Multiplex RT-qPCR for Breast Cancer Subtyping: A Revolutionary Approach for Precision Diagnostics and Therapy
This article explores the transformative role of multiplex Reverse Transcription quantitative PCR (RT-qPCR) in advancing breast cancer molecular subtyping.
Multiplex RT-qPCR for Breast Cancer Subtyping: A Revolutionary Approach for Precision Diagnostics and Therapy
Abstract
This article explores the transformative role of multiplex Reverse Transcription quantitative PCR (RT-qPCR) in advancing breast cancer molecular subtyping. It details the methodology for simultaneously profiling key biomarkers (ESR, PGR, HER2, Ki67) and emerging angiogenic factors, offering a rapid, cost-effective alternative to traditional immunohistochemistry. The content covers foundational principles, detailed protocols, optimization strategies, and rigorous validation against established standards. Furthermore, it examines the technology's expanding applications in monitoring treatment resistance via circulating tumor cells and liquid biopsy, positioning multiplex RT-qPCR as an indispensable tool for researchers and drug developers driving personalized oncology forward.
The Critical Need for Advanced Molecular Subtyping in Breast Cancer
Current Limitations of Traditional Immunohistochemistry (IHC) in Breast Cancer Diagnosis
Immunohistochemistry (IHC) serves as the cornerstone technique for breast cancer diagnosis and subtyping, providing critical information for treatment decisions by assessing the expression of estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and the proliferation marker Ki-67 [1]. This methodology enables classification of breast cancer into molecular subtypes that guide therapeutic strategies, particularly for targeted therapies and endocrine treatments [2]. Despite its widespread adoption in clinical pathology laboratories globally, traditional IHC faces significant limitations that impact diagnostic accuracy, reproducibility, and ultimately patient care. The emergence of new therapeutic paradigms, especially for HER2-low breast cancers, has further exposed critical vulnerabilities in conventional IHC approaches [3] [4]. This application note examines the documented limitations of traditional IHC and positions multiplex Reverse Transcription quantitative Polymerase Chain Reaction (RT-qPCR) as a complementary methodology that addresses these challenges within breast cancer research and drug development programs.
Documented Limitations of Traditional IHC
Recent research has identified several critical limitations in traditional IHC that affect its reliability for breast cancer biomarker assessment. The table below summarizes these key challenges with corresponding evidence from recent studies.
Table 1: Key Limitations of Traditional IHC in Breast Cancer Diagnosis
| Limitation Category | Specific Challenge | Impact on Diagnosis/Research | Supporting Evidence |
|---|---|---|---|
| Subjectivity & Reproducibility | High inter-observer variability in HER2 scoring [5] | Inconsistent scoring affects treatment eligibility | AI analysis reveals significant discordance among pathologists |
| Technical Limitations | Inability to reliably distinguish HER2-low expression (IHC 0 vs 1+) [3] | Impacts eligibility for novel ADC therapies (T-DXd) | Clinical trials demonstrate misclassification affects treatment access |
| Semi-Quantitative Nature | Limited dynamic range for biomarker quantification [6] [7] | Reduced precision in biomarker measurement | RT-qPCR shows continuous expression data vs. categorical IHC scores |
| Tumor Heterogeneity | Limited tissue representation in core biopsies [1] | Incomplete biomarker profiling | Focal expression patterns may be missed in small samples |
| Workflow Efficiency | Time-consuming process requiring skilled pathologists [6] [2] | Delays in diagnosis and treatment initiation | Multiplex RT-qPCR offers faster turnaround times |
| Biomarker Complexity | Single-parameter assessment limits multidimensional profiling [6] | Inability to concurrently assess multiple biomarkers | Angiogenesis markers cannot be easily integrated with standard markers |
HER2-Low Classification Challenges
The recent paradigm shift in HER2-targeted therapy has exposed a critical limitation in traditional IHC. With the DESTINY-Breast04 trial demonstrating significant survival benefits of trastuzumab deruxtecan (T-DXd) in metastatic breast cancer patients with low HER2 expression (defined as IHC 1+ or 2+/ISH-negative), accurate differentiation between HER2-negative (IHC 0) and HER2-low (IHC 1+) has become clinically essential [3] [4]. Traditional IHC struggles with this distinction due to several factors:
- Subtle staining differences between IHC 0 and 1+ are difficult to standardize across laboratories [4]
- Inter-observer variability is particularly pronounced in the lower expression ranges [5]
- Lack of standardized protocols specifically optimized for HER2-low detection [3]
This classification challenge has significant therapeutic implications, as HER2-low breast cancer accounts for approximately 50% of all breast cancer cases, making accurate identification crucial for patient access to novel antibody-drug conjugates (ADCs) [8].
Concordance Issues with Molecular Methods
Studies directly comparing IHC with molecular methods such as RT-qPCR have demonstrated discordance in biomarker assessment, particularly for borderline cases:
Table 2: Concordance Rates Between IHC and RT-qPCR for Breast Cancer Biomarkers
| Biomarker | Concordance Rate (Training Set) | Concordance Rate (Validation Set) | Recommended Cut-off Value (mRNA) |
|---|---|---|---|
| ER | 94.4% | 81.3% | 0.764 |
| PR | 88.0% | 78.3% | 0.709 |
| HER2 | 89.4% | 80.4% | 0.161 |
| Ki-67 | 67.8% | 69.1% | 0.554 |
A study of 323 breast cancer patients revealed high concordance rates for ER, PR, and HER2 between IHC and RT-qPCR, while Ki-67 showed only moderate concordance, highlighting the particular challenges in reproducibly assessing proliferation markers with IHC [7]. The 5-year recurrence-free interval rates based on subtyping by RT-qPCR were similar to those assessed by IHC (88% vs. 88% for luminal, 82% vs. 78% for HER2-enriched, and 58% vs. 47% for triple-negative, respectively), demonstrating comparable prognostic capability [7].
Multiplex RT-qPCR as a Complementary Approach
Multiplex RT-qPCR methodology addresses several key limitations of traditional IHC through its quantitative nature, higher throughput capacity, and reduced subjectivity. This approach enables simultaneous assessment of multiple biomarkers from minimal RNA samples, providing researchers with a complementary tool for breast cancer subtyping.
Workflow Comparison: Traditional IHC vs. Multiplex RT-qPCR
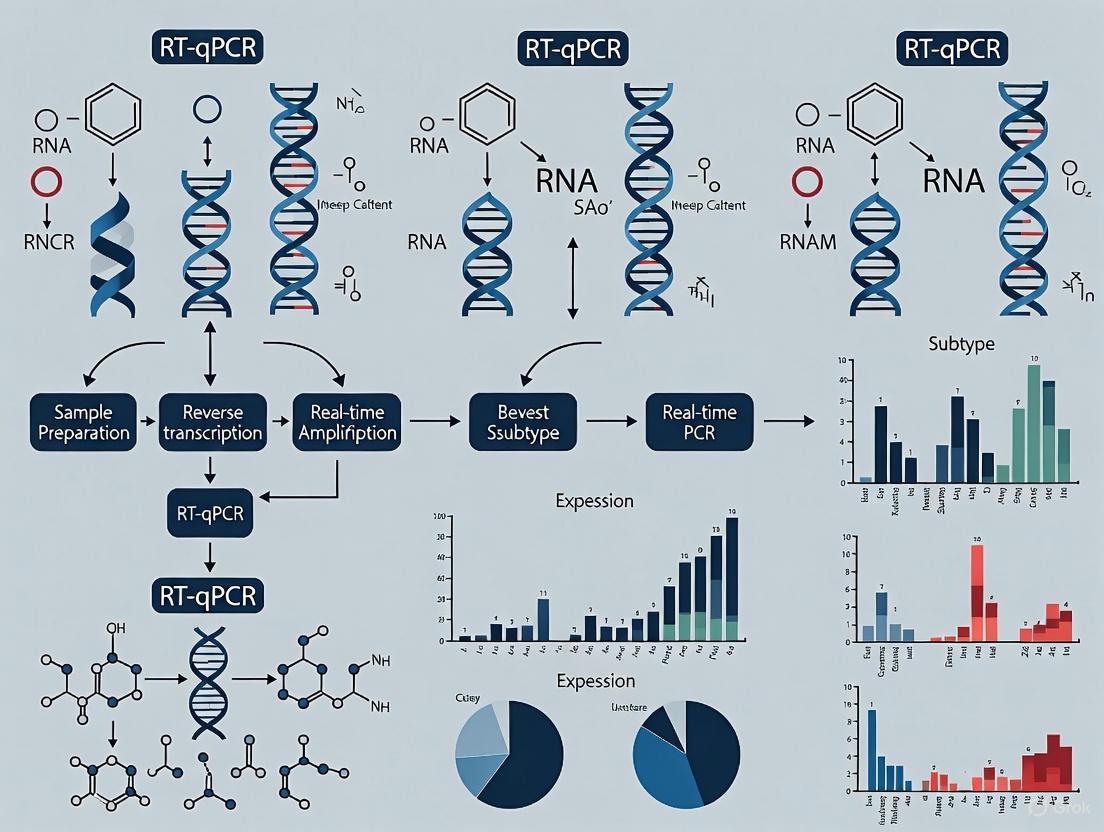
The following diagram illustrates the key procedural differences between traditional IHC and multiplex RT-qPCR workflows, highlighting steps where variability is introduced in IHC and standardization is achieved in RT-qPCR:
Advanced Multiplex RT-qPCR Protocol for Breast Cancer Subtyping
This protocol describes a standardized methodology for simultaneous detection of ESR1, PGR, ERBB2 (HER2), and MKI67 (Ki-67) gene expression using multiplex RT-qPCR, optimized for formalin-fixed paraffin-embedded (FFPE) breast cancer tissue samples.
RNA Extraction and Quality Control
- Input Material: 2-4 sections of FFPE tissue (5-10μm thickness) with >⅔ tumor content
- Extraction Method: Utilize commercial FFPE RNA extraction kits (e.g., Quick-DNA/RNA FFPE Kit)
- Quality Assessment: Measure RNA concentration and purity using spectrophotometry (A260/A280 ratio >1.8)
- Storage: Preserve extracted RNA at -80°C until cDNA synthesis
Reverse Transcription and Pre-Amplification
- Reaction Setup: Use 100-500ng total RNA in 20μL reaction volume
- Reverse Transcriptase: Employ MuLV reverse transcriptase or equivalent
- Conditions: 50°C for 10 minutes (cDNA synthesis), 95°C for 2 minutes (enzyme inactivation)
- Optional Pre-amplification: 10-14 cycles of target-specific pre-amplification for limited samples
Multiplex RT-qPCR Setup
Reaction Composition:
- 2X SYBR Master Mix or equivalent probe-based master mix
- cDNA template (diluted 1:10-1:20)
- Multiplex primer/probe mixtures (ESR1, PGR, ERBB2, MKI67, reference genes)
- Nuclease-free water to final volume
Primer/Probe Design:
- Final concentration: 100-400nM each primer, 50-200nM each probe
- TagMan or similar dual-labeled probes recommended
- Validate amplification efficiency (90-110%) for each target
Reference Genes: Include at least two stable reference genes (RPL13A, ACTB, GAPDH, or TFRC) [6] [7]
Touch-Down Thermal Cycling Protocol
Table 3: Thermal Cycling Conditions for Multiplex RT-qPCR
| Stage | Cycles | Temperature | Time | Purpose |
|---|---|---|---|---|
| Initial Denaturation | 1 | 95°C | 2 min | Template denaturation |
| Touch-Down Phase | 3 | 95°C | 10 s | Annealing optimization |
| 3 | 70°C | 15 s | ||
| Touch-Down Phase | 3 | 95°C | 10 s | Annealing optimization |
| 3 | 67°C | 15 s | ||
| Touch-Down Phase | 3 | 95°C | 10 s | Annealing optimization |
| 3 | 63°C | 15 s | ||
| Amplification | 40 | 95°C | 5 s | DNA denaturation |
| 40 | 60°C | 30 s | Annealing/extension with data collection |
The touch-down approach consistently yields significantly lower Cycle Threshold (CT) values, improving assay sensitivity and reproducibility [6] [9].
Data Analysis and Normalization
- CT Determination: Use consistent threshold settings across all runs
- Reference Normalization: Calculate ΔCT = CT(target) - CT(reference mean)
- Quantile Normalization: Apply for cross-sample comparison when using multiple batches
- Threshold Determination: Establish biomarker-specific cutoffs using ROC curve analysis against IHC results [7]
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Breast Cancer Biomarker Analysis
| Reagent Category | Specific Product/Assay | Research Application | Key Considerations |
|---|---|---|---|
| RNA Extraction | Quick-DNA/RNA FFPE Kit (ZYMO RESEARCH) | High-quality RNA from archived FFPE samples | Optimized for fragmented RNA from fixed tissues |
| cDNA Synthesis | RT² First Strand Kit (Qiagen) | Efficient reverse transcription of FFPE-derived RNA | Includes genomic DNA elimination step |
| qPCR Master Mix | 2X SYBR Master Mix or TagMan Universal PCR Master Mix | Sensitive detection of multiple targets | Low CT values and high amplification efficiency |
| Reference Genes | RPL13A, ACTB, GAPDH, TFRC | Data normalization across samples | Validation of stability in breast tissue required |
| Primer/Probe Sets | Custom-designed ESR1, PGR, ERBB2, MKI67 | Target-specific amplification | Validate specificity and efficiency (90-110%) |
| Automated Systems | PanelChip Analysis System (Quark BioSciences) | High-throughput qPCR analysis | Enables parallel processing of multiple samples |
Traditional IHC remains an essential tool in breast cancer diagnosis but demonstrates significant limitations in reproducibility, quantification, and precise classification, particularly with the emergence of therapeutically relevant HER2-low categories. Multiplex RT-qPCR methodology provides researchers with a complementary approach that offers quantitative data, reduced subjectivity, and ability to concurrently assess multiple biomarkers including those related to angiogenesis and metastatic potential [6]. The integration of both methodologies in research settings provides a more comprehensive understanding of breast cancer biology, ultimately supporting enhanced drug development and personalized treatment strategies. As breast cancer classification evolves to incorporate more continuous biomarker data, molecular methods like multiplex RT-qPCR will play an increasingly important role in research and clinical trial contexts.
Core Principles of Multiplex RT-qPCR for Gene Expression Analysis
Multiplex RT-qPCR is an advanced molecular technique that enables the simultaneous amplification and quantification of multiple gene targets in a single reaction tube using a shared reagent mix [10]. This method is particularly valuable in breast cancer research, where precious patient-derived samples are often limited. By allowing researchers to measure several biomarkers at once—such as the key genes used for subtyping (ESR, PGR, HER2, Ki67)—it conserves sample material while providing comprehensive data from a single, streamlined workflow [11] [9].
The core principle hinges on the use of distinct fluorescent reporter dyes for each target gene. During the PCR amplification process, these dyes emit light at different wavelengths, which are detected in real-time by the PCR instrument. This allows for the independent tracking and quantification of each target as it amplifies [10]. The simplest form, duplexing, involves one gene of interest and one endogenous control gene. With careful optimization, assays can be expanded to simultaneously detect three or four targets, offering even greater efficiency [10].
Key Advantages and Considerations
Core Benefits for Research
Multiplex RT-qPCR confers several significant advantages over singleplex approaches (amplifying one gene per reaction), especially in a complex field like breast cancer subtyping.
- Sample and Cost Efficiency: It dramatically reduces the amount of valuable sample required, a critical factor when working with scarce tumor biopsies [10]. Furthermore, by testing multiple genes in one well, it saves on reagents and reduces the time needed for experiment setup and data analysis [10] [12].
- Improved Precision: Amplifying all targets for a given sample in the same well minimizes pipetting errors and well-to-well variations in reagent and sample volumes. This enhances the precision of comparative gene expression analysis, such as calculating the fold-change between a target gene and a reference gene [10].
- Streamlined Workflow for Complex Profiling: The ability to run multi-parameter assays from a single sample is indispensable for molecular profiling. For instance, a study on breast cancer utilized multiplex RT-qPCR to analyze the expression of HER2, PGR, ESR, and Ki67 genes for precise subtyping, alongside angiogenesis-related genes (Hif1A, ANG, VEGFR) to profile metastatic potential, all from a 61-sample cohort [11] [9].
Technical Challenges and Solutions
Despite its advantages, multiplexing introduces complexity that requires careful management.
- Competition for Reagents: All assays in a single tube compete for the same pool of nucleotides, polymerase, and ions. This can lead to biased amplification, especially if one target is vastly more abundant than others [10].
- Primer/Probe Interactions: The presence of multiple primers and probes increases the probability of primer-dimer formation or other unintended interactions that can reduce assay efficiency and accuracy [10].
- Spectral Overlap: The fluorescent dyes used must have distinct emission spectra that the instrument can cleanly distinguish. Fluorescence spillover between channels must be measured and compensated for, a process facilitated by modern analysis software [12].
A key strategy to mitigate competition is primer limitation. For a highly abundant gene (often the endogenous control), primer concentrations are significantly reduced (e.g., from 900nM to 150nM). This causes the reaction for that target to plateau early due to primer exhaustion, leaving ample reagents for the efficient amplification of less abundant targets [10].
Experimental Protocol for Multiplex RT-qPCR
The following section outlines a detailed workflow for developing and running a multiplex RT-qPCR assay, with specific examples from breast cancer research.
Assay Design and Optimization
- Gene Selection: Identify the gene panel. For breast cancer subtyping, this typically includes ESR1 (ER), PGR (PR), ERBB2 (HER2), and MKi67 (Ki67), with a stable endogenous control like RPL13A [11] [9].
- In Silico Design:
- Primers and Probes: Design primers to be specific and to produce amplicons between 70-200 base pairs. The melting temperature (Tm) of TaqMan probes should be approximately 10°C higher than that of the primers [10] [13].
- Specificity and Dimers: Use tools like UCSC Genome Browser In Silico PCR and Multiple Primer Analyzer to ensure amplicons do not overlap and to check for potential primer-dimer formations [10].
- Dye Selection and Assignment: Choose fluorescent dyes with minimal spectral overlap. Assign the brightest dye (e.g., FAM) to the lowest abundance target and a dimmer dye (e.g., JUN) to a high-abundance internal control. For 3- or 4-plex assays, combine dyes like FAM and VIC (with MGB-NFQ quenchers) with ABY and JUN (with QSY quenchers) [10].
- Singleplex Validation: Before multiplexing, optimize each primer-probe set individually in a singleplex reaction. Determine the optimal annealing/extension temperature and confirm a single, specific amplification product [10] [12].
- Multiplex Optimization: Combine all assays into a single reaction. Use a master mix specifically formulated for multiplex PCR. Fine-tune the reaction by:
- Adjusting primer and probe concentrations (typically starting at 0.125-0.25 µM) [12].
- Using touch-down PCR methods to improve annealing specificity among different primers and probes [11] [9].
- Potentially increasing the number of PCR cycles (e.g., to 45 or more) to improve the separation between positive and negative populations [12].
The Research Reagent Toolkit
Table 1: Essential Reagents for Multiplex RT-qPCR Workflow
| Reagent Category | Specific Examples | Function in the Assay |
|---|---|---|
| Reverse Transcription Enzymes | Reverse transcriptase (e.g., from Moloney murine leukemia virus) | Converts purified RNA or RNA in a crude lysate into complementary DNA (cDNA) [13] [14] |
| PCR Polymerase | Hot-start Taq DNA polymerase | Amplifies the cDNA template with high specificity and efficiency; resistant to inhibitors in complex mixes [10] [13] |
| Fluorescent Reporters | TaqMan hydrolysis probes (FAM, VIC, ABY, JUN-labeled), SYBR Green dye | Generates a fluorescent signal proportional to the amount of amplified target DNA [10] [13] |
| Specialized Master Mixes | TaqMan Multiplex Master Mix, TaqPath ProAmp Master Mix | Provides an optimized buffer system, dNTPs, and salts for efficient co-amplification of multiple targets [10] |
| Sample Preparation Kits | Cells-to-CT Kit, RealTime Ready Cell Lysis Kit | Enables fast, high-throughput cDNA synthesis directly from cell cultures, bypassing RNA purification [14] |
Workflow Visualization
The following diagram illustrates the complete workflow from sample to data in a multiplex RT-qPCR experiment for breast cancer subtyping.
Multiplex RT-qPCR Workflow for Breast Cancer
Data Analysis and Interpretation
Key Data Analysis Parameters
Table 2: Key Quantitative Parameters in Multiplex RT-qPCR Data Analysis
| Parameter | Definition | Interpretation in Gene Expression |
|---|---|---|
| Cycle Threshold (Ct) | The PCR cycle number at which the fluorescence signal crosses a defined threshold above the baseline [15]. | A lower Ct value indicates a higher starting quantity of the target transcript. Values are typically between 15-35 cycles. |
| Amplification Efficiency (E) | The rate of product doubling per cycle, ideally ranging from 90% (1.8) to 110% (2.1) [16] [15]. | Efficiency outside this range suggests suboptimal reactions, leading to inaccurate fold-change calculations. |
| Relative Quantification (RQ) | The fold-change in expression of a target gene in a test sample relative to a control, normalized to one or more reference genes [16] [13]. | An RQ of 2.0 means the gene is twice as expressed in the test condition compared to the control. |
Calculation of Relative Expression
For relative quantification, the ∆∆Ct (Livak) method is commonly used if the amplification efficiencies of the target and reference genes are approximately equal and near 100% [16] [15].
Formula: FC = 2^(-∆∆Ct)
Where:
- ∆Ct = Ct(target gene) - Ct(reference gene) for each sample.
- ∆∆Ct = ∆Ct(test group) - ∆Ct(control group).
When amplification efficiencies are not ideal or differ between targets, the more robust Pfaffl method is recommended, as it incorporates actual efficiency values (E) into the calculation [16].
Formula: FC = (Etarget)^(-∆Cttarget) / (Eref)^(-∆Ctref)
Statistical analysis and visualization of results, including the calculation of standard errors and confidence intervals, can be efficiently handled by specialized software packages, such as the rtpcr package for R [16].
Validation in Breast Cancer Research
The application of multiplex RT-qPCR in breast cancer diagnostics has been rigorously validated. One study demonstrated that this method offers remarkable precision, nearly equivalent to Immunohistochemistry (IHC), the traditional standard, in detecting the expression of ESR, PGR, HER2, and Ki67 genes across 61 patient samples [11] [9]. Furthermore, the method's utility extends beyond simple subtyping, allowing for the parallel profiling of angiogenesis-related genes (Hif1A, ANG, VEGFR), providing insights into the metastatic potential of tumors [9]. This underscores the power of multiplex RT-qPCR as a comprehensive and efficient tool for both diagnostic and research applications in oncology.
The clinical management of breast cancer relies heavily on the molecular subtyping of tumors to predict patient prognosis and guide therapeutic decisions. The core biomarkers for this classification are the estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and the proliferation marker Ki67. In routine clinical practice, the expression of these proteins is most commonly assessed by immunohistochemistry (IHC) [17] [6]. However, IHC is subject to pre-analytical and analytical variability, as well as inter-observer interpretation differences, particularly for Ki67 [17] [18]. The quantification of the mRNA transcripts encoding these proteins—ESR1 (encoding ER), PGR (encoding PR), ERBB2 (encoding HER2), and MKI67 (encoding Ki67)—via reverse transcription quantitative polymerase chain reaction (RT-qPCR) presents a robust, quantitative, and standardized alternative for biomarker analysis [17] [6] [18]. When performed in a multiplex format, RT-qPCR enables the rapid and precise subtyping of breast cancers from a single RNA sample, forming a powerful foundation for personalized treatment strategies [6].
Essential Biomarker Profiles and Their Clinical Implications
The four canonical biomarkers define the primary intrinsic subtypes of breast cancer, each with distinct biological characteristics and clinical outcomes. Their profiles, as determined by gene expression, are summarized in the table below.
Table 1: Breast Cancer Intrinsic Subtypes Defined by Core Biomarkers
| Subtype | ESR1 / ER | PGR / PR | ERBB2 / HER2 | MKI67 / Ki67 | Clinical & Biological Characteristics |
|---|---|---|---|---|---|
| Luminal A | High | High (94%) [19] | Negative | Low (11% high) [19] | Less aggressive, best prognosis, highly endocrine-sensitive. |
| Luminal B | High | Lower (74%) [19] | Negative or Positive | High (77% high) [19] | More aggressive than Luminal A, poorer prognosis, less endocrine-sensitive. |
| HER2-Enriched | Negative | Negative | High | Variable | Aggressive tumor growth, targeted by HER2-therapies (e.g., Trastuzumab). |
| Basal-like | Negative | Negative | Negative | High | Highly aggressive, often overlaps with triple-negative breast cancer (TNBC). |
The PAM50 gene expression assay, which includes these core biomarkers, has demonstrated that the standard IHC panel does not perfectly align with the intrinsic molecular subtypes [19]. For instance, while the majority of estrogen receptor-positive (ER+) tumors by IHC are classified as Luminal (A or B) by PAM50, a significant portion of ER-negative (ER-) tumors are not classified as Basal-like or HER2-Enriched [19]. This highlights the added discriminatory power of quantitative gene expression analysis.
Experimental Workflow for Multiplex RT-qPCR Subtyping
The process of breast cancer subtyping using multiplex RT-qPCR involves a series of standardized steps from sample acquisition to data analysis. The workflow is designed to ensure reproducibility and accuracy.
The Scientist's Toolkit: Research Reagent Solutions
The successful implementation of a multiplex RT-qPCR assay for breast cancer subtyping depends on a set of well-validated reagents and tools. The following table details the essential components.
Table 2: Essential Research Reagents and Materials for Multiplex RT-qPCR Subtyping
| Item | Function / Role | Examples & Specifications |
|---|---|---|
| FFPE Tumor RNA | Source of template for gene expression analysis. | Quick-DNA/RNATM FFPE Kit (Zymo Research) [6]. Must have >30% tumor content; macro-dissection may be required [17]. |
| Reverse Transcriptase | Synthesizes complementary DNA (cDNA) from RNA template. | M-MLV RT (e.g., from Thermo Fisher Scientific) [6]. |
| qPCR Master Mix | Provides optimized buffer, enzymes, and dNTPs for amplification. | TaqMan Fast Advanced Master Mix (Thermo Fisher Scientific) [6]. |
| Gene-Specific Assays | Primers and probes for specific detection of target mRNAs. | TaqMan Assays: Pre-designed for ESR1, PGR, ERBB2, MKi67, and reference genes (e.g., CYFIP1, RPL13A) [17] [6]. |
| qPCR Instrument | Automated platform for thermal cycling and fluorescence detection. | GeneXpert System: Fully integrated, cartridge-based system (e.g., for STRAT4 assay) [17]. MIC PCR Machine or QuantStudio systems for plate-based formats [6]. |
| Reference Genes | Endogenous controls for normalization of RNA input and quality. | CYFIP1: Used in the Xpert Breast Cancer STRAT4 Assay [17]. RPL13A or GAPDH: Used in other multiplex protocols [6]. |
Quantitative Validation and Concordance with IHC
The clinical validity of mRNA-based biomarker testing is established through concordance studies with the current gold standard, IHC. The following table summarizes key performance metrics from recent studies.
Table 3: Concordance Between mRNA Expression (RT-qPCR) and Protein Expression (IHC)
| Biomarker (Gene/Protein) | Overall Concordance | Positive Percent Agreement (Sensitivity) | Negative Percent Agreement (Specificity) | Notes |
|---|---|---|---|---|
| ESR1 / ER | 93.7% [17] - 95.9% [18] | High | High | Demonstrates excellent agreement, supporting its use for confirming ER status. |
| PGR / PR | 79.3% [18] - 80.5% [17] | Moderate | Moderate | Agreement is moderate, potentially due to post-transcriptional regulation. |
| ERBB2 / HER2 | 94.1% (IHC 3+ vs 0/1+) [17], 100% [18] | High | High | mRNA testing shows very high agreement with IHC/FISH for clear positive and negative cases. |
| MKI67 / Ki67 | Good correlation [18] | N/A | N/A | Shows a moderate to good correlation with IHC, but a direct percent agreement is less commonly reported due to its continuous nature. |
These studies conclude that mRNA measurements have good to excellent agreement with centrally assessed IHC for ER and HER2, and moderate agreement for PR and Ki67 [17] [18]. Furthermore, the prognostic value of these biomarkers, as assessed by their association with outcomes like residual cancer burden and overall survival, is similar whether measured by RT-qPCR or central IHC [17].
Detailed Experimental Protocol
Sample Preparation and RNA Extraction
- Tissue Sectioning: Cut one 10μm section from a formalin-fixed, paraffin-embedded (FFPE) tumor block [17].
- Tumor Enrichment: Visually inspect a corresponding H&E slide. If the tumor content is less than 30%, perform macro-dissection to scrape tumor cells from the slide [17].
- RNA Extraction: Extract total RNA using a dedicated FFPE RNA extraction kit, such as the Quick-DNA/RNATM FFPE Kit, following the manufacturer's instructions [6].
- Quality Control: Quantify RNA concentration and assess purity using a spectrophotometer (e.g., NanoDrop). Store purified RNA at -80°C.
cDNA Synthesis and Multiplex RT-qPCR Setup
- Reverse Transcription: Synthesize cDNA from 400 ng of total RNA using random primers, dNTPs, DTT, and M-MLV Reverse Transcriptase in a 40 μl reaction volume [6].
- Assay Configuration: Prepare multiplex reactions as follows [6]:
- Tube 1: RPL13A (reference gene), ESR1, PGR, ERBB2.
- Tube 2: RPL13A (reference gene), MKi67.
- PCR Reaction: For each reaction, mix 1 μl of diluted cDNA, TaqMan Fast Advanced Master Mix, and the respective primer/probe sets. Perform reactions in a 10 μl total volume [6].
- Touch-Down Thermocycling: Use a touch-down protocol to improve annealing specificity and yield lower Ct values [6]. An example protocol is:
- cDNA Formation: 50°C for 10 minutes.
- Initial Denaturation: 95°C for 2 minutes.
- Pre-Cycles (3 cycles each): 95°C for 10s, 70°C for 15s; then 95°C for 10s, 67°C for 15s; then 95°C for 10s, 63°C for 15s.
- Cycling (40 cycles): 95°C for 5s, 60°C for 30s (with data collection).
Data Analysis and Interpretation
- Data Normalization: Calculate the ΔCt for each target gene using the formula: ΔCt = Ct (target gene) - Ct (reference gene) [17] [6].
- Thresholds for Positivity: Classify samples as positive or negative for each biomarker using predefined ΔCt thresholds. For the STRAT4 assay, these are [17]:
- ESR1 Positive: ΔCt ≥ -1.0
- PGR Positive: ΔCt ≥ -3.5
- ERBB2 Positive: ΔCt ≥ -1.0
- MKi67 High: ΔCt ≥ -4.0
- Subtype Assignment: Combine the results for all four biomarkers and assign the intrinsic subtype based on the profiles detailed in Table 1.
- Statistical Analysis: For research involving group comparisons, use established statistical methods for qPCR data. The
rtpcrpackage in R is a comprehensive tool that can perform t-tests, ANOVA, or ANCOVA on efficiency-weighted ΔCt values to calculate fold changes and statistical significance [16]. The Pfaffl method is recommended when amplification efficiencies of the target and reference genes are not equal to 2 [16] [20].
Within the context of breast cancer research, understanding the molecular drivers of angiogenesis and metastasis is critical for developing targeted therapeutic strategies. The hypoxia-inducible factor 1-alpha (HIF-1α), along with the angiogenic factors Angiogenin (ANG) and Vascular Endothelial Growth Factor (VEGF/VEGFR), form a crucial signaling axis that promotes tumor progression by stimulating new blood vessel formation and facilitating metastatic spread [6] [21]. In the tumor microenvironment, rapid cancer cell proliferation often outstrips the oxygen supply, creating hypoxic regions that trigger the stabilization and activation of HIF-1α [21]. This transcription factor then binds to hypoxia response elements (HREs) in the promoter regions of numerous target genes, including VEGF and ANG, initiating a transcriptional program that enables tumor cells to adapt to hypoxic stress and acquire aggressive characteristics [21] [22].
The integration of multiplex RT-qPCR into breast cancer subtyping research provides a powerful methodological framework for simultaneously quantifying the expression of these pro-angiogenic factors alongside established breast cancer biomarkers [6]. This approach offers significant advantages for comprehensive tumor characterization, allowing researchers to not only classify breast cancer subtypes but also assess their metastatic potential through evaluation of the HIF-1α/ANG/VEGF signaling axis. This application note details experimental protocols and analytical approaches for investigating this pathway within the broader context of multiplex RT-qPCR-based breast cancer research, providing researchers with standardized methods to advance our understanding of angiogenesis and metastasis in breast cancer.
Key Angiogenesis Players in Breast Cancer
The HIF1A/ANG/VEGFR pathway represents a coordinated molecular response to tumor hypoxia that drives multiple facets of cancer progression. Below is a detailed overview of these key mediators:
Hypoxia-Inducible Factor 1-Alpha (HIF-1α)
HIF-1α serves as the master regulator of cellular response to hypoxia. Under normoxic conditions, HIF-1α undergoes rapid degradation mediated by prolyl hydroxylases (PHDs) and the von Hippel-Lindau tumor suppressor protein (pVHL), which targets it for proteasomal degradation [21]. In hypoxic conditions, this degradation is halted, allowing HIF-1α to accumulate, dimerize with HIF-1β, and translocate to the nucleus where it activates the transcription of over 40 genes involved in adaptation to low oxygen [21]. In breast cancer, HIF-1α overexpression is associated with poor prognosis, therapeutic resistance, and aggressive tumor behavior [21]. Research has consistently demonstrated that HIF-1α is overexpressed in numerous types of cancer, significantly influencing cancer progression by activating genes associated with angiogenesis, cell growth and survival, invasion and metastasis, glucose metabolism, and immune system evasion [21].
Angiogenin (ANG)
Angiogenin, a member of the RNase A superfamily, is a potent inducer of blood vessel formation. Unlike other angiogenic factors, ANG uniquely promotes angiogenesis through its ribonucleolytic activity, enabling it to cleave tRNA and create stress-induced translational reprogramming that favors pro-angiogenic protein synthesis [6]. Within the tumor microenvironment, ANG expression is upregulated in response to HIF-1α activation and contributes to the formation of new blood vessels that supply nutrients and oxygen to growing tumors, while also facilitating cancer cell invasion and metastatic spread.
Vascular Endothelial Growth Factor and Receptor (VEGF/VEGFR)
The VEGF/VEGFR system represents one of the most potent and well-characterized pathways driving tumor angiogenesis. VEGF-A (commonly referred to as VEGF) is a key downstream target of HIF-1α transcriptional activation [22]. Upon binding to its receptors (primarily VEGFR-2) on endothelial cells, VEGF triggers a signaling cascade that promotes endothelial cell proliferation, migration, and survival, ultimately leading to the formation of new, often dysfunctional, tumor vasculature [6] [22]. This neovasculature not only supports tumor growth but also provides conduits for metastatic dissemination. Studies have shown significantly higher VEGF expression in breast tumor tissues compared to normal tissues, with particularly elevated levels in triple-negative breast cancer (TNBC) subgroups [22].
Table 1: Key Molecular Mediators of Angiogenesis and Metastasis in Breast Cancer
| Molecular Mediator | Full Name | Primary Function | Regulation by Hypoxia | Clinical Significance in Breast Cancer |
|---|---|---|---|---|
| HIF-1α | Hypoxia-Inducible Factor 1-Alpha | Master transcriptional regulator of hypoxia response; activates >40 genes promoting adaptation to low oxygen | Directly stabilized under hypoxic conditions; degraded under normoxia | Associated with poor prognosis, therapeutic resistance, and aggressive tumor behavior [21] |
| ANG | Angiogenin | Potent inducer of blood vessel formation; ribonucleolytic activity promotes stress-induced translation | Upregulated via HIF-1α transcriptional activation | Contributes to tumor angiogenesis and metastatic potential; potential biomarker for assessing metastatic status [6] |
| VEGF | Vascular Endothelial Growth Factor | Key mitogen for endothelial cells; promotes vasculature permeability and angiogenesis | Direct transcriptional target of HIF-1α [22] | Elevated in breast tumors, particularly TNBC; correlates with advanced disease and poorer outcomes [22] |
| VEGFR | Vascular Endothelial Growth Factor Receptor | Tyrosine kinase receptor that mediates VEGF signaling; primarily on endothelial cells | Indirectly regulated through increased VEGF availability | Primary therapeutic target for anti-angiogenic therapies; expression correlates with angiogenic activity |
Multiplex RT-qPCR Workflow for Angiogenesis Marker Detection
The simultaneous detection of HIF1A, ANG, VEGFR, and standard breast cancer markers via multiplex RT-qPCR requires careful experimental design and optimization. The following workflow outlines a comprehensive approach for assessing both breast cancer subtypes and their angiogenic potential:
Sample Preparation and RNA Extraction
- Sample Collection: Obtain Formalin-Fixed Paraffin-Embedded (FFPE) breast tumor tissue blocks or fresh frozen tissues, with preference for samples containing >⅔ tumor tissue [6]. Proper ethical approval and informed consent are mandatory prerequisites [22].
- RNA Extraction: Extract total RNA using specialized FFPE RNA extraction kits (e.g., Quick-DNA/RNA FFPE Kit, ZYMO RESEARCH) [6]. For fresh tissues, TRIzol-based methods can be employed [22].
- Quality Assessment: Evaluate RNA concentration and purity using spectrophotometry (e.g., NanoDrop One). Acceptable 260/280 ratios typically range from 1.8-2.1 [6].
- cDNA Synthesis: Reverse transcribe 1-2 μg of total RNA using reverse transcriptase kits (e.g., Revert Aid First Strand cDNA Synthesis Kit) in a 25 μL reaction volume [22].
Multiplex RT-qPCR Experimental Design
The multiplex approach should strategically group targets to minimize spectral overlap while maintaining amplification efficiency:
- Reaction Tube 1: Breast cancer subtyping markers (ESR, PGR, HER2) with reference gene (RPL13A) [6]
- Reaction Tube 2: Proliferation marker (Ki67) with reference gene (RPL13A) [6]
- Reaction Tube 3: Angiogenesis markers (HIF1A, ANG, VEGFR) with reference gene (RPL13A) [6]
This three-tube approach enables comprehensive molecular profiling while maintaining reaction efficiency through limited multiplexing. The use of a consistent reference gene across all tubes facilitates normalized comparisons between samples.
Primer and Probe Design
- Specificity Validation: Design primers and probes using specialized software and validate specificity using Primer-BLAST against the human genome to ensure exclusive target amplification [23].
- Avoid Polymorphisms: Ensure primer binding sites are free of common single nucleotide polymorphisms that might compromise amplification efficiency [23].
- Efficiency Testing: Validate each primer pair individually before multiplexing, with optimal amplification efficiencies ranging from 90-110% [24].
Table 2: Recommended Multiplex RT-qPCR Configuration for Breast Cancer Subtyping and Angiogenesis Marker Detection
| Reaction Tube | Target Genes | Endogenous Control | Primer/Probe Chemistry | Amplification Efficiency Target | Key Applications |
|---|---|---|---|---|---|
| Tube 1 | ESR, PGR, HER2 | RPL13A | Dual-labeled hydrolysis probes (FAM, HEX, CY5) | 90-110% [24] | Intrinsic subtyping: Luminal A, Luminal B, HER2-enriched |
| Tube 2 | Ki67 | RPL13A | Dual-labeled hydrolysis probe (FAM) | 90-110% [24] | Assessment of tumor proliferation index |
| Tube 3 | HIF1A, ANG, VEGFR | RPL13A | Dual-labeled hydrolysis probes (FAM, HEX, CY5) | 90-110% [24] | Evaluation of angiogenic potential and metastatic capability |
| Additional Validation | GAPDH, β-actin | - | SYBR Green or hydrolysis probes | 90-110% [24] | Supplementary reference gene validation |
Touch-Down PCR Protocol Implementation
Implement a touch-down PCR protocol to enhance annealing specificity, particularly crucial in multiplex reactions with multiple primer sets:
- cDNA Formation: 50°C for 10 minutes
- Initial Denaturation: 95°C for 2 minutes
- Pre-Cycling Phase:
- 3 cycles: 95°C for 10 seconds, 70°C for 15 seconds
- 3 cycles: 95°C for 10 seconds, 67°C for 15 seconds
- 3 cycles: 95°C for 10 seconds, 63°C for 15 seconds
- Amplification Phase (40 cycles): 95°C for 5 seconds, 60°C for 30 seconds (with data collection) [6]
This progressive reduction in annealing temperature during pre-cycling enhances specific primer-template binding, significantly reducing non-specific amplification and primer-dimer formation in complex multiplex reactions [6].
Data Analysis and Interpretation
- Quantification Cycle (Cq) Determination: Set consistent threshold levels across samples during the exponential amplification phase [24].
- Reference Gene Normalization: Calculate ΔCq values by subtracting reference gene Cq from target gene Cq (ΔCq = Cqtarget - Cqreference) [6].
- Relative Quantification: Use the 2^(-ΔΔCq) method to calculate fold changes in gene expression between sample groups [6] [22].
- Mathematical Normalization to IHC Scales: For comparison with immunohistochemistry data, invert ΔCq values by subtracting from maximum PCR cycle number, then normalize to IHC scoring scales [6].
Research Reagent Solutions
The following table outlines essential research reagents and their applications in multiplex RT-qPCR studies of angiogenesis in breast cancer:
Table 3: Essential Research Reagents for Multiplex RT-qPCR Analysis of Angiogenesis Markers
| Reagent Category | Specific Products | Application Notes | Function in Experimental Workflow |
|---|---|---|---|
| RNA Extraction Kits | Quick-DNA/RNA FFPE Kit (Zymo Research); TRIzol reagent | FFPE-optimized kits crucial for archival samples; TRIzol suitable for fresh/frozen tissues [6] [22] | High-quality RNA isolation from challenging sample types; preserves RNA integrity for accurate quantification |
| Reverse Transcriptase Kits | Revert Aid First Strand cDNA Synthesis Kit (ThermoScientific) [22] | Efficient cDNA synthesis from even degraded RNA typical of FFPE samples | Generation of stable template for multiple PCR reactions from limited RNA samples |
| qPCR Master Mixes | Luna qPCR/RT-qPCR Kits (NEB); Probe-based one-step multiplex RT-PCR mixes | Optimized for multiplex applications; minimal dye background; compatible with touchdown protocols [6] [24] | Provides reaction components for efficient, specific amplification with consistent performance across targets |
| Primers/Probes | Custom-designed oligonucleotides (Sigma-Aldrich) [6] | HPLC-purified; specific against HIF1A, ANG, VEGFR, standard BC markers, and reference genes | Target-specific amplification with minimal cross-reactivity; dual-labeled probes enable multiplex detection |
| Reference Genes | RPL13A, GAPDH, β-actin [6] [22] | Validation of stability across sample sets is essential; RPL13A demonstrates reliable performance in BC [6] | Normalization of technical variations; enables accurate relative quantification between samples |
| Quality Control Assays | NanoDrop One (Thermo Fisher); Agarose gel electrophoresis; Digital droplet PCR systems | RNA quality assessment pre-RT; amplification verification; absolute quantification validation [6] | Ensures input material quality; verifies reaction specificity; validates rare target detection |
HIF-1α Signaling Pathway in Angiogenesis
The following diagram illustrates the central role of HIF-1α in coordinating the cellular response to hypoxia and activating pro-angiogenic factors such as VEGF and ANG in the breast cancer microenvironment:
HIF-1α Signaling Pathway in Breast Cancer Angiogenesis and Metastasis
This graphical representation illustrates the molecular cascade initiated by tumor hypoxia, culminating in the acquisition of aggressive cancer phenotypes. Under hypoxic conditions, HIF-1α stabilization leads to heterodimerization with HIF-1β, forming a transcriptionally active complex that binds to hypoxia response elements (HREs) in promoter regions of target genes [21]. This results in increased expression of pro-angiogenic factors (VEGF, ANG) and glycolytic enzymes, driving tumor angiogenesis, metabolic reprogramming, and ultimately metastatic progression [21] [22].
Quantitative Data on Angiogenesis Markers in Breast Cancer
Recent clinical studies have provided compelling evidence for the significance of angiogenesis-related markers across different molecular subtypes of breast cancer. The following table summarizes key quantitative findings from recent research:
Table 4: Expression Profiles of Angiogenesis Markers in Breast Cancer Subtypes
| Gene Marker | Expression in Tumor vs Normal | Subtype-Specific Expression Patterns | Statistical Significance (p-value) | Correlation with Clinical Parameters |
|---|---|---|---|---|
| HIF-1α | Significantly higher in tumor tissues [22] | Highest expression in Triple-Negative Breast Cancer (TNBC) [22] | p = 0.0010 (tumor vs normal) [22]p = 0.0111 (TNBC expression) [22] | Associated with therapeutic resistance and poor prognosis [21] |
| VEGF | Significantly elevated in tumor tissues [22] | Highest expression in TNBC subgroups [22] | p = 0.0119 (tumor vs normal) [22]p = 0.0078 (TNBC expression) [22] | Correlates with advanced disease and angiogenesis [6] [22] |
| ANG | Elevated in numerous breast cancer samples [6] | Expression patterns vary across subtypes; potential biomarker for metastatic status [6] | Specific p-values not provided; reported as statistically significant [6] | Indicates angiogenic potential and metastatic capability [6] |
| HK-I | Not specifically reported | Higher expression in ER/PR-positive, HER2-negative subtypes [22] | p = 0.0106 (ER/PR-positive expression) [22] | Associated with glycolytic metabolism and survival advantage [22] |
These quantitative findings underscore the clinical relevance of angiogenesis markers in breast cancer, with particular significance in aggressive subtypes like TNBC. The elevated expression of HIF-1α and VEGF in TNBC aligns with the characteristically hypoxic microenvironment and aggressive behavior of this subtype [22]. Furthermore, the association between HIF-1α overexpression and therapeutic resistance highlights the potential value of targeting this pathway to improve treatment outcomes [21].
The integration of angiogenesis marker detection (HIF1A, ANG, and VEGFR) within multiplex RT-qPCR workflows for breast cancer subtyping represents a significant advancement in comprehensive tumor characterization. This approach enables researchers to simultaneously classify molecular subtypes and assess metastatic potential, providing a more complete understanding of tumor biology. The experimental protocols outlined in this application note, particularly the optimized touch-down multiplex RT-qPCR method, offer a robust framework for generating high-quality, reproducible data on both standard breast cancer markers and key mediators of angiogenesis.
The consistent observation of elevated HIF-1α and VEGF expression in aggressive breast cancer subtypes, particularly TNBC, underscores the clinical relevance of this pathway and highlights potential therapeutic targets. As research in this field progresses, the simultaneous assessment of angiogenic markers alongside standard classification biomarkers will increasingly inform personalized treatment approaches and contribute to the development of novel therapeutic strategies targeting the hypoxic tumor microenvironment. The methodologies detailed herein provide researchers with essential tools to advance these critical investigations in breast cancer biology and treatment.
The Impact of Rapid, Objective Diagnosis on Personalized Treatment Strategies
The paradigm of breast cancer management is shifting from a one-size-fits-all approach to personalized treatment strategies, a change driven by advances in rapid, objective diagnostic technologies. Personalized medicine tailors healthcare interventions to individual patients by considering differences in their genes, environments, and lifestyles [25] [26]. In breast cancer, this approach is critically dependent on the accurate and timely identification of tumor subtypes and molecular characteristics. The convergence of artificial intelligence (AI) and precision medicine promises to revolutionize health care by identifying patient phenotypes with unique therapeutic responses and healthcare needs [27]. This application note details protocols for breast cancer subtyping, emphasizing the central role of rapid, objective diagnostics in enabling personalized treatment strategies.
The Critical Role of Rapid, Objective Diagnosis in Personalized Therapy
Defining Rapid, Objective Diagnosis
Rapid, objective diagnosis in breast cancer involves the use of advanced technologies to quickly and accurately characterize tumors with minimal inter-observer variability. These methods move beyond traditional histology to provide quantitative data on tumor biology, including genomic, transcriptomic, and proteomic profiles. Precision medicine aims to target the right treatments to the right patients at the right time [25], a goal achievable only through such diagnostic precision.
Impact on Treatment Decision-Making
The development of personalized drug therapy represents the essence of personalized medicine in pharmacy, potentially reducing adverse effects, enhancing drug efficacy, and optimizing treatment outcomes [28]. For breast cancer patients, rapid subtyping directly informs therapeutic selection:
- Hormone receptor-positive (HR+) patients receive endocrine therapy as first-line treatment [29]
- HER2-positive patients benefit from adjuvant trastuzumab-based therapy [29]
- Triple-negative breast cancer (TNBC) requires alternative therapies due to the absence of targetable receptors [29]
CDK4/6 inhibitors (palbociclib, ribociclib, abemaciclib) combined with endocrine therapy have become standard for HR+/HER2- breast cancer [29]. The ability to quickly identify the appropriate patient population for these targeted therapies fundamentally depends on accurate initial diagnostic subtyping.
Quantitative Comparison of Diagnostic Modalities
The following table summarizes the performance characteristics of various diagnostic modalities relevant to breast cancer personalized treatment strategies.
Table 1: Performance Characteristics of Diagnostic Technologies in Breast Cancer
| Diagnostic Technology | Application in Breast Cancer | Performance Metrics | Impact on Personalization |
|---|---|---|---|
| Strain Elastography [30] | Differentiation of benign vs. malignant breast masses | Sensitivity: 96.0%Specificity: 98.5%Cut-off SR value: 2.42 | Predicts prognosis through association with nuclear grade, lymph node status, ER, PR, and HER-2 status |
| AI-Based Mammography Interpretation [31] | Breast cancer detection from mammograms | Absolute reduction in false positives: 5.7%Absolute reduction in false negatives: 9.4% | Improves early detection, enabling earlier intervention |
| Liquid Biopsy (Guardant360 CDx) [29] | Detection of ESR1 mutations for targeted therapy | FDA-approved for BC-targeted therapy | Monitors treatment response and resistance without invasive procedures |
| Liquid Biopsy (FoundationOne Liquid CDx) [29] | Analysis of 324 genes from blood draw | FDA-approved for solid tumors | Comprehensive genomic profiling guides targeted therapy selection |
Advanced Diagnostic Protocols for Breast Cancer Subtyping
Multiplex RT-qPCR for Breast Cancer Molecular Subtyping
Principle and Significance
Multiplex RT-qPCR enables simultaneous quantification of multiple RNA transcripts crucial for breast cancer classification. This protocol specifically targets biomarkers that define the principal molecular subtypes: Luminal A, Luminal B, HER2-enriched, and Triple-Negative/Basal-like. Rapid and objective subtyping is essential for personalized treatment strategies, as breast cancer represents a heterogeneous disease with distinct subtypes requiring different therapeutic approaches [29].
Experimental Workflow
The following diagram illustrates the complete workflow for breast cancer subtyping using multiplex RT-qPCR:
Detailed Protocol
Materials Required:
- Fresh frozen or FFPE breast tumor tissue specimens
- RNA extraction kit (compatible with FFPE tissues if applicable)
- DNase I treatment kit
- Spectrophotometer or fluorometer for RNA quantification
- Reverse transcription kit with random hexamers and oligo-dT primers
- Multiplex RT-qPCR master mix
- Primer-probe sets for target and reference genes
- Real-time PCR instrument with multiplex detection capabilities
Procedure:
RNA Extraction and Quality Control
- Extract total RNA from 10-20 mg of fresh frozen tissue or 3-5 sections of 10 µm FFPE tissue sections using a standardized kit.
- Treat extracted RNA with DNase I to remove genomic DNA contamination.
- Quantify RNA concentration using a spectrophotometer (A260/A280 ratio ≥1.8 indicates pure RNA).
- Assess RNA integrity using an automated electrophoresis system (RNA Integrity Number ≥7.0 for fresh frozen tissues).
cDNA Synthesis
- Use 500 ng - 1 µg of total RNA for reverse transcription in a 20 µL reaction volume.
- Apply the following thermal cycler conditions: 25°C for 10 minutes (primer annealing), 50°C for 60 minutes (reverse transcription), 85°C for 5 minutes (enzyme inactivation).
- Dilute synthesized cDNA 1:5 with nuclease-free water before use in qPCR reactions.
Multiplex RT-qPCR Setup
- Prepare reaction mix containing:
- 5 µL multiplex qPCR master mix (2X concentration)
- 1 µL primer-probe mix (containing all target-specific assays)
- 2 µL diluted cDNA template
- 2 µL nuclease-free water
- Perform reactions in triplicate for each sample.
- Use the following cycling conditions:
- Initial denaturation: 95°C for 10 minutes
- 45 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 60 seconds (with fluorescence acquisition)
- Prepare reaction mix containing:
Data Analysis and Interpretation
- Calculate ∆Cq values for each target gene relative to housekeeping genes (Cqtarget - Cqreference).
- Apply the following classification criteria based on established clinical thresholds:
Table 2: Breast Cancer Molecular Subtyping Criteria Using Multiplex RT-qPCR
| Subtype | ER (ESR1) | PR (PGR) | HER2 (ERBB2) | Proliferation (MKI67) | Recommended Targeted Therapies |
|---|---|---|---|---|---|
| Luminal A | Positive (∆Cq < -3) | Positive (∆Cq < -2) | Negative (∆Cq > -1) | Low (∆Cq > -2) | Endocrine therapy alone |
| Luminal B | Positive (∆Cq < -3) | Variable | Negative (∆Cq > -1) | High (∆Cq < -2) | Endocrine therapy + CDK4/6 inhibitors |
| HER2-Enriched | Negative (∆Cq > -3) | Negative (∆Cq > -2) | Positive (∆Cq < -1) | Variable | Anti-HER2 targeted therapies |
| Triple-Negative/Basal-like | Negative (∆Cq > -3) | Negative (∆Cq > -2) | Negative (∆Cq > -1) | Variable | Chemotherapy, Immunotherapy (if PD-L1+) |
Integration of Liquid Biopsy for Resistance Monitoring
Principle and Significance
Liquid biopsy addresses three major issues of traditional needle biopsy: it is less invasive, accounts for tumor heterogeneity, and provides a more comprehensive representation of the evolving tumor biology [29]. This protocol utilizes liquid biopsy to monitor treatment response and detect resistance mechanisms in advanced breast cancer patients.
Experimental Workflow
The following diagram illustrates the liquid biopsy workflow for monitoring treatment resistance:
Detailed Protocol
Materials Required:
- Cell-free DNA blood collection tubes (e.g., Streck Cell-Free DNA BCT)
- Plasma preparation tubes
- Circulating cell-free DNA extraction kit
- DNA quantification kit (fluorometric)
- NGS library preparation kit for low-input DNA
- Targeted breast cancer gene panel
- Next-generation sequencer
- Bioinformatics analysis software
Procedure:
Sample Collection and Processing
- Collect 10 mL peripheral blood into cell-free DNA preservation tubes.
- Process samples within 6 hours of collection.
- Centrifuge at 1600 × g for 20 minutes at room temperature to separate plasma.
- Transfer supernatant to a fresh tube and centrifuge at 16,000 × g for 10 minutes to remove residual cells.
- Aliquot plasma and store at -80°C if not processing immediately.
cfDNA Extraction and Quality Control
- Extract cfDNA from 2-4 mL plasma using a specialized cfDNA extraction kit.
- Elute cfDNA in 20-50 µL elution buffer.
- Quantify cfDNA using a fluorometric method suitable for low DNA concentrations.
- Assess cfDNA fragment size distribution using a high-sensitivity automated electrophoresis system.
NGS Library Preparation and Sequencing
- Use 20-50 ng cfDNA for library preparation with a kit designed for low-input degraded DNA.
- Employ a targeted hybridization capture approach using a breast cancer-specific gene panel covering key resistance genes (ESR1, PIK3CA, ERBB2, RB1, etc.).
- Amplify and barcode libraries according to manufacturer's instructions.
- Sequence on a next-generation sequencing platform to achieve minimum 5000x coverage.
Bioinformatic Analysis and Interpretation
- Align sequencing reads to the reference genome.
- Call somatic variants with a minimum variant allele frequency threshold of 0.5%.
- Annotate variants using population databases and clinical knowledgebases.
- Report clinically actionable mutations with associated targeted therapy options.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Breast Cancer Subtyping
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| RNA Stabilization Reagents | RNAlater, PAXgene Tissue System | Preserves RNA integrity in tumor specimens during storage and transport |
| Nucleic Acid Extraction Kits | QIAamp cfDNA Kit, AllPrep DNA/RNA FFPE Kit | Simultaneous extraction of high-quality DNA and RNA from limited clinical samples |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit | Converts RNA to cDNA with high efficiency, even from partially degraded FFPE-derived RNA |
| Multiplex qPCR Assays | TaqMan Multiplex Master Mix, pre-designed primer-probe sets | Enables simultaneous quantification of multiple biomarkers in single reaction |
| Targeted NGS Panels | FoundationOne CDx, Guardant360 CDx | Comprehensive genomic profiling from tissue or liquid biopsy samples |
| Reference Materials | Horizon Multiplex I, Seraseq ctDNA Reference Materials | Quality control for assay validation and performance monitoring |
Rapid, objective diagnosis represents the foundational element enabling personalized treatment strategies in breast cancer. The integration of multiplex RT-qPCR for initial subtyping with liquid biopsy for ongoing monitoring creates a comprehensive diagnostic framework that guides therapeutic decisions throughout the patient journey. These protocols provide researchers and clinicians with standardized methodologies to implement these approaches, ultimately contributing to improved patient outcomes through more precise targeting of therapies. As the field evolves, the continued refinement of these diagnostic approaches will further enhance our ability to match patients with optimal treatments while monitoring for and overcoming resistance mechanisms.
Implementing a Robust Multiplex RT-qPCR Workflow from Sample to Result
Optimized RNA Extraction from FFPE and Fresh-Frozen Tissue Specimens
Formalin-fixed, paraffin-embedded (FFPE) and fresh-frozen (FF) tissue specimens represent invaluable resources for breast cancer research, particularly in transcriptomic studies aimed at molecular subtyping. The reliability of gene expression profiling (GEP) heavily depends on the input of RNA in sufficient quantity and quality [32]. However, RNA extraction from these biospecimens presents distinct challenges. FFPE tissues undergo formalin-induced cross-linking and nucleic acid fragmentation during fixation and processing, while FF tissues require meticulous handling to prevent RNA degradation by endogenous RNases [33] [34]. Optimized protocols are therefore essential to generate high-quality RNA compatible with sophisticated downstream applications like multiplex RT-qPCR, which is emerging as a rapid, accurate, and cost-effective alternative to immunohistochemistry (IHC) for breast cancer subtyping [6] [9] [35]. This application note details standardized, optimized procedures for RNA extraction from both FFPE and FF tissues, framed within the context of enabling robust multiplex RT-qPCR for breast cancer research.
Challenges in RNA Extraction from Different Specimen Types
FFPE Tissues
The process of formalin fixation and paraffin embedding, while ideal for tissue preservation and histological analysis, is detrimental to RNA integrity. The primary challenges include:
- Chemical Modifications: Formaldehyde induces methylol adducts and cross-links between RNA and proteins, impairing downstream enzymatic reactions [33].
- RNA Fragmentation: The fixation process and the inherent acidity of formalin lead to random alkaline cleavage of RNA strands, resulting in severely fragmented RNA [36] [33].
- Impact of Pre-analytical Variables: Factors such as fixation time, storage duration of the FFPE blocks, and the initial handling of the tissue before fixation significantly influence RNA quality. Studies show that RNA integrity decreases with longer archiving times, but this can be mitigated by using short amplicons in subsequent assays [37]. Furthermore, improper tissue handling before fixation (e.g., prolonged storage at room temperature) can drastically alter the expression levels of sensitive genes [34].
Fresh-Frozen Tissues
While considered the gold standard for RNA quality, FF tissues present their own set of logistical challenges:
- RNase Activity: The most critical threat is rapid RNA degradation by endogenous RNases post-resection if tissues are not immediately stabilized [34].
- Tissue Handling Logistics: The window between surgical resection and freezing is critical. Contrary to common belief, one study found that RNA in non-fixed surgical specimens remained structurally intact for up to 6-16 hours under various conditions (room temperature, on ice, in saline, or in RNAlater). However, the expression of specific genes (e.g., cfos, HIF1α) can be markedly regulated during this time, especially at room temperature [34].
The table below summarizes the key challenges and the impact on downstream gene expression analysis.
Table 1: Key Challenges in RNA Extraction from FFPE and Fresh-Frozen Tissues
| Specimen Type | Primary Challenges | Impact on RNA | Consequence for Downstream Analysis |
|---|---|---|---|
| FFPE | Formalin-induced cross-linking | Chemical modifications; covalent bonds with proteins | Reduced reverse transcription efficiency; inaccurate quantification |
| Acidic hydrolysis during fixation/embedding | Extensive fragmentation (average size: 100-300 bp) | Bias against long transcripts; requires short amplicons (<150 bp) | |
| Long-term archive storage | Negative correlation between storage time and RNA Integrity Number (RIN) | Can be overcome with targeted approaches using short primers [37] | |
| Fresh-Frozen | Endogenous RNase activity | Rapid degradation post-resection | Complete loss of RNA integrity if not handled correctly |
| Delay to freezing/ stabilization | Altered gene expression profiles for stress-responsive genes | Introduces pre-analytical variation in expression data [34] |
Optimized Protocols for RNA Extraction
RNA Extraction from FFPE Tissues
The following protocol is optimized for breast cancer core needle biopsies (CNBs) and surgical specimens, incorporating steps to reverse formalin cross-links and maximize yield from degraded material [32] [33].
Materials & Reagents:
- PureLink FFPE RNA Isolation Kit (Invitrogen) or equivalent [38]
- Xylene or a compatible deparaffinization solution
- Ethanol (100% and 70-80%)
- Proteinase K
- DNase I (RNase-free)
- Heating block or oven (set to 56°C and 80°C)
- Microcentrifuge
Detailed Protocol:
- Sectioning and Deparaffinization:
- Cut four to six 8 μm thick sections from the FFPE block. Using a higher number of sections from remounted blocks can increase yield without significantly compromising quality [38].
- Transfer sections to a nuclease-free microcentrifuge tube.
- Add 1 mL of xylene (or a kit-specific deparaffinization solution). Vortex vigorously and incubate at room temperature for 5-10 minutes.
- Centrifuge at full speed for 5 minutes. Carefully remove and discard the supernatant.
- Wash the pellet by adding 1 mL of 70-80% ethanol, vortexing, and centrifuging for 5 minutes. Discard the supernatant. Air-dry the pellet briefly (5-10 minutes).
Proteinase K Digestion and Cross-link Reversal:
- Add appropriate volumes of digestion buffer and Proteinase K (e.g., 20 μL) to the deparaffinized tissue pellet.
- Incubate at 56°C for 10-60 minutes (or according to kit instructions) to digest proteins and release nucleic acids.
- Critical Step: To reverse formalin cross-links, incubate the lysate at 70-80°C for 20-60 minutes [33]. This heating step has been shown to improve the sensitivity of downstream RT-qPCR assays by decreasing Ct values [33].
RNA Isolation and Purification:
- Follow the kit-specific protocol for binding RNA to a silica membrane column.
- Perform an on-column DNase I treatment for 15-30 minutes to remove genomic DNA contamination.
- Wash the column with provided wash buffers.
- Elute RNA in a small volume (e.g., 20-50 μL) of nuclease-free water.
RNA Extraction from Fresh-Frozen Tissues
This protocol ensures the recovery of high-integrity RNA from frozen breast cancer tissues, suitable for whole-transcriptome analyses.
Materials & Reagents:
- Qiagen RNeasy Kit (or similar column-based kit) [36]
- Liquid nitrogen and pre-cooled mortar and pestle
- RLT (or similar) lysis buffer containing guanidine isothiocyanate and β-mercaptoethanol
- RNAlater solution (optional, for stabilization)
- DNase I (RNase-free)
Detailed Protocol:
- Tissue Stabilization and Homogenization:
- Immediate Stabilization: Upon surgical resection, the optimal approach is to immediately snap-freeze the tissue in liquid nitrogen and store it at -80°C. Alternatively, for logistical ease, tissue pieces can be immersed in RNAlater and stored at 4°C for up to 24 hours before long-term freezing [34].
- Pulverization: For frozen tissues, grind the tissue to a fine powder under liquid nitrogen using a pre-cooled mortar and pestle. Do not allow the tissue to thaw.
- Lysis and Homogenization: Transfer the powder to a tube containing a denaturing lysis buffer (e.g., RLT buffer with β-mercaptoethanol) and homogenize thoroughly using a rotor-stator homogenizer. This step is critical for complete cell lysis and RNase inhibition.
- RNA Isolation and Purification:
- Follow the manufacturer's instructions for the chosen kit. Typically, this involves precipitating impurities with ethanol, binding RNA to a silica membrane, and washing.
- Include an on-column DNase I digestion step.
- Elute the RNA in nuclease-free water.
Table 2: Troubleshooting Common RNA Extraction Issues
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low RNA Yield (FFPE) | Incomplete deparaffinization; insufficient tissue. | Ensure complete xylene removal; use more sections (e.g., six 8 μm slices) [38]. |
| Low RNA Yield (FF) | Incomplete homogenization; RNase degradation. | Ensure tissue is fully powdered under liquid nitrogen; use fresh, potent β-mercaptoethanol. |
| Poor RNA Purity (A260/280 ratio) | Protein or solvent carryover. | Ensure complete removal of wash buffers; extend drying time of the spin column. |
| DNA Contamination | Inefficient DNase treatment. | Ensure DNase I is active and the incubation is performed at the correct temperature and duration. |
| Incompatible with downstream RT-qPCR | Residual inhibitors or high fragmentation. | Perform an additional wash or ethanol precipitation; design assays with short amplicons (<150 bp) [33]. |
Quality Control and Assessment
Rigorous quality control is non-negotiable for successful gene expression analysis.
- Quantification and Purity: Use a spectrophotometer (e.g., NanoDrop) to measure concentration. Acceptable A260/A280 ratios are ~2.0 for pure RNA.
- RNA Integrity:
- For FF tissues: Use the Agilent Bioanalyzer to determine the RNA Integrity Number (RIN). A RIN > 7.0 is generally recommended for sequencing applications [36].
- For FFPE tissues: The DV200 index (percentage of RNA fragments >200 nucleotides) is a more reliable metric. Samples with a DV200 of 30-50% are considered low-quality but may still be usable with targeted methods, while a DV200 >50% is preferable [38] [36]. The median Transcript Integrity Number (TIN) from RNA-seq data can also be used post-hoc to assess integrity [36].
Application in Breast Cancer Research: Multiplex RT-qPCR for Subtyping
High-quality RNA extracted via these optimized protocols is directly applicable to advanced molecular diagnostics. Multiplex RT-qPCR allows for simultaneous quantification of multiple biomarkers from a single sample, offering a objective and rapid alternative to IHC.
A 2023 study demonstrated the power of this approach by profiling ESR1, PGR, ERBB2 (HER2), and MKi67 (Ki67) genes—the core determinants of clinical subtypes—using RPL13A as a reference gene [6] [9]. The methodology employed a touch-down multiplex RT-qPCR protocol, which consistently yielded low Cycle Threshold (CT) values, indicating high assay sensitivity and robustness [6]. The resulting gene expression profiles showed remarkable precision, nearly equivalent to IHC, in diagnosing breast cancer subtypes (Luminal A, Luminal B, HER2-positive, Triple-negative) [6]. Furthermore, the study extended the profiling to angiogenesis-related genes (Hif1A, ANG, VEGFR), providing insights into the metastatic potential of tumors [6]. This highlights how optimized RNA extraction enables not just accurate subtyping but also deeper molecular characterization.
Diagram 1: Workflow for RNA extraction from FFPE and fresh-frozen tissues for breast cancer subtyping.
The Scientist's Toolkit: Essential Reagents and Kits
Table 3: Research Reagent Solutions for Optimized RNA Extraction
| Reagent/Kits | Function/Application | Specific Example(s) |
|---|---|---|
| FFPE RNA Isolation Kits | Optimized for deparaffinization, cross-link reversal, and extraction of fragmented RNA. | PureLink FFPE RNA Isolation Kit [38], Quick-DNA/RNA FFPE Kit [6], RecoverAll Total Nucleic Acid Isolation Kit [33] |
| Fresh-Frozen RNA Isolation Kits | Designed for efficient homogenization and high-yield recovery of intact RNA. | Qiagen RNeasy Kit [36] |
| RNase Inhibitors | Critical for preventing RNA degradation during extraction from fresh tissues. | RNAsin [34] |
| DNase I (RNase-free) | Essential for removing genomic DNA contamination, which is crucial for accurate gene expression analysis. | Included in many kits or available separately [36] [34] |
| RNA Stabilization Solution | Stabilizes RNA in fresh tissues during transport or temporary storage. | RNAlater [36] [34] |
| Reverse Transcription Kits | For synthesizing high-quality cDNA from challenging FFPE-derived RNA. | High Capacity cDNA Reverse Transcription Kit [33] |
| TaqMan Gene Expression Assays | Ideal for degraded FFPE RNA due to short amplicon lengths (<150 bp) and MGB probe technology. | Various assays from Thermo Fisher Scientific [33] |
| Reference Genes | Essential for data normalization in RT-qPCR. | RPL13A [6], CYFIP1 (used in Xpert STRAT4 assay) [35], GAPDH [6] |
The success of multiplex RT-qPCR and other molecular techniques in breast cancer research is fundamentally rooted in the quality of the input RNA. The optimized protocols detailed herein for FFPE and fresh-frozen tissues provide a robust framework for overcoming the inherent challenges associated with each specimen type. By adhering to these standardized procedures—emphasizing cross-link reversal for FFPE, rapid stabilization for fresh tissues, and rigorous QC—researchers can ensure the generation of reliable, high-quality gene expression data. This, in turn, empowers advanced assays like multiplex RT-qPCR to accurately profile breast cancer subtypes and other oncogenic pathways, accelerating the development of personalized therapeutic strategies.
Primer and Probe Design for Reliable Multiplex Assays
The accurate molecular subtyping of breast cancer is a critical component of modern precision oncology, enabling the selection of targeted therapies and improving patient outcomes. Multiplex reverse transcription quantitative polymerase chain reaction (RT-qPCR) has emerged as a powerful technique for simultaneously detecting the expression of multiple genes from limited patient samples, such as formalin-fixed paraffin-embedded (FFPE) tissues. This application note details optimized protocols for designing primers and probes for reliable multiplex assays, specifically framed within breast cancer subtyping research. The methodologies described herein support the development of robust diagnostic assays that can classify breast cancer subtypes based on established gene expression profiles with precision nearly equivalent to immunohistochemistry (IHC) [6].
Compared to single-plex reactions, multiplex assays present unique challenges in primer and probe design, primarily due to the exponentially increasing number of potential primer-dimer interactions as additional targets are incorporated. For an N-plex PCR primer set comprising 2N primers, there are (2N choose 2) possible primer-dimer interactions, creating a complex optimization landscape that requires sophisticated computational approaches [39]. This technical guide addresses these challenges through systematic design principles, experimental validation protocols, and specialized reagent solutions tailored for breast cancer biomarker detection.
Breast Cancer Molecular Subtyping Markers
Molecular subtyping of breast cancer relies on the detection of specific biomarkers that define distinct biological entities with different clinical behaviors. The established markers for breast cancer subtyping include hormone receptors (ESR1, PGR), HER2 oncogene, and proliferation markers (Ki67), which form the foundation for treatment decisions [6]. Additionally, biomarkers related to angiogenesis and metastatic potential (Hif1A, ANG, VEGFR) provide valuable prognostic information and may guide additional therapeutic targeting.
Table 1: Key Biomarkers for Breast Cancer Subtyping
| Biomarker | Full Name | Role in Breast Cancer | Clinical Significance |
|---|---|---|---|
| ESR1 | Estrogen Receptor 1 | Hormone receptor | Defines luminal subtypes; predicts response to endocrine therapy |
| PGR | Progesterone Receptor | Hormone receptor | Defines luminal subtypes; predicts response to endocrine therapy |
| HER2 | Human Epidermal Growth Factor Receptor 2 | Tyrosine kinase receptor | HER2-positive subtype; predicts response to HER2-targeted therapies |
| Ki67 | Marker of Proliferation Ki-67 | Cellular proliferation marker | Assesses tumor aggressiveness and proliferation rate |
| Hif1A | Hypoxia Inducible Factor 1 Subunit Alpha | Angiogenesis transcription factor | Indicates tumor hypoxia; potential marker for metastatic risk |
| VEGF | Vascular Endothelial Growth Factor | Angiogenesis signaling protein | Promotes blood vessel formation; potential therapeutic target |
| ANG | Angiogenin | Angiogenesis factor | Stimulates new blood vessel formation; associated with metastasis |
Recent research has demonstrated that multiplex RT-qPCR can effectively assess the gene expression profiles of these biomarkers across 61 samples representing four breast cancer subtypes, using RPL13A as a stable endogenous control gene [6]. This approach offers remarkable precision in detecting gene expressions vital for breast cancer diagnosis and subtyping, while additionally providing insights into the metastatic potential of tumors through parallel assessment of angiogenesis-related genes.
Principles of Multiplex Assay Design
Computational Design Framework
The design of highly multiplexed PCR primer sets requires sophisticated computational approaches to manage the vast optimization space. Simulated Annealing Design using Dimer Likelihood Estimation (SADDLE) represents a state-of-the-art algorithmic framework that minimizes primer dimer formation in highly multiplexed assays [39]. This method addresses the fundamental challenge that for an N-plex PCR primer set with 2N primers, there are quadratically increasing potential primer dimer species, while the sequence selection choices grow exponentially.
The SADDLE algorithm implements a six-step process: (1) generation of forward and reverse primer candidates for each gene target; (2) selection of an initial primer set S0; (3) evaluation of a Loss function L(S) on the initial primer set; (4) generation of a temporary primer set T by randomly changing one or more primers; (5) probabilistic acceptance of the temporary set based on Loss function comparison; and (6) repetition of steps 4-5 until an acceptable primer set is constructed [39]. This stochastic optimization approach navigates the highly non-convex fitness landscape of multiplex primer design efficiently.
Core Design Parameters
Successful multiplex assay design depends on careful attention to several critical parameters that govern primer and probe behavior in combined reactions:
Primer Design Considerations:
- Length: Optimal primer length should be 18-25 nucleotides for stable binding [13] [40]
- GC Content: Maintain 40-60% GC content for appropriate melting temperature and stability [13]
- Specificity: Design primers to span exon-exon junctions where possible to avoid genomic DNA amplification [13]
- Amplicon Size: Preferable distance between forward and reverse primers is 70-200 base pairs for efficient qPCR [13]
TaqMan Probe Design Principles:
- Sequence Selection: The probe sequence should closely match the specific region of the target sequence to avoid binding with non-target sequences [40]
- Optimal Length: TaqMan probes should be 20-30 nucleotides in length [40]
- Melting Temperature (Tm): The Tm of TaqMan probes should be approximately 10°C higher than that of primers, typically between 65-70°C [40]
- Fluorescent Labels: Use distinct fluorophore-quencher pairs (e.g., FAM-BHQ1, HEX-BHQ2) for each target in the multiplex reaction
- Avoidance of Secondary Structures: Repetitive nucleotide sequences, especially consecutive G bases (no 4 consecutive G bases), should be avoided for efficiency and reproducibility [40]
Table 2: Key Design Parameters for Primers and Probes in Multiplex Assays
| Parameter | Primers | TaqMan Probes |
|---|---|---|
| Length | 18-25 nucleotides | 20-30 nucleotides |
| GC Content | 40-60% | 30-80% |
| Tm | 55-65°C | 65-70°C (10°C higher than primers) |
| Concentration | 50-900 nM (optimized per assay) | 50-250 nM |
| Specificity Check | BLAST against genome database | BLAST against genome database |
| Secondary Structures | Avoid self-dimers and hairpins | Avoid self-dimers and hairpins |
Multiplexing Strategy for Breast Cancer Subtyping
For breast cancer subtyping, a strategic multiplexing approach can be employed where related biomarkers are grouped into logical reaction sets. Research has demonstrated successful classification using a multiplexing strategy with three reaction tubes per sample: the first tube assesses expression of RPL13A (reference gene), ESR, PGR, and HER2; the second tube measures Ki67 and RPL13A; and the third tube detects RPL13A, HIF1A, ANG, and VEGF [6]. This approach maintains assay robustness while enabling comprehensive molecular profiling.
The touch-down PCR protocol implementation in breast cancer subtyping has been shown to yield significantly lower Cycle Threshold (CT) values, enhancing detection sensitivity [6]. This method progressively lowers the annealing temperature during initial cycles, promoting specific primer binding and increasing overall assay precision.
Experimental Protocols
RNA Extraction and cDNA Synthesis
Materials:
- Quick-DNA/RNATM FFPE Kit (ZYMO RESEARCH Catalog Number R1009) or equivalent [6]
- Nano-Drop One C spectrophotometer (Thermo Fisher Scientific) or equivalent for RNA quantification
- Reverse transcriptase with associated buffer system
- dNTP mix, MgCl2, RNase inhibitors
- Gene-specific primers, oligo(dT) primers, or random hexamers
Method:
- Extract total RNA from FFPE samples following manufacturer's instructions [6]. For FFPE tissues, select sample blocks with more than two-thirds tumor tissue and use only tumor tissue areas for RNA extraction.
- Assess RNA concentration and purity using spectrophotometry. Acceptable 260/280 ratios are typically 1.8-2.1.
- Denature RNA secondary structures by incubating at 65°C to 70°C for 5-10 minutes [13].
- For cDNA synthesis, use gene-specific primers to enhance sensitivity and specificity for targeted gene expression analysis [13]. Alternatively, random hexamers or oligo(dT) primers may be employed depending on application requirements.
- Prepare reverse transcription reaction mixture containing reverse transcriptase, dNTPs, RNase inhibitors, and MgCl2 [13].
- Incubate at 37°C to 50°C for 30-60 minutes for cDNA synthesis [13].
- Terminate reaction by inactivating reverse transcriptase at 70°C to 85°C for 5-10 minutes [13].
- Dilute cDNA 1:10 for medium to highly expressed targets or 1:2 to 1:5 for rare transcripts before use in qPCR reactions [41].
Multiplex qPCR Setup and Thermal Cycling
Materials:
- LuminoCt ReadyMix or equivalent qPCR master mix [41]
- Sequence-specific primers and TaqMan probes
- PCR-grade water
- 96-well or 384-well PCR plates compatible with qPCR instrument
- Quantitative PCR instrument with multiplex fluorescence detection capability
Method:
- Defrost all reaction components on ice, protecting fluorescent probes from light exposure [41].
- Prepare primer and probe blends based on optimized concentrations determined during assay development.
- Prepare master mix according to Table 3, calculating volumes for all reactions and adding 10% to account for pipetting error [41].
- Add 5 μL of cDNA solution to appropriate PCR tubes or wells.
- Aliquot 15 μL of master mix into each reaction tube or well.
- Cap tubes or seal plate, ensuring labels do not interfere with instrument optics.
- Centrifuge briefly to collect all liquid at the bottom of tubes/wells.
- Run samples using the thermal cycling protocol in Table 4 [41].
Table 3: Multiplex qPCR Master Mix Preparation
| Component | Initial Concentration | Volume per 20 μL Reaction | Final Concentration |
|---|---|---|---|
| qPCR ReadyMix | 2X | 10 μL | 1X |
| Forward Primer Mix | 100 μM | Variable | Optimized (50-900 nM each) |
| Reverse Primer Mix | 100 μM | Variable | Optimized (50-900 nM each) |
| TaqMan Probe Mix | 100 μM | Variable | Optimized (50-250 nM each) |
| PCR-grade Water | - | To volume | - |
| Template cDNA | - | 5 μL | 10-100 ng |
Table 4: Thermal Cycling Conditions for Multiplex qPCR
| Step | Temperature | Time | Cycles | Purpose |
|---|---|---|---|---|
| Initial Denaturation | 95°C | 2 minutes | 1 | Enzyme activation, template denaturation |
| Denaturation | 95°C | 10-15 seconds | 40 | Template denaturation |
| Annealing/Extension | 60°C | 30-60 seconds | 40 | Primer annealing, probe hydrolysis, data collection |
For assays requiring higher specificity, a three-step protocol with separate annealing and extension steps may be employed: denaturation at 95°C, annealing at optimized temperature (55-65°C), and extension at 72°C [13].
Data Analysis and Interpretation
Quantification Methods:
- Determine Ct values for each target gene in all samples.
- Select appropriate reference genes (e.g., RPL13A, GAPDH) with stable expression across sample types [6].
- Apply the ΔΔCt method for relative quantification: Calculate ΔCt values (Cttarget - Ctreference) for each sample [6].
- Compute ΔΔCt values (ΔCtsample - ΔCtcontrol) to determine fold changes using the formula 2^(-ΔΔCt) [6].
- For absolute quantification, establish standard curves using known concentrations of target templates [13].
Quality Control Parameters:
- Amplification efficiency: 90-110% [6]
- R² value for standard curves: >0.98
- No Template Control (NTC): No amplification or Ct >40
- Positive controls: Within expected Ct ranges
The Scientist's Toolkit
Table 5: Essential Research Reagent Solutions for Multiplex Breast Cancer Subtyping
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| RNA Extraction Kits | Quick-DNA/RNATM FFPE Kit (Zymo Research) | Isolation of high-quality RNA from FFPE tissues | Select kits optimized for degraded FFPE-derived RNA |
| Reverse Transcription Reagents | Gene-specific primers, Oligo(dT), Random hexamers | cDNA synthesis from RNA templates | Gene-specific primers enhance sensitivity for low-abundance targets |
| qPCR Master Mixes | LuminoCt ReadyMix | Provides enzymes, buffers, dNTPs for amplification | Select mixes optimized for multiplex reactions |
| Hydrolysis Probes | TaqMan probes with FAM, HEX, ROX fluorophores | Target-specific detection in multiplex qPCR | Ensure spectral compatibility of fluorophores |
| Reference Genes | RPL13A, GAPDH | Normalization of gene expression data | Validate stability across sample types |
| Positive Controls | Synthetic gBlocks, Control cell line cDNA | Assay validation and quality control | Should encompass all targets in multiplex panel |
| Digital PCR Reagents | naica system reagents, Crystal dPCR reagents | Absolute quantification of rare mutations | Enables detection of low-frequency mutations in liquid biopsies |
Workflow Visualization
Multiplex Assay Development Workflow
This workflow outlines the comprehensive process for developing multiplex RT-qPCR assays for breast cancer subtyping, from initial target selection through clinical application. The diagram highlights the critical design and validation phases that ensure assay reliability.
Primer Design Optimization Process
This diagram illustrates the SADDLE algorithm workflow for multiplex primer design, which systematically minimizes primer dimer formation through iterative optimization. The process involves candidate generation with specific biophysical constraints and loss function calculation to estimate potential primer dimer interactions.
Robust primer and probe design is fundamental to developing reliable multiplex RT-qPCR assays for breast cancer subtyping. By implementing the computational design frameworks, experimental protocols, and quality control measures outlined in this application note, researchers can establish multiplex assays that accurately classify breast cancer subtypes based on established biomarker panels. The strategic grouping of biomarkers into logical multiplex sets, combined with careful attention to primer and probe design parameters, enables comprehensive molecular profiling from limited patient samples.
The continued advancement of multiplex PCR technologies, including improved computational design algorithms and more sensitive detection chemistries, promises to further enhance the precision and throughput of breast cancer molecular subtyping. These developments will strengthen the foundation for personalized treatment approaches and ultimately improve patient outcomes in breast cancer management.
Touch-Down PCR Protocols for Enhanced Specificity and Lower CT Values
Touchdown (TD) PCR is a refined polymerase chain reaction technique that significantly enhances amplification specificity and sensitivity by employing a progressively decreasing annealing temperature during the initial cycling stages. This method systematically transitions from an initial annealing temperature set approximately 5–10°C above the calculated melting temperature (T~m~) of the primers down to a more permissive temperature below the T~m~ over successive cycles [42] [43]. In the context of breast cancer research, particularly for multiplex RT-qPCR-based subtyping, this technique offers a critical advantage by minimizing non-specific amplification and primer-dimer formation, which is paramount when simultaneously assessing multiple biomarkers from limited clinical samples [6] [9].
The fundamental principle behind TD-PCR is the preferential amplification of targets with perfect primer-template complementarity. During the initial high-stringency cycles, only these ideal hybrids form efficiently. As the temperature decreases in subsequent cycles, this specifically enriched amplicon outcompetes any non-specific products, leading to a substantial exponential advantage—often estimated at twofold per cycle—for the correct product [44] [45]. This is especially vital in breast cancer diagnostics, where accurately quantifying the expression of genes like ESR1, PGR, ERBB2 (HER2), and Ki67 directly impacts subtype classification and treatment decisions [6].
Key Principles and Mechanistic Workflow
The enhanced specificity of TD-PCR is achieved through a carefully orchestrated two-phase cycling process. The initial touchdown phase favors the accumulation of the most specific amplicons, which then dominate the reaction in the second, standard amplification phase.
The following diagram illustrates the logical workflow and temperature progression that underlies the TD-PCR process:
Mechanism of Specificity Enhancement
Competitive Advantage for Specific Products: The core mechanism of TD-PCR lies in the significant competitive advantage it confers to perfectly matched primer-template hybrids. Any difference in T~m~ between correct and incorrect annealing creates an exponential advantage of twofold per cycle for the desired amplicon [44]. This advantage is crucial in a multiplex setting, such as breast cancer subtyping, where multiple primer sets must work simultaneously without cross-reactivity [6].
Minimization of Mispriming: By starting with high-stringency conditions, TD-PCR effectively circumvents the issue of spurious priming during the critical early cycles of amplification. This is achieved by ensuring that primer binding to non-target sequences with lower complementarity is suppressed, thereby preferentially amplifying the intended target from the outset [45] [43].
Touchdown qPCR (TqPCR) for Enhanced Sensitivity
The principles of TD-PCR have been successfully adapted into quantitative PCR (qPCR), a method termed TqPCR. This adaptation offers remarkable improvements in detection sensitivity, which is paramount for quantifying lowly-expressed transcripts in clinical samples, such as those obtained from formalin-fixed, paraffin-embedded (FFPE) breast tumor tissues [46].
A study systematically comparing conventional qPCR to TqPCR demonstrated that incorporating a 4-cycle touchdown stage prior to the quantification cycles resulted in a significant reduction of 4.95 cycles (average) in C~q~ values for reference genes, directly translating to higher detection sensitivity [46]. This enhanced sensitivity is not merely a result of increased product yield but also stems from improved amplification efficiency [46]. Consequently, TqPCR enables reliable detection of low-abundance transcripts that might otherwise remain undetected with standard qPCR protocols, thereby providing a more complete molecular profile of breast cancer subtypes.
Table 1: Performance Comparison of Conventional qPCR vs. Touchdown qPCR (TqPCR)
| Parameter | Conventional qPCR | Touchdown qPCR (TqPCR) | Experimental Context |
|---|---|---|---|
| Average C~q~ Reduction | Baseline | 4.95 cycles | Analysis of Gapdh, Rps13, and Hprt1 reference genes [46] |
| Detection of Lowly-Expressed Genes | Failed to detect Oct4 and Gbx2 upregulation |
Successfully detected Oct4 and Gbx2 upregulation |
Analysis of Wnt3A-induced gene expression in mesenchymal stem cells [46] |
| Amplification Efficiency | Standard | Significantly Improved | SYBR Green-based assays [46] |
| Practical Application | Suitable for abundant transcripts | Essential for low-abundance transcripts and/or limited RNA samples | Breast cancer subtyping from FFPE samples [6] [46] |
Application in Breast Cancer Subtyping via Multiplex RT-qPCR
The integration of TD-PCR into multiplex RT-qPCR protocols presents a powerful tool for advancing the precision and efficiency of breast cancer molecular subtyping. A 2023 study established a novel diagnostic method using multiplex RT-qPCR with a touchdown approach to evaluate the gene expression profiles of HER2, PGR, ESR, and Ki67—the key biomarkers for breast cancer classification [6] [9].
This method demonstrated remarkable precision, nearly equivalent to immunohistochemistry (IHC), the current clinical gold standard, but with the added benefits of being faster, more cost-effective, and less dependent on subjective pathological interpretation [6]. The use of a touchdown protocol was critical to ensure accurate annealing among the different primers and probes within the same reaction, consistently yielding significantly lower C~T~ values and thus robust data for all targets simultaneously [6]. Furthermore, the protocol allowed for complementary profiling of angiogenesis-related genes (Hif1A, ANG, VEGFR), providing additional insights into the metastatic potential of the tumors [6].
Table 2: Summary of Key Experimental Details from Breast Cancer Subtyping Study
| Aspect | Details |
|---|---|
| Sample Type | 61 FFPE breast tumor blocks and 9 benign samples [6] |
| Key Target Genes | ESR, PGR, HER2, Ki67 (for subtyping); Hif1A, ANG, VEGF (for angiogenesis) [6] |
| Endogenous Control | RPL13A [6] |
| PCR Method | Multiplex RT-qPCR with touch-down protocol [6] |
| Amplification Efficiency | Calculated for each gene; e.g., RPL13A: 99.9%, ESR: 99.3%, PGR: 101.8% [6] |
| Data Analysis | ΔC~T~ and ΔΔC~T~ methods, with normalization to IHC scoring scale [6] |
Detailed Experimental Protocols
Standard Touchdown PCR Protocol
A robust and widely cited TD-PCR protocol involves a two-stage process as detailed in Nature Protocols [44]. The following workflow outlines the key steps:
- Reaction Setup: Prepare master mix on ice. The use of a hot-start DNA polymerase is strongly recommended to further suppress non-specific amplification during reaction setup and the initial denaturation step [45] [42].
- Initial Denaturation: 95°C for 3 minutes.
- Touchdown Phase (Stage 1): 10-15 cycles of:
- Denaturation: 95°C for 30 seconds.
- Annealing: Start at 10°C above the primer's calculated T~m~. Reduce the temperature by 1°C per cycle.
- Extension: 72°C for 45 seconds (adjust based on amplicon length and polymerase speed).
- Standard Amplification (Stage 2): 20-25 cycles of:
- Denaturation: 95°C for 30 seconds.
- Annealing: Use the final, lowest annealing temperature reached in the touchdown phase (typically 2-5°C below the primer T~m~).
- Extension: 72°C for 45 seconds.
- Final Extension: 72°C for 15 minutes.
Multiplex RT-qPCR with Touchdown for Breast Cancer
The protocol adapted from the 2023 breast cancer study utilizes a more complex, multi-stage touchdown approach to ensure efficient and specific amplification of multiple gene targets in few tubes [6].
Table 3: Thermocycling Protocol for Multiplex RT-qPCR Breast Cancer Subtyping
| Stage | Cycles | Temperature | Time | Function |
|---|---|---|---|---|
| cDNA Formation | 1 | 50°C | 10 min | Reverse Transcription |
| Initial Denaturation | 1 | 95°C | 2 min | Polymerase Activation |
| Pre-Cycle (Touchdown) | 3 | 95°C | 10 sec | Denaturation |
| 70°C | 15 sec | High-Stringency Annealing | ||
| 3 | 95°C | 10 sec | Denaturation | |
| 67°C | 15 sec | Medium-Stringency Annealing | ||
| 3 | 95°C | 10 sec | Denaturation | |
| 63°C | 15 sec | Lower-Stringency Annealing | ||
| Quantification | 40 | 95°C | 5 sec | Denaturation |
| 60°C | 30 sec | Annealing/Extension with Data Collection |
This protocol groups the touchdown stages into three discrete temperature steps (70°C -> 67°C -> 63°C) before settling at the final quantification annealing temperature of 60°C for 40 cycles [6].
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of TD-PCR, especially in complex applications like multiplex RT-qPCR, relies on carefully selected reagents and materials.
Table 4: Essential Research Reagents for Touchdown PCR Protocols
| Reagent/Material | Function/Purpose | Example from Literature |
|---|---|---|
| Hot-Start DNA Polymerase | Suppresses non-specific amplification during reaction setup and low-temperature steps; critical for specificity [45] [42]. | Kapa 2G HS taq polymerase [47] |
| Primers with Validated T~m~ | Designed for specific targets; accurate T~m~ calculation is essential for setting the initial and final annealing temperatures. | Primers/Probes for HER2, ESR, PGR, Ki67 [6] |
| RNA Extraction Kit (FFPE compatible) | To obtain high-quality, intact total RNA from challenging clinical sample types. | Quick-DNA/RNATM FFPE Kit [6] |
| Reverse Transcriptase | For cDNA synthesis from RNA templates in the first step of RT-qPCR. | Not specified in results, but essential. |
| Dual-Labeled Probes | For specific detection of target genes in multiplex qPCR assays without signal interference. | Hydrolysis probes used for multiplex detection [6] |
| dNTPs | Building blocks for new DNA strand synthesis. | dNTPS-kapa [47] |
| PCR Buffer with MgCl~2~ | Provides optimal chemical environment (pH, salts) and Mg~2+~ co-factor for polymerase activity. | Kapa 2G HS buffer [47] |
| PCR Additives | Can improve amplification of difficult templates (e.g., GC-rich); enhances specificity when combined with TD-PCR [45]. | Glycerol (6.5%) [47] |
Technical Tips for Optimization and Troubleshooting
- Keep Reactions Cool: Maintain all reaction components on ice until thermal cycling begins to prevent non-specific priming and primer-dimer formation [45].
- Limit Total Cycle Number: To avoid the appearance of non-specific bands in later cycles, keep the total number of amplification cycles (including the touchdown phase) below 35 [45].
- Address Difficult Templates: For templates with high GC content or complex secondary structures, combine TD-PCR with additives like DMSO, glycerol, or betaine, and consider adding an extra denaturation cycle at 96-97°C [45].
- Validate with Controls: Always include no-template controls (NTC) and positive controls to rule out contamination and confirm assay performance.
In the molecular subtyping of breast cancer using multiplex RT-qPCR, accurate data normalization is not merely a technical step but a fundamental prerequisite for biological relevance. The transcriptomic profiling of clinical samples, particularly those derived from formalin-fixed paraffin-embedded (FFPE) tissues, introduces multiple variables including RNA degradation, tumor heterogeneity, and varying cellular composition [48]. Without proper normalization, these technical artifacts can obscure true biological differences, leading to misinterpretation of biomarker expression patterns. The ΔΔCT method provides a robust framework for relative quantification, but its accuracy is critically dependent on the selection of stable reference genes that remain invariant across the experimental conditions [49]. This application note details a standardized protocol for implementing the ΔΔCT method with emphasis on validating RPL13A as a stable reference gene for breast cancer research, enabling reliable interpretation of gene expression signatures relevant to therapeutic stratification.
Theoretical Foundation of the ΔΔCT Method
Principles of Relative Quantification
Relative quantification in qPCR determines the change in expression of a target gene relative to a reference sample (such as untreated control) or a calibrator gene [50] [51]. Unlike absolute quantification, which measures exact copy numbers, relative quantification calculates expression fold changes, making it particularly suitable for gene expression analysis where the absolute quantity of mRNA per cell is not required [49]. The ΔΔCT method is predicated on the comparison of threshold cycle (CT) values between target and reference genes across different experimental groups, providing a normalized expression measure that accounts for sample-to-sample variations in RNA quality, reverse transcription efficiency, and cDNA loading [52].
The mathematical foundation of the ΔΔCT method assumes that the amplification efficiencies of both target and reference genes are approximately equal and close to 100% [49]. When these conditions are met, the difference in CT values (ΔCT) between target and reference genes can be used to calculate fold changes using the formula 2-ΔΔCT [52]. This approach eliminates the need for standard curves, thereby increasing throughput and reducing potential dilution errors associated with creating standard curve samples [50].
Critical Validation Requirements
Before implementing the ΔΔCT method, researchers must conduct validation experiments to confirm that the amplification efficiencies of target and reference genes are approximately equal [50] [51]. This typically involves generating a standard curve with serial dilutions of cDNA and ensuring that the difference between the slopes of target and reference genes is less than 0.1 [52]. Additionally, the reference gene must demonstrate stable expression across all experimental conditions, including different breast cancer subtypes, treatment regimens, and tissue processing methods [53] [49].
Table 1: Key Parameters for ΔΔCT Method Validation
| Parameter | Optimal Value | Validation Method | Impact on Data Quality |
|---|---|---|---|
| Amplification Efficiency | 90-110% (Efficiency value: 1.9-2.1) | Standard curve with serial dilutions (5-6 points) | Large efficiency differences (>10%) between target and reference genes cause inaccurate fold change calculations |
| Slope Difference | < 0.1 | Compare standard curve slopes of target and reference genes | Slope differences > 0.1 require efficiency correction methods (e.g., Pfaffl method) |
| Reference Gene Stability (M value) | < 0.5 (geNorm algorithm) | Expression stability analysis across all samples | High M values (>1.0) indicate unstable reference genes that introduce normalization errors |
| Linear Dynamic Range | At least 5 logs | Serial dilution of representative samples | Limited dynamic range reduces accuracy for low-abundance transcripts |
Experimental Protocol: ΔΔCT Implementation with RPL13A Normalization
Sample Preparation and RNA Isolation from Breast Cancer Tissues
Materials:
- Breast cancer FFPE tissue sections (5-10 μm thickness) or fresh frozen tissues
- Laser capture microdissection system (e.g., Arcturus XT) for precise cell population isolation [48]
- RNA isolation kit optimized for FFPE tissues (e.g., RecoverAll Total Nucleic Acid Isolation Kit)
- DNase I treatment reagents to remove genomic DNA contamination
- RNA quality assessment tools (e.g., Bioanalyzer with RNA Integrity Number equivalent calculation for FFPE RNA)
Procedure:
- Tissue Sectioning and Microdissection: Cut FFPE tissue sections at 5-10 μm thickness and mount on specially coated slides. For heterogeneous breast cancer samples, employ laser capture microdissection to isolate specific cellular compartments (epithelial vs. stromal components) to ensure analytical precision [48]. Circle target regions containing at least 42 mm² of tumor area for sufficient RNA yield.
- RNA Extraction: Follow manufacturer protocols for RNA isolation from FFPE tissues, including appropriate deparaffinization and protease digestion steps (typically 4-18 hours at 65°C). For fresh tissues, use guanidinium thiocyanate-phenol-chloroform extraction methods.
- DNA Digestion: Treat all RNA samples with DNase I to eliminate genomic DNA contamination that could lead to false positive amplification.
- RNA Quantification and Quality Control: Measure RNA concentration using fluorometric methods and assess quality through UV spectrophotometry (A260/A280 ratio >1.8) and fragment size distribution analysis. Although FFPE-derived RNA is typically degraded, ensure that the majority of fragments are >100 nucleotides for successful amplification.
cDNA Synthesis and qPCR Setup
Materials:
- Reverse transcription kit with random hexamers and/or oligo-dT primers
- RNase inhibitor
- qPCR master mix (SYBR Green or probe-based)
- Primers for target genes and reference genes (RPL13A and others)
- 96-well or 384-well qPCR plates compatible with the detection system
Procedure:
- Reverse Transcription: Convert 100 ng-1 μg of total RNA to cDNA using a high-capacity reverse transcription kit. Include controls without reverse transcriptase (-RT controls) to monitor genomic DNA contamination.
- Primer Validation: Prior to experimental analysis, validate all primer pairs for amplification efficiency and specificity. For RPL13A detection, use sequence-specific primers (e.g., Forward: 5'-CCTGGAGGAGAAGAGGAAAGAGA-3', Reverse: 5'-TTGAGGACCTCTGTGTATTTGTCAA-3') [53]. Ensure single amplification products through melt curve analysis (SYBR Green) or probe validation.
- Reaction Plate Setup: Prepare qPCR reactions in technical triplicates containing 1× qPCR master mix, forward and reverse primers (typically 200-500 nM each), and cDNA template (diluted 1:10-1:20). Use a total reaction volume of 10-20 μL depending on plate format.
- Thermal Cycling Conditions: Program the qPCR instrument with the following protocol:
- Initial denaturation: 95°C for 2 minutes
- 40 cycles of:
- Denaturation: 95°C for 5 seconds
- Annealing/Extension: 57-60°C for 20-30 seconds [53]
- Melt curve analysis (for SYBR Green): 65°C to 95°C with 0.5°C increments
Data Analysis and Normalization Workflow
Figure 1: Workflow diagram of the ΔΔCT method for qPCR data analysis, showing the sequential steps from raw data processing to fold change calculation.
Procedure:
- Baseline Correction and Threshold Setting: Apply baseline correction using the early cycles (typically cycles 5-15) to eliminate background fluorescence variations [52]. Set the threshold within the exponential phase of all amplification plots where they display parallel trajectories, ensuring consistent ΔCT measurements across samples.
- Reference Gene Validation: Confirm the stability of RPL13A expression across all experimental conditions by comparing its CT values and calculating stability measures (M value) using algorithms like geNorm or BestKeeper. An ideal reference gene should have an M value < 0.5.
- ΔCT Calculation: For each sample, calculate ΔCT values by subtracting the CT value of the reference gene (RPL13A) from the CT value of the target gene: ΔCT = CTtarget - CTRPL13A.
- ΔΔCT Calculation: Select an appropriate calibrator sample (e.g., pooled control samples or a specific reference group) and calculate ΔΔCT values by subtracting the calibrator's ΔCT from each test sample's ΔCT: ΔΔCT = ΔCTtest - ΔCTcalibrator.
- Fold Change Calculation: Convert ΔΔCT values to relative expression fold changes using the formula: Fold Change = 2-ΔΔCT.
- Statistical Analysis: Perform appropriate statistical tests (e.g., t-tests, ANOVA) on ΔCT values rather than fold changes to maintain data distribution properties. Report fold changes with confidence intervals derived from back-transformation of the statistical results.
RPL13A as a Stable Reference Gene in Cancer Research
Validation in Physiological Stress Models
RPL13A (ribosomal protein L13a) has emerged as a superior reference gene due to its consistent expression across diverse experimental conditions. In studies of physiological stress, such as adaptation to high-altitude hypoxia, RPL13A demonstrated remarkable stability with low variability in expression (average M value < 0.5) compared to traditional reference genes like GAPDH and β-actin [53]. This stability is particularly relevant in cancer research, where tumor hypoxia significantly influences gene expression patterns and therapeutic responses. The validation protocol involved assessing expression stability across multiple sample types, with RPL13A maintaining consistent CT values regardless of altitude adaptation status, making it suitable for normalizing hypoxia-responsive genes such as EPAS1 and EGLN1 [53].
Advantages in Breast Cancer Transcriptomics
In breast cancer research, where tumor heterogeneity and stromal contamination can significantly impact gene expression measurements, RPL13A provides a stable normalization factor across different molecular subtypes. Unlike traditional reference genes whose expression can vary with cellular proliferation rates or treatment responses, RPL13A exhibits minimal fluctuation, enabling more accurate quantification of biomarkers such as ER, PR, HER2, and proliferation indices [48]. Furthermore, in multiplex assays analyzing FFPE-derived RNA from laser-capture microdissected samples, RPL13A normalization has enabled precise stratification of breast cancer subtypes based on expression profiles of 40+ transcripts, demonstrating its utility in complex diagnostic applications [48].
Table 2: Performance Comparison of Reference Genes in Breast Cancer Studies
| Reference Gene | Stability in FFPE Tissues (M value) | Response to Chemotherapy | Expression Across Molecular Subtypes | Suitability for ΔΔCT |
|---|---|---|---|---|
| RPL13A | 0.15-0.35 | Minimal change | Stable across Luminal, HER2+, Triple-negative | Excellent |
| GAPDH | 0.45-0.85 | Often modulated | Variable in basal-like subtypes | Moderate (requires validation) |
| β-actin | 0.60-1.20 | Frequently altered | Higher in mesenchymal subtypes | Poor (not recommended) |
| 18S rRNA | 0.25-0.55 | Stable | Generally stable | Good (but requires separate normalization) |
| HPRT1 | 0.40-0.75 | Moderately stable | Some variation in HER2+ | Moderate |
Application in Breast Cancer Subtyping Using Multiplex RT-qPCR
Workflow Integration
The integration of RPL13A-normalized ΔΔCT method into breast cancer subtyping pipelines enhances the reliability of molecular classification. In the optimized protocol using archival breast cancer materials, the combination of laser capture microdissection, multiplex RT-qPCR, and RPL13A normalization has enabled reproducible stratification of tumors into therapeutic categories despite RNA degradation in FFPE samples [48]. The workflow involves simultaneous measurement of multiple biomarkers (e.g., ESR1, PGR, ERBB2, MKi67, and mesenchymal markers like FN1) normalized against RPL13A, followed by principal component analysis and classification algorithms to assign molecular subtypes [48].
Data Interpretation Guidelines
Figure 2: Diagram illustrating the relationship between normalized gene expression data and clinical application in breast cancer subtyping, highlighting the role of RPL13A normalization in therapeutic decision-making.
When interpreting ΔΔCT results for breast cancer subtyping, establish the following reference ranges based on normalized expression values:
- Luminal A Signature: ESR1+ (Fold Change > 5), PGR+ (Fold Change > 3), ERBB2- (Fold Change < 2.5), MKi67- (Fold Change < 3)
- Luminal B Signature: ESR1+ (Fold Change > 5), PGR variable (Fold Change 1-5), ERBB2±, MKi67+ (Fold Change > 3)
- HER2-Enriched Signature: ERBB2+ (Fold Change > 5), ESR1- (Fold Change < 2), PGR- (Fold Change < 1.5)
- Triple-Negative/Basal-like Signature: ESR1- (Fold Change < 2), PGR- (Fold Change < 1.5), ERBB2- (Fold Change < 2.5)
These thresholds should be established and validated within each laboratory using appropriate control samples and correlation with clinical parameters.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for ΔΔCT Implementation in Breast Cancer Studies
| Reagent/Category | Specific Examples | Function in Protocol | Technical Notes |
|---|---|---|---|
| RNA Isolation Kits | FFPE RNA Recovery Kits (e.g., RecoverAll) | Extraction of high-quality RNA from archived tissues | Optimize protease digestion time (12-18 hours) for maximum yield from FFPE [48] |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kits | cDNA synthesis with optimized efficiency | Include RNase inhibitor and use random hexamers for FFPE-derived RNA |
| qPCR Master Mixes | SYBR Green or TaqMan Master Mixes | Amplification and detection of target sequences | SYBR Green requires melt curve analysis; TaqMan offers higher specificity [51] |
| Validated Primers/Probes | RPL13A-specific primers (SEQ ID No. 2 & 3) [53] | Specific amplification of reference and target genes | Pre-validate efficiency (90-110%) and specificity (single peak in melt curve) |
| Reference Gene Panels | RPL13A, HPRT1, GAPDH, 18S rRNA | Assessment of reference gene stability | Use geNorm or BestKeeper to select most stable gene(s) for your experimental system |
| qPCR Plates and Seals | Optical reaction plates, clear seals | Reaction vessel for amplification | Ensure compatibility with instrument and optimal optical properties |
| Laser Microdissection Systems | Arcturus XT, PALM MicroBeam | Precise isolation of tumor cell populations | Essential for heterogeneous samples; requires 42 mm² area for sufficient RNA [48] |
Troubleshooting and Quality Control
Addressing Common Technical Challenges
Inconsistent Amplification Efficiencies: If the ΔΔCT method assumption of equal efficiencies is violated, employ efficiency-corrected calculations using the Pfaffl method [52]. Determine actual amplification efficiencies from standard curves using the formula: Efficiency = 10[-1/slope] - 1.
High Variation in Reference Gene Expression: When RPL13A shows unexpected variability, validate additional reference genes and use geometric means of multiple stable genes for normalization. Software tools like geNorm can determine the optimal number of reference genes required for reliable normalization.
Inhibition in FFPE-Derived Samples: For samples exhibiting delayed amplification or reduced efficiency, implement a pre-amplification step or further dilute the cDNA to reduce inhibitor concentrations. Include an internal positive control (IPC) to detect inhibition.
Quality Control Metrics
Establish the following quality control checkpoints in every experiment:
- Reverse Transcription Efficiency: Assess using no-reverse transcriptase controls (-RT) for each sample, which should show CT values >5 cycles higher than corresponding +RT samples or no amplification.
- PCR Inhibition: Include a spike of known template into representative samples and compare CT values to water controls; a shift >1 cycle indicates potential inhibition.
- Inter-plate Variation: Include inter-plate calibrator samples on each plate to normalize for run-to-run variations when experiments span multiple plates.
- Reference Gene Stability: Continuously monitor RPL13A CT values across all samples; coefficients of variation >0.5 cycles may indicate RNA quality issues or experimental artifacts.
By implementing this comprehensive protocol for the ΔΔCT method with RPL13A normalization, researchers can achieve robust, reproducible gene expression data essential for accurate breast cancer subtyping and biomarker validation in both research and clinical translation contexts.
Liquid biopsy has emerged as a transformative tool in oncology, enabling non-invasive profiling of tumors through the analysis of circulating biomarkers. Among these, circulating tumor cells (CTCs) provide a window into tumor heterogeneity, metastatic potential, and therapeutic response. In breast cancer, CTC analysis complements multiplex RT-qPCR-based subtyping by resolving spatial and temporal variations in biomarker expression (e.g., ESR1, PGR, ERBB2, MKI67). This Application Note details protocols for CTC isolation, molecular characterization, and integration with RT-qPCR workflows to advance precision oncology.
CTC Isolation and Analysis Techniques
CTC isolation relies on exploiting physical or biological properties to enrich rare cells from blood. The following table summarizes key methodologies:
Table 1: CTC Enrichment and Detection Techniques
| Method | Principle | Examples | Advantages | Limitations |
|---|---|---|---|---|
| Immunomagnetic Capture | Antibody-based targeting of surface antigens (e.g., EpCAM) | CellSearch (FDA-approved) [54] [55] | High specificity; clinical validation | Misses EpCAM-negative CTCs (e.g., EMT-type cells) |
| Microfluidic Systems | Label-free sorting based on size/deformability | ClearCell FX, IsoFlux [54] | High throughput; preserves cell viability | Lower specificity vs. antibody-based methods |
| Size-Based Filtration | Physical separation via membrane pores | ScreenCell, ISET [54] [56] | Rapid processing; no antigen dependency | Loss of small CTCs or clogging |
| Density Gradient | Buoyancy-based separation | OncoQuick [54] | Compatible with large sample volumes | Moderate purity and yield |
Workflow Diagram: Integrated CTC Analysis and RT-qPCR
Protocols for CTC-Derived Molecular Profiling
CTC Enrichment via Immunomagnetic Separation
Materials:
- CellSearch CTC Kit (EpCAM-coated magnetic beads) [55]
- EDTA blood collection tubes (10 mL peripheral blood)
- Centrifuge and automated CellSearch system
Steps:
- Collect blood in EDTA tubes; process within 4–6 h.
- Centrifuge at 800 × g for 10 min to separate plasma.
- Incubate with EpCAM beads for 30 min at 4°C.
- Use magnetic separation to isolate bound CTCs.
- Fix cells for downstream RNA/DNA analysis.
RNA Extraction and Multiplex RT-qPCR
Materials:
- Quick-DNA/RNA FFPE Kit (for CTC pellets) [6]
- Primers/probes for ESR1, PGR, ERBB2, MKI67, RPL13A (reference gene) [6] [35]
- Xpert Breast Cancer STRAT4 Assay (automated RT-qPCR) [35]
Steps:
- Extract RNA using FFPE kit protocols [6].
- Synthesize cDNA with reverse transcriptase.
- Perform multiplex RT-qPCR with touchdown cycling:
- Cycling Conditions:
- 50°C for 10 min (cDNA synthesis)
- 95°C for 2 min (denaturation)
- 40 cycles of 95°C for 5 s, 60°C for 30 s [6]
- Cycling Conditions:
- Calculate ∆Ct values: ∆Ct = Ctreference – Cttarget. Use pre-defined cutoffs for subtype classification [35].
Table 2: RT-qPCR Targets for Breast Cancer Subtyping
| Gene | Protein | Role in Subtyping | PCR Efficiency (%) |
|---|---|---|---|
| ESR1 | ERα | Luminal subtype identification | 99.3 [6] |
| PGR | PR | Luminal differentiation | 101.8 [6] |
| ERBB2 | HER2 | HER2+ classification | 99.0 [6] |
| MKI67 | Ki-67 | Proliferation index (Luminal A/B) | 98.4 [6] |
Advanced Applications: miRNA Logic Platforms
Beyond CTCs, miRNA profiling enables subtype discrimination via DNA-based computational assays. The following workflow uses miR-21, miR-587, and miR-210 to generate binary codes for subtype classification [57]:
Diagram: miRNA Logic Platform for Subtyping
Table 3: miRNA Biomarkers and Subtype Correlations
| miRNA | Expression | Subtype Association |
|---|---|---|
| miR-21 | Upregulated in BC | Universal biomarker (initiates DNAzyme cleavage) [57] |
| miR-587 | Upregulated in Luminal/TNBC | Distinguishes Luminal from HER2+ [57] |
| miR-210 | Upregulated in TNBC | Metastatic subtype signature [57] |
Research Reagent Solutions
Table 4: Essential Tools for CTC and RT-qPCR Workflows
| Reagent/Kit | Function | Example Application |
|---|---|---|
| CellSearch System | CTC enumeration and isolation | Prognostic monitoring in breast cancer [55] |
| Xpert STRAT4 Assay | Automated RT-qPCR for ESR1/PGR/ERBB2/MKI67 | Rapid subtyping (<2 h) [35] |
| Quick-DNA/RNA FFPE Kit | RNA extraction from CTCs/FFPE samples | Pre-PCR molecular profiling [6] |
| DNAzyme Probes (miR-21) | miRNA detection via cleavage cascade | Binary coding for subtypes [57] |
Integrating CTC analysis with multiplex RT-qPCR provides a robust framework for dynamic biomarker assessment in breast cancer. Protocols outlined here enable researchers to correlate CTC-derived molecular data with standard subtyping paradigms, advancing therapeutic monitoring and drug development. Future directions include single-cell CTC sequencing and automated miRNA logic systems for real-time subtype tracking.
Maximizing Assay Performance: Troubleshooting and Advanced Optimization
Preventing Primer-Dimers and Non-Specific Amplification
In the molecular diagnosis of breast cancer, reverse transcription quantitative polymerase chain reaction (RT-qPCR) has emerged as a powerful technique for quantifying gene expression profiles critical for subtyping and treatment selection. The transition to multiplex RT-qPCR formats enables simultaneous detection of multiple biomarkers—including ESR, PGR, HER2, and Ki67—from limited patient samples, significantly enhancing diagnostic efficiency [6]. However, this advanced methodology introduces substantial technical challenges, primarily through primer-dimer formation and non-specific amplification, which can compromise assay accuracy, sensitivity, and reproducibility.
Primer-dimers are small, unintended DNA artifacts that form when primers anneal to each other rather than to the intended template DNA, creating free 3' ends that DNA polymerase can extend [58]. In multiplex assays where numerous primer sets coexist, the probability of these interactions increases exponentially, potentially depleting reaction reagents and generating false-positive signals [59] [60]. Similarly, non-specific amplification occurs when primers bind to non-target sequences, amplifying incorrect products and skewing quantification results. These artifacts are particularly problematic in clinical breast cancer diagnostics, where accurate quantification of biomarker expression levels directly impacts therapeutic decisions [6].
This application note provides detailed protocols and optimization strategies to effectively prevent primer-dimer formation and non-specific amplification in multiplex RT-qPCR assays, with specific application to breast cancer subtyping research.
Understanding Primer-Dimer Formation
Mechanisms of Primer-Dimer Artifacts
Primer-dimers form through two primary mechanisms: self-dimerization and cross-dimerization. Self-dimerization occurs when a single primer contains self-complementary regions, enabling it to fold back and anneal to itself. Cross-dimerization happens when forward and reverse primers, or primers from different assays in a multiplex reaction, contain complementary sequences that allow them to anneal to each other [58]. Both scenarios create partially double-stranded structures with free 3'-OH ends that DNA polymerase recognizes and extends, synthesizing short DNA fragments that amplify efficiently throughout PCR cycles.
In probe-based qPCR systems, particularly those using hydrolysis probes (e.g., TaqMan), primer-dimers may not generate significant fluorescent signal if they don't contain the probe binding sequence. However, they still consume essential reaction components—including primers, dNTPs, and polymerase—reducing the resources available for target amplification and potentially decreasing assay sensitivity [61] [62]. In dye-based systems (e.g., SYBR Green), primer-dimers bind the fluorescent dye and generate strong false-positive signals that can be misinterpreted as specific amplification [61].
Impact on Multiplex RT-qPCR Performance
In multiplex RT-qPCR for breast cancer subtyping, where several genetic biomarkers are simultaneously quantified from precious patient samples, primer-dimer formation poses several critical challenges:
- Resource Competition: Primer-dimers compete with legitimate targets for polymerase, nucleotides, and primers, potentially reducing amplification efficiency for low-abundance targets [59] [60]
- Signal Interference: In dye-based detection, primer-dimers contribute background fluorescence that obscures specific amplification signals [61]
- Reduced Dynamic Range: Non-specific products limit the maximum number of targets that can be reliably amplified in a single reaction [60]
- False Positives: Late-cycle amplification of primer-dimers can be misinterpreted as low-level target expression, potentially impacting clinical interpretation [62]
The complex nature of breast cancer biomarker panels, which often include reference genes and multiple therapeutic targets, creates an environment where cross-reactivity between numerous primer sets becomes increasingly likely [6].
Primer Design Strategies
Computational Design Principles
Effective primer design represents the first and most crucial defense against primer-dimer formation. Bioinformatic tools should be employed to ensure primers meet specific criteria that minimize off-target interactions.
Table 1: Optimal Primer Design Parameters for Multiplex RT-qPCR
| Parameter | Recommended Value | Rationale |
|---|---|---|
| Length | 18-25 nucleotides | Provides sufficient specificity while minimizing interaction opportunities [13] |
| GC Content | 40-60% | Balanced composition reduces secondary structure formation [13] |
| Melting Temperature (Tm) | 55-65°C | Enables specific annealing; <5°C variation between multiplexed primers [6] |
| 3'-End Complementarity | Avoid >3 bp matches | Prevents polymerase extension from primer-primer hybrids [58] [59] |
| Self-Complementarity | ΔG > -5 kcal/mol | Minimizes hairpin formation and self-dimerization [62] |
| Cross-Complementarity | ΔG > -8 kcal/mol | Reduces primer-primer interactions in multiplex reactions [59] |
Primers should be designed to span exon-exon junctions when possible, ensuring amplification of cDNA but not genomic DNA [13]. The amplicon size should ideally range between 70-200 base pairs for efficient amplification in multiplex reactions [13].
Advanced Primer Chemistry
Self-Avoiding Molecular Recognition Systems (SAMRS) incorporate modified nucleobases that pair with natural nucleotides but not with other SAMRS nucleotides. This technology significantly reduces primer-primer interactions while maintaining efficient priming with target templates [59]. Strategic placement of 2-4 SAMRS components near the 3' end of primers can dramatically decrease dimer formation without compromising amplification efficiency. For breast cancer biomarker panels, SAMRS-modified primers for highly homologous gene family members or sequences with high GC content can improve multiplexing capability and single-nucleotide polymorphism discrimination [59].
Optimization of Reaction Components
Primer and Probe Concentration Titration
Balancing primer and probe concentrations is critical in multiplex RT-qPCR to prevent resource competition and dimer formation. The optimal concentration must provide sufficient amplification efficiency while minimizing non-specific interactions.
Table 2: Component Optimization for Multiplex RT-qPCR
| Component | Standard Concentration | Optimized Concentration | Effect |
|---|---|---|---|
| Primers | 400 nM each | 133-213 nM | Reduces primer-dimer formation by limiting interaction opportunities [62] |
| Probes | 100-250 nM | 54-100 nM | Minimizes probe-probe interactions while maintaining signal detection [62] |
| MgSO₄ | 3-4 mM | 5-6 mM | Stabilizes specific primer-template interactions [62] |
| dNTPs | 200-400 µM | 200-300 µM | Prevents non-template extensions while maintaining amplification efficiency |
Implementing primer-limiting strategies for highly abundant targets (such as reference genes) can prevent them from outcompeting lower-abundance targets for reaction resources. This approach ensures balanced amplification across all targets in the multiplex reaction [60].
Enzyme and Buffer Selection
Hot-start DNA polymerases are essential for multiplex RT-qPCR assays, as they remain inactive until activated by high temperature, preventing enzymatic activity during reaction setup when primer-dimer formation is most likely [58]. These polymerases are typically engineered to activate at 95°C, ensuring no extension occurs during the primer annealing phase of initial cycles.
Buffer composition significantly impacts reaction specificity. Magnesium concentration optimization is particularly important, as Mg²⁺ serves as a essential cofactor for polymerase activity but can also stabilize non-specific primer interactions. The addition of specific additives such as betaine, DMSO, or formamide can help destabilize secondary structures and improve amplification efficiency for difficult templates [59].
Thermal Cycling Parameters
Temperature Optimization
Precise control of thermal cycling parameters is crucial for minimizing non-specific amplification in multiplex RT-qPCR.
Table 3: Thermal Cycling Optimization Parameters
| Parameter | Standard Conditions | Optimized Conditions | Benefit |
|---|---|---|---|
| Reverse Transcription | 50°C for 10 min [6] | 50°C for 10-15 min | Ensures complete cDNA synthesis |
| Initial Denaturation | 95°C for 2 min [6] | 95°C for 2-5 min | Completely denatures complex secondary structures |
| Annealing Temperature | 60°C [62] | 63-65°C | Increases stringency to prevent non-specific binding [62] |
| Annealing Time | 30-60 seconds | 15-30 seconds | Limits time for non-specific interactions |
| Extension Temperature | 60°C (combined) [62] | 72°C (separate) | Provides optimal polymerase activity |
| Cycle Number | 40-45 | 35-40 | Redplicates late-cycle dimer amplification |
The implementation of touchdown PCR protocols, where the annealing temperature is gradually decreased over initial cycles from a higher starting temperature (e.g., 70°C down to 63°C over 3-6 cycles), can significantly improve specificity by ensuring that the first amplification cycles—which have the greatest impact on final product yield—occur under high-stringency conditions [6].
Cycle Structure Modification
For complex multiplex panels, separating the annealing and extension phases (rather than using combined anneal/extend steps) can improve performance. This approach allows independent optimization of each stage: higher temperatures for specific primer binding during annealing, followed by optimal extension temperatures (typically 72°C) for polymerase activity [6].
Reducing the number of amplification cycles to 35-40, when possible, minimizes the amplification of primer-dimers and other non-specific products that typically appear in late cycles (Ct > 38) [62].
Experimental Design and Quality Control
Control Reactions
Incorporating appropriate control reactions is essential for identifying and troubleshooting primer-dimer formation in multiplex RT-qPCR assays.
- No-Template Controls (NTC): Contain all reaction components except template cDNA, specifically detecting primer-dimer formation and reagent contamination [58] [62]
- No-Reverse Transcription Controls (-RT): Contain RNA template without reverse transcriptase, detecting genomic DNA amplification
- Singleplex Controls: Each primer set run individually alongside multiplex reactions, helping identify problematic primer pairs
- Inter-Run Calibrators: Standardized cDNA samples included across multiple runs to assess technical variation [63]
Specificity Verification
Melt curve analysis following dye-based qPCR provides valuable information about reaction specificity by characterizing amplification products based on their melting temperatures (Tm). Specific products typically display sharp, single peaks at expected Tm values, while primer-dimers and other non-specific products show broader peaks at lower temperatures [61]. For probe-based multiplex assays where melt curve analysis isn't feasible, agarose gel electrophoresis can visualize amplification products, with primer-dimers typically appearing as smeared bands below 100 bp [58].
Application to Breast Cancer Subtyping
Multiplex Panel Design for Breast Cancer Biomarkers
In breast cancer subtyping, multiplex RT-qPCR panels typically include biomarkers for estrogen receptor (ESR1), progesterone receptor (PGR), HER2 (ERBB2), and proliferation markers (Ki67), along with reference genes (e.g., RPL13A, GAPDH) for normalization [6]. The high-stakes diagnostic nature of these assays demands rigorous optimization to prevent artifacts that could impact patient classification.
A validated approach employs a multiplexing strategy utilizing three reaction tubes per sample: the first assessing RPL13A, ESR1, PGR, and HER2; the second measuring Ki67 and RPL13A; and the third detecting RPL13A along with angiogenesis markers HIF1A, ANG, and VEGF [6]. This balanced distribution prevents resource competition while providing necessary controls.
Workflow Optimization
The following workflow diagram illustrates an optimized process for multiplex RT-qPCR in breast cancer subtyping:
Research Reagent Solutions
Table 4: Essential Research Reagents for Multiplex RT-qPCR in Breast Cancer Subtyping
| Reagent Category | Specific Examples | Function in Assay |
|---|---|---|
| Reverse Transcriptase | GoScript Reverse Transcriptase | Converts RNA to cDNA for amplification [61] |
| Hot-Start Polymerase | GoTaq Hot Start Polymerase | Prevents non-specific amplification during reaction setup [58] |
| Fluorescent Probes | TaqMan Hydrolysis Probes | Sequence-specific detection with 5' FAM/VIC reporters [61] [60] |
| Multiplex Master Mix | GoTaq Probe qPCR Master Mix | Optimized buffer for multiplex reactions [61] |
| Reference Assays | TaqMan Endogenous Controls | Normalization genes (RPL13A, GAPDH) [6] [64] |
| SAMRS Nucleotides | SAMRS-modified phosphoramidites | Reduce primer-primer interactions [59] |
Effective prevention of primer-dimer formation and non-specific amplification is achievable through integrated optimization of primer design, reaction components, and thermal cycling parameters. For breast cancer subtyping using multiplex RT-qPCR, these strategies ensure accurate quantification of critical biomarkers, enabling reliable molecular classification that informs therapeutic decisions. The protocols outlined in this application note provide a foundation for robust, reproducible multiplex assays suitable for both research and clinical applications.
Balancing Primer and Probe Concentrations for Multiplex Reactions
The precise molecular subtyping of breast cancer is a cornerstone of modern personalized treatment strategies. Immunohistochemistry (IHC), while the traditional gold standard, presents limitations including subjectivity, relatively slow turnaround times, and significant inter-observer variability, particularly for the Ki-67 proliferation marker [65]. Multiplex Reverse Transcription quantitative Polymerase Chain Reaction (RT-qPCR) has emerged as a powerful, objective alternative for quantifying the mRNA expression of key biomarkers—ESR1 (ER), PGR (PR), ERBB2 (HER2), and MKI67 (Ki-67)—enabling robust classification into intrinsic subtypes (Luminal A-like, Luminal B-like, HER2-positive, and Triple-negative) [65]. The success of this multiplexing approach hinges on the meticulous optimization of reaction components, most critically, the balancing of primer and probe concentrations. Improper concentrations can lead to primer-dimer formation, competitive inhibition between assays, and unequal amplification efficiencies, ultimately compromising data accuracy. This application note provides detailed protocols and data for balancing these concentrations within the specific context of a multiplex RT-qPCR assay for breast cancer subtyping, as validated in recent research [11] [6].
Key Principles for Primer and Probe Design
The foundation of an efficient multiplex assay is the careful design of its oligonucleotides. Adherence to the following principles ensures high specificity, sensitivity, and compatibility between the different primer-probe sets in a single reaction [66] [67].
- Melting Temperature (Tm) and Annealing: Primers should have an optimal Tm of 60–64°C, with the Tm values of the forward and reverse primers for any given assay not differing by more than 2°C. This ensures both primers bind to the target simultaneously and efficiently. The annealing temperature (Ta) of the PCR reaction should be set no more than 5°C below the lowest Tm of the primer pairs [66].
- Probe Characteristics: Hydrolysis probes (e.g., TaqMan) should have a Tm 5–10°C higher than the accompanying primers to ensure they are bound to the target before primer extension begins. The use of double-quenched probes is recommended to lower background fluorescence and increase signal, especially for longer probes [66].
- Specificity and Secondary Structures: Oligonucleotides must be screened for self-dimers, heterodimers, and hairpin structures. The free energy (ΔG) for any such secondary structures should be weaker (more positive) than –9.0 kcal/mol. Tools like the IDT OligoAnalyzer are essential for this analysis. Furthermore, a BLAST search should be performed to ensure primer and probe sequences are unique to the intended target [66] [67].
- Amplicon Length and Location: Amplicons of 70–150 base pairs are ideal for robust amplification from FFPE-derived RNA. When working with RNA, designing assays to span an exon-exon junction can prevent the amplification of genomic DNA contaminants [66].
The following workflow diagrams the critical steps from initial design to final optimization of a multiplex RT-qPCR assay.
Experimental Protocol: Establishing a 4-plex Assay for Breast Cancer Biomarkers
This protocol is adapted from a study that successfully developed a multiplex RT-qPCR assay for subtyping 61 breast cancer samples using the reference gene RPL13A [6]. The protocol employs a touch-down approach for accurate annealing and multiplexes ESR1, PGR, ERBB2, and the reference gene in a single reaction.
Reagent Setup and Master Mix Composition
The following table outlines the core components of the multiplex RT-qPCR master mix. The precise concentrations of primers and probes are the critical variables that require optimization.
Table 1: Master Mix Components for a Single-Plex vs. Multiplex Reaction
| Component | Single-Plex Reaction (Initial Testing) | 4-Plex Reaction (Optimized) | Notes and Function |
|---|---|---|---|
| 2x RT-qPCR Master Mix | 10 µL | 10 µL | Contains buffer, dNTPs, enzyme mix, and MgCl₂. |
| Forward Primer (each) | 0.2–1.0 µM (final) | 0.1–0.5 µM (final) | Start high for single-plex; reduce in multiplex to minimize competition. |
| Reverse Primer (each) | 0.2–1.0 µM (final) | 0.1–0.5 µM (final) | Concentration typically matches forward primer. |
| Probe (each) | 0.1–0.3 µM (final) | 0.1–0.2 µM (final) | Probe concentration is often lower than primers. |
| Template RNA | 1–100 ng | 1–100 ng | Use consistent input from FFPE-derived RNA. |
| PCR-grade Water | To 20 µL | To 20 µL | Adjust volume to final reaction volume. |
Step-by-Step Cycling Protocol
The thermal cycling profile below incorporates a touch-down step to enhance specificity in the multiplex setting [6].
- Reverse Transcription: 50°C for 10 minutes.
- Initial Denaturation: 95°C for 2 minutes.
- Touch-Down Phase (9 cycles):
- Denaturation: 95°C for 10 seconds.
- Annealing: Start at 70°C for 15 seconds, decreasing by 1°C per cycle to a final temperature of 63°C.
- Amplification Phase (40 cycles):
- Denaturation: 95°C for 5 seconds.
- Annealing/Extension: 60°C for 30 seconds (with fluorescence data collection).
This touch-down protocol was shown to consistently yield significantly lower Cycle Threshold (CT) values, indicating improved amplification efficiency [11] [6].
Data Analysis and Optimization Metrics
The performance of the balanced multiplex assay must be rigorously compared against established single-plex assays for each biomarker.
Table 2: Performance Comparison of Single-Plex vs. Optimized Multiplex Assay
| Gene Target | Single-Plex CT Mean | Multiplex CT Mean | ΔCT | Single-Plex Efficiency | Multiplex Efficiency | Key Observations |
|---|---|---|---|---|---|---|
| ESR1 | 25.5 | 25.8 | +0.3 | 99.3% | 98.9% | Minimal shift in CT; efficiency maintained. |
| PGR | 27.1 | 27.5 | +0.4 | 101.8% | 100.2% | Robust performance in multiplex. |
| ERBB2 | 24.2 | 24.9 | +0.7 | 99.0% | 98.5% | Slightly larger CT shift; may need probe conc. adjustment. |
| RPL13A (Ref) | 20.8 | 21.0 | +0.2 | 99.9% | 99.9% | Stable reference gene is critical for normalization. |
Interpretation of Results and Troubleshooting
- Acceptable Performance: A ΔCT of less than 1 cycle between single-plex and multiplex reactions, with a PCR efficiency between 90–110%, is generally considered excellent [65] [67]. The data in Table 2 demonstrates a well-balanced assay.
- Correcting Imbalances: If one assay shows a significantly higher ΔCT (>1.5 cycles) or a drop in efficiency, systematically adjust the concentration of its primers and probe. Slightly increasing the concentration of the underperforming assay can improve its signal.
- Addressing Nonspecific Amplification: If amplification curves are irregular or there is high background, consider increasing the annealing temperature slightly or re-evaluating oligonucleotide sequences for specificity.
The relationship between primer and probe concentrations and the resulting CT values and efficiencies must be carefully analyzed to achieve a balanced multiplex assay.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of this protocol relies on specific reagents and tools. The following table lists essential materials, drawing from the cited studies and commercial best practices.
Table 3: Essential Research Reagents and Tools
| Item | Function/Description | Example from Literature/Suppliers |
|---|---|---|
| FFPE RNA Extraction Kit | Isolates high-quality RNA from formalin-fixed, paraffin-embedded tumor samples. The RNXtract kit was used in the MammaTyper validation study [65]. | Zymo Quick-DNA/RNA FFPE Kit [6], RNXtract Kit [65] |
| One-Step RT-qPCR Master Mix | An optimized buffer containing reverse transcriptase, DNA polymerase, dNTPs, and MgCl₂ for combined cDNA synthesis and amplification. | Applied Biosystems TaqMan, Roche Probes Master |
| Hydrolysis Probes | Double-quenched probes (e.g., with ZEN/TAO internal quencher) are recommended for lower background and higher signal-to-noise ratio in multiplex reactions [66]. | IDT PrimeTime, Thermo Fisher Scientific TaqMan |
| Validated Primer-Probe Sets | Pre-designed or custom-designed oligonucleotides for ESR1, PGR, ERBB2, MKI67, and stable reference genes (e.g., RPL13A). | The MammaTyper CE-IVD assay provides validated sequences [65]. |
| Real-time PCR Instrument | A thermal cycler with multi-channel fluorescence detection capable of running 96-, 384-, or 1536-well plates. | Applied Biosystems Viia 7, Roche LightCycler 480, Bio-Rad CFX [68] |
| Oligo Design & Analysis Tools | Free online software for calculating Tm, checking for secondary structures, and ensuring specificity. | IDT OligoAnalyzer, PrimerQuest [66] |
The strategic balancing of primer and probe concentrations is not merely a technical step but a fundamental requirement for generating reliable, quantitative data in multiplex RT-qPCR. The protocols and data presented here, contextualized within the framework of breast cancer molecular subtyping, provide a validated roadmap for researchers to develop robust assays. By adhering to these detailed design principles, optimization strategies, and validation metrics, scientists and drug development professionals can implement this powerful technique to achieve precise, objective, and high-throughput classification of breast cancer subtypes, thereby directly informing personalized therapeutic strategies [11] [6] [65].
Within breast cancer research, the drive towards personalized medicine makes the accurate molecular subtyping of tumors more critical than ever. Multiplex reverse transcription quantitative PCR (RT-qPCR) has emerged as a powerful tool for this purpose, enabling the simultaneous quantification of multiple biomarker genes, such as HER2, ESR, and PGR, from clinical samples [9]. However, the reliability of this technique is profoundly affected by the quality of the starting template. Challenging templates, characterized by high GC-rich content or derived from low-quality RNA commonly obtained from formalin-fixed paraffin-embedded (FFPE) tissues, can introduce significant inaccuracies. These inaccuracies compromise gene expression data and subsequently hinder correct cancer subtyping and treatment decisions. This application note provides detailed protocols and optimized strategies to overcome these specific challenges, ensuring robust and reliable multiplex RT-qPCR results in a breast cancer research context.
Understanding the Challenges
The Impact of GC-Rich Content
GC-rich sequences (GC content >60%) pose a significant challenge in RT-qPCR due to their propensity to form stable secondary structures and intra-molecular hydrogen bonds. These structures impede the progression of both the reverse transcriptase and the DNA polymerase enzymes, leading to inefficient cDNA synthesis, delayed quantification cycles (Cq), reduced amplification efficiency, and in severe cases, complete amplification failure. In the context of breast cancer subtyping, where the precise quantification of a panel of genes is crucial, such inefficiencies can skew expression ratios and lead to misinterpretation.
Consequences of Low RNA Quality
RNA integrity is a foundational pillar for accurate gene expression analysis. Clinical samples, particularly FFPE tissues, often yield partially degraded RNA and contain co-purified inhibitors of enzymatic reactions. The use of such compromised RNA results in poor conversion rates during reverse transcription, generating incomplete or low-yield cDNA templates [69]. This directly translates to a loss of sensitivity, as low-abundance transcripts may fall below the detection limit. Consequently, the resulting gene expression profiles do not accurately represent the tumor's molecular state, jeopardizing the validity of the cancer subtype assignment.
Optimized Experimental Protocols
Protocol 1: Optimized Workflow for GC-Rich Templates
This protocol is designed to denature stable secondary structures in GC-rich regions, ensuring efficient reverse transcription and PCR amplification.
Materials:
- Template: Total RNA or enriched mRNA.
- Enzymes: One-step RT-qPCR kit (e.g., Luna Universal Probe One-Step RT-qPCR Kit, NEB #E3006) or separate RT and qPCR kits.
- Additives: PCR additives such as GC-Rich Enhancer (e.g., from QIAGEN), Dimethyl sulfoxide (DMSO), or Betaine.
- Primers: Sequence-specific primers designed with stringent criteria.
Procedure:
- Primer Design: Design primers to amplify a short product (70–200 bp) with an optimal GC content of 40–60% [70]. Avoid repetitive sequences and significant secondary structures.
- Additive Optimization: Prepare a master mix containing the recommended components of your RT-qPCR kit. Aliquot the master mix and supplement with different additives:
- Condition A: No additive (control).
- Condition B: 5% DMSO (v/v).
- Condition C: 1 M Betaine.
- Condition D: 1X GC-Rich Enhancer.
- Touch-Down PCR: Utilize a touch-down cycling protocol to enhance specificity [9]. The protocol should start with an initial denaturation at 95°C for 2 minutes, followed by 5 cycles of denaturation at 95°C for 30 seconds, annealing starting at 65°C for 45 seconds (decreasing by 1°C per cycle), and extension at 72°C for 30 seconds. This is followed by 40 cycles of a standard cycling protocol (e.g., 95°C for 15s, 60°C for 45s).
- Analysis: Evaluate the Cq values, amplification efficiency, and linearity (R²) for each condition. Select the additive that yields the lowest Cq and an efficiency closest to 100%.
The following workflow summarizes the key steps for this protocol:
Protocol 2: Rescue Strategy for Low-Quality RNA
This protocol focuses on maximizing the amount of usable cDNA synthesized from degraded or inhibitor-containing RNA samples.
Materials:
- RNA Samples: Total RNA, accurately quantified and integrity-assessed (e.g., via RIN).
- DNase I: (e.g., NEB #M0303) to remove genomic DNA contamination [70].
- Reverse Transcriptase: A robust enzyme, such as M-MuLV or a WarmStart variant, capable of functioning at higher temperatures.
- Priming Strategy: A mixture of random hexamers and oligo-dT primers for comprehensive cDNA synthesis.
Procedure:
- RNA Assessment and Treatment: Quantify RNA using a fluorometric method for accuracy. Treat all samples with DNase I to eliminate genomic DNA.
- Input Optimization: Perform a linearity test. Prepare a 5-point serial dilution (e.g., 100 ng/µL to 1 ng/µL) of a representative RNA sample. Convert each dilution to cDNA in individual RT reactions using a kit that employs a mixture of random hexamers and oligo-dT primers [69].
- Enhanced Reverse Transcription: Increase the reverse transcription temperature. For the Luna RT, the default is 55°C, but it can be increased to 60°C for 10 minutes to improve performance on templates with complex secondary structures [70].
- Validation with qPCR: Amplify the resulting cDNAs using qPCR assays for your target genes (e.g., HER2, ESR) and a stable reference gene (e.g., RPL13A). Use an absolute quantification (standard curve) template in the analysis software to assess the linearity of RT efficiency across the dilution series for all genes [69].
- Define Optimal Range: The optimal RNA input is the highest concentration within the linear range for both reference and target genes. If linearity is lost at high concentrations, use a lower input amount.
The decision-making process for handling low-quality RNA is outlined below:
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and their optimized applications for managing challenging templates in multiplex RT-qPCR.
Table 1: Research Reagent Solutions for Challenging RT-qPCR Templates
| Item | Function/Application in Protocol | Optimization Tip |
|---|---|---|
| One-Step RT-qPCR Kit (e.g., Luna) | Integrated reverse transcription and amplification in a single tube, reducing hands-on time and contamination risk. | For GC-rich targets, use the included WarmStart feature and supplement with additives like DMSO or Betaine. |
| PCR Additives (DMSO, Betaine, GC-Rich Enhancer) | Disrupt secondary structures, lower the melting temperature of GC-rich duplexes, and improve polymerase processivity. | Titrate concentration (e.g., 2-10% DMSO) to avoid inhibition; test in a panel to find the optimal additive for your target. |
| High-Temperature Reverse Transcriptase (e.g., WarmStart Luna RT) | Synthesizes cDNA at elevated temperatures (up to 60°C), helping to denature RNA secondary structures that impede the enzyme. | Use a priming strategy with a mix of random hexamers and oligo-dT for comprehensive coverage of both normal and fragmented RNA. |
| DNase I (RNase-free) | Degrades contaminating genomic DNA prior to RT-qPCR, preventing false-positive amplification and inaccurate Cq values. | Include a dedicated control reaction without reverse transcriptase (-RT control) to confirm the absence of genomic DNA amplification. |
| Stable Reference Genes (e.g., RPL13A) | Used for normalization of gene expression data; their stable expression is critical for accurate relative quantification. | For breast cancer subtyping, validate reference gene stability (e.g., using geNorm or NormFinder) across all sample types and conditions [9]. |
Data Presentation and Analysis
Rigorous validation of the optimized protocols is essential. The following table summarizes the key quantitative parameters that must be assessed to ensure a robust assay.
Table 2: Key Quantitative Parameters for Assay Validation
| Parameter | Target Value | Importance & Calculation |
|---|---|---|
| Amplification Efficiency (E) | 90–110% (Ideal: 100 ± 5%) [71] [70] | Calculated from the slope of the standard curve: E = (10^(-1/slope) - 1) * 100%. Ensures the 2^(-ΔΔCt) method can be reliably used. |
| Linearity (R²) | ≥ 0.99 [71] [70] | The coefficient of determination from a standard curve of serial template dilutions. Indicates a highly linear and predictable reaction over a wide dynamic range. |
| Threshold Cycle (Cq) | Varies by target abundance | The cycle number at which amplification enters the exponential phase. Consistent Cq values in singleplex vs. multiplex reactions indicate good multiplexing compatibility. |
| Optimal RNA Input | Sample-dependent (e.g., 10-100 ng) | Determined via a linearity test. The maximum RNA amount that maintains linear RT efficiency for both high- and low-abundance genes [69]. |
The success of multiplex RT-qPCR in advanced breast cancer diagnosis and research hinges on overcoming the technical hurdles posed by challenging templates [9]. By implementing the detailed protocols outlined here—specifically addressing GC-rich content through specialized additives and touch-down PCR, and rescuing low-quality RNA via input optimization and enhanced reverse transcription—researchers can achieve the high levels of efficiency, specificity, and sensitivity required. This ensures that the resulting gene expression data for critical biomarkers like HER2, ESR, and PGR is reliable, enabling precise tumor subtyping and contributing to the development of personalized therapeutic strategies.
Incorporating Hot-Start Enzymes and Additives (DMSO, BSA) for Enhanced Specificity
Within the framework of thesis research focused on advancing multiplex RT-qPCR for the precise subtyping of breast cancer, the optimization of reaction specificity and efficiency is paramount. The simultaneous detection of multiple gene markers—such as ESR1, PGR, ERBB2 (HER2), and MKi67—from limited patient RNA samples presents significant challenges, including primer-dimer formation, non-specific amplification, and assay inhibition [11] [9]. This Application Note details a optimized protocol that leverages Hot-Start enzymes and key reaction additives, Dimethyl Sulfoxide (DMSO) and Bovine Serum Albumin (BSA), to overcome these hurdles. The methodologies described herein are designed to integrate seamlessly into breast cancer research pipelines, enabling robust, reproducible, and highly specific gene expression profiling that can complement or even streamline traditional immunohistochemistry (IHC) [11].
Background and Principles
The Role of Hot-Start Enzymes in Multiplex RT-qPCR
Hot-Start DNA polymerases are engineered to remain inactive at ambient temperatures until a high-temperature activation step is applied. This feature is critical in multiplex RT-qPCR because it prevents primer-dimer formation and mis-priming during reaction setup and the initial, low-temperature reverse transcription phase. By curtailing non-specific activity prior to the thermal cycling, Hot-Start enzymes significantly enhance the specificity and yield of the intended amplicons, which is especially crucial when amplifying multiple targets from scarce RNA samples [72].
Novel enzyme engineering further expands these capabilities. For instance, a novel Taq DNA polymerase variant was engineered to possess inherent reverse transcriptase activity, enabling single-enzyme, one-tube RT-qPCR. This innovation eliminates the need for viral reverse transcriptases and simplifies reaction assembly, thereby reducing the risk of contamination and streamlining the workflow for molecular diagnostics [73].
Mechanism of Action of Key Additives
DMSO (Dimethyl Sulfoxide): DMSO is a polar aprotic solvent that enhances reaction specificity by reducing the stability of secondary structures in DNA and RNA templates. It does so by disrupting base pairing, which facilitates primer annealing to the intended target sequences. This is particularly beneficial for amplifying GC-rich regions, such as those found in certain promoter or coding sequences. In the context of cancer research, DMSO has also been documented to modulate gene expression, including the upregulation of the tumor suppressor HLJ1 via AP-1 activation, underscoring its bioactivity beyond a mere reaction additive [74].
BSA (Bovine Serum Albumin): BSA functions as a non-specific protein competitor in PCR mixes. It binds to and neutralizes a range of inhibitors that may be co-extracted with nucleic acids from biological samples, such as polyphenols, polysaccharides, and proteases. By sequestering these inhibitors, BSA safeguards the activity of DNA polymerases and reverse transcriptases, ensuring maximal enzymatic efficiency and reliable amplification. Studies have demonstrated that BSA can completely restore a positive RT-qPCR signal in reactions that were otherwise inhibited by compounds found in produce rinsates, and its utility extends to reactions for detecting foodborne viruses and in advanced PCR techniques [75] [72].
Application Notes for Breast Cancer Subtyping
Experimental Design and Workflow
The following diagram illustrates the optimized workflow for a multiplex RT-qPCR assay designed for breast cancer subtyping, highlighting critical steps where Hot-Start enzymes and additives are incorporated to enhance performance.
Key Research Reagent Solutions
The successful implementation of this optimized protocol relies on a set of key reagents, each fulfilling a specific function to ensure assay robustness.
Table 1: Essential Research Reagents for Optimized Multiplex RT-qPCR
| Reagent | Function & Rationale | Exemplary Use Case |
|---|---|---|
| Hot-Start Taq DNA Polymerase | Suppresses non-specific amplification during reaction setup; essential for multiplexing. | One-tube RT-qPCR with novel engineered variants [73]. |
| BSA (Bovine Serum Albumin) | Binds and neutralizes PCR inhibitors; stabilizes enzymes. | Restoring detection sensitivity in inhibited reactions [75]. |
| DMSO (Dimethyl Sulfoxide) | Disrupts RNA secondary structures; improves primer annealing specificity. | Amplification of GC-rich target sequences [74]. |
| Multiplex PCR Probe Mix | Allows simultaneous detection of multiple targets with different fluorescent labels. | Subtyping using ESR1, PGR, ERBB2, MKi67 [11] [9]. |
| Nuclease-free Water | Serves as a reaction solvent; ensures an RNase-/DNase-free environment. | Diluent for all reaction components. |
Detailed Experimental Protocols
Protocol 1: One-Step Multiplex RT-qPCR for Gene Expression Profiling
This protocol is designed for the simultaneous reverse transcription and amplification of multiple breast cancer biomarker genes from total RNA in a single tube.
Materials:
- RNA Template: 10-100 ng total RNA from breast cancer tissue or cell lines.
- Enzyme: Hot-Start Taq DNA polymerase with reverse transcriptase activity [73].
- Primers/Probes: Primer sets and differentially labelled hydrolysis probes (e.g., FAM, HEX, Cy5) for ESR1, PGR, ERBB2, MKi67, and an endogenous control (e.g., RPL13A) [11] [9].
- Reaction Buffer: Commercial 2x RT-qPCR buffer or custom buffer.
- Additives: Molecular biology-grade DMSO and BSA (e.g., 20 mg/mL stock).
- Equipment: Real-time PCR instrument.
Procedure:
- Master Mix Preparation (on ice): For a single 20 µL reaction, combine the following components in the order listed:
- 10.0 µL of 2x Reaction Buffer
- 2.0 µL of 10x Primer/Probe Mix (containing all primers and probes)
- 1.0 µL of DMSO (final concentration 5% v/v)
- 0.5 µL of BSA (20 mg/mL stock, final concentration 0.5 mg/mL)
- 1.0 µL of Hot-Start Enzyme Mix (with RT activity)
- 1.0 µL of RNA Template (10-100 ng)
- 4.5 µL of Nuclease-free Water
- Thermal Cycling: Load the plate into the real-time PCR instrument and run the following program:
- Reverse Transcription: 50°C for 15-30 minutes.
- Initial Denaturation/Enzyme Activation: 95°C for 2-5 minutes.
- Amplification (45 cycles):
- Denature: 95°C for 15 seconds.
- Anneal/Extend: 60°C for 60 seconds (acquire fluorescence at this step).
- Hold: 4°C forever.
Protocol 2: Two-Step Multiplex RT-qPCR with Pre-Optimized cDNA
This protocol is recommended when the same cDNA sample will be used for multiple, separate qPCR assays.
Procedure:
- cDNA Synthesis (First Step):
- In a nuclease-free tube, set up a reverse transcription reaction containing total RNA, a reverse transcriptase, and an oligo(dT) and/or random hexamer primer mix according to the manufacturer's instructions.
- Incubate at the recommended temperature (e.g., 37-50°C for 60 minutes), followed by an enzyme inactivation step (e.g., 85°C for 5 minutes). The synthesized cDNA can be stored at -20°C.
- Multiplex qPCR (Second Step):
- For a single 20 µL reaction, combine:
- 10.0 µL of 2x Hot-Start PCR Master Mix
- 2.0 µL of 10x Multiplex Primer/Probe Mix
- 1.0 µL of DMSO (5%)
- 0.5 µL of BSA (0.5 mg/mL)
- 2.0 µL of cDNA (diluted 1:5 to 1:10)
- 4.5 µL of Nuclease-free Water
- Run the following thermal cycling protocol:
- Initial Denaturation: 95°C for 2 minutes.
- 45 Cycles of: 95°C for 15 sec, 60°C for 60 sec (with fluorescence acquisition).
- For a single 20 µL reaction, combine:
Data Analysis and Optimization
Quantitative Effects of Additives on PCR Performance
Systematic optimization of additive concentrations is critical. The following table summarizes typical effects and optimal concentration ranges for DMSO and BSA based on empirical data.
Table 2: Quantitative Effects of Additives on qPCR Performance
| Additive | Recommended Concentration | Impact on Ct Value | Effect on Amplicon Specificity | Considerations |
|---|---|---|---|---|
| DMSO | 2-10% (v/v) | Can reduce Ct by 1-3 cycles for GC-rich templates [74]. | Markedly improves; suppresses spurious bands. | >10% can inhibit Taq polymerase activity. |
| BSA | 0.1-0.5 mg/mL | Can restore amplification in inhibited samples (Ct shift from undetectable to ~32) [75]. | Minor direct effect, but improves specificity by mitigating inhibition. | Higher concentrations may increase background fluorescence. |
Troubleshooting Common Issues
- Loss of Signal or High Ct Values in Multiplex: Suspect inhibitor carryover. Solution: Increase the concentration of BSA to 0.5 mg/mL and ensure the use of a robust Hot-Start polymerase [75].
- Non-Specific Amplification or Primer-Dimer: This indicates inadequate "hot-start" conditions or suboptimal primer design. Solution: Verify the enzyme's Hot-Start mechanism. Titrate DMSO concentration (3-7%) and optimize the annealing temperature using a gradient PCR [74].
- Poor Resolution in Multiplex Curves: This occurs when signals from different dyes overlap. Solution: Check for spectral crosstalk calibration on your instrument and ensure probe labels are well-spaced in the emission spectrum.
The strategic incorporation of Hot-Start enzymes, DMSO, and BSA provides a powerful, synergistic approach to enhancing the specificity, sensitivity, and reliability of multiplex RT-qPCR assays. For thesis research focused on breast cancer subtyping, this optimized protocol offers a robust molecular tool that can deliver precise gene expression data for critical biomarkers. The methodologies outlined—from experimental design and reagent selection to detailed protocols and troubleshooting—provide a solid foundation for generating high-quality data. This contributes significantly to the broader goal of refining diagnostic accuracy and paving the way for personalized therapeutic strategies in breast cancer.
Strategies for Cross-Contamination Prevention and Assay Reproducibility
Multiplex reverse transcription quantitative polymerase chain reaction (RT-qPCR) has emerged as a powerful tool in molecular diagnostics and research, particularly for breast cancer subtyping. This technique enables simultaneous quantification of multiple gene targets—such as ESR1, PGR, ERBB2 (HER2), and MKi67—from limited patient samples, facilitating rapid molecular classification into luminal A-like, luminal B-like, HER2-positive, and triple-negative subtypes [6] [35]. However, the extreme sensitivity of RT-qPCR that makes it invaluable for detecting low-abundance transcripts also renders it highly vulnerable to contamination, potentially compromising assay reproducibility and clinical reliability.
In breast cancer research, where treatment decisions may hinge on precise molecular subtyping, false-positive results from carryover contamination or false negatives from reaction inhibition can directly impact experimental conclusions and their potential translational value. This application note details comprehensive strategies to mitigate contamination risks and enhance reproducibility in multiplex RT-qPCR workflows, with specific consideration for breast cancer subtyping applications.
Contamination in multiplex RT-qPCR workflows originates from several key sources, each requiring specific intervention strategies:
Amplicon Carryover Contamination: Amplified DNA fragments from previous PCR reactions represent the most significant contamination source in established laboratories. A single opened tube containing PCR amplicons can release millions of aerosolized copies into the laboratory environment, contaminating reagents, equipment, and subsequent reactions [76] [77]. This is particularly problematic in breast cancer subtyping where the same gene targets are repeatedly amplified across numerous patient samples.
Sample Cross-Contamination: During RNA extraction and reaction setup, cross-contamination between samples can occur, especially when processing multiple patient specimens concurrently. This risk escalates in high-throughput diagnostic settings where dozens of samples are processed daily [77].
Reagent Contamination: Enzymes, primers, probes, and water can become contaminated with nucleic acids from the manufacturing process or laboratory environment. For instance, recombinant enzymes produced in bacterial systems may contain trace bacterial DNA that could interfere with certain targets [77].
Environmental Contamination: Laboratory surfaces, equipment, and ventilation systems can accumulate amplified DNA over time, creating persistent contamination reservoirs [76].
Impact on Breast Cancer Subtyping
Contamination directly impacts the reliability of breast cancer molecular subtyping:
- False Positives: Contamination with target amplicons or positive controls can lead to misclassification of hormone receptor status, potentially directing patients toward ineffective endocrine therapies [35].
- False Negatives: Reaction inhibition from contaminating substances can suppress amplification, potentially resulting in false-negative results for critical markers like HER2 [77].
- Reduced Assay Reproducibility: Contamination contributes to inter-laboratory variability, undermining the consistency of research findings across institutions [35].
Table 1: Common Contamination Sources and Their Impacts on Breast Cancer Research
| Contamination Source | Result | Potential Impact on Breast Cancer Subtyping |
|---|---|---|
| Amplified DNA from previous reactions | False positives | Misclassification of hormone receptor status |
| Inhibitors carried over during sample preparation | False negatives | Underestimation of HER2 expression |
| Contaminated reagents | All reactions affected | Compromised batch of patient samples |
| Cross-contamination between samples | Erroneous results in specific samples | Incorrect molecular subtyping for individual patients |
| Bacterial DNA in enzyme preparations | Background signal | Reduced assay sensitivity for low-abundance targets |
Physical and Procedural Contamination Control Strategies
Laboratory Design and Workflow Separation
Implementing strict physical separation of PCR workflow stages is fundamental to contamination prevention:
Dedicated Pre- and Post-Amplification Areas: Establish physically separated laboratory areas for pre-amplification (reagent preparation, RNA extraction, reaction setup) and post-amplification (product analysis) procedures. Ideally, these areas should be in separate rooms with independent equipment, supplies, and ventilation systems [76].
Unidirectional Workflow: Maintain a one-way workflow from clean pre-amplification areas to post-amplification areas. Personnel should not return to pre-amplification areas after working in post-amplification spaces without changing protective equipment and decontaminating themselves [76].
Dedicated Equipment and Supplies: Assign separate pipettes, centrifuges, vortexers, and other equipment to each area. Use aerosol-resistant filter tips exclusively in pre-amplification areas to prevent aerosol contamination of pipette shafts [76].
Personal Protective Equipment and Technique
Proper Glove Usage: Change gloves frequently, especially when moving between workstations or after potential contamination events. Contaminated gloves can transfer amplification products to surfaces, reagents, and equipment [76].
Careful Tube Handling: Open tubes carefully with a deliberate technique to minimize aerosol generation. Keep tubes capped as much as possible during procedures and dispose of amplified products in dedicated, contained areas [76].
Workspace Organization: Arrange workstations to separate clean reagents from samples and amplified products. Use dedicated benchtop protectors for different workflow stages and decontaminate surfaces between procedures.
Technical and Reagent-Based Contamination Control
Enzymatic Contamination Prevention
The Uracil-N-Glycosylase (UNG) system provides robust protection against carryover contamination from previous PCR amplifications:
Mechanism of Action: UNG enzymatically degrades DNA containing uracil bases while leaving thymine-containing DNA intact. In this system, dTTP in the PCR master mix is replaced with dUTP, resulting in amplification products that incorporate uracil instead of thymine. Prior to each PCR amplification, UNG incubation at room temperature degrades any uracil-containing contaminants from previous reactions. The enzyme is then inactivated during the initial denaturation step, allowing normal amplification of the current reaction with dUTP incorporation [76] [78].
Implementation Considerations:
- UNG effectively degrades most carryover contamination but works best with thymine-rich (adenine-rich template) amplification products [76].
- The system requires using dUTP in all reactions to ensure contaminants are labeled with uracil.
- UNG is ineffective against contamination sources that don't contain uracil, such as genomic DNA or synthetic oligonucleotides [76].
Reagent Management and Quality Control
Aliquoting Strategies: Aliquot reagents such as primers, probes, enzymes, and master mixes into single-use volumes to prevent repeated freeze-thaw cycles and minimize contamination risk from repeated sampling [76].
Reagent Quality Verification: Source reagents from reputable manufacturers who implement contamination control during production. For critical applications, screen new reagent lots for contamination before putting them into use [77].
Nuclease-Free Water: Use molecular biology-grade nuclease-free water for all reagent preparations and reaction setups. Periodically test water stocks for contamination.
Multiplex RT-qPCR Optimization for Enhanced Reproducibility
Primer and Probe Design Considerations
Robust multiplex assays require careful primer and probe design to ensure compatibility and specific amplification:
Design Parameters: Aim for primers between 18-30 bases with optimal melting temperatures (Tm) of 60-64°C and GC content of 35-65%. Primers in a set should have Tm values within 2°C of each other [66]. Probes should have Tm values 5-10°C higher than the corresponding primers [66].
Specificity Validation: Screen all primer and probe sequences against relevant databases using BLAST analysis to ensure specificity for intended targets and minimize off-target binding [66]. This is particularly important for breast cancer subtyping where homologous genes or pseudogenes may exist.
Compatibility Testing: Systematically test primer-primer interactions to avoid dimer formation that can reduce amplification efficiency. Use tools like OligoAnalyzer to evaluate ΔG values for potential heterodimers and hairpins [66].
Table 2: Multiplex RT-qPCR Optimization Parameters for Breast Cancer Subtyping
| Parameter | Optimal Range | Considerations for Breast Cancer Subtyping |
|---|---|---|
| Primer Length | 18-30 bases | Sufficient for specificity without excessive length |
| Primer Tm | 60-64°C | Ensure compatibility within multiplex set |
| Probe Tm | 5-10°C higher than primers | Prevents probe displacement during amplification |
| GC Content | 35-65% | Balance between specificity and melting behavior |
| Amplicon Size | 70-150 bp | Compatible with degraded FFPE RNA samples |
| Primer Concentration | 200 nM (initial testing) | May require adjustment for balanced amplification |
Assay Validation and Quality Controls
Implement comprehensive control systems to monitor assay performance and detect contamination:
No Template Controls (NTCs): Include NTCs containing all reaction components except template nucleic acid in every run. Amplification in NTCs indicates contamination requiring investigation [76] [77].
Positive Controls: Use well-characterized control templates to verify reaction efficiency and detect inhibition. In breast cancer subtyping, cell lines with known molecular subtypes make excellent positive controls [77].
Internal Controls: Incorporate endogenous reference genes (e.g., RPL13A, CYFIP1) to monitor RNA quality and reverse transcription efficiency [6] [35]. Some protocols also include exogenous internal controls to detect amplification inhibition.
Standard Curves: Generate standard curves using serial dilutions of control templates to calculate amplification efficiency, which should ideally fall between 90-110% [71].
Surface Decontamination and Equipment Maintenance
Routine Decontamination Procedures
Bleach-Based Decontamination: Regularly clean work surfaces and equipment with fresh 10-15% bleach solution (sodium hypochlorite), allowing 10-15 minutes contact time before wiping with deionized water or 70% ethanol [76]. Bleach effectively degrades DNA through oxidative damage.
Ethanol Cleaning: Use 70% ethanol for routine cleaning of surfaces and equipment before and after use. While less effective than bleach for nucleic acid degradation, ethanol helps remove contaminants and reduce bioburden [76].
Equipment-Specific Protocols: Pay special attention to centrifuges, vortexers, and pipettes that are prone to contamination. Regularly decontaminate water baths, ice buckets, and tube racks.
UV Irradiation
Use UV light in biological safety cabinets and dedicated workstations to crosslink any contaminating DNA before setting up critical reactions. Note that UV effectiveness decreases with short amplicons (<300 bp) and GC-rich sequences [77].
Experimental Workflow for Breast Cancer Subtyping
The following diagram illustrates a comprehensive workflow for breast cancer subtyping using multiplex RT-qPCR that incorporates contamination control measures at each stage:
Figure 1: Comprehensive workflow for breast cancer subtyping using multiplex RT-qPCR with integrated contamination control measures. The strict physical separation between pre- and post-amplification areas is critical for preventing amplicon carryover contamination.
The Scientist's Toolkit: Essential Reagents and Controls
Table 3: Research Reagent Solutions for Contamination-Free Multiplex RT-qPCR
| Reagent/Category | Specific Examples | Function in Contamination Control |
|---|---|---|
| UNG/dUTP Systems | Thermolabile UDG, UNG Master Mixes | Prevents carryover contamination from previous amplifications |
| Master Mixes | LuminoCt ReadyMix, Luna Universal One-Step RT-qPCR Kit | Provides optimized buffer conditions and enzyme blends for multiplexing |
| Nucleic Acid Purification Kits | Quick-DNA/RNA FFPE Kit, Xpert FFPE Lysis Kit | Efficient extraction while minimizing cross-contamination between samples |
| Aerosol-Resistant Tips | Filtered pipette tips | Prevents aerosol contamination of pipette shafts |
| Decontamination Reagents | 10-15% bleach solution, 70% ethanol, DNA degradation solutions | Eliminates contaminating nucleic acids from surfaces and equipment |
| Control Templates | Synthetic gene fragments, cell line RNA with known subtype | Verifies assay performance and detects inhibition |
| Reference Genes | RPL13A, CYFIP1, GAPDH | Monitors RNA quality and reverse transcription efficiency |
Implementing comprehensive contamination control strategies is essential for maintaining the reproducibility and reliability of multiplex RT-qPCR in breast cancer subtyping research. A multi-layered approach combining physical separation, procedural discipline, technical solutions like UNG, and rigorous quality controls provides the most effective defense against contamination. As molecular subtyping continues to guide personalized treatment approaches in breast cancer, ensuring the accuracy of these assays through proper contamination control becomes increasingly critical to research integrity and, ultimately, patient care.
Clinical Validation and Comparative Analysis with Existing Technologies
Within breast cancer research and molecular diagnostics, accurate subtyping is paramount for guiding personalized treatment strategies. Immunohistochemistry (IHC) and Fluorescence In Situ Hybridization (FISH) represent the established standard techniques for determining the status of key biomarkers: estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and the proliferation marker Ki67 [7] [79]. However, these methods present challenges, including subjectivity in interpretation, inter-observer variability, and standardization difficulties, particularly for Ki67 [7] [5]. Multiplex Reverse Transcription quantitative Polymerase Chain Reaction (RT-qPCR) has emerged as a powerful, quantitative alternative for profiling gene expression. This document details application notes and protocols for conducting robust concordance studies to benchmark RT-qPCR methodologies against traditional IHC and FISH, providing a critical framework for researchers and drug development professionals engaged in the validation of molecular subtyping assays.
Data from multiple studies demonstrate a high degree of concordance between RT-qPCR and conventional protein-based or gene amplification assays. The table below summarizes key performance metrics across different biomarkers from recent investigations.
Table 1: Concordance Rates Between RT-qPCR and IHC/FISH for Key Breast Cancer Biomarkers
| Biomarker | RT-qPCR Target | Concordance with IHC/FISH | Area Under Curve (AUC) | Sample Size (n) | Citation |
|---|---|---|---|---|---|
| ER | ESR1 | 94.4% (Training Set)81.3% (Validation Set) | 0.99 | 323 | [7] [80] |
| PR | PGR | 88.0% (Training Set)78.3% (Validation Set) | 0.95 | 323 | [7] [80] |
| HER2 | ERBB2 | 89.4% (Training Set)80.4% (Validation Set) | 0.99 | 323 | [7] [80] |
| Ki67 | MKi67 | 67.8% (Training Set)69.1% (Validation Set) | 0.85 | 323 | [7] [80] |
| HER2 (DNA/RNA) | ERBB2 (CNA & Expression) | 100% (vs. IHC 3+) | Not Provided | 10 | [81] |
The variation in concordance, particularly for Ki67, underscores biological and technical differences between measuring a nuclear protein (IHC) and its corresponding mRNA transcript (RT-qPCR) [7]. Nevertheless, studies confirm that breast cancer subtypes stratified by RT-qPCR show prognostic power for recurrence-free interval equivalent to IHC-based subtyping [7]. Furthermore, RT-qPCR assays like the STRAT4 panel on automated systems offer a standardized and rapid (<3 hours) approach, demonstrating high concordance with central IHC/FISH laboratories [80].
Experimental Protocols for Concordance Studies
Sample Selection and Preparation
- Cohort Design: Retrospective collections of Formalin-Fixed, Paraffin-Embedded (FFPE) breast tumor specimens are standard. A minimum of 100 samples is recommended, with power calculations suggesting 62 patients may be sufficient for specific biomarker validation [7] [82]. Cohorts should be split into training and validation sets (e.g., 70:30 ratio) to establish and confirm cut-off values [7] [83].
- Tumor Enrichment: A certified pathologist must review a hematoxylin and eosin (H&E)-stained slide from each FFPE block to mark regions of invasive carcinoma. This guides macro-dissection of adjacent unstained sections to ensure high tumor content, mitigating potential dilution effects from non-tumor tissue [83] [80].
RNA Extraction and Reverse Transcription
- Nucleic Acid Extraction: Macro-dissected tumor material is lysed using a specialized FFPE lysis reagent and digested with proteinase K (e.g., incubation at 80°C for 30 minutes) [80]. Subsequent RNA extraction and purification can be performed manually using silica-membrane columns or automated on integrated platforms like the GeneXpert [80].
- cDNA Synthesis: Total RNA is reverse transcribed into complementary DNA (cDNA) using a reverse transcriptase enzyme and a mixture of random hexamers and/or oligo-dT primers. This step is critical for converting the RNA target into an amplifiable template [7].
Multiplex RT-qPCR Setup and Analysis
- Assay Design: The RT-qPCR assay must include primers and probes for the target genes (ESR1, PGR, ERBB2, MKi67) and one or more endogenous control genes (e.g., RPL13A, ACTB, RPLP0, TFRC, CYFIP1) to normalize for RNA input and quality [11] [7] [80].
- Reaction Conditions: Utilize a multiplexed RT-qPCR master mix containing DNA polymerase, dNTPs, and buffer. The touch-down PCR protocol can be employed to enhance annealing specificity among different primers and probes, yielding significantly lower Cycle Threshold (CT) values and improved accuracy [11]. Reactions are run on a real-time PCR instrument.
- Data Normalization and Cut-off Determination: Gene expression data is analyzed using the ΔCT method, where ΔCT = CT (reference gene) - CT (target gene) [7] [80]. In the training set, logistic regression models with IHC/FISH status as the binary response variable are constructed. Receiver Operating Characteristic (ROC) curve analysis determines the optimal ΔCT cut-off value for each biomarker to maximize agreement with IHC/FISH [7]. These cut-offs are then applied to the validation cohort.
Table 2: Key Reagents and Research Solutions for Multiplex RT-qPCR Concordance Studies
| Item | Function/Description | Example Products/Assays |
|---|---|---|
| FFPE RNA Extraction Kit | Isolves and purifies RNA from challenging FFPE tissue. | RNeasy FFPE Kit (Qiagen), FFPE Lysis Reagent [7] [80] |
| Reverse Transcription Kit | Converts purified RNA into stable cDNA for PCR amplification. | RT2 First Strand Kit (Qiagen) [7] |
| Multiplex RT-qPCR Assay | Pre-designed set of primers, probes, and master mix for simultaneous target amplification. | Xpert Breast Cancer STRAT4 (Cepheid), Laboratory-Developed Tests (LDTs) [11] [80] |
| Endogenous Control Genes | Stable reference genes for normalizing gene expression data and accounting for variations. | RPL13A, CYFIP1, ACTB, RPLP0, TFRC [11] [7] [80] |
| Automated Diagnostic Platform | Integrated system for automated RNA extraction, purification, and RT-qPCR analysis. | GeneXpert System (Cepheid) [80] |
IHC and FISH Benchmarking
- Standardized IHC/FISH Protocols: All comparator IHC and FISH testing should be performed in a CAP-certified or equivalent central reference laboratory adhering to ASCO/CAP guidelines [7] [80]. For HER2, IHC scores of 0/1+ are considered negative, 2+ is equivocal (requiring reflex FISH testing), and 3+ is positive [5].
- Blinded Analysis: To prevent bias, IHC/FISH and RT-qPCR analyses should be performed by different personnel who are blinded to the results of the other methodology.
Workflow and Pathway Visualizations
Experimental Workflow for Concordance Studies
The following diagram illustrates the end-to-end process for conducting a RT-qPCR vs. IHC/FISH concordance study, from sample collection to data analysis.
Data Analysis and Validation Pathway
This diagram outlines the logical process for analyzing data and validating the established RT-qPCR model against the IHC/FISH benchmark.
Benchmarking RT-qPCR against IHC and FISH is a critical step in validating robust molecular assays for breast cancer subtyping. The protocols outlined herein provide a standardized framework for such concordance studies. The high concordance rates reported across multiple studies, particularly for ER, PR, and HER2, affirm RT-qPCR as a highly precise and reliable methodology. Its advantages of objectivity, quantitation, ability to be automated, and capacity for multiplexing make it an indispensable tool for both clinical research and drug development, potentially complementing or even supplanting traditional methods in certain contexts to enhance the precision of breast cancer patient stratification.
Breast cancer (BC) remains the foremost cause of cancer-related mortality, with an estimated 2.3 million new cases anticipated globally. The timely and accurate diagnosis of BC subtypes is pivotal for effective treatment and personalized therapeutic strategies [11]. Immunohistochemistry (IHC) represents the current diagnostic mainstay but suffers from limitations including sluggishness, expense, and dependence on proficient pathologists [11] [9]. Multiplex Reverse Transcription quantitative Polymerase Chain Reaction (RT-qPCR) emerges as a powerful alternative, enabling simultaneous quantification of multiple gene expression markers critical for subtyping. However, the promising findings of qPCR-based tests have been hampered in their clinical application by a noticeable lack of technical standardization [84] [85]. This application note provides a detailed framework for the analytical validation of multiplex RT-qPCR assays, specifically within the context of breast cancer subtyping research, focusing on the core parameters of sensitivity, specificity, and reproducibility.
Core Analytical Validation Parameters
The validation of a biomarker includes an evaluation of its analytical performance and its clinical performance. For a test to be considered robust and reliable for research and eventual clinical application, it must meet stringent criteria as defined by its context of use (COU) and adhere to the "fit-for-purpose" (FFP) concept [84].
- Analytical Sensitivity refers to the ability of a test to detect the analyte, often defined as the minimum detectable concentration or limit of detection (LOD) [84]. In the context of multiplex RT-qPCR for breast cancer, this translates to the lowest expression level of a marker gene (e.g., ESR1, PGR, HER2, Ki67) that can be reliably distinguished from background noise.
- Analytical Specificity is the ability of a test to distinguish the target from nontarget analytes [84]. For a multiplex assay, this involves ensuring that primers and probes do not cross-react with one another or with non-target genetic sequences, thereby guaranteeing that the measured signal is unique to the intended transcript.
- Reproducibility encompasses both repeatability (closeness of agreement between consecutive measurements under unchanged conditions) and reproducibility (closeness of agreement between measurements under changed conditions, such as different operators, instruments, or days) [84]. It is a measure of the precision of the assay across the expected variables of a research environment.
The table below summarizes the key performance characteristics that require assessment during analytical validation.
Table 1: Key Analytical Performance Characteristics for Validation
| Parameter | Definition | Assessment in Multiplex RT-qPCR |
|---|---|---|
| Analytical Trueness/Accuracy | Closeness of a measured value to the true value [84] | Comparison of gene expression results against a gold-standard method (e.g., IHC/FISH) [11]. |
| Analytical Precision | Closeness of two or more measurements to each other [84] | Calculation of intra-assay and inter-assay Coefficients of Variation (%CV) for CT values across replicates, days, and operators. |
| Analytical Sensitivity (LOD) | The minimum detectable concentration of the analyte [84] | Serial dilution of synthetic oligonucleotides or RNA with known concentration to determine the lowest detectable level. |
| Analytical Specificity | Ability to distinguish target from nontarget analytes [84] | Evaluation of cross-reactivity by testing primers/probes against non-target genes and using no-template controls (NTCs). |
Experimental Protocol: Analytical Validation for Breast Cancer Subtyping
This protocol outlines the steps for validating a multiplex RT-qPCR assay designed to subtype breast cancer based on the expression profiles of ESR1, PGR, HER2, and Ki67, using RPL13A as an endogenous control gene, as demonstrated in recent research [11] [9].
Sample Acquisition and RNA Purification
- Sample Material: Use human breast cancer tissue specimens, fresh-frozen or preserved in RNAlater. The study by Awrahman et al. utilized 61 samples representing four BC subtypes [11] [9].
- RNA Extraction: Perform total RNA purification using a commercial silica-membrane column kit, including an on-column DNase I digestion step to remove genomic DNA contamination. Quantify RNA concentration and assess purity using spectrophotometry (A260/A280 ratio ~2.0, A260/A230 ratio >1.8). Verify RNA integrity using an automated electrophoresis system (RNA Integrity Number, RIN >7.0 is recommended).
Assay Design and Multiplex RT-qPCR Setup
- Primer and Probe Design: Design TaqMan-based primers and dual-labeled hydrolysis probes (FAM, VIC, etc.) for the target genes (ESR1, PGR, HER2, Ki67) and endogenous control (RPL13A). Ensure amplicons are located at the boundary of two exons to prevent genomic DNA amplification.
- Reverse Transcription: Convert equal amounts of total RNA (e.g., 100 ng - 1 µg) into cDNA using a reverse transcription kit with random hexamers and Moloney Murine Leukemia Virus (M-MLV) reverse transcriptase.
- Multiplex qPCR with Touch-Down Method: The following table details the reaction components and cycling conditions, which have been shown to yield significantly lower Cycle Threshold (CT) values, enhancing assay performance [11].
Table 2: Multiplex RT-qPCR Reaction Setup and Cycling Conditions
| Component | Volume/Final Concentration | ||
|---|---|---|---|
| cDNA template | 2 µL (equivalent to 10 ng total RNA) | ||
| 2x Multiplex PCR Master Mix | 10 µL | ||
| Primer/Probe Mix (each) | Optimized concentration (e.g., 0.1 - 0.9 µM each) | ||
| Nuclease-free Water | To a final volume of 20 µL | ||
| Cycling Step | Temperature | Time | Cycles |
| Initial Denaturation | 95°C | 2 - 5 min | 1 |
| Touch-Down PCR Phase | 95°C | 30 sec | 10 Cycles |
| 65°C -> 55°C (-1°C/cycle) | 30 sec | ||
| Amplification Phase | 95°C | 30 sec | 40 Cycles |
| 55°C | 30 sec |
Data Analysis and Interpretation
- Cycle Threshold (CT) Determination: Set the fluorescence threshold within the exponential phase of amplification for all reactions. The CT value for each reaction is the cycle number at which the fluorescence exceeds this threshold.
- Gene Expression Quantification: Use the comparative CT (2^(-ΔΔCT)) method. Normalize the CT value of each target gene (ESR1, PGR, HER2, Ki67) to the endogenous control gene (RPL13A) within the same sample to obtain ΔCT. For subtyping, establish a relative expression cut-off (e.g., normalized expression units) compared to a reference population or control samples to classify tumors as positive or negative for each marker.
Experimental Protocol for Assessing Sensitivity, Specificity, and Reproducibility
Sensitivity and Limit of Detection (LOD)
- Procedure:
- Synthesize in vitro transcripts (IVTs) for each target gene or use a calibrated total RNA sample with high expression.
- Perform a log10 serial dilution (e.g., from 100 pg/µL to 0.1 pg/µL) in nuclease-free water.
- Run each dilution in at least six replicates in a single RT-qPCR run.
- Determine the concentration at which 95% of the replicates are positive. This is the LOD.
Specificity and Cross-Reactivity
- Procedure:
- Test each primer/probe set individually in a singleplex reaction against a panel of cDNA from all other target genes to check for off-target amplification.
- Include a no-template control (NTC) for each primer/probe set to ensure no signal from contaminants.
- Assess the melt curve (if using SYBR Green) for a single peak, or ensure that the fluorescence from the TaqMan probe is specific with no increase in the NTC.
Reproducibility (Precision)
- Procedure:
- Select RNA samples with low, medium, and high expression levels for each target gene.
- For intra-assay precision, run each of the three samples in eight replicates within a single qPCR plate.
- For inter-assay precision, run each of the three samples in triplicate across three different qPCR runs performed on different days by different operators.
- Calculate the mean CT, standard deviation (SD), and coefficient of variation (%CV = (SD/Mean CT) * 100) for each set of replicates. A %CV of less than 5% is generally considered acceptable for CT values.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Multiplex RT-qPCR Breast Cancer Subtyping
| Item | Function/Description |
|---|---|
| TaqMan-based Primers & Probes | Sequence-specific oligonucleotides for ESR1, PGR, HER2, Ki67, and endogenous control (e.g., RPL13A). Probes are labeled with different fluorescent dyes (FAM, VIC). |
| Multiplex RT-qPCR Master Mix | Optimized buffer containing hot-start DNA polymerase, dNTPs, MgCl₂, and stabilizers for efficient multiplex amplification. |
| RNA Purification Kit | Silica-membrane column system for high-quality, DNase-free total RNA isolation from tissue. |
| Reverse Transcription Kit | Contains reverse transcriptase, buffer, dNTPs, and random hexamers for first-strand cDNA synthesis. |
| Class II Biological Safety Cabinet | Required for all aerosol-generating processes when handling human-derived biological samples to ensure operator and environmental safety [86]. |
| Real-Time PCR Instrument | Thermocycler equipped with multiple optical channels for detecting different fluorescent dyes simultaneously. |
| Microcentrifuge and Pipettes | Essential for precise liquid handling and sample preparation. |
Workflow and Pathway Diagrams
The following diagram illustrates the complete analytical validation workflow for the multiplex RT-qPCR assay, from sample preparation to data analysis.
Diagram 1: Analytical validation workflow for multiplex RT-qPCR.
The relationship between the core validation parameters and their role in establishing a reliable assay is summarized below.
Diagram 2: Pillars of analytical validation.
A rigorous analytical validation process is fundamental for the development of a robust multiplex RT-qPCR assay for breast cancer subtyping. By systematically assessing sensitivity, specificity, and reproducibility using the protocols and frameworks outlined in this document, researchers can ensure that their assays generate precise, accurate, and reliable data. This level of validation is a critical step in bridging the gap between research use and potential future clinical application, ultimately supporting the advancement of personalized therapeutic strategies for breast cancer patients [11] [84] [9].
Comparative Analysis with Other Genomic Assays (e.g., Oncotype DX)
The management of early-stage, hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2-) breast cancer presents a significant clinical challenge in determining which patients will derive meaningful benefit from adjuvant chemotherapy. Traditional clinicopathological parameters, including tumor size, grade, and Ki-67 scores, demonstrate suboptimal predictive utility and exhibit substantial inter-observer variability [87]. Multigene genomic assays have emerged as powerful tools to overcome these limitations, providing quantitative biological insights into tumor behavior. This application note provides a detailed comparative analysis of multiplex RT-qPCR approaches against established genomic tests, with particular focus on the Oncotype DX Breast Recurrence Score assay, to guide researchers in assay selection and development for breast cancer subtyping research.
The Oncotype DX assay, first described in 2004, ushered in the era of genomic-based personalized cancer care for ER-positive primary breast cancer [87]. This 21-gene assay analyzes the expression of 16 cancer-related genes and 5 reference genes using reverse transcription polymerase chain reaction (RT-PCR) on RNA extracted from formalin-fixed paraffin-embedded (FFPE) tumor tissue [88] [89]. The result is presented as a continuous Recurrence Score (RS) ranging from 0-100, which predicts the 10-year risk of distant recurrence and the likelihood of chemotherapy benefit [89] [87]. The assay has been extensively validated through multiple clinical trials and has been incorporated into major international treatment guidelines, including those from ASCO, NCCN, and ESMO [88].
Commercially Available Genomic Assays: Technical Specifications and Clinical Validation
Multiple genomic assays have been developed to address the need for improved risk stratification in breast cancer. While each provides prognostic information, they differ significantly in their technical approaches, gene panels, and evidence for predicting chemotherapy benefit.
Table 1: Comparison of Major Commercially Available Genomic Assays for Breast Cancer
| Assay Name | Gene Count | Technology Platform | Risk Categories | Predictive of Chemotherapy Benefit | Key Validating Studies |
|---|---|---|---|---|---|
| Oncotype DX | 21 genes | RT-qPCR (central lab) | Low: <18Intermediate: 18-30High: ≥31 (original)Low: <11Intermediate: 11-25High: ≥26 (TAILORx) | Yes | NSABP B-14, B-20, TAILORx, RxPONDER |
| MammaPrint | 70 genes | Microarray (central lab) | Low-risk vs High-risk | No (prognostic only) | MINDACT |
| Prosigna (PAM50) | 50 genes | nCounter (local lab) | Low, Intermediate, High (ROR score) | No (prognostic only) | ATAC, ABCSG-8 |
| EndoPredict | 11 genes | RT-qPCR (local lab) | Low-risk vs High-risk (EPclin) | No (prognostic only) | Multiple translational studies |
| Breast Cancer Index (BCI) | 7 genes | RT-qPCR (central lab) | Continuous score | No (prognostic only, predicts late recurrence) | Multiple translational studies |
Among these assays, only the Oncotype DX test has been directly validated as a tool to predict benefit from the addition of chemotherapy through retrospective analyses of prospective randomized trials including NSABP B-20 and SWOG 8814 [87]. The TAILORx trial prospectively validated the assay in node-negative disease, demonstrating that women with scores ≤25 derived minimal benefit from chemotherapy [87].
Multiplex RT-qPCR as an Alternative Platform: Technical Considerations
Multiplex reverse transcription quantitative polymerase chain reaction (RT-qPCR) represents a promising methodological approach for developing laboratory-developed tests that can emulate the functionality of commercial assays like Oncotype DX. This technology enables simultaneous quantification of multiple gene targets in a single reaction, offering potential advantages in throughput, cost-efficiency, and customization.
Experimental Protocol: Multiplex RT-qPCR for Breast Cancer Subtyping
Sample Preparation and RNA Extraction:
- Obtain FFPE breast cancer tissue blocks with documented tumor content >70% [6]
- Perform macrodissection to enrich tumor content when necessary [90]
- Extract total RNA using commercial kits specifically validated for FFPE tissue (e.g., Quick-DNA/RNA FFPE Kit or RNeasy FFPE Kit) [6]
- Include a second DNase digestion step to eliminate genomic DNA contamination [90]
- Quantify RNA purity and concentration using spectrophotometry (NanoDrop); acceptable 260/280 ratios: 1.8-2.1 [6]
cDNA Synthesis and Preamplification:
- Reverse transcribe 100-500ng RNA using reverse transcriptase with oligo(dT) and/or random primers [90] [6]
- Utilize preamplification protocols recommended for FFPE-derived RNA (8-10 cycles) to enhance detection of low-abundance transcripts [90]
- Include controls for reverse transcription (RTC), genomic DNA contamination (GDC), and positive PCR control (PPC) [90]
Multiplex RT-qPCR Setup:
- Design custom primer panels covering target genes (e.g., ESR1, PGR, ERBB2, MKI67, and reference genes)
- Implement touch-down PCR protocols to improve annealing specificity among different primers and probes [11] [6]
- Utilize dual hybridization probes for specific detection in multiplex reactions [6]
- Distribute reactions across multiple tubes: Tube 1 (reference genes, ESR1, PGR, ERBB2), Tube 2 (proliferation genes), Tube 3 (additional cancer-related genes) [6]
- Perform reactions in triplicate on 384-well plates using high-throughput thermal cyclers [90] [89]
- Cycling conditions: Initial denaturation (95°C for 10 minutes), 40-45 cycles of denaturation (95°C for 15 seconds) and annealing/extension (60°C for 60 seconds) [90] [6]
Data Analysis and Normalization:
- Calculate Ct values for each target gene
- Normalize target gene expression to reference genes (e.g., RPL13A, GAPDH, ACTB) using the ∆∆Ct method [6]
- Apply algorithm for risk score calculation based on validated gene expression signatures
- For Oncotype DX-like scores, use the formula: RS = (0.47 × HER2 group score) + (1.04 × proliferation group score) + (0.10 × invasion group score) + (0.05 × CD68) - (0.08 × ER group score) - (0.07 × PGR group score) [90]
Comparative Performance Analysis: Multiplex RT-qPCR vs. Established Assays
Reproducibility Challenges with Alternative Platforms
Despite the theoretical potential to replicate established assays like Oncotype DX using alternative RT-qPCR platforms, significant technical challenges exist. A 2019 study attempting to reproduce Oncotype DX results using customized RT2-Profiler assays reported considerable difficulties in achieving correlation with original Recurrence Score values [90]. The researchers faced multiple obstructions including lack of detailed information on RNA input quantities, missing units in single gene expression reports from the commercial test, and vague normalization procedures - highlighting the proprietary nature of optimized clinical assays [90].
The study concluded that despite consistent assay performance with their customized approach, it was "impossible to establish correlations between RT2-Profiler recurrence scores with the respective Oncotype DX values not to mention exact matches" [90]. This underscores the sophisticated optimization and validation required for clinical-grade assay development that may not be readily transferable to research settings.
Concordance with Traditional Pathological Parameters
Multiplex RT-qPCR demonstrates strong potential for replicating standard immunohistochemistry (IHC) classification. Recent research has shown that mRNA levels of key biomarkers may correlate more robustly with clinicopathological features and recurrence risk than protein-based IHC assessments [91]. In a study of 750 breast cancers sent for Oncotype DX testing, HER2 mRNA levels demonstrated better correlation with clinicopathologic features and Recurrence Score than HER2 IHC scores, suggesting potential advantages of quantitative mRNA approaches for identifying biologically meaningful tumor characteristics [91].
Table 2: Performance Metrics of Multiplex RT-qPCR Versus Standard Methodologies
| Parameter | Multiplex RT-qPCR | Oncotype DX | Traditional IHC |
|---|---|---|---|
| Turnaround Time | 1-2 days [11] | 10-14 days [92] | 1-2 days |
| RNA Input | 100-500ng [90] | Proprietary | Not applicable |
| Reproducibility | High (when optimized) [6] | High (centralized) [88] | Moderate (subjective) |
| Quantitative Output | Continuous Ct values | Continuous RS (0-100) | Semi-quantitative (0-3+) |
| Dynamic Range | >7 logs [6] | >7 logs | Limited |
| Objective Assessment | Yes | Yes | No (subjective) |
| Cost per Sample | $100-300 (research) | ~$4000 (clinical) [92] | $50-150 |
| Customization Potential | High | None | Low |
Integration of Angiogenesis and Metastasis Profiling
A significant advantage of customized multiplex RT-qPCR panels is the ability to incorporate additional biomarkers beyond standard classification genes. Recent research has demonstrated the feasibility of including angiogenesis-related genes (HIF1A, ANG, VEGFR) alongside standard subtyping genes, providing insights into metastatic potential [11] [6]. This expanded profiling enables researchers to simultaneously assess both tumor subtype and aggressive features within a single experimental workflow.
Studies evaluating angiogenesis profiles across breast cancer subtypes have found that "numerous samples exhibit elevated levels of Hif1A and VEGFR, indicating their potential as valuable biomarkers for assessing metastatic status" [6]. This additional dimension of biological information exceeds the capabilities of standardized commercial assays and may provide valuable insights for drug development programs targeting specific metastatic pathways.
Research Reagent Solutions for Multiplex RT-qPCR
Table 3: Essential Research Reagents for Multiplex RT-qPCR in Breast Cancer Subtyping
| Reagent Category | Specific Products | Function | Technical Notes |
|---|---|---|---|
| RNA Extraction Kits | RNeasy FFPE Kit (Qiagen), Quick-DNA/RNA FFPE Kit (Zymo Research) | Isolation of high-quality RNA from FFPE tissue | Include DNase treatment step; evaluate RNA integrity number (RIN) when possible |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems) | cDNA synthesis from RNA templates | Include controls for genomic DNA contamination |
| Preamplification Kits | RT2 PreAMP cDNA Synthesis Kit (Qiagen) | Amplification of limited RNA targets | 8-10 cycles recommended for FFPE-derived RNA |
| qPCR Master Mixes | TaqMan Fast Advanced Master Mix (Applied Biosystems) | Amplification and detection | Compatible with multiplex probe-based detection |
| Custom Primer Panels | RT2 Profiler Custom Panels (Qiagen), Sigma-Aldrich Custom Oligos | Target-specific amplification | Design for uniform annealing temperatures (60±2°C) |
| Reference Genes | RPL13A, GAPDH, ACTB, B2M | Normalization of expression data | Validate stability across sample types |
| Control Templates | External RNA Controls Consortium (ERCC) samples | Quality control and standardization | Include positive, negative, and no-template controls |
Emerging Approaches and Future Directions
Machine Learning and Digital Pathology Integration
Recent advances in computational approaches offer promising alternatives for replicating genomic assay information from routinely available pathological materials. Deep learning models trained on hematoxylin and eosin (H&E) stained whole-slide images have demonstrated remarkable capability in inferring Oncotype DX Recurrence Scores without direct molecular testing [92].
The Orpheus model, a multimodal deep learning tool developed to infer RS from H&E images, achieved an area under the curve (AUC) of 0.89 for identifying high-risk cases (RS > 25), outperforming traditional clinicopathological nomograms (AUC = 0.73) [92]. Furthermore, in patients with intermediate RS values (≤25), the model ascertained risk of metastatic recurrence more accurately than the RS itself (0.75 vs 0.49 mean time-dependent AUC) [92]. This approach potentially offers a more accessible and cost-effective method for obtaining genomic-level insights, particularly in resource-limited settings.
Network-Based Subtyping Approaches
Beyond predefined gene panels, novel network-based approaches are emerging for refined molecular stratification. Weighted gene co-expression network analysis (WGCNA) applied to triple-negative breast cancer has identified clinically relevant modules associated with distinct biological processes and treatment responses [93].
In metastatic TNBC, modules enriched for epithelial-to-mesenchymal transition (Mod1/Turquoise), immunomodulatory features (Mod2/Blue), and plasma/B-cell signatures (Mod3/Brown) have demonstrated significant associations with clinical response and Burstein subtypes (BLIA, BLIS, LAR) [93]. These de novo network-based approaches potentially offer more biologically informed stratification than predetermined gene panels, particularly for aggressive breast cancer subtypes.
Multiplex RT-qPCR represents a versatile and powerful research tool for breast cancer molecular subtyping, offering distinct advantages in customization potential, throughput, and cost-efficiency compared to centralized commercial assays. However, researchers should recognize the significant technical challenges in replicating clinically validated assays like Oncotype DX, as subtle differences in methodology, normalization, and algorithm application can substantially impact result concordance.
The future of breast cancer genomic stratification lies in the integration of multiple data modalities - including RT-qPCR, digital pathology, and network biology - to develop more comprehensive and biologically informed classification systems. While standardized commercial assays provide clinically validated thresholds, customized multiplex approaches offer unparalleled flexibility for investigating novel biomarkers and biological pathways in research settings, potentially accelerating the discovery of next-generation diagnostic and therapeutic targets.
Predictive Power for Treatment Response and Resistance Mechanisms (e.g., CDK4/6 inhibitors)
The introduction of cyclin-dependent kinase 4/6 inhibitors (CDK4/6i) has transformed the management of hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2-) metastatic breast cancer, becoming a standard of care in combination with endocrine therapy [94] [95]. Despite their proven efficacy in improving progression-free and overall survival, both intrinsic and acquired resistance to these targeted agents present substantial clinical challenges [94] [96]. A significant obstacle in optimizing patient selection is the current lack of reliable, clinically validated biomarkers to predict treatment response [95]. This application note explores the principal molecular mechanisms underlying CDK4/6i resistance and details how multiplex RT-qPCR methodologies can be integrated into breast cancer subtyping research to identify predictive biomarkers, ultimately guiding more personalized therapeutic strategies for researchers and drug development professionals.
Key Mechanisms of CDK4/6 Inhibitor Resistance
Resistance to CDK4/6 inhibitors can be categorized as either intrinsic (de novo) or acquired (secondary). The major molecular alterations associated with resistance are summarized in Table 1 and involve disruptions in the core cell cycle machinery, activation of compensatory signaling pathways, and alterations in the tumor microenvironment [94] [97] [98].
Table 1: Key Molecular Mechanisms of CDK4/6 Inhibitor Resistance
| Resistance Mechanism | Molecular Alteration | Functional Consequence | Therapeutic Implications |
|---|---|---|---|
| RB1 Loss | Inactivating mutations or deletions in RB1 gene; "double-hit" events [94] | Renders CDK4/6 inhibition ineffective as cell cycle progression becomes RB-independent [97] | PARP inhibitors; agents targeting downstream effectors [94] |
| Cell Cycle Dysregulation | Overexpression of cyclin E; amplification of E2F transcription factors; CDK2 activation [94] [97] | Bypasses G1/S checkpoint blockade by CDK4/6i via alternative cyclin E-CDK2 complex [97] | Investigational CDK2 inhibitors [97] |
| p16 Overexpression | High expression of p16 (CDKN2A) [99] | Associated with reduced antitumor activity of CDK4/6i; biomarker for primary resistance [99] | PI3K combination therapy may overcome resistance [99] |
| PI3K/AKT/mTOR Pathway Activation | Mutations in PIK3CA; other pathway aberrations [94] | Activates downstream survival signals and promotes cell cycle progression independent of CDK4/6 [94] | PI3Kα inhibitors (e.g., alpelisib) in combination [94] [99] |
| FGFR Signaling Aberrations | Amplification or overexpression of FGFR1 [94] | Activates mitogenic pathways leading to cyclin D upregulation [94] | FGFR-targeting strategies under investigation [94] |
Biomarkers of Response and Resistance
The quantitative assessment of biomarkers from tumor tissue and liquid biopsies provides critical insights into predicting and monitoring response to CDK4/6 inhibitor therapy.
Established and Emerging Biomarkers
Table 2: Biomarkers for CDK4/6 Inhibitor Response and Resistance
| Biomarker | Detection Method | Predictive Value | Clinical Evidence |
|---|---|---|---|
| RB1 Loss | NGS; ctDNA analysis [94] | Strong biomarker of acquired resistance; shorter PFS (3.6 vs 10.1 months with intact RB1) [94] | PALOMA-3, MONALEESA trials [94] |
| p16 Protein | IHC [99] | High expression associated with primary resistance in PDX models and patients [99] | Preclinical and patient cohort studies [99] |
| Composite Biomarker (p16/pRb/Cyclin D1/Cyclin E1) | Multiplex IHC [99] | High sensitivity (87%) and accuracy (85%) for identifying resistant models [99] | Patient-derived xenograft study [99] |
| CTC Gene Signature (STAT3/PRKCB/CDK6) | RT-qPCR of circulating tumor cells [96] | STAT3highPRKCBhighCDK6low signature accurately classifies non-responders (AUC >0.8) [96] | Multicenter cohort study [96] |
| PIK3CA Mutations | NGS; RT-qPCR of ctDNA [94] | Not a standalone resistance biomarker but guides subsequent therapy lines after progression [94] | Clinical guidelines post-CDK4/6i progression [96] |
Experimental Protocols for Biomarker Analysis
Multiplex RT-qPCR for Breast Cancer Subtyping and Biomarker Detection
The following protocol is adapted from validated methodologies for determining breast cancer molecular subtypes via mRNA quantification [100] [11] and can be expanded to include resistance biomarkers.
Protocol: RNA Extraction and Multiplex RT-qPCR
- Sample Requirements: Formalin-fixed, paraffin-embedded (FFPE) breast tumor specimens or liquid biopsy samples (for ctDNA/CTC analysis).
- RNA Extraction:
- Use the RNXtract RNA extraction kit or equivalent.
- For FFPE sections, perform deparaffinization followed by proteinase K digestion.
- Extract total RNA, including small RNA species. Assess RNA quality and quantity using spectrophotometry.
- Expected Yield: Average RNA output of 233 ng/μl with DNA contamination <15 ng/μl [100].
- Reverse Transcription:
- Convert 50-500 ng of total RNA to cDNA using a high-capacity reverse transcription kit with random hexamers.
- Multiplex RT-qPCR:
- Gene Targets: Core subtyping genes (ESR1, PGR, ERBB2, MKI67) and resistance biomarkers (RB1, CDKN2A, CCNE1, STAT3). Use RPL13A or GAPDH as endogenous controls [100] [11].
- Reaction Setup: Prepare a master mix containing TaqMan Universal PCR Master Mix, gene-specific primers, and probes. Use a touch-down PCR protocol for accurate annealing when primer Tm values vary [11].
- Amplification Conditions:
- Hold stage: 95°C for 10-20 min.
- Amplification stage (40-45 cycles): Denature at 95°C for 15 sec, anneal/extend at 60°C for 1-60 min (optimize based on assay).
- Data Analysis: Calculate ∆Cq (Cqtarget - Cqendogenous control). Establish and validate cutoff values for each biomarker (e.g., high/low expression) [100].
Circulating Tumor Cell (CTC) Enrichment and Gene Expression Analysis
This protocol enables real-time monitoring of treatment response and resistance emergence through liquid biopsy [96].
Protocol: CTC Isolation and Transcriptomic Profiling
- CTC Enrichment:
- RNA Extraction and Preamplification:
- Extract total RNA from the enriched CTC fraction. Due to low RNA yield, perform a targeted preamplification step using a multiplexed primer pool.
- Gene Expression Analysis:
- Platform: Utilize the nCounter Pancancer Pathways panel (NanoString) for a discovery phase or RT-qPCR for validation.
- Key Resistance Targets: STAT3, PRKCB, CDK6, CCND1, MAPK3, EZH2, HDAC6, CDC7 [96].
- Data Interpretation: The gene expression signature STAT3highPRKCBhighCDK6low in baseline CTCs is predictive of non-response to CDK4/6i + ET [96].
Signaling Pathways and Resistance Mechanisms
The following diagram illustrates the core CDK4/6-RB-E2F pathway and the key mechanisms by which resistance arises.
Diagram 1: CDK4/6 Signaling and Resistance Mechanisms. This figure outlines the canonical cyclin D-CDK4/6-RB pathway targeted by CDK4/6 inhibitors (in blue) and the major molecular alterations (in yellow/red) that confer resistance, including RB1 loss, p16 overexpression, and activation of bypass pathways such as cyclin E-CDK2 and PI3K/AKT/mTOR [94] [97] [95].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Kits
| Product | Function/Application | Key Features |
|---|---|---|
| RNXtract RNA Extraction Kit | Total RNA isolation from FFPE specimens [100] | High yield (avg. 233 ng/μl); low DNA contamination; compatible with downstream RT-qPCR [100] |
| MammaTyper RT-qPCR Kit | IVD test for molecular subtyping via ERBB2, ESR1, PGR, MKI67 mRNA [100] | CE-marked; high inter-site concordance (>94%); standardized cut-offs [100] |
| RosetteSep CTC Enrichment Cocktail | Negative selection for CTC isolation from whole blood [96] | Antibody-based depletion of CD45+ cells; label-free CTCs [96] |
| AdnaTest EMT-2/StemCell Select | Positive immunomagnetic CTC selection [96] | Targets EpCAM, EGFR, HER2; suitable for transcriptomic analysis [96] |
| nCounter Pancancer Pathways Panel | Multiplexed gene expression analysis from low-input RNA [96] | Digital counting of mRNA molecules; no amplification bias; used in CTC profiling [96] |
The integration of multiplex RT-qPCR and liquid biopsy technologies into breast cancer research provides a powerful framework for elucidating and monitoring mechanisms of response and resistance to CDK4/6 inhibitors. The protocols and analytical approaches detailed in this application note empower researchers to move beyond static histopathological subtyping toward dynamic, molecularly driven stratification. By validating and implementing the biomarkers discussed—such as RB1 loss, p16 overexpression, and CTC-derived gene signatures—the scientific community can accelerate the development of novel combination therapies and overcome the critical challenge of resistance in HR+ breast cancer.
Breast cancer remains a formidable global health challenge, characterized by profound molecular heterogeneity. The timely and accurate diagnosis of its subtypes is pivotal for directing effective, personalized treatment strategies [11] [9]. While immunohistochemistry (IHC) has been the traditional cornerstone for classifying breast cancer based on protein expression markers, this method is constrained by its semi-quantitative nature, subjectivity, and relatively slow turnaround [11]. The evolving landscape of molecular pathology is now dominated by three powerful nucleic acid-based technologies: Multiplex Reverse Transcription quantitative PCR (RT-qPCR), Digital PCR (dPCR), and Next-Generation Sequencing (NGS). Within the specific context of breast cancer subtyping research, these techniques offer a complementary arsenal for precise gene expression profiling. Multiplex RT-qPCR provides a rapid, cost-effective, and highly accurate platform for quantifying established biomarkers like ESR, PGR, HER2, and Ki67 [11] [9]. Digital PCR enables absolute quantification of nucleic acids without a standard curve, offering unparalleled sensitivity for detecting rare transcripts and copy number variations (CNV), such as ERBB2/HER2 amplification, even in challenging samples like cell-free DNA (cfDNA) [101] [102]. Next-Generation Sequencing offers a hypothesis-free, comprehensive discovery platform, revealing the full transcriptomic diversity, novel fusion genes, and the complex genetic landscapes of rare breast tumor subtypes [103] [104]. This application note delineates the distinct and synergistic roles of these technologies, providing structured data and detailed protocols to guide their application in breast cancer research and drug development.
Technology Comparison and Applications
The selection of an appropriate molecular technique depends on the specific research question, balancing the need for throughput, sensitivity, discovery power, and cost. The table below provides a quantitative comparison of Multiplex RT-qPCR, dPCR, and NGS to inform this decision.
Table 1: Comparative Analysis of Key Molecular Technologies in Breast Cancer Research
| Feature | Multiplex RT-qPCR | Digital PCR (dPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Primary Application | Targeted expression profiling of known biomarkers (e.g., ESR1, PGR, HER2) [11] | Absolute quantification; rare allele detection; CNV analysis; liquid biopsy [101] [105] [102] | Novel discovery; comprehensive genomic/transcriptomic profiling; variant identification [106] [103] |
| Throughput | Medium to High (96-384 well formats) [106] | Medium (Limited by partition count) [107] | Very High (Millions of reads per run) [103] |
| Sensitivity | High (Sufficient for most expression studies) [106] | Very High (Can detect single molecules; variant allele frequency <0.1%–0.2%) [105] [107] | High (Dependent on sequencing depth) [108] |
| Quantification | Relative (Requires reference genes) [11] | Absolute (No standard curve needed) [105] [107] | Relative (Read counts) |
| Cost per Sample | Low to Medium [106] | Medium [106] | High [106] |
| Turnaround Time | 1–2 days [106] | 1–2 days | Days to weeks (includes library prep and bioinformatics) [106] |
| Key Strength | Speed, cost-effectiveness, and established workflows for validated targets [106] [11] | Ultra-sensitive and precise quantification; ideal for low-abundance targets and longitudinal tracking [101] [105] | Unbiased, hypothesis-free exploration of the entire transcriptome [106] [103] |
These technologies are not mutually exclusive but are often used in a complementary manner. A common workflow involves using NGS for initial discovery to identify a panel of differentially expressed genes or novel variants. Subsequently, multiplex RT-qPCR or dPCR can be employed to rapidly and cost-effectively validate these findings across a larger patient cohort or for routine testing [106]. Furthermore, dPCR is exceptionally suited for validating low-frequency variants or CNVs identified by NGS with higher precision and confidence [101] [102].
Experimental Protocols for Breast Cancer Research
Protocol A: Multiplex RT-qPCR for Breast Cancer Subtyping and Angiogenesis Profiling
This protocol is adapted from a study that demonstrated precise breast cancer typing using a touch-down PCR method, which enhances annealing specificity in multiplex reactions [11] [9].
1. Sample Preparation and RNA Extraction
- Obtain breast tumor tissue samples via core needle biopsy or surgical resection.
- Homogenize tissue samples using a mechanical homogenizer.
- Extract total RNA using a commercial column-based kit. Ensure RNA Integrity Number (RIN) is >7.0 for optimal cDNA synthesis.
- Treat samples with DNase I to remove genomic DNA contamination.
2. Reverse Transcription (cDNA Synthesis)
- Use 500 ng – 1 µg of total RNA for first-strand cDNA synthesis.
- Employ a reverse transcription kit with oligo(dT) and/or random hexamer primers.
- Perform the reaction according to the manufacturer's instructions (e.g., 25°C for 10 min, 37°C for 120 min, 85°C for 5 min).
- Dilute the synthesized cDNA 1:5 in nuclease-free water before qPCR.
3. Multiplex RT-qPCR Setup
- Primers and Probes: Design TaqMan hydrolysis probes for target genes. The study specifically targeted ESR1, PGR, ERBB2 (HER2), MKi67, and the endogenous control RPL13A [11]. For angiogenesis profiling, include HIF1A, ANG, and VEGFR [11] [9].
- Reaction Mix: Prepare a master mix containing:
- 1X TaqMan Fast Advanced Master Mix
- Primers and probes for the 4-plex assay (ESR1, PGR, ERBB2, MKi67, RPL13A)
- 2 µL of diluted cDNA template
- Adjust total volume to 10 µL with nuclease-free water.
- Touch-Down PCR Cycling Conditions [11]:
- Initial Denaturation: 95°C for 20 seconds.
- Touch-Down Cycles: 10 cycles of 95°C for 3 seconds and 68–58°C for 30 seconds (decreasing the annealing temperature by 1°C per cycle).
- Standard Cycles: 40 cycles of 95°C for 3 seconds and 58°C for 30 seconds.
4. Data Analysis
- Analyze data using the comparative Cq (ΔΔCq) method. The touch-down protocol consistently yields lower Cq values, indicating improved amplification efficiency [11].
- Normalize the Cq values of target genes to the reference gene RPL13A.
- Classify subtypes based on relative gene expression profiles against IHC-defined standards.
Protocol B: Digital PCR for ERBB2/HER2 Copy Number Variation Analysis
This protocol outlines the use of dPCR for ultrafast and precise absolute quantification of HER2 CNV, which can predict response to anti-HER2 therapy [101] [102].
1. Sample and Assay Preparation
- Sample Input: Use 10-50 ng of genomic DNA from breast tumor tissue or cell-free DNA from liquid biopsies. Restriction enzyme digestion (e.g., HindIII) is recommended for gDNA to fragment large strands and prevent viscosity issues [102].
- Assay Design: Use validated hydrolysis probe assays for the ERBB2 (HER2) gene and a stable reference gene panel (e.g., DCK, HBB, PMM1, RPS27A, RPPH1) located on different chromosomes to mitigate bias from genomic instability [102].
2. dPCR Reaction Partitioning and Amplification
- Prepare the dPCR reaction mix containing the DNA sample, master mix, and assays for HER2 and the multiplexed reference genes.
- Partition the reaction mix into thousands of nanoliter-sized droplets or microchambers using a commercial dPCR system (e.g., Bio-Rad QX200, Thermo Fisher QuantStudio, or Qiagen QIAcuity).
- Transfer the partitions to a thermal cycler and run the following program:
- Enzyme Activation: 95°C for 10 minutes.
- Denaturation/Annealing/Extension: 40 cycles of 94°C for 30 seconds and 60°C for 60 seconds.
- Signal Stabilization: 98°C for 10 minutes (for droplet-based systems).
3. Fluorescence Reading and Data Analysis
- Read the endpoint fluorescence of each partition using a droplet reader or chip imager.
- The software will count the positive (containing target) and negative (without target) partitions.
- The absolute copy number of HER2 and the reference genes is calculated directly using Poisson statistics, without the need for a standard curve.
- CNV Calculation: The HER2 copy number is normalized to the median copy number of the reference gene panel to determine the CNV status. A ratio >2.0 is typically indicative of amplification [102].
Table 2: Key Research Reagent Solutions for Featured Protocols
| Reagent / Material | Function / Application | Example Product / Note |
|---|---|---|
| TaqMan Fast Advanced Master Mix | Provides enzymes, dNTPs, and buffer for efficient, highly specific qPCR amplification in multiplex assays. | Thermo Fisher Scientific [106] |
| TaqMan Gene Expression Assays | Predesigned, optimized primer-probe sets for specific gene targets (e.g., ESR1, PGR, HER2). | Assays can be searched via the TaqMan Assay Search Tool [106] |
| dPCR Partitioning Oil & Surfactant | Creates stable, monodisperse droplets for droplet-based dPCR systems, preventing coalescence. | Bio-Rad Droplet Generation Oil [107] |
| Multiplex Reference Gene Panel Assays | A set of assays for stable reference genes used for absolute quantification and normalization in dPCR CNV studies. | A 5-plex panel (DCK, HBB, PMM1, RPS27A, RPPH1) is described [102] |
| Restriction Endonuclease (HindIII) | Digests genomic DNA into smaller fragments prior to dPCR, reducing viscosity and improving partition efficiency. | New England Biolabs (NEB) [102] |
| Cell-free DNA Extraction Kit | Isolves high-quality, low-abundance cfDNA from blood plasma for liquid biopsy applications. | Promega Maxwell RSC ccfDNA Plasma Kit [102] |
Visualizing Workflows and Pathways
To elucidate the experimental journey and the underlying biology, the following diagrams map the core protocol workflow and the angiogenesis signaling pathway relevant to breast cancer subtyping.
Diagram 1: Multiplex RT-qPCR subtyping workflow. This workflow outlines the key steps from RNA extraction to final subtype classification, highlighting the use of a touch-down PCR protocol and a defined gene panel for precise results [11] [9].
Diagram 2: Key angiogenesis pathway. This diagram illustrates the core signaling pathway involving HIF1A, VEGF/VEGFR, and Angiogenin (ANG), which are potential biomarkers for assessing the metastatic potential of breast cancer tumors [11] [9]. Their expression can be quantified using the multiplex RT-qPCR protocol to further characterize cancer subtypes.
Conclusion
Multiplex RT-qPCR has firmly established itself as a precise, rapid, and cost-effective cornerstone for breast cancer molecular subtyping, demonstrating remarkable concordance with traditional IHC. Its utility extends beyond initial diagnosis into dynamic monitoring of treatment response and resistance mechanisms through liquid biopsy applications. Future directions will focus on standardizing panels for clinical adoption, integrating novel biomarkers for metastatic potential, and combining this robust technology with artificial intelligence and other omics data to build comprehensive predictive models. For researchers and drug developers, these advancements pave the way for more refined clinical trials, novel therapeutic targets, and ultimately, highly personalized patient management strategies that improve survival outcomes.
References
- 1. Updates on utility of immunohistochemistry in diagnosis ... [https://www.sciencedirect.com/science/article/abs/pii/S004681772500108X]
- 2. H&E to IHC virtual staining methods in breast cancer [https://www.nature.com/articles/s41746-025-01741-9]
- 3. Advances in research and current challenges in the ... [https://pubmed.ncbi.nlm.nih.gov/40177129/]
- 4. HER2-Low Breast Cancer—Current Knowledge and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12028887/]
- 5. Systematic review and meta-analysis of artificial ... [https://www.nature.com/articles/s41746-025-01483-8]
- 6. Advanced breast cancer diagnosis: Multiplex RT-qPCR for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10776909/]
- 7. Concordance of RT-qPCR with immunohistochemistry and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10519502/]
- 8. Advances in research and current challenges in the ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1451471/full]
- 9. Advanced breast cancer diagnosis: Multiplex RT-qPCR for ... [https://pubmed.ncbi.nlm.nih.gov/38205186/]
- 10. What is multiplex qPCR? [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/what-is-multiplex-qpcr.html]
- 11. Advanced breast cancer diagnosis: Multiplex RT-qPCR for ... [https://www.sciencedirect.com/science/article/pii/S2405580823001966]
- 12. Guidelines for 6-color multiplex assay design for optimized ... [https://www.stillatechnologies.com/digital-pcr/naica-system-analysis/guidelines-for-6-color-multiplex-assay-design-for-optimized-performance-with-crystal-digital-pcr/]
- 13. Brief guide to RT-qPCR - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11612376/]
- 14. Accurate RT-qPCR gene expression analysis on cell ... [https://www.nature.com/articles/srep00222]
- 15. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOorLDuQ-_sehSxazqliNwkjixTf349BBvl_Qwx4LpS7waSmOsuKB]
- 16. rtpcr: a package for statistical analysis and graphical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530193/]
- 17. ESR1, PGR, ERBB2, and MKi67 mRNA expression in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639300/]
- 18. Assessment of ESR1, PGR, ERBB2, and MKI67 mRNA in ... [https://pubmed.ncbi.nlm.nih.gov/40666735/]
- 19. PAM50 Breast Cancer Subtyping by RT-qPCR and ... [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/1755-8794-5-44]
- 20. Statistical analysis of real-time PCR data - BMC Bioinformatics [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-7-85]
- 21. Frontiers | Hypoxia-inducible factor in breast cancer: role and target for breast cancer treatment [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1370800/full]
- 22. Expression of HIF-1α and markers of angiogenesis and metabolic adaptation in molecular subtypes of breast cancer | Translational Medicine Communications | Full Text [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-023-00135-x]
- 23. Development and validation of cost-effective one-step ... [https://www.nature.com/articles/s41598-022-10413-7]
- 24. High-Throughput Data Analysis for qPCR [https://www.neb.com/en-us/tools-and-resources/feature-articles/development-of-a-high-throughput-data-analysis-method-for-quantitative-real-time-pcr?srsltid=AfmBOoqBHy8QRqPZeoroWAmYet38-37yfw5E_EC5jIuS1JzKYriBprmZ]
- 25. Precision Medicine [https://www.fda.gov/medical-devices/in-vitro-diagnostics/precision-medicine]
- 26. Personalised Medicine—Implementation to the Healthcare ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10058568/]
- 27. Precision Medicine, AI, and the Future of Personalized Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7877825/]
- 28. Personalized Drug Therapy: Innovative Concept Guided ... [https://www.sciencedirect.com/science/article/pii/S1535947624000276]
- 29. Current Trends in Liquid Biopsy Tracking Resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027453/]
- 30. Quantitative and Qualitative Evaluation of Breast Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6913513/]
- 31. Revolutionizing healthcare: the role of artificial intelligence in ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-023-04698-z]
- 32. Overcoming the Challenges of High Quality RNA Extraction ... [https://pubmed.ncbi.nlm.nih.gov/33922016/]
- 33. Optimized Gene Expression Analysis from FFPE Samples [https://www.thermofisher.com/us/en/home/references/ambion-tech-support/rna-isolation/tech-notes/optimized-gene-expression-analysis-from-ffpe-samples.html]
- 34. Biobanking of fresh frozen tissue: RNA is stable in nonfixed ... [https://www.nature.com/articles/3700372]
- 35. Comparison of breast cancer surrogate subtyping using a ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-021-08171-2]
- 36. The impact of RNA extraction method on ... - BMC Cancer [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-019-6363-0]
- 37. Optimization of RNA Extraction from Formalin-Fixed ... [https://pubmed.ncbi.nlm.nih.gov/29285045/]
- 38. Optimizing RNA extraction and library preparation from oral ... [https://bmrat.org/index.php/BMRAT/article/view/840]
- 39. Designing highly multiplex PCR primer sets with Simulated ... [https://www.nature.com/articles/s41467-022-29500-4]
- 40. Precision and Accuracy with TaqMan Probes _Synbio Technologies [https://synbio-tech.com/taqman-probe]
- 41. Multiplex qPCR Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/genomics/qpcr/multiplex-qpcr?srsltid=AfmBOop0f48tRyQQet6EnwkZWJ6M48ao5C2UKN-QeiToDporQPnpxE1U]
- 42. Touchdown Polymerase Chain Reaction (PCR) [https://pubmed.ncbi.nlm.nih.gov/29717053/]
- 43. What is touchdown PCR (TD-PCR) and when would I need ... [https://help.takarabio.com/36168/kb/article/110050/what-is-touchdown-pcr-tdpcr-and-when-would-i-need-to-use-it]
- 44. Touchdown PCR for increased specificity and sensitivity in ... [https://pubmed.ncbi.nlm.nih.gov/18772872/]
- 45. Touchdown PCR: Easy Intro Plus 5 Expert Tips [https://bitesizebio.com/2203/touchdown-pcr-a-primer-and-some-tips/]
- 46. TqPCR: A Touchdown qPCR Assay with Significantly ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0132666]
- 47. Protocol 24978 - D1Mit15 [https://www.jax.org/Protocol?stockNumber=002624&protocolID=24978]
- 48. 使用乳腺癌档案材料优化基于多重RNA 的表达检测 [https://www.jove.com/cn/v/57148/optimization-multiplex-rna-based-expression-assay-using-breast-cancer]
- 49. qPCR技术介绍(五)——绝对定量与相对定量 [https://www.takarabiomed.com.cn/Info.aspx?m=20141217163031750657&n=20230329115555807727]
- 50. qPCR 的绝对定量与相对定量| Thermo Fisher Scientific - CN [https://www.thermofisher.cn/cn/zh/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/absolute-vs-relative-quantification-real-time-pcr.html]
- 51. 实时荧光定量PCR原理及基础知识 - 赛默飞 [https://www.thermofisher.cn/cn/zh/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/essentials-real-time-pcr.html]
- 52. PCR/qPCR 数据分析 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/genomics/qpcr/data-analysis?srsltid=AfmBOooGtmcDOdDb6pOcQl8RN-A-JX15eaz0PtEwV7d7oJAwJH8CZ64z]
- 53. RPL13A作为内参基因在RT-qPCR检测进入高原前后血液中 ... [https://patents.google.com/patent/CN108611423A/zh]
- 54. Beyond blood: Advancing the frontiers of liquid biopsy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11007055/]
- 55. Research progress of CTC, ctDNA, and EVs in cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1303335/full]
- 56. Exploration of Circulating Tumour Cell (CTC) Biology [https://pmc.ncbi.nlm.nih.gov/articles/PMC7994460/]
- 57. Precision breast cancer subtype diagnostics with multi-bit ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894725047011]
- 58. Troubleshooting primer dimer in PCR [https://www.minipcr.com/primer-dimer-pcr/]
- 59. Eliminating primer dimers and improving SNP detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7200914/]
- 60. Multiplex vs. Singleplex qPCR: What Do I Need To Know? [https://www.thermofisher.com/blog/behindthebench/multiplex-vs-singleplex-qpcr-what-do-i-need-to-know/]
- 61. qPCR and RT-qPCR [https://www.promega.com/resources/guides/nucleic-acid-analysis/qpcr-and-rt-qpcr-amplification/]
- 62. Adjusting RT-qPCR conditions to avoid unspecific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7598553/]
- 63. Efficient experimental design and analysis of real-time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3710343/]
- 64. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 65. Technical validation of an RT-qPCR in vitro diagnostic test ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-016-2476-x]
- 66. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 67. qPCR primer design revisited - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5702850/]
- 68. High-Throughput RT-PCR for small-molecule screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3593604/]
- 69. Your reverse transcription may not be optimal [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/real-time-pcr-troubleshooting-tool/gene-expression-quantitation-troubleshooting/abnormal-amplification-curves/amplification-occurs-later/your-reverse-transcription-may-not-be-optimal.html]
- 70. Optimization Tips for Luna® One-Step RT-qPCR [https://www.neb.com/en-us/tools-and-resources/usage-guidelines/optimization-tips-for-luna-one-step-rt-qpcr?srsltid=AfmBOorhA3hkse8QuAZwCWgK8RIf1XBG3c6eFU_CkHmzHed0g_WQzI_Q]
- 71. An optimized protocol for stepwise optimization of real-time ... [https://www.nature.com/articles/s41438-021-00616-w]
- 72. An amplification velocity-controlled PCR device for ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894722066049]
- 73. Engineering of novel DNA polymerase variants for single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274487/]
- 74. Dimethyl Sulfoxide Promotes the Multiple Functions of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3328470/]
- 75. The use of bovine serum albumin to improve the RT-qPCR ... [https://pubmed.ncbi.nlm.nih.gov/21219370/]
- 76. Avoiding Contamination | Thermo Fisher Scientific - ES [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/good-laboratory-practice-avoid-contamination-qpcr-experiments.html]
- 77. Controlling for contamination in qPCR testing - LGC [https://blog.biosearchtech.com/how-to-control-for-contamination-in-qpcr-testing]
- 78. RT-qPCR strategies for molecular diagnostics, OEM and ... [https://www.neb.com/en/nebinspired-blog/rt-qpcr-strategies-for-molecular-diagnostics-and-oem?srsltid=AfmBOoqws1n6t3ry9eToXf1C7Cp-pcA7iZZugOg4LrUE8OpVwxvvPp0A]
- 79. Revolutionizing breast cancer immunotherapy by integrating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123773/]
- 80. Comparison of central laboratory assessments of ER, PR, ... [https://link.springer.com/article/10.1007/s10549-018-4889-5]
- 81. Molecular Biological Determination of HER2 Status Using ... [https://www.mdpi.com/1422-0067/26/5/2148]
- 82. THSD4 is a novel mediator of T cell exclusion and anti-PD-1 ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00850-7]
- 83. The spatially informed mFISHseq assay resolves ... [https://www.nature.com/articles/s41467-024-55583-2]
- 84. Consensus guidelines for the validation of qRT-PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8792405/]
- 85. Consensus guidelines for the validation of quantitative RT ... [https://www.sciencedirect.com/science/article/pii/S2329050122000018]
- 86. Biosafety Level (BSL) Practices Chart [https://blink.ucsd.edu/safety/research-lab/biosafety/containment/chart.html]
- 87. Spotlight on the utility of the Oncotype DX® breast cancer assay [https://pmc.ncbi.nlm.nih.gov/articles/PMC5827461/]
- 88. Oncotype DX Breast Recurrence Score® Test [https://www.exactsciences.com/cancer-testing/oncotype-dx-breast-recurrence-score-providers]
- 89. About the test - Oncotype DX by Exact Sciences. [https://www.oncotypedxtest.com/en-ie/healthcare-professionals/what-is-the-oncotype-dx-test]
- 90. Oncotype DX Breast Cancer recurrence score resists inter- ... [https://www.nature.com/articles/s41598-019-56910-0]
- 91. In ER-Positive, HER2-Negative Breast Cancers, ... [https://www.sciencedirect.com/science/article/pii/S0023683723002520]
- 92. Multimodal histopathologic models stratify hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11873197/]
- 93. Utilizing cohort-level and individual networks to predict ... [https://www.nature.com/articles/s41698-025-00959-w]
- 94. Understanding and overcoming CDK4/6 inhibitor resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12254669/]
- 95. Targeting CDK4/6 in breast cancer [https://www.nature.com/articles/s12276-025-01395-3]
- 96. Gene expression analysis in circulating tumour cells to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11971781/]
- 97. CDK4/6 inhibitor resistance mechanisms and treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9448295/]
- 98. CDK4/6 inhibitors in breast cancer therapy: mechanisms of ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1549520/full]
- 99. High p16 expression and heterozygous RB1 loss are ... [https://www.nature.com/articles/s41467-022-32828-6]
- 100. Technical validation of an RT-qPCR in vitro diagnostic test ... [https://pubmed.ncbi.nlm.nih.gov/27389414/]
- 101. Improving HER2 Diagnostics with Digital Real-Time PCR ... [https://pubmed.ncbi.nlm.nih.gov/40913387/]
- 102. Multiplexed Digital PCR Reference Gene Measurement for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523864/]
- 103. Next-generation sequencing in breast cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502106/]
- 104. Genetic landscapes of breast tumors by next-generation ... [https://www.sciencedirect.com/science/article/pii/S0046817725001133]
- 105. How Digital PCR Enables Early Molecular Relapse Detection [https://www.thermofisher.com/blog/behindthebench/early-molecular-relapse-detection-dpcr/]
- 106. Real-Time PCR (qPCR) and Whole-Transcriptome NGS [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/ngs-comparison.html]
- 107. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 108. Comparison of Next-Generation Sequencing, Real-Time ... [https://www.mdpi.com/2076-2607/13/10/2344]