR and ICC in liquid biopsy research.
Table 3: Key Research Reagent Solutions for ICC and RT-qPCR
| Reagent / Kit | Function / Application | Experimental Notes |
|---|---|---|
| Anti-GD2 Antibody (e.g., 14.G2a) [108] | ICC detection of disseminated neuroblastoma cells. | Critical for identifying tumor cells; specificity must be validated. |
| Anti-Pan Cytokeratin Antibody (e.g., A45-B/B3) [109] | ICC detection of disseminated epithelial cells (e.g., in breast cancer). | A standard marker for carcinomas; helps distinguish tumor cells from hematopoietic cells. |
| PAXgene Blood RNA Kit [89] | Stabilization and extraction of total RNA from bone marrow samples. | Preserves RNA integrity for transport and storage, crucial for accurate RT-qPCR. |
| TaqMan Universal PCR Master Mix [89] | Core reagent for the fluorescence-based qPCR amplification step. | Provides high efficiency and reproducibility for quantitative detection. |
| Primer/Probe Sets for mRNA Markers (e.g., PHOX2B, TH, CK-19) [109] [89] | Target-specific amplification and detection of tumor-derived mRNA. | The selection of a multi-marker panel increases the sensitivity and robustness of MRD detection. |
| High-Capacity cDNA Reverse Transcription Kit [109] | Synthesis of complementary DNA (cDNA) from isolated RNA. | The first critical step for moving from RNA to an amplifiable DNA template. |
The comprehensive comparison of RT-qPCR and immunocytology solidifies RT-qPCR's position as the more sensitive technique for detecting disseminated tumor cells and MRD in liquid biopsies. Its quantitative nature, lower observer dependency, and superior analytical sensitivity make it an invaluable tool for predicting patient outcomes, especially after induction therapy where residual disease may be minimal. While ICC provides direct morphological confirmation, its lower sensitivity limits its prognostic power in the MRD setting. The future of liquid biopsy monitoring lies in multi-modal approaches, but the implementation of sensitive, standardized, and quantitative RT-qPCR is a crucial step forward for precision oncology in high-risk cancers.
In the rapidly advancing field of liquid biopsy for cancer detection, researchers have an expanding arsenal of molecular tools at their disposal. Next-generation sequencing (NGS), digital PCR (dPCR), and real-time quantitative PCR (RT-qPCR) each offer distinct advantages for analyzing circulating tumor DNA (ctDNA) and other cancer-derived biomarkers. This technical guide provides a comprehensive benchmarking of these three core technologies, focusing on the critical parameters of cost, throughput, and sensitivity within the context of liquid biopsy research. Understanding these trade-offs is essential for designing robust experimental protocols, allocating resources efficiently, and generating clinically meaningful data from precious liquid biopsy samples.
Fundamental Principles and Applications
Next-Generation Sequencing (NGS): NGS encompasses high-throughput technologies that enable massively parallel sequencing of millions of DNA fragments, providing both qualitative and quantitative data. In liquid biopsy, whole-genome or targeted sequencing approaches allow for comprehensive profiling of ctDNA, including variant discovery, mutational signature analysis, and genome-wide copy number alteration detection without prior knowledge of specific mutations [111]. The method's ability to perform unbiased sequence discovery makes it invaluable for exploratory biomarker identification.
Digital PCR (dPCR): As the third generation of PCR technology, dPCR operates by partitioning a PCR reaction into thousands of nanoscale reactions, enabling absolute quantification of nucleic acids without the need for standard curves. This partitioning allows for precise counting of individual DNA molecules, making it exceptionally suitable for detecting rare mutations (e.g., oncogenic variants in a background of wild-type DNA) and monitoring minimal residual disease with high precision and sensitivity [74] [112]. Its calibration-free nature provides robust quantification resistant to PCR efficiency variations.
Real-Time Quantitative PCR (RT-qPCR): RT-qPCR monitors the amplification of DNA in real-time using fluorescent reporters, providing relative quantification of target sequences based on the cycle threshold (Ct) values. For liquid biopsy applications, it offers a rapid, cost-effective solution for analyzing a limited number of predefined mutations or expression markers, making it suitable for high-volume screening of known cancer-associated alterations where extreme sensitivity is not the primary requirement [111].
Direct Performance Benchmarking
Table 1: Technical and Performance Specifications Comparison
| Parameter | NGS | Digital PCR (dPCR) | Real-Time PCR (qPCR) |
|---|---|---|---|
| Quantitative Capability | Yes (relative) | Yes (absolute) | Yes (relative, requires standard curve) |
| Sequence Discovery | Yes (unbiased) | No | No |
| Theoretical Sensitivity | ~0.1%-1% variant allele frequency (VAF) [111] | ~0.001%-0.01% VAF [74] [112] | ~1-5% VAF [112] |
| Number of Targets per Reaction | 1 to >10,000 [111] | 1 to 5 (multiplexing) [111] | 1 to 5 (multiplexing) [111] |
| Sample-to-Answer Time | Library prep: Hours to daysSequencing: Hours to days [111] | ~1-3 hours (after DNA extraction) [111] | ~1-3 hours (after DNA extraction) [111] |
| Cost per Sample | $$$$ (whole genome)$$ (targeted) [111] | $$ [111] | $ [111] |
| Throughput (Samples per Run) | Moderate to High (depending on platform) | Low to Moderate (typically 1-96 samples) [113] | High (96-384+ well formats) |
| Data Complexity | High (requires bioinformatics) | Low to Moderate | Low |
| Best Applications in Liquid Biopsy | Novel biomarker discovery, comprehensive mutational profiling, methylation analysis | Absolute quantification, rare variant detection, treatment monitoring, validation of NGS findings [74] [112] | Screening of known high-frequency mutations, gene expression analysis, rapid clinical screening |
Table 2: Economic and Operational Considerations for Research Laboratories
| Consideration | NGS | Digital PCR (dPCR) | Real-Time PCR (qPCR) |
|---|---|---|---|
| Instrument Cost (Entry-Level) | High ($50,000-$1,000,000+) | Moderate ($38,000-$150,000) [113] [114] | Low ($20,000-$80,000) |
| Cost per Sample | High for WGS, moderate for targeted | Moderate to High [113] | Low [111] |
| Hands-On Time | Extensive | Moderate | Low |
| Personnel Expertise Required | Advanced bioinformatics & molecular biology | Standard molecular biology with specific training | Standard molecular biology |
| Reagent Costs | High | Moderate to High | Low |
| Return on Investment | For discovery applications | For validation and clinical applications | For high-volume routine testing |
| Automation Potential | Moderate to High | Moderate | High |
Experimental Design and Methodological Considerations
Complementary Workflows in Liquid Biopsy Research
The most effective liquid biopsy research programs strategically integrate all three technologies throughout the research pipeline. The following workflow diagram illustrates how NGS, dPCR, and RT-qPCR complement each other in a comprehensive liquid biopsy study:
Detailed Experimental Protocols
NGS Protocol for ctDNA Mutation Discovery
Sample Preparation and Library Construction
- Extract cell-free DNA from 2-10 mL plasma using specialized cfDNA isolation kits (e.g., QIAamp Circulating Nucleic Acid Kit) to maximize yield from low-volume samples.
- Quantify DNA using fluorometric methods (e.g., Qubit dsDNA HS Assay) and assess quality via capillary electrophoresis (e.g., Bioanalyzer/TapeStation).
- Prepare sequencing libraries using ligation-based methods compatible with low DNA input (1-50 ng), incorporating unique molecular identifiers (UMIs) to correct for amplification biases and PCR errors.
- Enrich for cancer-relevant targets using either:
- Hybrid capture-based panels (100-500 genes) for comprehensive profiling
- Amplicon-based panels (10-50 genes) for higher sensitivity at lower cost
- Amplify libraries with limited-cycle PCR (8-12 cycles) to maintain representation while generating sufficient material for sequencing.
Sequencing and Data Analysis
- Sequence on appropriate platform (Illumina NovaSeq, MiSeq, or NextSeq) to achieve minimum 10,000x raw coverage (yielding ~1000x deduplicated coverage with UMIs).
- Process data through bioinformatic pipeline:
- Alignment (BWA-MEM) to reference genome (hg38)
- Umi processing (fgbio) to group duplicate reads
- Variant calling (VarScan2, MuTect2) with minimum 0.1% VAF threshold
- Annotation (ANNOVAR, VEP) for biological interpretation
dPCR Protocol for Rare Variant Quantification
Assay Design and Optimization
- Design TaqMan assays targeting specific mutations identified through NGS screening, with amplicon sizes <120 bp to accommodate fragmented cfDNA.
- Include both mutant-specific and wild-type control assays in separate reactions for calculation of variant allele frequency.
- Optimize primer and probe concentrations through checkerboard titrations (50-900 nM primers, 100-250 nM probes).
Partitioning and Amplification
- Prepare reaction mix containing 5-20 ng cfDNA, dPCR supermix, and optimized primer-probe concentrations in total volume of 20-40 μL.
- Generate partitions according to platform specifications:
- Droplet-based systems (Bio-Rad QX200/600): 20,000 droplets per sample
- Chip-based systems (Qiagen QIAcuity): 5,000-26,000 partitions per sample
- Amplify with thermal cycling conditions:
- 95°C for 10 minutes (enzyme activation)
- 40 cycles of: 94°C for 30 seconds, 55-60°C (assay-specific) for 60 seconds
- 98°C for 10 minutes (enzyme deactivation)
Data Analysis and Interpretation
- Read partitions using appropriate fluorescence detection system.
- Apply Poisson correction to raw counts to account for multiple targets per partition.
- Calculate absolute concentration (copies/μL) and variant allele frequency using the formula:
- Include negative controls (no-template) and positive controls (synthetic references) in each run.
RT-qPCR Protocol for High-Throughput Screening
Assay Configuration
- Utilize commercially available TaqMan assays or design custom assays for known cancer mutations.
- Implement multiplex reactions (2-5 targets) with different fluorophores (FAM, VIC, CY5, etc.) to maximize information per well.
- Include reference genes (e.g., ALB, RNase P) for normalization and quality control.
Amplification and Quantification
- Prepare reactions in 96- or 384-well plates with 5-10 ng cfDNA per reaction.
- Run amplification with standard conditions:
- 50°C for 2 minutes (UNG incubation, if used)
- 95°C for 20 seconds
- 40 cycles of: 95°C for 1 second, 60°C for 20 seconds
- Analyze using relative quantification (ΔΔCt) method with standard curve or comparative Ct approach.
Technical Performance and Validation Data
Sensitivity and Accuracy Benchmarking Studies
Recent comparative studies demonstrate the distinct performance characteristics of each technology in liquid biopsy applications:
dPCR vs. RT-qPCR for Copy Number Variation: A 2025 study comparing dPCR, RT-qPCR, and pulsed-field gel electrophoresis (PFGE) for measuring DNA copy number variations found that dPCR showed 95% concordance with PFGE (considered the gold standard), while qPCR results were only 60% concordant. The dPCR method demonstrated superior accuracy, particularly at higher copy numbers where qPCR efficiency declines [112].
dPCR vs. RT-qPCR for Viral Detection: In respiratory virus detection, dPCR demonstrated superior accuracy for high viral loads of influenza A, influenza B, and SARS-CoV-2, and for medium loads of RSV. It showed greater consistency and precision than RT-qPCR, particularly in quantifying intermediate viral levels, highlighting its robustness for quantitative applications [115].
NGS vs. PCR for Pathogen Detection: A 2025 comparison of NGS, real-time PCR, and HRM-PCR for Helicobacter pylori detection found that while all three methods showed similar detection rates, both PCR variants were slightly more sensitive, identifying H. pylori in two additional samples not detected by NGS. This demonstrates that despite NGS's comprehensive nature, PCR methods can provide superior sensitivity for specific targets [116].
Sensitivity Limits and Practical Detection Thresholds
The following diagram illustrates the relative detection sensitivities and optimal working ranges for each technology in liquid biopsy applications:
Implementation and Cost Analysis
Economic Considerations for Research Laboratories
The economic landscape for these technologies varies significantly based on scale, application, and instrumentation requirements:
Instrument Acquisition Costs: dPCR systems represent a moderate investment with entry-level instruments starting around $38,000, escalating with additional modules and maintenance contracts [113]. This positions dPCR between RT-qPCR (lower cost) and NGS (significantly higher cost) in terms of capital expenditure.
Consumables and Recurring Costs: Consumables dominate the ongoing expenses, representing 57.38% of the total dPCR market revenue in 2024 [113]. The per-sample cost for dPCR typically exceeds high-throughput qPCR by 2-3 times in community hospital settings [113], making project budgeting an essential consideration.
Market Growth and Adoption Trends: The dPCR market is experiencing rapid expansion, projected to grow from $857.2 million in 2025 to $3,678.8 million by 2032, exhibiting a CAGR of 23.1% [114]. This growth reflects increasing adoption in clinical research, particularly in oncology applications.
Research Reagent Solutions for Liquid Biopsy
Table 3: Essential Reagents and Materials for Liquid Biopsy Research
| Reagent/Material | Function | Technology Application | Key Considerations |
|---|---|---|---|
| cfDNA Extraction Kits (e.g., QIAamp Circulating Nucleic Acid Kit) | Isolation of cell-free DNA from plasma samples | All technologies | Maximize yield from limited plasma volumes (1-10 mL); preserve fragment integrity |
| Library Preparation Kits (e.g., Illumina DNA Prep) | Preparation of sequencing libraries | NGS | Optimize for low-input DNA (1-50 ng); incorporate UMIs for error correction |
| Target Enrichment Panels (e.g., Twist Pan-Cancer Panel) | Selection of cancer-relevant genomic regions | NGS | Balance comprehensiveness with sequencing depth; custom designs for specific cancer types |
| dPCR Supermix (e.g., Bio-Rad ddPCR Supermix) | Partition-stable PCR reaction mixture | dPCR | Ensure compatibility with partitioning technology; optimize for probe-based detection |
| TaqMan Assays | Sequence-specific detection with fluorescent probes | dPCR, RT-qPCR | Design for short amplicons (<120 bp) compatible with fragmented cfDNA |
| Quality Control Tools (e.g., Agilent Bioanalyzer) | Assessment of nucleic acid quality and quantity | All technologies | Verify fragment size distribution; confirm absence of degradation |
| Reference Standards (e.g., Seraseq ctDNA Reference Materials) | Process controls and assay validation | All technologies | Monitor technical performance; enable inter-laboratory comparison |
Strategic Implementation in Cancer Research
Technology Selection Framework
Choosing the appropriate technology depends on multiple factors, including research question, sample availability, budget, and timeline:
Select NGS when: Conducting exploratory biomarker discovery, requiring comprehensive genomic profiling, analyzing complex samples with unknown alterations, or investigating structural variants and novel fusion genes.
Choose dPCR when: Absolute quantification is required, detecting rare variants (<1% VAF), validating NGS findings, monitoring treatment response with high precision, or working with limited sample material where maximum sensitivity is needed.
Utilize RT-qPCR when: Screening for known mutations at higher allele frequencies, working with large sample cohorts requiring cost-effective analysis, operating under time constraints with rapid turnaround needs, or when institutional resources limit access to more advanced technologies.
Future Directions and Emerging Trends
The technological landscape continues to evolve with several promising developments:
Workflow Integration: Research demonstrates that these technologies are increasingly used in complementary workflows, with RT-qPCR employed both upstream for quality control and downstream for validation of NGS results [117].
Automation and Standardization: New platforms are addressing throughput limitations through automation and standardized workflows, making dPCR more accessible for routine clinical research applications [113] [114].
Multiplexing Capabilities: Advances in dPCR instrumentation, such as the Bio-Rad QX600 system, enable higher multiplexing (up to 6 colors), expanding the information obtainable from single reactions [114].
Cost Reduction Strategies: As technologies mature and competition increases, cost reductions are making these tools more accessible, particularly in the dPCR market where emerging competitors are introducing more affordable solutions [114].
The strategic selection and implementation of NGS, dPCR, and RT-qPCR technologies enables researchers to address distinct challenges in liquid biopsy for cancer detection. NGS provides unparalleled comprehensive profiling capabilities, dPCR offers exceptional sensitivity for rare variant detection and absolute quantification, while RT-qPCR delivers cost-effective, rapid analysis for high-throughput applications. By understanding the specific strengths, limitations, and optimal applications of each technology within integrated workflows, research laboratories can maximize their scientific output and advance the field of liquid biopsy for improved cancer detection and monitoring.
Regulatory Landscape and Guidelines for Clinical Implementation
The integration of reverse transcription quantitative polymerase chain reaction (RT-qPCR) into liquid biopsy workflows represents a transformative approach for cancer detection and monitoring. This sensitive technique enables researchers to detect and quantify circulating RNA biomarkers from minimally invasive blood samples, providing insights into tumor heterogeneity, treatment response, and emerging resistance mechanisms. However, the path from promising research to clinically validated diagnostic test is fraught with regulatory and technical challenges. The regulatory landscape for such tests is necessarily stringent, requiring demonstrated analytical validity, clinical validity, and clinical utility [26]. Compliance with established guidelines is not merely a bureaucratic hurdle but a fundamental requirement for ensuring that liquid biopsy tests produce reliable, reproducible, and clinically actionable results. This guide examines the current regulatory frameworks and provides detailed technical protocols for developing RT-qPCR-based liquid biopsy tests that meet the exacting standards required for clinical implementation.
Navigating the Regulatory Framework
Key Regulatory Bodies and Approval Pathways
The journey to clinical implementation requires navigation through complex regulatory pathways governed by agencies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). These bodies evaluate diagnostic tests based on robust evidence of their safety and effectiveness. The FDA Breakthrough Device Program has fast-tracked several liquid biopsy tests, acknowledging their potential to address unmet clinical needs. For example, multi-cancer early detection tests like Galleri (GRAIL) and OverC MCDBT have received this designation, signaling a regulatory environment conducive to innovation while maintaining rigorous standards [26].
Table 1: Key Regulatory Designations for Liquid Biopsy Tests
| Designation/Approval | Agency | Example Test | Cancer Type | Purpose |
|---|---|---|---|---|
| FDA Approval | FDA | Epi proColon, Shield | Colorectal Cancer | Detection |
| FDA Breakthrough Device | FDA | Galleri (GRAIL) | Multiple Cancers | Early Detection |
| FDA Breakthrough Device | FDA | OverC MCDBT | Multiple Cancers | Early Detection |
The specific regulatory pathway depends on the test's intended use. Tests developed and used within a single laboratory (Laboratory Developed Tests, or LDTs) historically fell under the enforcement discretion of the FDA, but they are now transitioning toward more active FDA oversight. Regardless of the pathway, the foundational requirements of analytical and clinical validation remain paramount.
Foundational Guidelines: The MIQE Framework
For any RT-qPCR assay intended for clinical use, adherence to the Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines is considered the gold standard for ensuring technical rigor [118]. The updated MIQE 2.0 guidelines, published in 2025, provide a critical framework for the entire qPCR workflow, from sample handling to data analysis. These guidelines were developed by an international consortium of experts and have informed the development of ISO standards for molecular diagnostics [118].
Compliance with MIQE is essential because it addresses common points of failure in translational research:
- Poor transparency in reporting methods and results.
- Absent or inappropriate assay validation, including failure to calculate PCR efficiency.
- Use of unvalidated reference genes for normalization.
- Overinterpretation of small fold-changes (e.g., 1.2- to 1.5-fold) without assessment of technical variance [118].
The consequences of non-compliance are not merely academic; they can lead to exaggerated sensitivity claims, irreproducible data, and ultimately, diagnostic tests that are not fit for clinical purpose.
Technical Validation and Quality Control
The MIQE 2.0 Checklist for Liquid Biopsies
Successfully navigating the regulatory landscape requires meticulous experimental design and validation. The following checklist, adapted from MIQE 2.0, outlines the essential technical data required for a regulatory submission.
Table 2: Essential Technical Validation Data for Regulatory Submissions
| Category | Requirement | Details & Acceptable Range |
|---|---|---|
| Sample Information | Pre-analytical processing | Sample type (e.g., plasma), collection tube, processing protocol, storage conditions |
| RNA Integrity | RIN (RNA Integrity Number) or equivalent metric | |
| Assay Validation | PCR Efficiency | 85%–110% (must be calculated, not assumed) [119] |
| Specificity | Amplicon sequencing or melt curve analysis | |
| Dynamic Range | At least 5 logs of concentration | |
| Data Analysis | Normalization | Use of one or more validated reference genes |
| Controls | No-RT control, no-template control | |
| Statistical Justification | Description of replication scheme and statistical tests |
Detailed Experimental Protocol: A Roadmap to Compliance
The following protocol provides a step-by-step guide for developing a robust RT-qPCR assay for liquid biopsy applications, incorporating regulatory requirements at each stage.
Step 1: Sample Collection and RNA Extraction
- Liquid Biopsy Source: Collect blood in cell-stabilizing tubes (e.g., Streck, PAXgene) to prevent genomic DNA contamination and preserve RNA integrity. Plasma is preferred over serum for ctDNA and RNA analyses due to lower background and higher stability of tumor-derived material [26]. Process samples within a strict pre-analytical window (e.g., within 6 hours of draw) to minimize RNA degradation.
- RNA Extraction: Use silica-membrane or magnetic bead-based kits designed for low-abundance RNA from plasma. Include carrier RNA to improve yield. Document the elution volume and quantify RNA using a sensitive fluorescence-based method. Assess RNA integrity if sufficient material is available.
Step 2: Reverse Transcription and Assay Design
- Reverse Transcription: Use a robust reverse transcriptase with high thermal stability to handle RNA secondary structures. For comprehensive coverage of both poly-A and non-poly-A RNAs (including some circular RNAs), use a mixture of random hexamers and anchored oligo(dT) primers [4] [5]. Always include a no-reverse transcriptase control (-RT control) to detect genomic DNA contamination [4].
- qPCR Primer/Probe Design:
- Design primers to span exon-exon junctions wherever possible to prevent amplification of contaminating genomic DNA [4] [5].
- Ensure amplicon length is between 70–200 base pairs for optimal efficiency from fragmented circulating RNA.
- Maintain primer GC content between 40%–60% and avoid self-complementarity or secondary structures using tools like OligoAnalyzer or Primer3Plus [5].
- For maximum specificity, use hydrolysis probes (e.g., TaqMan) instead of intercalating dyes like SYBR Green, especially for multiplex assays.
Step 3: PCR Efficiency Calculation and Validation
- Procedure: Prepare a standard curve using a serial dilution (e.g., 1:10, 1:100, 1:1000, 1:10000) of a synthetic template or a calibrator cDNA with known concentration [119].
- Calculation: Run the dilution series in triplicate by qPCR. Plot the average Ct value against the log10 of the dilution factor. The slope of the standard curve is used in the formula: Efficiency (%) = (10–1/slope – 1) × 100 [119].
- Acceptance Criterion: Assays with efficiencies between 85% and 110% are typically considered acceptable. An efficiency outside this range requires re-optimization of the assay [119].
Step 4: Data Normalization and Analysis
- Normalization: Normalize target gene expression to one or more validated reference genes (e.g., GAPDH, β-actin) that are stably expressed across all sample groups. The stability of reference genes must be empirically validated for the specific liquid biopsy matrix and patient cohort [118].
- Quantification Methods:
- Livak (2–ΔΔCt) Method: Use this method only when the amplification efficiencies of the target and reference genes are approximately equal and close to 100% [119] [120].
- Pfaffl Method: This is the more rigorous approach, as it corrects for differences in amplification efficiency between the target and reference genes. The formula is: Fold Change = (Etarget)–ΔCt(target) / (Eref)–ΔCt(ref) [120].
- Statistical Analysis: Use specialized software and packages like the
rtpcrpackage in R, which incorporates efficiency values into its calculations for statistical tests (t-test, ANOVA) and graphical presentation, aligning with the Pfaffl method [120].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for RT-qPCR Liquid Biopsy Assays
| Item | Function | Technical Considerations |
|---|---|---|
| Cell-Free RNA Collection Tubes | Stabilizes blood cells & preserves cell-free RNA | Prevents dilution of tumor-derived RNA by genomic RNA from lysed blood cells. |
| Reverse Transcriptase with High Thermal Stability | Synthesizes cDNA from RNA templates | Enables cDNA synthesis at higher temperatures, facilitating the transcription of RNA with significant secondary structure [4]. |
| qPCR Probes (TaqMan) | Target-specific fluorescence detection | Provide superior specificity over dye-based methods; essential for multiplexing. |
| Validated Reference Genes | Normalization of gene expression data | Must demonstrate stable expression in healthy and disease-state liquid biopsies [118]. |
| Synthetic Standard Curves | Absolute quantification & efficiency calculation | Allows for precise determination of copy number and PCR efficiency without biological variability. |
| RNase Inhibitors | Prevents degradation of RNA templates | Critical for maintaining RNA integrity throughout the RT and qPCR workflow [5]. |
Visualizing the Clinical Implementation Workflow
The following diagram outlines the critical stages from assay development to regulatory approval, highlighting key decision points and requirements.
The successful clinical implementation of an RT-qPCR-based liquid biopsy test hinges on a steadfast commitment to regulatory and technical rigor from the earliest stages of development. By integrating the MIQE 2.0 guidelines, meticulously validating each step of the analytical workflow, and designing studies that unequivocally demonstrate clinical value, researchers can bridge the translational gap between promising laboratory results and a robust, clinically deployed diagnostic tool. The regulatory pathway, while demanding, provides the necessary structure to ensure that these powerful tests are safe, effective, and reliable, ultimately building a foundation of trust for their use in guiding patient care.
Minimal residual disease (MRD) refers to the residual cancer cells that persist in patients following treatment, even when no visible tumor is detected, and is a primary cause of relapse in cancer [121]. In high-risk neuroblastoma, the most common extracranial solid tumor in children, MRD monitoring is particularly crucial as more than half of patients achieving initial remission eventually relapse due to residual disease [121] [89]. Despite intensive multimodal treatment, long-term survival for high-risk neuroblastoma remains approximately 50%, creating an urgent need for sensitive MRD detection methods to guide therapy adjustments [121] [122].
Reverse transcriptase quantitative polymerase chain reaction (RT-qPCR) has emerged as a highly sensitive technique for detecting MRD in neuroblastoma by quantifying neuroblastoma-associated messenger RNAs (NB-mRNAs) in bone marrow (BM), peripheral blood (PB), and other biological fluids [121] [53]. This case study examines the technical implementation, clinical validation, and research applications of RT-qPCR for MRD monitoring in high-risk neuroblastoma, positioning it within the broader context of liquid biopsy advancements for cancer management.
Technical Foundations of RT-qPCR for Neuroblastoma MRD
Neuroblastoma-Associated mRNA Targets
Neuroblastoma presents a unique challenge for MRD detection due to its lack of recurrent genetic aberrations like the fusion genes found in leukemias and sarcomas [121]. Consequently, MRD detection relies on quantifying mRNAs specifically expressed in tissues of neuroblastoma origin. Over 28 NB-mRNAs have been identified as potential MRD markers over the past decades [121].
The most robust targets demonstrate high expression in neuroblastoma tumors with minimal or no expression in normal BM and PB. PHOX2B (paired-like homeobox 2b) has emerged as the most specific and sensitive single marker, encoding a transcription factor involved in the development of noradrenergic neuron populations [121] [53] [89]. Other well-validated markers include TH (tyrosine hydroxylase), the rate-limiting enzyme in catecholamine biosynthesis; DDC (dopa decarboxylase); CHGA (chromogranin A); and DCX (doublecortin) [121] [123].
Table 1: Key Neuroblastoma-Associated mRNA Markers for MRD Detection
| Gene Symbol | Gene Name | Cellular Function | Expression Specificity | Clinical Utility |
|---|---|---|---|---|
| PHOX2B | Paired-like homeobox 2b | Transcription factor development | Highly specific to neuroblastoma lineage | Most sensitive single marker [53] [89] |
| TH | Tyrosine hydroxylase | Catecholamine synthesis rate-limiting enzyme | Adrenergic phenotype | First NB-mRNA used for MRD detection [121] [123] |
| DDC | Dopa decarboxylase | Catecholamine synthesis | Adrenergic phenotype | Component of 5-gene panel (NB5) [123] |
| CHGA | Chromogranin A | Neuroendocrine secretory protein | Adrenergic phenotype | Component of 5-gene panel (NB5) [123] |
| GAP43 | Growth associated protein 43 | Neural development protein | Adrenergic phenotype | BM panel component [53] [89] |
| CHRNA3 | Cholinergic receptor nicotinic alpha 3 subunit | Neuronal signaling | Adrenergic phenotype | PB panel component [53] [89] |
| DBH | Dopamine beta-hydroxylase | Catecholamine synthesis | Adrenergic phenotype | PB panel component [53] |
| POSTN | Periostin | Extracellular matrix protein | Mesenchymal phenotype | Detects therapy-resistant cells [53] [54] |
| PRRX1 | Paired related homeobox 1 | Transcription factor | Mesenchymal phenotype | Mesenchymal panel component [53] |
Tumor Heterogeneity and Marker Panels
Neuroblastoma tumors exhibit significant heterogeneity, comprising at least two interconvertible cell types with distinct gene expression profiles: committed adrenergic (ADR) cells and undifferentiated mesenchymal (MES) cells [121] [53]. This plasticity necessitates multiple mRNA targets for comprehensive MRD detection, as no single marker identifies all neuroblastoma cells [53].
The NB5 assay incorporates five genes (CHGA, DCX, DDC, PHOX2B, and TH) and demonstrates significantly higher sensitivity for detecting MRD compared to flow cytometry or histology [123]. Alternative panels have been optimized for different sample types, with PHOX2B, TH, CHRNA3, and GAP43 forming the core BM panel, while PHOX2B, TH, CHRNA3, and DBH constitute the PB panel [53] [89].
The recognition that MES-type cells may resist therapy and contribute to relapse has prompted development of MES-specific marker panels including POSTN and PRRX1, which identify the therapy-resistant cell population [53] [54].
Methodological Workflow and Protocol Optimization
Sample Collection and RNA Extraction
Standardized sample collection is critical for reliable MRD detection. BM aspirates are typically collected from bilateral iliac crests in EDTA tubes, with PB collected in PAXgene Blood RNA tubes [54] [89]. Within 24 hours of collection, samples should be transferred to PAXgene Blood RNA tubes (if not already collected in them) and stored at -20°C until processing [89].
RNA isolation employs the PAXgene Blood RNA Kit (QIAGEN), with 2-3 µg of total RNA used for cDNA synthesis [89]. The cDNA synthesis utilizes random hexamers (25 µmol/L), dNTPs (1 mmol/L), and MMLV reverse transcriptase (100U) in a 40 µL reaction volume incubated at 42°C for 45 minutes [89]. The resulting cDNA is diluted to 100 µL for subsequent RT-qPCR analysis [89].
Multiplex RT-qPCR Assay Development
To address the limited sample volumes available from pediatric patients, multiplex RT-qPCR assays have been developed that simultaneously detect multiple NB-mRNAs in a single reaction [53]. This approach conserves precious samples while providing comprehensive phenotyping of residual disease.
The technical optimization requires careful primer and probe redesign with fluorophores (FAM, Yakima Yellow, Dragonfly Orange) matched to available detection channels and appropriate quenchers [53]. Master mix composition must be optimized to prevent fluorescence quenching; specifically, ROX reference dye must be replaced with Mustang Purple when using Dragonfly Orange fluorophores, and dithiothreitol (DTT) should be eliminated from reverse transcription mixes as it quenches Mustang Purple fluorescence [53]. The High-Capacity RNA-to-cDNA Kit (Applied Biosystems) provides superior cDNA synthesis efficiency, yielding lower Ct values for reference genes [53].
Table 2: Key Performance Parameters for RT-qPCR MRD Detection
| Parameter | Target Specification | Validation Approach |
|---|---|---|
| Sensitivity | 1 tumor cell in 10^5-10^6 normal cells [121] [54] | Dilution curves of neuroblastoma cell lines in normal BM/PB [53] |
| Specificity | No amplification in control BM/PB [53] | Testing on 54 control BM and 50 control PB samples [53] |
| RNA Input | As low as 80 ng total RNA [53] | GUSB Ct value ≤24 with 4.5 ng RNA per reaction [53] |
| Positivity Threshold | ΔCtsample < 3.0 Ct than median ΔCtcontrol tissue [53] | Based on expression in control BM/PB samples following ESMRD guidelines [53] |
| Dynamic Range | 5-6 logs of detection [53] | Serial dilutions of neuroblastoma cell line RNA [53] |
Quality Control and Technical Considerations
Robust quality control measures are essential for reliable MRD detection. The reference gene beta-glucoronidase (GUSB) is typically used for normalization [89]. False positives from genomic DNA amplification can occur with certain markers, particularly TH, requiring careful primer design and data interpretation algorithms incorporating AMPSCORE, CQCONF score, and ΔRn values to distinguish true from false amplifications [53].
Sample-specific positivity thresholds must be established based on expression levels in control BM and PB samples, generally defined as ΔCtsample < 3.0 Ct than median ΔCtcontrol tissue, with Ct_sample < 40 [53]. This standardized approach ensures consistent MRD detection across different laboratories and sample types.
Clinical Validation and Prognostic Significance
Prospective Multicenter Studies
Recent large-scale prospective studies have validated the clinical utility of RT-qPCR for MRD monitoring in high-risk neuroblastoma. The international GPOH-DCOG validation study analyzed 345 high-risk neuroblastoma patients treated in NB2004 (GPOH) or NBL2009 (DCOG) trials, assessing serial BM samples using PHOX2B, TH, DDC, CHRNA3, and GAP43 mRNA markers [89].
This study demonstrated that BM infiltration >10% by RT-qPCR at diagnosis was prognostic for inferior survival, with adjusted hazard ratios of 1.82 for event-free survival (EFS) and 2.04 for overall survival (OS) [89]. Critically, any post-induction RT-qPCR positivity correlated with poor outcomes, with EFS of 26.6% versus 60.4% for RT-qPCR-negative patients [89]. In contrast, post-induction immunocytology positivity showed no significant association with survival, highlighting the superior predictive value of RT-qPCR [89].
A separate multicenter study of 509 BM specimens from 108 high-risk patients demonstrated that combined automatic immunofluorescence plus iFISH (AIPF) and RT-qPCR complemented each other in detecting MRD and characterizing ADRN and MES phenotypes [54]. RT-qPCR-ADRN alone frequently detected low tumor cell burden missed by conventional methods, while RT-qPCR-MES identified 37 additional cases and showed delayed clearance of MES markers post-chemotherapy [54].
Comparative Analytical Performance
The analytical performance of RT-qPCR surpasses conventional detection methods. A study of 71 patients with relapsed/refractory neuroblastoma demonstrated that the NB5 assay (CHGA, DCX, DDC, PHOX2B, TH) showed 100% sensitivity and specificity for predicting relapse, significantly outperforming flow cytometric MRD detection [123]. BM specimens exhibited 45.455% positive results by NB5 assay compared to 17.045% by flow cytometry [123].
Table 3: Clinical Validation of RT-qPCR MRD Detection in Multicenter Studies
| Study | Patients | MRD Markers | Key Findings | Prognostic Impact |
|---|---|---|---|---|
| GPOH-DCOG Validation [89] | 345 high-risk patients | PHOX2B, TH, DDC, CHRNA3, GAP43 | Post-induction positivity: 26.6% 5-year EFS vs 60.4% for negative patients | HR 2.10 for EFS; HR 1.76 for OS |
| Multicenter BM Study [54] | 108 high-risk patients | ADRN and MES panels | RT-qPCR-MES identified 37 additional cases; delayed MES clearance post-chemotherapy | MES increases prior to relapse |
| NB5 Assay Study [123] | 71 relapsed/refractory patients | CHGA, DCX, DDC, PHOX2B, TH | 100% sensitivity and specificity for predicting relapse | Independent prognostic factor (HR 3.046) |
| SIOPEN Study [121] | Multiple centers | TH, PHOX2B, DCX | mRNA transcripts above threshold correlate with poorer prognosis | Validated in different treatment regimens |
Temporal Dynamics and MRD Clearance
The timing of MRD assessment critically impacts its prognostic value. BM infiltration levels at diagnosis provide initial risk stratification, but persistence after induction therapy is particularly predictive of poor outcomes [89]. The rate of MRD clearance during treatment offers dynamic response assessment, with rapid clearance associated with favorable prognosis [54] [89].
Longitudinal monitoring reveals distinct patterns for ADRN and MES markers. While ADRN markers typically decrease during effective therapy, MES markers may persist or even increase following chemotherapy, potentially indicating phenotype switching and emergence of therapy-resistant clones [54]. This differential clearance pattern underscores the importance of monitoring both phenotypic states throughout treatment.
Advanced Research Applications
Phenotype Switching and Therapy Resistance
Neuroblastoma cells demonstrate remarkable plasticity, transitioning between ADRN and MES states in response to therapy [53] [54]. MES-type cells lack expression of conventional MRD markers like PHOX2B and DBH, and may also show reduced expression of immunotherapy targets such as GD2 and CD56, enabling immune escape [53] [54].
Multimodal BM analysis demonstrates that MES markers (POSTN, PRRX1) frequently persist after chemotherapy and increase prior to relapse, suggesting enrichment of therapy-resistant MES cells during treatment [54]. This phenotype switching has direct implications for immunotherapy efficacy, as evidenced by the identification of GD2-negative tumor cells in 5/108 patients, potentially explaining limited responses to anti-GD2 antibody therapy in some cases [54].
Integration with Other Liquid Biopsy Modalities
RT-qPCR-based MRD detection complements other liquid biopsy approaches. Circulating tumor DNA (ctDNA) analysis detects tumor-specific mutations, while RT-qPCR identifies living tumor cells based on their transcriptional profile [3] [1]. These approaches provide orthogonal information about tumor burden and evolution.
Automated immunofluorescence plus interphase FISH (AIPF) enables quantification of disseminated tumor cells (DTCs) at the single-cell level with genetic verification, providing morphological and genetic context that complements RT-qPCR's higher throughput and sensitivity [54]. The integration of these techniques creates a comprehensive liquid biopsy platform for disease monitoring and therapy personalization.
Research Reagent Solutions
Table 4: Essential Research Reagents for RT-qPCR MRD Detection
| Reagent/Catalog Item | Function | Application Notes |
|---|---|---|
| PAXgene Blood RNA Tubes (QIAGEN) | RNA stabilization during sample collection | Maintains RNA integrity for 24h at room temperature [89] |
| PAXgene Blood RNA Kit (QIAGEN) | RNA isolation from blood/BM | Integrated DNase treatment prevents gDNA contamination [89] |
| High-Capacity RNA-to-cDNA Kit (Applied Biosystems) | cDNA synthesis | Replaces traditional MMLV-based methods; eliminates DTT quenching [53] |
| TaqMan Fast Universal PCR Master Mix (Applied Biosystems) | qPCR amplification | Optimized for fast cycling conditions [89] |
| Custom TaqMan Assays | Target-specific detection | FAM/YY/DFO fluorophores with BHQ quenchers [53] |
| Neuroblastoma Cell Lines (IMR32, SH-SY5Y, 691-MES/691-ADRN) | Assay validation | ADRN and MES phenotypes for sensitivity controls [53] |
| Step-One-Plus or Viia7 Real-Time PCR Systems (Applied Biosystems) | Amplification detection | Compatible with multiplex fluorophores [53] [89] |
RT-qPCR has matured into a validated, highly sensitive method for MRD detection in high-risk neuroblastoma, with demonstrated prognostic significance in large prospective multicenter studies. The technology's ability to detect residual disease at levels far below conventional methods provides critical insights into treatment response and disease dynamics. The development of multiplex assays addressing tumor heterogeneity through ADRN and MES marker panels represents a significant advancement in comprehensive disease monitoring.
Implementation of standardized RT-qPCR protocols in clinical trials enables robust MRD assessment that can guide therapy intensification or de-escalation. The integration of RT-qPCR with other liquid biopsy modalities creates a powerful multidimensional approach to monitoring treatment response, phenotype switching, and emergence of therapy resistance. As neuroblastoma therapy evolves, particularly with the expanding role of immunotherapies, RT-qPCR-based MRD detection will play an increasingly important role in personalizing treatment strategies and improving outcomes for high-risk patients.
Conclusion
RT-qPCR remains a cornerstone technology in liquid biopsy, offering a highly sensitive, standardized, and cost-effective method for cancer detection and monitoring. Its proven utility in prospective clinical studies, such as for minimal residual disease in neuroblastoma where it outperforms traditional immunocytology, solidifies its role in modern oncology. The successful implementation of multi-marker mRNA panels demonstrates high prognostic value for patient stratification. Future directions involve standardizing protocols across laboratories, integrating with emerging technologies like CRISPR and AI for enhanced sensitivity, and expanding its application into multi-cancer early detection and real-time therapy response monitoring. For researchers and drug developers, RT-qPCR provides a robust and clinically actionable platform to advance personalized cancer medicine.
References
- 1. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 2. Longitudinal Multi-Parametric Liquid Biopsy Approach ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7912374/]
- 3. Cancer in a Drop: Liquid biopsy insights from AACR 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223554/]
- 4. Basic Principles of RT-qPCR [https://www.thermofisher.com/us/en/home/brands/thermo-scientific/molecular-biology/molecular-biology-learning-center/molecular-biology-resource-library/spotlight-articles/basic-principles-rt-qpcr.html]
- 5. Brief guide to RT-qPCR - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11612376/]
- 6. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 7. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOooQ2Ciiib_JP603xtZSl2gwiLktEnoK5CIjy8dbTipNSW1zf1ly]
- 8. Significant Expansion of Real-Time PCR Multiplexing with ... [https://www.nature.com/articles/s41598-018-37732-y]
- 9. Liquid biopsy for human cancer: cancer screening, monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11130638/]
- 10. The growing field of liquid biopsy and its Snowball effect on ... [https://www.sciencedirect.com/science/article/pii/S2950195425000098]
- 11. innovative approaches for cancer diagnosis and analysis [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05908-y]
- 12. Circulating microRNAs in Cancer: A 5-Year Update with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10969845/]
- 13. functional biomarkers for melanoma prognosis and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02298-7]
- 14. MicroRNAs: circulating biomarkers for the early detection ... [https://www.nature.com/articles/s41388-024-03076-3]
- 15. Current Trends in Liquid Biopsy Tracking Resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027453/]
- 16. A Novel High-Fidelity DNA Polymerase-driven or Taq ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400525013358]
- 17. Integrating AI and RNA biomarkers in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512311/]
- 18. qPCR in Early Cancer Detection: Why It Still Leads the Pack [https://www.meridianbioscience.com/lifescience-blog/why-qpcr-still-leads-in-oncology/]
- 19. Analysis, How a qPCR Machine Works... | Technology Networks qPCR [https://www.technologynetworks.com/analysis/articles/qpcr-analysis-how-a-qpcr-machine-works-and-qpcr-protocol-356835]
- 20. A simple and cost-effective real-time PCR method using ... [https://www.nature.com/articles/s41598-024-78802-8]
- 21. Optimizing SARS-CoV-2 Detection: A Rapid, Cost-Effective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374254/]
- 22. of Standardisation from real-time data methods... quantitative PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC1326201/]
- 23. Selection and validation of reference genes for RT-qPCR ... [https://www.nature.com/articles/s41598-025-02951-7]
- 24. Advanced breast cancer diagnosis: Multiplex RT-qPCR for ... [https://www.sciencedirect.com/science/article/pii/S2405580823001966]
- 25. Circular RNA-based liquid biopsy: a promising approach for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635984/]
- 26. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 27. Liquid biopsy: Comprehensive overview of circulating tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11420644/]
- 28. Assessment of Pre-Analytical Sample Handling Conditions ... [https://www.sciencedirect.com/science/article/pii/S1525157820303512]
- 29. Not All Blood Collection Tubes are Created Equal [https://myadlm.org/cln/cln-industry-insights/2025/not-all-blood-collection-tubes-are-created-equal-choosing-the-right-tube-for-the-right-test]
- 30. Laboratory Tube Collection - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK555991/]
- 31. Liquid biopsy: A tool for non-invasive cancer detection and ... [https://www.abcam.com/en-us/knowledge-center/oncology/liquid-biopsy-for-non-invasive-cancer-detection]
- 32. Comprehensive Protocol to Sample and Process Bone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5931431/]
- 33. Bone marrow aspirates and cryopreservation [https://bio-protocol.org/exchange/minidetail?id=18758205&type=30]
- 34. Clinical application and detection techniques of liquid biopsy ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01715-z]
- 35. The top pros and cons of different RNA extraction methods [https://lifescience.roche.com/global/en/article-listing/article/the-top-pros-and-cons-of-different-rna-extraction-methods.html]
- 36. RNA isolation: Methods, challenges, and applications [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/rna/rna-purification/rna-isolation-sample-source-considerations]
- 37. A straightforward method to quantify circulating mRNAs as ... [https://www.nature.com/articles/s41598-023-29948-4]
- 38. Current Nucleic Acid Extraction Methods and Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5529626/]
- 39. Common Issues and Troubleshooting in RNA Extraction Using ... [https://www.yeasenbio.com/blogs/molecular-biology/common-issues-and-troubleshooting-in-rna-extraction-using-trizol]
- 40. Comparison of Methods for miRNA Extraction from Plasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3655275/]
- 41. Review of microRNA detection workflows from liquid biopsy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11879380/]
- 42. Amplification-Free Testing of microRNA Biomarkers in ... [https://www.mdpi.com/2072-6694/17/16/2715]
- 43. Quantification of distinct let-7 microRNA family members by a modified... [https://www.spandidos-publications.com/mmr/17/3/3690]
- 44. Accurate quantification of 3′-terminal 2′-O-methylated small RNAs by... [https://link.springer.com/article/10.1007/s11684-021-0909-7]
- 45. - Stem - loop for miRNAs RT qPCR [https://pubmed.ncbi.nlm.nih.gov/21732315/]
- 46. Optimization and Validation of a Folate Ligand-Targeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530657/]
- 47. Advances in Research on Isothermal Signal Amplification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190449/]
- 48. Comparison of SYBR Green and TaqMan methods in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3988599/]
- 49. How qPCR works: SYBR Green vs TaqMan | INTEGRA [https://www.integra-biosciences.com/united-states/en/blog/article/how-qpcr-works-sybrr-green-vs-taqmanr]
- 50. TaqMan vs. SYBR Chemistry for Real-Time PCR [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/taqman-vs-sybr-chemistry-real-time-pcr.html]
- 51. Comparison of analytical sensitivity and efficiency for SARS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8881549/]
- 52. Development and validation of cost-effective SYBR Green ... [https://www.nature.com/articles/s41598-024-52250-w]
- 53. Specific and Sensitive Detection of Neuroblastoma mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7796198/]
- 54. Sensitive detection of minimal residual disease and ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03481-w]
- 55. MiRNA expression profiling in adenocarcinoma and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9388044/]
- 56. Profiling of 179 miRNA Expression in Blood Plasma ... [https://www.nature.com/articles/s41598-018-24769-2]
- 57. Identification of New Molecular Biomarkers in Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9267752/]
- 58. Innovative qPCR Algorithm Using Platelet-Derived RNA for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11988175/]
- 59. Sensitive liquid biopsy monitoring correlates with outcome in the prospective international GPOH-DCOG high-risk neuroblastoma RT-qPCR validation study - PubMed [https://pubmed.ncbi.nlm.nih.gov/39722049/]
- 60. Distinct Expression Profiles of Neuroblastoma-Associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11117621/]
- 61. Assessment of a six gene panel for the molecular detection of ... [https://bmccancer.biomedcentral.com/articles/10.1186/1471-2407-10-666]
- 62. Expression Pattern of Tumor-associated Antigens in ... [https://www.cancerdiagnosisprognosis.org/article/275/expression-pattern-of-tumor-associated-antigens-in-neuroblastoma-association-with-cytogenetic-features-and-survival]
- 63. PHOX2B is a novel and specific marker for minimal residual disease testing in neuroblastoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/18838715/?dopt=Abstract]
- 64. A multimarker QPCR-based platform for the detection of ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3111197/]
- 65. Establishment of a multimarker qPCR panel for the ... [https://www.oncotarget.com/article/9528/text/]
- 66. Expression of neuroblastoma-related genes in bone marrow ... [https://pubmed.ncbi.nlm.nih.gov/35441784/]
- 67. The Impact of Hemolysis on Cell-Free microRNA Biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC3663194/]
- 68. A simple method to monitor hemolysis in real time [https://www.nature.com/articles/s41598-020-62041-8]
- 69. Evaluation of the impact of pre-analytical conditions on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9374597/]
- 70. Sampling, Logistics, and Analytics of Urine for RT-qPCR- ... [https://pubmed.ncbi.nlm.nih.gov/34503191/]
- 71. Impact of different stabilization methods on RT-qPCR ... [https://www.nature.com/articles/s41598-020-60618-x]
- 72. Real-Time qPCR-Based Detection of Circulating Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4960365/]
- 73. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 74. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 75. Ultrasensitive detection of clinical pathogens through a ... [https://www.nature.com/articles/s41467-025-59219-x]
- 76. Evaluation and validation of reference genes for RT-qPCR ... [https://www.nature.com/articles/s41598-025-22650-7]
- 77. Integrating AI and RNA biomarkers in cancer: advances in ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02434-2]
- 78. Validation of reference genes for the normalization of RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5431254/]
- 79. Validation of Endogenous Control Genes by Real-Time ... [https://www.mdpi.com/2073-4425/15/2/151]
- 80. Assessing the necessity of technical replicates in reverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12315840/]
- 81. International society of liquid biopsy (ISLB) perspective on ... [https://www.sciencedirect.com/science/article/pii/S2950195425000177]
- 82. Sensitive liquid biopsy monitoring correlates with outcome ... [https://pubmed.ncbi.nlm.nih.gov/39722049]
- 83. Establishing PNB-qPCR for quantifying minimal ctDNA ... [https://www.nature.com/articles/s41598-017-09137-w]
- 84. Determining lower limits of detection of digital PCR assays ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5129438/]
- 85. Validation of a liquid biopsy assay with increased ... [https://www.sciencedirect.com/science/article/pii/S2950195425000384]
- 86. Standardization of Sequencing Coverage Depth in NGS [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2019.00851/full]
- 87. Review Liquid biopsy-based multi-cancer early detection [https://www.sciencedirect.com/science/article/pii/S2095927325006565]
- 88. Liquid biopsy and PCR-free ultrasensitive detection systems ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6086621/]
- 89. Sensitive liquid biopsy monitoring correlates with outcome in ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-024-03261-y]
- 90. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 91. Optimization Tips for Luna® One-Step RT-qPCR [https://www.neb.com/en-us/tools-and-resources/usage-guidelines/optimization-tips-for-luna-one-step-rt-qpcr?srsltid=AfmBOorIv6Pen_pWMhd6tTH974F8k-ghO5tIE_0dchmFXSxkf6EceB4f]
- 92. qPCR Primer Design: A Handy Step-by-Step Guide [https://bitesizebio.com/10041/designing-qpcr-primers/]
- 93. Multiplexed, universal probe-based rare variant detection ... [https://www.nature.com/articles/s41598-025-08814-5]
- 94. Standardized Workflow and Analytical Validation of Cell ... [https://www.mdpi.com/2073-4409/14/14/1062]
- 95. PrimerQuest PCR & qPCR Primer Design Tool | IDT [https://www.idtdna.com/pages/tools/primerquest]
- 96. Clinical application and detection techniques of liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9832643/]
- 97. Preoperative liquid biopsy transcriptomic panel for risk ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03305-x]
- 98. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOorYD_-ebBGXvTqwKRs1q1UsCa4-YNaP101G__lhMpvBa3pHZw77]
- 99. RNA isolation, RT-PCR, qPCR and endpoint PCR [https://lantsandlaminins.com/writing-guides/writing-materials-and-methods-section-for-your-phd-project-manuscript/rna-isolation-rt-pcr-qpcr-and-endpoint-pcr/]
- 100. Consensus Statement From the Third Neuroblastoma Drug ... [https://pubmed.ncbi.nlm.nih.gov/40509548/]
- 101. RT-PCR demonstrates superior sensitivity and specificity in ... [https://tp.amegroups.org/article/view/120154/html]
- 102. Level of Seven Neuroblastoma-Associated mRNAs ... [https://www.sciencedirect.com/science/article/pii/S1525157819304374]
- 103. Recent Research Advances for High-Risk Neuroblastoma [https://www.mskcc.org/clinical-updates/msk-kids-recent-research-advances-for-high-risk-neuroblastoma]
- 104. Sensitive liquid biopsy monitoring correlates with outcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11670466/]
- 105. Case series on clinical applications of liquid biopsy in ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1209150/full]
- 106. Prediction Model of Bone Marrow Infiltration in Patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9256353/]
- 107. Quantitative PCR detection of NPM/ALK fusion gene and ... [https://www.sciencedirect.com/science/article/abs/pii/S0145212607000112]
- 108. Comparison of immunocytochemistry, real-time quantitative ... [https://pubmed.ncbi.nlm.nih.gov/15942651/]
- 109. Real-time RT–PCR correlates with immunocytochemistry for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2410046/]
- 110. Sensitive detection of minimal residual disease and ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12317575/]
- 111. NGS, qPCR, or Sanger Sequencing: An Assay Selection ... [https://blog.genewiz.com/ngs-qpcr-or-sanger-sequencing-an-assay-selection-guide]
- 112. Digital droplet PCR is an accurate and precise method to ... [https://www.nature.com/articles/s41598-025-20944-4]
- 113. Digital PCR Market Size, Forecast Report [https://www.mordorintelligence.com/industry-reports/digital-pcr-market]
- 114. Digital PCR Market Share, Growth Analysis | Forecast [2032] [https://www.fortunebusinessinsights.com/digital-pcr-market-102014]
- 115. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 116. Comparison of Next-Generation Sequencing, Real-Time ... [https://www.mdpi.com/2076-2607/13/10/2344]
- 117. Real-Time PCR (qPCR) and Whole-Transcriptome NGS [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/ngs-comparison.html]
- 118. MIQE 2.0 and the Urgent Need to Rethink qPCR Standards [https://pmc.ncbi.nlm.nih.gov/articles/PMC12154065/]
- 119. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOor_wwwEWfHngBuEcR2UNLcNUZuct-gVbJvyXsYZt4dPkXEhaDU3]
- 120. rtpcr: a package for statistical analysis and graphical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530193/]
- 121. Evaluation of Minimal Residual Disease in Patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227348/]
- 122. Neuroblastoma Treatment (PDQ®) - NCI [https://www.cancer.gov/types/neuroblastoma/hp/neuroblastoma-treatment-pdq]
- 123. RT-PCR demonstrates superior sensitivity and specificity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10772832/]