From Sequence to Diagnosis: A Practical Guide to Machine Learning for DNA-Based Cancer Detection
This article provides a comprehensive guide for researchers and drug development professionals on the practical implementation of machine learning (ML) for cancer detection using DNA sequence data.
From Sequence to Diagnosis: A Practical Guide to Machine Learning for DNA-Based Cancer Detection
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the practical implementation of machine learning (ML) for cancer detection using DNA sequence data. It explores the foundational principles of DNA-based biomarkers, including mutations, methylation patterns, and fragmentation profiles. The piece details methodological workflows for data processing, feature extraction, and the application of both traditional and advanced deep learning models. It further addresses critical troubleshooting and optimization strategies for handling real-world data challenges like class imbalance and low signal-to-noise ratios. Finally, the article offers a framework for the rigorous validation, benchmarking, and clinical interpretation of models, synthesizing key insights to guide the development of robust, translatable ML tools for oncology.
The Genetic Blueprint of Cancer: Core Concepts and Data Sources for ML
The advancement of precision oncology hinges on the ability to decipher the complex molecular signatures of cancer. DNA biomarkers, including somatic mutations, DNA methylation changes, and copy number variations (CNVs), serve as critical indicators for cancer detection, classification, and prognosis. The integration of these biomarkers with machine learning (ML) algorithms has revolutionized oncological research, enabling the analysis of high-dimensional data from technologies like next-generation sequencing (NGS) to uncover patterns that traditional methods might overlook [1]. These computational approaches are particularly vital for tasks such as identifying the tissue-of-origin for cancers of unknown primary, predicting patient outcomes, and tailoring personalized therapeutic strategies [2]. This document outlines the practical application of these key DNA biomarkers within ML frameworks, providing detailed protocols and resources for researchers and drug development professionals.
Biomarker Fundamentals and Data Characteristics
The effective use of DNA biomarkers in ML requires a deep understanding of their biological nature and the specific challenges associated with their data representations.
Somatic Mutations
Somatic mutations are acquired genetic alterations present in tumor cells but not in the patient's germline. They represent a cornerstone of cancer genomics. In ML applications, somatic mutation data is often represented as a binary matrix, where rows correspond to patient samples and columns to specific genes or genomic positions, with values indicating the presence (1) or absence (0) of a mutation [3]. A key challenge is the inherent sparsity of this data; even in large cohorts, most genes are mutated in only a small fraction of samples [2]. Common ML features include driver mutations in genes like KRAS (lung and colorectal cancer), BRAF (melanoma), PIK3CA (breast cancer), and EGFR (non-small cell lung cancer) [4]. These mutations can inform treatment selection and serve as targets for therapeutic interventions.
DNA Methylation
DNA methylation involves the addition of a methyl group to a cytosine base, typically in a CpG dinucleotide context. In cancer, aberrant methylation manifests as global hypomethylation, which can genomic instability, and localized hypermethylation at CpG islands in promoter regions, leading to the silencing of tumor suppressor genes [5]. Methylation data is generated using array-based (e.g., Illumina Infinium 450K or 850K) or sequencing-based (e.g., whole-genome bisulfite sequencing) technologies. The data is quantitative, often reported as β-values ranging from 0 (completely unmethylated) to 1 (fully methylated) [6]. This creates a continuous, high-dimensional dataset ideal for many ML models. Its tissue-specific patterns make it exceptionally valuable for diagnostic and classification tasks [7].
Copy Number Variations (CNVs)
CNVs are somatic alterations that result in gains or losses of genomic DNA segments, leading to deviations from the normal diploid state. These variations can amplify oncogenes or delete tumor suppressor genes. In ML datasets, CNV data is typically represented as a continuous or discrete numerical matrix, where values indicate the copy number state (e.g., -2 for homozygous deletion, -1 for heterozygous deletion, 0 for neutral, 1 for gain, 2 for amplification) for each genomic segment across patient samples [1]. While not the primary focus of all cited studies, CNV data provides crucial complementary information for tumor subtyping and understanding cancer pathogenesis.
Table 1: Characteristics of Key DNA Biomarkers for Machine Learning
| Biomarker | Data Type | Typical Data Format | Key Characteristics in Cancer | Common ML Applications |
|---|---|---|---|---|
| Somatic Mutations | Discrete | Sparse binary matrix | Driver vs. passenger mutations; varies widely between cancer types. | Tumor subtyping, prediction of therapeutic targets, prognosis. |
| DNA Methylation | Continuous | β-values (0 to 1) or M-values | Tissue-specific; global hypomethylation with promoter-specific hypermethylation. | Early detection, tissue-of-origin identification, disease classification. |
| Copy Number Variations | Discrete/Continuous | Integer or segmented log-R ratios | Amplifications of oncogenes; deletions of tumor suppressor genes. | Molecular classification, understanding tumorigenesis pathways. |
Machine Learning Data Processing Protocols
Proper data preprocessing is a critical step for building robust and accurate ML models with genomic data.
Data Sourcing and Multi-Omics Integration
Large, well-curated datasets are the foundation of effective ML. The Cancer Genome Atlas (TCGA) is a primary source, containing multi-omics data from over 20,000 primary cancer and matched normal samples across 33 cancer types [1] [3]. The Genomic Data Commons (GDC) and cBioPortal provide streamlined access to this data. For methylation-specific data, repositories like the Gene Expression Omnibus (GEO) are invaluable [1]. Integration of multiple data types (e.g., RNA-seq, methylation, somatic mutation) has been shown to improve classification accuracy. For instance, a stacking ensemble model that integrated these three data types achieved 98% accuracy in classifying five common cancers, outperforming models using any single data type alone [3].
Preprocessing and Feature Selection
High-dimensional genomic data necessitates rigorous preprocessing and feature selection to avoid overfitting.
- Normalization: Techniques like Transcripts Per Million (TPM) for RNA-seq data correct for technical variations and sequencing depth, enhancing cross-sample comparability [8] [3].
- Handling Missing Data: Methods such as k-nearest neighbors (k-NN) imputation can be used to estimate and fill in missing values, ensuring a complete dataset for analysis [8].
- Dimensionality Reduction: Given the large number of features (e.g., >20,000 genes), feature selection is essential. Methods include:
- Filter Methods: Using statistical tests (e.g., Pearson correlation) to select features based on their association with the sample labels [2] [9].
- Minimum Redundancy Maximum Relevance (mRMR): An advanced filter method that selects features that are highly relevant to the target class while being minimally redundant with each other [8] [9].
- Autoencoders: A deep learning technique for non-linear dimensionality reduction that can compress data while preserving its essential biological structure [3].
- Addressing Class Imbalance: In cancer datasets, some cancer types may be over-represented. Techniques like Synthetic Minority Oversampling Technique (SMOTE) or downsampling can balance class distribution and prevent model bias [3].
Experimental and Analytical Protocols
This section provides detailed methodologies for generating and analyzing DNA biomarker data.
Protocol for Identifying Cancer-Specific Methylation Markers
Objective: To discover and validate DNA methylation markers specific to a cancer type (e.g., Breast Cancer) using array-based technology [6].
Materials:
- Tumor and tumor-adjacent tissue samples.
- Plasma samples from cancer patients, individuals with benign tumors, and healthy donors.
- Infinium Human Methylation 850K BeadChip kit (Illumina).
- Reagents for bisulfite conversion (e.g., EZ DNA Methylation Kit from Zymo Research).
- Equipment for digital droplet PCR (ddPCR), such as the Bio-Rad QX200 system.
Methodology:
- Discovery Phase:
- Extract DNA from tumor and tumor-adjacent tissues.
- Perform genome-wide methylation profiling using the 850K array.
- Identify differentially methylated CpG sites (DMCs) with an absolute methylation difference (Δβ) > 0.10 and an adjusted p-value < 0.05 using a package like "ChAMP" in R.
- Cross-reference DMCs with public datasets (e.g., TCGA, GEO) to filter for sites that are consistently differential and specific to the cancer of interest, while excluding sites methylated in white blood cells or other cancers.
Assay Development (for Plasma cfDNA):
- Design primers and minor groove binder (MGB) TaqMan probes for the top candidate methylation markers.
- Develop a multiplex droplet digital PCR (mddPCR) assay. Optimize the reaction mixture using ddPCR Supermix for Probes and bisulfite-converted DNA.
- Generate droplets, perform PCR, and read the droplets on a QX200 Droplet Reader. Analyze data with QuantaSoft software to quantify the copies of methylated alleles per mL of plasma.
Validation:
- Apply the mddPCR assay to a independent cohort of plasma cfDNA samples from confirmed patients, benign tumor individuals, and healthy controls.
- Evaluate diagnostic performance by calculating the Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) curve.
- Assess prognostic value by correlating methylation levels with overall survival data using Cox regression models.
Protocol for Multi-Omics Cancer Classification with ML
Objective: To build a high-accuracy classifier for cancer types by integrating somatic mutation, DNA methylation, and gene expression data [3].
Materials:
- RNA-seq, somatic mutation, and DNA methylation data from TCGA and LinkedOmics.
- Computational resources (e.g., high-performance computing cluster).
- Python environment with libraries: Scikit-learn, XGBoost, TensorFlow/Keras.
Methodology:
- Data Preprocessing:
- RNA-seq: Normalize raw count data using a method like DESeq2's median-of-ratios or TPM [8] [3].
- Somatic Mutation: Create a binary matrix of mutated genes.
- Methylation: Use β-values from array data.
- Clean data by removing samples with >7% missing values and reduce dimensionality using feature selection (e.g., mRMR) or an autoencoder.
Model Training with Stacking Ensemble:
- Base Models: Train a diverse set of five base classifiers on the multi-omics data: Support Vector Machine (SVM), k-Nearest Neighbors (KNN), Artificial Neural Network (ANN), Convolutional Neural Network (CNN), and Random Forest (RF).
- Meta-Model: Use the predictions from these base models as input features to train a final meta-classifier (e.g., a logistic regression model or another neural network) to make the ultimate prediction.
Validation:
- Evaluate model performance using a held-out test set or cross-validation.
- Report key metrics: Accuracy, Precision, Recall, and AUC.
- Use explainability tools like SHapley Additive exPlanations (SHAP) to interpret the model's predictions and identify the most important biomarkers [8].
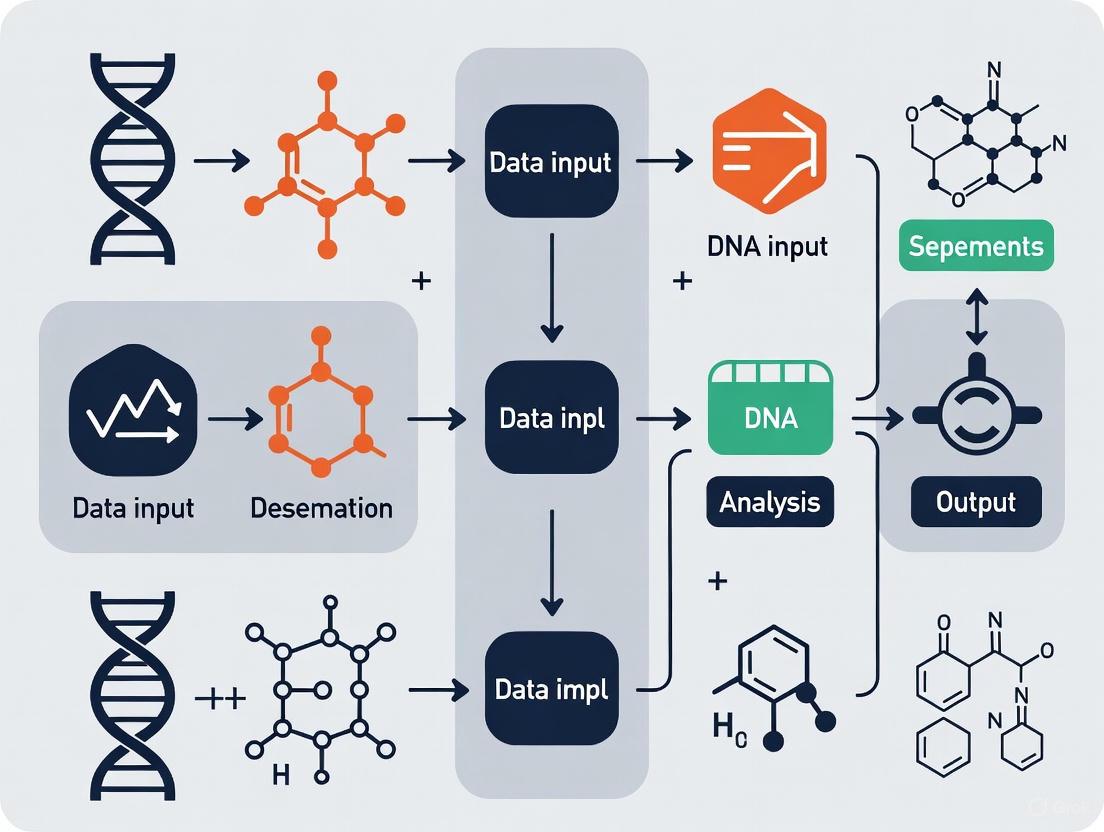
The following diagram illustrates the logical workflow of the multi-omics data integration and analysis process for cancer classification.
Multi-Omics Cancer Classification Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for DNA Biomarker and ML-Based Cancer Research
| Category / Item | Specific Examples | Function & Application in Research |
|---|---|---|
| Data Sources | The Cancer Genome Atlas (TCGA) | Primary source for multi-omics data (genomics, epigenomics, transcriptomics) from thousands of tumor samples [1] [3]. |
| Genomic Data Commons (GDC) | Data repository and portal providing unified access to TCGA and other cancer genomics datasets [1]. | |
| Gene Expression Omnibus (GEO) | Public repository for high-throughput functional genomics data, including methylation array datasets [1] [6]. | |
| Wet-Lab Reagents & Kits | Infinium MethylationEpic (850K) Kit | Array-based platform for genome-wide methylation profiling at over 850,000 CpG sites [6]. |
| EZ DNA Methylation Kit | Used for bisulfite conversion of unmethylated cytosines to uracils, a critical step for most methylation analysis methods [7]. | |
| ddPCR Supermix for Probes | Reagent for highly sensitive and absolute quantification of low-abundance nucleic acids in droplet digital PCR assays [6] [4]. | |
| Bioinformatics Tools | "ChAMP" (R/Bioconductor) | Comprehensive pipeline for the analysis of Illumina methylation array data, including DMC identification [6]. |
| "DESeq2" (R/Bioconductor) | Standard tool for differential expression analysis of RNA-seq count data, also used for normalization [8]. | |
| ANNOVAR | Tool for functional annotation of genetic variants from DNA sequencing data [1]. | |
| Machine Learning Libraries | Scikit-learn (Python) | Provides a wide array of classical ML algorithms (SVM, RF, KNN) and utilities for preprocessing and evaluation [3]. |
| XGBoost (Python/R) | Optimized gradient boosting library known for its performance and success in bioinformatics competitions [8] [2]. | |
| TensorFlow/Keras (Python) | Open-source libraries for building and training deep learning models like ANNs and CNNs [3]. | |
| Tutin | Tutin|Glycine Receptor Antagonist|Neurotoxin Research | High-purity Tutin, a potent neurotoxin and glycine receptor antagonist. Essential for neuroscience research into convulsant mechanisms. For Research Use Only. Not for human or veterinary use. |
| Tabac | Tabac|2,4,6-triiodo-3-acetamidobenzoic acid ester | Tabac (C18H21I3N2O5) is a high-purity chemical for research use only (RUO). Not for human or veterinary diagnostics or therapeutic use. |
The integration of somatic mutations, DNA methylation, and copy number variations with sophisticated machine learning models represents a powerful paradigm in modern precision oncology. As detailed in these application notes, the successful implementation of this approach relies on rigorous data preprocessing, robust experimental protocols for biomarker discovery, and the strategic use of ensemble and other ML methods to integrate multi-omics data. The provided protocols and toolkit offer a practical roadmap for researchers to contribute to this rapidly evolving field, ultimately driving forward the development of more accurate diagnostic tools and personalized cancer therapies.
Foundational Concepts: cfDNA and ctDNA
Cell-free DNA (cfDNA) refers to degraded fragments of DNA that are released into bodily fluids, such as blood plasma, through cellular processes like apoptosis and necrosis [10] [11]. In healthy individuals, the majority of cfDNA originates from normal hematopoietic cells [12]. Its fragment size typically shows a characteristic peak at approximately 166 base pairs, which corresponds to DNA protected by nucleosomes [11].
Circulating Tumor DNA (ctDNA) is a specific subset of cfDNA that is derived exclusively from tumor cells [13]. ctDNA carries tumor-specific genetic alterations, such as somatic mutations, and can exhibit a more variable fragment size profile, often including shorter fragments [11]. In cancer patients, ctDNA typically constitutes a very small fraction (0.1% to 1%) of the total cfDNA pool, making its detection technologically challenging [10] [13].
The table below summarizes the key differences between these two molecules.
Table 1: Fundamental Characteristics of cfDNA and ctDNA
| Feature | cfDNA | ctDNA |
|---|---|---|
| Source | Apoptotic/Necrotic normal cells (primarily hematopoietic lineage) | Tumor cells (via necrosis, apoptosis, or active secretion) |
| Fragment Size | Predominantly ~166 bp (mononucleosomal) | Bimodal distribution, often shorter (<150 bp) and longer fragments |
| Concentration | 1-100 ng/mL plasma (in healthy individuals) | Often < 1% of total cfDNA |
| Genetic Alterations | Wild-type | Tumor-specific (e.g., mutations in EGFR, TP53, KRAS) |
| Primary Clinical Utility | Non-invasive prenatal testing (NIPT), transplant rejection monitoring | Cancer detection, treatment monitoring, therapy selection |
Detection Technologies and Analytical Approaches
The low abundance of ctDNA necessitates highly sensitive detection methods. Common technologies include digital PCR (dPCR) and next-generation sequencing (NGS). NGS, in particular, enables a wide range of analyses, from targeted panels to whole-genome sequencing [13] [11].
The following workflow diagram illustrates a generalized protocol for cfDNA/ctDNA analysis, from sample collection to data interpretation.
Beyond simple mutation detection, several advanced analytical paradigms leverage different features of cfDNA:
- Fragmentomics: This approach analyzes the fragmentation patterns of cfDNA. Tumor-derived DNA often exhibits altered fragmentation due to differences in nucleosome positioning in cancer cells. Research has shown that nucleosome-depleted regions (NDRs) at gene promoters and first exon-intron junctions can be used to infer ctDNA burden and even the tissue of origin [12].
- Methylation Analysis: DNA methylation patterns are highly tissue-specific. Profiling the methylome of cfDNA allows for the detection of cancer signals and can help identify the tumor's origin [11].
- Long-Read Sequencing: Emerging technologies like Oxford Nanopore Sequencing (ONT) enable the simultaneous detection of multiomics features—including genetics, fragmentomics, and direct methylation profiling—in a single assay, offering a more comprehensive view from limited sample material [14].
Experimental Protocol: A Targeted NGS Approach for ctDNA Detection
This protocol outlines the key steps for detecting and analyzing ctDNA from patient blood samples using a targeted next-generation sequencing approach.
Pre-Analytical Phase: Sample Collection and Processing
- Blood Collection: Draw a minimum of 10 mL of whole blood into cell-stabilizing tubes (e.g., Streck tubes) to preserve cfDNA integrity and prevent gDNA contamination from white blood cell lysis. Streck tubes can be stored at room temperature for up to 7 days [11].
- Plasma Separation: Process samples within the recommended timeframe. Centrifuge blood at 1,600 × g for 10-20 minutes at 4°C to separate plasma from cellular components. Carefully transfer the supernatant (plasma) to a new tube without disturbing the buffy coat. Perform a second, high-speed centrifugation at 16,000 × g for 10 minutes at 4°C to remove any remaining cellular debris [13] [11].
- cfDNA Extraction: Extract cfDNA from the clarified plasma using a bead-based method (e.g., MagMAX kits) optimized for the recovery of short DNA fragments. Bead-based methods are preferred over silica-column techniques for their superior recovery of ctDNA's characteristic short fragments [11]. Elute the purified cfDNA in a low-EDTA TE buffer or nuclease-free water.
- Quality Control (QC): Quantify the extracted cfDNA using a fluorescence-based assay (e.g., Qubit dsDNA HS Assay). Assess the fragment size distribution using a Bioanalyzer High Sensitivity DNA kit or similar. A successful extraction from a healthy individual should show a dominant peak at ~166 bp [11].
Library Preparation and Sequencing
- Library Construction: Use 10-50 ng of cfDNA as input. Prepare sequencing libraries using a hybrid-capture-based targeted NGS panel. The steps include:
- End-Repair and A-Tailing: Convert DNA fragments to blunt-ended, 5'-phosphorylated molecules and add a single 'A' nucleotide to the 3' ends.
- Adapter Ligation: Ligate platform-specific sequencing adapters to the fragments. For multiplexing, use unique dual-indexed adapters for each sample.
- Target Enrichment: Hybridize the library to biotinylated probes designed to capture a panel of cancer-related genes. Wash away non-specific fragments and amplify the captured library with a limited number of PCR cycles [15].
- Sequencing: Pool the enriched, indexed libraries and sequence on an Illumina platform (e.g., NextSeq 550Dx) to a high depth of coverage (>5,000x is recommended for reliable detection of low-frequency variants) [15].
Bioinformatics Analysis
- Primary Analysis: Demultiplex sequenced reads and assess raw data quality using tools like FastQC.
- Alignment: Map the sequencing reads to a reference genome (e.g., hg19/GRCh37) using a splice-aware aligner like BWA-MEM.
- Variant Calling: Identify single nucleotide variants (SNVs) and small insertions/deletions (indels) using a variant caller such as Mutect2, which is designed for detecting low-frequency somatic variants. A common variant allele frequency (VAF) threshold of ≥2% is often applied [15].
- Annotation and Reporting: Annotate called variants using tools like SnpEff and filter them against population databases. Classify variants according to clinical significance guidelines (e.g., AMP/ASCO/CAP tiers), focusing on Tier I (strong clinical significance) and Tier II (potential clinical significance) alterations for reporting [15].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for cfDNA/ctDNA Analysis
| Item | Function/Application | Example Products/Types |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes | Stabilizes nucleated blood cells to prevent gDNA release and preserve cfDNA profile for up to 7 days at room temperature. | Streck Cell-Free DNA BCT, PAXgene Blood cDNA Tube |
| Bead-Based Nucleic Acid Extraction Kits | Isolate short-fragment DNA with high efficiency; critical for ctDNA recovery. | MagMAX Cell-Free DNA Isolation Kit, Dynabeads |
| Targeted Hybrid-Capture Sequencing Panels | Enrich for genomic regions of interest (e.g., cancer genes) to enable deep sequencing and low-frequency variant detection. | SNUBH Pan-Cancer Panel, Illumina TruSight Oncology, Guardant360 |
| Ultra-Sensitive DNA Quantitation Assays | Accurately quantify low concentrations and small volumes of cfDNA. | Qubit dsDNA HS Assay, Agilent High Sensitivity DNA Kit |
| Molecular Barcoded Adapters | Tag individual DNA molecules pre-amplification to correct for PCR and sequencing errors, improving sensitivity and specificity. | Unique Molecular Identifiers (UMIs) in kits from vendors like Illumina and IDT |
| Pfetm | Pfetm, CAS:91112-39-9, MF:C16H26Cl2N4O2S, MW:409.4 g/mol | Chemical Reagent |
| Dhesn | DHESN (Dihydroergosine) | Research-grade DHESN (Dihydroergosine), a serotoninergic ergot alkaloid. For research use only. Not for human or veterinary diagnostic or therapeutic use. |
Integration with Machine Learning for Cancer Detection
The complex, high-dimensional data generated from cfDNA/ctDNA sequencing is an ideal substrate for machine learning (ML) and artificial intelligence (AI). ML models can integrate diverse features—including genetic mutations, fragmentomics, and methylation patterns—to improve the sensitivity and specificity of cancer detection.
The diagram below illustrates a typical predictive modeling pipeline for DNA sequence analysis in cancer detection.
Key ML Applications in cfDNA/ctDNA Analysis:
- Overcoming Biological Noise: A primary challenge in early cancer detection is the low concentration of ctDNA. Machine learning algorithms are capable of modeling complex data relationships to distinguish subtle oncogenic patterns from the background noise of normal cfDNA [10]. For instance, models can be trained on fragmentation patterns (fragmentomics) to predict the tissue of origin of cfDNA fragments, effectively acting as a "nucleosome positioning" scanner [10] [12].
- Multi-Feature Integration: ML models can simultaneously analyze multiple data types. A model might take as input mutation calls, copy number variations, and fragmentation profiles from the same NGS run to generate a more robust cancer detection score than any single feature could provide alone [14].
- Sensitivity for Early Detection: Groundbreaking research has demonstrated the potential of this approach. One study used a multi-cancer early detection test on prospectively collected plasma samples and found that ctDNA was detectable in some individuals more than three years prior to their clinical cancer diagnosis [16]. Achieving this level of sensitivity requires analytical methods capable of identifying extremely faint tumor signals, a task for which ML is uniquely suited.
Clinical Applications and Practical Implementation
The analysis of cfDNA and ctDNA has a rapidly expanding set of clinical applications across the cancer care continuum.
Table 3: Key Clinical Applications of cfDNA/ctDNA in Oncology
| Application | Description | Real-World Impact / Example |
|---|---|---|
| Early Cancer Detection & Screening | Identifying cancer signals in asymptomatic individuals via MCED (Multi-Cancer Early Detection) tests. | ctDNA detectable >3 years prior to clinical diagnosis in some cases [16]. GRAIL's Galleri test screens for 50+ cancers [11]. |
| Therapy Selection | Identifying targetable mutations to guide use of targeted therapies or immunotherapies. | Detection of EGFR, KRAS, or BRAF mutations to select appropriate tyrosine kinase inhibitors [15] [11]. |
| Minimal Residual Disease (MRD) & Recurrence Monitoring | Detecting molecular residual disease after curative-intent surgery to predict relapse. | ctDNA positivity post-surgery predicts recurrence months before radiological evidence (e.g., Signatera assay). Guides adjuvant therapy decisions [17] [11]. |
| Therapeutic Response Monitoring | Dynamically tracking ctDNA burden to assess treatment efficacy in real-time. | Declining ctDNA levels correlate with tumor regression; rising levels indicate progression or resistance [17]. |
Considerations for Practical Implementation:
- Test Validation and Concordance: While ctDNA testing is becoming standard in advanced disease, its concordance with tissue-based testing is not perfect. Studies show a concordance rate of approximately 70-80% for detecting key mutations, with sensitivity influenced by disease stage and tumor shedding [17].
- Economic and Logistical Factors: The implementation of NGS and ctDNA testing in clinical practice requires significant investment in bioinformatics infrastructure, specialized personnel, and rigorous quality control to ensure reasonable turnaround times [15].
- Interpretation in Context: ctDNA results must be interpreted with caution. False negatives can occur in patients with low tumor shedding, and false positives can arise from clonal hematopoiesis. A multidisciplinary approach, integrating ctDNA results with clinical, radiological, and pathological findings, is essential for optimal patient management [17].
The shift from broad, genome-wide methylation analysis to focused, targeted panels represents a significant evolution in the application of next-generation sequencing (NGS) for cancer research. Whole-genome bisulfite sequencing (WGBS) provides a comprehensive, single-base resolution map of DNA methylation across the entire genome, serving as a powerful discovery tool for identifying novel epigenetic biomarkers [18] [19]. In contrast, targeted sequencing panels enable researchers to concentrate resources on specific genomic regions with known or suspected associations with cancer, facilitating deeper sequencing at lower costs [20]. This strategic progression from unbiased discovery to focused validation is particularly crucial for developing machine learning models in cancer detection, as it dictates both the quality and quantity of training data required for building accurate predictive algorithms. The integration of these complementary approaches provides the foundational data necessary for advancing precision oncology through artificial intelligence.
Whole Genome Bisulfite Sequencing (WGBS)
Principle and Mechanism: WGBS combines sodium bisulfite conversion with high-throughput DNA sequencing to detect methylated cytosines at single-nucleotide resolution across the entire genome [18] [19]. The fundamental principle relies on the differential chemical reactivity of methylated versus unmethylated cytosines when treated with sodium bisulfite. Unmethylated cytosines undergo deamination to form uracils, which are then converted to thymines during PCR amplification and subsequent sequencing. In contrast, methylated cytosines (5-methylcytosine, 5mC) are protected from this conversion and remain as cytosines [18]. This chemical modification creates distinct sequencing signatures that allow for precise mapping of methylation status when aligned to an untreated reference genome.
Key Methodological Steps:
- DNA Extraction and Quality Control: High-quality genomic DNA is extracted, with input requirements varying by specific protocol (ranging from >100 ng for standard protocols to as low as ~20 ng for tagmentation-based methods) [18].
- Bisulfite Conversion: DNA is treated with sodium bisulfite, facilitating the deamination of unmethylated cytosines to uracils while leaving methylated cytosines unchanged.
- Library Preparation: Converted DNA undergoes library preparation, with emerging methods like Tagmentation-based WGBS (T-WGBS) combining fragmentation and adapter ligation in a single step to minimize DNA loss [18].
- Sequencing and Data Analysis: Libraries are sequenced using NGS platforms, followed by alignment to a reference genome and methylation calling using specialized bioinformatics tools.
The following diagram illustrates the core workflow and principle of bisulfite sequencing:
Variants of Bisulfite Sequencing
Several specialized bisulfite sequencing methods have been developed to address specific research needs and limitations of conventional WGBS:
Table 1: Comparison of Bisulfite Sequencing Methods
| Method | Key Features | Advantages | Disadvantages | Best Applications |
|---|---|---|---|---|
| Whole-Genome Bisulfite Sequencing (WGBS) | Genome-wide mapping at single-base resolution [18] | Covers CpG and non-CpG methylation; comprehensive [18] | High cost; substantial DNA degradation; complex data analysis [18] [19] | Discovery of novel methylation biomarkers; pan-cancer studies [21] |
| Reduced-Representation Bisulfite Sequencing (RRBS) | Uses restriction enzymes for sequence-specific fragmentation [18] | Cost-effective; focuses on CpG-rich regions [18] | Covers only ~10-15% of CpGs; biased selection [18] | High-throughput population studies; specific promoter analysis [18] |
| Oxidative Bisulfite Sequencing (oxBS-Seq) | Differentiates 5mC from 5-hydroxymethylcytosine (5hmC) [18] | Clearly distinguishes between 5mC and 5hmC [18] | Complex protocol; same limitations as BS-Seq for alignment [18] | Fine epigenetic mapping; studying active demethylation pathways |
| Tagmentation-based WGBS (T-WGBS) | Uses Tn5 transposase for fragmentation and adapter ligation [18] | Minimal DNA input (~20 ng); fast protocol [18] | Does not distinguish 5mC from 5hmC; alignment challenges [18] | Limited sample availability; clinical specimens |
| Single-cell Bisulfite Sequencing (scBS-Seq) | Adapted from BS-Seq and PBAT for single cells [18] | Enables methylation analysis at single-cell resolution [18] | Extremely low input DNA; technical noise | Tumor heterogeneity studies; developmental biology |
Targeted Sequencing Panels
Targeted sequencing panels represent a focused approach that sequences specific genes or genomic regions with known or suspected associations with disease. These panels are particularly valuable in clinical applications where resources must be strategically allocated to maximize information yield from limited samples [20].
Design Strategies:
- Predesigned Panels: Contain curated gene content selected from published literature and expert guidance for specific diseases or phenotypes [20].
- Custom Panels: Allow researchers to target specific genomic regions relevant to their research interests, enabling follow-up on discoveries from WGBS or other genome-wide approaches [20].
Methodological Approaches:
- Amplicon Sequencing: Utilizes highly multiplexed PCR to amplify regions of interest prior to sequencing. This approach is ideal for smaller gene sets (<50 genes) and offers a simpler, more affordable workflow with less hands-on time [20].
- Hybrid Capture: Involves solution-based hybridization of genomic DNA to biotinylated probes complementary to targeted regions, followed by magnetic pulldown. This method is better suited for larger gene content (>50 genes) and provides more comprehensive variant detection, though with longer turnaround times [20] [22].
Targeted panels sequence genes of interest to exceptional depth (500-1000× or higher), enabling identification of rare variants that might be missed in broader approaches [20]. The manageable data size simplifies storage and analysis while reducing costs compared to whole-genome methods.
Experimental Protocols for Key Applications
WGBS Protocol for Cancer Epigenomics
Sample Preparation:
- Input Requirements: 20-100 ng of high-quality genomic DNA, depending on the specific protocol [18]. For tagmentation-based WGBS, inputs as low as 20 ng are feasible [18].
- Quality Control: Assess DNA integrity using agarose gel electrophoresis or fragment analyzers. Ensure DNA is free of contaminants that may inhibit bisulfite conversion.
Bisulfite Conversion and Library Preparation:
- Bisulfite Treatment: Treat DNA with sodium bisulfite using commercial kits (e.g., Zymo Research EZ DNA Methylation kits). Typical conditions: incubation at 95°C for 30-60 seconds followed by 50-60°C for 45-60 minutes [18] [19].
- Library Construction: For standard WGBS, fragment converted DNA by sonication or enzymatic digestion to ~300 bp fragments. Ligate methylated adapters to fragment ends [18]. For T-WGBS, use Tn5 transposase for simultaneous fragmentation and adapter incorporation [18].
- PCR Amplification: Amplify libraries with DNA polymerases optimized for bisulfite-converted templates. Limit PCR cycles (typically 8-12) to minimize bias in amplification of methylated versus unmethylated sequences [19].
- Library Quantification and Validation: Quantify libraries using fluorometric methods and validate size distribution using bioanalyzer or tape station systems.
Sequencing and Data Analysis:
- Sequencing Parameters: Sequence on Illumina platforms (NovaSeq, HiSeq) with 2×150 bp paired-end reads recommended for adequate alignment efficiency [18].
- Bioinformatic Processing:
- Quality Control: Use FastQC to assess read quality.
- Alignment: Map reads to a bisulfite-converted reference genome using specialized aligners (Bismark, BS-Seeker2).
- Methylation Calling: Extract methylation information at each cytosine position, generating coverage files and methylation ratios (number of C reads/total reads).
- Differential Analysis: Identify differentially methylated regions (DMRs) between sample groups using tools like methylKit or DMRept.
Targeted Panel Protocol for Liquid Biopsy Applications
Sample Preparation:
- Cell-Free DNA Extraction: Isolate cfDNA from 5-10 mL of plasma using specialized extraction kits (e.g., Illumina Cell-Free DNA Prep with Enrichment). Typical yields range from 1-100 ng cfDNA per mL plasma [20].
- Quality Assessment: Verify cfDNA size distribution (expected peak ~167 bp) using bioanalyzer systems.
Library Preparation and Target Enrichment:
- Library Construction: Use library prep kits designed for low-input cfDNA (e.g., Illumina Cell-Free DNA Prep with Enrichment) with incorporation of unique molecular identifiers (UMIs) to distinguish true variants from PCR errors [20].
- Target Enrichment: For hybrid capture approaches, hybridize libraries with biotinylated probes targeting cancer-associated genes (e.g., 50-200 gene panels). Incubate for 16-24 hours, then capture with streptavidin beads [20]. For amplicon approaches, use multiplex PCR with primers targeting regions of interest.
- Post-Capture Amplification: Amplify captured libraries with limited PCR cycles (8-12) to maintain representation.
Sequencing and Variant Calling:
- Sequencing Parameters: Sequence to high depth (typically >3000× for cfDNA applications) using Illumina platforms to detect variants at low allele frequencies (down to 0.2%) [20].
- Bioinformatic Analysis:
- Alignment: Map reads to reference genome using optimized aligners (BWA-MEM).
- Variant Calling: Use specialized callers (MuTect2, VarScan2) with UMI correction to identify somatic mutations at low allele fractions.
- Annotation: Annotate variants with population frequency, functional impact, and clinical significance using databases (COSMIC, ClinVar).
Integration with Machine Learning for Cancer Detection
Data Requirements for Machine Learning Models
The successful application of machine learning (ML) to cancer detection requires carefully curated training data with specific characteristics. WGBS provides comprehensive methylation data ideally suited for discovery-phase ML, while targeted panels offer focused data for validated biomarker applications.
Table 2: Data Characteristics for Machine Learning Applications
| Data Characteristic | WGBS for ML | Targeted Panels for ML |
|---|---|---|
| Genomic Coverage | ~28 million CpG sites in humans [19] | Hundreds to thousands of validated CpG sites |
| Sample Requirements | Higher input DNA (typically >20 ng) [18] | Lower input (cfDNA feasible) [20] |
| Data Volume | Very large (hundreds of GB per sample) | Manageable (GB range per sample) |
| Feature Selection | Unbiased, discovery-oriented [5] | Hypothesis-driven, focused on known biomarkers |
| Best ML Applications | Novel biomarker discovery; pan-cancer classification [5] | Clinical diagnostics; minimal residual disease detection [23] |
AI-Driven Methylation Analysis in Multi-Cancer Detection
Artificial intelligence has revolutionized the analysis of DNA methylation patterns for cancer detection and classification. Advanced ML algorithms, including convolutional neural networks (CNNs) and gradient boosting machines (GBMs), can recognize subtle cancer-specific methylation signatures in complex datasets [5]. These approaches have enabled the development of Multi-Cancer Early Detection (MCED) tests that analyze circulating tumor DNA (ctDNA) methylation patterns to detect multiple cancer types from a single blood sample [5].
Notable Applications:
- GRAIL's Galleri Test: Employs targeted methylation sequencing of over 100,000 informative regions and ML algorithms to detect more than 50 cancer types with high specificity [5].
- CancerSEEK: Integrates mutation data with protein biomarkers to improve diagnostic sensitivity across eight cancer types [5].
- Prostate Cancer Detection: Machine learning-prioritized targeted sequencing panels have demonstrated improved detection of tumor-derived variants in cfDNA from patients with localized prostate cancer [23].
The typical workflow for ML-driven cancer detection from methylation data involves multiple stages of data processing and model development, as shown in the following diagram:
Essential Research Reagents and Solutions
Successful implementation of DNA sequencing technologies for cancer research requires carefully selected reagents and platforms optimized for specific applications.
Table 3: Essential Research Reagents and Solutions
| Category | Specific Products/Solutions | Key Features | Applications |
|---|---|---|---|
| Library Preparation | Illumina DNA Prep with Enrichment [20] | Flexible targeted sequencing for genomic DNA, tissue, blood, saliva, and FFPE samples | Targeted panel sequencing |
| Illumina Cell-Free DNA Prep with Enrichment [20] | Scalable library prep for highly sensitive mutation detection from cfDNA | Liquid biopsy applications | |
| Bisulfite Conversion | Zymo Research EZ DNA Methylation kits | Efficient conversion with minimal DNA degradation | WGBS, RRBS |
| Target Enrichment | Illumina Custom Enrichment Panel v2 [20] | Fully customized enrichment solution (20 kb-62 Mb regions) | Custom targeted sequencing |
| AmpliSeq for Illumina Custom Panels [20] | Custom panels optimized for specific content of interest | Focused gene panels | |
| Sequencing Platforms | Illumina NovaSeq, HiSeq, MiSeq [24] | High-throughput sequencing with various output options | WGBS, targeted panels |
| Ion Torrent Personal Genome Machine [24] | Semiconductor-based sequencing technology | Targeted sequencing | |
| Design Tools | DesignStudio Software [20] | Online tool for optimizing custom probe designs | Custom panel design |
The strategic selection of DNA sequencing technologies—from comprehensive WGBS to focused targeted panels—provides researchers with a powerful toolkit for advancing cancer detection and precision medicine. WGBS offers an unbiased discovery platform for identifying novel methylation biomarkers across the entire genome, while targeted panels enable cost-effective, deep sequencing of validated markers in clinical samples. The integration of these technologies with advanced machine learning algorithms has already demonstrated significant promise in multi-cancer early detection tests and precision oncology applications. As sequencing costs continue to decline and analytical methods improve, these approaches will increasingly converge, enabling more sensitive, specific, and accessible cancer diagnostics that leverage the full potential of epigenetic information for improving patient outcomes.
Public Data Repositories and Standards for Acquiring Cancer DNA Sequence Data
The effective application of machine learning (ML) to cancer detection hinges on access to high-quality, well-annotated DNA sequence data. For researchers building ML models to identify oncogenic signatures, understanding the landscape of public data repositories and the standards governing data acquisition is a critical first step. These resources provide the foundational data upon which predictive models for cancer detection, diagnosis, and treatment are built. This guide details the primary sources of cancer genomic data, the standard file formats encountered, and practical protocols for accessing and utilizing this data within an ML research workflow.
Major Public Data Repositories
Large-scale public repositories house vast amounts of genomic data from cancer studies, serving as indispensable resources for the research community. The following table summarizes key repositories used in cancer genomics research.
Table 1: Key Public Data Repositories for Cancer Genomics
| Repository Name | URL | Primary Focus | Data Types | Bulk Data Retrieval |
|---|---|---|---|---|
| NCI Genomic Data Commons (GDC) | https://gdc.cancer.gov/ | Unified repository for NCI cancer genome programs like TCGA [25]. | Clinical data, somatic mutations, gene expression, DNA methylation [25]. | Yes [26] |
| Gene Expression Omnibus (GEO) | https://www.ncbi.nlm.nih.gov/geo/ | Public repository for functional genomics data from tens of thousands of studies [25]. | Array- and sequence-based data from published studies [25]. | Yes [25] |
| Genome Sequence Archive (GSA) | https://ngdc.cncb.ac.cn/gsa/ | International repository for raw sequence data, based in China [27]. | Raw sequence data [27]. | Information missing |
| cBioPortal | http://www.cbioportal.org/ | Visualization, analysis, and download of large-scale cancer genomics datasets [25]. | Gene sequencing data from cancer studies, including TCGA [25]. | Yes [25] |
| Broad GDAC Firehose | http://gdac.broadinstitute.org/ | Provides standardized analysis outputs on the entire TCGA dataset [25]. | Analysis results and high-level standardized data tables [25]. | Yes [25] |
The NCI Genomic Data Commons (GDC) is a cornerstone for cancer genomics, providing a unified platform that harmonizes data from multiple projects, including The Cancer Genome Atlas (TCGA) [25]. The GDC not only provides access to data but also includes web-based tools for searching, viewing, and downloading datasets. For large-volume data transfers, the GDC offers a high-performance Data Transfer Tool [26]. It's important to note that access to controlled data, which includes detailed patient-level information, requires authorization through the database of Genotypes and Phenotypes (dbGaP) [26].
For researchers seeking user-friendly interfaces to explore genetic alterations across cancer types, tools like cBioPortal are invaluable. It allows for the visualization of mutation and copy number alteration patterns for a set of input genes across samples within a given study [25]. Similarly, Oncomine and UALCAN focus on enabling researchers to explore differential gene expression between cancer and normal samples [25].
Data Formats and Standards
Understanding the structure and content of genomic file formats is essential for data preprocessing and feature extraction in ML pipelines. The two primary text-based formats for nucleotide sequences are FASTA and FASTQ.
Table 2: Comparison of FASTA and FASTQ File Formats
| Feature | FASTA Format | FASTQ Format |
|---|---|---|
| Information Content | Nucleotide or protein sequences [28] | Nucleotide sequences and per-base quality scores [28] |
| Standard Use | Reference genomes, assembled contigs, protein sequences [28] | Raw sequence reads from high-throughput sequencers [28] |
| Quality Information | Typically none, though some conventions use lower-case for low-confidence bases [28] | Yes (Phred-scaled quality scores for each base) [28] |
| File Structure | 1. Identifier line starting with >2. Sequence data on subsequent lines [28] |
1. Identifier line starting with @2. Sequence data3. A + line (may repeat identifier)4. Quality scores string [28] |
| Typical File Size | Relatively smaller | Very large (often 10s of GB compressed), due to quality scores and raw data volume [28] |
FASTA Format
A FASTA file contains one or more sequences. Each entry consists of an identifier line beginning with a > symbol, followed by the sequence data. The identifier can include a unique ID and optional descriptive information about the sequence, such as gene function, species, or location in the genome [28]. This format is the standard input for sequence alignment tools like BLAST and HMMER, and for reference genomes used in read mapping [28].
FASTQ Format
FASTQ is the standard format for raw sequencing reads from platforms like Illumina, PacBio, and Oxford Nanopore. Each read is represented by four lines: the sequence identifier (starting with @), the nucleotide sequence, a separator line (often just a +), and a string of quality score characters [28]. The quality scores are encoded in Phred scale, where each character represents the probability of a base-calling error [29]. These scores are crucial for ML applications as they provide a measure of confidence for each base, allowing preprocessing steps to trim or filter low-quality data, thereby improving downstream model accuracy.
Data Access Tiers and Acquisition Workflow
Genomic data is often organized into different tiers of accessibility. Open-access data is freely available to all users without restrictions. Controlled-access data, which includes personally identifiable information, requires researchers to apply for access through dbGaP by submitting a research protocol for approval [26].
The data within repositories can also be understood through a "level" framework, which describes the degree of processing:
- Level 1: Raw data (e.g., FASTQ files, microarray images) [25].
- Level 2: Essential processed information (e.g., BAM alignment files) [25].
- Level 3: Data ready for analysis (e.g., variant calls, normalized expression tables) [25].
- Level 4: Results from platform-specific analyses (e.g., significantly mutated genes) [25].
- Level 5: Integrated findings, combining multiple data types and external knowledge [25].
ML researchers often start with Level 3 or 4 data for model training, while those developing novel base-calling or variant-calling algorithms may require Level 1 or 2 data.
The following diagram illustrates the typical workflow for acquiring and preparing cancer DNA sequence data for ML research.
Protocols for Data Acquisition and Preprocessing
Protocol: Accessing Controlled Data from the GDC
This protocol outlines the steps to acquire controlled-access genomic data, which is often essential for building robust ML models in cancer research.
Prerequisites:
- eRA Commons Account: Ensure you have a registered account in the NIH eRA Commons system.
- Institutional Signing Official: Identify the appropriate official at your institution who can approve and sign data access requests.
Procedure:
- dbGaP Application: Navigate to the dbGaP website and submit a Data Access Request (DAR) for the specific dataset of interest (e.g., a TCGA dataset via the GDC) [26].
- Research Protocol Submission: As part of the DAR, you will be required to provide a detailed research protocol outlining the planned use of the data, including specific research objectives and the measures you will take to protect data confidentiality.
- Review and Approval: The request is reviewed by the Data Access Committee (DAC) associated with the dataset. This process ensures the proposed use is scientifically valid and ethically sound.
- Download Data: Once approved, use the GDC Data Portal or the high-performance GDC Data Transfer Tool for downloading large volumes of data [26]. The transfer tool is essential for managing the large file sizes typical of genomic data.
Protocol: From Raw FASTQ to ML-Ready Features
This protocol describes a common preprocessing workflow to transform raw sequencing reads (FASTQ) into structured numerical features suitable for machine learning. This is a generalized protocol; specific tools and parameters will vary based on the research goal.
Materials:
Procedure:
- Quality Control (QC): Run FastQC on the raw FASTQ files to assess per-base sequence quality, adapter contamination, and other potential issues. This step informs the parameters for subsequent trimming.
- Adapter Trimming and Quality Filtering: Use a tool like Trimmomatic to remove sequencing adapters and trim low-quality bases from the ends of reads. This improves the quality of the data used for alignment.
- Alignment to Reference Genome: Map the quality-filtered reads to a reference genome using an aligner like BWA or Bowtie2 [28]. This generates a BAM file, which stores the aligned reads and their positions.
- Post-Alignment Processing and Variant Calling: This includes sorting and indexing BAM files. For mutation-based ML models, use a variant caller like GATK [28] to identify single nucleotide variants (SNVs) and small insertions/deletions (indels) from the BAM file. The output is a VCF file listing genomic variants.
- Feature Engineering: Convert the biological data into a numerical feature matrix. This could involve:
- Variant-Based Features: Creating a sample x gene matrix where values represent mutation counts or a binary indicator of mutation presence/absence.
- Coverage-Based Features: Calculating read depth or copy number variation (CNA) in genomic bins [10].
- Fragmentation Features: For cell-free DNA (cfDNA) analyses, features can include fragment size distributions, nucleosome positioning patterns, and preferred end sites [10].
Table 3: Essential Research Reagent Solutions for cfDNA-based ML Detection
| Reagent / Material | Function in the Protocol |
|---|---|
| Cell-Free DNA (cfDNA) from Plasma | The target analyte containing the signal of circulating tumor DNA (ctDNA) for non-invasive liquid biopsy [10]. |
| Whole Genome Bisulfite Sequencing (WGBS) Kit | A protocol for treating DNA with bisulfite to convert unmethylated cytosines to uracils, allowing for the assessment of methylation states, a key cancer signature [10]. |
| High-Throughput Sequencer (e.g., Illumina) | The instrument platform for generating raw sequence reads in FASTQ format from the input DNA [10]. |
| Genome Analysis Toolkit (GATK) | A software package for variant discovery and genotyping; used in the protocol for variant calling and sequence analysis [10]. |
| Reference Genome FASTA File | The standardized reference sequence (e.g., GRCh38) against which cfDNA reads are aligned to identify genomic origins and variations [28] [10]. |
The path to acquiring and standardizing cancer DNA sequence data is a structured process critical for powering ML-driven detection algorithms. By leveraging the rich data from repositories like the GDC and GEO, and adhering to standardized preprocessing protocols, researchers can generate high-quality, ML-ready datasets. Mastering these foundational steps of data acquisition and preparation is paramount for developing robust, generalizable models that can ultimately contribute to advancements in early cancer detection and precision oncology.
Building the Model: ML Workflows and Algorithm Selection for DNA Sequence Analysis
The shift towards data-driven methodologies in genomics has made the effective conversion of raw DNA sequences into informative features a critical step in machine learning (ML) pipelines for cancer detection. This process, known as feature engineering, directly influences a model's ability to identify pathological patterns. This Application Note details three advanced feature extraction techniques—k-mer analysis, sentence embeddings (SBERT/SimCSE), and DNA methylation profiling—within the practical context of cancer research. Each method bridges the gap between complex biological sequences and quantifiable features, enabling researchers to build more accurate and robust diagnostic and classification models. We provide structured protocols, comparative data, and visualization tools to facilitate implementation by research scientists and drug development professionals.
k-mer Analysis for DNA Sequence Classification
k-mer analysis is a foundational technique in genomic machine learning that involves breaking down long DNA sequences into shorter, overlapping subsequences of length k. This approach treats DNA as a text string, allowing the application of Natural Language Processing (NLP) methods to identify sequence-based motifs and variations associated with different cancer types [30]. The core principle is that the frequency and composition of these k-mers provide a numerical signature that can distinguish between sequences derived from healthy and cancerous tissues, or between different cancer subtypes.
Detailed Experimental Protocol
Step 1: Data Collection and Preprocessing
- Source: Obtain DNA/Genomic sequences in FASTA format from public repositories like the National Center for Biotechnology Information (NCBI) [31].
- Handling Class Imbalance: If certain cancer types are underrepresented (e.g., MERS and dengue in viral datasets), employ the Synthetic Minority Oversampling Technique (SMOTE). This algorithm generates synthetic samples for minority classes by interpolating between existing instances in feature space [31].
Step 2: k-mers Generation
- Generate all possible subsequences of length k from a DNA sequence via a sliding window.
- The choice of k is critical: small k (e.g., 3-6) captures simple motifs, while larger k captures more complex, specific sequences but increases dimensionality.
- Python Function Example:
For a sequence "CCGAGGGCT" with
k=3, output is['CCG', 'CGA', 'GAG', 'AGG', 'GGG', 'GGC', 'GCT'][30].
Step 3: k-mers Concatenation and Vectorization
- Concatenate all k-mers from a sequence into a single "document."
- Convert this document into a numerical format using:
- Bag-of-Words (BoW): Creates a count vector of all possible k-mers.
- TF-IDF (Term Frequency-Inverse Document Frequency): Weights k-mer frequencies by their importance across the entire dataset, often yielding superior results [30].
Step 4: Model Training and Classification
- Feed the vectorized features into standard ML classifiers (e.g., Random Forest, SVM) or deep learning models.
Table 1: Performance of Different Models and k-mer Encoding on DNA Sequence Classification
| Model Architecture | Encoding Method | Reported Testing Accuracy | Application Context |
|---|---|---|---|
| CNN | K-mer (size not specified) | 93.16% | Classification of COVID, MERS, SARS, dengue, hepatitis, influenza [31] |
| CNN-Bidirectional LSTM | K-mer (size not specified) | 93.13% | Classification of COVID, MERS, SARS, dengue, hepatitis, influenza [31] |
| Extreme Gradient Boosting (XGBoost) | Hybrid k-mer/probabilistic | 89.51% | Classification of mutated DNA to identify virus origin [31] |
| Ensemble Decision Tree | K-mer based features | 96.24% | Classification of complex DNA sequence datasets [31] |
Workflow Visualization
Sentence Embeddings (SBERT/SimCSE) for Genomic Sequences
Sentence-BERT (SBERT) is a modification of the BERT architecture designed to derive semantically meaningful sentence embeddings that can be compared using cosine-similarity [32]. When applied to genomics, DNA sequences are treated as sentences, and k-mers or other representations are treated as words. SBERT uses siamese and triplet networks to create embeddings where semantically similar sequences (e.g., from the same cancer subtype) are close in vector space. SimCSE is a simple, unsupervised extension that uses dropout as a form of noise to create positive pairs for training, significantly improving embedding quality without labeled data [33]. This approach is powerful for semantic similarity search and clustering of genomic data.
Detailed Experimental Protocol
Step 1: DNA Sequence Preprocessing and "Sentence" Formation
- Convert DNA sequences into a textual format suitable for embedding models.
- Recommended Approach: Generate k-mers (e.g., k=3-6) for a sequence and join them with spaces to form a "sentence" (e.g.,
CCG CGA GAG AGG GGG). This preserves local context and creates an input structure analogous to natural language.
Step 2: Unsupervised Training with SimCSE
- SimCSE leverages dropout for creating positive pairs, requiring no manually labeled data.
- Python Code Skeleton: [33].
Step 3: Generating and Using Embeddings
- Use the trained model to compute dense vector embeddings for any DNA sequence.
- Inference:
- These embeddings can be used for:
- Clustering: Group unlabeled sequences to discover novel cancer subtypes.
- Semantic Search: Find sequences most similar to a query sequence in a large database in seconds, a task that is computationally prohibitive with raw BERT [32].
Table 2: Impact of Model and Training Parameters on Embedding Quality (AskUbuntu MAP)
| Parameter | Option 1 | Performance (MAP) | Option 2 | Performance (MAP) | Option 3 | Performance (MAP) |
|---|---|---|---|---|---|---|
| Base Model | distilbert-base-uncased | 53.59 | bert-base-uncased | 54.89 | distilroberta-base | 56.16 |
| Batch Size (distilroberta-base) | 128 | 56.16 | 256 | 56.63 | 512 | 56.69 |
| Pooling Mode (distilroberta-base, 512 batch) | CLS Pooling | 56.56 | Mean Pooling | 56.69 | Max Pooling | 52.91 |
Workflow Visualization
Methylation Profiling for Cancer Classification
DNA methylation is an epigenetic modification involving the addition of a methyl group to a cytosine base in a CpG dinucleotide context. Aberrant methylation patterns are stable, organ-specific, and play a key role in cancer development, making them ideal biomarkers for diagnosis and classification [34] [35]. Machine learning models can leverage data from platforms like the Illumina Infinium Human Methylation 450k BeadChip (interrogating 450,000 CpG sites) to distinguish cancerous from normal tissues and identify the tissue of origin for cancers of unknown primary (CUP) with high accuracy [34] [35].
Detailed Experimental Protocol
Step 1: Data Acquisition and Preprocessing
- Source: Download methylation β-values (ranging from 0 unmethylated to 1 fully methylated) for cancer and normal tissue samples from The Cancer Genome Atlas (TCGA) via the Genomic Data Commons (GDC) portal [34] [35].
- Preprocessing:
- Remove low-variance features: Filter out CpG sites with minimal variation across samples.
- Batch effect correction: Correct for technical artifacts using methods like ComBat.
- Data split: Divide data into training (70%) and test (30%) sets, stratifying by cancer type [34].
Step 2: Feature Selection for Biomarker Discovery
- Given the high dimensionality (~485,000 features), aggressive feature reduction is essential.
- Two-Step Filter and Embedded Method:
- Decision Tree Approach: An alternative is to use a decision tree to identify a small panel of CpG sites where the median β-value for cancer and normal groups fall on opposite sides of a biologically relevant threshold (e.g., β=0.3) [35].
Step 3: Model Training and Validation
- Train a classifier on the selected CpG sites.
- Model Choices: Extreme Gradient Boosting (XGBoost), CatBoost, Random Forest, and Neural Networks have shown high performance [34] [35].
- Validation: Use stratified 5-fold cross-validation and an independent test set. Evaluate using accuracy, F1 score, and AUC.
Table 3: Performance of Methylation-Based Classifiers Across Studies
| Cancer Types | Number of Samples / Types | Feature Selection Method | Final # of CpG Sites | Best Model(s) | Reported Accuracy |
|---|---|---|---|---|---|
| 10 types (e.g., BRCA, COAD, LUAD) [34] | 890 / 10 | ANOVA/Gain Ratio -> Gradient Boosting | 100 | XGBoost, CatBoost, Random Forest | 87.7% - 93.5% |
| Urological Cancers (Prostate, Bladder, Kidney) [35] | Not Specified / 3 | Decision Tree | 6 - 14 (per cancer type) | Neural Network | High (Visual separation via PCA) |
Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Resources for Feature Extraction in Genomic ML
| Category / Item | Function / Description | Example Sources / Tools |
|---|---|---|
| Data Sources | ||
| The Cancer Genome Atlas (TCGA) | Provides comprehensive, publicly available genomic datasets (including methylation and sequence data) for multiple cancer types. | Genomic Data Commons (GDC) Portal [34] [35] |
| National Center for Biotechnology Information (NCBI) | Repository for DNA sequence data in FASTA format, essential for sequence-based classification tasks. | NCBI Nucleotide Database [31] |
| Wet-Bench Profiling | ||
| Illumina Infinium Methylation BeadChip | Platform for genome-wide methylation profiling, generating β-values for ~450,000 or ~850,000 CpG sites. | Illumina 450k/850k Array [34] [35] |
| Software & Computational Tools | ||
| Orange Data Mining Suite | A Python-based, visual tool for data analysis, machine learning, and preprocessing of methylation and other biological data. | Orange v3.32 [34] |
| Sentence Transformers (SBERT) | The primary Python library for using and training state-of-the-art sentence embedding models like SBERT and SimCSE. | sbert.net [32] [33] [36] |
| Scikit-learn, XGBoost, CatBoost | Standard Python libraries for implementing a wide range of machine learning models and evaluation metrics. | [34] [31] |
| Bioinformatics Packages | Custom Python packages for genomic data preprocessing, including k-mer generation and vectorization. | PyDNA (hypothetical example) [30] |
| Azido | Azido, MF:N3, MW:42.021 g/mol | Chemical Reagent |
| AR-42 | AR-42, MF:C18H20N2O3, MW:312.4 g/mol | Chemical Reagent |
The transition from raw DNA sequences to meaningful features is a critical enabler for modern machine learning applications in cancer research. K-mer analysis provides a robust and interpretable method for sequence-based classification. Sentence embedding techniques like SBERT and SimCSE offer a powerful, modern approach for understanding semantic similarity and clustering in genomic data without the need for extensive labeled datasets. Finally, methylation profiling leverages well-established epigenetic biology to deliver highly accurate tissue-of-origin and diagnostic classifications, even with a minimal set of CpG sites. The protocols and analyses provided here serve as a practical guide for researchers aiming to implement these techniques, ultimately contributing to more precise cancer detection and diagnosis.
The application of machine learning (ML) to DNA sequence analysis is revolutionizing the field of cancer detection, offering new pathways for early diagnosis and personalized treatment strategies. As the volume and complexity of genomic data grow, selecting and implementing the appropriate model architecture becomes critical for translating data into actionable clinical insights. This practical guide focuses on three powerful architectures demonstrating significant promise in oncology research: blended ensembles, XGBoost, and convolutional neural networks (CNNs). We detail their practical implementation through specific application notes, experimental protocols, and performance benchmarks derived from recent studies, providing researchers with a framework for applying these techniques to DNA-based cancer detection.
Performance Comparison of Model Architectures
The table below summarizes the performance of different model architectures as reported in recent cancer detection and classification studies.
Table 1: Comparative Performance of ML Architectures in Cancer Detection
| Model Architecture | Application Context | Data Types | Reported Performance | Reference |
|---|---|---|---|---|
| Blended Ensemble (LR + GNB) | Multi-cancer type classification | DNA Sequencing | 100% accuracy for BRCA1, KIRC, COAD; 98% for LUAD, PRAD; ROC AUC 0.99 | [37] |
| Stacked Deep Learning Ensemble | Multi-cancer type classification | RNA-seq, Somatic Mutation, DNA Methylation | 98% accuracy with multiomics data | [3] |
| XGBoost | Cancer-specific chromatin feature analysis | Cell-free DNA, Open Chromatin | Improved cancer detection accuracy | [38] |
| Convolutional Neural Network (CNN) | Cancer type prediction | Gene Expression (RNA-seq) | 93.9–95.0% accuracy across 33 cancer types and normal tissue | [39] |
| Random Forest, NN, XGBoost Ensemble | General cancer detection and classification | Genomic Data | 99.45% detection accuracy, 93.94% type classification accuracy | [40] |
Application Notes & Experimental Protocols
Blended Ensemble for DNA Sequencing Data
Application Note: A high-performance blended ensemble combining Logistic Regression (LR) and Gaussian Naive Bayes (GNB) has been developed for DNA-based cancer prediction [37]. This architecture leverages the strengths of both models—GNB's strong foundational assumptions and LR's ability to model complex decision boundaries. The blend creates a lightweight, interpretable, yet highly effective tool suitable for clinical settings where both accuracy and explainability are valued. The model was validated on a cohort of 390 patients across five cancer types (BRCA1, KIRC, COAD, LUAD, PRAD), achieving near-perfect accuracies [37].
Experimental Protocol:
Data Preparation:
- Input: DNA sequencing data from patient samples.
- Processing: Perform standard genomic data preprocessing, including quality control, alignment, and variant calling. Structure the data into a feature matrix suitable for traditional ML algorithms.
Model Training & Hyperparameter Tuning:
- Implement both Logistic Regression and Gaussian Naive Bayes base models.
- Hyperparameter Optimization: Conduct a comprehensive grid search to optimize key parameters for both models. This includes regularization strength (
C) and solver for LR, as well as variance smoothing for GNB. - Blending: Train a meta-learner (often a linear model) on the predictions (or class probabilities) generated by the base models' cross-validated folds. This prevents overfitting.
Model Validation:
- Validate the final blended model on a held-out test set.
- Performance Metrics: Report accuracy, precision, recall, F1-score, and ROC-AUC. The benchmark for this architecture includes accuracies of 100% for several cancer types and a macro-average ROC AUC of 0.99 [37].
The following diagram illustrates the workflow for developing this blended ensemble model:
XGBoost for Open Chromatin Analysis in Cell-free DNA
Application Note: XGBoost has proven highly effective for analyzing nucleosome enrichment patterns in cell-free DNA (cfDNA) at open chromatin regions, providing a non-invasive method for cancer detection [38]. Its key advantage in this context is the combination of high predictive performance with interpretability. By using SHAP or built-in feature importance, researchers can identify which specific genomic loci (e.g., cancer-specific or immune cell-specific open chromatin regions) most significantly contribute to the prediction, yielding biologically actionable insights [38].
Experimental Protocol:
Feature Engineering from cfDNA:
- Input: cfDNA sequencing data from blood plasma of cancer patients and healthy donors.
- Feature Definition: Define features based on read-count enrichment or nucleosome positioning patterns within cell type-specific open chromatin regions (e.g., from ATAC-seq peaks of relevant cancer and immune cells) [38].
- Data Wrangling: Structure these enrichment scores into a feature matrix where rows are samples and columns are genomic regions.
Model Training with Interpretability:
- Training: Train an XGBoost classifier on the feature matrix, using cancer vs. healthy as the target variable.
- Handling Class Imbalance: Apply techniques like SMOTE (Synthetic Minority Over-sampling Technique) or adjusting class weights to manage imbalanced datasets [41].
- Interpretation: Use SHAP (SHapley Additive exPlanations) analysis or XGBoost's native feature importance to rank the genomic regions by their contribution to the model's predictions [38]. This identifies key cancer-associated chromatin features.
Validation:
- Use cross-validation and hold-out testing.
- Performance Metrics: Assess model performance using ROC-AUC, accuracy, and precision. The model should demonstrate a distinct improvement in cancer prediction compared to baseline methods [38].
Convolutional Neural Networks for Gene Expression Data
Application Note: CNNs, while traditionally applied to image data, can be successfully adapted to one-dimensional genomic data, such as gene expression profiles. Their ability to learn local patterns and hierarchical features makes them powerful for cancer type classification from RNA-seq data [39]. Studies have achieved high accuracy (93.9–95.0%) in classifying 33 different cancer types from TCGA data using various CNN architectures [39].
Experimental Protocol:
Data Preprocessing & Structuring:
- Input: Gene expression data (e.g., FPKM or TPM values from RNA-seq).
- Normalization: Apply log2(FPKM + 1) transformation and normalize the data [39].
- Gene Filtering: Filter out low-information genes (e.g., those with low mean expression or standard deviation).
- Input Structuring: For a 1D-CNN, structure the expression values of ~7,100 genes into a 1D vector. For a 2D-CNN, reshape the vector into a 2D matrix, though the gene order may not be biologically meaningful [39].
Model Architecture & Training:
- Architecture Choice:
- 1D-CNN: Uses 1D convolutional kernels that scan the input vector. This is often sufficient and computationally efficient [39].
- 2D-CNN: Reshapes data into a 2D matrix and uses 2D kernels.
- Training: Use a shallow architecture (one convolutional layer) to prevent overfitting, given the typically limited number of patient samples. The network typically includes a convolution layer, a max-pooling layer, and fully connected layers [39].
- Regularization: Employ dropout and L2 regularization to further mitigate overfitting.
- Architecture Choice:
Model Interpretation & Validation:
- Interpretation: Use guided saliency maps or other interpretability techniques to identify genes with the greatest influence on the classification outcome. This can reveal known and novel cancer marker genes [39].
- Validation: Perform robust k-fold cross-validation and test on independent datasets. Report accuracy, confusion matrices, and per-class metrics.
The workflow for implementing a 1D-CNN for gene expression classification is as follows:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Resources for ML-based Cancer Detection
| Resource Name | Type | Primary Function in Research | Example Source |
|---|---|---|---|
| The Cancer Genome Atlas (TCGA) | Data Repository | Provides a vast, publicly available collection of genomic, epigenomic, and clinical data from multiple cancer types for model training and validation. | [3] [39] |
| LinkedOmics | Data Repository | Offers multiomics data (e.g., methylation, somatic mutations) integrated with TCGA, facilitating multi-modal model development. | [3] |
| UK Biobank | Data Repository | A large-scale biomedical database containing genetic, lifestyle, and health information from participants, useful for developing broad population-level models. | [42] |
| SHAP (SHapley Additive exPlanations) | Software Library | Provides model-agnostic interpretability, explaining the output of any ML model (e.g., XGBoost) by quantifying feature importance. | [38] [42] |
| Autoencoder | Algorithm | Used for unsupervised feature extraction and dimensionality reduction of high-dimensional genomic data (e.g., RNA-seq) prior to classification. | [3] |
| SMOTE | Algorithm | A synthetic oversampling technique to address class imbalance in datasets, preventing model bias toward majority classes. | [3] [41] |
| Appna | Appna, CAS:60189-44-8, MF:C14H18N4O4, MW:306.32 g/mol | Chemical Reagent | Bench Chemicals |
| YM758 | YM758|If Channel Inhibitor|CAS 312752-85-5 | YM758 is a novel, specific sinoatrial node If current channel inhibitor for cardiovascular research. This product is for Research Use Only. | Bench Chemicals |
Cancer remains one of the most complex challenges in global healthcare, with accurate and early diagnosis being crucial for effective treatment and improved patient outcomes [3]. The inherent heterogeneity of cancer, where tumors can exhibit significant molecular differences even within the same type, complicates diagnosis and treatment planning [43]. Traditional single-omics approaches often fail to capture the complete biological picture of carcinogenesis, limiting their diagnostic accuracy [44].
Recent advances in machine learning (ML) and deep learning (DL), particularly ensemble methods that blend multiple algorithms, have demonstrated remarkable potential in overcoming these limitations [45]. This case study examines the implementation of a high-accuracy blended ensemble framework for multi-cancer classification, focusing on practical implementation within the broader context of DNA sequence analysis and multi-omics data integration. We present a detailed analysis of the methodology, experimental protocols, and performance outcomes based on recent research, providing researchers and drug development professionals with actionable insights for developing robust cancer classification systems.
Background and Rationale
The Multi-Omics Approach in Cancer Classification
Multi-omics data integration has emerged as a powerful paradigm in cancer research, providing complementary insights into disease mechanisms across genomic, transcriptomic, and epigenomic dimensions [43]. The fundamental premise is that while single-omics data (e.g., RNA sequencing alone) can yield valuable insights, integrating multiple data types captures more comprehensive biological signatures, leading to improved classification accuracy [3] [46].
Key omics data types relevant to cancer classification include:
- RNA sequencing: Provides information about gene expression levels and transcriptome activity [3]
- DNA methylation: An epigenetic mechanism that regulates gene expression and shows characteristic changes in cancer [3] [46]
- Somatic mutation data: Reveals acquired genetic alterations that drive carcinogenesis [3]
- miRNA and lncRNA expression: Offers insights into regulatory networks that control cellular processes [43]
Studies have consistently demonstrated that models integrating multiple omics data types outperform single-omics approaches. For instance, one investigation showed that while RNA sequencing and methylation data individually achieved 96% accuracy, and somatic mutation data reached 81%, their integration boosted performance to 98% accuracy [3] [46].
Ensemble Learning in Cancer Diagnostics
Ensemble learning methods combine multiple base classifiers to produce a single, more accurate predictive model [47]. These approaches are particularly well-suited to cancer classification tasks due to their ability to:
- Mitigate overfitting in high-dimensional data
- Handle class imbalance through specialized sampling techniques
- Capture complementary patterns across diverse data types
- Improve generalization to unseen data [3] [44]
The "blended ensemble" approach referenced in this case study typically involves stacking or voting mechanisms that leverage the strengths of diverse algorithms, including both traditional machine learning models and deep learning architectures [37] [48].
Materials and Data Preparation
Publicly available multi-omics databases serve as foundational resources for developing cancer classification models. Key repositories include:
Table 1: Primary Data Sources for Multi-Omics Cancer Classification
| Data Source | Description | Relevant Data Types | Scale |
|---|---|---|---|
| The Cancer Genome Atlas (TCGA) | Comprehensive database containing molecular profiles of multiple cancer types [3] [43] | RNA sequencing, somatic mutations, DNA methylation | ~20,000 primary cancer and matched normal samples across 33 cancer types [3] |
| LinkedOmics | Multi-omics database extending TCGA data [3] | Somatic mutations, DNA methylation | 32 TCGA cancer types and 10 CPTAC cohorts [3] |
| UCSC Xena Repository | Platform for cancer genomics data [44] | Exon expression, mRNA expression, miRNA expression, DNA methylation | Multiple TCGA cohorts including STAD (gastric cancer) [44] |
Data Preprocessing Pipeline
Effective preprocessing is critical for handling the high-dimensionality, noise, and technical variability inherent in multi-omics data. The standard workflow includes:
Data Cleaning and Quality Control
Initial data cleaning involves identifying and removing cases with missing or duplicate values. In one implementation, this step resulted in the removal of approximately 7% of cases [3]. For DNA methylation data, missing values can be imputed using K-nearest neighbor (KNN) interpolation [44].
Normalization
Normalization addresses technical variations across experiments and platforms. For RNA sequencing data, the transcripts per million (TPM) method is widely used, calculated as:
[ TPM = \frac{10^6 \times (\text{reads mapped to transcript} / \text{transcript length})}{\sum(\text{reads mapped to transcript} / \text{transcript length})} ]
This approach reduces bias resulting from choice of technique, experimental conditions, and measurement precision [3]. For other data types, min-max scaling to [0, 1] range is commonly employed [44].
Feature Extraction and Dimensionality Reduction
The high-dimensional nature of omics data (often thousands of features per sample) necessitates effective dimensionality reduction. Autoencoders have demonstrated particular utility for this task, preserving essential biological properties while reducing computational complexity [3] [44]. A typical architecture includes:
- Five dense layers with 500 nodes each
- Rectified linear unit (ReLU) activation functions
- Dropout of 0.3 to prevent overfitting [3]
Alternative feature selection methods include differential expression analysis using packages like LIMMA, with Benjamini-Hochberg adjusted p-value thresholds of <0.001 [44].
Handling Class Imbalance
Class imbalance is a common challenge in cancer datasets, where sample sizes may vary significantly across cancer types. Effective strategies include:
Table 2: Approaches for Handling Class Imbalance
| Method | Description | Application Example |
|---|---|---|
| SMOTE-Tomek | Hybrid approach combining synthetic minority oversampling (SMOTE) with Tomek link undersampling [44] | Generates synthetic instances of minority class while removing ambiguous boundary samples [44] |
| Downsampling | Randomly removing samples from majority classes | Used in ensemble frameworks to balance class distribution [3] |
| SMOTE | Synthetic Minority Oversampling Technique | Creates artificial examples of underrepresented classes [3] |
The following diagram illustrates the complete data preprocessing workflow:
Figure 1: Multi-omics Data Preprocessing Workflow
Experimental Protocol and Ensemble Framework
Blended Ensemble Architecture
The core innovation in high-accuracy cancer classification involves blending multiple machine learning models into an ensemble framework. The stacking ensemble approach has demonstrated particular effectiveness, achieving up to 98% accuracy in multi-cancer classification tasks [3] [46].
A typical implementation includes two main stages:
Base Learners
The first layer consists of diverse base classifiers that capture complementary patterns in the data. Commonly employed algorithms include:
- Support Vector Machine (SVM): Effective for high-dimensional data [3] [44]
- Random Forest (RF): Ensemble of decision trees resistant to overfitting [3] [44]
- k-Nearest Neighbors (KNN): Simple instance-based learning [3]
- Convolutional Neural Network (CNN): Captures spatial hierarchies in data [3] [44]
- Artificial Neural Network (ANN): Standard feedforward networks [3]
- Decision Trees (DT): Interpretable tree-based models [44]
- AdaBoost: Adaptive boosting algorithm [44]
Meta-Learner
The predictions from base learners serve as input to a meta-classifier that learns optimal combination weights. XGBoost has demonstrated excellent performance in this role, though logistic regression and other algorithms are also used [48] [44].
The following diagram illustrates this ensemble architecture:
Figure 2: Blended Ensemble Architecture for Cancer Classification
Implementation Protocol
Computational Environment
Ensemble frameworks for multi-omics data typically require substantial computational resources. Implementations are commonly conducted in Python 3.10 using high-performance computing infrastructure, such as the Aziz Supercomputer at King Abdulaziz University, which ranks as the second fastest supercomputer in the Middle East and North Africa region [3].
Model Training and Validation
A rigorous validation protocol is essential for reliable performance assessment:
- Data Splitting: Partition data into training (70-80%), validation (10-15%), and test (10-15%) sets
- Cross-Validation: Employ k-fold cross-validation (typically k=5 or k=10) to mitigate overfitting
- Hyperparameter Tuning: Use grid search or Bayesian optimization to optimize model parameters [37]
- External Validation: Test models on independent datasets to assess generalizability [44]
Performance Evaluation and Results
Classification Accuracy
Blended ensemble approaches have demonstrated state-of-the-art performance across multiple cancer types and datasets. The following table summarizes key results from recent implementations:
Table 3: Performance Comparison of Ensemble Methods for Cancer Classification
| Study | Cancer Types | Data Types | Ensemble Method | Accuracy | Key Metrics |
|---|---|---|---|---|---|
| Stacked Deep Learning Ensemble [3] [46] | Breast, colorectal, thyroid, non-Hodgkin lymphoma, corpus uteri | RNA sequencing, somatic mutation, DNA methylation | Stacking ensemble (SVM, KNN, ANN, CNN, RF) | 98% | Multi-omics integration crucial for highest accuracy |
| MASE-GC Framework [44] | Gastric cancer | Exon expression, mRNA, miRNA, DNA methylation | Autoencoder + stacking ensemble (SVM, RF, DT, AdaBoost, CNN) with XGBoost meta-learner | 98.1% | Precision: 98.45%, Recall: 99.2%, F1-score: 98.83% |
| Blended Ensemble [37] | BRCA1, KIRC, COAD, LUAD, PRAD | DNA sequencing | Logistic Regression + Gaussian Naive Bayes | 100% for BRCA1, KIRC, COAD; 98% for LUAD, PRAD | Micro- and macro-average ROC AUC: 0.99 |
| Voting Classifier [48] | Pancreatic cancer | Urine biomarkers | Ensemble voting classifier | 96.61% | Precision: 98.72%, AUC: 99.05% |
Ablation Studies and Comparative Analysis
Ablation studies consistently demonstrate the value of both multi-omics integration and ensemble approaches. For example:
- In the MASE-GC framework, ablation confirmed the complementary contributions of autoencoders and ensemble components, with CNN and Random Forest providing the largest performance gains [44]
- The stacked deep learning ensemble showed that multi-omics integration (98% accuracy) substantially outperformed single-omics approaches (96% for RNA-seq or methylation alone, 81% for somatic mutations) [3]
- External validation of the MASE-GC framework on independent cohorts (GSE62254, GSE15459, GSE84437, and ICGC) maintained accuracy above 95.8% with F1-scores exceeding 96.9%, demonstrating robust generalizability [44]
Implementing a high-accuracy blended ensemble for multi-cancer classification requires both computational resources and biological data. The following table details essential components:
Table 4: Essential Research Reagents and Resources for Multi-Cancer Ensemble Classification
| Resource Category | Specific Tools/Resources | Function/Purpose |
|---|---|---|
| Data Sources | The Cancer Genome Atlas (TCGA) [3] [43] | Provides standardized multi-omics data across cancer types |
| LinkedOmics [3] | Extends TCGA with additional multi-omics data | |
| UCSC Xena Repository [44] | Platform for accessing and analyzing cancer genomics data | |
| Computational Frameworks | Python 3.10 [3] | Primary programming language for implementation |
| Scikit-learn | Machine learning library for traditional algorithms (SVM, RF, KNN) | |
| TensorFlow/PyTorch | Deep learning frameworks for implementing CNNs and autoencoders | |
| XGBoost [44] | Gradient boosting implementation for meta-learners | |
| Preprocessing Tools | Autoencoders [3] [44] | Dimensionality reduction while preserving biological information |
| SMOTE-Tomek [44] | Hybrid approach for addressing class imbalance | |
| LIMMA R package [44] | Differential feature analysis and selection | |
| Computational Infrastructure | High-performance computing clusters [3] | Aziz Supercomputer or equivalent for processing large datasets |
Discussion and Implementation Considerations
Interpretation and Explainability
As ensemble models grow in complexity, interpretability becomes increasingly important for clinical translation. Explainable AI (XAI) methods, particularly Shapley Additive Explanations (SHAP), can identify the most influential features in classification decisions [48]. For instance, in pancreatic cancer diagnosis, SHAP analysis revealed top influential features with the greatest positive SHAP values, providing biological insights alongside predictions [48].
Clinical Translation Potential
The high accuracy demonstrated by blended ensemble approaches (98%+ across multiple studies) suggests strong potential for clinical application. These models could serve as:
- Decision support tools in primary care settings [3]
- Second-reader systems for pathological assessment
- Triage mechanisms for prioritizing high-risk cases
However, successful translation requires addressing several challenges:
- Regulatory approval for clinical decision support systems
- Integration with existing clinical workflows
- Validation in diverse patient populations
- Real-time performance requirements for clinical settings
Limitations and Future Directions
Current implementations face several limitations that represent opportunities for future research:
Data Quality and Availability: Despite large aggregate datasets, individual cancer types may have limited samples, potentially leading to overfitting [3]
Computational Complexity: Ensemble methods with multiple base learners and meta-classifiers require substantial computational resources [3]
Interpretability Challenges: Complex ensemble models function as "black boxes," complicating biological interpretation [48]
Generalization Across Populations: Most models are trained on TCGA data, which may not represent global population diversity
Future research directions should focus on:
- Developing more efficient ensemble architectures that maintain accuracy with reduced complexity
- Integrating explainable AI directly into the ensemble framework
- Expanding validation across diverse, multi-ethnic cohorts
- Exploring transfer learning to adapt models to new cancer types with limited data
This case study demonstrates that blended ensemble approaches represent a powerful methodology for multi-cancer classification, achieving accuracies of 98%+ by effectively integrating multi-omics data and leveraging the complementary strengths of diverse machine learning algorithms. The detailed experimental protocols and performance benchmarks provided here offer researchers and drug development professionals a practical foundation for implementing these approaches in their own work.
As sequencing technologies continue to advance and multi-omics datasets expand, blended ensemble methods are poised to play an increasingly important role in precision oncology. Their ability to synthesize complex, high-dimensional biological data into accurate classification decisions holds significant promise for improving early cancer detection, diagnosis, and ultimately, patient outcomes.
Leveraging Transfer Learning and Pre-trained Models for Enhanced Performance
The application of artificial intelligence (AI) in oncology represents a paradigm shift in how researchers approach cancer detection and diagnosis. Within this domain, transfer learning has emerged as a particularly powerful strategy, especially when working with complex genomic data such as DNA sequences. This approach addresses a fundamental challenge in medical AI: obtaining sufficiently large, labeled datasets for training models from scratch. By leveraging knowledge gained from pre-existing models trained on large-scale datasets in related domains, transfer learning enables researchers to achieve robust performance even when the availability of labeled genomic data is limited [49] [50].
In the specific context of cancer detection from DNA sequences, transfer learning demonstrates particular value. Cancer biomarkers often manifest as subtle patterns within vast genomic landscapes, requiring sophisticated models to detect. Traditional machine learning approaches frequently struggle with the high-dimensionality of methylation data and relatively small sample sizes typically available in genomic cancer studies [51]. Transfer learning circumvents these limitations by allowing models to first learn general genomic patterns from large, diverse datasets before specializing in cancer-specific detection tasks. This methodology has shown remarkable success across various cancer types, including breast, lung, and other common malignancies, often achieving performance metrics that surpass traditional approaches [51] [52] [49].
The integration of pre-trained models from related domains, such as natural language processing, has further accelerated advances in this field. Interestingly, large language models pre-trained on DNA sequence information can provide valuable embeddings that, when integrated with methylation profiles, significantly enhance feature representation for cancer detection tasks [51]. This cross-disciplinary approach exemplifies how transfer learning bridges domains to extract more meaningful insights from genomic data, ultimately pushing the boundaries of what's possible in early cancer detection and diagnosis.
Quantitative Performance Analysis of Transfer Learning Approaches
The application of transfer learning methodologies to cancer detection from genomic data has yielded quantitatively superior results across multiple studies. The table below summarizes key performance metrics reported in recent research, providing a comparative view of different approaches.
Table 1: Performance Metrics of Transfer Learning Models in Cancer Detection
| Model/Approach | Cancer Type | Key Metrics | Data Type | Reference |
|---|---|---|---|---|
| cfMethylPre | Multiple (82 cancer types) | Weighted F1-score: 0.942, Matthews Correlation Coefficient: 0.926 | cfDNA methylation profiling | [51] |
| ResNet50 + SVM | 18 cancer types | Accuracy: 0.98 | Gene sequences (FCGR6 features) | [52] |
| ResNet50 + Fully Connected | 18 cancer types | Accuracy: 0.97 | Gene sequences (FCGR5 features) | [52] |
| Deep Transfer Learning Framework | Lung cancer | Significant improvement over baseline (specific metrics not provided) | CT imaging and genomic data | [49] |
Beyond the metrics captured in the table, several studies reported additional qualitative advantages of transfer learning approaches. The cfMethylPre framework demonstrated not only high predictive accuracy but also biological interpretability, successfully identifying three novel breast cancer genes (PCDHA10, PRICKLE2, and PRTG) through model interpretation and biological experimental validation [51]. These genes demonstrated inhibitory effects on cell proliferation and migration in breast cancer cell lines, validating the clinical relevance of the model's predictions.
The ResNet50-based approaches highlighted how different feature extraction strategies impact final model performance. The combination of ResNet50 with Support Vector Machines (SVM) using FCGR6 features achieved 98% accuracy in classifying 18 cancer diseases based on gene sequence composition, outperforming the same architecture with fully connected layers and FCGR5 features [52]. This demonstrates that transfer learning effectiveness depends significantly on both the base architecture and the complementary algorithms used in conjunction.
When evaluated against traditional machine learning methods, transfer learning approaches consistently demonstrate advantages in handling the high-dimensional nature of genomic data while mitigating the challenges of limited sample sizes. This performance preservation, even with smaller cancer-specific datasets, underscores the value of knowledge transfer from larger, more general genomic databases [51] [50].
Experimental Protocols for Transfer Learning Implementation
Protocol 1: cfMethylPre Framework for Methylation-Based Cancer Detection
The cfMethylPre framework represents a sophisticated implementation of transfer learning specifically designed for cancer detection using circulating cell-free DNA (cfDNA) methylation profiling. The protocol involves a structured, two-phase learning approach as detailed below.
Table 2: Key Research Reagents and Computational Tools for cfMethylPre
| Resource Type | Name/Specification | Function in Protocol |
|---|---|---|
| Pretraining Data | Bulk DNA methylation data (2,801 samples across 82 cancer types and normal controls) | Provides base knowledge for initial model training before specialization to cfDNA |
| Fine-tuning Data | cfDNA methylation profiling data | Enables model adaptation to specific characteristics of circulating cell-free DNA |
| Computational Framework | Deep transfer learning with large language model embeddings | Integrates DNA sequence information with methylation profiles to enhance feature representation |
| Validation Method | Biological experimental validation | Confirms biological relevance of identified biomarkers through cell proliferation and migration assays |
Step-by-Step Procedure:
Data Acquisition and Preprocessing: Collect bulk DNA methylation data encompassing 2,801 samples across 82 cancer types and normal controls. Simultaneously, obtain cfDNA methylation profiling data for the target application. Apply standard preprocessing including quality control, normalization, and batch effect correction to both datasets.
Feature Enhancement with DNA Sequence Embeddings: Leverage pre-trained large language model embeddings from DNA sequence information. Integrate these embeddings with methylation profiles to create enhanced feature representations that capture both sequence context and methylation status.
Pretraining Phase: Initialize the model architecture suitable for methylation data analysis. Train the model on the bulk DNA methylation dataset to learn general patterns of methylation across multiple cancer types. This phase allows the model to develop a foundational understanding of cancer-related methylation patterns.
Transfer Learning Phase: Adapt the pre-trained model to the specific characteristics of cfDNA methylation data through fine-tuning. Replace the final layers of the model to specialize for the target task. Train with a lower learning rate to preserve general knowledge while adapting to cfDNA-specific patterns.
Model Validation: Evaluate performance using appropriate metrics including weighted Matthews Correlation Coefficient and F1-score. Perform biological validation of identified methylation signatures through experimental assays in relevant cell lines to confirm functional relevance to cancer processes.
Protocol 2: DNA Sequence Classification via Transfer Learning and FCGR
This protocol details an alternative approach that utilizes Frequency Chaos Game Representation (FCGR) to transform DNA sequences into image-like representations suitable for analysis with pre-trained computer vision models.
Step-by-Step Procedure:
Sequence Preprocessing: Obtain gene sequences relevant to the cancer types of interest. Perform quality control to ensure sequence integrity and remove low-quality regions.
Feature Extraction with FCGR: Convert DNA sequences into numerical representations using Frequency Chaos Game Representation. This technique calculates the frequency of each k-mer (subsequences of length k) in the sequence. For optimal performance with ResNet50, use FCGR6 (6-mer frequency counts) which provides the appropriate balance between specificity and computational efficiency.
DeepInsight Feature Selection: Process the FCGR features using DeepInsight methodology to transform non-image data into an image format compatible with convolutional neural networks. This step identifies and retains the most representative k-mers while reducing dimensionality to manage computational complexity.
Transfer Learning with ResNet50: Utilize a pre-trained ResNet50 model, initially trained on the ImageNet dataset, as the feature extractor. Remove the final classification layer of ResNet50 and replace it with either:
- A Support Vector Machine (SVM) classifier for classification into 18 cancer types, or
- A fully connected layer tailored to the specific cancer classification task.
Model Training and Optimization: Freeze the initial layers of ResNet50 to preserve general feature extraction capabilities while training only the final layers on the FCGR-transformed genomic data. Use appropriate regularization techniques to prevent overfitting given the typically limited genomic dataset sizes.
Performance Evaluation: Assess model accuracy using standard classification metrics through cross-validation. Compare performance against alternative approaches including fully connected networks and different FCGR parameters (e.g., FCGR5 vs. FCGR6) to validate the optimal configuration.
Workflow Visualization of Transfer Learning Methodologies
cfMethylPre Framework Workflow
FCGR and ResNet Integration Workflow
Essential Research Reagents and Computational Tools
Successful implementation of transfer learning approaches for cancer detection from DNA sequences requires specific research reagents and computational resources. The table below details the essential components referenced in the experimental protocols.
Table 3: Essential Research Reagents and Computational Tools for Transfer Learning in Cancer Detection
| Category | Resource | Specification/Parameters | Function in Research |
|---|---|---|---|
| Genomic Data Resources | Bulk DNA Methylation Data | 2,801 samples across 82 cancer types and normal controls | Pretraining foundation for transfer learning models |
| cfDNA Methylation Profiling Data | Patient-derived circulating cell-free DNA | Target data for fine-tuning and specialized cancer detection | |
| Gene Sequences | Cancer-related genes from databases | Raw input for sequence-based classification approaches | |
| Computational Frameworks | Deep Learning Framework | TensorFlow/PyTorch with transfer learning capabilities | Model development, training, and implementation |
| Pre-trained Language Models | DNA sequence-trained embeddings | Enhanced feature representation integrating sequence context | |
| FCGR Algorithm | K-mer frequency calculation (FCGR5, FCGR6) | Transformation of DNA sequences into numerical representations | |
| Model Architectures | ResNet50 | Pre-trained on ImageNet, modified final layers | Feature extraction from FCGR-transformed genomic data |
| Custom CNN Architectures | Tailored for methylation data analysis | Specialized processing of methylation patterns | |
| Analysis Tools | DeepInsight Methodology | Non-image to image data transformation | Compatibility with computer vision models |
| SVM Classifier | Linear or RBF kernel | Final classification layer for cancer type prediction |
The effective utilization of these resources requires careful consideration of their complementary roles within the transfer learning pipeline. Genomic data resources form the foundation, with large-scale bulk data enabling robust pre-training and specialized cfDNA data facilitating domain adaptation. The computational frameworks provide the infrastructure for implementing complex deep learning approaches, while specialized model architectures offer the structural capacity to learn hierarchical representations from genomic data. Finally, analysis tools like DeepInsight and SVM classifiers enable the transformation and interpretation of features for final cancer detection and classification tasks.
The integration of these components into a cohesive workflow, as visualized in the previous section, enables researchers to leverage pre-trained knowledge while specializing in the nuances of cancer genomics. This approach has consistently demonstrated superior performance compared to models trained exclusively on limited cancer-specific datasets, highlighting the practical value of transfer learning in advancing genomic medicine for oncology applications.
Navigating Real-World Challenges: Data, Design, and Model Optimization
Addressing Low ctDNA Fraction and Signal-to-Noise Ratio in Early-Stage Detection
The analysis of circulating tumor DNA (ctDNA) present in patient blood samples represents a transformative, non-invasive approach for early cancer detection, treatment monitoring, and minimal residual disease assessment [10] [53]. The fundamental challenge in early-stage cancer detection lies in the extremely low abundance of tumor-derived DNA fragments within the total cell-free DNA (cfDNA) pool. In patients with early-stage or localized disease, ctDNA often comprises less than 0.1% of total cfDNA, which translates to potentially fewer than 15 tumor-derived molecules in a standard blood sample [53]. This minimal signal exists amidst high background noise from healthy cell-derived cfDNA, creating a significant signal-to-noise ratio (SNR) challenge that demands sophisticated technological and computational solutions [54].
This Application Note outlines integrated experimental and computational protocols to overcome these limitations, enabling robust ctDNA detection even at ultralow tumor fractions.
Quantitative Landscape of the Detection Challenge
Table 1: ctDNA Abundance and Detection Limits Across Cancer Stages
| Disease Context | Typical ctDNA Fraction | Tumor-Derived Molecules per 10 mL Blood* | Primary Detection Challenges |
|---|---|---|---|
| Advanced/Metastatic Cancer | ≥5% - 10% | ~750 - 1,500 molecules | Clonal hematopoiesis; Technical artifacts |
| Locally Advanced Cancer | ~1% | ~150 molecules | Background cfDNA noise; Limited tumor material |
| Early-Stage Cancer | ≤0.1% - 1.0% | <15 - 150 molecules | Extremely low SNR; Molecular scarcity |
| Minimal Residual Disease (MRD) | ≤0.1% | <15 molecules | Near-limit of detection; False negatives |
| Precancerous Lesions | ≤0.01% | ~1-2 molecules | Below conventional LOD |
Calculation based on approximately 15,000 haploid genome equivalents isolated from 5 mL of plasma [53].
Table 2: Performance Comparison of Current ctDNA Detection Technologies
| Technology | Theoretical LOD (VAF) | Key Strengths | Key Limitations | Reported Early-Stage Sensitivity |
|---|---|---|---|---|
| Digital Droplet PCR (ddPCR) | 0.01% - 0.1% [53] | High sensitivity for known variants; Quantitative | Limited multiplexing; Requires prior variant knowledge | Not broadly applicable for de novo detection |
| Hybrid Capture NGS (CAPP-Seq) | ~0.02% - 0.05% [53] | Flexible panel design; Broad genomic coverage | Expensive for high depth; Complex data analysis | Varies by cancer type and panel design |
| Whole-Genome Sequencing (Shallow) | ~5% - 10% (for CNA detection) [55] | Genome-wide view; No prior knowledge needed | Low sensitivity for SNVs at low coverage | 94.9% sensitivity (multimodal TAPS WGS, symptomatic cohort) [55] |
| TAPS-Based WGS (80x) | ~0.7% (in silico validation) [55] | Simultaneous genome/methylome analysis; Less DNA damage | New methodology; Limited clinical validation | 86% AUC at 0.7% TF [55] |
| Machine Learning-Enhanced WGS | Not explicitly stated | Learns complex patterns from high-dimensional data | Requires large training datasets; Complex validation | 85% sensitivity (CRC, stages I/II) at 85% specificity [56] |
| RCA-PEG-FET Biosensor | Single-base mutation in 10,000x WT background [54] | Ultra-sensitive; Portable potential; Electrical readout | Early development; Limited clinical data | Successfully detected EGFR mutations in NSCLC patient serum [54] |
VAF: Variant Allele Frequency; LOD: Limit of Detection; SNV: Single Nucleotide Variant; CNA: Copy Number Aberration; TAPS: TET-Assisted Pyridine Borane Sequencing; RCA: Rolling Circle Amplification
Experimental Protocols for Enhanced ctDNA Detection
Protocol: Multimodal Whole-Genome TET-Assisted Pyridine Borane Sequencing (TAPS)
Principle: TAPS is a less-destructive alternative to bisulfite sequencing that enables simultaneous acquisition of genomic and methylomic data from the same DNA molecule, doubling the informative yield from precious cfDNA samples [55].
Procedure:
Sample Collection & cfDNA Extraction:
- Collect 8-20 mL of whole blood into cell-stabilizing tubes (e.g., Streck cfDNA BCT).
- Process within 14 days at room temperature or within 48 hours if using K2EDTA tubes [53].
- Isolate plasma via double centrifugation (1,600 × g for 20 min, then 16,000 × g for 10 min at 4°C).
- Extract cfDNA from 4-10 mL plasma using a silica-membrane-based kit (e.g., MagMAX cfDNA Isolation Kit). Elute in 20-50 µL of low-EDTA TE buffer.
- Quantify using fluorometry (e.g., Qubit dsDNA HS Assay).
Library Preparation for TAPS:
- Convert 10-50 ng of cfDNA into sequencing libraries using a ligation-based kit (e.g., NEBNext Ultra II DNA Library Prep Kit) with unique molecular identifiers (UMIs) to tag original molecules.
- TET Enzyme Oxidation: Incubate libraries with TET2 enzyme in a reaction buffer (e.g., 50 mM HEPES, 50 µM (NH4)2Fe(SO4)2, 1 mM α-ketoglutarate, 2 mM ascorbate, pH 8.0) for 2 hours at 37°C. This converts 5-methylcytosine (5mC) and 5-hydroxymethylcytosine (5hmC) to 5-carboxylcytosine.
- Pyridine Borane Reduction: Add pyridine borane complex to a final concentration of 0.5 M and incubate for 1 hour at 37°C. This reduces 5-carboxylcytosine to dihydrouracil, which is read as thymine during sequencing [55].
- Purify reactions using solid-phase reversible immobilization (SPRI) beads.
Sequencing:
- Perform deep (e.g., 80x) whole-genome sequencing on an Illumina platform using paired-end reads (2x150 bp recommended).
- Target 500-800 million read pairs per sample to ensure sufficient depth for joint genomic and epigenetic analysis.
Bioinformatic Processing:
- Alignment: Align reads to the human reference genome (hg38) using bisulfite-aware aligners (e.g., BWA-meth or HiSAT2).
- Variant Calling: Use a multisample caller (e.g., GATK Mutect2) with UMI processing to generate consensus reads and suppress errors.
- Methylation Calling: Call methylation states from TAPS conversion events using tools like TAPScaller or Methyldackel.
- Copy Number Analysis: Bin the genome into 1 kb non-overlapping windows. Count reads, correct for GC bias and mappability, and denoise using a panel of non-cancer controls to remove systematic artifacts [55].
Protocol: Machine Learning-Guided Analysis of Whole-Genome Sequencing Data
Principle: Machine learning (ML) models can integrate fragmentomic, copy number, and methylation features from WGS data to discern subtle cancer-specific patterns that are imperceptible through univariate analysis [10] [56].
Procedure:
Data Featurization:
- Fragmentomic Features: Generate a 1 kb binned genome. For each bin, calculate: read depth, fragment length distribution (mean, median, mode), and nucleosome positioning signals (e.g., 10-bp periodicity around dyads) [10].
- Coverage Features: From the binned read counts, compute GC-corrected and mappability-corrected coverage values. Perform principal component analysis (PCA) on a control panel to define and remove background noise [55].
- Methylation Features: Calculate the proportion of methylated cytosines in CpG context for each 1 kb bin or genic region.
- Variant Features: Count the number of somatic single-nucleotide variants and indels in each bin, normalized by base count.
Model Training with Confounder Control:
- Structure the problem as a binary classification (cancer vs. non-cancer). Use a cohort of 546 colorectal cancer patients (80% stage I/II) and 271 non-cancer controls as a representative training set [56].
- Feature Preprocessing: Standardize each feature by subtracting the mean and dividing by the standard deviation. Replace large outliers with the 99th percentile value.
- Dimensionality Reduction: Apply truncated Singular Value Decomposition (SVD) or PCA to the standardized feature matrix.
- Train Classifier: Use a Support Vector Machine (SVM) or Logistic Regression model with hyperparameter optimization via random search in a cross-validated manner.
- Critical: Confounder-Aware Cross-Validation: Implement k-fold cross-validation where partitions are defined by potential confounders (e.g., processing batch, institution, age bin) rather than random splitting. This provides a more accurate estimate of real-world generalization performance [56].
Validation and Reporting:
- Apply the trained model to held-out test sets.
- Report mean Area Under the Curve (AUC) with 95% confidence intervals, and sensitivity at a fixed high specificity (e.g., 85%).
Protocol: RCA-PEG-FET Biosensor for Ultrasensitive Mutation Detection
Principle: This protocol combines isothermal Rolling Circle Amplification (RCA) for specific mutation recognition and signal amplification with an antifouling polyethylene glycol (PEG)-modified Field-Effect Transistor (FET) for highly sensitive electrical detection in complex biofluids [54].
Procedure:
Biosensor Functionalization:
- Fabricate a Carbon Nanotube (CNT) FET sensor with a HfOâ‚‚ insulating layer and an Ag/AgCl reference electrode.
- Incubate the CNT-FET channel with a solution of 1-pyrenebutanoic acid succinimidyl ester (10 µM in DMSO) for 1 hour to create an amine-reactive monolayer.
- Immerse the sensor in a solution of amine-terminated DNA capture probes (1 µM in PBS) complementary to the RCA product for 2 hours. The probes covalently attach to the surface.
- Passivate the surface by incubating with mPEG-succinimidyl valerate (5 mM) for 1 hour to form an antifouling layer that increases Debye length and reduces non-specific binding [54].
Padlock Probe Assay and RCA:
- Design: Create a padlock probe (PLP, ~100 nt) with ends complementary to the flanking region of a target mutation (e.g., EGFR L858R). The 5' and 3' ends should be immediately adjacent upon hybridization to the mutant template.
- Hybridization and Ligation: Mix cfDNA sample (1-10 ng) with PLP (10 nM) and T4 DNA ligase in appropriate buffer. Incubate at 37°C for 1 hour. The PLP circularizes only upon perfect match to the mutant allele.
- RCA: Add Phi29 DNA polymerase (10 U) and dNTPs (0.4 mM) to the ligation reaction. Incubate at 30°C for 90 minutes. This generates long single-stranded DNA concatemers (~10ⴠrepeats) from circularized PLPs.
Electrical Detection:
- Inject the RCA product directly onto the functionalized RCA-PEG-FET biosensor.
- Incubate for 15 minutes at room temperature to allow hybridization between the RCA concatemers and the surface-bound capture probes.
- Wash with a low-ionic-strength buffer (e.g., 1 mM PBS) to enhance the FET's charge-sensing capability.
- Measure the drain current (Id) versus gate voltage (Vg) transfer characteristic. A significant shift in the threshold voltage (V_T) indicates the presence of the negatively charged DNA backbone, confirming mutation detection.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Advanced ctDNA Research
| Category | Specific Product / Technology | Critical Function | Key Considerations |
|---|---|---|---|
| Sample Collection | Cell-Free DNA BCT Tubes (Streck) | Preserves blood sample integrity; prevents background release of genomic DNA from blood cells | Enables room temperature storage for up to 14 days [53] |
| cfDNA Extraction | MagMAX cfDNA Isolation Kit (Thermo Fisher) | High-efficiency isolation of short-fragment cfDNA from plasma | Optimized for 250 µL to 4 mL plasma input volumes |
| Library Prep | NEBNext Ultra II DNA Library Prep Kit (NEB) | Converts cfDNA into sequencing-ready libraries with high complexity | Compatible with UMI adapters for error suppression [56] |
| UMI Adapters | ThruPLEX Tag-seq Kit (Takara Bio) | Tags original DNA molecules with unique barcodes | Allows bioinformatic consensus calling to remove PCR/sequencing errors [57] |
| Targeted Enrichment | IDT xGen Lockdown Probes | Hybrid capture probes for targeted NGS; customizable for panel design | Used for hybrid capture-based ctDNA assays (e.g., FoundationOne Liquid CDx) [58] |
| Bisulfite Conversion | EZ DNA Methylation-Lightning Kit (Zymo Research) | Converts unmethylated cytosines to uracils for methylation analysis | Note: TAPS is a less-destructive alternative [55] |
| TAPS Chemistry | TET2 Enzyme & Pyridine Borane | Chemical conversion for methylation sequencing with less DNA damage | Preserves genetic information for simultaneous variant calling [55] |
| qPCR/ddPCR | ddPCR Mutation Detection Assays (Bio-Rad) | Absolute quantification of known mutant alleles; high sensitivity | Ideal for validating specific mutations found via NGS [53] |
| Biosensor Platform | Custom CNT-FET with PEG Coating | Ultrasensitive electrical detection of nucleic acids | Requires cleanroom fabrication; enables direct detection in serum [54] |
| BX517 | BX517, CAS:946843-63-6, MF:C15H14N4O2, MW:282.30 g/mol | Chemical Reagent | Bench Chemicals |
| CK7 | CK7, CAS:507487-89-0, MF:C14H12N6O2S, MW:328.35 g/mol | Chemical Reagent | Bench Chemicals |
Overcoming the challenges of low ctDNA fraction and poor signal-to-noise ratio in early-stage cancer detection requires a multi-faceted approach. As detailed in these protocols, the integration of less-destructive sequencing methods (TAPS), sensitive detection platforms (RCA-PEG-FET), and sophisticated machine learning algorithms that control for technical confounders provides a robust pathway toward clinically viable liquid biopsy applications. The consistent finding that a measured ctDNA tumor fraction ≥1% significantly increases confidence in negative liquid biopsy results underscores the importance of quantitative signal assessment in clinical interpretation [58]. These methodologies, collectively, push the boundaries of detection sensitivity and specificity, paving the way for the practical implementation of liquid biopsies in early cancer detection and minimal residual disease monitoring.
Class imbalance is a pervasive challenge in the development of machine learning (ML) models for cancer detection, where the number of negative samples (e.g., healthy tissues or benign cases) often significantly outweighs the number of positive samples (e.g., cancerous tissues or malignant cases). This imbalance can lead to models that are biased toward the majority class, resulting in poor diagnostic performance for the critical minority class. In oncology, where early and accurate detection of cancer is paramount, such bias can directly impact patient outcomes.
Synthetic data generation has emerged as a powerful strategy to counteract this issue by artificially creating new, realistic samples of the minority class, thereby balancing the dataset and allowing models to learn more discriminative features. This document provides detailed Application Notes and Protocols for three prominent techniques used to address class imbalance in cancer detection research: Gaussian Copula, Tabular Variational Autoencoder (TVAE), and Oversampling methods like SMOTE. Framed within the context of a broader thesis on the practical implementation of ML for cancer detection from DNA sequences, this guide is designed for researchers, scientists, and drug development professionals.
The following table summarizes the core characteristics, advantages, and disadvantages of the three techniques discussed in this protocol.
Table 1: Comparison of Class Imbalance Techniques
| Feature | Gaussian Copula | TVAE (Tabular Variational Autoencoder) | Oversampling (e.g., SMOTE) |
|---|---|---|---|
| Core Principle | Statistical model based on probability theory and correlation capture [59]. | Deep learning model using an encoder-decoder architecture to learn data distribution [60] [61]. | Interpolates between existing minority class instances in feature space to create new samples. |
| Data Type Suitability | Structured, tabular data (e.g., clinical features, gene expression counts). | Structured, tabular data with mixed data types (continuous & categorical) [60]. | Structured, tabular data. |
| Handling of Complex Relationships | Models linear correlations well; may struggle with highly non-linear relationships. | Capable of capturing complex, non-linear relationships in data [61]. | Limited to linear interpolations; may not capture complex manifolds. |
| Implementation Complexity | Low to Moderate. Based on statistical modeling. | Moderate to High. Requires defining neural network architecture and training [60]. | Low. Simple and widely available in libraries. |
| Computational Overhead | Relatively low. | High, due to neural network training, but can be accelerated with CUDA [60]. | Low. |
| Noted Application & Performance | Used to create synthetic training data for a regression model, which performed similarly to a model trained on real data [59]. | Outperformed in breast cancer prediction studies when combined with AutoML (H2OXGBoost) [62]. | A study on lung cancer prediction achieved 98.8% accuracy using SVM with SMOTE [63]. |
| Key Advantage | Preserves marginal distributions and pairwise correlations. Good interpretability. | High flexibility and capacity to model complex, high-dimensional tabular data. | Simple and fast to implement. No training required. |
| Key Disadvantage | May oversimplify complex, real-world data distributions. | Requires more data for training and careful hyperparameter tuning; can be a "black box." [60] | Can lead to overfitting and generation of noisy samples. |
Experimental Protocols
Protocol 1: Synthetic Data Generation using Gaussian Copula
This protocol is ideal for researchers beginning with synthetic data generation, as it provides a robust statistical foundation with relatively lower computational demands. It is well-suited for tabular datasets such as clinical risk factors or gene expression counts.
1. Research Reagent Solutions
- Software Library:
copulaslibrary in Python. - Dataset: Your pre-processed tabular dataset (e.g., a matrix of patients x gene expression values with associated cancer labels).
- Computing Environment: Standard Python environment (e.g., Jupyter Notebook) with
pandas,numpy, andcopulasinstalled.
2. Step-by-Step Methodology
- Step 1: Data Preparation. Isolate the minority class samples (e.g., all "malignant" cases) from your full dataset into a new DataFrame.
- Step 2: Model Initialization. Create an instance of the
GaussianMultivariatecopula model. - Step 3: Model Fitting. Fit the model on the isolated minority class data. The model will learn the marginal distribution of each variable and the covariance structure between them [59].
- Step 4: Synthetic Data Sampling. Use the fitted model to generate a number of synthetic samples sufficient to balance your dataset.
- Step 5: Dataset Reconstitution. Combine the newly generated synthetic data with the original majority class data to form a balanced dataset for downstream ML tasks.
3. Validation and Quality Control
- Statistical Comparison: Compare the descriptive statistics (mean, standard deviation, correlation matrix) of the synthetic data against the original minority class data to ensure fidelity.
- Dimensionality Reduction: Visualize both original and synthetic data using PCA or t-SNE to check for overlap in the latent space.
Protocol 2: Synthetic Data Generation using TVAE
Use this protocol when working with complex, high-dimensional tabular data containing both continuous and categorical variables, where simpler models like Gaussian Copula may be insufficient.
1. Research Reagent Solutions
- Software Library: The
sdv(Synthetic Data Vault) library, specifically theTVAESynthesizer[60]. - Dataset: Your pre-processed tabular dataset.
- Computing Environment: Python environment with
sdvandtorch(PyTorch) installed. CUDA is recommended for accelerated training [60].
2. Step-by-Step Methodology
- Step 1: Metadata Definition. Define a
metadataobject that describes the structure and data types of your table. - Step 2: Synthesizer Configuration & Creation. Instantiate the
TVAESynthesizerwith appropriate parameters [60]. - Step 3: Model Training. Fit the synthesizer on the entire training set or just the minority class. The model will learn a lower-dimensional, latent representation of the data and how to decode it back to the original feature space [61].
- Step 4: Synthetic Data Sampling. Generate the desired number of synthetic samples.
- Step 5: Balanced Dataset Creation. Combine the synthetic data with the original data.
3. Validation and Quality Control
- Loss Monitoring: Use
synthesizer.get_loss_values()to plot the training loss and ensure convergence [60]. - ML Efficacy Test: The most critical test is to train a classifier on a dataset augmented with TVAE-generated data and evaluate its performance on a held-out real test set, a method which has shown high accuracy in cancer prediction studies [62] [63].
Protocol 3: Data Augmentation for Image-Based Cancer Detection
While this guide focuses on DNA sequence and tabular data, many cancer diagnostics rely on medical imaging. The following workflow outlines a standard data augmentation pipeline for image-based cancer detection, which can improve model generalization.
The Scientist's Toolkit
Table 2: Essential Research Reagents and Software for Synthetic Data Generation
| Item | Function in Protocol | Example/Note |
|---|---|---|
copulas Python Library |
Implements the Gaussian Copula model for statistical synthetic data generation. | Key class: GaussianMultivariate [59]. |
sdv (Synthetic Data Vault) Python Library |
Provides a high-level interface for multiple synthetic data models, including TVAESynthesizer. |
Required for Protocol 2 [60]. |
| PyTorch | A deep learning framework; the computational backend for the TVAE model. | Enables GPU-accelerated training when cuda=True [60]. |
| Clinical & Genomic Datasets | The real, imbalanced data upon which synthetic data generation models are trained. | Examples: UCI Breast Cancer dataset [62], NLST cohort for lung cancer [64], gene expression datasets from RNA-Seq [65]. |
| Computational Resources (GPU) | Hardware accelerator for training deep learning models like TVAE. | Significantly reduces training time. Not strictly required for Gaussian Copula [60]. |
Effectively managing class imbalance is not merely an academic exercise but a practical necessity for building reliable ML models in oncology. Gaussian Copula offers a statistically sound and computationally efficient starting point, while TVAE provides a more powerful, flexible deep learning-based alternative for complex data. Oversampling methods like SMOTE serve as a simple baseline. The choice of technique depends on the specific data modality, complexity, and available computational resources. By integrating these synthetic data generation protocols into their workflow, researchers can significantly enhance the performance and generalizability of their cancer detection models, ultimately contributing to more accurate and earlier diagnoses.
In the high-stakes field of cancer detection from DNA sequences, the performance of machine learning models can directly impact diagnostic accuracy and patient outcomes. Model generalization—the ability to accurately predict outputs from unseen data—is particularly crucial for production models in clinical settings, as they must handle dynamic, real-world data while remaining robust to noise and errors [66]. Hyperparameter tuning stands as a critical step in achieving this generalization, significantly influencing how well algorithms learn from complex genomic data [67]. This paper presents practical protocols for implementing two fundamental hyperparameter optimization strategies—Grid Search and Cross-Validation—within the context of cancer genomics research. By providing structured methodologies and comparative analyses, we aim to equip researchers and drug development professionals with tools to build more reliable, high-performing predictive models for oncological applications.
Theoretical Foundation
Hyperparameters in Machine Learning
Hyperparameters are configuration variables set prior to the training process that govern how the model learns, significantly influencing its performance and ability to generalize [67] [68]. Unlike model parameters learned during training, hyperparameters are not derived from the data itself but are predetermined based on the practitioner's knowledge and optimization techniques. In deep learning models for sequence analysis, key hyperparameters include learning rate, batch size, number of epochs, optimizer selection, activation functions, and regularization strength [67]. Each hyperparameter controls different aspects of the learning process; for instance, the learning rate controls how much the model updates its weights after each step, while the number of epochs determines how many passes the model makes through the entire training dataset [67].
The Imperative of Tuning in Cancer Genomics
In cancer detection from DNA sequences, hyperparameter tuning transcends mere performance enhancement—it becomes essential for clinical validity. Genomic data presents unique challenges including high dimensionality, complex interaction effects, and significant class imbalances in cancer versus non-cancer sequences [66]. Proper tuning helps prevent both overfitting, where the model learns training data too well and fails on unseen clinical data, and underfitting, where the model fails to capture meaningful biological patterns [66]. The optimization process systematically navigates the vast space of potential hyperparameter value combinations to find the optimal configuration that maximizes detection accuracy while ensuring robust generalization to new patient data [67].
Core Methodologies
Cross-Validation Techniques
Cross-validation (CV) assesses a model's generalization capability by creating multiple dataset subsets (folds) and iteratively performing training and evaluation on different data splits [66]. This technique is particularly valuable in cancer genomics where dataset sizes may be limited due to the challenges of genomic data acquisition.
Table 1: Cross-Validation Techniques for Genomic Data
| Technique | Mechanism | Advantages | Ideal Use Cases |
|---|---|---|---|
| K-Fold [66] | Divides data into k equal folds; uses k-1 for training, 1 for testing | Full dataset utilization; reduced variance | Small genomic datasets; balanced classes |
| Stratified K-Fold [66] | Maintains class distribution proportions in each fold | Preserves imbalance structure; reliable metrics | Cancer classification with imbalanced outcomes |
| Holdout Method [66] | Simple single split (e.g., 80/20) | Computationally efficient; works with large data | Preliminary experiments; massive genomic datasets |
Hyperparameter Optimization Strategies
Hyperparameter optimization systematically searches for the optimal combination of hyperparameters that yields the best model performance [68].
Table 2: Hyperparameter Optimization Methods Comparison
| Method | Search Strategy | Computation Cost | Scalability | Best for Cancer Genomics When... |
|---|---|---|---|---|
| Grid Search [66] [68] | Exhaustive: tries all combinations in a predefined grid | High | Low | Hyperparameter space is small and well-understood |
| Random Search [66] [68] | Stochastic: samples random combinations from distributions | Medium | Medium | Initial exploration of large hyperparameter spaces |
| Bayesian Optimization [67] [69] | Probabilistic: uses surrogate model to guide search | High (but efficient) | Low-Medium | Computational resources limited; model training expensive |
Integrated Experimental Protocols
Protocol 1: Stratified K-Fold Cross-Validation for Cancer Classification
Purpose: To evaluate model generalization while maintaining class distribution in imbalanced cancer genomic datasets.
Materials:
- Labeled DNA sequence data (e.g., cancer vs. normal sequences)
- Python 3.7+ environment
- Scikit-learn library
- Computational resources (CPU/GPU based on dataset size)
Procedure:
- Data Preparation:
- Load genomic sequence features (e.g., k-mer frequencies, mutation profiles) and corresponding cancer labels
- Perform necessary preprocessing (normalization, feature scaling)
Stratified Split Configuration:
Cross-Validation Execution:
Performance Analysis:
- Calculate mean and standard deviation of performance metrics across folds
- Identify folds with significant performance variations for further investigation
Validation: Ensure each fold maintains approximately the same proportion of cancer-positive and cancer-negative samples as the complete dataset.
Protocol 2: Grid Search CV with Nested Cross-Validation
Purpose: To identify optimal hyperparameters while providing unbiased performance estimation in cancer prediction models.
Materials:
- Processed genomic dataset with features and labels
- Scikit-learn library
- Defined hyperparameter grid for selected algorithm
- High-performance computing resources for computationally intensive searches
Procedure:
- Hyperparameter Space Definition:
Nested CV Configuration:
Grid Search Implementation:
Final Model Training:
- Train final model on entire dataset using optimal hyperparameters identified through grid search
- Validate on held-out test set or through external validation cohort
Considerations: This protocol is computationally intensive but provides the most reliable performance estimation by preventing optimistic bias from tuning on the entire dataset.
Workflow Visualization
K-Fold Cross-Validation Workflow
Diagram 1: K-Fold Cross-Validation Workflow. The dataset is partitioned into K folds of approximately equal size. In each iteration, one fold serves as the test set while the remaining K-1 folds form the training set. Performance metrics from all iterations are aggregated to provide a robust estimate of model generalization capability [66].
Grid Search with Cross-Validation Methodology
Diagram 2: Grid Search with Cross-Validation Methodology. The algorithm systematically works through all possible combinations of hyperparameter values defined in the grid. For each combination, cross-validation is performed to evaluate performance. The best-performing parameter set is selected to train the final model [66] [68].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for Hyperparameter Tuning in Cancer Genomics
| Tool/Resource | Type | Function | Application in Cancer Research |
|---|---|---|---|
| Scikit-learn [66] [68] | Python Library | Provides GridSearchCV, RandomizedSearchCV, and cross-validation implementations | Accessible ML model development and optimization for genomic data |
| StratifiedKFold [66] | CV Algorithm | Maintains class distribution in splits | Crucial for imbalanced cancer vs. normal classification |
| Optuna/HyperOpt [70] | Optimization Frameworks | Bayesian optimization for hyperparameter tuning | Efficient search in high-dimensional spaces of deep learning models |
| TensorFlow/PyTorch [67] | Deep Learning Frameworks | Neural network implementation with GPU acceleration | Complex sequence model development for DNA analysis |
| TPOT [71] | AutoML Library | Automated ML pipeline optimization including hyperparameter tuning | Rapid prototyping of predictive models for biomarker discovery |
Case Study: Optimized Hybrid Model for Cervical Cancer Detection
A recent study demonstrated the practical efficacy of hyperparameter tuning in cancer diagnostics through the development of an optimized hybrid CNN-RNN model for cervical cancer detection [72]. Researchers combined convolutional neural networks (CNNs) for spatial feature extraction with recurrent neural networks (RNNs) for temporal analysis of cervical cancer images. Through rigorous grid search hyperparameter optimization, the hybrid model achieved a remarkable validation accuracy of 89.64% with low validation loss of 0.3222, significantly outperforming standalone models including CNN and MLP (~19%), RNN (59.28%), and LSTM (74.28%) [72]. The study exemplifies how systematic hyperparameter tuning can unlock synergistic potential in hybrid architectures, resulting in substantially improved diagnostic accuracy with balanced precision-recall characteristics critical for clinical application.
Performance Analysis and Discussion
Quantitative Comparison of Optimization Methods
Table 4: Empirical Performance Comparison on Cancer Genomic Datasets
| Optimization Method | Average Accuracy | Standard Deviation | Computational Time (Relative) | Best Application Context |
|---|---|---|---|---|
| Grid Search [68] | 85.3% | ± 2.1% | 1.0 (reference) | Small hyperparameter spaces (<50 combinations) |
| Random Search [68] | 84.2% | ± 2.8% | 0.6 | Initial exploration of large parameter spaces |
| Bayesian Optimization [67] [69] | 86.7% | ± 1.9% | 0.8 | Expensive model training; limited computational budget |
Practical Considerations for Genomic Data
When applying these techniques to cancer detection from DNA sequences, several domain-specific considerations emerge. Genomic data often exhibits high dimensionality with numerous features (e.g., SNP positions, k-mer frequencies) but limited samples, increasing the risk of overfitting [66]. Stratified cross-validation becomes essential to maintain representation of rare cancer subtypes across folds. Additionally, the computational intensity of grid search must be balanced against the potential clinical impact of improved accuracy. For large-scale whole genome sequence analysis, randomized search or Bayesian optimization may offer more practical alternatives to exhaustive grid search [67] [68].
Grid search and cross-validation represent foundational methodologies for developing robust machine learning models in cancer detection from DNA sequences. Through systematic implementation of these protocols—particularly stratified k-fold cross-validation for handling class imbalances and grid search with nested cross-validation for unbiased hyperparameter optimization—researchers can significantly enhance model generalization and diagnostic accuracy. The integrated workflows and analytical frameworks presented here provide practical guidance for advancing oncological predictive models from experimental concepts toward clinically applicable tools. As precision medicine continues to evolve, these hyperparameter optimization strategies will play an increasingly vital role in translating complex genomic data into reliable cancer diagnostics and therapeutic insights.
Mitigating Overfitting and Ensuring Generalizability in Genomic Data Models
The application of machine learning (ML) to genomic data for cancer detection represents a frontier in precision oncology. However, the high-dimensionality of genomic data, where the number of features (e.g., methylation sites, mutations) vastly exceeds the number of samples, creates a significant risk of overfitting. This results in models that perform well on their training data but fail to generalize to new, unseen datasets or diverse clinical populations. The "black-box" nature of many complex models further complicates clinical trust and adoption [73]. This document outlines practical protocols and application notes for mitigating overfitting and ensuring the generalizability of genomic data models, framed within the context of a broader thesis on the practical implementation of ML for cancer detection from DNA sequences.
Several strategies have been successfully employed to combat overfitting in genomic models. The table below summarizes the quantitative outcomes of various approaches as demonstrated in recent literature.
Table 1: Quantitative Outcomes of Overfitting Mitigation Strategies in Genomic Studies
| Strategy | Specific Technique | Reported Performance | Key Outcome |
|---|---|---|---|
| Dimensionality Reduction | Machine Learning (ANOVA, LASSO) for methylation probe selection [74] | Reduced 850,000 probes to a final 9 probes. | AUC of 100% in initial set; 84% in external validation. |
| Quantum-Enhanced Models | Variational Quantum Circuit (VQC) in Swin Transformer [75] | 62.5% reduction in parameters vs. classical layer. | Balanced Accuracy (BACC) improved by 3.62% in external validation. |
| Interpretable ML Models | XGBoost on open chromatin data [76] | Not Specified | Provided a robust and interpretable framework for cfDNA-based cancer detection. |
| Advanced Sequencing & DL | Deep Methylation Sequencing & ML [77] | Detection at dilution factors of 1 in 10,000. | 52-81% sensitivity (stages IA-III) at 96% specificity. |
Detailed Experimental Protocols
Protocol 1: Dimensionality Reduction for Methylation-Based Detection
This protocol details the methodology for identifying a minimal set of highly predictive DNA methylation probes for ovarian cancer detection, as exemplified by Gonzalez Bosquet et al. [74].
1. Sample Preparation and Data Acquisition:
- Tissue Samples: Obtain 99 high-grade serous ovarian cancer (HGSC) tissue samples and 12 normal fallopian tube control samples from a well-annotated biobank.
- Methylation Profiling: Process the DNA samples using the Illumina Infinium MethylationEPIC BeadChip Array, which Interrogates over 850,000 methylation sites (CpG probes) across the genome.
2. Initial Feature Reduction with Deep Learning:
- Tool: Utilize MethylNet, a deep learning tool, for initial feature reduction.
- Process: Input the 850,000+ methylation probes. MethylNet will perform non-linear dimensionality reduction, capturing the most salient methylation patterns associated with the cancer phenotype.
3. Statistical Feature Selection:
- Univariate Analysis: Perform univariate ANOVA analyses on the reduced feature set from MethylNet to identify probes with statistically significant differences between cancer and normal groups.
- Multivariate Regularization: Apply LASSO (Least Absolute Shrinkage and Selection Operator) regression to the significant probes from the ANOVA. LASSO penalizes the absolute size of regression coefficients, driving coefficients of less important features to zero, resulting in a sparse model with a minimal set of predictive probes (e.g., the final 9 probes).
4. Model Validation:
- Internal Validation: Use cross-validation on the initial dataset to assess performance.
- External Validation: Validate the final model (with the 9 probes) on an independent, geographically distinct dataset (e.g., GSE65820 from Australia). This is critical for testing generalizability.
Protocol 2: Integrating Quantum Circuits to Reduce Parameters
This protocol describes the integration of a Variational Quantum Circuit (VQC) into a classical deep learning architecture to reduce model complexity and mitigate overfitting, as demonstrated in breast cancer screening [75].
1. Base Model Setup:
- Architecture: Employ a Swin Transformer model as a feature extractor. Initialize the model with weights pre-trained on a large-scale dataset like ImageNet (transfer learning).
- Input: Use Full-Field Digital Mammography (FFDM) images, cropped to regions of interest (ROI) and resized to 224x224 pixels. Apply standard data augmentation (flipping, rotation, color jitter).
2. Hybrid Quantum-Classical Classifier Design:
- Replacement: Remove the final fully-connected (classical) classification layer of the Swin Transformer.
- Quantum Layer: Replace it with a Variational Quantum Circuit (VQC).
- Quantum Embedding: Encode the features extracted by the Swin Transformer into a quantum state using an embedding method (e.g., Angle Embedding).
- Variational Circuit: Apply a series of parameterized quantum gates (e.g., rotational gates) whose parameters are optimized during training.
- Measurement: Measure the quantum state to obtain a classical output for classification.
- Parameter Efficiency: The VQC requires only O(KN) parameters compared to the O(N²) parameters of the replaced classical layer, where K is the number of quantum gates and N is related to the number of qubits.
3. Model Training and Evaluation:
- Training: Train the entire hybrid network (Swin Transformer + VQC) end-to-end using a standard optimizer (e.g., Adam) and loss function (e.g., cross-entropy).
- Evaluation:
- Compare accuracy and loss on training and validation sets against the classical Swin Transformer to monitor overfitting.
- Perform external validation on a separate dataset (e.g., INbreast database) to assess generalizability and report metrics like Balanced Accuracy (BACC).
Protocol 3: Interpretable ML on Cell-Free DNA Chromatin Data
This protocol uses an interpretable ML model trained on cell-free DNA (cfDNA) chromatin features to detect cancer, providing both accuracy and biological insights [76].
1. Sample Processing and Sequencing:
- Sample Collection: Isolate plasma from blood samples collected from breast cancer patients and healthy donors.
- cfDNA Extraction: Purify cell-free DNA (cfDNA) from the plasma.
- Library Preparation and Sequencing: Prepare next-generation sequencing libraries from the cfDNA and sequence to a sufficient depth (e.g., ~30 million reads).
2. Feature Extraction from Open Chromatin:
- Reference Data: Obtain cell type-specific (e.g., from cancer cell lines, CD4+ T cells) open chromatin region data from assays like ATAC-seq.
- Signal Mapping: Map the sequenced cfDNA fragments to the genome and calculate read counts (enrichment signals) at these pre-defined open chromatin regions. These enrichment values serve as the features for the model.
3. Model Training with Explainable AI:
- Algorithm: Train an XGBoost (eXtreme Gradient Boosting) model using the open chromatin enrichment features to classify samples as "cancer" or "healthy."
- Advantage: XGBoost is a powerful, yet relatively interpretable, tree-based model that provides feature importance scores.
- Interpretation: Use SHAP (SHapley Additive exPlanations) or similar methods to analyze the trained model. This identifies which specific genomic loci (open chromatin regions) most strongly contributed to the prediction, offering a biological explanation for the model's decision and helping to validate it against known cancer biology.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for Genomic Cancer Detection Models
| Item Name | Function / Application | Specific Example / Note |
|---|---|---|
| Illumina Infinium MethylationEPIC BeadChip | Genome-wide methylation profiling at over 850,000 CpG sites. | Used for initial high-throughput methylation data acquisition [74]. |
| Targeted Methylation Sequencing Panel | For deep, cost-effective sequencing of a pre-defined set of methylation markers. | Enables ultrasensitive detection of circulating tumour DNA; key for MCED tests [5] [77]. |
| ATAC-seq Kit | Assay for Transposase-Accessible Chromatin with sequencing to map open chromatin regions. | Generates reference data for cell type-specific chromatin accessibility used in cfDNA analysis [76]. |
| Cell-free DNA Extraction Kit | Isolation of high-quality cfDNA from blood plasma. | Critical first step for all liquid biopsy-based genomic analyses [76] [78]. |
| H2O AutoML Platform | Automated machine learning platform for model selection, training, and tuning. | Streamlines the development of robust models, as demonstrated in cervical cancer prediction [79]. |
| Quantum Computing Simulator/Access | Software/Hardware for simulating or running hybrid quantum-classical algorithms. | Essential for developing and testing models like the Quantum-Enhanced Swin Transformer (QEST) [75]. |
Proving Efficacy: Model Validation, Benchmarking, and Clinical Readiness
In the field of machine learning (ML) for cancer detection, selecting appropriate performance metrics is not merely a technical formality but a critical determinant of clinical validity and utility. For applications involving DNA sequence analysis—such as circulating tumor DNA (ctDNA) detection or cancer risk prediction from genomic data—metrics translate algorithmic performance into clinically actionable insights. The choice of metric directly influences how model performance is interpreted against the backdrop of clinical consequences, where false negatives can delay life-saving interventions and false positives lead to unnecessary, invasive follow-ups [80] [81]. This document provides a structured framework for selecting and interpreting accuracy, ROC-AUC, and sensitivity/specificity within the specific context of cancer detection research, complete with experimental protocols and resource guides for practitioners.
Core Metric Definitions and Clinical Interpretations
The following table summarizes the key performance metrics, their calculations, and—most importantly—their clinical significance in cancer detection.
Table 1: Core Performance Metrics for Cancer Detection Models
| Metric | Formula | Clinical Interpretation | Strength in Cancer Context | Limitation in Cancer Context |
|---|---|---|---|---|
| Accuracy | (TP + TN) / (TP + FP + FN + TN) [82] | The overall proportion of correct cancer and non-cancer classifications. | Intuitive; useful for balanced datasets where both cancer and healthy cases are equally represented. | Highly misleading with class imbalance (e.g., low cancer prevalence in screening populations), as it can be inflated by correctly predicting the majority "healthy" class [82]. |
| Sensitivity (Recall) | TP / (TP + FN) [83] | The ability to correctly identify patients who have cancer. | Primary goal in early detection: Minimizes false negatives, ensuring cancer cases are not missed. A high sensitivity is often the primary target for screening tests [55]. | Does not consider false positives. A test can have 100% sensitivity by classifying everyone as positive, which is clinically impractical. |
| Specificity | TN / (TN + FP) [83] | The ability to correctly identify patients without cancer. | Reduces unnecessary psychological stress and invasive diagnostic procedures (e.g., biopsies) caused by false positives [84]. | Does not consider false negatives. A high-specificity test might miss early-stage cancers. |
| ROC-AUC | Area Under the Receiver Operating Characteristic Curve [83] | Measures the model's ability to separate cancer and non-cancer classes across all possible classification thresholds. | Excellent for assessing overall ranking capability; indicates the probability that a random cancer sample is ranked higher than a random non-cancer sample [82]. | Can be overly optimistic for imbalanced datasets, as the large number of true negatives inflates the False Positive Rate denominator [82]. |
| Precision (PPV) | TP / (TP + FP) | When a test predicts cancer, the probability that it is correct. | Critical for confirmatory tests and triage, as it relates to the cost and burden of false positives. | Highly dependent on disease prevalence. |
Experimental Protocols for Metric Evaluation
This section outlines detailed protocols for evaluating machine learning models in cancer detection, from data preparation to metric calculation, with a focus on ctDNA methylation analysis as a representative and high-impact application.
Protocol 1: Multi-Layered ctDNA Methylation Analysis Pipeline
This protocol is adapted from automated systems for dissecting ctDNA methylation landscapes for early cancer detection [85].
1. Objective: To build and evaluate a model for cancer detection via ctDNA methylation patterns, utilizing a multi-layered evaluation pipeline that integrates a dynamic "HyperScore" for final classification.
2. Data Ingestion & Normalization:
- Input: Raw whole-genome bisulfite sequencing (WGBS) reads (FASTQ format) from plasma samples of cancer patients and healthy controls [85].
- Processing:
- Quality Control: Use FastQC and Trimmomatic to filter low-quality reads and adapters.
- Alignment: Align bisulfite-treated reads to a reference genome (e.g., hg38) using Bismark.
- Methylation Calling: Determine methylation status at each cytosine using a Bayesian method to generate a methylation map.
- Normalization: Apply the Trimmed Mean of M-values (TMM) method to correct for systematic technical biases across samples [85].
3. Feature Extraction & Semantic Decomposition:
- Transcription Factor Binding Site (TFBS) Extraction: Identify TFBS motifs within differentially methylated regions using tools like MEME.
- Gene Annotation & Pathway Mapping: Link methylated regions to their nearest genes and correlate methylation status with gene expression data from public repositories (e.g., TCGA). Construct a network of known cancer pathways (e.g., from KEGG, Reactome) to contextualize findings [85].
4. Multi-Layered Model Evaluation & HyperScore Calculation: This core module assesses the discriminatory power of methylation patterns through several logical and statistical layers.
- Logical Consistency Engine: Use a logic programming framework (e.g., SWI-PROLOG) encoded with known cancer pathway rules to check for contradictory methylation signals (e.g., simultaneous activation and repression of the same gene) [85].
- Novelty Analysis: Compare detected methylation profiles against a vector database of known profiles using cosine similarity to identify novel cancer signatures.
- Impact Forecasting: Use mechanistic models (e.g., differential equations) to predict patient outcomes based on the identified methylation features.
- Score Fusion & HyperScore Calculation: Integrate scores from the above layers (V) into a final, dynamically weighted HyperScore.
HyperScore = 100 × [1 + (σ(β ⋅ ln(V) + γ)) ᵞ]whereσis the sigmoid function, andβ, γ, κare tuned parameters that adjust the sensitivity and power of the score based on biomarker correlations [85].
5. Performance Metric Calculation:
- Apply a threshold to the continuous HyperScore to assign positive (cancer) or negative (healthy) class labels.
- Using the resulting confusion matrix, calculate Accuracy, Sensitivity, Specificity, and Precision.
- To calculate ROC-AUC, use the raw, threshold-independent HyperScore as the predictor and the ground truth (clinical diagnosis) as the target. Plot the ROC curve by varying the classification threshold and compute the area underneath [82] [83].
The workflow for this protocol is illustrated below.
Protocol 2: Benchmarking with a Curated Cancer Risk Dataset
This protocol uses a structured dataset combining lifestyle and genetic factors to provide a clear framework for comparing multiple ML models [84].
1. Objective: To benchmark the performance of multiple supervised learning algorithms on a curated cancer risk dataset, evaluating them across standard metrics to identify the most suitable model for deployment.
2. Dataset Preparation:
- Source: Utilize a structured dataset (e.g., the Cancer Prediction Dataset) with features such as age, gender, BMI, smoking status, genetic risk level, and personal cancer history [84].
- Preprocessing:
- Handle missing values using imputation.
- Encode categorical variables (e.g., smoking status) numerically.
- Scale numerical features (e.g., age, BMI) to a standard range.
- Split data into training (70%), validation (15%), and a held-out test set (15%), ensuring stratification to maintain the class distribution.
3. Model Training & Hyperparameter Tuning:
- Algorithms: Train a diverse set of classifiers, including Logistic Regression, Decision Trees, Random Forest, Support Vector Machines, and advanced ensemble methods like Categorical Boosting (CatBoost) [84].
- Tuning: Use the validation set and techniques like stratified cross-validation to tune hyperparameters for each model, optimizing for the target metric (e.g., ROC-AUC).
4. Evaluation on Held-Out Test Set:
- Generate predictions (both class labels and probability scores) for the unseen test set.
- For each model, compute the suite of metrics outlined in Table 1.
- Compare Models: Rank models based on the primary metric of interest. For instance, a study might find CatBoost achieving the highest test accuracy and F1-score, outperforming other models [84].
The following diagram outlines the key decision points for metric selection based on the clinical and dataset context.
The Scientist's Toolkit: Essential Research Reagents & Computational Solutions
Table 2: Key Reagents and Tools for Cancer Detection ML Research
| Category | Item | Function / Application | Example in Context |
|---|---|---|---|
| Wet-Lab & Sequencing | TET-Assisted Pyridine Borane Sequencing (TAPS) [55] | A less-destructive method for base-resolution methylation sequencing that preserves DNA for simultaneous genomic and methylomic analysis. | Used in multimodal cfDNA WGS for sensitive cancer signal detection, avoiding the DNA degradation of bisulfite sequencing [55]. |
| Whole-Genome Bisulfite Sequencing (WGBS) [85] | The traditional method for creating genome-wide, base-resolution methylation maps. Treats DNA with bisulfite, converting unmethylated cytosines to uracils. | Used as input for automated ctDNA methylation analysis pipelines [85]. | |
| Bioinformatics & Data Processing | Bismark [85] | A aligner and methylation caller specifically designed for bisulfite-converted sequencing reads. | Used to align WGBS reads and call methylation status in ctDNA analysis [85]. |
| FastQC & Trimmomatic [85] | Tools for quality control and adapter trimming of raw sequencing reads. | Ensures high-quality, clean data is fed into the analysis pipeline [85]. | |
| MEME Suite [85] | A toolkit for motif-based sequence analysis, used to discover transcription factor binding sites. | Identifies potential TFBS motifs within methylated regions for network construction [85]. | |
| DRAGEN Secondary Analysis [86] | A highly accelerated, accurate platform for secondary analysis of NGS data, including alignment and variant calling. | Used for rapid whole-genome sequencing analysis of tumor-normal pairs [86]. | |
| Model Evaluation & Validation | Precision-Recall (PR) Curves [82] | A plot of precision vs. recall for different probability thresholds, highly recommended for imbalanced datasets. | More informative than ROC curves when evaluating a cancer detection model on a screening population with low disease prevalence [82]. |
| Stratified Cross-Validation [84] | A resampling technique that preserves the percentage of samples for each class in every training/validation fold. | Ensures reliable performance estimation on imbalanced cancer datasets [84]. |
Performance Considerations and Best Practices
- Context is King: No single metric is universally best. The choice must be driven by the clinical context. For early cancer screening, where missing a case (false negative) is critical, Sensitivity is paramount. For confirmatory testing or triaging patients for invasive procedures, minimizing false alarms becomes crucial, warranting a focus on Specificity and Precision [81].
- The Imbalance Problem: In asymptomatic screening populations, cancer prevalence is low (e.g., 1-5%). In such scenarios, Accuracy is a poor metric, and ROC-AUC can be overly optimistic. Instead, prioritize Precision-Recall (PR) curves and F1-score/F-beta scores, which focus on the performance of the positive (cancer) class [82].
- Report a Suite of Metrics: Always report multiple metrics (e.g., Sensitivity, Specificity, PPV, NPV, AUC) to provide a comprehensive view of model performance from different clinical angles [84] [80].
- Validate with Real-World Data: Ultimately, model performance must be validated on independent, real-world datasets that reflect the target patient population to ensure generalizability beyond the initial research cohort [80] [55].
The integration of artificial intelligence (AI) in oncology represents a paradigm shift in cancer diagnostics, offering unprecedented opportunities for early detection and personalized treatment strategies. This document provides a structured framework for benchmarking machine learning (ML) and deep learning (DL) models against each other and existing clinical methods within the specific context of cancer detection from DNA sequences. For researchers and drug development professionals, rigorous benchmarking is a critical step in translating algorithmic innovations into clinically viable tools that can improve patient outcomes [87]. The following sections detail performance metrics, experimental protocols, and essential resources to standardize this evaluation process, with a focus on practical implementation.
Performance Benchmarking Tables
Table 1: Comparative Performance of ML, DL, and Clinical Methods in Cancer Detection
| Cancer Type | Method Category | Specific Model/Technique | Key Performance Metrics | Reference/Notes |
|---|---|---|---|---|
| Various Cancers (via DNA) | Deep Learning | CNN-based Models for DNA Sequencing Data | Accuracy up to 100% in controlled studies; demonstrates high feature learning capability [88]. | Performance highly dependent on data quality and volume. |
| Machine Learning | SVM, Random Forests | Maximum achieved accuracy: 99.89% [88]. | Relies on manually designed features [89]. | |
| Clinical Method | Multicancer Early Detection (MCED) Blood Test | Detected cancer signals up to 3 years before clinical diagnosis in a proof-of-concept study [90]. | Not yet FDA-approved for widespread use; requires further validation. | |
| Colorectal Cancer | Statistical Model (Trends) | ColonFlag Model (Uses FBC trends) | Pooled c-statistic = 0.81 for 6-month risk prediction [91]. | Meta-analysis of 4 validation studies. |
| Skin Cancer | Deep Learning | Convolutional Neural Networks (CNN) | Accuracy: 92.5%, Sensitivity: 91.8%, Specificity: 93.1% [92]. | Superior performance compared to traditional ML. |
| Machine Learning | SVM, Random Forests | Lower accuracy compared to CNN [92]. | ||
| Gastric Cancer | Deep Learning | CNN on Pathology Images | Accuracy over 95% in detection tasks [89]. | Most commonly used DL architecture in pathology. |
Table 2: Analysis of Model Strengths and Limitations
| Method | Primary Strength | Primary Limitation | Data Dependency | Interpretability |
|---|---|---|---|---|
| Traditional ML (e.g., SVM, Random Forests) | High performance with well-curated features; less computationally intensive than DL [89]. | Performance limited by quality of manual feature engineering [89]. | Lower volume required, but high-quality feature curation is essential. | Generally higher; models are often more transparent. |
| Deep Learning (e.g., CNN) | Automatically learns complex feature representations from raw data; state-of-the-art accuracy in many tasks [87] [89]. | "Black box" nature raises concerns about interpretability and trust in clinical settings [92]. | Requires very large, annotated datasets for training [87]. | Low; models are complex and difficult to interpret (the "black box" problem). |
| Clinical Blood Tests (Trend Analysis) | Utilizes routinely collected, low-cost data (e.g., full blood count); can identify risk from trends within the normal range [91]. | Models are not available for most cancer sites; often lack external validation and calibration assessment [91]. | Relies on longitudinal data from electronic health records. | High; trends in specific biomarkers (e.g., hemoglobin) are clinically understandable. |
Experimental Protocols for Benchmarking
Protocol 1: Benchmarking ML/DL Models on DNA Sequence Data from Cell-Free DNA
Objective: To compare the sensitivity and specificity of ML and DL models in detecting cancer-derived mutations from whole-genome sequencing data of cell-free DNA (cfDNA) [93].
Workflow Diagram: cfDNA Analysis for Cancer Detection
Materials:
- Patient Plasma Samples: Collected from individuals with cancer and matched healthy controls [93].
- Reference DNA: Genomic DNA from matched normal tissue (e.g., lymphoblastoid cell lines) or healthy donor samples to establish a baseline [94].
- cfDNA Extraction Kit: For isolating circulating DNA from plasma.
- Next-Generation Sequencing (NGS) Platform: For high-throughput whole-genome sequencing of cfDNA libraries [93].
- Computational Resources: High-performance computing cluster with sufficient storage and memory for NGS data analysis.
Methodology:
- Sample Preparation and Sequencing:
- Extract cfDNA from patient plasma using a standardized kit.
- Prepare sequencing libraries from the extracted cfDNA.
- Perform whole-genome sequencing on an NGS platform to a sufficient depth (e.g., 30x-60x) to detect low-frequency variants [93].
- Bioinformatic Processing:
- Feature Engineering and Model Training:
- For traditional ML models (e.g., SVM, Random Forest), extract features from the aligned BAM and VCF files. These may include: mutation allele frequency, read depth, local sequence context, and genomic annotation of the variant.
- For DL models (e.g., CNNs), the models can be trained on more raw data representations, such as stacked read alignments (images) around genomic coordinates of interest, allowing for automatic feature learning [88].
- Split data into training, validation, and held-out test sets. Train ML and DL models on the training set.
- Benchmarking and Evaluation:
- Apply all trained models to the same held-out test set.
- Calculate key performance metrics: Accuracy, Sensitivity (recall), Specificity, Precision, and Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) curve.
- Compare the performance of ML vs. DL models against each other and against a baseline (e.g., a simple statistical threshold).
Protocol 2: Validating Against a Somatic Mutation Reference Standard
Objective: To assess the false positive and false negative rates of a novel detection pipeline using a genetically defined reference sample with a known ground truth of somatic mutations [94].
Workflow Diagram: Validation with Reference Samples
Materials:
- Reference Cell Lines: Paired tumor and normal genomic DNA (gDNA) samples, such as the HCC1395 breast cancer cell line and the matched HCC1395BL lymphoblastoid cell line, which are highly heterogeneous and enriched for somatic alterations [94].
- Gold Standard Call Set: The validated set of somatic mutations for the reference sample, available from repositories like NCBI's SRA (SRP162370) [94].
Methodology:
- Data Generation: Sequence the gDNA from the reference tumor and normal cell lines using your established NGS pipeline (WGS or WES).
- Variant Detection: Process the sequencing data through your novel ML/DL pipeline to generate a set of called somatic mutations.
- Comparison to Benchmark: Compare your pipeline's output to the gold standard call set.
- Performance Calculation:
- False Negative Rate (FNR): Proportion of mutations in the gold standard set that were missed by your pipeline.
- False Positive Rate (FPR): Proportion of mutations called by your pipeline that are not present in the gold standard set.
- This provides an unbiased measure of your method's accuracy compared to other published pipelines that have been validated on the same standard.
| Resource Category | Specific Item | Function & Application | Example / Source |
|---|---|---|---|
| Reference Samples & Data | Genomic DNA Reference Samples | Provide a genetically defined ground truth for benchmarking variant callers and sequencing pipelines [94]. | HCC1395/HCC1395BL cell lines from ATCC [94]. |
| Gold Standard Somatic Call Sets | A validated list of known mutations in a reference sample; serves as the benchmark for calculating FPR/FNR [94]. | Available for HCC1395 via NCBI's SRA (SRP162370) [94]. | |
| Large-Scale Genomic Databases | Provide large, well-curated datasets for training and testing ML/DL models on diverse cancer types [95]. | The Cancer Genome Atlas (TCGA) [95]. | |
| Computational Tools | Sequence Aligner | Aligns raw sequencing reads to a reference genome. | BWA-MEM [94]. |
| Somatic Variant Caller | Identifies somatic mutations from aligned sequencing data of tumor-normal pairs. | Strelka2, VarDict, MuSE [94]. | |
| Deep Learning Framework | Provides the programming environment to build, train, and test DL models (e.g., CNNs). | TensorFlow, PyTorch. | |
| Experimental Materials | Cell-Free DNA Extraction Kits | Isolate circulating DNA from blood plasma for liquid biopsy applications [93]. | Various commercial suppliers. |
| Next-Generation Sequencers | Generate the high-throughput sequencing data that serves as the input for analysis pipelines. | Platforms from Illumina, Thermo Fisher, etc. |
The transition of ML and DL models from research benchmarks to clinical tools for cancer detection hinges on rigorous, standardized evaluation. The protocols and resources outlined herein provide a roadmap for researchers to conduct such assessments, focusing on the critical metrics and validation strategies that underpin clinical credibility. Future progress will depend not only on algorithmic innovation but also on addressing challenges such as model interpretability, the need for large and diverse datasets, and the execution of robust external validation studies to ensure generalizability across populations [87] [91] [89].
The Role of Explainable AI (XAI) and SHAP Analysis for Model Interpretability and Biomarker Discovery
The application of artificial intelligence (AI) in oncology has ushered in a transformative era for cancer diagnostics and biomarker discovery. Deep learning and machine learning models are increasingly deployed to find complex, non-intuitive patterns within vast and diverse datasets, from genomic sequences to medical images [96]. However, these sophisticated models are often perceived as "black boxes," whose decision-making processes are opaque and difficult to interpret. This lack of transparency poses a significant barrier to clinical adoption, as healthcare professionals require understandable reasoning to trust and act upon AI-generated predictions [97] [98]. Explainable AI (XAI) addresses this critical challenge by making the workings of AI models transparent and interpretable to human experts.
Within the XAI toolkit, SHapley Additive exPlanations (SHAP) has emerged as a premier method for interpreting model outputs. Rooted in cooperative game theory, SHAP quantifies the contribution of each input feature (e.g., a specific gene's expression level or a lipid concentration) to a individual model prediction [97] [99]. By doing so, it bridges the gap between high-performance AI and clinical practicality. In the context of cancer research, SHAP and other XAI techniques are not merely diagnostic tools; they are powerful instruments for biomarker discovery. They enable researchers to move beyond simple prediction to identify and validate the specific molecular features that drive cancer classification, thereby uncovering new potential therapeutic targets and diagnostic biomarkers [98] [99]. This document outlines practical protocols and applications for integrating XAI and SHAP into cancer biomarker discovery workflows.
Key Applications and Performance of XAI in Cancer Research
The integration of XAI, particularly SHAP analysis, has led to significant advancements across various cancer types and data modalities. The table below summarizes key findings from recent studies that successfully employed these techniques.
Table 1: Summary of XAI and SHAP Applications in Cancer Biomarker Discovery
| Cancer Type | Data Modality | Key XAI Finding | Model Performance | Citation |
|---|---|---|---|---|
| Breast Cancer | Gene Expression & Proteomics | SHAP identified distinct gene signatures for ER, PR, and HER2 status, clarifying decision drivers. | CNN models achieved 89% (ER) and 86% (PR) accuracy; HER2 was more challenging (72%). [98] | |
| Breast Cancer | Cytology (FNA) Image Features | SHAP revealed "concave points" of cell nuclei as the most influential feature for classification. | Deep neural network achieved an accuracy of 99.2% and precision of 100%. [97] | |
| Liver Cancer | Serum Lipidomics | SHAP identified phosphatidylcholine PC 40:4 and sphingomyelins (SM d41:2, SM d36:3) as top biomarkers. | AdaBoost model achieved an AUC of 0.875 for classifying liver cancer vs. controls. [99] | |
| Pan-Cancer | DNA Methylation | XAI frameworks are used to interpret models that detect and classify cancer from epigenetic patterns. | Critical for developing Multi-Cancer Early Detection (MCED) tests like Galleri. [100] | |
| Non-Small Cell Lung Cancer | Multi-Omics Data | Explainable AI (XAI) frameworks assisted in linking specific biomarkers to patient outcomes for clinical decision-making. | Improved diagnostic accuracy and boosted clinician confidence in AI results. [96] |
Experimental Protocols for XAI-Driven Biomarker Discovery
Protocol 1: Biomarker Discovery from Gene Expression Data using CNN and SHAP
This protocol is adapted from studies on predicting breast cancer biomarker status (ER, PR, HER2) from gene expression data [98].
1. Objective: To train a convolutional neural network (CNN) for classifying cancer biomarker status and use SHAP to identify the gene features most critical to the model's predictions.
2. Materials and Reagents:
- Gene Expression Dataset: A matrix of normalized gene expression values (e.g., RNA-Seq or microarray data) from patient samples, with rows representing samples and columns representing genes. The dataset must include confirmed clinical status for the biomarkers of interest.
- Computational Environment: A Python environment with TensorFlow/Keras or PyTorch for deep learning, and the
shaplibrary for explainability.
3. Procedure:
Step 1: Data Preprocessing and Feature Scaling
- Data Cleaning: Remove samples with excessive missing data. Impute remaining missing values using appropriate methods (e.g., k-nearest neighbors).
- Normalization: Apply standard scaling (z-score normalization) to each gene expression feature to achieve a mean of zero and a standard deviation of one. This ensures no single gene dominates the model training due to its native scale.
- Train-Test Split: Partition the dataset into a training set (e.g., 70-80%) and a held-out test set (e.g., 20-30%) using stratified sampling to preserve the class distribution.
Step 2: Model Training with a Convolutional Neural Network
- Model Architecture:
- Input Layer: Accepts the vector of gene expression values.
- Reshape Layer: Transform the 1D gene vector into a 2D format (e.g., a 1D convolutional layer can be used to capture local patterns in gene sequences).
- Convolutional Layers: Use 1D convolutional layers with ReLU activation to extract local, high-level features from the gene expression profile.
- Pooling Layers: Apply max-pooling to reduce dimensionality and enhance feature invariance.
- Fully Connected Layers: Flatten the output and use dense layers for final classification.
- Output Layer: A softmax layer for multi-class classification or a sigmoid layer for binary classification.
- Model Compilation and Training:
- Compile the model using the Adam optimizer and binary cross-entropy loss.
- Train the model on the training set, using a validation split to monitor for overfitting. Employ early stopping if the validation performance plateaus.
Step 3: Model Interpretation with SHAP
- SHAP Explainer Selection: For deep learning models, use the
SHAP.DeepExplainerorKernelExplainer. - Calculating SHAP Values: Compute SHAP values for a representative subset of the test set (e.g., 100-500 samples). This quantifies the marginal contribution of each gene to the prediction for each sample.
- Visualization and Analysis:
- Summary Plot: Generate a SHAP summary plot to display the most important genes across all sampled instances and the distribution of their impacts.
- Force Plots: Create individual force plots for specific samples to illustrate how each gene's expression value "pushes" the model's output from the base value to the final prediction.
4. Expected Output:
- A trained CNN model with validated performance metrics (Accuracy, Precision, AUC).
- A ranked list of genes based on their mean absolute SHAP values, indicating their global importance as potential biomarkers.
- Visualizations that provide both global model interpretability and local explanations for individual predictions.
Protocol 2: Lipidomic Biomarker Identification using Ensemble Models and SHAP
This protocol is based on a study that identified lipidomic biomarkers for liver cancer diagnosis from serum samples [99].
1. Objective: To apply machine learning ensemble methods to untargeted lipidomic data and use SHAP to identify lipid species with diagnostic potential for liver cancer.
2. Materials and Reagents:
- Lipidomic Data: Serum lipidomic profiles obtained via Liquid Chromatography Quadrupole Time-of-Flight Mass Spectrometry (LC-QTOF-MS). Data should be pre-processed (peak picking, alignment, annotation) and normalized (e.g., using Systematic Error Reduction using Random Forest - SERRF).
- Clinical Cohorts: Data from age-matched case (cancer) and control groups.
3. Procedure:
Step 1: Feature Selection and Statistical Analysis
- Univariate Analysis: Perform t-tests and calculate Fold Change (FC) for each lipid species between cancer and control groups. Apply False Discovery Rate (FDR) correction. Retain lipids with FDR-adjusted p-value ≤ 0.05 and FC ≥ 1.2 (upregulated) or ≤ 1.2 (downregulated).
- Multivariate Analysis: Use Partial Least Squares Discriminant Analysis (PLS-DA) to obtain Variable Importance in Projection (VIP) scores. Also, apply embedded feature selection methods like Elastic Net to select lipids that best discriminate between groups.
- Final Lipid Candidate List: Select the intersection of significant lipids from the univariate (FC), PLS-DA (VIP), and Elastic Net analyses for model training.
Step 2: Building and Evaluating Ensemble Classifiers
- Model Selection: Train and compare multiple tree-based ensemble models, including AdaBoost, Random Forest, and Gradient Boosting.
- Robust Validation: Use a stratified 4:1 train-test split. Repeat the training and evaluation process multiple times (e.g., 100 iterations) with different random seeds to ensure robustness and minimize overfitting.
- Performance Assessment: Evaluate models on the held-out test set using Area Under the Curve (AUC), accuracy, F1-score, sensitivity, and specificity. Select the best-performing model (e.g., AdaBoost, which achieved an AUC of 0.875 [99]) for interpretation.
Step 3: Model Interpretation with SHAP
- Tree Explainer: Use
SHAP.TreeExplainer, which is optimized for tree-based models, to compute SHAP values. - Biomarker Identification:
- Generate a SHAP summary plot (bar plot) to visualize the top lipids contributing to the model's predictive power.
- Analyze the direction of impact (e.g., higher levels of PC 40:4 increase the risk score for cancer, while higher levels of SM d41:2 decrease it).
- Use dependence plots to explore the interaction between the top lipids and their impact on the model output.
4. Expected Output:
- A validated ensemble model for classifying liver cancer based on serum lipids.
- A shortlist of candidate lipid biomarkers (e.g., PC 40:4, SM d41:2) with diagnostic potential, backed by both statistical and model-based interpretability.
Visualization of Workflows and Relationships
XAI-Informed Biomarker Discovery Workflow
The following diagram illustrates the end-to-end pipeline for discovering and validating biomarkers using machine learning and XAI.
SHAP Value Calculation Logic
This diagram outlines the core computational logic behind SHAP for explaining an individual prediction, based on cooperative game theory.
Table 2: Key Research Reagent Solutions for XAI-Based Biomarker Discovery
| Item Name | Function / Application | Example / Specification |
|---|---|---|
| RNA-Seq Kit | Provides transcriptome-wide gene expression data for model input. | Illumina NovaSeq Series; Samples with 1,941 gene features used in breast cancer study [98]. |
| LC-QTOF-MS System | Performs untargeted lipidomic profiling from serum/plasma samples. | Liquid Chromatography Quadrupole Time-of-Flight Mass Spectrometry; Used for 462 lipid species in liver cancer study [99]. |
| Bisulfite Conversion Kit | Prepares DNA for methylation analysis, a key epigenetic biomarker. | Required for Whole Genome Bisulfite Sequencing (WGBS) used in pan-cancer detection tests [100]. |
| Python SHAP Library | Open-source Python package for calculating and visualizing SHAP values. | pip install shap; Compatible with major ML frameworks (TensorFlow, PyTorch, Scikit-learn) [97] [98] [99]. |
| Wisconsin Breast Cancer Dataset | Public benchmark dataset for developing and testing diagnostic models. | Contains FNA image-derived features (radius, concavity, etc.) for 569 patients [97]. |
| High-Performance Computing (HPC) Cluster | Provides computational power for training complex models and calculating SHAP values. | Essential for processing high-dimensional omics data and running multiple model iterations [65] [10]. |
The transition of a machine learning (ML) model for cancer detection from a research setting to clinical use is a critical and complex journey. This path demands robust validation on independent cohorts and a clear navigation of the regulatory landscape. For an ML model that analyzes DNA sequences to detect cancer, such as those utilizing circulating cell-free DNA (cfDNA) fragmentation patterns or methylation profiles, demonstrating generalizability and compliance with regulatory standards is paramount for clinical adoption [101] [102]. This document outlines the essential protocols and considerations for validating your model and preparing for regulatory submission, framed within the practical implementation of ML in cancer diagnostics.
Validation on Independent Cohorts
The Critical Role of Independent Validation
Validation on independent cohorts is the cornerstone of establishing model credibility. It assesses whether a model trained on one dataset can perform reliably on new, unseen data from different populations or clinical sites. This process tests the model's generalizability and helps identify issues like overfitting to the training data's specific noise or demographic biases. For cancer detection models, high performance on independent cohorts is necessary to prove that the test will work consistently in the diverse patient populations encountered in real-world clinical practice [101].
Protocol for Cohort Validation
A rigorous, multi-stage validation protocol is required to build sufficient evidence for clinical translation.
Step 1: Cohort Sourcing and Selection Identify and acquire samples from independent cohorts that are entirely separate from the training and internal validation sets. These cohorts should be prospectively collected where possible. Key considerations include:
- Population Relevance: The cohort should reflect the intended-use population for the test (e.g., high-risk individuals for early detection).
- Sample Size: The cohort must be adequately sized to provide precise estimates of performance metrics (e.g., sensitivity, specificity) with sufficiently narrow confidence intervals. For early-stage cancers, where the signal may be faint, larger sample sizes are often necessary [101] [102].
- Data Completeness: Ensure the independent cohort has all the necessary data points required by the model (e.g., NGS data from blood plasma cfDNA) and high-quality clinical annotation [101].
Step 2: Blinded Analysis The model's predictions on the independent validation cohort must be generated in a blinded manner. The personnel running the model and the bioinformaticians analyzing the outputs should have no access to the true clinical outcomes of the samples until after the final predictions are locked.
Step 3: Performance Assessment Calculate key performance metrics by comparing the model's predictions against the ground truth clinical diagnoses. Essential metrics include:
- Sensitivity (Recall): The model's ability to correctly identify patients with cancer.
- Specificity: The model's ability to correctly identify patients without cancer.
- Area Under the Receiver Operating Characteristic Curve (AUC-ROC): A comprehensive measure of the model's discriminatory power.
- Precision and F1-Score: Particularly important in imbalanced datasets.
The performance should be reported overall and stratified by relevant clinical subgroups, such as cancer stage, histology, and demographic factors [101].
Step 4: Comparison to Standards Where applicable, compare the model's performance to the current standard of care (e.g., low-dose computed tomography for lung cancer screening [101] or mammography for breast cancer [102]). This demonstrates clinical utility and the potential value-add of the new test.
Table 1: Example Performance Metrics from an Independent Validation Study on a Lung Cancer Detection Model [101]
| Cancer Stage | Sensitivity (%) | Specificity (%) | AUC |
|---|---|---|---|
| Stage I | 66.7 - 85.7 | 79.3 - 90.0 | 0.872 - 0.875 |
| Stage II | 77.8 - 100.0 | 79.3 - 90.0 | 0.872 - 0.875 |
| Stage III | 70.0 - 80.0 | 79.3 - 90.0 | 0.872 - 0.875 |
| Overall | ~80.0 | ~85.0 | 0.872 - 0.875 |
Navigating the Regulatory Landscape
Key Regulatory Bodies and Frameworks
Achieving regulatory approval is a mandatory step for clinical implementation. The primary regulatory bodies and their relevant guidelines include:
- U.S. Food and Drug Administration (FDA): Requires that all information provided to trial subjects and patients is understandable and complete. Its guidance emphasizes clarity in informed consent and documentation, which extends to the claims and instructions of an in vitro diagnostic (IVD) [103] [104].
- European Medicines Agency (EMA) & EU Clinical Trials Regulation (EU CTR): The EU CTR requires that participant-facing documents be available in the languages of the participants. For a marketed device, the European Union Medical Device Regulation (EU MDR) mandates specific requirements for labelling, instructions for use (IFU), and technical documentation in official EU languages [103] [104].
- International Council for Harmonisation (ICH) Good Clinical Practice (GCP): Sets international standards for clinical trials, stating that information given to subjects must be "in a language that is non-technical and understandable to the subject" [103].
Protocol for Regulatory Preparation
A proactive and documented approach is essential for successful regulatory engagement.
Step 1: Establish a Quality Management System (QMS) Implement a QMS, such as one compliant with ISO 13485, which is the international standard for medical device quality systems. This system will govern all aspects of design, development, manufacturing, and post-market surveillance [104].
Step 2: Define the Intended Use and Claims Precisely define the test's intended use. This includes the specific disease or condition, the target population, the specimen type (e.g., blood plasma), and the clinical claims (e.g., "for early detection of lung cancer"). The scope of the intended use directly determines the amount and type of validation data required.
Step 3: Analytical Validation Demonstrate that your test accurately and reliably measures the analyte it claims to measure. This is separate from clinical validation and includes:
- Precision/Reproducibility: Show consistent results across multiple runs, days, operators, and laboratories.
- Analytical Sensitivity (Limit of Detection): Determine the lowest amount of the analyte (e.g., tumor DNA fraction) that can be reliably detected.
- Analytical Specificity: Show that the test is not affected by interfering substances (e.g., genomic DNA from white blood cells) [102].
Step 4: Clinical Validation This is the stage where the independent cohort validation data is presented. The objective is to provide robust evidence that the test performs as claimed in the intended-use population. The study design (e.g., case-control vs. prospective cohort) must be appropriate for the claims.
Step 5: Prepare the Regulatory Submission Compile all required documentation into a submission package. This typically includes:
- Technical File (EU MDR) or 510(k)/PMA Application (FDA): A comprehensive dossier detailing the device description, intended use, software as a medical device (SaMD) information, quality system information, and the complete analytical and clinical validation reports [104].
- Clinical Evidence Report: A summary of the clinical validation study and its results.
- Labelling and IFU: Proposed labelling in the required languages, ensuring clarity for end-users [103] [104].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for developing and validating an ML-based cancer detection assay from DNA sequences.
Table 2: Essential Research Reagents and Materials for cfDNA-Based Cancer Detection Assays
| Item | Function/Application | Key Considerations |
|---|---|---|
| cfDNA Extraction Kits | Isolation of high-quality, non-degraded cfDNA from blood plasma. | Yield, purity, and fragment size preservation are critical. Optimized for low-input samples. |
| DNA Library Prep Kits (NGS) | Preparation of sequencing libraries from cfDNA for subsequent analysis. | Should be compatible with low DNA inputs and preserve fragmentomics information. Kits with unique molecular identifiers (UMIs) are beneficial. |
| Bisulfite Conversion Kits | Chemical treatment of DNA to differentiate methylated from unmethylated cytosines for methylation-based models. | Conversion efficiency and DNA degradation are major factors. Bisulfite-free alternatives (e.g., EM-seq, TAPS) are emerging [102]. |
| Targeted Sequencing Panels | Hybrid-capture or amplicon-based panels to enrich for cancer-specific genomic regions or methylation sites. | Allows for cost-effective, deep sequencing of defined biomarkers. Panel design is crucial for performance [102]. |
| Reference Standards | Commercially available synthetic or cell-line derived DNA with known mutations and methylation status. | Essential for assay validation, calibration, and inter-laboratory reproducibility studies. |
| Bioinformatics Pipelines | Software for processing raw NGS data, generating features (e.g., fragment size, coverage, methylation calls), and running the ML model. | Must be version-controlled, validated, and documented for regulatory approval. |
Workflow Visualization
The following diagram illustrates the integrated pathway from research to clinical translation, encompassing both the validation and regulatory stages.
Clinical Translation Pathway
This workflow outlines the key stages for translating a research model into a clinical tool, highlighting the parallel streams of technical/clinical validation and regulatory preparation that converge for a successful submission.
Detailed Experimental Protocols
Protocol for Independent Cohort Validation Using cfDNA Fragmentomics
This protocol is adapted from methodologies used in studies for lung cancer detection [101].
Objective: To validate a pre-trained machine learning model for distinguishing between healthy subjects and cancer patients using cfDNA fragmentation patterns from NGS data of an independent cohort.
Materials:
- Blood plasma samples from an independent cohort (e.g., N=286, with 148 healthy, 138 with lung cancer) [101].
- Extracted cfDNA, quantified and quality-controlled.
- NGS library preparation kit.
- Illumina NovaSeq 6000 or equivalent sequencer.
- High-performance computing cluster for bioinformatic analysis.
Procedure:
- Sample Processing: Process all samples from the independent cohort uniformly. Isolate cfDNA from blood plasma according to a standardized, validated protocol to minimize pre-analytical variability.
- Sequencing Library Preparation: Prepare sequencing libraries from the isolated cfDNA. Aim for a deep sequencing coverage (e.g., 100 million reads per sample) to ensure sufficient data for fragmentation analysis [101].
- Bioinformatic Processing:
- Alignment: Map the sequenced reads to the reference human genome (e.g., hg38).
- Feature Extraction: Calculate the defined feature set used by your model for each genomic interval or sample. This typically includes:
- Fragment Size Distribution (FSD): The abundance and length distribution of cfDNA fragments (e.g., variables describing short vs. long fragments).
- End Motif Analysis (EDM): Variables based on position-weight matrices describing the frequency of 5-bp-long terminal motifs of cfDNA fragments [101].
- Data Compilation: Compile the feature matrix for the entire independent cohort, ensuring sample identifiers are blinded to the clinical outcomes.
- Model Prediction: Run the locked, pre-trained ML model on the feature matrix from the independent cohort to generate predictions (e.g., cancer vs. healthy probability scores).
- Statistical Analysis: After unblinding, perform the following analyses:
- Calculate overall sensitivity, specificity, and AUC with 95% confidence intervals.
- Stratify performance by cancer stage (I, II, III) as shown in Table 1.
- Perform subgroup analyses if the cohort size permits (e.g., by age, sex).
Protocol for Regulatory Documentation Preparation
Objective: To compile the necessary documentation for a regulatory submission to a body like the FDA or under the EU MDR.
Materials:
- All data and reports from analytical and clinical validation studies.
- Standard Operating Procedures (SOPs) from the QMS.
- Detailed design history file.
Procedure:
- Compile the Technical Documentation:
- Device Description: Provide a detailed description of your test, including its principle of operation, components (software, reagents), and hardware requirements.
- Intended Use Statement: Formally define the intended use, indications for use, and target population.
- Software as a Medical Device (SaMD) Documentation: If applicable, provide architecture design, software requirements, risk management file (per ISO 14971), and verification/validation reports for the algorithm and user interface.
- Analytical Performance Report: Present all data from the analytical validation studies (precision, sensitivity, specificity, etc.).
- Clinical Performance Report: Incorporate the final report from the independent cohort validation study, including the protocol, statistical analysis plan, and results.
Prepare Quality System Evidence:
- Demonstrate that the device is designed and manufactured under a quality system, typically by referencing ISO 13485 certification.
- Include the device master record and design history file.
Develop Labelling and IFU:
- Create the proposed labelling, including all packaging and accompanying documents.
- The IFU must be clear and comprehensible to the end-user and include information on intended use, specimen collection, test procedure, interpretation of results, limitations, and warnings [104]. For global markets, plan for linguistic validation of the IFU to ensure accuracy and cultural appropriateness [103] [105].
Submit and Engage: Submit the complete package to the regulatory authority and be prepared to respond to questions and provide additional data during the review process.
Conclusion
The integration of machine learning with DNA sequence analysis marks a transformative shift in cancer detection, moving towards non-invasive, highly accurate, and early diagnosis. The synthesis of insights across the four intents confirms that successful implementation hinges on a deep understanding of cancer genomics, careful selection and optimization of ML methodologies, proactive tackling of data-centric challenges, and rigorous, clinically-relevant validation. Future progress will be driven by the development of explainable AI frameworks to build clinical trust, the integration of multi-omics data for a holistic view of tumor biology, and the execution of large-scale clinical trials to validate these tools in diverse populations. For researchers and drug developers, this convergence of computational and biological sciences opens unprecedented avenues for creating the next generation of precision oncology diagnostics and therapeutics.
References
- 1. A Comprehensive Review of Bioinformatics Tools for Genomic Biomarker Discovery Driving Precision Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11353282/]
- 2. Evaluating DNA , Gene Expression, Methylation ... Somatic Mutation [https://pubmed.ncbi.nlm.nih.gov/34012960/]
- 3. JMIR Bioinformatics and Biotechnology - Stacked Deep Learning Ensemble for Multiomics Cancer Type Classification: Development and Validation Study [https://bioinform.jmir.org/2025/1/e70709]
- 4. Circulating tumor DNA to monitor treatment response in solid tumors and advance precision oncology | npj Precision Oncology [https://www.nature.com/articles/s41698-025-00876-y]
- 5. Artificial Intelligence in cancer epigenomics: a review on advances in... [https://epigeneticsandchromatin.biomedcentral.com/articles/10.1186/s13072-025-00595-5]
- 6. Discovery and validation of cell-free DNA methylation markers for specific diagnosis, differentiation from benign tumors, and prognosis of breast cancer | Breast Cancer Research | Full Text [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-025-02066-x]
- 7. Frontiers | DNA in esophageal methylation : technological... cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1543190/full]
- 8. Multimodal AI/ML for discovering novel biomarkers and predicting disease using multi-omics profiles of patients with cardiovascular diseases | Scientific Reports [https://www.nature.com/articles/s41598-024-78553-6]
- 9. Machine Learning Approaches for Biomarker Discovery Using Gene Expression Data - Bioinformatics - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK569564/]
- 10. Unlocking Early Cancer : Leveraging Detection in... Machine Learning [https://pmc.ncbi.nlm.nih.gov/articles/PMC12099344/]
- 11. Comparative Overview of cfDNA and ctDNA: Biology, Utility, and Extraction - CD Genomics [https://www.cd-genomics.com/resource-cfdna-ctdna-key-differences-applications-extraction-considerations.html]
- 12. Tissue-specific cell-free DNA degradation quantifies circulating tumor DNA burden | Nature Communications [https://www.nature.com/articles/s41467-021-22463-y]
- 13. ctDNA Sequencing Services - CD Genomics [https://www.cd-genomics.com/ctdna-sequencing-services.html]
- 14. Frontiers | Advances of nanopore direct sequencing technology and... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1662587/full]
- 15. Clinical implementation of next-generation sequencing testing and genomically-matched therapy: a real-world data in a tertiary hospital | Scientific Reports [https://www.nature.com/articles/s41598-024-84909-9]
- 16. of Detection Three Years prior to Diagnosis Using Plasma... Cancers [https://pubmed.ncbi.nlm.nih.gov/40402478/]
- 17. HOPA 2025 : The Promise and Pitfalls of ctDNA ... | Pharmacy Times [https://www.pharmacytimes.com/view/hopa-2025-the-promise-and-pitfalls-of-ctdna-testing-in-oncology]
- 18. (BS-Seq)/ Bisulfite Sequencing WGBS [https://emea.illumina.com/techniques/sequencing/methylation-sequencing/bisulfite-sequencing.html]
- 19. How Does Whole Work? Genome Bisulfite Sequencing [https://www.news-medical.net/life-sciences/How-Does-Whole-Genome-Bisulfite-Sequencing-Work.aspx]
- 20. Gene Targeted Sequencing Panels [https://emea.illumina.com/techniques/sequencing/dna-sequencing/targeted-resequencing/targeted-panels.html]
- 21. in the Real World: 5 Uses... Whole Genome Bisulfite Sequencing [https://www.linkedin.com/pulse/whole-genome-bisulfite-sequencing-real-world-5-uses-bwszc]
- 22. Next-generation sequencing to guide cancer therapy | Genome Medicine | Full Text [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-015-0203-x]
- 23. A machine learning approach to optimizing cell-free DNA sequencing panels: with an application to prostate cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/32859160/]
- 24. Next-generation sequencing in cancer diagnosis and treatment: clinical applications and future directions | Discover Oncology [https://link.springer.com/article/10.1007/s12672-025-01816-9]
- 25. Making use of cancer genomic databases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5774229/]
- 26. Access Data | NCI Genomic Data Commons [https://gdc.cancer.gov/access-data]
- 27. Genome Sequence Archive - CNCB-NGDC [https://ngdc.cncb.ac.cn/gsa/]
- 28. Similarities, differences and usage contexts of FASTA and FASTQ ... [https://sequenceserver.com/blog/fasta-vs-fastq-formats/]
- 29. and Sequences / FASTA files — HTSeq 2.0.5 documentation FASTQ [https://htseq.readthedocs.io/en/latest/sequences.html]
- 30. Advanced DNA Text Classification Using Natural... | Medium Sequence [https://ernest-bonat.medium.com/advanced-dna-sequence-text-classification-using-natural-language-processing-8860c3c05692]
- 31. of Analysis Classification Using CNN and Hybrid... DNA Sequence [https://pmc.ncbi.nlm.nih.gov/articles/PMC8285202/]
- 32. [1908.10084] Sentence-BERT: Sentence Embeddings using Siamese BERT-Networks [https://arxiv.org/abs/1908.10084]
- 33. SimCSE — Sentence Transformers documentation [https://www.sbert.net/examples/unsupervised_learning/SimCSE/README.html]
- 34. A machine learning-based method for feature reduction of methylation data for the classification of cancer tissue origin - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11588780/]
- 35. Diagnostic classification based on DNA methylation profiles using sequential machine learning approaches | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0307912]
- 36. SentenceTransformers Documentation — Sentence Transformers documentation [https://sbert.net/]
- 37. Refining cancer prediction with DNA and combined... sequencing [https://pubmed.ncbi.nlm.nih.gov/41225036/]
- 38. Open chromatin-guided interpretable machine reveals... learning [https://www.nature.com/articles/s42003-025-08920-0?error=cookies_not_supported&code=ad5c5761-3acb-4142-8640-ed7b38a771a7]
- 39. Convolutional neural network models for cancer type prediction based on gene expression | BMC Medical Genomics | Full Text [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-020-0677-2]
- 40. and Classification Using ML Algorithms Cancer Detection [https://ijctjournal.org/cancer-detection-classification-ml/]
- 41. classification for diabetes mellitus using... | PLOS One DNA sequence [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0328253]
- 42. [2511.14816] XGBoost -Powered Digital Twins Leverage Routine Blood... [https://arxiv.org/abs/2511.14816]
- 43. Frontiers | Computational models for pan-cancer classification based on multi-omics data [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1667325/full]
- 44. Frontiers | MASE-GC: a multi -omics autoencoder and stacking... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1704237/full]
- 45. Revolutionizing tumor detection and classification in multimodality imaging based on deep learning approaches: Methods, applications and limitations - PubMed [https://pubmed.ncbi.nlm.nih.gov/38701131/]
- 46. Stacked Deep Learning Ensemble for Multiomics Cancer Type Classification: Development and Validation Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342693/]
- 47. Enhancing Breast Cancer Detection and Classification Using Advanced Multi-Model Features and Ensemble Machine Learning Techniques - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10608611/]
- 48. Incorporation of explainable artificial intelligence in ensemble machine learning-driven pancreatic cancer diagnosis | Scientific Reports [https://www.nature.com/articles/s41598-025-98298-0]
- 49. Transfer Learning in Lung Cancer : Leveraging Detection - Pre ... Trained [https://www.easychair.org/publications/preprint/kNQD]
- 50. Deep Learning for Cancer Based on Genomic and Imaging... Detection [https://www.dovepress.com/deep-learning-for-cancer-detection-based-on-genomic-and-imaging-data-a-peer-reviewed-fulltext-article-CMAR]
- 51. cfMethylPre: deep transfer enhances learning ... cancer detection [https://pubmed.ncbi.nlm.nih.gov/40581983/]
- 52. disease multinomial classification using Cancer and... transfer learning [https://publications.eai.eu/index.php/phat/article/view/3220]
- 53. Genomic approaches to cancer and minimal residual disease detection ... [https://ncbi.nlm.nih.gov/pmc/articles/PMC10314661]
- 54. Signal-to-noise enhanced detection of circulating tumor DNA via rolling circle amplification and amphiphilic polymer-integrated field-effect transistor sensors - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0026265X2502329X]
- 55. Multimodal cell-free DNA whole-genome... | Nature Communications [https://www.nature.com/articles/s41467-024-55428-y?error=cookies_not_supported]
- 56. enables Machine of learning - detection colorectal early ... stage cancer [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-019-6003-8]
- 57. A machine learning approach to optimizing cell-free DNA sequencing panels: with an application to prostate cancer | BMC Cancer | Full Text [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-020-07318-x]
- 58. Measurement of ctDNA Tumor Fraction Identifies Informative Negative Liquid Biopsy Results and Informs Value of Tissue Confirmation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11145175/]
- 59. for Synthetic — Data ... Machine Learning Copulas [https://sdv.dev/Copulas/tutorials/04_Synthetic_Data_for_Machine_Learning.html]
- 60. TVAESynthesizer | Synthetic Vault Data [https://docs.sdv.dev/sdv/single-table-data/modeling/synthesizers/tvaesynthesizer]
- 61. Model | sdv-dev/CTGAN | DeepWiki TVAE [https://deepwiki.com/sdv-dev/CTGAN/2.2-tvae-model]
- 62. Advancing breast cancer prediction: Comparative analysis... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0326221]
- 63. AI-Driven Predictive Modeling for Lung Cancer Detection and Management Using Synthetic Data Augmentation and Random Forest Classifier | International Journal of Computational Intelligence Systems [https://link.springer.com/article/10.1007/s44196-025-00879-4]
- 64. Frontiers | Data augmented lung cancer prediction framework using the nested case control NLST cohort [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1492758/full]
- 65. Methods for Machine Classification Using Gene... Learning Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC9952758/]
- 66. Optimizing Models: Cross - Validation and Hyperparameter ... Tuning [https://stackabuse.com/optimizing-models-cross-validation-and-hyperparameter-tuning-guide/]
- 67. The Ultimate Guide to Deep Learning Hyperparameter Tuning - Train in Data's Blog [https://www.blog.trainindata.com/the-ultimate-guide-to-deep-learning-hyperparameter-tuning/]
- 68. Hyperparameter Tuning - GeeksforGeeks [https://www.geeksforgeeks.org/machine-learning/hyperparameter-tuning/]
- 69. - ML - GeeksforGeeks Hyperparameters Optimization methods [https://www.geeksforgeeks.org/machine-learning/hyperparameters-optimization-methods-ml/]
- 70. A Beginner’s Guide to Hyperparameter in Optimization ... Machine [https://www.coursera.org/articles/hyperparameter-optimization]
- 71. Harnessing Genetic Algorithms for Hyperparameter in... Optimisation [https://dev.to/bikashdaga/harnessing-genetic-algorithms-for-hyperparameter-optimisation-in-2025-a-deep-dive-4bek]
- 72. Optimized hybrid CNN-RNN model with grid ... search hyperparameter [https://ijirss.com/index.php/ijirss/article/view/6091]
- 73. Frontiers | Editorial: Interpretable and explainable machine learning models in oncology [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1184428/full]
- 74. AI-Powered Ovarian Cancer Through Detection Methylation DNA [https://www.targetedonc.com/view/ai-powered-ovarian-cancer-detection-through-dna-methylation]
- 75. Quantum integration in swin transformer mitigates in... overfitting [https://www.nature.com/articles/s41598-025-17075-1?error=cookies_not_supported&code=98d5957b-0440-451b-9bca-9cc441efcb39]
- 76. Open chromatin-guided interpretable machine learning reveals cancer-specific chromatin features in cell-free DNA | Communications Biology [https://www.nature.com/articles/s42003-025-08920-0]
- 77. Ultrasensitive detection of circulating tumour DNA via deep... [https://pubmed.ncbi.nlm.nih.gov/34131323/]
- 78. Development of a deep learning model for cancer diagnosis by inspecting cell-free DNA end-motifs | npj Precision Oncology [https://www.nature.com/articles/s41698-024-00635-5]
- 79. Explainable AI based cervical cancer prediction using FSAE feature engineering and H2O AutoML | Scientific Reports [https://www.nature.com/articles/s41598-025-23593-9]
- 80. Evaluating the analytical validity of circulating tumor DNA sequencing assays for precision oncology | Nature Biotechnology [https://www.nature.com/articles/s41587-021-00857-z]
- 81. Models for the Identification of Prognostic and... Machine Learning [https://pmc.ncbi.nlm.nih.gov/articles/PMC10178491/]
- 82. F1 Score vs ROC vs AUC vs PR AUC: Which Evaluation... Accuracy [https://neptune.ai/blog/f1-score-accuracy-roc-auc-pr-auc]
- 83. Receiver Operating Characteristic ( ROC ) Curve for Medical... Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC3755824/]
- 84. Predicting cancer risk using machine on lifestyle and genetic... learning [https://www.nature.com/articles/s41598-025-15656-8?error=cookies_not_supported&code=f082e702-1915-4b8c-a1e5-68049989cfe7]
- 85. Automated Dissection and Interpretation of Circulating Tumor DNA ... [https://www.linkedin.com/pulse/automated-dissection-interpretation-circulating-tumor-kyungjun-lim-ek2hc]
- 86. Cancer Whole-Genome Sequencing | Tumor-normal comparisons to discover driver mutations [https://www.illumina.com/areas-of-interest/cancer/research/sequencing-methods/cancer-whole-genome-seq.html]
- 87. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 88. A comprehensive analysis of recent advancements in cancer detection using machine learning and deep learning models for improved diagnostics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11796559/]
- 89. Application of deep learning models in gastric cancer pathology image analysis: a systematic scoping review | BMC Cancer | Full Text [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14662-3]
- 90. New blood test can detect 3 years before symptoms cancer [https://nypost.com/2025/06/17/health/new-blood-test-can-detect-cancer-3-years-before-symptoms/]
- 91. JMIR Cancer - Clinical Prediction Models Incorporating Blood Test... [https://cancer.jmir.org/2025/1/e70275]
- 92. Analysis of Machine Comparative Models for Automated... Learning [https://inlibrary.uz/index.php/tajmspr/article/view/60551]
- 93. Cancer detection using whole-genome sequencing of cell free DNA - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3787139/]
- 94. Establishing community reference samples... | Nature Biotechnology [https://www.nature.com/articles/s41587-021-00993-6?error=cookies_not_supported&code=13e8f5bc-8e39-4d7c-a5ee-3cc096b6fb1e]
- 95. The Cancer Genome Atlas Program (TCGA) - NCI [https://www.cancer.gov/ccg/research/genome-sequencing/tcga]
- 96. -driven AI : enhancing precision in biomarker ... discovery cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906928/]
- 97. Bridging Accuracy and Interpretability : Deep Learning with XAI for... [https://arxiv.org/html/2510.21780v1]
- 98. Integrating Gene Expression and Proteomics for Breast Cancer ... [https://www.researchsquare.com/article/rs-7151673/v1]
- 99. Untargeted Lipidomic Biomarkers for Liver Cancer Diagnosis... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11943538/]
- 100. Artificial Intelligence in cancer epigenomics: a review on advances in... [https://link.springer.com/article/10.1186/s13072-025-00595-5]
- 101. Frontiers | Diagnostics of lung cancer by fragmentated blood circulating... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1435428/full]
- 102. methylation in breast DNA : early cancer and biomarker... detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020129/]
- 103. 7 Vital Translation for Requirements Trials Clinical [https://www.conversis.com/insights/translation-requirements-for-clinical-trials]
- 104. Understanding the Regulatory Landscape for Medical Translation [https://www.mylanguageconnection.com/understanding-the-regulatory-landscape-for-medical-translation/]
- 105. Linguistic Validation Services: Why Clinical Trials in 2025 Demand... [https://www.somyatrans.com/linguistic-validation-services-why-clinical-trials-in-2025-demand-more-than-translations/]