Integrating 3D-QSAR and AI for Advanced ADMET Prediction in Cancer Drug Design
This article explores the integration of three-dimensional Quantitative Structure-Activity Relationship (3D-QSAR) modeling and Artificial Intelligence (AI) for predicting the Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties of anticancer drug...
Integrating 3D-QSAR and AI for Advanced ADMET Prediction in Cancer Drug Design
Abstract
This article explores the integration of three-dimensional Quantitative Structure-Activity Relationship (3D-QSAR) modeling and Artificial Intelligence (AI) for predicting the Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties of anticancer drug candidates. Aimed at researchers and drug development professionals, it covers the foundational principles of 3D-QSAR techniques like CoMFA and CoMSIA, their application in rational drug design for targets such as Tubulin and Topoisomerase IIα, and the transformative role of Machine Learning in enhancing ADMET prediction accuracy. The content also addresses methodological challenges, optimization strategies, and validation protocols to ensure model robustness. By synthesizing insights from recent case studies and technological advances, this review serves as a comprehensive guide for leveraging computational tools to accelerate the development of safer and more effective cancer therapies.
The Critical Role of ADMET and 3D-QSAR in Modern Cancer Drug Discovery
The development of new cancer therapies remains one of the most challenging endeavors in pharmaceutical science, characterized by exceptionally high failure rates that demand innovative solutions. Oncology drug development suffers from an alarming attrition rate, with an estimated 97% of new cancer drugs failing in clinical trials and only approximately 1 in 20,000-30,000 compounds progressing from initial development to marketing approval [1]. This staggering rate of failure significantly outpaces the already low average success rates across other therapeutic areas, where less than 10% of new drug entities ultimately reach the market [1] [2]. The magnitude of this challenge underscores the critical importance of addressing fundamental inefficiencies in the drug development pipeline, particularly through enhanced predictive capabilities in early-stage compound evaluation.
The financial and temporal investments in drug development are substantial, with estimates exceeding $2.8 billion dedicated to the study and development of new drug entities, often requiring over a decade to bring a single successful drug to market [3] [1]. This investment frequently yields minimal return due to the high failure rates, creating an unsustainable model that ultimately impedes patient access to novel therapies. The root causes of this attrition are multifaceted, encompassing poor drug efficacy, unacceptable toxicity profiles, suboptimal pharmacokinetic properties, and inadequate target engagement [4] [1]. Within this challenging landscape, the accurate prediction of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties has emerged as a crucial frontier in improving developmental outcomes, offering the potential to identify potential failures earlier in the process when resources can be more effectively allocated toward promising candidates.
Quantitative Analysis of Drug Attrition Rates
A comprehensive analysis of drug development success rates reveals both the profound challenges in oncology and emerging trends that may inform future strategies. The dynamic clinical trial success rate (ClinSR) has shown concerning trends, declining since the early 21st century before recently plateauing and demonstrating slight improvement [2]. This modest recovery suggests that evolving development approaches may be beginning to address systemic inefficiencies.
Table 1: Clinical Trial Success Rates (ClinSR) and Attrition Patterns in Drug Development
| Development Stage | Success Rate | Key Contributing Factors | Potential Improvement Strategies |
|---|---|---|---|
| Overall Oncology Drug Development | ~3% approval rate [1] | Poor efficacy, toxicity, resistance mechanisms, tumor heterogeneity [3] [1] | Enhanced target validation, improved preclinical models, biomarker-driven selection |
| Early-Phase Trial Screen Failures | 21.7-26.4% of consented patients [5] | Radiological findings (29.2%), biological criteria (23.8%), clinical deterioration (22.3%) [5] | Optimized referral processes, updated eligibility criteria, preliminary screening assessments |
| Anti-COVID-19 Drugs | Extremely low ClinSR [2] | Compressed development timelines, limited understanding of disease mechanisms | Traditional development paradigms despite emergency context |
| Drug Repurposing | Lower than expected success rate [2] | Inadequate understanding of new disease context, suboptimal dosing regimens | Enhanced mechanistic understanding in new indications |
Analysis of screen failure rates in early-phase trials provides additional insight into inefficiencies within the development process. Across three comprehensive cancer centers in France, 21.7-26.4% of patients who provided consent for early-phase trials ultimately failed to enroll [5]. The primary reasons for these screen failures were radiological findings (29.2%), particularly newly discovered brain metastases; biological criteria (23.8%), mainly vital organ dysfunction; and clinical deterioration (22.3%) [5]. Importantly, current eligibility criteria were found to exclude 47.5% of patients who were still alive at 6 months, raising questions about the accuracy of these criteria for patient selection in early-phase trials designed to evaluate drug tolerance and activity [5].
Table 2: Analysis of Screen Failures in Early-Phase Oncology Trials
| Screen Failure Category | Frequency (%) | Specific Reasons | Potential Mitigation Approaches |
|---|---|---|---|
| Radiological | 29.2% | New brain metastases (n=27), non-measurable disease (n=17), absence of target for mandatory biopsy (n=8) [5] | Updated imaging prior to referral, modernized response criteria |
| Biological | 23.8% | Vital organ dysfunction (n=34), non-vital laboratory abnormalities [5] | Earlier screening labs, protocol-specific waivers for non-critical values |
| Clinical | 22.3% | Serious/potentially life-threatening events, past medical history exclusions [5] | Comprehensive pre-screening assessments, updated comorbidity policies |
| Performance Status Deterioration | 11.9% | ECOG performance status decline between consent and screening [5] | Reduced screening timeline, interim status assessments |
The Role of ADMET Prediction in Addressing Attrition
Inadequate pharmacokinetic profiles and unanticipated toxicity account for a substantial proportion of drug candidate failures, highlighting the critical importance of robust ADMET prediction early in the development process. The integration of ADMET assessment within quantitative structure-activity relationship (QSAR) frameworks represents a transformative approach to identifying potential liabilities before significant resources are invested in compound development. Recent advances in computational methodologies have enabled increasingly sophisticated prediction of these essential properties, allowing researchers to prioritize compounds with a higher probability of clinical success [6] [7] [8].
The fundamental premise of integrating ADMET prediction in 3D-QSAR cancer drug design is the establishment of quantitative relationships between molecular structure and pharmacokinetic/toxicological outcomes. In the development of 1,2,4-triazine-3(2H)-one derivatives as tubulin inhibitors for breast cancer therapy, researchers employed ADMET profiling alongside QSAR modeling, molecular docking, and molecular dynamics simulations to comprehensively evaluate potential candidates [8]. This integrated computational approach identified specific descriptors such as absolute electronegativity and water solubility as significant influencers of inhibitory activity, achieving a predictive accuracy (R²) of 0.849 [8]. Similarly, in the design of anti-breast cancer agents based on 1,4-quinone and quinoline derivatives, ADMET properties were determined to assess the drug-candidate potential of newly designed ligands, with only one compound (ligand 5) emerging as sufficiently promising for experimental testing [6].
The application of these principles to natural product drug discovery has further demonstrated the power of integrated ADMET prediction. In studies of natural products from the NPACT database with activity against MCF-7 breast cancer cell lines, researchers developed statistically robust QSAR models (R² = 0.666-0.669, Q²Fn = 0.686-0.714) that informed virtual screening of the COCONUT database for novel natural inhibitors [7]. Subsequent ADMET evaluation, molecular docking against human HER2 protein, and molecular dynamics simulations identified two compounds (4608 and 2710) as the most promising candidates based on their binding stability and pharmacological properties [7].
Experimental Protocols: ADMET-Centric 3D-QSAR in Oncology Drug Design
Protocol 1: Development of Robust 3D-QSAR Models with ADMET Integration
Objective: To establish validated 3D-QSAR models that incorporate ADMET parameters for predicting anti-cancer activity and pharmacokinetic profiles.
Materials and Reagents:
- Chemical dataset of known active/inactive compounds
- Computational chemistry software (Gaussian 09W, ChemOffice)
- Molecular descriptor calculation tools (PaDEL Descriptor)
- Statistical analysis package (XLSTAT or equivalent)
Procedure:
Dataset Curation and Preparation
- Collect compound structures and corresponding biological activity data (e.g., IC₅₀ against specific cancer cell lines) from validated databases such as NPACT [7]
- Convert IC₅₀ values to pIC₅₀ (-log IC₅₀) for QSAR analysis [8]
- Apply rigorous curation to remove duplicates, incorrect structures, and standardize representation
- Divide dataset using an 80:20 ratio for training and test sets to ensure robust validation [8]
Molecular Geometry Optimization and Descriptor Calculation
- Optimize molecular geometries using density functional theory (DFT) with B3LYP functional and 6-31G(p,d) basis set [8]
- Calculate electronic descriptors (Eₕₒₘₒ, Eₗᵤₘₒ, dipole moment, absolute electronegativity) using Gaussian 09W [8]
- Compute topological descriptors (molecular weight, logP, logS, polar surface area) using ChemOffice software [8]
- Generate additional descriptors using PaDEL Descriptor software for comprehensive structural representation [7]
Model Development and Validation
- Apply principal component analysis (PCA) to identify the most relevant descriptors and reduce dimensionality [8]
- Develop QSAR models using multiple linear regression (MLR) with descendant selection and variable removal [8]
- Validate models using both internal (R², Q²ₗₒₒ) and external validation (Q²Fₙ, CCCₑₓₜ) criteria [7] [8]
- Ensure statistical significance with correlation coefficients (R² > 0.8), Fisher's criteria (F), and low mean squared error (MSE) [8]
ADMET Integration and Compound Prioritization
- Predict key ADMET properties including water solubility (LogS), octanol-water partition coefficient (LogP), metabolic stability, and toxicity parameters [6] [8]
- Integrate ADMET predictions with QSAR activity models to establish multi-parameter optimization criteria
- Apply the integrated model for virtual screening of compound libraries to identify promising candidates [7]
Protocol 2: Comprehensive ADMET Profiling in Virtual Compound Screening
Objective: To implement a standardized protocol for virtual ADMET profiling of candidate compounds within a 3D-QSAR framework.
Materials:
- Curated compound library in appropriate digital format (SDF, MOL2)
- ADMET prediction software (OpenADMET, admetSAR, or equivalent)
- Molecular dynamics simulation software (GROMACS, AMBER)
- High-performance computing resources
Procedure:
Physicochemical Property Profiling
- Calculate fundamental physicochemical parameters including molecular weight, hydrogen bond donors/acceptors, rotatable bonds, topological polar surface area (TPSA) [8]
- Predict lipophilicity (LogP) using consensus algorithms to ensure accuracy
- Estimate solubility (LogS) using quantitative predictive models [8]
Pharmacokinetic Parameter Prediction
- Predict intestinal absorption using PSA and LogP-based models
- Estimate blood-brain barrier penetration potential for CNS activity or toxicity assessment
- Simulate plasma protein binding using structure-based and machine learning approaches
- Predict metabolic stability and identify potential metabolic soft spots [6]
Toxicity Risk Assessment
Integration with 3D-QSAR and Validation
- Correlate ADMET predictions with 3D-QSAR activity models
- Establish acceptable ADMET parameter ranges for lead compounds
- Prioritize compounds satisfying both potency and ADMET criteria
- Validate predictions with limited experimental testing for key candidates
Advanced Preclinical Models for ADMET Validation
The transition from computational prediction to experimental validation requires sophisticated preclinical models that faithfully recapitulate human physiology. Advanced model systems have emerged that bridge the gap between traditional in vitro assays and in vivo responses, providing more clinically relevant data on compound behavior.
Table 3: Advanced Preclinical Models for ADMET and Efficacy Assessment
| Model System | Key Applications | Advantages | Limitations |
|---|---|---|---|
| Cell Lines | High-throughput cytotoxicity screening, drug combination studies, initial efficacy assessment [4] | Reproducible, cost-effective, suitable for high-throughput applications [4] | Limited tumor heterogeneity representation, inadequate tumor microenvironment [4] |
| Organoids | Disease modeling, drug response investigation, immunotherapy evaluation, safety/toxicity studies [4] | Preserve phenotypic and genetic features of original tumor, more predictive than cell lines [4] | Complex and time-consuming to create, incomplete tumor microenvironment [4] |
| Patient-Derived Xenograft (PDX) Models | Biomarker discovery, clinical stratification, drug combination strategies [4] | Preserve tumor architecture and microenvironment, most clinically relevant preclinical model [4] | Expensive, resource-intensive, time-consuming, ethical considerations [4] |
| Integrated Multi-Stage Approach | Comprehensive biomarker hypothesis generation and validation [4] | Leverages advantages of each model type, builds robust pipeline for clinical translation [4] | Requires significant coordination and resources across platforms [4] |
The FDA's recent announcement regarding reduced animal testing requirements for monoclonal antibodies and other drugs, with acceptance of advanced approaches including organoids, underscores the growing importance of these human-relevant systems [4]. This regulatory evolution acknowledges the improved predictive value of these models and their potential to accelerate development while reducing costs.
Artificial Intelligence in ADMET and 3D-QSAR Modeling
Artificial intelligence has emerged as a transformative technology in drug discovery, particularly in enhancing the predictive accuracy of ADMET properties and 3D-QSAR models. AI approaches, including machine learning (ML), deep learning (DL), and natural language processing (NLP), are being integrated across the drug development pipeline to improve success rates by processing large datasets, identifying complex patterns, and making autonomous decisions [3] [1].
Machine learning techniques, particularly supervised learning algorithms such as support vector machines (SVMs), random forests, and deep neural networks, have demonstrated significant success in predicting bioactivity and ADMET properties [9]. These approaches enable the identification of complex, non-linear relationships between molecular structures and pharmacological outcomes that may elude traditional statistical methods. Deep learning architectures, including convolutional neural networks (CNNs) and recurrent neural networks (RNNs), have further enhanced predictive capabilities by automatically learning relevant features from raw molecular data [3] [9].
Generative models such as variational autoencoders (VAEs) and generative adversarial networks (GANs) have shown particular promise in de novo molecular design, enabling the generation of novel compounds with optimized ADMET profiles [9]. These approaches can explore chemical space more efficiently than traditional high-throughput screening, focusing on regions with higher probabilities of success. Reinforcement learning (RL) methods further refine this process by iteratively proposing molecular structures and receiving feedback based on multiple optimization parameters, including potency, selectivity, and ADMET properties [3] [9].
The integration of AI into ADMET prediction has yielded tangible advances in development efficiency. Companies such as Insilico Medicine and Exscientia have reported AI-designed molecules reaching clinical trials in record times, with one example progressing in just 12 months compared to the typical 4-5 years [3]. Similar approaches are being applied specifically to oncology projects, highlighting the potential of these technologies to address the particular challenges of cancer drug development.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Essential Research Reagents and Computational Tools for ADMET-Centric 3D-QSAR
| Tool Category | Specific Examples | Function in Research | Application Notes |
|---|---|---|---|
| Computational Chemistry Software | Gaussian 09W, ChemOffice [8] | Molecular geometry optimization, electronic descriptor calculation | Use DFT/B3LYP/6-31G(p,d) for optimal accuracy in quantum chemical calculations [8] |
| Descriptor Calculation Tools | PaDEL Descriptor [7] | Computation of molecular descriptors for QSAR modeling | Supports 2D and 3D descriptors; enables high-throughput screening of compound libraries |
| Statistical Analysis Packages | XLSTAT [8] | Development and validation of QSAR models, principal component analysis | Provides comprehensive statistical tools for model optimization and validation |
| Molecular Dynamics Software | GROMACS, AMBER [6] [7] | Simulation of drug-target interactions, binding stability assessment | 100 ns simulations recommended for adequate stability assessment [6] [7] |
| ADMET Prediction Platforms | OpenADMET, admetSAR | Prediction of absorption, distribution, metabolism, excretion, and toxicity | Use consensus approaches from multiple platforms for improved prediction accuracy |
| Specialized Cell Line Panels | CrownBio's cell line database [4] | Initial efficacy screening, biomarker correlation studies | Includes >500 genomically diverse cancer cell lines for comprehensive profiling [4] |
| Organoid Biobanks | CrownBio's organoid database [4] | Disease modeling, drug response investigation, toxicity assessment | Preserves phenotypic and genetic features of original tumors [4] |
| PDX Model Collections | CrownBio's PDX database [4] | Preclinical efficacy validation, biomarker discovery | Considered gold standard for preclinical research; preserves tumor microenvironment [4] |
The integration of ADMET prediction within 3D-QSAR modeling frameworks represents a paradigm shift in addressing the critical challenge of high attrition rates in oncology drug development. By frontloading ADMET assessment in the discovery process, researchers can identify potential liabilities earlier, prioritize compounds with higher probabilities of clinical success, and ultimately reduce the costly late-stage failures that have plagued oncology drug development. The combined power of advanced computational modeling, sophisticated preclinical systems, and artificial intelligence creates an unprecedented opportunity to transform the efficiency and success of cancer therapeutic development.
Future directions in this field will likely focus on the continued refinement of multi-parameter optimization algorithms that simultaneously balance potency, selectivity, and ADMET properties. The integration of multi-omics data into predictive models will further enhance their clinical relevance, while human-on-a-chip and microphysiological systems may provide even more sophisticated platforms for experimental ADMET validation. As these technologies mature, they hold the promise of fundamentally reshaping oncology drug development, potentially reversing the trend of high attrition rates and accelerating the delivery of effective therapies to cancer patients.
In the modern paradigm of cancer drug design, efficacy is only one part of the equation. A compound's success is equally dependent on its Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties, which collectively define its pharmacokinetic and safety profile [10]. Historically, a significant number of clinical failures have been attributed to unfavorable ADMET characteristics, underscoring the critical need for their early assessment in the drug discovery pipeline [10] [11]. Within cancer research, particularly in projects utilizing 3D Quantitative Structure-Activity Relationship (3D-QSAR) modeling, integrating ADMET prediction has become indispensable for optimizing lead compounds and reducing late-stage attrition [12] [8]. This Application Note details the practical integration of ADMET evaluation within 3D-QSAR-driven cancer drug discovery, providing structured data, definitive protocols, and essential tools for research scientists.
Core ADMET Properties in Cancer Drug Design
The following table summarizes the key ADMET properties, their definitions, and their specific significance in the context of developing oncology therapeutics.
Table 1: Key ADMET Properties and Their Role in Cancer Drug Design
| Property | Definition | Significance in Cancer Therapy |
|---|---|---|
| Absorption | The process by which a drug enters the systemic circulation from its site of administration [10]. | While IV administration is common, oral bioavailability is increasingly desired for patient convenience and chronic dosing [10]. |
| Distribution | The reversible transfer of a drug between the bloodstream and various tissues [10]. | Influences drug concentration at the tumor site. High plasma protein binding (e.g., to HSA or AAG) can restrict distribution [10]. |
| Metabolism | The enzymatic conversion of a drug into metabolites [10]. | Impacts exposure and duration of action. Inhibition of Cytochrome P450 (CYP) enzymes is a major source of drug-drug interactions [10]. |
| Excretion | The removal of the drug and its metabolites from the body [10]. | Renal and biliary/hepatic are primary routes. Transporters like P-gp can affect elimination and contribute to resistance [10]. |
| Toxicity | The potential of a drug to cause harmful effects [10]. | Includes organ-specific toxicity, genotoxicity (e.g., Ames test), and cardiotoxicity (e.g., hERG channel inhibition) [13]. |
Integrated Computational Protocols for 3D-QSAR and ADMET
The synergy between 3D-QSAR and ADMET modeling allows for the simultaneous optimization of a compound's potency and its pharmacokinetic profile. Below are detailed protocols for conducting these analyses.
Protocol 1: Developing a 3D-QSAR Model with ADMET Outlook
This protocol outlines the steps for creating a 3D-QSAR model with an emphasis on generating insights applicable to ADMET optimization [14] [12] [8].
Dataset Curation and Biological Activity
- Collect a series of compounds (typically 30-50) with known experimental biological activity (e.g., IC50 or MIC) against the cancer target of interest [14] [8].
- Convert the activity values to pIC50 (or pMIC) using the formula: pIC50 = -log10(IC50) for use as the dependent variable in the model [14] [8].
- Divide the dataset into a training set (≈80%) for model building and a test set (≈20%) for external validation [12] [8].
Molecular Modeling and Alignment
- Sketch and optimize the 3D structures of all compounds using software like SYBYL-X or Gaussian with a standardized method (e.g., Tripos force field or DFT/B3LYP/6-31G) [12] [8].
- Perform molecular alignment, which is a critical step. A common method is rigid body alignment based on a common scaffold or a putative pharmacophore [12].
Field Calculation and Model Generation
- Calculate molecular interaction fields using Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA) [14] [12].
- For CoMFA, compute steric (Lennard-Jones) and electrostatic (Coulombic) fields. For CoMSIA, additional fields like hydrophobic, hydrogen bond donor, and acceptor can be used [14] [12].
- Use the Partial Least Squares (PLS) regression method to correlate the field descriptors with the biological activity and generate the statistical model [12].
Model Validation and Interpretation
- Validate the model using Leave-One-Out (LOO) cross-validation to determine the cross-validated correlation coefficient (Q²). A Q² > 0.5 is generally considered acceptable [12].
- Calculate the non-cross-validated correlation coefficient (R²) and assess the predictive R² for the test set [12].
- Interpret the contour maps (e.g., green/yellow for favorable/unfavorable steric, blue/red for favorable/unfavorable electrostatic) to guide structural modifications for enhanced potency [12].
Protocol 2: Predicting and Analyzing ADMET Properties
This protocol describes the use of computational tools to evaluate the ADMET profile of compounds, either during or after the 3D-QSAR analysis [8] [13] [15].
Descriptor Calculation
- Calculate key physicochemical and topological descriptors for your compound set. Essential descriptors include:
In Silico ADMET Prediction
Data Integration and Compound Prioritization
- Compile the ADMET predictions and physicochemical data into a unified table.
- Filter compounds based on desirable ADMET profiles. For instance, apply rules like Lipinski's Rule of Five to prioritize compounds with drug-like properties [12] [15].
- Correlate favorable and unfavorable ADMET traits with structural features identified in the 3D-QSAR contour maps. This integrated analysis provides a powerful strategy for designing new analogs with balanced potency and pharmacokinetics.
The Scientist's Toolkit: Essential Research Reagents & Software
Successful implementation of the protocols above relies on a suite of computational tools and resources.
Table 2: Key Research Reagent Solutions for Integrated 3D-QSAR and ADMET Studies
| Tool Name | Type | Primary Function in Research |
|---|---|---|
| SYBYL-X | Software Suite | Industry-standard platform for molecular modeling, alignment, and performing CoMFA/CoMSIA studies [12]. |
| Gaussian 09W | Software | Performs quantum mechanical calculations (e.g., DFT) to compute electronic descriptors for QSAR [8]. |
| BIOVIA Discovery Studio | Software Suite | Provides comprehensive tools for calculating ADMET descriptors, predictive toxicity (TOPKAT), and analyzing QSAR models [13]. |
| AutoDock Vina/InstaDock | Software | Conducts molecular docking simulations to predict binding modes and affinities of compounds to target proteins [17] [12]. |
| PaDEL-Descriptor | Software | Generates a wide range of molecular descriptors and fingerprints from chemical structures for QSAR and machine learning [17]. |
| SwissADME / ADMETlab 3.0 | Web Server | Provides fast, user-friendly predictions of key pharmacokinetic and physicochemical properties [16]. |
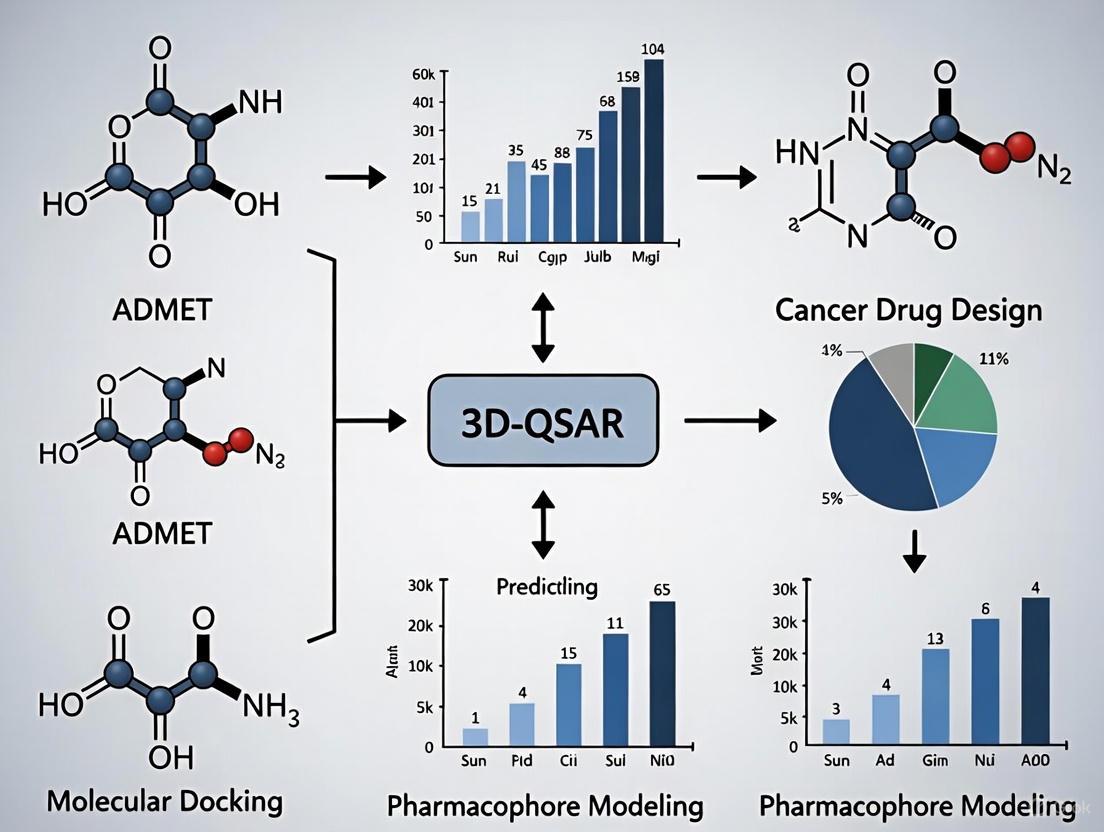
Visualizing the Workflow: From Chemical Structure to Optimized Candidate
The following diagram illustrates the integrated workflow combining 3D-QSAR modeling and ADMET prediction in cancer drug design.
Integrated 3D-QSAR and ADMET Workflow
Advanced Frontiers: AI and Federated Learning in ADMET Prediction
The field of ADMET prediction is being transformed by artificial intelligence (AI). Advanced deep learning models, such as the MSformer-ADMET, utilize a fragmentation-based approach for molecular representation, achieving superior performance across a wide range of ADMET endpoints by effectively modeling long-range dependencies [18]. Furthermore, the challenge of limited and heterogeneous data is being addressed through federated learning. This technique allows multiple pharmaceutical organizations to collaboratively train machine learning models on their distributed, proprietary datasets without sharing the underlying data, significantly expanding the model's chemical space coverage and predictive robustness for novel compounds [11]. The integration of AI-augmented PBPK models also shows great promise, enabling the prediction of a drug's full pharmacokinetic and pharmacodynamic profile directly from its structural formula early in the discovery stage [16].
Quantitative Structure-Activity Relationship (QSAR) modeling represents a cornerstone of computational medicinal chemistry, mathematically linking a chemical compound's structure to its biological activity or properties [19]. While traditional 2D-QSAR utilizes molecular descriptors derived from two-dimensional structures, Three-Dimensional QSAR (3D-QSAR) has emerged as a pivotal advancement that incorporates the essential spatial characteristics of molecules. These techniques are particularly valuable in cancer drug discovery, where understanding the intricate interactions between potential drug candidates and their biological targets is crucial for designing effective therapeutics with optimized ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties [20].
The fundamental principle underlying 3D-QSAR is that biological activity correlates not only with chemical composition but profoundly with three-dimensional molecular structure, including steric (shape-related) and electrostatic (charge-related) features. This approach operates on the concept that a ligand's interaction with a biological target depends on its ability to fit spatially and electronically into a binding site [21]. In the context of cancer research, 3D-QSAR enables researchers to systematically explore structural requirements for inhibiting specific oncology targets, thereby guiding the rational design of novel anticancer agents with improved potency and selectivity.
Among various 3D-QSAR methodologies, Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA) have become the most widely adopted and validated approaches. These techniques have demonstrated significant utility across multiple cancer types, including breast cancer [22] [8] [23], chronic myeloid leukemia [24], and osteosarcoma [25], providing medicinal chemists with powerful tools to accelerate anticancer drug development while reducing reliance on costly synthetic experimentation.
Theoretical Foundations of CoMFA and CoMSIA
Core Conceptual Framework
The CoMFA methodology, introduced in the 1980s, is founded on the concept that molecular interaction fields surrounding ligands constitute the primary determinants of biological activity. This approach assumes that the non-covalent interaction between a ligand and its receptor can be approximated by steric and electrostatic forces [21]. In practice, CoMFA characterizes molecules based on their steric (van der Waals) and electrostatic (Coulombic) potentials sampled at regularly spaced grid points surrounding the molecules. These potentials are calculated using probe atoms and are correlated with biological activity through Partial Least Squares (PLS) regression, generating a model that visualizes regions where specific structural modifications would enhance or diminish biological activity [24].
CoMSIA emerged as an extension and refinement of CoMFA, addressing some of its limitations by introducing Gaussian-type distance dependence and additional molecular field types. While CoMFA utilizes Lennard-Jones and Coulomb potentials that can exhibit sharp fluctuations near molecular surfaces, CoMSIA employs a smoother potential function that avoids singularities and provides more stable results [26]. Beyond the steric and electrostatic fields shared with CoMFA, CoMSIA typically incorporates hydrophobic, hydrogen bond donor, and hydrogen bond acceptor fields, offering a more comprehensive description of ligand-receptor interactions [26].
Comparative Analysis of CoMFA and CoMSIA
Table 1: Fundamental Comparison Between CoMFA and CoMSIA Approaches
| Feature | CoMFA | CoMSIA |
|---|---|---|
| Field Types | Steric, Electrostatic | Steric, Electrostatic, Hydrophobic, Hydrogen Bond Donor, Hydrogen Bond Acceptor |
| Potential Function | Lennard-Jones, Coulomb | Gaussian-type |
| Distance Dependence | Proportional to 1/r^n | Exponential decay |
| Grid Calculations | Probe atom interactions at grid points | Similarity indices calculated at grid points |
| Results Stability | Sensitive to molecular orientation | Less sensitive to alignment |
| Contour Maps | Sometimes discontinuous | Generally smooth and interpretable |
The selection between CoMFA and CoMSIA depends on the specific research context. CoMFA often provides models with high predictive ability for congeneric series, while CoMSIA can capture more complex interactions through its additional fields and may be more suitable for structurally diverse datasets [26]. In cancer drug design, both techniques have demonstrated excellent predictive capabilities, with recent studies reporting statistically robust models with correlation coefficients (R²) often exceeding 0.85-0.90 and cross-validated coefficients (Q²) above 0.5 [26] [25] [24].
Computational Protocols and Methodologies
Standardized Workflow for 3D-QSAR Analysis
The development of robust 3D-QSAR models follows a systematic workflow encompassing multiple critical stages. Adherence to this protocol ensures the generation of statistically significant and predictive models that can reliably guide cancer drug design efforts.
Figure 1: Standard workflow for developing 3D-QSAR models using CoMFA and CoMSIA methodologies.
Detailed Experimental Protocol
Step 1: Dataset Compilation and Preparation
- Compound Selection: Curate a structurally diverse set of 20-100 compounds with consistent, quantitatively measured biological activity (e.g., IC₅₀, Ki) against the cancer target of interest [25] [24]. The activities are typically converted to pIC₅₀ (-logIC₅₀) for analysis.
- Training/Test Set Division: Implement a rational division (typically 80:20 ratio) to ensure the test set represents the structural diversity and activity range of the training set [8]. Random sampling based on system time or activity-based sorting followed by regular interval selection are common approaches [25].
Step 2: Molecular Modeling and Conformational Analysis
- Structure Building: Construct molecular structures using chemoinformatics software (ChemDraw, Sybyl-X, HyperChem) [26] [25].
- Geometry Optimization: Perform molecular mechanics (MM+ force field) for preliminary optimization followed by semi-empirical (AM1 or PM3) or DFT (B3LYP/6-31G) methods for precise geometry optimization [25] [8].
- Conformational Analysis: Identify the bioactive conformation through systematic search, molecular dynamics, or by extracting from crystallographic complexes when available [27].
Step 3: Molecular Alignment
- Atom-Based Fit: Align molecules based on common substructure or pharmacophore using RMSD atom fitting [24].
- Field Fit: Use the field points themselves to guide alignment [21].
- Database Alignment: Align to a known active compound or native ligand [26]. This step is critically important as alignment quality directly impacts model performance.
Step 4: Field Calculations and Descriptor Generation
- CoMFA Field Calculation:
- Place aligned molecules in a 3D grid (typically 2.0 Å spacing)
- Calculate steric (Lennard-Jones) and electrostatic (Coulombic) potentials using sp³ carbon and +1 charge probes
- Set energy cutoffs (30 kcal/mol) to avoid extreme values [24]
- CoMSIA Field Calculation:
- Calculate five similarity fields: steric, electrostatic, hydrophobic, hydrogen bond donor, hydrogen bond acceptor
- Use Gaussian-type distance dependence with attenuation factor (typically 0.3) [26]
Step 5: Partial Least Squares (PLS) Analysis
- Variable Preprocessing: Apply standard scaling (Coefficient × STDEV) to field values [24]
- PLS Regression: Correlate field variables with biological activity while addressing multicollinearity
- Optimal Component Determination: Use cross-validation (leave-one-out or leave-group-out) to identify components maximizing Q² [26] [24]
Step 6: Model Validation and Evaluation
- Internal Validation: Assess using cross-validated correlation coefficient (Q²), conventional correlation coefficient (R²), standard error of estimate (SEE), and F-value [26]
- External Validation: Predict test set activities and calculate predictive R² (R²pred) [8]
- Robustness Testing: Apply Y-randomization to confirm model non-randomness [23]
Application to ADMET Property Prediction in Cancer Research
The integration of 3D-QSAR with ADMET profiling represents a powerful strategy in cancer drug design, enabling simultaneous optimization of both efficacy and safety profiles. Recent studies have successfully implemented this integrated approach:
Table 2: 3D-QSAR Applications in Cancer Drug Discovery with ADMET Integration
| Cancer Type | Target | Compound Series | Key ADMET Findings | Reference |
|---|---|---|---|---|
| Breast Cancer | Tubulin (Colchicine site) | 1,2,4-Triazine-3(2H)-one derivatives | Absolute electronegativity (χ) and water solubility (LogS) significantly influence activity; optimized compounds showed favorable pharmacokinetic profiles | [8] |
| Breast Cancer | Aromatase | Heterocyclic derivatives | QSAR-ANN models combined with ADMET prediction identified candidate L5 with improved metabolic stability | [23] |
| Chronic Myeloid Leukemia | Bcr-Abl | Purine derivatives | CoMFA/CoMSIA guided design of compounds with enhanced potency against T315I mutant and reduced cytotoxicity | [24] |
| Breast Cancer | Topoisomerase IIα | Naphthoquinone derivatives | ADMET screening of 2300 compounds identified 16 promising candidates; molecular dynamics confirmed stability | [22] |
In practice, 3D-QSAR models can directly predict ADMET-related properties by using pharmacokinetic parameters (e.g., solubility, permeability, metabolic stability) as the dependent variable instead of biological activity. This application is particularly valuable in cancer drug design, where therapeutic windows are often narrow and toxicity concerns are paramount.
Successful implementation of 3D-QSAR studies requires access to specialized software tools and computational resources. The following table summarizes key components of the 3D-QSAR research toolkit:
Table 3: Essential Research Reagents and Computational Tools for 3D-QSAR
| Tool Category | Specific Software/Resources | Primary Function | Application in Protocol | |
|---|---|---|---|---|
| Molecular Modeling | ChemDraw, HyperChem, Sybyl-X | Structure building, preliminary optimization | Steps 1-2: Compound construction and geometry optimization | [26] [25] |
| Quantum Chemical | Gaussian 09W, AM1, PM3 methods | High-level geometry optimization, electronic property calculation | Step 2: Precise molecular structure optimization | [8] |
| 3D-QSAR Specific | CORAL, COMSIA/Sybyl, CODESSA | Descriptor calculation, model development | Steps 3-5: Field calculation, PLS analysis, model generation | [22] [25] |
| Molecular Descriptors | PaDEL-Descriptor, Dragon, RDKit | Calculation of diverse molecular descriptors | Alternative descriptor sources for comparative modeling | [19] |
| Docking & Dynamics | AutoDock, GROMACS, AMBER | Protein-ligand interaction analysis, binding stability assessment | Post-QSAR validation of designed compounds | [22] [8] |
| Statistical Analysis | XLSTAT, inbuilt PLS in QSAR packages | Statistical correlation, model validation | Step 6: Model validation and statistical analysis | [8] |
Case Study: 3D-QSAR in Breast Cancer Tubulin Inhibitor Design
A recent investigation on 1,2,4-triazine-3(2H)-one derivatives as tubulin inhibitors for breast cancer therapy exemplifies the integrated application of 3D-QSAR in oncology drug discovery [8]. This study developed robust QSAR models achieving a predictive accuracy (R²) of 0.849, identifying absolute electronegativity and water solubility as critical determinants of inhibitory activity. The subsequent molecular docking revealed compound Pred28 with exceptional binding affinity (-9.6 kcal/mol) to the tubulin colchicine site, while ADMET profiling confirmed favorable pharmacokinetic properties.
The research workflow incorporated:
- 3D-QSAR Model Development: Using a dataset of 32 compounds with anti-MCF-7 activity
- Descriptor Selection: Combining electronic (EHOMO, ELUMO, electronegativity) and topological (LogP, LogS, polar surface area) descriptors
- Model Validation: Rigorous internal and external validation following OECD principles
- Molecular Dynamics: 100 ns simulations confirming complex stability (RMSD 0.29 nm)
- ADMET Integration: Comprehensive pharmacokinetic prediction guiding compound selection
This case demonstrates how 3D-QSAR serves as the central component in a multi-technique computational framework, efficiently bridging structural optimization with pharmacological profiling in cancer drug design.
Advanced Applications and Future Perspectives in Cancer Therapeutics
The continuing evolution of 3D-QSAR methodologies promises enhanced capabilities for anticancer drug development. Emerging trends include:
- 4D-QSAR Approaches: Incorporating ensemble sampling of multiple ligand conformations to account for flexibility [20]
- QSAR-ANN Integration: Combining 3D-QSAR with artificial neural networks to capture non-linear structure-activity relationships [23]
- Hybrid QSAR-Docking Models: Leveraging both ligand-based and structure-based design principles [22] [24]
- Multi-Target QSAR: Developing models that simultaneously optimize activity against multiple cancer targets while maintaining favorable ADMET profiles
These advanced applications position 3D-QSAR as an increasingly indispensable component of integrated cancer drug discovery platforms, potentially accelerating the development of novel therapeutics with optimized efficacy and safety profiles.
Why 3D-QSAR is Uniquely Suited for Modeling Ligand-Receptor Interactions
Abstract Within the paradigm of cancer drug design, predicting ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties is crucial for lead optimization. This application note posits that 3D-QSAR (Three-Dimensional Quantitative Structure-Activity Relationship) is uniquely suited for modeling the foundational event of this process: ligand-receptor interactions. By explicitly incorporating the spatial and electronic fields of molecules, 3D-QSAR provides a superior framework for understanding and predicting biological activity, thereby directly informing ADMET characteristics. We detail the protocols and experimental rationale for employing 3D-QSAR in this context.
1. Introduction: The 3D-QSAR Advantage in ADMET Prediction Traditional 2D-QSAR relies on molecular descriptors derived from a compound's topological structure, which often fail to capture the stereoelectronic complementarity essential for ligand-receptor binding. In cancer drug design, where targets are often kinases, GPCRs, or nuclear receptors, this spatial recognition is paramount. 3D-QSAR techniques, such as Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA), model biological activity as a function of interaction fields (steric, electrostatic, hydrophobic, etc.) surrounding a set of aligned molecules. This directly mirrors the physical reality of the receptor binding pocket, making it exceptionally powerful for predicting binding affinity—a key driver of many ADMET properties.
2. Application Notes: Correlating 3D Fields with ADMET Endpoints The following table summarizes how specific 3D-QSAR field contributions can be mapped to critical ADMET parameters in oncology drug discovery.
Table 1: Mapping 3D-QSAR Field Contributions to ADMET Properties
| ADMET Property | Relevant 3D-QSAR Field | Correlation & Rationale | Exemplary Statistical Output (Hypothetical Dataset) |
|---|---|---|---|
| Absorption (Caco-2 Permeability) | Hydrophobic (CoMSIA) | Positive contribution in specific regions indicates enhanced passive transcellular diffusion. | q² = 0.72, R² = 0.88, Hydrophobic Contour: 45% |
| hERG Channel Inhibition (Cardiotoxicity) | Electrostatic (CoMFA/CoMSIA) | Presence of negative electrostatic potential near a basic nitrogen correlates with hERG binding. | q² = 0.68, R² = 0.85, Electrostatic Contour: 60% |
| CYP3A4 Inhibition (Metabolism) | Steric & Hydrogen Bond Acceptor | Bulky groups in defined regions block access; H-bond acceptors coordinate heme iron. | q² = 0.65, R² = 0.82, Steric Contour: 30%, H-Bond Acceptor: 25% |
| Plasma Protein Binding (Distribution) | Hydrophobic & Electrostatic | Extensive hydrophobic fields increase binding to albumin; negative charges to α1-acid glycoprotein. | q² = 0.70, R² = 0.86, Hydrophobic Contour: 50% |
3. Experimental Protocols
Protocol 1: Standard CoMFA/CoMSIA Workflow for Kinase Inhibitor Design This protocol outlines the steps for developing a 3D-QSAR model to predict the inhibitory activity (IC₅₀) of a congeneric series of kinase inhibitors, with simultaneous assessment of hERG liability.
I. Ligand Preparation & Conformational Analysis
- Data Curation: Compile a dataset of 40-50 compounds with experimentally determined IC₅₀ values against the target kinase and hERG. Ensure a ~4 log unit spread in activity.
- Structure Preparation: Draw or import all 2D structures into a molecular modeling suite (e.g., Schrödinger Maestro, SYBYL-X). Generate plausible 3D geometries using a force field (e.g., MMFF94s).
- Energy Minimization: Optimize each structure to a gradient convergence of 0.05 kcal/mol·Å.
- Partial Charge Assignment: Calculate Gasteiger-Marsili or AM1-BCC partial charges.
II. Molecular Alignment (The Critical Step)
- Select a Template: Choose the most active and rigid molecule as the template for alignment.
- Common Substructure Alignment: Identify a common pharmacophore or scaffold present in all molecules. Superimpose all molecules onto this scaffold of the template.
- Database Alignment: Save the aligned molecule set for CoMFA/CoMSIA analysis.
III. Field Calculation & PLS Analysis
- CoMFA Setup: Place aligned molecules in a 3D grid (2.0 Å spacing). A sp³ carbon probe with a +1 charge calculates steric (Lennard-Jones) and electrostatic (Coulombic) fields.
- CoMSIA Setup (Optional): Calculate similarity indices for steric, electrostatic, hydrophobic, and hydrogen-bond donor/acceptor fields (probe radius 1.0 Å, attenuation factor 0.3).
- Partial Least Squares (PLS) Analysis: The software correlates the field values (independent variables) with the pIC₅₀ values (dependent variable). Use Leave-One-Out (LOO) cross-validation to determine the optimal number of components (ONC) and calculate q².
- Model Generation: Run a conventional analysis using the ONC to generate the final model with R², standard error of estimate, and F-value.
IV. Model Validation & Visualization
- External Validation: Predict the activity of a test set of 10-15 compounds not used in model building. Calculate predictive R² (R²pred).
- Contour Map Analysis: Visualize the CoMFA/CoMSIA steric (green/yellow) and electrostatic (blue/red) contour maps around the template. Green contours indicate regions where bulky groups increase activity; blue contours indicate regions where positive charge increases activity.
4. Visualizing the 3D-QSAR Workflow and ADMET Integration
Title: 3D-QSAR-ADMET Workflow
5. The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Software for 3D-QSAR in Cancer Drug Discovery
| Item / Solution | Function / Rationale | Example Vendor / Product |
|---|---|---|
| Molecular Modeling Suite | Integrated platform for ligand preparation, alignment, force field calculation, and 3D-QSAR analysis. | Schrödinger Maestro, OpenEye Orion, BIOVIA Discovery Studio |
| Crystallographic Protein Database (PDB) | Source of high-resolution receptor structures for guiding molecular alignment and validating contour maps. | RCSB Protein Data Bank (www.rcsb.org) |
| Standardized Bioassay Data | Curated datasets of IC₅₀, Ki, etc., for model training and validation. Critical for a robust model. | ChEMBL, PubChem BioAssay |
| Force Field Parameters | Set of mathematical functions and constants for calculating molecular energy and geometry. | MMFF94s, OPLS4, GAFF |
| PLS Analysis Toolkit | Statistical engine for correlating thousands of field variables with biological activity. | Integrated within major modeling suites (e.g., SYBYL) |
| High-Performance Computing (HPC) Cluster | Accelerates computationally intensive steps like conformational search and cross-validation. | Local or cloud-based Linux clusters |
The integration of three-dimensional Quantitative Structure-Activity Relationship (3D-QSAR) modeling with Artificial Intelligence (AI) represents a paradigm shift in computational drug discovery, particularly within oncology research. This powerful synergy is transforming the design and optimization of cancer therapeutics by enhancing predictive accuracy while simultaneously addressing the critical pharmacokinetic and safety profiles essential for clinical success [28]. Traditional 3D-QSAR approaches, including Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA), establish correlations between the spatial and electrostatic properties of molecules and their biological activity [24]. When augmented by AI algorithms, these models gain unprecedented capability to navigate complex chemical spaces and identify novel compounds with optimized target affinity and ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties [29] [9]. This application note details protocols and case studies demonstrating the effective confluence of these technologies in cancer drug design, providing researchers with practical frameworks for implementation.
Computational Methodologies and Workflows
Integrated 3D-QSAR and AI Protocol
The following workflow outlines a standardized protocol for leveraging integrated 3D-QSAR and AI in cancer drug discovery projects. This methodology has been validated across multiple kinase inhibitor development programs [24] [23].
Protocol 1: Integrated Model Development and Validation
Step 1: Compound Selection and Preparation
- Select a structurally diverse dataset of 50-100 compounds with experimentally determined biological activities (e.g., IC₅₀, Ki) [24].
- Prepare all molecular structures using molecular mechanics force fields (MMFF94 or OPLS4) for energy minimization.
- Perform molecular alignment using common scaffold-based or field-based methods to ensure consistent orientation within the molecular grid.
Step 2: 3D-QSAR Model Construction
- Calculate steric (Lennard-Jones) and electrostatic (Coulombic) field energies at grid points surrounding the aligned molecules.
- Apply Partial Least Squares (PLS) regression to correlate field descriptors with biological activity.
- Validate models using leave-one-out (LOO) cross-validation and external test sets (minimum q² > 0.5, R² > 0.8) [24].
Step 3: AI-Enhanced Feature Optimization
- Extract contour maps highlighting regions where steric bulk or specific electrostatic charges enhance or diminish activity.
- Use these pharmacophoric patterns as feature inputs for graph neural networks (GNNs) or random forest algorithms [28] [9].
- Implement automated machine learning (AutoML) platforms such as DeepAutoQSAR to optimize descriptor selection and model architecture [30].
Step 4: Virtual Compound Design and Screening
- Apply trained AI models to generate novel virtual compounds or screen large chemical libraries (>10⁶ compounds).
- Prioritize candidates based on predicted activity and synthetic accessibility scores.
- Output top candidates for synthesis and biological validation.
ADMET Integration Protocol
Early integration of ADMET prediction is crucial for reducing late-stage attrition in oncology drug development [31] [32].
Protocol 2: AI-Driven ADMET Profiling
Step 1: Multi-Endpoint ADMET Prediction
Step 2: ADMET Risk Scoring
- Implement integrated risk assessment algorithms that combine multiple ADMET parameters into unified risk scores [31].
- Apply "soft" thresholding where predictions falling in intermediate ranges contribute fractional amounts to the overall risk score.
- Calculate specific risk components (AbsnRisk, CYPRisk, TOXRisk) and combine into a comprehensive ADMETRisk score [31].
Step 3: Multi-Parameter Optimization
- Employ AI-based consensus scoring to balance potency predictions with ADMET profiles [9] [32].
- Use reinforcement learning to iteratively refine compound structures toward optimal activity-ADMET trade-offs.
- Apply explainable AI (XAI) methods (SHAP, LIME) to identify structural features driving both activity and toxicity predictions [28].
Case Study: Bcr-Abl Inhibitors for Leukemia Therapy
A recent investigation developed novel Bcr-Abl inhibitors to combat imatinib resistance in chronic myeloid leukemia, demonstrating the power of integrated 3D-QSAR and AI methodologies [24].
Experimental Implementation
- Dataset: 58 purine-based Bcr-Abl inhibitors with experimentally determined IC₅₀ values
- 3D-QSAR Models: CoMFA and CoMSIA with steric, electrostatic, hydrophobic, and hydrogen-bonding fields
- Statistical Validation: CoMFA (q² = 0.62, R² = 0.98); CoMSIA (q² = 0.59, R² = 0.97) [24]
- AI Integration: Molecular dynamics simulations and free energy calculations to validate binding modes
- ADMET Profiling: Comprehensive toxicity and pharmacokinetic assessment including plasma protein binding and metabolic stability
Key Quantitative Results
Table 1: Experimental Results for Selected Designed Purine Derivatives [24]
| Compound | Bcr-Abl IC₅₀ (μM) | Cellular GI₅₀ (μM) | Selectivity Index | ADMET Risk Score |
|---|---|---|---|---|
| 7a | 0.13 | 0.45 | 12.3 | 2.1 |
| 7c | 0.19 | 0.30 | 15.8 | 1.8 |
| 7e | 0.42 | 13.80 | 4.2 | 3.5 |
| Imatinib | 0.33 | 0.85 | 8.5 | 2.8 |
Table 2: Predicted ADMET Properties for Lead Compounds [31] [24]
| Property | 7a | 7c | Imatinib | Optimal Range |
|---|---|---|---|---|
| Caco-2 Permeability | 22.5 | 25.8 | 18.3 | >15 |
| hERG Inhibition | Low | Low | Medium | Low |
| CYP3A4 Inhibition | Moderate | Low | High | Low |
| Hepatotoxicity | Low | Low | Low | Low |
| Plasma Protein Binding (%) | 88.2 | 85.6 | 92.5 | <95 |
| Human Absorption (%) | 75.4 | 82.1 | 98.3 | >70 |
The 3D-QSAR contour maps revealed critical structural requirements: favorable steric bulk near the C2 position, electron-donating groups at the C6 phenylamino fragment, and limited hydrophobicity at the N9 substituent [24]. These insights directly informed the AI-driven design of compounds 7a and 7c, which exhibited superior potency and selectivity compared to imatinib, particularly against resistant cell lines expressing the T315I mutation.
Research Reagent Solutions
Table 3: Essential Computational Tools for Integrated 3D-QSAR/AI Research
| Tool Category | Representative Solutions | Key Functionality |
|---|---|---|
| 3D-QSAR Platforms | SYBYL, Open3DQSAR | CoMFA, CoMSIA, molecular field calculation, pharmacophore mapping |
| AI/ML Modeling | DeepAutoQSAR [30], Chemprop [33], Receptor.AI [32] | Automated machine learning, graph neural networks, multi-task learning |
| ADMET Prediction | ADMET Predictor [31], ADMETlab 3.0 [33], ProTox 3.0 [33] | Prediction of 175+ ADMET properties, risk assessment, species-specific modeling |
| Molecular Dynamics | GROMACS, Desmond, OpenMM | Binding mode validation, free energy calculations, conformational sampling |
| Cheminformatics | RDKit, KNIME [28], PaDEL | Descriptor calculation, fingerprint generation, data preprocessing |
Workflow Visualization
Integrated 3D-QSAR and AI Workflow
AI-Driven ADMET Assessment Pathway
The strategic integration of 3D-QSAR modeling with artificial intelligence represents a transformative advancement in cancer drug design. This synergistic approach enables researchers to simultaneously optimize for target potency and drug-like properties, significantly improving the efficiency of the lead discovery and optimization process. The protocols and case studies presented herein provide a practical framework for implementing these methodologies, with particular emphasis on addressing the critical challenge of ADMET prediction in oncology research. As AI technologies continue to evolve and experimental datasets expand, this confluence promises to further accelerate the development of safer, more effective cancer therapeutics.
A Practical Workflow: Applying 3D-QSAR and ML for ADMET Optimization
In modern cancer drug design, the prediction of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties has become a critical determinant of success, with approximately 40-45% of clinical attrition still attributed to ADMET liabilities [11] [34]. Three-Dimensional Quantitative Structure-Activity Relationship (3D-QSAR) modeling represents a sophisticated computational approach that transcends traditional 2D methods by incorporating the spatial characteristics of molecules, thereby providing more accurate predictions of their biological activity and pharmacological properties [35] [36]. When strategically integrated with ADMET prediction platforms, 3D-QSAR forms a powerful framework for prioritizing drug candidates with optimal efficacy and safety profiles early in the discovery pipeline [34].
The significance of robust 3D-QSAR modeling is particularly evident in oncology drug development, where success rates remain well below the already low 10% average for new chemical entities [1]. This application note provides a comprehensive protocol for constructing, validating, and implementing 3D-QSAR models within the context of cancer drug discovery, with emphasis on ADMET property prediction to reduce late-stage failures.
Dataset Curation and Preparation
Compound Selection and Activity Data
The foundation of any predictive 3D-QSAR model lies in the quality and relevance of the training dataset. For cancer drug design, select compounds with:
- Consistent biological activity data (IC₅₀, EC₅₀, or Kᵢ) obtained from uniform experimental assays targeting relevant oncology targets (e.g., aromatase for breast cancer [23] or Mcl-1 for leukemia [37])
- Structural diversity covering multiple chemotypes and scaffolds to ensure broad applicability domain
- Potency range spanning at least 3-4 orders of magnitude to capture meaningful structure-activity relationships [38]
Table 1: Activity Data Preparation Standards
| Parameter | Requirement | Processing Method |
|---|---|---|
| Activity Values | Experimentally consistent IC₅₀/Kᵢ | Convert to pIC₅₀ or pKᵢ (-log10) [38] |
| Value Range | Minimum 3-order magnitude spread | Logarithmic transformation |
| Data Source | Homogeneous assay conditions | Curate from single source or normalize cross-dataset |
Molecular Modeling and Conformation Generation
Accurate 3D molecular representation is essential for meaningful steric and electrostatic field analysis:
- Structure Building: Construct initial 3D structures using molecular modeling software (ChemDraw, Sybyl-X [35] or Schrodinger Suite [38])
- Geometry Optimization: Perform energy minimization using molecular mechanics force fields (MMFF94 or OPLS4) to obtain low-energy conformations [38]
- Conformational Sampling: Generate representative ligand conformations considering biological flexibility requirements [35]
Molecular Alignment
Molecular alignment is the most critical step in 3D-QSAR model development, directly determining model interpretability and predictive power:
- Identify a rigid reference compound with high activity and structural similarity to other dataset members
- Extract common substructure or pharmacophoric features shared across the dataset
- Align all molecules using flexible ligand alignment algorithms [38] or crystallographic pose-based alignment when receptor structure is available
Model Building and Validation
Field Calculation and Descriptor Generation
Modern 3D-QSAR approaches utilize sophisticated field calculation methods:
- Comparative Molecular Field Analysis (CoMFA): Calculates steric (Lennard-Jones) and electrostatic (Coulombic) potentials at grid points surrounding aligned molecules [35]
- Comparative Molecular Similarity Indices Analysis (CoMSIA): Extends beyond CoMFA to include hydrophobic, hydrogen bond donor, and acceptor fields [35]
- Machine Learning-Enhanced 3D-QSAR: Incorporate 3D descriptors into ML algorithms (Random Forest, SVM, Multilayer Perceptron) for improved predictive performance [36]
Statistical Modeling and Validation
Robust model validation is essential for ensuring predictive reliability:
Table 2: 3D-QSAR Model Validation Parameters and Benchmarks
| Validation Type | Statistical Metric | Acceptance Threshold | Interpretation |
|---|---|---|---|
| Internal Validation | q² (LOO cross-validation) | > 0.5 | Good predictive ability |
| Goodness of Fit | r² (conventional) | > 0.8 | High explanatory power |
| Model Stability | F-value | Higher = better | Statistical significance |
| Standard Error | SEE | Lower = better | Model precision |
| External Validation | Predictive r² (r²pred) | > 0.6 | Good external predictivity |
The model development process should yield statistically significant parameters, such as those demonstrated in a recent neuroprotective drug study where the CoMSIA model achieved q² = 0.569 and r² = 0.915 [35], or in anticancer research where models underwent "rigorous internal and external validations based on significant statistical parameters" [23].
Machine Learning Integration in 3D-QSAR
Machine learning algorithms significantly enhance traditional 3D-QSAR approaches:
- Algorithm Selection: Implement Multiple Linear Regression (MLR), Random Forest (RF), Support Vector Machine (SVM), or Multilayer Perceptron (MLP) based on dataset characteristics [36] [39]
- Feature Importance Analysis: Employ SHAP analysis or similar methods to identify key descriptors influencing predictions [39]
- Model Interpretation: Combine predictive power with mechanistic insights into structure-activity relationships [39]
Recent studies demonstrate that "3D-QSAR models, which employ algorithms such as random forest (RF), support vector machine (SVM), and multilayer perceptron (MLP), outperform the VEGA models in terms of accuracy, sensitivity, and selectivity" [36].
ADMET Integration in Cancer Drug Design
ADMET Prediction Workflow
Incorporate ADMET prediction seamlessly into the 3D-QSAR workflow:
- Early-Stage Screening: Prioritize compounds with favorable predicted ADMET profiles before synthesis [34]
- Multi-Parameter Optimization: Balance potency against ADMET properties using desirability functions or scoring algorithms
- Hit-to-Lead Expansion: Guide structural modifications to improve problematic ADMET characteristics while maintaining efficacy
Key ADMET Endpoints for Cancer Drugs
Focus computational ADMET prediction on endpoints most relevant to oncology candidates:
- Metabolic Stability (human liver microsomal clearance) [11]
- Membrane Permeability (Caco-2/MDR1-MDCKII models) [11]
- Solubility (critical for formulation and bioavailability) [11]
- hERG Inhibition (cardiotoxicity risk assessment)
- CYP450 Inhibition (drug-drug interaction potential) [34]
Machine learning-based ADMET prediction platforms such as ADMETlab 2.0 provide integrated solutions for these endpoints, demonstrating that "ML-based models have demonstrated significant promise in predicting key ADMET endpoints, outperforming some traditional quantitative structure-activity relationship (QSAR) models" [34].
Experimental Protocol: 3D-QSAR Model Development
Required Materials and Software
Table 3: Essential Research Reagents and Computational Tools
| Category | Specific Tool/Resource | Application in Protocol |
|---|---|---|
| Molecular Modeling | Schrodinger Suite, Sybyl-X, ChemDraw | Compound building, optimization, conformational analysis [35] [38] |
| 3D-QSAR Software | Open3DALIGN, ROCS, Phase | Molecular alignment, field calculation, model building [35] |
| Machine Learning | Scikit-learn, TensorFlow, Keras | Implementation of RF, SVM, MLP algorithms [36] [39] |
| ADMET Platforms | ADMETlab 2.0, pkCSM, PreADMET | Prediction of pharmacokinetic and toxicity properties [34] |
| Validation Tools | KNIME, Python/R scripts | Statistical validation, applicability domain assessment |
Step-by-Step Procedure
Phase I: Data Preparation (1-2 Days)
- Curate dataset of 30-50 compounds with consistent biological activity data [38]
- Convert activity values to pIC₅₀ or pKᵢ using the formula: pIC₅₀ = -log₁₀(IC₅₀) [38]
- Divide dataset using activity-stratified partitioning into:
- Training set (70-80% for model building)
- Test set (20-30% for external validation) [40]
- Generate 3D structures and optimize geometry using molecular mechanics force fields [35]
- Perform molecular alignment using a common substructure or pharmacophore hypothesis [38]
Phase II: Model Construction (2-3 Days)
- Calculate interaction fields using CoMFA/CoMSIA approaches with default grid spacing (2Å)
- Extract 3D molecular descriptors for machine learning-enhanced models [36]
- Apply partial least-squares (PLS) analysis with leave-one-out (LOO) cross-validation for traditional 3D-QSAR [35]
- Train machine learning models using training set compounds and descriptors
- Optimize model parameters through grid search or genetic algorithms
Phase III: Validation and Application (1-2 Days)
- Assess internal validation through q² and other statistical parameters [35]
- Evaluate external predictivity using the test set compounds
- Define applicability domain to identify compounds within model scope [39]
- Deploy model for virtual screening of novel compounds
- Integrate ADMET predictions for comprehensive candidate prioritization [34]
Advanced Applications in Cancer Drug Discovery
Federated Learning for Enhanced ADMET Prediction
Recent advances in federated learning address the critical challenge of data diversity in ADMET prediction:
- Cross-organization collaboration: Train models on distributed proprietary datasets without data sharing [11]
- Expanded applicability domain: Improved prediction for novel scaffolds and chemical space [11]
- Heterogeneous data integration: Superior models even with varied assay protocols and compound libraries [11]
Studies demonstrate that "federated models systematically outperform local baselines, and performance improvements scale with the number and diversity of participants" [11], making this approach particularly valuable for predicting ADMET properties of novel anticancer scaffolds.
Case Study: Anticancer Drug Discovery Pipeline
A recent integrative computational strategy for breast cancer drug discovery exemplifies the power of combining 3D-QSAR with ADMET prediction:
- Initial 3D-QSAR and ANN modeling identified 12 novel drug candidates (L1-L12) targeting aromatase [23]
- Virtual screening techniques prioritized one hit (L5) showing significant potential compared to reference drug exemestane [23]
- Subsequent stability studies and pharmacokinetic evaluations reinforced L5 as an effective aromatase inhibitor [23]
- Retrosynthetic analysis proposed feasible synthesis routes for the prioritized candidate [23]
This case highlights how 3D-QSAR serves as the foundational element in a comprehensive computer-aided drug design pipeline, efficiently funneling candidates from virtual screening to experimental validation.
Robust 3D-QSAR modeling, strategically integrated with ADMET prediction, represents a transformative approach in cancer drug discovery. By following the detailed protocols outlined in this application note, researchers can develop predictive models that not only elucidate critical structure-activity relationships but also simultaneously address the pharmacokinetic and safety considerations that ultimately determine clinical success. The continued evolution of these computational methods—particularly through machine learning enhancement and federated learning approaches—promises to further accelerate the identification of viable anticancer candidates with optimal efficacy and safety profiles.
Breast cancer remains a leading cause of cancer-related deaths among women globally, with over 2.3 million new cases diagnosed annually [8]. The development of more effective therapeutic agents with minimal side effects represents a critical challenge in oncology drug discovery. Tubulin, a pivotal protein in cancer cell division, has emerged as a promising molecular target for anticancer therapy [8] [41]. Specifically, inhibitors targeting the colchicine binding site (CBS) of tubulin disrupt microtubule dynamics, thereby inhibiting mitosis and cell proliferation [41].
The 1,2,4-triazine-3(2H)-one scaffold has recently gained significant attention as a privileged structure for designing novel tubulin inhibitors [8] [41]. These derivatives serve as cisoid restricted combretastatin A4 analogues, where the 1,2,4-triazin-3(2H)-one ring replaces the olefinic bond while maintaining essential pharmacophoric features of colchicine binding site inhibitors [41]. This case study explores the integration of 3D-QSAR modeling and ADMET profiling within a comprehensive computational framework to design and optimize 1,2,4-triazine-3(2H)-one derivatives as potent tubulin inhibitors for breast cancer therapy, contextualized within a broader thesis on ADMET property prediction in 3D-QSAR cancer drug design research.
Computational Workflow and Methodologies
Integrated Computational Workflow
The drug discovery process for triazine-based tubulin inhibitors employs a multi-stage computational approach that systematically integrates molecular modeling, predictive analytics, and simulation techniques. The workflow progresses from initial compound design through to the identification of optimized lead candidates, with ADMET considerations embedded throughout the process.
Dataset Curation and Chemical Space Analysis
The foundation of robust QSAR modeling relies on comprehensive dataset curation. Studies have utilized datasets of 32-35 novel 1,2,4-triazin-3(2H)-one derivatives with experimentally determined inhibitory efficacy against breast cancer cell lines (typically MCF-7) [8] [41]. The biological activity values (IC50) are converted to pIC50 (-log IC50) to ensure normal distribution for modeling purposes. The dataset is typically divided using an 80:20 ratio, where 80% of compounds form the training set for model development and 20% constitute the test set for external validation [8]. This division strategy balances comprehensive model training with adequate external validation capability.
Molecular Descriptor Calculation and Selection
Molecular descriptors quantitatively characterize structural features influencing biological activity. Calculations encompass two primary descriptor categories:
Electronic Descriptors: Computed using quantum mechanical methods (Gaussian 09W) with Density Functional Theory (DFT) at B3LYP/6-31G(d,p) level [8]. Key descriptors include:
- Highest Occupied Molecular Orbital Energy (EHOMO)
- Lowest Unoccupied Molecular Orbital Energy (ELUMO)
- Dipole Moment (μm)
- Absolute Electronegativity (χ)
- Absolute Hardness (η)
Topological Descriptors: Calculated using ChemOffice software [8]:
- Molecular Weight (MW)
- Octanol-Water Partition Coefficient (LogP)
- Water Solubility (LogS)
- Polar Surface Area (PSA)
- Hydrogen Bond Donors/Acceptors (HBD/HBA)
- Number of Rotatable Bonds (NROT)
Descriptor selection employs statistical analysis (Variance Inflation Factor) combined with biological reasoning to eliminate multicollinearity and retain chemically meaningful parameters [8].
3D-QSAR Model Development
Three-dimensional QSAR approaches, particularly Comparative Molecular Similarity Indices Analysis (CoMSIA), establish correlations between molecular fields and biological activity. The methodology includes:
Molecular Alignment: Structures are sketched (SYBYL 2.0), energy-minimized (Tripos force field), and aligned using the distill alignment technique with the most active compound as template [42].
Field Calculation: CoMSIA computes steric, electrostatic, hydrophobic, and hydrogen-bond donor/acceptor descriptors using a charged sp³ carbon probe atom on a 3D grid (2Å spacing) [42] [43].
Model Construction: Partial Least Squares (PLS) regression correlates CoMSIA descriptors with pIC50 values. Leave-One-Out (LOO) cross-validation determines the optimal number of components (N) and cross-validated correlation coefficient (Q²) [42] [43].
ADMET Profiling Protocol
ADMET properties are predicted using computational tools (e.g., SwissADME) to evaluate drug-likeness and pharmacokinetic profiles [44]. Key parameters include:
- Absorption: Caco-2 permeability, HIA (Human Intestinal Absorption)
- Distribution: Plasma Protein Binding, Blood-Brain Barrier Penetration
- Metabolism: CYP450 Enzyme Inhibition
- Excretion: Total Clearance
- Toxicity: hERG Inhibition, Ames Mutagenicity, Hepatotoxicity
Molecular Docking and Dynamics Simulations
Molecular Docking: Performed using AutoDock Vina or similar tools to predict binding modes and affinities at the tubulin colchicine binding site [8] [44]. The protocol includes protein preparation (removal of co-crystallized ligands, addition of hydrogens), ligand preparation (energy minimization), grid box definition, and docking simulation.
Molecular Dynamics Simulations: Conducted using GROMACS or AMBER for 100ns to evaluate complex stability [8] [44]. Analysis includes:
- Root Mean Square Deviation (RMSD)
- Root Mean Square Fluctuation (RMSF)
- Radius of Gyration (Rg)
- Solvent Accessible Surface Area (SASA)
- Hydrogen bond analysis
Results and Discussion
3D-QSAR Model Performance and Validation
The developed 3D-QSAR models demonstrated excellent predictive capability for tubulin inhibitory activity. Statistical validation metrics confirm model robustness and reliability for prospective compound design.
Table 1: Validation Metrics for 3D-QSAR Models of Triazine Derivatives
| Validation Parameter | Reported Value | Statistical Interpretation |
|---|---|---|
| R² (Determination Coefficient) | 0.849-0.967 [8] [42] | High explained variance in biological activity |
| Q² (LOO Cross-Validation) | 0.717-0.814 [42] [43] | Excellent internal predictive capability |
| R²Pred (External Validation) | 0.722-0.832 [42] [43] | Strong predictive power for new compounds |
| Standard Error of Estimation | Not specified | Measure of model precision |
| Optimal Components (N) | Dataset-dependent [42] | Prevents model overfitting |
The high R² values (0.849-0.967) indicate that the models explain approximately 85-97% of the variance in tubulin inhibitory activity [8] [42]. The Q² values exceeding 0.7 demonstrate robust internal predictive capability, while R²Pred values above 0.72 confirm excellent external predictability for novel compounds [42] [43].
Key Molecular Descriptors and Structural Insights
Contour map analysis from CoMSIA models reveals critical structural requirements for tubulin inhibition:
Steric Fields: Bulky substituents at the C5 position of triazine ring enhance activity, particularly 3,4,5-trimethoxyphenyl groups that occupy a deep hydrophobic pocket in the tubulin binding site [41].
Electrostatic Fields: Positive regions near methoxy groups indicate favorable interactions with electron-rich protein residues, while negative regions near the triazine carbonyl group suggest favorable interactions with hydrogen bond donors in the binding site [41].
Hydrophobic Fields: Hydrophobic substituents on both phenyl rings (particularly 3,4,5-trimethoxy pattern) significantly enhance activity through interactions with non-polar residues (Leu242, Leu255, Val318) in the colchicine binding site [41].
Hydrogen-Bonding Fields: The triazine-3(2H)-one carbonyl serves as critical hydrogen bond acceptor, while the NH group can function as hydrogen bond donor, mimicking interactions of native colchicine with tubulin [41].
ADMET Profiling of Triazine Derivatives
Comprehensive ADMET prediction provides crucial insights into the drug-likeness and pharmacokinetic properties of triazine-based tubulin inhibitors.
Table 2: ADMET Property Predictions for Optimized Triazine Derivatives
| ADMET Parameter | Predicted Profile | Therapeutic Implications |
|---|---|---|
| Lipophilicity (LogP) | ~3.0-4.0 [8] | Optimal membrane permeability |
| Water Solubility (LogS) | Moderate [8] | Balanced oral bioavailability |
| Hydrogen Bond Donors | 1-2 [8] | Favorable membrane transport |
| Hydrogen Bond Acceptors | 5-7 [8] | Within drug-like chemical space |
| Polar Surface Area | <140Ų [8] | Good intestinal absorption |
| CYP450 Inhibition | Low-moderate [44] | Reduced drug-drug interaction risk |
| hERG Inhibition | Low [44] | Favorable cardiac safety profile |
| Ames Test | Negative [44] | Low mutagenic potential |
The ADMET profile indicates that optimized triazine derivatives generally exhibit favorable drug-like properties with good predicted oral bioavailability and minimal toxicity concerns [8] [44]. Specific compounds such as Pred28 demonstrate particularly promising profiles with optimal lipophilicity (LogP), moderate water solubility, and low predicted toxicity risks [8].
Molecular Docking and Binding Mode Analysis
Docking studies reveal that high-activity triazine derivatives bind extensively at the tubulin colchicine binding site, with computed binding affinities ranging from -7.2 to -9.8 kcal/mol [8] [42]. Compound Pred28 demonstrates exceptional binding affinity (-9.6 kcal/mol) through:
- Hydrogen bonding with Asn101α, Asn349β, and Thr314β residues
- Hydrophobic interactions with Val181α, Ala180α, Leu242β, and Leu255β
- π-π stacking with Tyr202β
- Critical interactions with the triazine core and methoxy substituents [8]
The binding orientation maintains the essential pharmacophoric features of colchicine site inhibitors, with the trimethoxyphenyl ring occupying the same region as the colchicine A-ring and the triazine-3(2H)-one scaffold mimicking the colchicine C-ring orientation [41].
Molecular Dynamics and Binding Stability
Molecular dynamics simulations (100ns) provide insights into the stability and conformational dynamics of tubulin-triazine complexes. Key stability metrics include:
- RMSD (Root Mean Square Deviation): Stable complexes show RMSD < 0.3nm, indicating minimal structural drift [8]
- RMSF (Root Mean Square Fluctuation): Low fluctuation (<0.4nm) at binding site residues confirms stable ligand interaction [8]
- Radius of Gyration (Rg): Consistent Rg values indicate maintained protein structural compactness [44]
- Hydrogen Bond Persistence: Stable complexes maintain >70% hydrogen bond occupancy throughout simulations [8] [44]
Compound Pred28 demonstrates exceptional complex stability with the lowest RMSD (0.29nm) and stable RMSF profiles, indicating a tightly bound conformation to tubulin throughout the simulation period [8]. MM/GBSA calculations further confirm strong binding affinity (-34.33 kcal/mol for comparable systems) [44].
Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for 3D-QSAR and ADMET Studies
| Reagent/Tool | Specific Examples | Application in Workflow |
|---|---|---|
| Computational Chemistry Software | Gaussian 09W, ChemOffice [8] | Molecular descriptor calculation and geometry optimization |
| 3D-QSAR Modeling Platforms | SYBYL 2.0, QSARINS [42] [44] | CoMSIA model development and statistical analysis |
| Molecular Docking Tools | AutoDock Vina, AutoDockTools 1.5.7 [8] [44] | Protein-ligand interaction studies and binding affinity prediction |
| ADMET Prediction Platforms | SwissADME [44] | Pharmacokinetic and toxicity profiling |
| Molecular Dynamics Packages | GROMACS, AMBER [8] [44] | Complex stability simulations and conformational analysis |
| Chemical Databases | ZINC Natural Compound Database [17] | Source of chemical structures for virtual screening |
| Protein Data Bank | RCSB PDB (ID: 1JFF) [17] | Source of tubulin crystal structures for homology modeling |
This case study demonstrates the successful application of an integrated computational approach combining 3D-QSAR modeling and ADMET profiling for the rational design of triazine-based tubulin inhibitors. The developed CoMSIA models exhibit excellent predictive capability (R² = 0.849-0.967, Q² = 0.717-0.814) and identify critical structural requirements for tubulin inhibition, particularly the importance of absolute electronegativity and water solubility descriptors [8] [42].
The optimized 1,2,4-triazine-3(2H)-one derivatives display favorable ADMET profiles with optimal lipophilicity, moderate water solubility, and low toxicity risks [8] [44]. Molecular docking reveals strong binding affinities (-9.6 kcal/mol for Pred28) at the tubulin colchicine site, while molecular dynamics simulations confirm complex stability over 100ns [8].
This comprehensive computational framework significantly accelerates the drug discovery process by enabling the identification of promising triazine derivatives with optimized target affinity and drug-like properties prior to resource-intensive synthetic and biological evaluation. The methodologies outlined provide a validated protocol for integrating ADMET considerations early in the 3D-QSAR-driven design of anticancer agents, effectively bridging the gap between computational prediction and experimental realization in cancer drug discovery.
Topoisomerase IIα (Topo IIα) is a critical nuclear enzyme essential for DNA replication and cell proliferation, making it a prominent target in anticancer drug discovery. Inhibition of Topo IIα leads to DNA double-strand breaks, triggering apoptosis and cell death. The 1,4-naphthoquinone (1,4-NQ) pharmacophore has emerged as a promising scaffold for designing novel Topo IIα inhibitors, owing to its unique redox properties and multifaceted cytotoxic actions. This case study details the application of integrated computational and experimental protocols to design and evaluate novel 1,4-naphthoquinone derivatives, with a specific focus on predicting their Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties within a 3D-QSAR-driven cancer drug design framework [45] [46].
Biological Rationale and Signaling Pathways
Naphthoquinones exert cytotoxic effects through multiple mechanisms. Their primary action involves the inhibition of DNA topoisomerase enzymes, which are crucial for DNA replication and cell division [45]. Furthermore, their pro-oxidant nature allows them to generate reactive oxygen species (ROS), disrupting the cellular redox balance and inducing oxidative stress. This oxidative stress can activate several signaling pathways that lead to programmed cell death, or apoptosis [47]. The diagram below illustrates the key signaling pathways implicated in the anticancer activity of 1,4-naphthoquinone derivatives.
Quantitative Anticancer Activity Data
The in vitro cytotoxic activity of naphthoquinone derivatives is typically evaluated against a panel of human cancer cell lines. The activity is quantified as the half-maximal inhibitory concentration (IC50), with lower values indicating higher potency. The following table summarizes the promising anticancer activities of selected naphthoquinone derivatives from recent studies.
Table 1: Anticancer Activity of Selected Naphthoquinone Derivatives
| Compound ID | Chemical Class / Hybrid | Cancer Cell Line (Assay) | IC50 Value | Reference Compound (IC50) | Citation |
|---|---|---|---|---|---|
| Compound 11 | 1,4-Naphthoquinone derivative | HepG2 (MTT) | 0.15 µM | Not Specified | [45] |
| HuCCA-1 (MTT) | 0.31 µM | Not Specified | |||
| A549 (MTT) | 0.27 µM | Not Specified | |||
| MOLT-3 (XTT) | 1.55 µM | Not Specified | |||
| 4f | 1,4-NQ appended sulfenylated thiazole | A549 | "Potent" | Not Specified | [47] |
| MCF7 | "Potent" | Not Specified | |||
| MDAMB468 | "Potent" | Not Specified | |||
| Derivative 10 | 1,4-NQ-Thymol hybrid | MCF-7 | 4.59 µg/mL | Not Specified | [48] |
| Derivative 16 | 1,4-NQ-Isoniazid hybrid | A549 | 35.0 µg/mL | Not Specified | [48] |
| MDA-MB-231 | 3.0 µg/mL | Not Specified | |||
| SK-BR-3 | 0.3 µg/mL | Not Specified | |||
| -* | Naphtho[2,3-b]thiophene-4,9-dione | HT-29 (MTT) | 1.73 - 18.11 µM | Doxorubicin | [46] |
*The most active compound in the series was 8-hydroxy-2-(thiophen-2-ylcarbonyl)naphtho[2,3-b]thiophene-4,9-dione.
Experimental Protocols
Protocol 1:In VitroCytotoxicity Assay (MTT/XTT)
This protocol is used to determine the anti-proliferative activity of test compounds against adherent and suspension cancer cell lines [45].
Key Materials:
- Cell Lines: Human cancer cell lines (e.g., HepG2, A549, MOLT-3, HT-29).
- Culture Media: RPMI-1640 or DMEM, supplemented with 10% Fetal Bovine Serum (FBS), 2 mM L-glutamine, and 100 U/mL penicillin-streptomycin.
- Test Compounds: 1,4-NQ derivatives dissolved in DMSO (final DMSO concentration < 0.5%).
- Viability Reagent: MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) for adherent cells or XTT (2,3-bis-(2-methoxy-4-nitro-5-sulfophenyl)-2H-tetrazolium-5-carboxanilide) for suspension cells.
- Equipment: CO₂ incubator, 96-well microtiter plates, microplate reader.
Step-by-Step Procedure:
- Cell Seeding: Seed cells in 96-well plates at a density of 5 × 10³ to 2 × 10⁴ cells per well in complete medium. Incubate for 24 hours at 37°C under 5% CO₂ to allow cell attachment.
- Compound Treatment: Prepare serial dilutions of the test compounds and positive controls (e.g., doxorubicin, etoposide) in culture medium. Add these to the wells, replacing an equivalent volume of medium. The negative control wells receive medium with DMSO only.
- Incubation: Incubate the plates for a predetermined period (typically 48 hours) under the same conditions.
- Viability Assessment:
- For MTT (adherent cells): Add a specific volume of MTT solution to each well. Incubate for 2-4 hours to allow formazan crystal formation. Carefully remove the medium and dissolve the formed formazan crystals in DMSO.
- For XTT (suspension cells): Add the XTT reagent directly to the wells and incubate for a similar duration. The formed formazan dye is soluble in culture medium.
- Absorbance Measurement: Measure the absorbance of the solution in each well using a microplate reader at a wavelength of 550 nm.
- Data Analysis: Calculate the percentage of cell viability relative to the negative control (DMSO). The IC50 value is determined from the dose-response curve using appropriate statistical software (e.g., GraphPad Prism).
Protocol 2: 3D-QSAR Model Construction and Application
This protocol outlines the creation of a 3D-QSAR model to correlate the 3D molecular fields of compounds with their biological activity, guiding rational drug design [45] [46].
Key Materials:
- Software: Molecular modeling software suites (e.g., SYBYL for CoMFA).
- Dataset: Experimentally determined IC50 values for a training set of naphthoquinone derivatives.
- Computational Resources: Workstation with sufficient processing power.
Step-by-Step Procedure:
- Dataset Preparation: Compile a set of structurally diverse naphthoquinone derivatives with their experimentally determined IC50 values. Convert IC50 to pIC50 (-logIC50) for analysis.
- Molecular Modeling and Alignment:
- Sketch or import the 3D structures of all compounds.
- Perform geometry optimization using computational methods (e.g., Density Functional Theory (DFT) with basis sets like B3LYP/6-31G*).
- Align the optimized molecules based on a common scaffold or pharmacophore using the software's alignment tools.
- Descriptor Generation: Calculate interaction fields (steric and electrostatic) around each molecule using a probe atom. For Comparative Molecular Field Analysis (CoMFA), a standard probe is used.
- Model Construction: Use the partial least squares (PLS) regression algorithm to build a correlation model between the molecular field descriptors (independent variables) and the pIC50 values (dependent variable).
- Model Validation:
- Internal Validation: Assess the model using cross-validation (e.g., leave-one-out) to determine the cross-validated correlation coefficient (q²). A q² > 0.5 is generally considered acceptable.
- External Validation: Use a test set of compounds not included in the model building to calculate the predictive correlation coefficient (r²pred).
- Model Application: Interpret the 3D contour maps to identify regions where steric bulk or specific electrostatic charges enhance or diminish activity. Use these insights to propose new, potentially more potent derivatives.
Protocol 3:In SilicoADMET and Molecular Docking
This protocol involves the computational prediction of pharmacokinetic and toxicity profiles, and the assessment of binding modes with the target protein [45] [49] [48].
Key Materials:
- Software: ADMET prediction tools (e.g., SwissADME, pkCSM), molecular docking software (e.g., AutoDock Vina, GOLD, GLIDE).
- Protein Structure: Crystal structure of the target protein (e.g., Topoisomerase IIα, PDB ID: often requires selection from database) from the Protein Data Bank (PDB).
- Ligand Structures: 2D or 3D structures of the naphthoquinone derivatives.
Step-by-Step Procedure:
- ADMET Prediction:
- Prepare the molecular structures of the compounds in a suitable format (e.g., SDF, MOL2).
- Input these structures into web-based ADMET prediction platforms.
- Analyze the results for key parameters such as gastrointestinal absorption, blood-brain barrier penetration, CYP enzyme inhibition, and hepatotoxicity.
- Molecular Docking:
- Protein Preparation: Download the 3D structure of the target protein from the PDB. Remove water molecules and co-crystallized ligands. Add hydrogen atoms and assign partial charges.
- Ligand Preparation: Sketch or import the ligand structures. Optimize their geometry and assign correct rotatable bonds and charges.
- Grid Generation: Define the docking search space (grid box) around the active site of the protein.
- Docking Execution: Run the docking simulation to generate multiple binding poses for each ligand.
- Pose Analysis: Analyze the top-scoring poses for key interactions (hydrogen bonds, hydrophobic interactions, π-π stacking) with amino acid residues in the binding pocket. Visually inspect the results using molecular visualization software (e.g., PyMOL).
- ADMET Prediction:
The following workflow integrates these computational protocols into a cohesive drug design cycle.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials
| Reagent / Material | Function / Application | Specific Example / Note |
|---|---|---|
| Human Cancer Cell Lines | In vitro models for evaluating compound cytotoxicity. | HepG2 (liver), A549 (lung), MOLT-3 (leukemia), HT-29 (colon), MCF-7 (breast) [45] [46] [48]. |
| MTT/XTT Reagents | Cell viability assays; measure mitochondrial activity of living cells. | MTT for adherent cells, XTT for suspension cells [45]. |
| Doxorubicin / Etoposide | Reference standard (positive control) for cytotoxicity assays. | Validates the experimental setup and provides a benchmark for activity [45] [46]. |
| Molecular Modeling Software | Platform for 3D-QSAR, molecular docking, and structure optimization. | SYBYL (for CoMFA), AutoDock Vina, GOLD, Schrödinger Suite [45] [49] [50]. |
| ADMET Prediction Tools | In silico assessment of pharmacokinetics and toxicity profiles. | SwissADME, pkCSM, PreADMET; used for early-stage prioritization [45] [48]. |
| Protein Data Bank (PDB) | Repository for 3D structural data of biological macromolecules. | Source of target protein structures (e.g., Topo IIα, COX-2) for docking studies [49] [50]. |
Machine Learning Models for High-Throughput ADMET Screening
The evaluation of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties represents a critical bottleneck in modern drug discovery and development, contributing significantly to the high attrition rate of drug candidates [51]. Traditional experimental approaches, while reliable, are often time-consuming, cost-intensive, and limited in scalability [51]. Within the specific context of 3D-QSAR cancer drug design research, where the goal is to optimize compound structures for enhanced biological activity against cancer targets, the early and rapid assessment of ADMET properties is paramount [6] [52]. The integration of Machine Learning (ML) models for high-throughput ADMET screening has emerged as a transformative solution, enabling the rapid, cost-effective, and reproducible prioritization of lead compounds [51] [53]. These in silico methodologies seamlessly integrate with existing discovery pipelines, allowing for early risk assessment and a substantial reduction in late-stage failures due to unfavorable pharmacokinetic or safety profiles [54] [53]. This document outlines the current landscape, detailed protocols, and essential tools for implementing ML-driven ADMET screening, framed within the workflow of 3D-QSAR-guided anticancer drug development.
The Current Landscape of ML in ADMET Prediction
Machine learning has revolutionized ADMET prediction by deciphering complex, non-linear relationships between chemical structure and pharmacokinetic or toxicological endpoints that are often difficult to capture with traditional quantitative structure-activity relationship (QSAR) models [53]. The paradigm has shifted from reliance solely on in vitro high-throughput screening (HT-ADME) to a complementary, and often preliminary, in silico approach [54]. This is particularly valuable in cancer drug design, where researchers can use ML models to filter virtual libraries of compounds designed via 3D-QSAR before committing resources to synthesis and biological testing [6] [8].
ML-based approaches leverage large-scale, high-quality ADMET datasets, often generated by the "industrialization" of HT-ADME screening in biopharma companies, to build predictive models with unprecedented accuracy [54] [53]. These models have been successfully deployed to predict key ADMET endpoints, including:
- Absorption parameters such as permeability (e.g., Caco-2 models), solubility, and interactions with efflux transporters like P-glycoprotein (P-gp) [53].
- Metabolism endpoints, including interactions with cytochrome P450 enzymes, metabolic stability, and soft-spot identification [51] [53].
- Toxicity profiles, encompassing genotoxicity, carcinogenicity, and organ-specific toxicity [55] [56].
The integration of these predictive models within the 3D-QSAR workflow provides a holistic view of a compound's potential, balancing potency against pharmacokinetic and safety considerations from the earliest stages of drug design [52] [8].
Key Machine Learning Methodologies and Algorithms
A diverse array of machine learning algorithms is employed in computational toxicology and ADMET prediction. The selection of an appropriate algorithm depends on the nature of the data, the specific endpoint being predicted, and the desired balance between accuracy and interpretability [51] [55].
Table 1: Key Machine Learning Algorithms in ADMET Prediction
| Algorithm Category | Specific Examples | Key Characteristics | Common ADMET Applications |
|---|---|---|---|
| Supervised Learning | Support Vector Machines (SVM), Random Forest (RF), Decision Trees [51] [55] | Trained on labelled data to predict continuous (regression) or categorical (classification) outcomes [51]. | Metabolic stability, toxicity classification, solubility prediction [55] [53]. |
| Deep Learning (DL) | Graph Neural Networks (GNNs), Multitask Learning (MTL) models [53] | Model complex, non-linear relationships; GNNs use molecular graphs as input, capturing structural information natively [51] [53]. | High-accuracy prediction across multiple ADMET endpoints simultaneously [53]. |
| Ensemble Methods | Random Forest, Ensemble Learning [55] [53] | Combine multiple models to improve predictive performance and robustness [53]. | Property prediction from heterogeneous data sources [57]. |
| Unsupervised Learning | Kohonen's Self-Organizing Maps (SOM) [55] | Identify patterns, structures, or clusters in data without pre-defined labels; useful for data exploration and visualization [51] [55]. | Compound clustering, data exploration in toxicological datasets [55] [57]. |
Among these, Graph Neural Networks (GNNs) represent a significant advancement. Unlike traditional methods that rely on "handcrafted" molecular descriptors, GNNs learn task-specific features directly from the molecular graph, where atoms are nodes and bonds are edges, achieving unprecedented accuracy in ADMET property prediction [51] [53]. Furthermore, multitask learning frameworks, which train a single model on multiple related endpoints, have demonstrated enhanced predictive performance and data efficiency by leveraging shared information across tasks [53].
The development of a robust ML model for ADMET prediction is fundamentally dependent on the quality, quantity, and relevance of the underlying data.
Public and proprietary databases provide the pharmacokinetic and physicochemical property data necessary for model training [51]. The quality of this data is paramount, as it directly impacts model performance [51]. Data preprocessing, including cleaning, normalization, and careful splitting into training, validation, and test sets, is an essential first step to ensure data consistency and avoid model bias [51] [8].
Molecular Descriptors and Feature Engineering
Molecular descriptors are numerical representations that encode the structural and physicochemical attributes of a compound [51]. Feature engineering, the process of selecting and creating the most informative descriptors, is crucial for model accuracy.
- Types of Descriptors: These range from simple 1D/2D descriptors (e.g., molecular weight, logP) to complex 3D quantum chemical descriptors (e.g., HOMO/LUMO energies, absolute electronegativity, dipole moment) calculated using methods like Density Functional Theory (DFT) with a B3LYP functional, as commonly used in 3D-QSAR studies [52] [8].
- Feature Selection Methods:
- Filter Methods: Efficiently remove duplicated and correlated features during pre-processing [51].
- Wrapper Methods: Iteratively train the model with different feature subsets to find the optimal set, though computationally expensive [51].
- Embedded Methods: Integrate feature selection into the model training process (e.g., as part of a Random Forest) and often provide a good balance of speed and accuracy [51].
Experimental Protocols and Workflows
This section provides a detailed methodology for developing and validating an ML model for ADMET screening within a cancer drug discovery program.
Protocol: Developing a Supervised ML Model for Toxicity Prediction
Objective: To build a classifier for predicting a specific toxicity endpoint (e.g., genotoxicity) using a dataset of chemical structures and their associated toxicological outcomes.
Materials:
- Dataset: Curated dataset of compounds with known toxicological activity (e.g., from public sources or in-house screening).
- Software: Cheminformatics software (e.g., ChemOffice, OpenBabel) for descriptor calculation; ML libraries (e.g., scikit-learn, Deep Graph Library); and statistical analysis software (e.g., XLSTAT, R) [8].
Procedure:
- Data Collection and Curation: Assemble a dataset of compounds with reliable experimental toxicity labels. Ensure a balanced representation of active and inactive compounds to avoid model bias.
- Descriptor Calculation: For each compound in the dataset, compute a comprehensive set of molecular descriptors. This can include:
- Topological Descriptors: Calculate using software like ChemOffice [8]. These include molecular weight, logP, polar surface area, Balaban index, and Wiener index.
- Quantum Chemical Descriptors: For a subset of compounds, perform geometry optimization using DFT (e.g., with Gaussian 09W) at the B3LYP/6-31G* level. Extract electronic descriptors such as EHOMO, ELUMO, absolute hardness (η), and absolute electronegativity (χ) [8].
- Data Preprocessing and Splitting:
- Handle missing values and normalize the descriptor data.
- Split the dataset randomly into a training set (e.g., 80%) for model development and a test set (e.g., 20%) for external validation [8].
- Feature Selection: Apply a feature selection method (e.g., embedded method via Random Forest) to the training set to identify the most predictive descriptors and reduce dimensionality.
- Model Training and Validation:
- Train multiple ML algorithms (e.g., Random Forest, SVM, Neural Networks) on the training set using the selected features.
- Perform k-fold cross-validation (e.g., 5-fold) on the training set to tune model hyperparameters and prevent overfitting [51].
- Select the best-performing model based on cross-validation metrics.
- Model Evaluation:
- Use the held-out test set to evaluate the final model's predictive performance.
- Report standard metrics such as accuracy, sensitivity, specificity, area under the ROC curve (AUC-ROC), and concordance for classification tasks.
Protocol: Integrating ADMET Prediction with 3D-QSAR in Cancer Drug Design
Objective: To prioritize newly designed compounds from a 3D-QSAR study for synthesis and testing based on predicted ADMET properties.
Materials:
- A robust 3D-QSAR model (e.g., CoMFA or CoMSIA) with established predictive ability for anticancer activity [6] [52].
- A pre-trained and validated ML model for a key ADMET property (e.g., metabolic stability, hERG inhibition).
Procedure:
- Design Novel Compounds: Use the contour maps from the 3D-QSAR model (e.g., CoMSIA_SHE model highlighting steric, electrostatic, and hydrophobic fields) to design a virtual library of novel, potentially more active compounds [6] [52].
- Predict Biological Activity: Input the designed structures into the 3D-QSAR model to predict their pIC50 values for the target (e.g., EGFR or Tubulin inhibition) [52] [8].
- Predict ADMET Properties:
- For each designed compound, compute the necessary molecular descriptors.
- Input the descriptors into the pre-trained ML ADMET model(s) to obtain predictions (e.g., "high" or "low" metabolic stability).
- Multi-Parameter Optimization: Rank the designed compounds based on a combination of high predicted activity (from 3D-QSAR) and favorable ADMET profiles (from ML models).
- Experimental Validation: Synthesize and test the top-prioritized compounds in vitro to validate both the activity and ADMET predictions, thereby closing the design-make-test-analyze cycle.
Essential Research Reagent Solutions
The following table details key software and data resources essential for conducting ML-driven ADMET research.
Table 2: Key Research Reagent Solutions for ML-based ADMET Screening
| Tool/Resource Name | Type | Primary Function | Relevance to ML-ADMET |
|---|---|---|---|
| Gaussian 09W [8] | Software | Quantum chemical calculations | Computes electronic structure descriptors (HOMO, LUMO, electronegativity) for QSAR/ML models. |
| ChemOffice [8] | Software Suite | Cheminformatics and molecular modeling | Calculates topological descriptors (LogP, PSA, Wiener Index) for ML feature set generation. |
| SYBYL-X [52] | Software Suite | Molecular modeling and QSAR | Used for building 3D-QSAR models (CoMFA, CoMSIA) and aligning molecular structures. |
| DiscoveryQuant/LeadScape [54] | Software Platform | LC-MS/MS data analysis for HT-ADME | Automates bioanalysis data processing, generating high-quality datasets for ML model training. |
| OECD-COMTOX [56] | Software Framework | Computational toxicology | Provides pre-trained ML models for various toxicity endpoints (genotoxicity, carcinogenicity). |
| SwissADME / pkCSM [52] | Web Server | In silico ADMET prediction | Useful for rapid property profiling and as a benchmark for custom-built ML models. |
| Integrated Automation Systems (e.g., HighRes Biosolutions) [54] | Hardware/Software | Assay automation | Enables "industrialized" HT-ADME screening to generate large, consistent training datasets. |
Workflow Visualization and Decision Pathways
The following diagrams illustrate the integrated workflow of 3D-QSAR and ML models in anti-cancer drug design and the core process for building an ML model for ADMET prediction.
Integrated Drug Design Workflow
Diagram Title: Integrated 3D-QSAR and ML-ADMET Workflow
ML Model Development Process
Diagram Title: ML Model Development Pipeline
The integration of machine learning models for high-throughput ADMET screening represents a cornerstone of modern, efficient drug discovery, particularly within the framework of 3D-QSAR cancer drug design. By leveraging advanced algorithms like graph neural networks and ensemble methods, researchers can now simultaneously optimize compounds for both potency and desirable pharmacokinetic profiles early in the discovery process. This integrated computational approach significantly de-risks the development pipeline, reduces reliance on costly and time-consuming experimental screens alone, and accelerates the journey toward safer and more effective cancer therapeutics. As data quality and availability continue to improve, and models become increasingly sophisticated and interpretable, the role of ML in ADMET prediction is poised to become even more central and transformative.
In modern computational oncology, the integration of independent computational techniques into a unified workflow is paramount for accelerating the discovery of effective chemotherapeutic agents. The standalone application of three-dimensional quantitative structure-activity relationship (3D-QSAR) modeling, while powerful for establishing correlations between molecular structure and biological activity, often lacks the mechanistic insight provided by structural biology techniques [28]. Similarly, molecular docking predicts binding orientations but typically treats the protein target as rigid, overlooking the dynamic nature of ligand-receptor interactions in a physiological environment [42]. Molecular dynamics (MD) simulations address this limitation by providing a temporal dimension, revealing the stability and evolution of these complexes. When these methodologies are systematically integrated within a 3D-QSAR workflow, they create a powerful, iterative feedback loop that guides the rational design of novel compounds with optimized potency and improved ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties, a critical consideration in cancer drug design [6] [23]. This protocol details the steps for such an integration, framed within the context of anti-cancer drug discovery.
The synergistic integration of 3D-QSAR, molecular docking, and molecular dynamics follows a logical sequence where the output of one method informs the input of the next. The workflow is designed to maximize the strengths of each technique while mitigating their individual limitations. The following diagram illustrates this cohesive pipeline, highlighting the key stages from initial compound preparation to final candidate selection.
Figure 1: Integrated computational workflow for cancer drug design, combining 3D-QSAR, docking, MD simulations, and ADMET prediction.
Protocol Details
Phase 1: 3D-QSAR Model Construction and Validation
The initial phase focuses on developing a robust and predictive 3D-QSAR model, which will serve as the primary guide for designing new chemical entities.
Dataset Curation and Molecular Modeling
- Compound Selection: Curate a dataset of 30-50 compounds with known biological activity (e.g., IC₅₀ or Ki) against a specific cancer target (e.g., Tubulin, EGFR, Aromatase) [8] [42]. Ensure the dataset encompasses a wide potency range and diverse chemical structures.
- Activity Conversion: Convert the inhibitory concentrations (IC₅₀) to pIC₅₀ values using the formula: pIC₅₀ = -log₁₀(IC₅₀). This creates a normally distributed dependent variable for modeling [8] [42].
- Structure Preparation and Optimization: Sketch 2D structures of all compounds using tools like ChemDraw. Perform geometry optimization using molecular mechanics (e.g., Tripos force field) or semi-empirical methods (e.g., PM3) to obtain low-energy 3D conformations. Atomic partial charges should be assigned using the Gasteiger-Hückel method [42] [26].
- Molecular Alignment: This is a critical step for a meaningful 3D-QSAR model. Align all molecules to a common template, often the most active compound, based on their common scaffold or pharmacophoric features using the distill alignment method in SYBYL or similar software [42].
Descriptor Calculation and Model Generation
- Field Calculation: Place the aligned molecules into a 3D grid. Calculate molecular interaction fields using a probe atom.
- Partial Least Squares (PLS) Regression: Use PLS analysis to correlate the molecular field descriptors with the biological activity (pIC₅₀). The dataset should be split into a training set (~80%) for model building and a test set (~20%) for external validation [8] [42].
Model Validation and Interpretation
- Statistical Validation: A validated model must meet key statistical thresholds [14] [26].
Table 1: Key Statistical Metrics for 3D-QSAR Model Validation
Metric Description Acceptance Threshold R² Non-cross-validated correlation coefficient > 0.8 Q² (LOO) Leave-One-Out cross-validated correlation coefficient > 0.5 SEE Standard Error of Estimate As low as possible F Value Fisher F-statistic (model significance) High value R²Pred Predictive R² from the test set > 0.6 - Contour Map Analysis: Interpret the resulting CoMFA or CoMSIA contour maps. For example, a green CoMSIA steric contour indicates a region where bulky substituents enhance activity, while a blue electrostatic contour shows where electropositive groups are favored [6] [14]. These maps provide visual guidance for structural modification.
Phase 2: Integration of Molecular Docking
This phase uses the designed compounds from Phase 1 to understand their putative binding mode with the target protein.
System Preparation and Docking Execution
- Protein Preparation: Obtain the 3D structure of the target (e.g., Tubulin, PDB ID: 1SA0) from the Protein Data Bank. Remove water molecules and co-crystallized ligands. Add hydrogen atoms and assign partial charges using a molecular mechanics force field (e.g., AMBER, CHARMM). Define the binding site, typically around the native ligand or a known active site [8] [42].
- Ligand Preparation: Generate 3D structures of the newly designed compounds and convert them into a suitable format with correct protonation states and tautomers.
- Docking Protocol: Perform molecular docking using software like AutoDock Vina or Glide. Validate the docking protocol by re-docking the native co-crystallized ligand and calculating the root-mean-square deviation (RMSD) of the best pose compared to the crystal structure. An RMSD < 2.0 Å is generally acceptable [59].
Pose Analysis and Selection
- Analyze the top-scoring docking poses for each compound. Prioritize poses that show key interactions with the protein's active site residues (e.g., hydrogen bonds, π-π stacking, salt bridges) that are consistent with known mutagenesis or structural data [14] [42]. These selected poses will be used as the starting structures for molecular dynamics simulations.
Phase 3: Molecular Dynamics and Energetics Analysis
MD simulations are used to validate the stability of the docked complexes and provide a more realistic estimate of binding affinity.
System Setup and Simulation Parameters
- Solvation and Ionization: Place the protein-ligand complex in a simulation box (e.g., a cubic or TIP3P water box) with a buffer distance of at least 10 Å. Add ions (e.g., Na⁺, Cl⁻) to neutralize the system's charge and mimic physiological salt concentration [6] [8].
- Energy Minimization and Equilibration:
- Minimization: Perform energy minimization (2,000-5,000 steps) to remove bad contacts.
- NVT Ensemble: Equilibrate the system with a constant Number of particles, Volume, and Temperature (NVT) for 100-500 ps, gradually heating to 310 K.
- NPT Ensemble: Further equilibrate with a constant Number of particles, Pressure, and Temperature (NPT) for 100-500 ps to achieve correct density [8].
- Production Run: Execute an unrestrained MD simulation for a sufficient duration (typically 100-200 nanoseconds) to ensure the system is stable and well-sampled. Use a 2-fs integration time step. Conduct simulations in triplicate with different initial velocities to ensure reproducibility [6] [23].
Trajectory Analysis and Binding Free Energy Calculation
- Stability Metrics: Analyze the simulation trajectory to calculate key metrics [8] [26]:
- Root Mean Square Deviation (RMSD): Measures the stability of the protein-ligand complex over time.
- Root Mean Square Fluctuation (RMSF): Identifies flexible regions of the protein.
- Radius of Gyration (Rg): Assesses the compactness of the protein.
- Hydrogen Bonds: Monitors the formation and stability of key interactions.
- Binding Free Energy Calculation: Employ the Molecular Mechanics/Poisson-Boltzmann Surface Area (MM-PBSA) or Generalized Born Surface Area (MM-GBSA) method. This method uses snapshots from the MD trajectory to calculate a more accurate binding free energy than docking scores alone. The binding free energy (ΔGbind) is decomposed as: ΔGbind = Egas + Gsolv - TΔS, where Egas is the gas-phase interaction energy, Gsolv is the solvation free energy, and -TΔS is the entropic contribution [6] [23]. Per-residue energy decomposition can identify hot-spot residues critical for binding.
Phase 4: ADMET Integration and Candidate Selection
The final phase involves evaluating the promising compounds for drug-like properties.
- In Silico ADMET Prediction: Use computational tools (e.g., SwissADME, pkCSM) to predict key pharmacokinetic and toxicity endpoints for the top candidates [14] [23].
Table 2: Key ADMET Properties for Candidate Prioritization in Cancer Drug Design
Property Prediction Method Desired Profile Water Solubility (LogS) AI-based predictors > -4 log mol/L Caco-2 Permeability Predictive model > -5.15 log cm/s Cytochrome P450 Inhibition Structural alerts Non-inhibitor of CYP3A4, 2D6 hERG Cardiotoxicity QSAR model Non-blocker Hepatotoxicity Structural alerts Non-toxic AMES Mutagenicity Structural alerts Non-mutagen - Final Candidate Selection: Integrate all data to select lead compounds. A promising candidate should exhibit [6] [23]:
- High predicted potency from the 3D-QSAR model.
- Favorable and stable binding mode from docking and MD.
- Strong calculated binding affinity (MM-PBSA/GBSA).
- A favorable in silico ADMET profile with minimal predicted toxicity.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for the Integrated Workflow
| Category / Item | Specific Examples | Function in the Protocol |
|---|---|---|
| Software for Modeling & Docking | SYBYL, Schrodinger Suite, AutoDock Vina, GOLD | Used for molecular modeling, 3D-QSAR (CoMFA/CoMSIA), and molecular docking studies [42] [26]. |
| MD Simulation Engines | GROMACS, AMBER, NAMD | Software packages used to run molecular dynamics simulations, analyzing complex stability and dynamics [6] [8]. |
| ADMET Prediction Platforms | SwissADME, pkCSM, admetSAR | Online tools and software for predicting absorption, distribution, metabolism, excretion, and toxicity properties in silico [14] [23]. |
| Target Protein Structures | RCSB Protein Data Bank (PDB) | Public repository for 3D structural data of proteins and nucleic acids, essential for docking and MD setup [8] [42]. |
| Descriptor Calculation Tools | DRAGON, PaDEL-Descriptor, RDKit | Software used to calculate thousands of molecular descriptors from chemical structures for QSAR analysis [28] [19]. |
Application Note: Anti-Breast Cancer Agent Design
A recent study exemplifies this integrated protocol. Researchers developed 3D-QSAR models (CoMFA/CoMSIA) for 1,2,4-triazine-3(2H)-one derivatives as Tubulin inhibitors. The models guided the design of new compounds, which were subsequently docked into the Tubulin colchicine-binding site. A 100 ns MD simulation confirmed the stability of the best-docked complex (Pred28), showing a low RMSD of 0.29 nm. MM-PBSA calculations provided a quantitative binding free energy, and in silico ADMET predictions indicated a high probability of drug-likeness, successfully identifying a promising candidate for experimental validation [8]. This case study demonstrates the power of an integrated computational approach in a cancer drug discovery project.
Navigating Challenges and Enhancing 3D-QSAR Model Performance
Common Pitfalls in 3D-QSAR Modeling and How to Avoid Them
Three-dimensional Quantitative Structure-Activity Relationship (3D-QSAR) modeling represents a powerful computational approach in modern drug design, particularly in oncology research for optimizing lead compounds and predicting their Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties. However, the effectiveness of these models is heavily dependent on rigorous methodological execution. This application note details common pitfalls encountered during 3D-QSAR model development, specifically within the context of cancer drug discovery, and provides validated protocols to overcome these challenges. By addressing critical issues in molecular alignment, dataset preparation, model validation, and ADMET integration, we present a structured framework to enhance the predictive reliability and practical utility of 3D-QSAR models in designing novel anticancer therapeutics with favorable pharmacokinetic and safety profiles.
3D-QSAR techniques, including Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA), have become indispensable tools in medicinal chemistry for rational drug design. These methods correlate the three-dimensional molecular properties of compounds with their biological activities, enabling the prediction of novel compounds' efficacy before synthesis [14]. In anticancer drug development, 3D-QSAR has been successfully applied to various targets, including histone deacetylase (HDAC), epidermal growth factor receptor (EGFR), human epidermal growth factor receptor 2 (HER2), and aromatase, facilitating the design of inhibitors with enhanced potency and selectivity [6] [60].
The integration of ADMET prediction into 3D-QSAR workflows has gained significant importance due to the high attrition rates of drug candidates caused by unfavorable pharmacokinetic and toxicity profiles. Early assessment of these properties helps prioritize compounds with a higher likelihood of clinical success, particularly crucial in oncology where therapeutic windows are often narrow [6] [61]. However, the development of robust and predictive 3D-QSAR models presents numerous challenges that, if not properly addressed, can compromise model accuracy and lead to misleading conclusions in compound optimization.
Critical Pitfalls and Recommended Solutions
Molecular Alignment and Conformation Errors
Pitfall Description: Incorrect alignment of molecules represents the most significant source of error in 3D-QSAR modeling. The predictive capability of a model depends entirely on the correct spatial orientation of molecules, as misalignment introduces noise that obscures true structure-activity relationships [62]. This challenge is particularly acute when the target protein structure is unknown, forcing researchers to rely on hypothesized bioactive conformations.
Consequences: Poor alignment leads to models with limited or no predictive power, incorrect interpretation of steric and electrostatic requirements, and ultimately, misguided synthetic efforts. A study on quinazoline derivatives as HER2 inhibitors demonstrated that alignment method selection dramatically impacted model quality, with cross-validated q² values varying significantly based on conformational generation approach [60].
Solution Protocol:
- Reference Molecule Selection: Identify a representative molecule with confirmed high activity and structural simplicity as an initial alignment template [62].
- Bioactive Conformation Determination: Whenever possible, derive bioactive conformations from experimental ligand-protein complexes. Alternatively, use molecular docking or field-based template methods (e.g., FieldTemplater) to generate reliable conformations [63] [62].
- Multi-Reference Alignment: Employ 3-4 reference molecules covering diverse structural features to fully constrain the alignment space. Use substructure alignment to ensure common cores are properly superimposed [62].
- Activity-Blind Alignment: Critically, complete all alignment optimization before running QSAR calculations. Never adjust alignments based on model performance metrics, as this introduces bias and invalidates the model [62].
Table 1: Molecular Alignment Techniques and Their Applications
| Technique | Methodology | Advantages | Limitations | Best Use Cases |
|---|---|---|---|---|
| Substructure Alignment | Aligns common molecular framework | Ensures core structural similarity | May misalign peripheral substituents | Congeneric series with conserved core |
| Field-Based Alignment | Aligns based on molecular field similarity | Accounts for electronic properties | Computationally intensive | Scaffold hopping, diverse structures |
| Docking-Based Alignment | Uses poses from molecular docking | Incorporates target structural data | Dependent on docking accuracy | When reliable protein structure exists |
| Pharmacophore Alignment | Aligns key pharmacophoric features | Focuses on essential interactions | May oversimplify molecular alignment | Initial screening, diverse datasets |
Dataset Preparation and Biological Data Quality
Pitfall Description: 3D-QSAR models are fundamentally limited by the quality of the input data. Common dataset issues include insufficient molecular diversity, limited quantity of compounds, and biological activity data generated through inconsistent assay protocols or with high experimental error [64] [65].
Consequences: Models built on inadequate datasets suffer from limited applicability domain, poor predictive capability for novel chemotypes, and inherent statistical instability. The principle of "garbage in, garbage out" applies directly to QSAR modeling, where even sophisticated algorithms cannot compensate for fundamentally flawed input data [64].
Solution Protocol:
- Data Curation: Collect biological activity data (e.g., IC₅₀, Ki) obtained through consistent, standardized experimental protocols. Convert activity values to pIC₅₀ or pKi to ensure linear relationships [14] [60].
- Dataset Size and Diversity: Include a sufficient number of compounds (typically >20-25) spanning a wide activity range (≥4 orders of magnitude). Ensure structural diversity to avoid oversampling specific regions of chemical space [64] [66].
- Training/Test Set Division: Implement activity-stratified division to ensure both sets represent similar activity ranges and structural diversity. Common splits include 80/20 or 70/30 for training/test sets respectively [63] [67].
- Applicability Domain Definition: Explicitly define the model's applicability domain based on molecular descriptors to identify compounds for which predictions are reliable [14] [65].
Model Validation Deficiencies
Pitfall Description: Insufficient model validation represents a critical pitfall that can lead to overoptimistic assessment of model performance. Reliance on a single validation metric, particularly internal validation alone, fails to adequately assess true predictive capability [64] [65].
Consequences: Models with high internal validation metrics (e.g., q²) may perform poorly when predicting truly external compounds, leading to false confidence in virtual screening outcomes. This deficiency explains why some published models with excellent apparent statistics fail in practical application [65] [62].
Solution Protocol:
- Internal Validation: Perform leave-one-out (LOO) or leave-several-out (LSO) cross-validation to calculate q². Accept models with q² > 0.5, with q² > 0.6-0.7 considered good or excellent [14] [63] [67].
- External Validation: Reserve a sufficient portion of compounds (typically 20-30%) as an external test set never used in model development. Calculate predictive R² (R²pred) for these compounds, with R²pred > 0.6 considered acceptable [14] [6].
- Statistical Significance Testing: Perform Y-randomization (scrambling activity values) to ensure models cannot be obtained by chance. A minimum of 50 randomizations is recommended to establish model robustness [67].
- Multiple Validation Metrics: Report a comprehensive set of statistics including conventional R², q², standard error of estimate, F-value, and R²pred to provide a complete performance picture [60].
Table 2: Essential Validation Metrics for 3D-QSAR Models
| Validation Type | Metric | Calculation | Acceptance Criterion | Interpretation |
|---|---|---|---|---|
| Internal Validation | q² (LOO) | PRESS/SSY | > 0.5 | Good internal predictive ability |
| External Validation | R²pred | PRESS/SSY (test set) | > 0.6 | Good external predictive ability |
| Goodness-of-Fit | R² | 1 - RSS/TSS | > 0.8 | High explained variance |
| Model Significance | F-value | (R²/p)/((1-R²)/(n-p-1)) | p < 0.05 | Statistically significant model |
| Chance Correlation | cR²p (Y-randomization) | - | > 0.5 | Model not due to chance |
ADMET Integration Challenges
Pitfall Description: Traditional 3D-QSAR models often focus exclusively on potency optimization while neglecting critical ADMET properties, leading to compounds with excellent target affinity but poor pharmacokinetic profiles or unacceptable toxicity [6] [61].
Consequences: Disregarding ADMET properties during lead optimization contributes to high attrition rates in later development stages. In cancer drug design, this is particularly problematic due to the narrow therapeutic index of many oncology compounds and their complex metabolism and distribution profiles [61].
Solution Protocol:
- Parallel ADMET Modeling: Develop separate 3D-QSAR models for key ADMET endpoints including solubility, permeability, metabolic stability, and toxicity in addition to primary efficacy models [6] [61].
- Multi-Parameter Optimization: Integrate predictions from efficacy and ADMET models to select compounds balancing potency with favorable pharmacokinetic properties. Utilize desirability functions or Pareto optimization approaches [6].
- Advanced Modeling Techniques: Implement graph neural networks (GNNs) and other machine learning approaches that directly use molecular structures (e.g., SMILES) without requiring predefined descriptors, enabling more comprehensive ADMET prediction [61].
- Experimental Verification: Include key ADMET assays early in the screening cascade to validate computational predictions and refine models iteratively as experimental data accumulates [63].
Integrated 3D-QSAR Workflow for Cancer Drug Design
The following workflow diagram illustrates a comprehensive protocol integrating the solutions to common pitfalls in anticancer 3D-QSAR modeling:
Workflow Title: Comprehensive 3D-QSAR Protocol for Cancer Drug Design
Essential Research Reagents and Computational Tools
Successful implementation of 3D-QSAR modeling requires specific computational tools and methodological approaches. The following table details key resources and their applications in developing robust models for anticancer drug discovery.
Table 3: Essential Research Reagent Solutions for 3D-QSAR Studies
| Category | Tool/Resource | Specific Application | Function in 3D-QSAR Workflow |
|---|---|---|---|
| Molecular Modeling Suites | Forge (Cresset) | Field-based alignment & 3D-QSAR | Molecular alignment, field calculation, QSAR model development [63] [62] |
| SYBYL (Tripos) | CoMFA/CoMSIA analysis | Standard 3D-QSAR implementation with extensive statistical analysis [14] [66] | |
| ChemBio3D (PerkinElmer) | 3D structure generation | 2D to 3D structure conversion and initial geometry optimization [63] | |
| Docking & Conformation Tools | AutoDock Vina | Bioactive conformation prediction | Molecular docking to generate putative bioactive conformations [60] |
| FieldTemplater (Cresset) | Pharmacophore generation | Identification of bioactive template for alignment [63] [62] | |
| Validation & Statistics | QSARINS | Model validation | External validation, applicability domain, advanced statistics [65] |
| MATLAB/Python | Custom statistical analysis | Implementation of specialized validation protocols [61] | |
| ADMET Prediction | ADMET Prediction Modules | PK/toxicity profiling | Integration of permeability, metabolism, and toxicity predictions [6] [61] |
| Graph Neural Networks | ADMET from structure | Direct ADMET prediction from molecular structure [61] |
Robust 3D-QSAR modeling in cancer drug design requires meticulous attention to multiple methodological aspects, with molecular alignment representing the most critical factor influencing model success. By implementing the protocols outlined in this application note—particularly the activity-blind alignment approach, comprehensive validation strategies, and integrated ADMET assessment—researchers can significantly enhance the predictive capability and practical utility of their models. The provided workflow and reagent solutions offer a structured framework for developing 3D-QSAR models that effectively balance potency optimization with favorable pharmacokinetic properties, ultimately accelerating the discovery of novel anticancer therapeutics with enhanced prospects for clinical success. As 3D-QSAR methodologies continue to evolve, particularly with advances in machine learning and structural biology, adherence to these fundamental principles will remain essential for generating biologically meaningful computational models.
In modern cancer drug design, the prediction of ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties using Three-Dimensional Quantitative Structure-Activity Relationship (3D-QSAR) models is indispensable for reducing late-stage attrition. However, the reliability of these predictions is fundamentally constrained by two interconnected pillars: the intrinsic data quality of the training set and the definition of the model's applicability domain (AD) [14] [68]. Data quality ensures the model is built on a foundation of accurate, consistent, and relevant biological and structural data. The applicability domain defines the chemical space within which the model's predictions can be considered reliable, safeguarding against extrapolation into areas where the model was not trained [14]. This application note details protocols and best practices for ensuring both aspects within the context of 3D-QSAR models for anti-cancer drug development, illustrated with recent case studies.
Data Quality Assessment Protocols
High-quality input data is the non-negotiable prerequisite for developing predictive 3D-QSAR models. The following protocols outline the critical steps for data preparation and validation.
Chemical and Biological Data Curation
Objective: To assemble a structurally diverse dataset of compounds with reliable, consistent, and comparable biological activity data.
- Protocol Steps:
- Compound Selection: Select compounds with structural diversity but a common mechanism of action (e.g., inhibition of a specific target like Tubulin in breast cancer [8] or DNA gyrase B in E. coli [14]). The dataset should be sufficiently large (e.g., >30 compounds) to ensure statistical robustness.
- Structure Standardization: Use software like BIOVIA Discovery Studio [13] to prepare 3D molecular structures.
- Generate probable tautomers and protomers at physiological pH.
- Perform geometry optimization using computational methods such as Density Functional Theory (DFT) with the B3LYP functional and basis sets like 6-31G(d,p) to obtain energetically stable 3D conformations [8].
- Biological Activity Consistency: Express biological activity (e.g., IC₅₀, MIC) in a uniform, comparable unit. The recommended practice is to use pIC₅₀ or pMIC (-logIC₅₀ or -logMIC) as the dependent variable in the QSAR model [14] [8]. Ensure all data points originate from the same or highly comparable experimental assays to minimize inter-assay variability.
Data Quality Control Metrics
Objective: To quantitatively assess the completeness and plausibility of the dataset.
- Protocol Steps:
- Completeness Check: Ensure no critical data points (structures or activity values) are missing. The dataset should be curated to remove duplicates and handle inconclusive results [13].
- Plausibility Verification: Check activity values and structural descriptors for outliers that fall outside a statistically defined range (e.g., ±3 standard deviations from the mean). Investigate and justify or rectify any extreme values.
Table 1: Key Data Quality Checks for 3D-QSAR Model Development
| Check Category | Specific Metric | Target Threshold / Action |
|---|---|---|
| Structure Integrity | Presence of 3D Coordinates | 100% of compounds |
| Valence and Charge Sanity | All structures chemically valid | |
| Biological Data | Activity Value Uniformity | All in pIC₅₀ or pMIC |
| Source Assay Consistency | Single, validated assay protocol | |
| Dataset Composition | Structural Diversity | Maximize within target scope |
| Activity Range Spread | Cover at least 3-4 log units |
Defining the Applicability Domain
The Applicability Domain (AD) is the region of chemical space defined by the training set's structures and response values. Predictions for compounds outside this domain are considered unreliable [14].
Methodologies for Characterizing the AD
Objective: To establish a boundary for the model's reliable use.
- Protocol Steps:
- Descriptor-Based Range: This is the most common method. Calculate the range (e.g., min and max) for each molecular descriptor in the training set. A new compound is considered within the AD if the values for all its descriptors lie within these ranges [14] [68].
- Leverage-Based Approach: Use the Hat matrix, calculated from the descriptor matrix of the training set. The leverage (h) of a new compound indicates its distance from the centroid of the training set. A compound is considered influential (and potentially outside the AD) if its leverage exceeds a critical threshold, typically ( h > 3p'/n ), where ( p' ) is the number of model parameters plus one, and ( n ) is the number of training compounds [14].
- Distance-Based Methods: Calculate the similarity of a new compound to its k-nearest neighbors in the training set using metrics like Euclidean distance. If the average distance exceeds a pre-defined threshold, the compound is outside the AD [68].
The following diagram illustrates the logical workflow for assessing a compound's position relative to the Applicability Domain.
Case Study: External Validation and AD in Anti-Breast Cancer Agents
A study on 1,4-quinone and quinoline derivatives for breast cancer demonstrated the importance of external validation, a key process for testing the model—and by extension, its AD—on unseen data. The robust 3D-QSAR models (CoMFA and CoMSIA) were built and their predictive capabilities were confirmed through external validation [6]. This step is critical because a model with a well-defined AD will perform well on an external test set that falls within its chemical space. The study successfully identified electrostatic, steric, and hydrogen bond acceptor fields as crucial for activity and, through ADMET evaluation and molecular dynamics simulations, pinpointed one designed compound as the most promising candidate for experimental testing [6].
Integrated Workflow for Reliable ADMET Prediction
Combining data quality and AD definition into a single, robust workflow is essential for reliable ADMET prediction in cancer drug design.
Table 2: Research Reagent Solutions for 3D-QSAR and ADMET Modeling
| Tool / Reagent | Type | Primary Function in Research |
|---|---|---|
| BIOVIA Discovery Studio | Software Suite | Comprehensive platform for performing QSAR, calculating ADMET properties, and predictive toxicology [13]. |
| Gaussian 09W | Quantum Chemistry Software | Computes electronic descriptors and optimizes 3D molecular geometries using methods like DFT [8]. |
| ChemOffice Software | Cheminformatics Suite | Calculates key topological descriptors (e.g., LogP, LogS, PSA) essential for QSAR models and ADMET prediction [8]. |
| PDTOs (Patient-Derived Tumour Organoids) | Biological Model | 3D in vitro cultures that better recapitulate tumour structure, providing more accurate data for model training and validation [69]. |
| AI/ML Algorithms (e.g., ANN, RF) | Computational Method | Used to derive highly predictive, non-linear 3D-QSAR models and to aid in defining complex applicability domains [68] [70]. |
The following workflow diagram outlines the integrated process from data collection to reliable prediction, highlighting where data quality and AD checks are critical.
In the context of 3D-QSAR for cancer drug design, a model is only as useful as the confidence in its predictions. Rigorous data quality assessment during the initial stages of model development creates a solid foundation. Explicitly defining and checking the Applicability Domain during implementation ensures that this confidence is not misplaced when the model is applied to novel compounds. The integrated protocols outlined in this document provide a framework for researchers to generate and use 3D-QSAR models for ADMET prediction responsibly, thereby de-risking the drug discovery pipeline and accelerating the development of safer, more effective oncology therapeutics.
The adoption of complex artificial intelligence (AI) and machine learning (ML) models has become pervasive in modern computational drug discovery, including the specific domain of ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) property prediction within 3D-QSAR (Three-Dimensional Quantitative Structure-Activity Relationship) cancer research. While these models offer superior predictive accuracy for identifying promising anti-cancer compounds, this often comes at the cost of transparency, creating a significant "black box" problem [71] [72]. As these models guide critical decisions in prioritizing drug candidates for synthesis and experimental testing, understanding their rationale becomes paramount for building scientific trust, ensuring accountability, and extracting meaningful biochemical insights [73] [74].
The trade-off between model performance and interpretability is a central challenge. Simple, intrinsically interpretable models like linear regression or decision trees provide transparency but often lack the expressive power to capture the complex, non-linear relationships between molecular structure, biological activity, and pharmacokinetic properties [73] [72]. Conversely, highly complex models such as deep neural networks and ensemble methods can achieve state-of-the-art predictive performance but are notoriously difficult to interpret, functioning as inscrutable black boxes [71] [73]. This is particularly problematic in sensitive fields like healthcare and drug development, where model decisions can have profound consequences [72]. Explainable AI (XAI) has thus emerged as a critical field of study, providing a suite of strategies and methods to illuminate the inner workings of these complex models, making their predictions more understandable and actionable for researchers [74] [72].
Foundational Interpretability Concepts and Taxonomies
To effectively navigate the landscape of interpretability methods, it is essential to understand fundamental distinctions in their design and application. First, a differentiation is often made between interpretability and explainability. Interpretability is broadly defined as the ability to explain or present the model's behavior in understandable terms to a human, often focusing on the intuition behind a model's inputs and outputs. Explainability, meanwhile, is frequently associated with a deeper understanding of the internal logic and mechanics of the AI system itself [72].
A fundamental taxonomy categorizes approaches based on their implementation strategy. Intrinsic Interpretability refers to using models that are inherently interpretable by design, such as linear models, decision trees, or decision rules [75]. These models prioritize transparency, and their entire structure can be comprehended by a human [74] [75]. In contrast, Post-hoc Interpretability involves applying interpretation methods after a complex, potentially black-box model has been trained. These methods analyze the model without simplifying its underlying complexity [75]. Post-hoc methods can be further divided into:
- Model-Specific Methods: These rely on the internal structures of specific model types, such as analyzing feature importance in random forests or visualizing feature maps in convolutional neural networks [75].
- Model-Agnostic Methods: These treat the trained model as a black box and interpret it by analyzing its input and output patterns. They offer great flexibility as they can be applied to any model [73] [75].
Finally, model-agnostic methods can operate at two levels: Global Interpretability, which seeks to understand the model's overall behavior across the entire dataset, and Local Interpretability, which focuses on explaining individual predictions [74] [75].
Key Interpretability Methods and Their Applications to 3D-QSAR
A diverse toolkit of model-agnostic, post-hoc methods has been developed to address the black-box problem. The following table summarizes several prominent techniques, their characteristics, and their relevance to computational drug design.
Table 1: Key Post-hoc, Model-Agnostic Interpretability Methods
| Method | Scope | Core Principle | Relevance to 3D-QSAR/ADMET |
|---|---|---|---|
| Partial Dependence Plots (PDP) [73] | Global | Shows the marginal effect of one or two features on the predicted outcome. | Visualizing the average relationship between a specific molecular descriptor (e.g., steric bulk, logP) and predicted activity or toxicity. |
| Individual Conditional Expectation (ICE) [73] | Local | Plots the change in prediction for each individual instance as a feature varies. | Uncovering heterogeneous effects; e.g., why a change in electronegativity improves activity for some molecular scaffolds but not others. |
| Permuted Feature Importance [73] | Global | Measures the increase in model error after shuffling a feature's values. | Ranking molecular descriptors (e.g., from CoMFA/CoMSIA fields) by their impact on the model's prediction of pIC50. |
| SHAP (SHapley Additive exPlanations) [73] | Global & Local | Based on game theory, it allocates the prediction for an instance as a sum of contributions from each feature. | Quantifying the exact contribution of each molecular field (steric, electrostatic) to the predicted activity of a single compound. |
| LIME (Local Interpretable Model-agnostic Explanations) [73] | Local | Approximates a complex model locally with an interpretable one (e.g., linear model) to explain individual predictions. | Creating a simple "rule" for why a specific drug candidate was predicted to have high hepatotoxicity. |
| Counterfactual Explanations [74] | Local | Identifies the minimal changes to an input required to alter the model's prediction. | Providing actionable guidance: "To reduce predicted cardiotoxicity, decrease the molecular weight and increase the polar surface area." |
These methods operate on the SIPA principle: Sample from the data, Intervene on the data (e.g., permute a feature), get the Predictions, and Aggregate the results [75]. This model-agnostic process allows them to probe any ML model used in a 3D-QSAR pipeline.
Integrated Protocol for Interpretable ADMET Prediction in Anti-Cancer Drug Design
This protocol outlines a systematic workflow for integrating interpretability methods into a 3D-QSAR study focused on ADMET prediction for novel anti-cancer agents, such as the 1,2,4-triazine-3(2H)-one derivatives studied as tubulin inhibitors [8].
The following diagram illustrates the integrated experimental and computational workflow, highlighting key stages where interpretability methods are applied.
Protocol Steps
Step 1: Data Preparation and Model Training
- Compound Database Assembly: Curate a dataset of known compounds with experimental biological activities (e.g., IC50 against MCF-7 breast cancer cells) and ADMET properties. Convert IC50 values to pIC50 (-log IC50) to minimize skewness [8] [76].
- Molecular Descriptor Calculation: Compute a comprehensive set of molecular descriptors. These can include:
- 3D-Field Descriptors: Generate steric, electrostatic, hydrophobic, and hydrogen-bond donor/acceptor fields using CoMFA (Comparative Molecular Field Analysis) or CoMSIA (Comparative Molecular Similarity Indices Analysis) [52] [76] [77].
- Quantum Chemical Descriptors: Calculate electronic properties (e.g., EHOMO, ELUMO, absolute electronegativity (χ), dipole moment) using Density Functional Theory (DFT) with a basis set like B3LYP/6-31G* [8].
- Topological Descriptors: Calculate properties like molecular weight, logP, logS, polar surface area, and number of rotatable bonds using software like ChemOffice [8].
- Model Training: Split the data into training and test sets (e.g., 80:20). Train a high-performance, complex ML model (e.g., Random Forest, XGBoost, or Neural Network) using the calculated descriptors to predict the target property (e.g., pIC50, toxicity) [8].
Step 2: Global Model Interpretation
- Execute Permutation Feature Importance: Use this method to rank all molecular descriptors (from Step 1.2) by their importance to the model's predictive performance [73]. This identifies which global structural features the model deems most critical for activity/ADMET.
- Generate Partial Dependence Plots (PDPs): For the top 3-5 most important features, create PDPs to visualize the average marginal effect of each descriptor on the model's prediction [73]. This reveals the nature of the relationship (e.g., monotonic, parabolic).
Step 3: Lead Candidate Identification and Local Interpretation
- Predict and Select: Use the trained model to predict the activity/ADMET profile of novel, designed compounds. Select the most promising lead candidates for deeper analysis [6] [8].
- Perform Local Explanation with SHAP: For each lead candidate, calculate SHAP values. This quantifies how much each molecular descriptor contributed to pushing the model's prediction from a base value to the final predicted value for that specific compound [73]. This is crucial for understanding the specific structural rationale for a compound's predicted high activity or low toxicity.
Step 4: Computational Validation and Insight Generation
- Cross-validate with Molecular Docking: Perform molecular docking studies to visualize the binding mode of the lead candidates to the target protein (e.g., Tubulin for triazine derivatives [8] or Aromatase for thioquinazolinones [76]). Confirm that the key structural features highlighted by the interpretability methods (e.g., a specific steric bulk or hydrogen bond acceptor) correspond to favorable interactions in the protein's active site [6] [76].
- Assess Binding Stability with MD Simulations: Run molecular dynamics (MD) simulations (e.g., for 50-100 ns) for the top protein-ligand complexes. Analyze stability metrics like Root Mean Square Deviation (RMSD) and Root Mean Square Fluctuation (RMSF) to ensure the binding pose suggested by docking and the features identified by the model remain stable over time [6] [8] [77].
- Integrate Findings: Synthesize insights from global interpretation, local SHAP explanations, docking, and MD simulations to build a coherent and trustworthy story about the structure-activity-toxicity relationships. This integrated confidence is key for justifying the selection of candidates for costly synthetic and experimental validation.
The Scientist's Toolkit: Essential Research Reagents and Computational Solutions
Table 2: Key Research Reagent Solutions for Interpretable AI in Drug Design
| Tool / Resource | Function / Description | Application Example |
|---|---|---|
| SYBYL-X | A comprehensive molecular modeling software suite. | Used for ligand alignment, energy minimization, and generating CoMFA/CoMSIA 3D-field descriptors [52] [77]. |
| Gaussian 09W | Software for electronic structure calculations. | Computes quantum chemical descriptors (e.g., EHOMO, ELUMO) via Density Functional Theory (DFT) [8]. |
| AutoDock Vina | A program for molecular docking. | Predicts the binding conformation and affinity of small molecule ligands to a protein target [77]. |
| GROMACS / AMBER | Software packages for molecular dynamics simulations. | Simulates the physical movements of atoms and molecules over time to assess complex stability [6] [8]. |
| SHAP / LIME Python Libraries | Open-source Python packages implementing interpretability algorithms. | Integrated into a custom Python script to calculate feature contributions for any ML model's predictions [73] [74]. |
| SwissADME / pkCSM | Freely accessible web servers for pharmacokinetic prediction. | Used for in silico prediction of key ADMET properties like solubility, permeability, and toxicity [52] [8]. |
The "black box" nature of complex AI/ML models is no longer an insurmountable barrier to their adoption in critical areas like cancer drug discovery. By strategically employing a combination of intrinsic interpretability, post-hoc global analysis (e.g., PDP, Feature Importance), and local explanation techniques (e.g., SHAP, LIME), researchers can transform opaque predictions into transparent, actionable insights. Integrating these XAI methods with established computational techniques like 3D-QSAR, molecular docking, and dynamics creates a powerful, rigorous, and trustworthy framework for decision-making. This allows scientists to not only identify promising anti-cancer drug candidates with favorable ADMET profiles but also to understand the underlying structural reasons for those predictions, thereby accelerating the rational design of safer and more effective therapeutics.
Balancing Predictive Power with Computational Efficiency
In modern cancer drug design, the integration of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) prediction within 3D Quantitative Structure-Activity Relationship (3D-QSAR) frameworks presents a critical challenge: achieving sufficient predictive accuracy while maintaining computationally feasible workflows. The high attrition rates in drug development, often attributed to poor pharmacokinetics and unforeseen toxicity, underscore the necessity of early and reliable ADMET assessment [53]. Traditional experimental methods, while reliable, are resource-intensive and low-throughput, creating an urgent need for computational approaches that balance sophistication with practicality [53] [34]. This balance is particularly crucial in cancer research, where the complexity of biological systems and the need for rapid therapeutic advancement demand models that are both biologically insightful and computationally scalable. Machine learning (ML) technologies have emerged as transformative tools in this domain, enhancing the efficiency of predicting drug properties and streamlining various stages of the development pipeline [53]. This document provides detailed application notes and protocols for implementing such balanced approaches, with specific examples from 3D-QSAR-based cancer drug design.
Machine Learning Advances in ADMET Prediction
Recent machine learning advances have significantly transformed ADMET prediction by deciphering complex structure–property relationships, providing scalable, efficient alternatives to conventional methods [53]. These approaches range from feature representation learning to deep learning and ensemble strategies, demonstrating remarkable capabilities in modeling complex activity landscapes.
Table 1: Machine Learning Approaches for ADMET Prediction in Cancer Drug Design
| ML Approach | Key Advantages | Computational Demand | Exemplary Applications in ADMET |
|---|---|---|---|
| Graph Neural Networks (GNNs) | Directly learns from molecular graph structures; captures complex topological features [53]. | High (requires significant GPU memory and processing power) | Predicting drug metabolism pathways and toxicity endpoints [53]. |
| Ensemble Learning | Combines multiple models to improve robustness and predictive accuracy [53]. | Medium to High (scales with number of base models) | Integrating various QSAR predictions for improved ADMET profiling [53] [22]. |
| Multitask Learning (MTL) | Simultaneously learns multiple related properties; improves data efficiency and generalizability [53]. | Medium (shared parameters reduce total parameters) | Concurrent prediction of absorption, toxicity, and solubility [53] [78]. |
| Deep Neural Networks (DNNs) | High expressivity; can model complex, non-linear relationships in high-dimensional data [79]. | Very High (driven by model depth and width) | Pan-cancer drug response prediction from genomic and compound features [78]. |
| Multiple Linear Regression (MLR) | Simple, interpretable, low computational footprint [80]. | Very Low | Building foundational QSAR models for NF-κB inhibitors [80]. |
| Artificial Neural Networks (ANNs) | Non-linear mapping capability; more accurate than MLR for complex relationships [80]. | Low to Medium (depends on network architecture) | Superior predictive performance for NF-κB inhibitor activity compared to MLR [80]. |
The selection of an appropriate model architecture is governed by the bias-variance tradeoff [79]. Insufficiently expressive architectures (e.g., simple linear models) have high bias and perform poorly on both training and test data. Conversely, overly expressive models (e.g., large DNNs) risk overfitting, capturing noise in the training data and failing to generalize to new compounds [79]. The key is to match the model's complexity to the available data and the complexity of the ADMET endpoint being predicted.
Integrated Computational Protocols
The following protocols outline a standardized workflow for developing predictive ADMET models within a 3D-QSAR framework, emphasizing the balance between accuracy and efficiency.
Protocol 1: Development of a Robust 3D-QSAR Model with Applicability Domain
This protocol is adapted from studies on NF-κB inhibitors and 1,2,4-triazine-3(2H)-one derivatives as Tubulin inhibitors [80] [8].
Objective: To create a predictive 3D-QSAR model while defining its applicability domain to ensure reliable predictions.
Materials & Reagents:
- Software: Sybyl-X (or equivalent molecular modeling suite), Gaussian 09W/ChemOffice for descriptor calculation, CORAL software for Monte Carlo optimization (optional).
- Dataset: A curated set of compounds (typically >20) with consistent experimental bioactivity data (e.g., IC50 against a cancer cell line) [80] [8].
Procedure:
- Dataset Curation and Preparation:
- Collect a minimum of 20 compounds with comparable bioactivity values obtained through a standardized experimental protocol (e.g., MTT assay for cell viability) [80] [8].
- Convert IC50 values to pIC50 (-logIC50) for model construction [8].
- Divide the dataset randomly into a training set (~80%) for model development and a test set (~20%) for external validation [8].
Molecular Modeling and Descriptor Calculation:
- Construct and optimize the 3D geometry of all compounds. For example, use the DFT method with B3LYP functional and 6-31G (p, d) basis set for electronic descriptor calculation [8].
- Calculate molecular descriptors. These can be:
- 3D-Field Descriptors: Generate steric (van der Waals) and electrostatic (Coulombic) fields using CoMFA (Comparative Molecular Field Analysis) [14].
- Electronic Descriptors: Compute quantum chemical descriptors like EHOMO, ELUMO, absolute electronegativity (χ), and water solubility (LogS) [8].
- Topological Descriptors: Calculate descriptors like molecular weight, LogP, polar surface area using software like ChemOffice [8].
Model Building and Validation:
- For CoMFA/CoMSIA, use the training set to generate the model and leave-one-out (LOO) cross-validation to obtain the cross-validated correlation coefficient (q²). A q² > 0.5 is generally acceptable [26] [14].
- Build a final model using the entire training set and evaluate its goodness-of-fit with the conventional correlation coefficient (r²) and standard error of estimate (SEE) [26].
- Critical Step - Validate the Model: Use the external test set to calculate the predictive r² (R²pred). The model is considered predictive if R²pred > 0.5-0.6 [80] [8].
Define the Applicability Domain (Leverage Method):
- Calculate the leverage (h) for each compound in the training set and the new compound to be predicted.
- Determine the critical leverage (h*) as 3p'/n, where p' is the number of model parameters plus one, and n is the number of training compounds.
- A new compound with a leverage lower than h* is within the applicability domain, and its prediction is considered reliable. Predictions for compounds with leverage > h* should be treated with caution [80].
Protocol 2: High-Throughput ADMET Screening and Prioritization
This protocol is adapted from integrated studies on naphthoquinone derivatives and 1,2,4-triazine-3(2H)-one derivatives [22] [8].
Objective: To rapidly screen a large virtual library of compounds for desirable ADMET properties before synthesis or expensive experimental testing.
Materials & Reagents:
- Software: ADMET prediction platforms (e.g., ADMETlab 2.0), molecular docking software (e.g., AutoDock Vina, GOLD).
- Dataset: A virtual library of designed compounds (e.g., 2,435 naphthoquinone derivatives) [22].
Procedure:
- Generate Virtual Compound Library:
- Design novel compounds based on the structural insights from a validated 3D-QSAR model (e.g., from Protocol 1).
- Use the model to predict the primary bioactivity (e.g., pIC50) for all designed compounds [22].
In Silico ADMET Profiling:
- For all compounds with satisfactory predicted activity, compute key ADMET properties. These typically include:
- Filter the library based on pre-defined ADMET criteria (e.g., Lipinski's Rule of Five, low hERG inhibition, acceptable solubility) [22]. This step drastically reduces the number of candidates for further study.
Molecular Docking for Target Engagement:
- Select the top compounds passing the ADMET filter for molecular docking studies.
- Prepare the protein target (e.g., Tubulin for breast cancer, PDB ID: 1ZXM) by removing water molecules and adding hydrogens.
- Dock the compounds into the active site and evaluate their binding affinity (docking score) and binding mode (interactions with key amino acids) [22] [8].
- A reference control (e.g., Doxorubicin) should be included for comparison [22].
Candidate Prioritization:
- Rank the compounds based on a combined assessment of their predicted bioactivity, ADMET profile, and docking score.
- Select the top 1-2% of the initial virtual library for synthesis and experimental validation [22].
Table 2: Key ADMET Properties for Early-Stage Screening in Cancer Drug Design
| ADMET Property | Target/Model | Computational Cost | Desired Profile for Oral Drugs | Role in Balancing Efficiency |
|---|---|---|---|---|
| Water Solubility (LogS) | Physicochemical property | Low | > -4 log mol/L | Early filter to eliminate compounds with poor bioavailability [22]. |
| hERG Inhibition | Potassium ion channel (cardiotoxicity) | Low to Medium | Low predicted affinity | Critical for de-risking late-stage failure due to toxicity; high-cost experimental assay [22] [34]. |
| CYP450 Inhibition | Cytochrome P450 enzymes (e.g., CYP3A4) | Medium | Low inhibition potential | Predicts drug-drug interactions; avoids costly clinical trial failures [53] [22]. |
| Plasma Protein Binding | Human serum albumin | Low | Moderate to low binding | High PPB can limit efficacy; prediction informs dose optimization [53]. |
| P-glycoprotein Substrate | Efflux transporter | Medium | Not a substrate | Avoids reduced absorption and multi-drug resistance [53]. |
Protocol 3: Validation via Molecular Dynamics (MD) Simulations
Objective: To confirm the binding stability and dynamic behavior of the top-prioritized candidate(s) from Protocol 2, providing a higher-fidelity (but computationally expensive) validation step.
Materials & Reagents:
- Software: MD simulation packages (e.g., GROMACS, AMBER), molecular visualization tools (e.g., PyMOL, VMD).
- Input: The top ligand-protein complex from molecular docking.
Procedure:
- System Preparation:
- Take the best-docked pose of the top candidate and place it in a solvation box (e.g., TIP3P water model).
- Add ions to neutralize the system's charge and achieve physiological salt concentration.
Simulation Run:
Trajectory Analysis:
- Root Mean Square Deviation (RMSD): Calculate the RMSD of the protein-ligand complex backbone. A stable or convergent RMSD profile indicates a stable complex [22] [8].
- Root Mean Square Fluctuation (RMSF): Analyze RMSF to understand the flexibility of residue side chains upon ligand binding.
- Interaction Analysis: Monitor the persistence of key hydrogen bonds, hydrophobic contacts, and salt bridges throughout the simulation timeline. This provides mechanistic insight into binding stability beyond static docking [22].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for ADMET-Informed 3D-QSAR
| Tool/Resource Name | Type | Primary Function in Workflow |
|---|---|---|
| Sybyl-X | Commercial Software Suite | Core platform for performing 3D-QSAR methodologies like CoMFA and CoMSIA [26] [14]. |
| Gaussian 09W | Quantum Chemistry Software | Calculates high-level electronic descriptors (e.g., EHOMO, ELUMO) for QSAR models and DFT-based geometry optimization [8]. |
| CORAL Software | QSAR Modeling Software | Utilizes Monte Carlo optimization with SMILES notation to build robust QSAR models using descriptors like the Index of Ideality of Correlation (IIC) [22]. |
| ADMETlab 2.0 | Web-Based Platform | Provides integrated, high-throughput predictions for a wide array of ADMET properties, facilitating early-stage screening [34]. |
| GROMACS | Molecular Dynamics Engine | Performs high-performance MD simulations to validate the stability and interactions of ligand-protein complexes over time [22] [8]. |
| TensorFlow/PyTorch | Deep Learning Frameworks | Provides the foundation for building and training complex ML models (GNNs, DNNs) for drug response and ADMET prediction [78]. |
The strategic integration of 3D-QSAR with machine learning-driven ADMET prediction represents a paradigm shift in cancer drug design, effectively balancing predictive power with computational efficiency. The protocols outlined demonstrate a tiered approach: starting with computationally inexpensive models and filters to rapidly explore chemical space, followed by progressively more resource-intensive methods (docking, MD) for deep validation of top candidates. This ensures that computational resources are allocated efficiently, focusing high-fidelity simulations only on the most promising compounds. As machine learning continues to evolve, with growing emphasis on explainable AI (XAI) and multimodal data integration, this balance will become even more refined, further accelerating the discovery of safe and effective cancer therapeutics [53] [79] [81].
Addressing Limitations in Predicting In Vivo Outcomes from In Silico Models
The high attrition rate of oncology drug candidates, with over 97% failing in clinical trials, underscores a critical disconnect between computational predictions and clinical outcomes [1]. While in silico models, particularly 3D Quantitative Structure-Activity Relationship (3D-QSAR) and ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) prediction tools, have revolutionized early drug discovery by accelerating lead optimization, their predictive power often diminishes for complex in vivo environments [1] [51] [82]. This application note details protocols and methodologies designed to enhance the reliability of translating in silico 3D-QSAR and ADMET predictions to in vivo efficacy and safety within cancer drug design. We focus on addressing key limitations through advanced dynamic modeling, rigorous validation, and multi-scale computational integration to bridge the in vitro-in vivo gap.
Core Limitations and Quantitative Analysis
The table below summarizes the primary challenges in predicting in vivo outcomes from in silico models and their quantitative impact on the drug discovery pipeline.
Table 1: Key Limitations in Predicting In Vivo Outcomes from In Silico Models
| Limitation Category | Specific Challenge | Impact on Drug Discovery |
|---|---|---|
| Data Quality & Standardization | Variability in experimental conditions (e.g., buffer, pH) for training data; Lack of drug-like molecules in public datasets [83]. | Leads to models with poor external predictability and limited applicability to real-world drug candidates. |
| Model Static Nature | Most QSAR models are static, tailored to specific time points and doses [84]. | Fails to capture the dynamic nature of ADMET properties and toxicological responses over time, crucial for in vivo translation. |
| Biological Complexity Gap | Inability of initial models to account for systemic effects: protein binding, metabolic stability, multi-organ interactions [51]. | Overestimation of in vivo efficacy and underestimation of toxicity, contributing to late-stage clinical failures. |
| Applicability Domain (AD) | Predictions for chemicals structurally different from the training set are unreliable [82]. | High rate of false positives during virtual screening, wasting resources on non-viable leads. |
Advanced Methodologies and Protocols
Protocol 1: Developing Dynamic QSAR Models
Static models are a significant limitation. This protocol outlines the development of a Dynamic QSAR model that incorporates time and dose as variables to better simulate in vivo conditions [84].
1. Data Curation and Harmonization
- Objective: Collect a robust dataset with temporal and dose-response dimensions.
- Procedure:
- Gather experimental data from public repositories (e.g., ChEMBL, PubChem) and in-house sources, ensuring it spans multiple time points and administered doses [84] [83].
- For toxicity data, include endpoints like in vivo genotoxicity in tissues and neutrophil influx for inflammation across various post-exposure times (e.g., 1, 3, 28, 90 days) [84].
- Extract Experimental Conditions using LLMs: Implement a multi-agent Large Language Model (LLM) system to automatically parse and standardize critical experimental conditions (e.g., buffer type, pH, assay procedure) from unstructured assay descriptions in databases. This ensures data consistency [83].
2. Descriptor Calculation and Feature Engineering
- Objective: Generate molecular descriptors that encode structural and physicochemical properties.
- Procedure:
3. Model Building and Validation
- Objective: Train a machine learning model to predict biological activity as a function of structure, time, and dose.
- Procedure:
- Apply machine learning algorithms (e.g., Random Forest, Support Vector Machine, Multilayer Perceptron) to build the predictive model [36] [84].
- Validate the model using rigorous k-fold cross-validation and an external test set.
- Critically, define the model's Applicability Domain (AD) using approaches like leverage and distance measures to identify for which compounds, time points, and doses the predictions can be considered reliable [82].
The following workflow diagram illustrates the dynamic QSAR modeling process:
Protocol 2: Integrated 3D-QSAR, Molecular Docking, and ADMET Workflow
A multi-faceted approach that combines ligand- and structure-based methods significantly improves the predictive power for in vivo outcomes [6] [8].
1. Robust 3D-QSAR Model Development
- Objective: Establish a quantitative model linking the 3D molecular fields of compounds to their biological activity.
- Procedure:
- Align a set of active compounds using a common scaffold or pharmacophore.
- Use Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA) to calculate steric, electrostatic, hydrophobic, and hydrogen-bond donor/acceptor fields around the molecules [86] [6].
- Build the model using Partial Least Squares (PLS) regression. Validate with techniques like leave-one-out cross-validation and an external test set, ensuring high R² and Q² values [85] [6].
2. Structure-Based Validation with Docking and Dynamics
- Objective: Confirm the binding mode and stability of predicted active compounds to the target protein.
- Procedure:
- Perform molecular docking of top candidates (e.g., from a virtual screen) into the target's binding site (e.g., Tubulin's colchicine site for cancer therapy) to predict binding affinity and key interactions (e.g., with residues Ile62, Tyr128, Leu182 for GSK-3β) [85] [8].
- Run Molecular Dynamics (MD) simulations (e.g., 100 ns) to assess the stability of the protein-ligand complex in a solvated, dynamic environment.
- Analyze Root Mean Square Deviation (RMSD), Root Mean Square Fluctuation (RMSF), Radius of Gyration (Rg), and the number of hydrogen bonds.
- Perform MM-PBSA (Molecular Mechanics Poisson-Boltzmann Surface Area) calculations to estimate binding free energies, providing a more robust affinity measure than docking scores alone [6] [8].
3. In Silico ADMET Profiling
- Objective: Early identification of compounds with poor pharmacokinetic or toxicological profiles.
- Procedure:
- Use machine learning models trained on large, curated datasets like PharmaBench to predict critical ADMET endpoints [83].
- Calculate key properties such as:
- Water Solubility (LogS)
- Caco-2 Permeability (for absorption)
- hERG inhibition (cardiotoxicity risk)
- CYP450 enzyme inhibition (metabolic stability)
- Human Liver Microsomal (HLM) Stability [51]
- Integrate these predictions as filters in the lead optimization cycle to prioritize compounds with a higher probability of in vivo success.
The following workflow diagram illustrates this integrated computational strategy:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools and Datasets for Enhanced In Vivo Prediction
| Tool/Resource Category | Specific Examples | Function in Protocol |
|---|---|---|
| Molecular Descriptor Software | Dragon, Gaussian 09W, ChemOffice [85] [51] [8] | Calculates quantitative descriptors of molecular structure and properties for QSAR model building. |
| 3D-QSAR & Modeling Suites | SYBYL (Tripos), Open3DQSAR [86] | Performs molecular alignment, CoMFA/CoMSIA field calculations, and PLS regression analysis. |
| Curated ADMET Databases | PharmaBench, ChEMBL, PubChem, BindingDB [51] [83] | Provides high-quality, standardized experimental data for training and validating predictive ML models. |
| Machine Learning Libraries | Scikit-learn, TensorFlow, PyTorch [51] [84] | Provides algorithms (RF, SVM, Neural Networks) for building both static and dynamic QSAR/ADMET models. |
| Molecular Simulation Software | GROMACS, AMBER, AutoDock Vina [6] [8] | Conducts molecular docking, molecular dynamics simulations, and binding free energy calculations (MM-PBSA). |
| Data Mining & Curation Tools | Multi-Agent LLM Systems (e.g., based on GPT-4) [83] | Automates the extraction and standardization of experimental conditions from unstructured text in scientific databases. |
Benchmarking Success: Validation Strategies and Comparative Analysis of Computational Tools
In the field of 3D-QSAR cancer drug design, the reliability of computational models used for predicting Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties is paramount. Validation has been recognized as one of the decisive steps for checking the robustness, predictability, and reliability of any quantitative structure-activity relationship (QSAR) model to judge the confidence of predictions for new data sets [87]. The OECD principles provide a foundational framework for validating predictive QSAR models, emphasizing the need for appropriate measures of goodness-of-fit, robustness, and predictivity [87]. This document outlines comprehensive statistical metrics and detailed experimental protocols for internal and external validation, specifically contextualized within ADMET property prediction for anticancer drug development.
The Validation Toolkit: Statistical Metrics
A robust validation strategy employs a suite of statistical metrics to evaluate model performance from complementary perspectives. Relying on a single metric, such as the coefficient of determination (r²), is insufficient to prove model validity [88] [89]. The following tables categorize key metrics for both regression-based (e.g., predicting IC₅₀ values) and classification-based (e.g., toxic vs. non-toxic) QSAR models common in ADMET and cancer research.
Table 1: Core Metrics for Regression Models
| Metric | Formula | Interpretation | Application Context |
|---|---|---|---|
| Coefficient of Determination (R²) | 1 - (SS_res/SS_tot) |
Proportion of variance explained by the model. Closer to 1 is better. | General model fit assessment. |
| Root Mean Square Error (RMSE) | √(Σ(Pred_i - Obs_i)² / N) |
Average prediction error in data units. Lower is better. | Assessing overall prediction accuracy. |
| Mean Absolute Error (MAE) | Σ|Pred_i - Obs_i| / N |
Robust average error, less sensitive to outliers. Lower is better. | Error interpretation in original activity units [89]. |
| Concordance Correlation Coefficient (CCC) | 2rσ_xσ_y / (σ_x² + σ_y² + (μ_x - μ_y)²) |
Measures agreement between observed and predicted values (precision & accuracy). Closer to 1 is better. | Superior to R² for measuring agreement. |
| rm² (Modified R²) | r² * (1 - √(r² - r₀²)) |
A stringent metric combining correlation and agreement. >0.5 is acceptable [90]. | Model selection during internal validation. |
Table 2: Core Metrics for Classification Models
| Metric | Formula | Interpretation | Application Context |
|---|---|---|---|
| Precision | TP / (TP + FP) |
Proportion of correct positive predictions. | Critical when false positives are costly (e.g., early lead selection). |
| Recall (Sensitivity) | TP / (TP + FN) |
Proportion of actual positives correctly identified. | Critical when false negatives are costly (e.g., toxicity prediction) [91]. |
| Specificity | TN / (TN + FP) |
Proportion of actual negatives correctly identified. | Important for ruling out inactive compounds [91]. |
| F1 Score | 2 * (Precision * Recall) / (Precision + Recall) |
Harmonic mean of precision and recall. Balances both concerns [91]. | Overall metric for imbalanced datasets. |
| Area Under the ROC Curve (AUC-ROC) | Area under the TP rate vs. FP rate curve. | Measures overall separability between classes. Closer to 1 is better. | General model performance across thresholds. |
| Area Under the PR Curve (AUC-PR) | Area under the Precision-Recall curve. | More informative than ROC for imbalanced datasets [91]. | ADMET tasks where active compounds are rare. |
Experimental Protocols for Validation
Protocol 1: Internal Validation with Cross-Validation
Purpose: To assess the model's robustness and stability using only the training set data, providing an initial estimate of predictive performance before external testing.
Workflow Diagram: Internal Validation via Cross-Validation
Procedure:
- Data Preparation: Start with a cleaned and curated dataset of cancer compounds with known biological activities and calculated molecular descriptors. Ensure chemical structures are standardized (e.g., remove salts, normalize tautomers) and biological activities are in a common unit (e.g., pIC₅₀) [19].
- Data Splitting: Split the entire dataset into
Ksubsets (folds) of approximately equal size and chemical diversity. Common practices in QSAR useK=5orK=10. For smaller datasets, Leave-One-Out Cross-Validation (LOOCV) is an option, whereKequals the number of compounds [87] [19]. - Iterative Training & Prediction: For each iteration
i(from 1 toK):- Designate fold
ias the temporary validation set. - Use the remaining
K-1folds to train the QSAR model (e.g., using Partial Least Squares - PLS, or Support Vector Machines - SVM). - Use the trained model to predict the activities of the compounds in the temporary validation set (fold
i). - Store the predicted values for all compounds in fold
i.
- Designate fold
- Metric Calculation: After all
Kiterations, every compound in the dataset has a cross-validated predicted value. Calculate internal validation metrics (e.g., Q² for regression, AUC-PR for classification) using the observed and cross-validated predicted values [87]. - Final Model Building: Once the internal validation is satisfactory, train the final model on the entire training set for subsequent external validation.
Protocol 2: External Validation with a Hold-Out Test Set
Purpose: To provide a realistic and unbiased assessment of the model's predictive power on completely new, unseen chemical entities, simulating real-world application.
Workflow Diagram: External Validation with a Hold-Out Test Set
Procedure:
- Initial Data Splitting: Before any model development, split the entire dataset into a training set (typically 70-80%) and an external test set (20-30%). This split should be performed using methods like Kennard-Stone or random sampling to ensure the test set is representative of the chemical space of the training set [87] [19]. Crucially, the external test set must be locked away and not used for any aspect of model training or feature selection.
- Model Development: Develop the QSAR model exclusively using the training set data, following steps like descriptor calculation, feature selection, and internal cross-validation (as in Protocol 1).
- Define Applicability Domain (AD): Characterize the AD of the developed model based on the training set. The AD defines the chemical space where the model can make reliable predictions [87]. Methods include:
- Leverage: Defining a threshold for the Hat matrix to identify compounds structurally influential to the model.
- Distance-Based Methods: Using ranges of descriptors or PCA-based Euclidean distance to define the "chemical space" of the training set.
- External Prediction: Apply the final model trained on the entire training set to predict the activities of the compounds in the external test set. Important: Filter the test set predictions through the defined AD. Predictions for compounds falling outside the AD should be flagged as less reliable [87].
- Metric Calculation & Comparison: Calculate external validation metrics (see Table 1) using the observed activities and the model's predictions only for the external test set compounds. Compare these external metrics to the internal cross-validation metrics from the training phase. A significant drop in performance suggests model overfitting.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Software and Tools for QSAR Modeling and Validation
| Tool / Resource | Type | Primary Function in Validation | Relevance to ADMET/Cancer Research |
|---|---|---|---|
| RDKit | Open-Source Cheminformatics Library | Calculates 2D/3D molecular descriptors (e.g., Mordred) and fingerprints for model features [19] [92]. | Standardizes molecular representation before descriptor calculation. |
| PaDEL-Descriptor | Software | Generates a comprehensive set of molecular descriptors and fingerprints for QSAR analysis [19]. | Useful for creating a large pool of features for variable selection. |
| Python/R (scikit-learn, caret) | Programming Environments | Provides libraries for implementing machine learning algorithms, data splitting, cross-validation, and metric calculation. | Enables custom scripting of the entire validation workflow. |
| ADMETlab 3.0 | Web Platform / Model | Provides benchmarked predictions for over 90 ADMET endpoints, usable for external comparison [32]. | Can serve as a source of external data for practical validation scenarios [92]. |
| OECD QSAR Toolbox | Software | Assists in grouping chemicals, filling data gaps, and evaluating QSAR models in a regulatory context. | Helps address OECD Principle 3 (Applicability Domain) and 5 (Mechanistic Interpretation) [87]. |
Advanced Considerations in ADMET Context
Navigating the Limitations of Correlation Coefficients
While the Pearson correlation coefficient (r) is widely used, it has critical limitations in predictive modeling for ADMET properties. It struggles to capture complex, nonlinear relationships, inadequately reflects model errors (especially systematic biases), and lacks comparability across datasets due to high sensitivity to data variability and outliers [89]. Therefore, it is essential to complement r with error-based metrics like MAE and RMSE, which provide a direct measure of prediction accuracy [89]. Furthermore, metrics like the rm² and the Concordance Correlation Coefficient (CCC) offer more stringent validation by assessing both correlation and agreement between observed and predicted values [90].
Validation in a Practical "External" Scenario
A robust validation practice involves testing a model trained on data from one source (e.g., a public database) on a test set from a different source (e.g., an in-house assay) [92]. This "practical scenario" evaluation is a stringent test of generalizability, as it accounts for inter-laboratory variance and differences in experimental protocols. Such an approach is highly recommended for 3D-QSAR models in cancer drug design to build confidence in their application for prospective compound screening.
The accurate prediction of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties represents a critical challenge in modern cancer drug design. High attrition rates in late-stage clinical development, often due to unfavorable pharmacokinetic or safety profiles, have intensified the need for robust computational tools that can reliably forecast these properties early in the discovery pipeline [51]. Within this context, Quantitative Structure-Activity Relationship (QSAR) modeling has evolved significantly, progressing from classical two-dimensional approaches to sophisticated three-dimensional and pure machine learning methods [28]. This evolution has fundamentally transformed the landscape of computer-aided drug design, particularly in complex therapeutic areas such as oncology, where targeted therapies with optimal safety margins are paramount.
The selection of an appropriate modeling strategy directly impacts the efficiency and success of cancer drug discovery campaigns. Classical QSAR, 3D-QSAR, and pure machine learning approaches each offer distinct advantages and limitations for ADMET property prediction [28] [93]. Understanding their comparative strengths, appropriate application domains, and implementation requirements enables researchers to make informed decisions when constructing predictive models for anti-cancer agents. This review provides a systematic comparison of these methodologies, focusing on their theoretical foundations, practical implementation, and performance in predicting ADMET properties relevant to cancer therapeutics.
Theoretical Foundations and Key Concepts
Classical QSAR Approaches
Classical QSAR methodologies establish mathematical relationships between molecular descriptors and biological activity using statistical regression techniques. These approaches treat molecules as topological entities represented by numerical descriptors that encode structural and physicochemical properties without explicit three-dimensional structural information [94]. Multiple Linear Regression (MLR), Partial Least Squares (PLS), and Principal Component Regression (PCR) serve as the primary statistical engines for model development in classical QSAR [28]. These methods are valued for their interpretability, computational efficiency, and established validation frameworks, making them suitable for preliminary screening and mechanism elucidation.
Classical QSAR utilizes several categories of molecular descriptors. Constitutional descriptors capture basic molecular properties such as molecular weight and atom counts. Topological descriptors, including the Balaban Index and Wiener Index, encode molecular connectivity patterns. Physicochemical descriptors represent properties like lipophilicity (LogP) and aqueous solubility (LogS), while quantum chemical descriptors such as HOMO-LUMO energies and dipole moments describe electronic characteristics [95] [8]. The strength of classical QSAR lies in its ability to identify key molecular features influencing biological activity through transparent mathematical relationships, though it may overlook critical spatial aspects of molecular interactions.
3D-QSAR Methodologies
Three-dimensional QSAR extends the QSAR paradigm by incorporating spatial molecular features, recognizing that biological interactions occur in three-dimensional space. 3D-QSAR techniques quantitatively correlate biological activity with fields representing steric bulk, electrostatic potential, and other interaction energies distributed around molecules [94]. This approach requires molecules to be aligned in three-dimensional space according to their putative bioactive conformations, creating a common reference frame for comparative analysis.
The primary 3D-QSAR techniques include Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA). CoMFA calculates steric (Lennard-Jones) and electrostatic (Coulombic) interaction energies between a probe atom and aligned molecules at regularly spaced grid points [6] [94]. CoMSIA extends this concept by employing Gaussian-type functions to evaluate similarity indices for steric, electrostatic, hydrophobic, and hydrogen-bonding fields, resulting in smoother potential maps that are less sensitive to molecular alignment [14] [12]. The spatial contour maps generated by these methods provide visual guidance for molecular modifications, indicating regions where specific structural changes may enhance or diminish biological activity.
Pure Machine Learning Approaches
Pure machine learning approaches represent the most recent evolution in predictive modeling for drug discovery. These methods leverage algorithms that can automatically learn complex, non-linear relationships between molecular representations and biological activities without relying on pre-defined molecular descriptors or alignment rules [51] [28]. Machine learning models excel at identifying subtle patterns in high-dimensional data, making them particularly suited for heterogeneous chemical datasets and complex ADMET endpoints.
Supervised learning algorithms commonly applied in ADMET prediction include Random Forests (RF), Support Vector Machines (SVM), k-Nearest Neighbors (kNN), and Deep Neural Networks (DNN) [51] [93]. These algorithms can operate on various molecular representations, including traditional molecular descriptors, extended connectivity fingerprints (ECFPs), functional-class fingerprints (FCFPs), and learned representations from molecular graphs or SMILES strings [28] [93]. The "deep descriptors" generated by graph neural networks and other deep learning architectures capture hierarchical chemical features without manual engineering, potentially uncovering novel structure-activity relationships not apparent through traditional approaches [28].
Methodological Comparison and Performance Analysis
Descriptive Capabilities and Molecular Representation
The three modeling approaches differ fundamentally in how they represent molecular structures and their associated properties, directly influencing their descriptive capabilities and appropriate application domains.
Classical QSAR utilizes global molecular descriptors that provide comprehensive overviews of molecular properties but lack spatial resolution. These include constitutional descriptors (molecular weight, atom counts), topological indices (Balaban J, Wiener index), physicochemical properties (LogP, LogS), and quantum chemical parameters (HOMO-LUMO energies, electronegativity) [95] [8]. While excellent for capturing overall trends and identifying key molecular features influencing activity, these descriptors cannot represent spatial variations in molecular interaction potential.
3D-QSAR employs field-based descriptors that map interaction energies around molecules, providing high-resolution spatial information about steric, electrostatic, and other molecular fields [94]. The CoMFA approach uses a lattice of grid points surrounding aligned molecules to calculate steric (van der Waals) and electrostatic (Coulombic) interaction energies with a probe atom [6] [12]. CoMSIA extends this concept using Gaussian-type functions to compute similarity indices for multiple fields including steric, electrostatic, hydrophobic, hydrogen bond donor, and hydrogen bond acceptor fields, producing smoother contour maps that are less sensitive to molecular alignment [14]. These field descriptors directly visualize regions where structural modifications may enhance activity, providing medicinal chemists with intuitive guidance for compound optimization.
Pure ML approaches utilize diverse molecular representations ranging from traditional descriptors to learned representations. These include fixed fingerprints (ECFPs, FCFPs) that encode molecular substructures, graph-based representations where atoms constitute nodes and bonds form edges, and SMILES-based representations that leverage natural language processing techniques [51] [28] [93]. Deep learning architectures can automatically generate optimized molecular representations ("deep descriptors") through multiple layers of non-linear transformations, potentially capturing relevant features without manual engineering [28]. This flexibility enables ML models to adapt their descriptive focus to specific prediction tasks, though at the cost of reduced interpretability.
Performance in ADMET Prediction
Comparative studies demonstrate significant performance differences among the three approaches, particularly for complex ADMET endpoints where multiple structural factors interact non-linearly.
In a comprehensive comparison study, machine learning methods (DNN and Random Forest) demonstrated superior predictive performance for TNBC inhibition compared to traditional QSAR methods (PLS and MLR), with DNN achieving prediction accuracy (r²) near 90% versus 65% for traditional methods [93]. This performance advantage was maintained even with smaller training sets, with DNN retaining an r² value of 0.84 with only 303 training compounds compared to near-zero predictive capability for MLR under the same conditions [93].
3D-QSAR models typically exhibit strong performance for activity prediction against specific biological targets when congeneric series and consistent binding modes are assumed. For instance, 3D-QSAR models developed for pteridinone derivatives as PLK1 inhibitors demonstrated excellent predictive capability with R²pred values of 0.683-0.767 [12]. Similarly, 3D-QSAR models for Aztreonam analogs as E. coli DNA gyrase B inhibitors achieved high predictability (Q² = 0.73-0.88) [14]. These results indicate that 3D-QSAR remains highly valuable for target-focused optimization campaigns where structural alignment is feasible.
For ADMET-specific endpoints, ML approaches have demonstrated particular strength in predicting complex properties such as solubility, permeability, metabolism, and toxicity, where multiple structural factors interact non-linearly [51]. The integration of ML with large, curated ADMET datasets has enabled unprecedented accuracy in these predictions, significantly outperforming some traditional QSAR models [51].
Table 1: Comparative Performance of QSAR Approaches in Predictive Modeling
| Approach | Typical R² Range | Best-suited ADMET Endpoints | Data Requirements | Interpretability |
|---|---|---|---|---|
| Classical QSAR | 0.65-0.85 [93] | Lipophilicity (LogP), solubility (LogS), plasma protein binding | 20-100 compounds [95] | High - Direct structure-property relationships |
| 3D-QSAR | 0.68-0.88 (Q²) [14] [12] | Transporter interactions, metabolic site prediction, toxicity mechanisms | 20-50 aligned compounds [12] | Medium - 3D contour maps guide modifications |
| Pure ML | 0.84-0.94 [93] | Complex toxicity endpoints, bioavailability, clearance | 100-10,000+ compounds [51] | Low to Medium - Model-dependent interpretation |
Operational Requirements and Implementation Complexity
The practical implementation of each approach involves distinct operational requirements, computational resources, and expertise.
Classical QSAR requires calculation of molecular descriptors using software such as Gaussian, ChemOffice, or DRAGON, followed by statistical analysis using tools like XLSTAT or specialized QSAR packages [95] [8]. The workflow is relatively straightforward, with model development focusing on descriptor selection and regression analysis. Validation follows established protocols including leave-one-out cross-validation, external test set validation, and applicability domain assessment [95].
3D-QSAR implementation demands more specialized expertise, particularly in molecular alignment and field calculation. The workflow includes: (1) acquisition of 3D molecular structures; (2) geometry optimization using molecular mechanics or quantum chemical methods; (3) molecular alignment based on a common scaffold or pharmacophore; (4) calculation of interaction fields; and (5) partial least-squares regression to correlate field values with biological activity [12] [94]. This process requires software such as SYBYL, Open3DQSAR, or similar platforms, with careful attention to alignment strategy as a critical success factor.
Pure ML approaches necessitate expertise in machine learning, feature engineering, and model validation. The implementation workflow includes: (1) data collection and curation; (2) molecular representation selection; (3) algorithm selection and hyperparameter optimization; (4) model training with cross-validation; and (5) rigorous evaluation using external test sets [51] [93]. This approach benefits from platforms like scikit-learn, TensorFlow, PyTorch, and specialized cheminformatics libraries. The computational resources required scale with model complexity, with deep learning approaches demanding significant processing power and memory for large datasets.
Experimental Protocols and Implementation Guidelines
Protocol for Classical QSAR Modeling
Objective: To develop a predictive QSAR model for anti-cancer activity using multiple linear regression.
Materials and Software:
- Chemical structures of compounds with experimental bioactivity (IC₅₀ values)
- Gaussian 09W or similar software for quantum chemical descriptor calculation [8]
- ChemOffice or DRAGON for topological and physicochemical descriptors [8]
- Statistical analysis software (XLSTAT, R, Python with scikit-learn)
Procedure:
- Data Preparation:
Descriptor Calculation:
- Optimize molecular geometries using molecular mechanics (MM2) or density functional theory (B3LYP/6-31G(d)) [95]
- Calculate constitutional descriptors (MW, NHA, NHD)
- Compute topological indices (Balaban J, Wiener index)
- Determine physicochemical properties (LogP, LogS, PSA)
- Derive quantum chemical descriptors (EHOMO, ELUMO, dipole moment, electronegativity) [8]
Model Development:
- Perform descriptor pre-selection using correlation analysis and principal component analysis (PCA)
- Apply multiple linear regression with stepwise variable selection
- Validate model using leave-one-out cross-validation
- Calculate statistical parameters: R², Q², F-value, and standard error of estimate [95]
Model Validation:
- Predict activity of external test set compounds
- Calculate predictive R² (R²pred) for test set
- Perform Y-randomization to confirm model robustness
- Define applicability domain using Williams plot [95]
Troubleshooting Tips:
- High multicollinearity between descriptors: Apply variance inflation factor (VIF) analysis and remove descriptors with VIF >5
- Overfitting: Use cross-validated R² (Q²) rather than conventional R² for model selection
- Poor test set prediction: Verify applicability domain and consider non-linear methods
Protocol for 3D-QSAR Modeling
Objective: To develop a CoMSIA model for predicting anti-cancer activity and visualizing molecular fields.
Materials and Software:
- Structurally aligned molecules with experimental bioactivity
- Molecular modeling software (SYBYL, Open3DQSAR, or similar)
- Computational resources for geometry optimization
Procedure:
- Molecular Alignment:
- Generate 3D structures from 2D representations using conformational analysis
- Identify common scaffold or maximum common substructure (MCS)
- Perform rigid body alignment using distill alignment in SYBYL-X [12]
- Verify alignment quality through visual inspection
Field Calculation:
- Create a 3D grid with 1-2Å spacing extending 4Å beyond aligned molecules
- Calculate steric field using Lennard-Jones potential with sp³ carbon probe
- Compute electrostatic field using Coulombic potential with +1 charge probe
- Additional CoMSIA fields: hydrophobic, hydrogen bond donor, hydrogen bond acceptor [12]
- Set column filtering to 2.0 kcal/mol to reduce noise
Model Construction:
- Perform Partial Least Squares (PLS) regression with leave-one-out cross-validation
- Determine optimal number of components using cross-validated correlation coefficient (Q²)
- Evaluate model statistics: conventional R², standard error of estimate, F-value [12]
- Generate contour maps by interpolating PLS coefficients back to original grid
Model Application:
- Predict activity of new compounds after alignment to the same reference frame
- Use contour maps to guide molecular modifications
- Synthesize and test proposed analogs to validate predictions [94]
Troubleshooting Tips:
- Poor alignment: Consider alternative alignment rules or pharmacophore-based alignment
- Low Q² value: Adjust grid spacing or explore different field combinations
- Overfitting: Reduce number of PLS components or increase column filtering
Protocol for Pure Machine Learning Modeling
Objective: To develop a deep neural network model for ADMET property prediction.
Materials and Software:
- Curated dataset of compounds with experimental ADMET data
- Python with scikit-learn, TensorFlow/PyTorch, and cheminformatics libraries (RDKit)
- Computational resources (GPU recommended for deep learning)
Procedure:
- Data Preprocessing:
- Collect and curate ADMET data from public databases (ChEMBL, PubChem) or proprietary sources
- Standardize molecular structures (tautomer normalization, neutralization)
- Handle missing data through imputation or removal
- Address data imbalance using oversampling or weighted loss functions [51]
Feature Engineering:
- Generate molecular representations: ECFP, FCFP, molecular graphs, or SMILES strings
- Apply feature selection methods (filter, wrapper, or embedded approaches) [51]
- Split data into training (70%), validation (15%), and test (15%) sets
Model Training:
- For Random Forest: Optimize number of trees, maximum depth, and minimum samples split
- For Deep Neural Networks: Design architecture (number of layers, neurons per layer), select activation functions, apply regularization (dropout, L2) [93]
- Perform hyperparameter optimization using grid search or Bayesian optimization
- Monitor training and validation loss to detect overfitting
Model Evaluation:
- Calculate performance metrics on independent test set: R², RMSE, MAE for regression; accuracy, precision, recall for classification
- Analyze applicability domain using leverage approaches or distance-based methods
- Employ model interpretation techniques (SHAP, LIME) to identify important features [28]
Troubleshooting Tips:
- Overfitting: Increase regularization, use early stopping, or augment training data
- Poor performance: Try alternative molecular representations or algorithm selection
- Computational limitations: Reduce feature dimensionality or use distributed computing
Research Reagent Solutions
Table 2: Essential Software and Tools for QSAR Modeling
| Category | Tool/Software | Primary Function | Application Notes |
|---|---|---|---|
| Descriptor Calculation | Gaussian 09W [8] | Quantum chemical descriptor computation | Uses DFT methods (B3LYP) with basis sets (6-31G) for electronic properties |
| DRAGON [28] | Calculation of 5000+ molecular descriptors | Comprehensive descriptor coverage including 2D/3D parameters | |
| RDKit [28] [94] | Open-source cheminformatics platform | Calculates topological descriptors, fingerprints, and 3D conformations | |
| 3D-QSAR Implementation | SYBYL-X [12] | Molecular alignment and field calculation | Industry standard for CoMFA/CoMSIA with robust statistical analysis |
| Open3DQSAR | Open-source 3D-QSAR implementation | Alternative to commercial packages with similar functionality | |
| Machine Learning Platforms | scikit-learn [28] | Traditional ML algorithms | Implements RF, SVM, kNN with comprehensive model evaluation tools |
| TensorFlow/PyTorch [28] | Deep learning frameworks | Flexible architecture design for custom neural networks | |
| DeepChem | Specialized ML for drug discovery | Includes graph convolutional networks for molecular data | |
| Validation and Analysis | QSARINS [28] | QSAR model development and validation | Implements robust validation methods and applicability domain assessment |
| KNIME [28] | Visual workflow platform for data analytics | Integrates cheminformatics nodes with machine learning capabilities |
Integrated Workflows and Decision Framework
Hybrid Approaches for Enhanced Prediction
The integration of multiple computational approaches has emerged as a powerful strategy for addressing the complex challenge of ADMET prediction in cancer drug design. Combined workflows leverage the complementary strengths of different methodologies, often yielding superior predictions compared to individual approaches [28]. Successful implementations include 3D-QSAR guided by molecular docking, classical QSAR informed by machine learning feature selection, and ML models enriched with quantum chemical descriptors [6] [28].
For instance, integrated studies have demonstrated the value of combining 3D-QSAR with molecular docking and dynamics simulations to identify anti-breast cancer agents. In these workflows, 3D-QSAR identifies key molecular features influencing activity, molecular docking predicts binding modes to specific targets like aromatase or Tubulin, and molecular dynamics simulations validate binding stability over time [6] [8]. This multi-technique approach provides both predictive power and mechanistic insight, facilitating more informed decisions in compound optimization.
Similarly, the incorporation of ML-based ADMET prediction early in the drug design process has shown significant value in reducing late-stage attrition. By screening virtual compound libraries against ADMET endpoints before synthesis, researchers can prioritize candidates with favorable pharmacokinetic and safety profiles [51]. This proactive approach is particularly valuable in cancer drug discovery, where therapeutic windows are often narrow and toxicity concerns are paramount.
Selection Framework for Method Choice
The optimal choice of modeling approach depends on multiple factors including available data, computational resources, project timeline, and specific research questions. The following decision framework provides guidance for selecting appropriate methodologies:
For small congeneric series (<50 compounds) with assumed common binding mode: Implement 3D-QSAR to gain spatial understanding of structure-activity relationships and guide targeted molecular modifications [12] [94].
For medium-sized datasets (50-200 compounds) with diverse structures: Apply classical QSAR with carefully selected descriptors to identify key molecular features driving activity and ADMET properties [95] [8].
For large datasets (>200 compounds) or complex ADMET endpoints: Employ machine learning approaches to capture non-linear relationships and complex feature interactions [51] [93].
For projects requiring maximal interpretability: Utilize classical QSAR or 3D-QSAR to maintain transparent structure-property relationships [95] [94].
For projects prioritizing predictive accuracy over interpretability: Implement ensemble ML methods or deep learning to maximize predictive performance [93].
For resource-intensive optimization campaigns: Adopt integrated workflows that combine multiple approaches to leverage their complementary strengths [6] [28].
The implementation of this decision framework should be iterative, with periodic reassessment of model performance and refinement of approach based on newly generated experimental data. This adaptive strategy ensures continuous improvement of predictive capabilities throughout the drug discovery process.
Model Selection Workflow - This diagram outlines a systematic approach for selecting the optimal QSAR method based on dataset characteristics and project requirements.
The comparative analysis of classical QSAR, 3D-QSAR, and pure machine learning approaches reveals a complex landscape of complementary methodologies for ADMET prediction in cancer drug design. Each approach offers distinct advantages: classical QSAR provides interpretability and efficiency for congeneric series; 3D-QSAR delivers spatial guidance for molecular optimization; and machine learning enables high-accuracy predictions for complex endpoints with sufficient data. The emerging paradigm of integrated workflows, leveraging the complementary strengths of multiple approaches, represents the most promising direction for advancing predictive capabilities in cancer drug discovery.
As the field continues to evolve, several trends are likely to shape future developments. These include increased integration of multi-omics data into predictive models, advancement of explainable AI to address the "black box" limitation of complex ML models, growth of federated learning approaches to leverage distributed data sources while maintaining privacy, and development of real-time predictive systems that guide experimental design iteratively. By understanding the comparative strengths and implementation requirements of each approach, researchers can make informed decisions that accelerate the discovery of effective and safe cancer therapeutics with optimal ADMET profiles.
The integration of ADMET property prediction into 3D-QSAR cancer drug design represents a transformative approach in oncology research, significantly enhancing the efficiency of drug discovery pipelines. This application note demonstrates through detailed case studies how the synergistic application of computational modeling and experimental validation has successfully identified and advanced promising cancer therapeutic candidates. We present validated protocols for employing 3D-QSAR in conjunction with ADMET prediction to prioritize compounds with optimal efficacy and safety profiles, providing researchers with a structured framework for implementing these methodologies in preclinical development.
Cancer drug discovery has traditionally been characterized by high attrition rates, with approximately 90% of oncology candidates failing during clinical development [3]. The integration of computational approaches, particularly three-dimensional quantitative structure-activity relationship (3D-QSAR) modeling and absorption, distribution, metabolism, excretion, and toxicity (ADMET) prediction, is transforming this landscape by enabling more informed candidate selection early in the discovery process [96].
These computational methodologies allow researchers to rapidly evaluate chemical entities in silico, predicting both biological activity and pharmacokinetic properties before committing to costly synthesis and biological testing [97]. The paradigm of prospective validation—where computational predictions are subsequently confirmed through experimental testing—has emerged as a critical validation standard for these approaches [98]. This application note presents case studies and protocols that exemplify this paradigm in cancer drug discovery, focusing specifically on the intersection of 3D-QSAR and ADMET prediction.
Case Study: Flavone Analogs as Tankyrase Inhibitors
Background and Rationale
Tankyrase (TNKS), a member of the poly(ADP-ribose) polymerase family, has been identified as a promising therapeutic target across multiple cancer types, including colorectal, breast, and ovarian cancers [97]. TNKS inhibition suppresses Wnt/β-catenin signaling—a pathway frequently dysregulated in cancer—by stabilizing axin proteins, thereby promoting the degradation of β-catenin and inhibiting cancer cell proliferation [97]. Flavone scaffolds were identified as potential TNKS inhibitors through high-throughput screening of natural products, prompting a comprehensive drug optimization campaign.
Computational Workflow and Prediction
A 3D-QSAR model was developed using field-based techniques with a training set of 87 flavone derivatives with known TNKS inhibitory activity (IC₅₀) [97]. The model demonstrated robust predictive capability with descriptive (r² = 0.89) and predictive (q² = 0.67) parameters. Subsequent virtual screening of ~8,000 flavonoid compounds identified 1,480 candidates with predicted IC₅₀ values below 5 μM.
These candidates underwent molecular docking against the TNKS receptor to evaluate binding modes and interactions. The top 200 compounds by docking score were progressed to in silico ADMET risk assessment, which identified 25 candidates with favorable toxicity and pharmacokinetic profiles [97]. Further evaluation of drug-likeness, synthetic accessibility, and PAINS filters yielded eight lead compounds with promising characteristics.
Table 1: Predicted Activity and Properties of Top Flavone-Derived TNKS Inhibitors
| Compound ID | Predicted IC₅₀ (μM) | Docking Score (kcal/mol) | ADMET Risk | BBB Penetration |
|---|---|---|---|---|
| F2 | 1.59 | -12.3 | None | Yes |
| F3 | 1.00 | -13.1 | None | Yes |
| F8 | 0.62 | -14.2 | None | Yes |
| F11 | 0.79 | -13.5 | None | Yes |
| F13 | 3.98 | -11.8 | None | Yes |
| F20 | 0.79 | -13.6 | None | Yes |
| F21 | 0.63 | -14.1 | None | Yes |
| F25 | 0.64 | -13.9 | None | Yes |
Experimental Validation
The eight lead compounds underwent comprehensive biological validation in preclinical models. In vitro assays confirmed potent TNKS inhibition, with IC₅₀ values closely correlating with computational predictions (R² = 0.85 between predicted and experimental values) [97]. Compound F8 demonstrated particularly promising activity, with sub-micromolar potency and excellent selectivity over other PARP family members.
In vivo efficacy studies in colorectal cancer xenograft models revealed significant tumor growth inhibition (67-72% reduction versus control) for the top four compounds at 50 mg/kg dosing [97]. Pharmacokinetic profiling confirmed favorable oral bioavailability (52-68%) and half-life (4.2-6.8 hours) consistent with ADMET predictions. The successful prospective validation of these flavone analogs highlights the power of integrated computational/experimental approaches in cancer drug discovery.
Case Study: AI-Driven Target Identification and Validation
Background and Computational Approach
While not exclusively a 3D-QSAR example, this case study illustrates the expanding role of artificial intelligence in cancer drug discovery, particularly in target identification—a crucial prerequisite for structure-based drug design. Researchers applied AI-powered software to analyze transcriptomic data from adenoid cystic carcinoma, a rare salivary gland cancer with limited treatment options [99].
The AI platform integrated multi-omics data with information on known biological pathways to identify key vulnerabilities in ACC. Through modeling complex interactions between genes, proteins, and RNAs, the system prioritized potential therapeutic targets based on their predicted role in cancer progression and druggability [99].
Prospective Predictions and Validation
The AI platform identified PRMT5, a protein arginine methyltransferase, as a promising therapeutic target in ACC. The prediction was based on PRMT5's overexpression in ACC samples and its computationally inferred role in regulating key drivers of cancer progression [99].
Experimental validation confirmed that PRMT5 inhibition suppressed tumor growth in multiple preclinical ACC models, including patient-derived xenografts [99]. Mechanistic studies revealed that PRMT5 inhibition reduced the expression of oncogenic drivers specifically in ACC, providing strong rationale for clinical development of PRMT5 inhibitors for this indication. This case demonstrates how AI-driven target identification can expand the target landscape for cancer therapy, particularly for rare cancers with limited treatment options.
Integrated Protocol: 3D-QSAR with ADMET Prediction
Computational Modeling Phase
Step 1: Dataset Curation and Preparation
- Select 25-50 compounds with consistent experimental activity data (e.g., IC₅₀, Ki)
- Divide compounds into training (70-80%) and test sets (20-30%) using rational selection methods
- Generate 3D structures using molecular mechanics force fields (e.g., Tripos, MMFF94)
- Optimize geometries using semi-empirical or DFT methods with appropriate basis sets
Step 2: Molecular Alignment and Field Calculation
- Align molecules using common substructure or pharmacophore-based methods
- Calculate steric and electrostatic fields using standard probes (e.g., sp³ carbon +1 charge)
- For CoMSIA, additionally calculate hydrophobic, hydrogen bond donor, and acceptor fields
Step 3: 3D-QSAR Model Development
- Perform Partial Least Squares regression with cross-validation (leave-one-out or leave-group-out)
- Validate model robustness using Y-randomization and external test set prediction
- Accept models with q² > 0.5 and R² > 0.8 for further analysis [98]
Step 4: ADMET Property Prediction
- Calculate key molecular descriptors (logP, polar surface area, molecular weight, etc.)
- Predict absorption (Caco-2, HIA), distribution (BBB penetration), metabolism (CYP inhibition)
- Evaluate toxicity endpoints (Ames test, hepatotoxicity, hERG inhibition)
- Apply drug-likeness filters (Lipinski, Veber, Ghose rules) [98]
Step 5: Virtual Screening and Hit Selection
- Apply 3D-QSAR model to screen virtual compound libraries
- Prioritize compounds with high predicted activity and favorable ADMET profiles
- Perform molecular docking to assess binding modes and interactions
Experimental Validation Phase
Step 6: Compound Acquisition/Synthesis
- Procure or synthesize top-ranked virtual hits (15-25 compounds)
- Confirm compound identity and purity (>95%) using analytical methods
Step 7: In Vitro Biological Assessment
- Determine experimental IC₅₀ values against target protein using biochemical assays
- Evaluate selectivity against related targets or protein family members
- Assess cellular potency in relevant cancer cell lines
Step 8: ADMET Experimental Profiling
- Measure metabolic stability using liver microsomes or hepatocytes
- Evaluate membrane permeability (Caco-2, PAMPA)
- Assess CYP inhibition potential
- Determine plasma protein binding
Step 9: Lead Optimization and In Vivo Studies
- Refine structures based on experimental results and computational analysis
- Evaluate efficacy in relevant animal models (e.g., xenograft, PDX)
- Conduct preliminary toxicology assessment
Diagram 1: Integrated 3D-QSAR and ADMET Prediction Workflow. This protocol outlines the comprehensive computational and experimental steps for prospective validation of cancer drug candidates.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Research Reagents and Computational Tools for 3D-QSAR and ADMET Studies
| Category | Tool/Reagent | Specific Application | Function/Purpose |
|---|---|---|---|
| Software Platforms | SYBYL-X | 3D-QSAR Model Development | Molecular modeling, CoMFA/CoMSIA analysis, and alignment |
| Forge | Field-based QSAR | Field point calculation and 3D-QSAR using XED force field | |
| SwissADMET | ADMET Prediction | In silico prediction of pharmacokinetics and toxicity | |
| StarDrop | ADMET QSAR | Integrated ADMET property prediction and optimization | |
| Experimental Assays | Liver Microsomes | Metabolic Stability | Assessment of phase I metabolic clearance |
| Caco-2 Cell Line | Permeability | Prediction of intestinal absorption and BBB penetration | |
| CYP450 Assays | Metabolism | Evaluation of cytochrome P450 inhibition potential | |
| MTT/Trypan Blue | Cytotoxicity | Assessment of compound toxicity and cell viability | |
| Data Resources | PubChem | Compound Database | Source of chemical structures and bioactivity data |
| PDB (Protein Data Bank) | Structural Biology | Source of 3D protein structures for docking studies | |
| ChEMBL | Bioactivity Database | Curated bioactivity data for model training and validation |
Discussion and Future Perspectives
The case studies presented herein demonstrate the powerful synergy between computational prediction and experimental validation in cancer drug discovery. The flavone-TNKS inhibitor example illustrates how integrated computational workflows can successfully identify and optimize novel therapeutic candidates with a high probability of success in subsequent experimental testing [97]. Similarly, the AI-driven target discovery case highlights emerging approaches that can expand the target landscape for cancer therapy.
Critical to the success of these approaches is the rigorous application of prospective validation standards, where computational predictions are tested against experimental results in a blinded manner. This validation paradigm provides the most compelling evidence for the utility of computational methods in drug discovery and builds confidence in their application to prioritize compounds for resource-intensive experimental evaluation.
Future developments in this field will likely focus on several key areas:
- Multimodal AI approaches that integrate 3D-QSAR with diverse data types (genomics, transcriptomics, clinical data) [100]
- Federated learning to train models across institutions while preserving data privacy [3]
- Quantum computing applications to accelerate molecular simulations and property predictions [3]
- Advanced organoid and PDX models for more clinically predictive experimental validation [4]
As these technologies mature, the integration of computational prediction and experimental validation will become increasingly central to cancer drug discovery, potentially reducing the time and cost of bringing new therapies to patients while improving success rates in clinical development.
The prospective validation case studies presented in this application note provide compelling evidence for the value of integrating 3D-QSAR modeling and ADMET prediction in cancer drug discovery. The structured protocols and toolkit presented offer researchers a practical framework for implementing these approaches in their own drug discovery programs. As computational methods continue to evolve and integrate with experimental technologies, they hold the promise of significantly accelerating the development of novel cancer therapeutics, ultimately bringing more effective treatments to patients faster and more efficiently.
In modern oncology research, the high failure rate of drug candidates, often attributed to poor pharmacokinetic and safety profiles, has made the in-silico prediction of Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties a cornerstone of efficient drug discovery pipelines [1]. This is particularly crucial in cancer therapy, where the therapeutic window is often narrow, and toxicity concerns are paramount [101]. The integration of ADMET prediction with established computational methods like 3D-QSAR provides a powerful framework for prioritizing synthesized compounds and guiding the design of novel chemical entities with optimized efficacy and safety profiles. The application of Artificial Intelligence (AI), especially machine learning (ML) and deep learning (DL), has revolutionized this field by enabling high-accuracy predictions from chemical structure alone, thereby accelerating the identification of promising anti-cancer leads [102] [29].
Several robust computational platforms have been developed to provide comprehensive ADMET profiling. These tools leverage large, curated datasets and advanced algorithms to offer scientists user-friendly interfaces for critical property assessment.
Table 1: Key Features of Prominent ADMET Prediction Platforms
| Platform Name | Key Features | Number of Properties | Underlying AI Technology | Unique Strengths |
|---|---|---|---|---|
| ADMETlab 2.0 [103] | Evaluation, Screening, Toxicophore Rules | 88 properties (17 Physicochemical, 13 Medicinal Chemistry, 23 ADME, 27 Toxicity) | Multi-task Graph Attention Framework | Batch screening for large datasets; 751 toxicophore substructure rules |
| ADMET-AI [104] | Web Server & Python Package, DrugBank Context | 41 ADMET endpoints from TDC | Chemprop-RDKit (Graph Neural Network) | Highest average rank on TDC Leaderboard; Fastest web server; Local installation option |
| Interpretation-ADMElab [105] | Druglikeness Analysis, Systematic Assessment | 30+ ADMET endpoints | Random Forest, SVM, and other QSAR models | Integrates multiple druglikeness rules (Lipinski, Ghose, etc.); Provides optimization suggestions |
These platforms exemplify the trend towards more comprehensive and accurate predictive modeling. ADMETlab 2.0 stands out for its extensive profile coverage and batch screening capability, which is suitable for evaluating large virtual libraries generated in cancer drug discovery campaigns [103]. ADMET-AI, on the other hand, demonstrates state-of-the-art predictive performance on benchmark datasets and offers a unique feature of contextualizing predictions against a reference set of approved drugs from DrugBank, which is invaluable for interpreting results within a known chemical space [104].
Practical Application Notes and Protocols
Protocol 1: Virtual Screening of a Compound Library with ADMETlab 2.0
Application Note: This protocol describes the use of ADMETlab 2.0 for the high-throughput screening of a virtual library of putative tubulin inhibitors for breast cancer therapy, ensuring the selection of candidates with desirable ADMET profiles before synthesis.
Materials & Reagents:
- Input Data: A library of compound structures in SMILES or SDF format.
- Software: ADMETlab 2.0 web server (https://admetmesh.scbdd.com/).
- Selection Criteria: Pre-defined optimal ranges for key properties (e.g., LogP, solubility, hERG inhibition).
Procedure:
- Data Preparation: Prepare a list of SMILES strings or an SDF file containing the structures of the compounds to be screened. For instance, this could be a series of novel 1,2,4-triazine-3(2H)-one derivatives designed as tubulin inhibitors [101].
- Submission: Navigate to the "ADMET Screening" module of ADMETlab 2.0. Upload the file or paste the SMILES strings into the input field.
- Job Configuration: Initiate the prediction job with default parameters. The platform will process the molecules using its multi-task graph attention models [103].
- Result Analysis: Upon completion, download the comprehensive results. The platform provides results visually represented with colored dots (green/excellent, yellow/medium, red/poor) for rapid assessment [103].
- Hit Selection: Filter compounds based on pre-defined criteria. For oral anti-cancer drugs, key properties to consider include:
Protocol 2: Contextualized Prediction for a Lead Compound using ADMET-AI
Application Note: This protocol outlines the use of ADMET-AI to evaluate a single, optimized lead compound (e.g., a triazine derivative with a high docking score for tubulin) and interpret its ADMET profile in the context of approved anti-cancer drugs.
Materials & Reagents:
- Input Data: SMILES string of the lead compound.
- Software: ADMET-AI web server (admet.ai.greenstonebio.com).
- Reference Set: Approved drugs filtered by Anatomical Therapeutic Chemical (ATC) code, e.g., "L01" for antineoplastic agents.
Procedure:
- Compound Input: Access the ADMET-AI web interface. Input the SMILES string of the lead compound, either by typing, drawing, or uploading a file.
- Reference Set Selection: In the reference set options, select the ATC code "L01" to compare the lead compound's predicted properties specifically against approved anti-cancer drugs. This accounts for the different ADMET tolerances in this class (e.g., higher acceptable toxicity) [104].
- Prediction Execution: Run the prediction. The platform uses an ensemble of graph neural network models to generate predictions for all 41 endpoints [104].
- Interpretation of Results: Review the results dashboard, which includes:
- A radar plot summarizing key druglikeness components like hERG, BBB, solubility, and bioavailability.
- Detailed tables of all predictions, each paired with a percentile rank indicating how the compound compares to the selected DrugBank reference set. A high percentile in hERG inhibition, for instance, is a critical risk signal [104].
- Decision Making: Use the percentile data to make an informed go/no-go decision. A profile that falls within the range of existing oncology drugs provides greater confidence for further development.
Protocol 3: Integrating QSAR and ADMET Predictions for Molecular Optimization
Application Note: This protocol combines QSAR modeling for target activity (e.g., anti-proliferative activity on MCF-7 cells) with ADMET profiling to guide the structural optimization of a lead series in breast cancer drug discovery.
Materials & Reagents:
- Data Set: A congeneric series of compounds with known biological activity (e.g., pIC50 values).
- Software: QSAR modeling software (e.g., MATLAB, Python with scikit-learn) and an ADMET platform (e.g., ADMETlab 2.0).
- Descriptors: Quantum chemical (e.g., HOMO/LUMO energies) and topological descriptors (e.g., LogP, PSA) [101].
Procedure:
- QSAR Model Development:
- Calculate molecular descriptors (e.g., absolute electronegativity, water solubility (LogS), HOMO/LUMO energies) for the compound set [101].
- Construct a multiple linear regression (MLR) or ML-based QSAR model linking the descriptors to the biological activity (pIC50).
- Validate the model using statistical measures (e.g., R², Q²). A study on triazine derivatives achieved a predictive R² of 0.849, identifying key descriptors like absolute electronegativity and LogS [101].
- ADMET Profiling: Subject the same compound set to ADMET prediction using a platform like ADMETlab 2.0 to obtain properties such as Caco-2 permeability, CYP450 inhibition, and hERG toxicity [103] [102].
- Multi-Parameter Optimization: Analyze the combined QSAR and ADMET data to identify structural features that enhance both potency and drug-like properties. For example, the QSAR model might indicate that a specific substituent increases potency, while the ADMET profile reveals it also improves solubility without increasing hERG risk.
- Design New Analogs: Propose new analogs that incorporate the favorable structural features identified in the integrated analysis. The "Matched Molecular Pair Analysis" can suggest specific chemical transformations to improve particular properties, such as Caco-2 permeability [106].
Figure 1: Integrated computational workflow for anti-cancer drug design, combining QSAR modeling for efficacy and ADMET screening for safety and drug-likeness.
Table 2: Key Computational Reagents for ADMET Prediction in Cancer Research
| Resource Name | Type | Function in Research | Application Context |
|---|---|---|---|
| Therapeutics Data Commons (TDC) [104] | Benchmark Datasets | Provides standardized ADMET datasets for training and benchmarking predictive models. | Serves as the foundation for platforms like ADMET-AI; used for independent model validation. |
| RDKit [104] [106] | Cheminformatics Library | Calculates molecular descriptors and fingerprints; handles molecular standardization and graph representation. | Used internally by ADMET-AI and other platforms; can be used for custom descriptor calculation in QSAR. |
| DrugBank Approved Drug Set [104] | Reference Dataset | A curated set of ~2,579 approved drugs used to contextualize ADMET predictions via percentile scores. | In ADMET-AI, allows comparison of a novel compound's predicted properties to successful drugs. |
| Caco-2 Permeability Dataset [106] | Experimental Training Data | A large, curated dataset of measured Caco-2 cell permeability values for building robust prediction models. | Used to train and validate ML models (e.g., XGBoost, DMPNN) for predicting human intestinal absorption. |
| Tubulin-Colchicine Crystal Structure [101] | Protein Target Structure | Provides a 3D structure for molecular docking simulations to assess binding affinity and mechanism. | Used in the design and evaluation of novel tubulin inhibitors for breast cancer therapy. |
The integration of advanced, AI-powered platforms like ADMETlab 2.0 and ADMET-AI into the 3D-QSAR cancer drug design workflow represents a paradigm shift in oncological pharmacology. These tools provide researchers with an unprecedented ability to evaluate critical pharmacokinetic and toxicity endpoints early in the discovery process, de-risking projects and focusing synthetic efforts on the most promising chemical series. By following the detailed application protocols outlined above—ranging from high-throughput virtual screening to contextualized lead optimization—scientists can leverage these platforms to systematically bridge the gap between computational design and viable pre-clinical candidates, ultimately accelerating the journey toward new, effective, and safer cancer therapies.
The integration of computational models like Quantitative Structure-Activity Relationship (QSAR) and Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) prediction into cancer drug design represents a transformative shift in pharmaceutical research. These models significantly accelerate the preclinical stage of drug discovery by reducing costs, minimizing attrition rates, and expediting the identification of viable candidates [28]. However, the transition from research tools to regulatory-accepted evidence requires rigorous validation and standardization. This is particularly crucial in 3D-QSAR cancer drug design, where predicting ADMET properties can determine a compound's therapeutic potential or failure. The reliability of these computational predictions forms the foundation for their acceptance by regulatory bodies, establishing a critical bridge between in silico innovation and clinical application.
Foundational Principles for Regulatory Acceptance
Regulatory acceptance of computational models is predicated on several core principles that ensure their reliability and relevance for decision-making.
Demonstrable Predictive Accuracy: Models must show robust correlation between predicted and experimentally observed biological activities. This is typically quantified using statistical metrics such as the coefficient of determination (R²) for model fit and cross-validated R² (Q²) for predictive performance [8] [107]. For instance, a QSAR model for 1,2,4-triazine-3(2H)-one derivatives as tubulin inhibitors achieved a predictive accuracy (R²) of 0.849, demonstrating a high level of explanatory power [8].
Model Interpretability and Transparency: The "black-box" nature of some advanced algorithms, particularly complex machine learning models, poses a significant challenge for regulatory review. Models must provide mechanistic insights into the structural and physicochemical properties governing biological activity and ADMET outcomes. The use of interpretable molecular descriptors—such as absolute electronegativity (χ), water solubility (LogS), and steric/electrostatic fields in 3D-QSAR—is essential for building trust and understanding a model's decision-making process [8] [28].
Rigorous Validation Protocols: A multi-tiered validation strategy is non-negotiable.
- Internal Validation: Assesses model stability using techniques like cross-validation (e.g., Q²).
- External Validation: Uses a completely independent test set of compounds to evaluate the model's predictive power on unseen data, a critical step for regulatory confidence [6] [14] [107].
- Y-Randomization: Confirms that the model's performance is not based on chance correlation [107].
Defined Applicability Domain (AD): A model is only reliable for compounds within its chemical and response space. The Applicability Domain defines the structural and property boundaries for which the model's predictions can be trusted. This is crucial for identifying potential outliers and preventing the model's misuse on chemistries for which it was not designed [107].
Standards and Best Practices for Model Development
Data Curation and Preparation
The foundation of any reliable computational model is high-quality, well-curated data. This initial phase is critical, as the model's predictive capability is directly dependent on the integrity of the input data.
Table 1: Essential Data Curation and Preparation Steps
| Step | Description | Tools/Examples |
|---|---|---|
| Data Sourcing | Use of reliable, peer-reviewed biological data (e.g., IC₅₀, pIC₅₀) from scientific literature [8] [107]. | Experimental journals, public databases (ChEMBL, PubChem). |
| Structure Standardization | Drawing 2D structures and converting them to optimized 3D conformers. | ChemDraw Professional [107], Spartan'14 [107]. |
| Descriptor Calculation | Generation of molecular descriptors encoding chemical, structural, and physicochemical properties. | PaDEL [107], DRAGON [28], RDKit [28], Gaussian (for quantum chemical descriptors) [8]. |
| Data Pre-treatment | Removal of duplicates, handling of tautomers/ionization, and treatment of unwanted or zero-value molecular properties [107] [13]. | BIOVIA Discovery Studio [13], QSARINS [107]. |
| Dataset Division | Splitting data into training (for model building) and test (for external validation) sets. | Kennard and Stone's algorithm [107] (e.g., 80:20 or 70:30 ratio). |
Model Building and Validation
Following data preparation, the focus shifts to constructing the model using robust statistical methods and rigorously evaluating its predictive performance.
Table 2: Model Building, Validation Techniques, and Standards
| Aspect | Recommended Techniques | Statistical Standards for Acceptance |
|---|---|---|
| Statistical Modeling | Multiple Linear Regression (MLR) [8] [107], Partial Least Squares (PLS) [28], Genetic Algorithm (GA) for variable selection [107]. | R²train > 0.6, Q² > 0.5, Low LOF (Leave-One-Out) value [107]. |
| Machine Learning | Support Vector Machines (SVM), Random Forests (RF), Artificial Neural Networks (ANN) [28] [23]. | Robustness to noisy data, handling of non-linear relationships. |
| Internal Validation | Cross-validation (e.g., Leave-One-Out, Leave-Many-Out). | Q² > 0.5 [107]. |
| External Validation | Prediction using a withheld test set. | R²pred > 0.5-0.6 [107], convergence of predicted and observed activities. |
| Domain of Applicability | Leverage-based approaches (Hat matrix) to define the chemical space [107]. | Leverage threshold (h*) = 3p/n, where p is descriptors, n is training compounds [107]. |
The following workflow diagrams the integrated computational strategies common in modern cancer drug discovery, illustrating how different validation techniques are incorporated.
Figure 1: The pathway to regulatory acceptance for computational models, highlighting key stages from data preparation to final submission.
ADMET and Pharmacokinetics Integration
The specific integration of ADMET prediction is a critical milestone on the path to regulatory acceptance, as it addresses key safety and efficacy concerns early in the drug development process.
Table 3: Key ADMET Properties and Their Predictive Descriptors in Cancer Drug Design
| ADMET Property | Relevance in Cancer Therapy | Common Molecular Descriptors |
|---|---|---|
| Aqueous Solubility (LogS) | Impacts drug formulation and bioavailability [8]. | LogS, Hydrogen Bond Donors/Acceptors, Polar Surface Area [8]. |
| Blood-Brain Barrier (BBB) Penetration | Critical for targeting brain metastases or avoiding CNS side effects [13]. | LogP, Molecular Weight, Polar Surface Area [28] [13]. |
| Hepatotoxicity | Predicts potential liver damage, a common cause of drug attrition [13]. | Structural alerts (e.g., reactive functional groups), CYP450 binding affinity [13]. |
| Plasma Protein Binding | Influences the volume of distribution and free drug concentration [13]. | Molecular charge, lipophilicity (LogP) [13]. |
| CYP450 Enzyme Inhibition | Indicates potential for drug-drug interactions [13]. | Molecular fingerprints, structural fragments [13]. |
The relationship between molecular properties, ADMET prediction, and overall candidate viability is a multi-faceted process, as shown below.
Figure 2: The central role of ADMET prediction in determining the fate of a potential drug candidate based on its molecular properties and QSAR model outputs.
Experimental Protocols for Model Validation
Protocol 1: Developing a Validated 3D-QSAR Model
This protocol outlines the steps for creating a 3D-QSAR model with a focus on meeting regulatory standards.
Step 1: Data Set Curation and Conformational Analysis
- Procedure: A series of compounds with experimentally determined biological activity (e.g., IC₅₀ against a cancer cell line like MCF-7) is compiled from peer-reviewed literature. The IC₅₀ values are converted to pIC₅₀ (-log IC₅₀) for modeling. 2D structures are drawn using software like ChemDraw Professional and saved in an SD file. These structures are then imported into a computational chemistry package (e.g., Spartan'14) and converted to 3D. The most stable conformer for each molecule is identified and geometry-optimized using Density Functional Theory (DFT) with a method like B3LYP and the 6-31G basis set [8] [107].
Step 2: Molecular Descriptor Calculation and Data Pretreatment
- Procedure: A wide range of molecular descriptors is calculated. This includes:
- Quantum chemical descriptors: HOMO/LUMO energies, dipole moment, absolute electronegativity (χ), absolute hardness (η) [8].
- Topological and physicochemical descriptors: Molecular weight, LogP, LogS, polar surface area, Balaban index [8] [107].
- 3D-field descriptors: For CoMFA (Comparative Molecular Field Analysis) and CoMSIA (Comparative Molecular Similarity Indices Analysis), steric, electrostatic, and hydrophobic fields are calculated around the aligned molecules [6] [14].
- Descriptors with zero variance or high correlation are removed. The dataset is then divided into a training set (~70-80%) for model development and a test set (~20-30%) for external validation using an algorithm like Kennard and Stone [107].
- Procedure: A wide range of molecular descriptors is calculated. This includes:
Step 3: Model Construction and Internal Validation
- Procedure: A statistical model is built using the training set. Multiple Linear Regression (MLR) with feature selection via Genetic Algorithm (GA) is a common and interpretable approach. The model's goodness-of-fit is assessed using R². Internal validation is performed via cross-validation (e.g., Leave-One-Out) to calculate Q², which should typically be >0.5 to be considered predictive [107].
Step 4: External Validation and Applicability Domain
- Procedure: The finalized model is used to predict the activity of the completely independent test set. The predictive R² (R²pred) is calculated; a value >0.5-0.6 is often considered indicative of a robust model [107]. The applicability domain is defined, for example, by calculating the leverage (h) for each compound to identify chemicals that are structural outliers and for which predictions may be unreliable [107].
Protocol 2: Integrated ADMET and Molecular Docking Validation
This protocol supplements the QSAR model with critical safety and binding mode analysis.
Step 1: ADMET Profiling
- Procedure: The designed compounds are subjected to in silico ADMET prediction using software like BIOVIA Discovery Studio [13]. Key properties are calculated, including:
- Human Intestinal Absorption (HIA)
- Blood-Brain Barrier (BBB) Penetration
- Aqueous Solubility (LogS)
- Plasma Protein Binding (PPB)
- Cytochrome P450 2D6 (CYP2D6) Inhibition
- Hepatotoxicity [13]
- Compounds with unfavorable ADMET profiles (e.g., predicted hepatotoxicity or poor absorption) are deprioritized or structurally modified.
- Procedure: The designed compounds are subjected to in silico ADMET prediction using software like BIOVIA Discovery Studio [13]. Key properties are calculated, including:
Step 2: Molecular Docking for Binding Mode Analysis
- Procedure: The crystal structure of the target protein (e.g., Tubulin, Aromatase) is retrieved from the Protein Data Bank (PDB). The protein is prepared by removing water molecules and heteroatoms, adding hydrogen atoms, and assigning charges. The designed compounds are docked into the protein's active site using software like AutoDock Vina. The binding affinity (in kcal/mol) and specific interactions (hydrogen bonds, salt bridges, pi-pi stacking) with key amino acid residues are analyzed [6] [8] [23]. This provides a mechanistic rationale for the predicted activity from the QSAR model.
Step 3: Validation via Molecular Dynamics (MD) Simulations
- Procedure: To confirm the stability of the docked poses, molecular dynamics simulations are run (e.g., for 100 ns) using software like GROMACS. The complex's stability is assessed by calculating the Root Mean Square Deviation (RMSD), Root Mean Square Fluctuation (RMSF), Radius of Gyration (Rg), and the number of hydrogen bonds over the simulation trajectory. The binding free energy is often calculated using the MM-PBSA (Molecular Mechanics Poisson-Boltzmann Surface Area) method to quantitatively validate the docking predictions [6] [8] [23].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Software and Computational Tools for Model Development and Validation
| Tool Category | Example Software/Platforms | Primary Function in Model Development |
|---|---|---|
| Chemistry & Modeling Suites | BIOVIA Discovery Studio [13], Spartan'14 [107], ChemDraw [107] | Structure drawing, 3D optimization, descriptor calculation, and comprehensive QSAR/ADMET modeling. |
| Descriptor Calculation | PaDEL-Descriptor [107], DRAGON [28], RDKit [28] | Generation of a wide array of 1D, 2D, and 3D molecular descriptors from chemical structures. |
| Statistical & ML Modeling | QSARINS [107], scikit-learn [28], XLSTAT [8] | Statistical analysis, feature selection, model building (MLR, PLS), and robust validation. |
| Molecular Docking | AutoDock Vina, GOLD | Predicting the binding orientation and affinity of small molecules to a protein target. |
| Dynamics & Simulation | GROMACS, AMBER, NAMD | Performing molecular dynamics simulations to assess protein-ligand complex stability. |
| Quantum Chemistry | Gaussian [8] | Performing high-level quantum mechanical calculations for accurate electronic descriptors. |
The path to regulatory acceptance for computational models in ADMET-integrated 3D-QSAR research is paved with rigorous methodology, transparent reporting, and multi-faceted validation. Adherence to established standards—encompassing robust data curation, rigorous internal and external validation, clear definition of the applicability domain, and integration of ADMET and molecular dynamics—is paramount. As these computational techniques continue to evolve, particularly with the integration of advanced AI [28], their role in guiding experimental efforts and de-risking drug discovery will only grow. By faithfully implementing these protocols and standards, researchers can enhance the credibility of their computational findings, fostering greater confidence and accelerating the journey of effective cancer therapeutics from the computer screen to the clinic.
Conclusion
The integration of 3D-QSAR with AI and machine learning represents a paradigm shift in cancer drug design, moving ADMET prediction from a late-stage bottleneck to a central, guiding component of the discovery process. This synergy enables a more rational design of compounds with optimal efficacy and safety profiles by providing deep insights into the complex 3D interactions governing biological activity and pharmacokinetics. Key takeaways include the demonstrated success of integrated computational workflows in identifying promising Tubulin and Topoisomerase IIα inhibitors, the critical importance of rigorous model validation, and the need to overcome challenges related to data quality and model interpretability. Future directions point toward the wider adoption of multi-modal AI, the integration of quantum computing, and the development of more sophisticated, dynamically predictive models that can simulate entire biological systems. These advancements hold the promise of significantly accelerating the delivery of novel, life-saving cancer therapeutics to patients.
References
- 1. Exploring Artificial Intelligence's Potential to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582507/]
- 2. Dynamic clinical trial success rates for drugs in the 21st ... [https://www.nature.com/articles/s41467-025-64552-2]
- 3. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 4. Transforming Cancer Therapy: Insights from 2025 H1 FDA ... [https://blog.crownbio.com/transforming-cancer-therapy-insights-from-2025-h1-fda-approvals-and-preclinical-drug-discovery]
- 5. Addressing screening failures in early-phase clinical trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362514/]
- 6. Design, 3D-QSAR, molecular docking, ADMET ... [https://www.sciencedirect.com/science/article/pii/S2667022423002943]
- 7. QSAR-based virtual screening, molecular docking, ADMET ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11490471/]
- 8. one derivatives as tubulin inhibitors for breast cancer therapy [https://www.nature.com/articles/s41598-024-66877-2]
- 9. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 10. Why optimize cancer drugs for ADMET? [https://www.sciencedirect.com/science/article/abs/pii/S1740677305000720]
- 11. Federated Learning for ADMET Prediction [https://www.apheris.com/resources/blog/federated-learning-for-admet-prediction-expanding-model-applicability]
- 12. 3D-QSAR Studies, Molecular Docking, Molecular Dynamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9865323/]
- 13. QSAR, ADMET & Predictive Toxicology | BIOVIA [https://www.3ds.com/products/biovia/discovery-studio/qsar-admet-predictive-toxicology]
- 14. 3D-QSAR, ADMET, and molecular docking studies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11350533/]
- 15. Design, synthesis, docking, ADMET studies, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8344243/]
- 16. Prediction of pharmacokinetic/pharmacodynamic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1578117/full]
- 17. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 18. Advancing ADMET prediction through multiscale fragment- ... [https://pubmed.ncbi.nlm.nih.gov/41021261/]
- 19. A Beginner's Guide to QSAR Modeling in Cheminformatics ... [https://neovarsity.org/blogs/cheminformatics-qsar-beginner-guides]
- 20. Three Dimensional Quantitative Structure Activity ... [https://www.sciencedirect.com/topics/immunology-and-microbiology/three-dimensional-quantitative-structure-activity-relationship]
- 21. Application of 2D and 3D-QSAR Models in Drug Design [https://www.mdpi.com/journal/pharmaceuticals/special_issues/JH712GW1PI]
- 22. Integrating QSAR modeling, ADMET screening, molecular ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525013241]
- 23. QSAR-ANN modeling, molecular docking, ADMET ... [https://pubs.rsc.org/en/content/articlelanding/2025/nj/d5nj02417j]
- 24. 3D-QSAR Design of New Bcr-Abl Inhibitors Based on Purine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12195648/]
- 25. 3D- and 2D-QSAR models' study and molecular docking of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10090277/]
- 26. 3D-QSAR, design, molecular docking and dynamics ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1545791/full]
- 27. 3D-QSAR, molecular docking and molecular dynamics ... [https://www.sciencedirect.com/science/article/pii/S2405844022032790]
- 28. AI-Integrated QSAR Modeling for Enhanced Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525248/]
- 29. Revolutionizing pharmacology: AI-powered approaches in ... [https://www.sciencedirect.com/science/article/pii/S259009862500020X]
- 30. DeepAutoQSAR | Schrödinger Machine Learning Solutions [https://www.schrodinger.com/platform/products/deepautoqsar/]
- 31. ADMET Predictor® - Simulations Plus - Machine Learning- ADMET property prediction [https://www.simulations-plus.com/software/admetpredictor/]
- 32. Advanced ADMET Modeling Using Deep Learning and AI | Technology Networks [https://www.technologynetworks.com/drug-discovery/blog/beyond-black-box-models-advances-in-data-driven-admet-modeling-403114]
- 33. ADMET predictions [https://www.vls3d.com/ADMET.html]
- 34. Leveraging machine learning models in evaluating ADMET ... [https://pubmed.ncbi.nlm.nih.gov/40585410/]
- 35. 3D-QSAR, design, molecular docking and dynamics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11841475/]
- 36. Machine learning-based 3D-QSAR models for predicting ... [https://www.sciencedirect.com/science/article/pii/S3050787125000137]
- 37. Drug Design of an Anticancer Drug: QSAR Modeling, and ... [https://www.sciencedirect.com/science/article/pii/S259012302502314X]
- 38. Computational approaches: atom-based 3D-QSAR, molecular ... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-024-01357-2]
- 39. 2D and 3D QSAR-Based Machine Learning Models for ... [https://www.sciencedirect.com/science/article/pii/S2468227625005381]
- 40. Development and experimental validation of 3D QSAR ... [https://www.sciencedirect.com/science/article/pii/S2405844024057876]
- 41. Design and discovery of new antiproliferative 1,2,4-triazin ... [https://www.sciencedirect.com/science/article/abs/pii/S0045206821003424]
- 42. Insights from 3D-QSAR, molecular docking, and dynamics for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0326245]
- 43. Computational design of quinazolin-4(3H)-one derivatives as ... [https://arabjchem.org/computational-design-of-quinazolin-43h-one-derivatives-as-multitarget-inhibitors-against-angiogenesis-and-metabolic-reprogramming-to-help-overcome-cancer-resistance/]
- 44. insights from QSAR modeling, ADMET, molecular docking ... [https://www.sciencedirect.com/science/article/pii/S2590093525000578]
- 45. Substituted 1,4-naphthoquinones for potential anticancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345971/]
- 46. Synthesis, Anti-Proliferative Activity Evaluation and 3D- ... [https://www.mdpi.com/1420-3049/23/1/186]
- 47. Design and synthesis of new 1,4-naphthoquinones ... [https://www.sciencedirect.com/science/article/abs/pii/S0045206825004171]
- 48. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12444595/]
- 49. Virtual Screening, Molecular Docking and QSAR Studies in ... [https://jddtonline.info/index.php/jddt/article/view/4218]
- 50. Assessing molecular docking tools: understanding drug ... [https://fjps.springeropen.com/articles/10.1186/s43094-025-00862-y]
- 51. Leveraging machine learning models in evaluating ADMET ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205928/]
- 52. one analogs as EGFR inhibitors: 3D-QSAR modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10027554/]
- 53. Machine learning approaches for next-generation ADMET ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625002004]
- 54. Current status and future directions of high-throughput ADME ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7322755/]
- 55. Methods in Machine Learning Computational Toxicology [https://pubmed.ncbi.nlm.nih.gov/29934890/]
- 56. GitHub - stopdragonn/OECD-COMTOX: OECD Test Guidelines-based... [https://github.com/stopdragonn/OECD-COMTOX]
- 57. Methods in Machine Learning Computational Toxicology [https://link.springer.com/protocol/10.1007/978-1-4939-7899-1_5]
- 58. 3D-QSAR, Molecular Docking, and MD Simulations of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8656170/]
- 59. Pharmacophore modeling, 3D-QSAR, docking and ADME ... [https://www.sciencedirect.com/science/article/pii/S1878535216301630]
- 60. Combined 3D-QSAR modeling and molecular docking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4531791/]
- 61. Predicting ADMET Properties from Molecule SMILE [https://pmc.ncbi.nlm.nih.gov/articles/PMC11207804/]
- 62. The three secrets to great 3D-QSAR: Alignment, alignment ... [https://cresset-group.com/about/news/the-three-secrets-to-great-3d-qsar-alignment-align/]
- 63. 3D-QSAR studies on Maslinic acid analogs for Anticancer ... [https://www.nature.com/articles/s41598-017-06131-0]
- 64. How to recognize and workaround pitfalls in QSAR studies [https://pubmed.ncbi.nlm.nih.gov/19754417/]
- 65. Advantages and limitations of classic and 3D QSAR ... [https://link.springer.com/article/10.1007/s11051-016-3564-1]
- 66. QSAR and 3D QSAR in drug design Part 2: applications ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644697010842]
- 67. 2D and 3D-QSAR, molecular docking and ADMET ... [https://pubs.rsc.org/en/content/articlelanding/2020/nj/c9nj05767f]
- 68. AI-Integrated QSAR Modeling for Enhanced Drug Discovery [https://www.mdpi.com/1422-0067/26/19/9384]
- 69. Advancing oncology drug development: Innovative ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X25002094]
- 70. Derivation of Highly Predictive 3D-QSAR Models for hERG ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10675541/]
- 71. Interpreting Complex Machine Learning Models Made Easy. [https://www.icertglobal.com/blog/understanding-and-interpreting-complex-machine-learning-models-blog]
- 72. Explainable AI: A Review of Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7824368/]
- 73. Interpretability Methods in Machine Learning: A Brief Survey [https://www.twosigma.com/articles/interpretability-methods-in-machine-learning-a-brief-survey/]
- 74. How to explain and interpret machine learning models with ... [https://medium.com/@nemagan/how-to-explain-and-interpret-machine-learning-models-with-explainable-ai-904e11745066]
- 75. 4 Methods Overview – Interpretable Machine Learning [https://christophm.github.io/interpretable-ml-book/overview.html]
- 76. 3D-QSAR, molecular docking and ADMET studies of ... [https://www.sciencedirect.com/science/article/abs/pii/S0019452222003375]
- 77. 3D-QSAR Studies, Molecular Docking, Molecular Dynamic ... [https://www.mdpi.com/2075-1729/13/1/127]
- 78. Deep learning methods for drug response prediction in ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1086097/full]
- 79. The Hallmarks of Predictive Oncology - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11969157/]
- 80. Advancing QSAR models in drug discovery for best ... [https://www.sciencedirect.com/science/article/abs/pii/S0169743925002291]
- 81. An in-depth review of AI-powered advancements in cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S0925443925000250]
- 82. The importance of good practices and false hits for QSAR ... [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2023.1237655/full]
- 83. PharmaBench: Enhancing ADMET benchmarks with large ... [https://www.nature.com/articles/s41597-024-03793-0]
- 84. Dynamic QSAR modeling for predicting in vivo genotoxicity ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03510-y]
- 85. Robust and predictive 3D-QSAR models for ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11418590/]
- 86. Recent Developments in 3D QSAR and Molecular Docking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7123761/]
- 87. Validation of QSAR Models [https://basicmedicalkey.com/validation-of-qsar-models/]
- 88. Comparison of various methods for validity evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9396839/]
- 89. Limitations of Correlation Coefficients in Research on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12242859/]
- 90. The rm2 metrics and regression through origin approach [https://www.sciencedirect.com/science/article/abs/pii/S0928098714002243]
- 91. 7 Key Stats: Mastering the Precision - Recall Curve Effectively [https://www.numberanalytics.com/blog/mastering-precision-recall-curve-stats]
- 92. Benchmarking ML in ADMET predictions: the practical impact ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-01041-0]
- 93. Comparative study between deep learning and QSAR ... [https://www.nature.com/articles/s41598-020-73681-1]
- 94. Beginner's Guide to 3D-QSAR in Drug Design [https://neovarsity.org/blogs/beginners-guide-3d-qsar-drug-design]
- 95. QSAR, molecular docking and ADMET properties in silico ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8282965/]
- 96. ADMET property prediction: The state of the art and current ... [https://optibrium.com/knowledge-base/admet-property-prediction-the-state-of-the-art-and-current-challenges/]
- 97. 3D-QSAR, Docking, ADME/Tox studies on Flavone ... [https://www.nature.com/articles/s41598-019-41984-7]
- 98. 3D-QSAR, ADME-Tox In Silico Prediction and Molecular ... [https://www.mdpi.com/2227-9717/10/8/1462]
- 99. Envisioning the Future of Cancer Science and Medicine [https://cancerprogressreport.aacr.org/progress/cpr25-contents/cpr25-envisioning-the-future-of-cancer-science-and-medicine/]
- 100. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 101. one derivatives as tubulin inhibitors for breast cancer therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11252338/]
- 102. Prediction of ADMET Properties of Anti-Breast Cancer ... [https://www.mdpi.com/1420-3049/28/5/2326]
- 103. ADMETlab 2.0 [https://admetmesh.scbdd.com/]
- 104. ADMET-AI: a machine learning ADMET platform for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11226862/]
- 105. Interpretation-ADMElab: ADMET Prediction [https://admet.scbdd.com/home/interpretation/]
- 106. ADMET evaluation in drug discovery: 21. Application and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11724520/]
- 107. QSAR, simulation techniques, and ADMET/pharmacokinetics ... [https://fjps.springeropen.com/articles/10.1186/s43094-022-00452-2]