De Novo Drug Design for Oncology: AI-Driven Methods for Novel Cancer Therapeutics
This article provides a comprehensive overview of modern de novo drug design methods and their transformative application in oncology.
De Novo Drug Design for Oncology: AI-Driven Methods for Novel Cancer Therapeutics
Abstract
This article provides a comprehensive overview of modern de novo drug design methods and their transformative application in oncology. Tailored for researchers and drug development professionals, it explores the foundational principles of generative AI, delves into specific methodological approaches for creating novel anti-cancer compounds, addresses key challenges in optimization and validation, and offers a comparative analysis of leading platforms and their clinical progress. The synthesis of current innovations and real-world case studies aims to equip scientists with the knowledge to leverage these technologies for accelerating the discovery of next-generation cancer therapies.
The New Frontier: How AI is Redefining Oncology Drug Discovery
The development of novel oncology therapeutics is defined by a critical paradox: despite unprecedented understanding of cancer biology, the successful translation of this knowledge into new medicines remains hampered by persistently high attrition rates and the profound complexity of tumor heterogeneity. Traditional drug discovery approaches are increasingly insufficient to address these challenges, with approximately 90% of oncology drugs failing during clinical development [1]. This attrition imposes tremendous costs, both temporal and financial, with traditional drug development requiring 12-15 years and investments reaching $1-2.6 billion per approved therapy [2]. The convergence of these challenges has created an imperative for innovation, particularly in de novo drug design methods that can fundamentally reshape our approach to oncology therapeutic development.
Tumor heterogeneity manifests at multiple levels, encompassing genetic, epigenetic, and microenvironmental diversity both between patients (inter-tumoral) and within individual tumors (intra-tumoral) [1]. This heterogeneity drives differential treatment responses and facilitates the emergence of resistance through Darwinian selection pressures [3]. Under conventional discovery paradigms, this biological complexity translates to formidable obstacles in target identification, candidate optimization, and clinical trial design. The industry's response has been the rapid integration of artificial intelligence (AI) and novel preclinical models that collectively offer a path toward more predictive, efficient, and personalized oncology drug development [2] [4].
Application Note: AI-Driven De Novo Drug Design
Core Principles and Workflow
Artificial intelligence has emerged as a transformative force in de novo drug design, employing generative models to create novel molecular structures with optimized drug-like properties. These approaches leverage machine learning (ML), deep learning (DL), and reinforcement learning (RL) to explore chemical space with unprecedented breadth and efficiency [4] [1]. The fundamental paradigm shift involves transitioning from screening existing compound libraries to computationally generating novel chemical entities designed for specific therapeutic targets and pharmacological profiles.
Leading AI-driven drug discovery platforms have demonstrated remarkable efficiency gains, compressing early-stage discovery timelines from the typical 3-5 years to as little as 12-18 months [5]. For instance, Exscientia's platform has achieved clinical candidate selection while synthesizing only 136 compounds, compared to thousands typically required in traditional medicinal chemistry campaigns [5]. Similarly, Insilico Medicine advanced an idiopathic pulmonary fibrosis drug from target discovery to Phase I trials in just 18 months, showcasing the transformative potential of AI-accelerated workflows [1] [5].
Key Technological Approaches
Table 1: AI Techniques in De Novo Drug Design for Oncology
| AI Technique | Key Applications | Representative Algorithms | Impact on Oncology Drug Discovery |
|---|---|---|---|
| Generative Models | De novo molecular design, scaffold hopping | Variational Autoencoders (VAEs), Generative Adversarial Networks (GANs) | Generates novel chemical structures with optimized properties for difficult oncology targets (e.g., KRAS, PD-L1) |
| Reinforcement Learning (RL) | Multi-parameter optimization, chemical space exploration | Deep Q-Learning, Actor-Critic Methods | Balances potency, selectivity, and ADMET properties through iterative design cycles |
| Graph Neural Networks | Molecular property prediction, binding affinity estimation | Message Passing Neural Networks (MPNNs) | Models complex molecular interactions and predicts target engagement for cancer-relevant proteins |
| Natural Language Processing (NLP) | Target identification, literature mining | Transformer Models, BERT Variants | Extracts hidden relationships from biomedical literature and multi-omics data to identify novel oncology targets |
The application of these AI technologies has produced several clinical-stage candidates. Exscientia's DSP-1181, designed for obsessive-compulsive disorder, became the world's first AI-designed drug to enter Phase I trials, demonstrating the platform's generalizability [5]. In oncology specifically, Exscientia has advanced multiple candidates, including a CDK7 inhibitor (GTAEXS-617) for solid tumors and an LSD1 inhibitor (EXS-74539) [5]. Insilico Medicine has applied its generative chemistry platform to identify novel inhibitors for targets relevant to tumor immune evasion, such as QPCTL [1]. These examples underscore how AI-driven de novo design can address oncology's unique challenges, particularly for targets that have proven difficult to drug through conventional approaches.
Application Note: Advanced Preclinical Models for Addressing Tumor Heterogeneity
Integrated Model Systems
The predictive validity of oncology drug development depends critically on preclinical models that faithfully recapitulate tumor heterogeneity and microenvironmental complexity. Traditional 2D cell cultures have significant limitations in capturing this complexity, driving the adoption of more physiologically relevant systems. An integrated approach leveraging multiple model types provides complementary insights throughout the drug discovery pipeline [6].
Table 2: Advanced Preclinical Models in Oncology Drug Discovery
| Model Type | Key Characteristics | Applications in Oncology | Advantages | Limitations |
|---|---|---|---|---|
| Patient-Derived Organoids | 3D structures grown from patient tumor samples, preserve histopathology | High-throughput drug screening, biomarker identification, personalized therapy testing | Maintains patient-specific genetic and phenotypic features; more predictive than 2D cultures | Limited tumor microenvironment representation; technical complexity in establishment |
| Patient-Derived Xenografts | Patient tumor tissue implanted in immunodeficient mice | Biomarker discovery, clinical stratification, drug combination strategies | Preserves tumor architecture and heterogeneity; considered "gold standard" for preclinical studies | Time-consuming, expensive, limited throughput; ethical concerns regarding animal use |
| Organ-on-Chip | Microfluidic devices with human cells, simulating tissue-level complexity | ADME profiling, tumor-immune interactions, toxicity assessment | Dynamic system capturing fluid flow and mechanical forces; human-relevant biology | Technically challenging; not yet standardized for regulatory submissions |
| 3D Bioprinted Tumors | Layer-by-layer deposition of cells and biomaterials to create tumor constructs | Studies of tumor invasion, drug penetration, microenvironmental interactions | Precise control over spatial organization of multiple cell types; customizable complexity | Limited maturity; requires specialized equipment and expertise |
The FDA's evolving stance on New Approach Methodologies (NAMs), including through the FDA Modernization Act 2.0, has accelerated the adoption of these human-relevant models [7]. By 2022, NAM-based assays accounted for approximately 30% of oncology-related safety submissions to the FDA, with organ-on-chip models projected to grow at a compound annual growth rate of 20% through 2030 [7].
Protocol: Integrated Preclinical Screening Workflow for Addressing Tumor Heterogeneity
Objective: To establish a standardized, multi-stage screening protocol that leverages complementary preclinical models for comprehensive evaluation of novel oncology therapeutics against tumor heterogeneity.
Materials and Equipment:
- Cryopreserved patient-derived tumor samples
- Organoid culture media and extracellular matrix
- Immunodeficient mice (NSG, NOG, or similar)
- Automated cell culture systems (e.g., Hamilton, Sartorius)
- High-content imaging system
- Microsampling equipment (capable of collecting 50μL blood samples)
- Liquid handling robotics
- AI-powered image analysis software
Procedure:
Step 1: Primary Screening in PDX-Derived Cell Lines
- Establish 2D cultures from dissociated PDX tumors, preserving patient-derived genetic heterogeneity
- Conduct high-throughput cytotoxicity screening against 500+ genomically diverse cancer cell lines
- Perform initial biomarker hypothesis generation by correlating genetic mutations (e.g., EGFR, KRAS, BRAF status) with drug response
- Identify response and resistance patterns across diverse genetic backgrounds
- Select top 20% of compounds for further evaluation based on potency and therapeutic index
Step 2: Secondary Screening in Patient-Derived Organoids
- Establish patient-derived organoid biobanks from multiple cancer indications (e.g., colorectal, pancreatic, breast)
- Culture organoids in 3D extracellular matrix with organ-specific media formulations
- Treat organoids with candidate compounds identified from Step 1, using concentration-response curves (8-point, 1:3 dilution series)
- Assess efficacy using high-content imaging metrics (viability, apoptosis, proliferation)
- Perform multi-omics analysis (genomics, transcriptomics, proteomics) to refine biomarker signatures
- Evaluate mechanisms of resistance through single-cell RNA sequencing of treated organoids
Step 3: Tertiary Validation in PDX Models
- Implant patient-derived tumor fragments into immunodeficient mice (n=6-8 per group)
- Randomize mice when tumors reach 150-200mm³ and initiate treatment at human-equivalent doses
- Administer candidate compounds via appropriate route (oral, IV, IP) using clinically relevant schedules
- Monitor tumor growth by caliper measurements three times weekly
- Collect serial blood samples via microsampling (50μL) for PK/PD analysis
- Perform terminal harvest at study endpoint for immunohistochemistry and biomarker validation
- Analyze intra-tumoral heterogeneity through spatial transcriptomics of harvested tumors
Step 4: Data Integration and Biomarker Validation
- Correlate drug responses across all three model systems using concordance metrics
- Validate predictive biomarker hypotheses through orthogonal techniques (IHC, FISH, NGS)
- Utilize AI algorithms to integrate multi-omics data and identify complex biomarker signatures
- Generate a final biomarker report to guide clinical trial design and patient stratification strategies
Quality Control Considerations:
- Regularly authenticate cell lines and organoids via STR profiling
- Monitor mycoplasma contamination monthly
- Standardize passage number limits for biological models (organoids < passage 10)
- Implement automated media exchange systems to reduce variability in 3D cultures
- Use reference compounds with known activity as positive controls in all assays
This integrated protocol leverages the distinct advantages of each model system while compensating for their individual limitations, creating a comprehensive framework for evaluating novel therapeutics against the backdrop of tumor heterogeneity.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Advanced Oncology Drug Discovery
| Reagent/Platform | Manufacturer/Provider | Function and Application | Key Benefits |
|---|---|---|---|
| Crown Bioscience PDX Database | Crown Bioscience | World's largest collection of clinically relevant PDX models for efficacy studies | Extensive clinical annotation, including patient treatment history and multi-omics data |
| HuPrime PDX Collection | Crown Bioscience | Comprehensive PDX library covering multiple cancer types and rare subtypes | Well-characterized models with genomic and pharmacological profiling data |
| Organoid Biobanks | Various (Crown Bioscience, ATCC, academic institutions) | Biobanks of patient-derived organoids for high-throughput screening | Preserves genetic diversity of original tumors; enables personalized therapy testing |
| Curiox C-Free System | Curiox | Automated media exchange technology for cell culture workflows | Enhanced cell retention without detachment; improves reproducibility in 3D assays |
| Pluto Wash System | Curiox | Automated washing system for cell-based assays | Reduces background staining in flow cytometry; maintains cell viability |
| AI-Driven Design Platforms | Exscientia, Insilico Medicine, Schrödinger | De novo molecular design and optimization | Accelerates lead identification; optimizes multiple drug properties simultaneously |
| Multi-omics Integration Tools | Recursion, BenevolentAI | Integration of genomic, transcriptomic, proteomic data for target identification | Identifies novel therapeutic targets; discovers biomarker signatures |
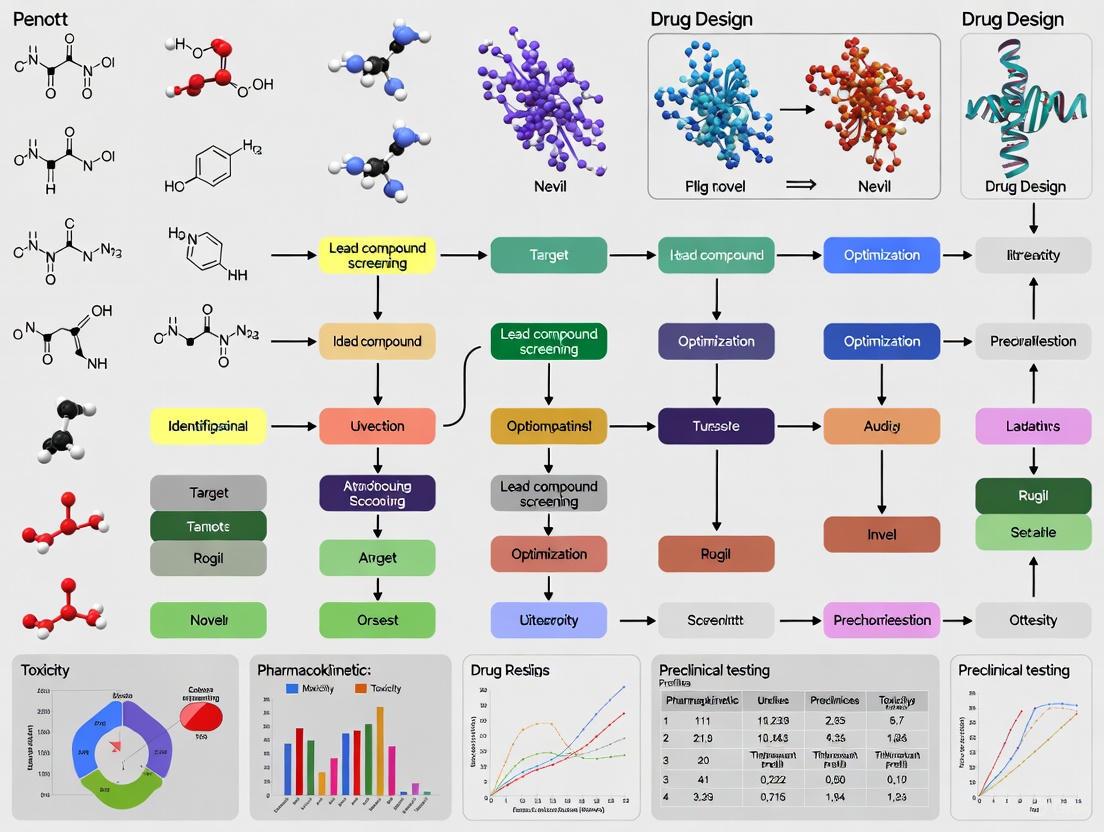
Visualization of Key Concepts and Workflows
AI-Driven De Novo Drug Design Workflow
Integrated Preclinical Screening Strategy
Tumor Heterogeneity and Resistance Mechanisms
The imperative for innovation in oncology drug development has never been clearer. High attrition rates and tumor heterogeneity represent interconnected challenges that demand fundamentally new approaches to therapeutic discovery. The integration of AI-driven de novo design with advanced preclinical models creates a powerful framework for addressing these challenges, enabling more predictive candidate selection and personalized therapeutic strategies. As these technologies continue to mature and validate their clinical utility, they offer the promise of fundamentally transforming oncology drug development from a process of incremental optimization to one of rational design, ultimately delivering more effective therapies to cancer patients in significantly less time. The convergence of computational and biological innovations documented in these Application Notes provides researchers with both the conceptual framework and practical methodologies to advance this transformative agenda.
The development of novel oncology therapeutics is undergoing a paradigm shift, moving from a linear, high-attrition pipeline to an integrated, AI-accelerated discovery engine. This application note provides a comparative analysis of traditional versus artificial intelligence (AI)-enhanced drug discovery pathways, focusing on de novo design methods for oncology. We present structured quantitative comparisons, detailed experimental protocols for AI-driven methodologies, pathway visualizations, and essential research reagent solutions to guide researchers and drug development professionals in navigating this transformative landscape.
Cancer drug discovery has traditionally been a time-intensive and resource-heavy process, often requiring over a decade and exceeding $2.6 billion to bring a single drug to market, with approximately 90% of oncology candidates failing during clinical development [1] [8]. This high attrition rate, particularly in Phase II trials where nearly 70% of drugs fail due to insufficient efficacy, underscores the critical need for more predictive and efficient methodologies [8].
Artificial intelligence (AI) is now redefining this pipeline by leveraging machine learning (ML), deep learning (DL), and natural language processing (NLP) to integrate massive, multimodal datasets. These technologies accelerate target identification, optimize lead compounds, and personalize therapeutic approaches, potentially compressing discovery timelines from years to months and dramatically reducing costs [1] [4]. This document details both traditional and AI-accelerated pathways, providing practical protocols and resources for implementing these advanced approaches in oncology drug discovery.
Comparative Pipeline Analysis: Traditional vs. AI-Accelerated Pathways
Table 1: Stage-by-Stage Comparison of Traditional and AI-Accelerated Drug Discovery Pipelines
| Discovery Stage | Traditional Approach | AI-Accelerated Approach | Key AI Technologies | Reported Efficiency Gains |
|---|---|---|---|---|
| Target Identification | Literature review, genetic studies, biochemical assays [1] | Multi-omics data integration, network analysis [1] [9] | NLP, knowledge graphs, ML classifiers | Identification of novel targets in complex datasets [2] |
| Hit Identification | High-Throughput Screening (HTS) of physical libraries [9] | Virtual screening of billions of compounds [8] | Deep learning, QSAR models | Evaluation of ~10⁶⁰ chemical space in silico [8] |
| Lead Optimization | Iterative synthesis & testing (1000s of compounds) [10] | Generative molecular design & in silico ADMET prediction [1] [4] | Generative AI (VAE, GAN), Reinforcement Learning | 70% faster design cycles; 10x fewer compounds synthesized [5] |
| Preclinical Testing | Animal models (limited predictability) [10] | Patient-derived organoids/PDX models with AI-based biomarker prediction [6] | Predictive toxicology models, digital twins | Improved clinical translatability; reduced animal testing [6] |
| Clinical Trials | Manual patient recruitment, fixed design [1] | EHR mining for recruitment, predictive enrollment, synthetic control arms [1] [9] | Predictive analytics, NLP for EHR analysis | Accelerated recruitment; optimized trial design [1] |
Table 2: Quantitative Performance Metrics of Traditional vs. AI-Accelerated Pipelines
| Performance Metric | Traditional Pipeline | AI-Accelerated Pipeline | Data Source |
|---|---|---|---|
| Discovery to Phase I Timeline | ~5 years | 18-24 months (e.g., Insilico Medicine) [5] | Industry case studies [5] |
| Cost per Approved Drug | ~$2.6 Billion [8] | Potential for significant reduction (data still emerging) | Industry analysis [8] |
| Clinical Trial Success Rate | ~10% overall [8] | Aim to significantly improve (data still emerging) | Industry analysis [8] |
| Phase II Attrition Rate | ~70% failure [8] | Aim to reduce via better patient stratification [1] | Industry analysis [1] [8] |
| Compounds Synthesized for Lead Optimization | 1000s [10] | 100s (e.g., 136 for Exscientia's CDK7 program) [5] | Company reports [5] |
Experimental Protocols for AI-Accelerated Oncology Drug Discovery
Protocol: AI-Driven Target Identification Using Multi-Omics Data
Purpose: To identify novel, druggable oncology targets by integrating heterogeneous multi-omics data sources. Experimental Principles: This protocol uses AI to analyze genomic, transcriptomic, proteomic, and clinical data to uncover hidden patterns and novel therapeutic vulnerabilities that are difficult to detect with traditional methods [1] [9].
Procedure:
- Data Acquisition and Curation: Collect multi-omics data from public repositories (e.g., The Cancer Genome Atlas - TCGA) and proprietary sources. Manually curate literature and patent information to build a comprehensive knowledge base [1] [2].
- Data Preprocessing: Normalize and scale diverse data types. Impute missing values using advanced algorithms like autoencoders. Annotate data with unified biomedical ontologies.
- Network-Based Analysis: Construct biological networks using NLP-derived relationships and omics data. Apply graph ML algorithms to identify key network nodes (proteins/genes) central to oncogenic processes [9].
- Druggability Assessment: Utilize structure prediction tools (e.g., AlphaFold) to model protein structures and identify well-defined binding pockets for candidate targets [9]. Filter targets based on novelty, disease association, and chemical tractability.
- Experimental Validation: Prioritize top candidates for in vitro validation using CRISPR-Cas9 knockout screens in relevant cancer cell lines. Confirm essentiality via cell viability and functional assays [9].
Protocol: De Novo Molecular Design Using Generative AI
Purpose: To generate novel, synthetically accessible small molecules with optimized properties for a validated oncology target. Experimental Principles: Generative AI models learn from vast chemical libraries to design new molecular structures with desired pharmacological properties, balancing potency, selectivity, and ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) characteristics [1] [4].
Procedure:
- Training Data Preparation: Assemble a curated dataset of known active and inactive compounds against the target. Annotate molecules with properties such as binding affinity, solubility, and metabolic stability.
- Model Selection and Training: Train a Generative Adversarial Network (GAN) or Variational Autoencoder (VAE) on the prepared chemical dataset. The model learns the underlying probability distribution of "drug-like" molecules and their associated properties [4] [8].
- Conditional Generation: Define a target product profile (TPP) specifying desired properties (e.g., high binding affinity, low CYP inhibition). Use this TPP as a conditional input to the generative model to steer the generation of novel molecules meeting these criteria.
- Output Evaluation and Filtering: Generate a library of candidate molecules. Filter them using predictive QSAR and ADMET models to prioritize the most promising leads for synthesis [4].
- Iterative Optimization: Synthesize and test top candidates (e.g., 100-200 compounds) in biochemical and cellular assays. Feed the experimental results back into the AI model as a reinforcement learning signal for the next design cycle, creating a closed-loop optimization system [5].
Pathway and Workflow Visualizations
AI vs Traditional Drug Discovery Funnel
Generative AI de novo Design Workflow
The Scientist's Toolkit: Research Reagent Solutions for AI-Driven Oncology Discovery
Table 3: Essential Research Reagents and Platforms for AI-Driven Oncology Discovery
| Research Reagent / Platform | Type | Function in AI-Driven Discovery | Example Use Case |
|---|---|---|---|
| Patient-Derived Organoids [6] | 3D Cell Culture | Faithfully recapitulates patient tumor biology for validating AI-predicted drug responses. | High-throughput screening of AI-generated compounds; biomarker hypothesis testing. |
| PDX Models [6] | In Vivo Model | Preserves tumor heterogeneity and microenvironment, serving as a gold-standard for in vivo validation of AI-designed candidates. | Final preclinical validation of efficacy and biomarker strategies before clinical trials. |
| CRISPR-Cas9 Screening Libraries [9] | Functional Genomics Tool | Generates genetic dependency data for AI target identification algorithms. | Experimental validation of AI-predicted novel oncogenic vulnerabilities and synthetic lethality. |
| Multi-Omics Datasets (Genomics, Proteomics) [10] [9] | Data Resource | Provides the foundational data for training and validating AI models for target and biomarker discovery. | Input for network-based AI algorithms to identify novel targets and patient stratification biomarkers. |
| AI Drug Discovery Platforms (e.g., Exscientia, Insilico) [5] | Software Platform | Provides integrated environments for generative chemistry, virtual screening, and property prediction. | De novo design of small molecules against novel, AI-identified immuno-oncology targets. |
The integration of AI into the oncology drug discovery pipeline represents a fundamental shift from a slow, sequential, and high-failure process to an integrated, data-driven, and iterative engine. While the traditional pipeline provides a necessary foundation, the AI-accelerated pathway demonstrates compelling advantages in speed, efficiency, and predictive power, as quantified in this application note. The successful implementation of these approaches, supported by the detailed protocols and research tools outlined, holds the potential to reverse the trend of Eroom's Law and deliver more effective, personalized cancer therapies to patients in need.
Application Notes: Core AI Technologies in De Novo Drug Design
The integration of artificial intelligence (AI) is revolutionizing the paradigm of de novo drug design for novel oncology therapeutics. This shift moves the discovery process from a labor-intensive, serendipitous endeavor to a predictive, engineered science. Core AI technologies—Machine Learning (ML), Deep Learning (DL), and Natural Language Processing (NLP)—are enabling the rapid generation and optimization of novel chemical entities with desired properties from scratch, significantly accelerating the path to effective cancer treatments [11] [12].
The following table summarizes the distinct roles and quantitative impact of these core technologies in oncology drug discovery.
Table 1: Core AI Technologies in Oncology Drug Discovery
| AI Technology | Key Function in De Novo Design | Specific Applications in Oncology | Reported Efficacy/Impact |
|---|---|---|---|
| Machine Learning (ML) | Identifies patterns in structure-activity relationships to predict compound properties [4]. | - Quantitative Structure-Activity Relationship (QSAR) modeling [13].- Predicting target binding affinity and ADMET properties [14] [4].- Virtual screening of compound libraries [14]. | Reduces costly late-stage attrition by predicting toxicity and efficacy early [12]. |
| Deep Learning (DL) | Generates novel molecular structures and predicts complex biological interactions using multi-layered neural networks [14] [1]. | - De novo molecule design using Generative Adversarial Networks (GANs) & Variational Autoencoders (VAEs) [14] [4].- Prediction of protein-ligand binding structures (e.g., AlphaFold) [14].- Analysis of histopathology images for biomarker discovery [1]. | Novel drug candidate for idiopathic pulmonary fibrosis designed in 18 months (vs. 3-6 years traditionally) [14] [1]. |
| Natural Language Processing (NLP) | Extracts and structures knowledge from unstructured biomedical text data [15] [16]. | - Mining electronic health records (EHRs) for patient recruitment in clinical trials [14] [15].- Identifying novel drug-target-disease relationships from scientific literature [1].- Named Entity Recognition (NER) for genes, compounds, and diseases [16]. | Identifies eligible patients for clinical trials from EHRs, addressing a major recruitment bottleneck [14] [15]. |
Experimental Protocol: AI-DrivenDe NovoDesign of a Small Molecule Immunomodulator
Objective: To design a novel, potent, and synthetically accessible small molecule inhibitor of the PD-L1 immune checkpoint pathway for cancer immunotherapy using an integrated AI workflow.
Background: Targeting the PD-1/PD-L1 axis with small molecules is structurally challenging but offers advantages over biologics, such as oral bioavailability and better tumor tissue penetration [4]. AI accelerates the identification and optimization of such molecules.
Research Reagent Solutions
Table 2: Essential Research Reagents and Computational Tools
| Item Name | Function/Description | Application in Protocol |
|---|---|---|
| Public Compound Databases (e.g., ChEMBL, PubChem) | Provide large-scale, labeled data on chemical structures and biological activities for model training [13]. | Source of known PD-L1 binders and non-binders for supervised learning. |
| Generative AI Model (e.g., VAE or GAN) | Learns the chemical space of drug-like molecules and generates novel molecular structures [14] [4]. | De novo generation of novel candidate PD-L1 inhibitors. |
| Molecular Docking Software (e.g., AutoDock Vina) | Computationally predicts how a small molecule binds to a protein target's binding site [17]. | Initial virtual screening and ranking of generated molecules based on predicted binding affinity to PD-L1. |
| ADMET Prediction Model | A supervised ML model (e.g., Random Forest, SVM) trained to predict absorption, distribution, metabolism, excretion, and toxicity [13] [4]. | Filters generated molecules for desirable pharmacokinetic and safety profiles early in the pipeline. |
| Reinforcement Learning (RL) Agent | An algorithm that optimizes a sequence of decisions; it is rewarded for generating molecules that meet multiple objectives [4]. | Optimizes the generated molecules iteratively for a combination of high binding affinity, good ADMET properties, and synthetic accessibility. |
Methodology
The following diagram illustrates the multi-stage, iterative workflow for the AI-driven de novo design protocol.
Workflow Diagram 1: AI-Driven De Novo Design Pipeline
Step 1: Data Curation and Preprocessing
- Action: Compile a dataset of known PD-1/PD-L1 inhibitors (active compounds) and decoys (inactive compounds) from public databases like ChEMBL and PubChem [13]. Annotate data with molecular descriptors (e.g., SMILES strings) and experimental binding affinities (e.g., IC50 values).
- Protocol: Standardize chemical structures, remove duplicates, and curate the data to ensure quality. Split the data into training (80%), validation (10%), and test sets (10%).
Step 2: Training the Generative Model
- Action: Train a Deep Learning generative model, such as a Variational Autoencoder (VAE) or a Generative Adversarial Network (GAN), on the curated dataset of drug-like molecules [4].
- Protocol:
- Input: Represent molecules as SMILES strings or molecular graphs.
- Training: The VAE encoder learns to compress molecules into a latent vector space, and the decoder learns to reconstruct them. The model learns the fundamental rules of chemical structure and functionality.
- Validation: Assess the model's ability to generate valid, novel, and unique molecular structures not present in the training set.
Step 3: De Novo Molecule Generation
- Action: Use the trained generative model to create a large library (e.g., 1,000,000) of novel molecular structures.
- Protocol: Sample random vectors from the latent space of the VAE and decode them into new SMILES strings. Alternatively, use the generator from the GAN to produce new structures.
Step 4: Virtual Screening and Molecular Docking
- Action: Screen the generated library in silico to identify molecules with a high predicted affinity for the PD-L1 protein.
- Protocol:
- Pre-screening: Filter molecules based on drug-likeness rules (e.g., Lipinski's Rule of Five).
- Docking: Use software like AutoDock Vina to dock each candidate molecule into the binding site of a 3D crystal structure of PD-L1 [17].
- Scoring: Rank molecules based on their calculated binding free energy (docking score). Select the top 1,000-10,000 candidates for further analysis.
Step 5: In Silico ADMET Prediction
- Action: Employ supervised Machine Learning models to predict the pharmacokinetic and toxicity profiles of the top-ranked candidates [13] [4].
- Protocol: Input the molecular structures of the candidates into pre-trained ML models that predict key properties such as:
- Absorption: Caco-2 permeability.
- Toxicity: hERG channel inhibition (cardiotoxicity).
- Metabolism: Stability in human liver microsomes. Filter out molecules with poor predicted ADMET properties.
Step 6: Multi-parameter Optimization via Reinforcement Learning (RL)
- Action: Iteratively refine the generated molecules to simultaneously optimize multiple properties [4].
- Protocol:
- Define Reward Function: The RL agent receives a positive reward for generating molecules with strong predicted binding affinity, favorable ADMET scores, and high synthetic accessibility.
- Optimization Loop: The agent explores the chemical space by making small modifications to molecular structures. It learns to maximize its cumulative reward over many iterations.
- Output: A focused set of 10-50 lead-like molecules that are optimized for both activity and developability.
Step 7: Experimental Validation
- Action: Synthesize the top AI-prioritized molecules and validate their activity and safety in in vitro and in vivo models.
- Protocol: Proceed to standard preclinical assays, including:
- In vitro binding assays to confirm PD-1/PD-L1 blockade.
- Cell-based assays to measure T-cell reactivation.
- In vivo efficacy studies in mouse cancer models.
- Preliminary toxicity studies.
Experimental Protocol: NLP-Enhanced Patient Stratification for Oncology Clinical Trials
Objective: To use Natural Language Processing (NLP) to efficiently identify and recruit eligible cancer patients for a clinical trial from Electronic Health Records (EHRs).
Background: Patient recruitment is a major bottleneck in clinical development, with about 80% of trials failing to enroll on time [1]. NLP can automate the screening of unstructured clinical notes to find eligible patients [15].
Methodology
The workflow for identifying eligible patients using NLP is outlined below.
Workflow Diagram 2: NLP-Driven Patient Stratification
Step 1: Define Eligibility Criteria
- Action: Translate the trial's formal eligibility criteria (e.g., "Metastatic non-small cell lung cancer," "EGFR wild-type," "No prior immunotherapy") into a structured query format [15].
Step 2: Data Collection and Preprocessing
- Action: Anonymize and aggregate unstructured clinical notes, pathology reports, and discharge summaries from the hospital's EHR system.
Step 3: NLP Text Processing and Named Entity Recognition (NER)
- Action: Process the text to identify and extract key clinical concepts.
- Protocol:
- Model Selection: Use a pre-trained biomedical NLP model like BioBERT or AdaBioBERT, which are specifically designed to recognize biomedical entities [16].
- Entity Extraction: The model scans the text and tags entities such as:
- Diseases: "metastatic adenocarcinoma"
- Genes & Biomarkers: "EGFR", "wild-type"
- Drugs: "pembrolizumab"
- Procedures: "lobectomy"
- Relationship Extraction: Advanced models can determine relationships between entities (e.g., that the "wild-type" status refers to the "EGFR" gene).
Step 4: Structured Data Output
- Action: Convert the extracted information into a structured database (e.g., a table) where each patient has standardized fields for cancer type, biomarkers, treatment history, etc.
Step 5: Apply Eligibility Logic
- Action: Run the structured query from Step 1 against the structured database from Step 4 to automatically flag patients who meet the inclusion/exclusion criteria.
Step 6: Output and Review
- Action: Generate a list of potential candidates for the clinical trial team to review and contact, significantly accelerating the recruitment process [14] [15].
In the field of oncology therapeutics research, de novo drug design represents a paradigm shift, moving away from the incremental modification of existing compounds toward the computational generation of novel molecular entities from scratch [18]. This approach is critically dependent on a clear understanding of three foundational concepts: "hit," "lead," and "chemical space." The integration of artificial intelligence (AI) has revitalized de novo strategies, enabling researchers to navigate the vast chemical universe with unprecedented precision to discover and optimize new cancer treatments [18] [19]. This document delineates these core concepts and provides detailed experimental protocols framed within the context of oncology drug discovery.
Core Conceptual Definitions
The drug discovery pipeline is a multi-stage process that aims to transform a biological hypothesis into a clinically effective drug. The precise definition of key terms at each stage is vital for clear communication and effective strategy among research teams.
Chemical Space: This concept refers to the total ensemble of all possible organic molecules that are theoretically stable and synthesizable. Estimates suggest this space contains up to 10^60 drug-like molecules, a near-infinite landscape from which potential therapeutics can be drawn [19]. Traditional methods, such as high-throughput screening (HTS), explore only a minuscule fraction of this space. De novo design, powered by generative AI, allows researchers to systematically navigate and sample previously inaccessible regions of this chemical universe to identify novel compounds with desired properties from the outset [18] [19].
Hit: A "hit" is a molecule that demonstrates a desired pharmacological effect, such as binding to or modulating the activity of a validated oncology target (e.g., a specific kinase or protein implicated in cancer progression) during initial screening assays [18] [2]. Hits are the starting points in the drug discovery pipeline and are typically identified from large-scale screening of compound libraries or, increasingly, through generative AI models that design molecules tailored to a target [18]. A hit confirms the initial hypothesis that a molecule can interact with the target but usually requires significant optimization to become a viable drug candidate.
Lead: A "lead" compound is a refined version of a hit that has undergone preliminary optimization to improve its properties. The transition from hit to lead focuses on enhancing efficacy, specificity, and drug-like characteristics while minimizing early red flags for toxicity or poor pharmacokinetics [18] [2]. A lead compound possesses a more favorable profile, making it suitable for further extensive optimization and preclinical testing. AI algorithms are particularly valuable in this phase, as they can suggest optimal structural modifications to the core scaffold or its substituents to accelerate this development [18].
Table 1: Key Characteristics of Hits and Leads in Oncology Drug Discovery
| Characteristic | Hit Compound | Lead Compound |
|---|---|---|
| Primary Origin | High-Throughput Screening (HTS) or AI-generated de novo design [18] [1] | Optimized derivative of a hit compound [18] |
| Biological Activity | Confirmed activity against the target in initial assays [2] | Improved potency and selectivity in more complex models [18] |
| Chemical Structure | May have suboptimal properties (e.g., potency, solubility) [18] | Chemically modified scaffold to enhance properties [18] |
| Role in Pipeline | Starting point for further investigation | Candidate for preclinical development [2] |
| Key Goal | Validate interaction with the therapeutic target | Establish a promising profile for a drug candidate [18] |
Quantitative Landscape of Chemical Space
The scale of chemical space underscores both the challenge and the opportunity in drug discovery. The following table quantifies the different scopes of molecular exploration, highlighting the transformative potential of de novo design.
Table 2: The Scale of Explored and Unexplored Chemical Space
| Category | Estimated Number of Molecules | Context and Significance |
|---|---|---|
| Approved Drugs | ~10⁴ [19] | The small number of successfully marketed drugs highlights the high attrition rate in traditional discovery. |
| Large Combinatorial Libraries | Up to 10²⁰ [19] | Represents the largest experimentally accessible libraries, yet is still a tiny fraction of the total chemical space. |
| Total Drug-like Chemical Space | Up to 10⁶⁰ [19] | The vast theoretical universe of possible molecules, which de novo design aims to access computationally. |
Experimental Protocols for Hit Identification and Lead Optimization
The following protocols outline established methodologies for identifying hits and optimizing leads, with an emphasis on the integration of AI-driven de novo design strategies.
Protocol 1: AI-Driven De Novo Hit Identification
Objective: To generate novel hit compounds against a defined oncology target using generative AI models. Application: Initial phase of drug discovery for a new or undrugged target in oncology.
Materials and Reagents:
- Generative AI Software Platform (e.g., AIDDISON): Utilizes algorithms like variational autoencoders (VAEs) or generative adversarial networks (GANs) for molecular generation [1] [19].
- Target Structure: 3D crystal structure or high-quality predicted structure of the target protein (e.g., from Protein Data Bank).
- Training Data: Curated datasets of known active/inactive compounds and ADMET properties from public and proprietary sources [19].
Procedure:
- Target Preparation: Prepare the 3D structure of the oncology target by removing water molecules, adding hydrogen atoms, and defining the binding pocket.
- Model Configuration: Configure the generative AI model with multi-parameter optimization goals, including high binding affinity, favorable drug-likeness (e.g., Lipinski's Rule of Five), and synthetic accessibility [19].
- Molecular Generation: Execute the AI model to generate a library of novel molecular structures. For Structure-Based De Novo Design, the model uses docking scores to guide generation for optimal fit in the binding pocket [19].
- In Silico Hit Validation:
- Docking Analysis: Screen generated molecules using molecular docking simulations against the target to predict binding modes and affinities.
- ADMET Prediction: Employ machine learning models to predict key ADMET properties to filter out compounds with poor predicted pharmacokinetics or toxicity [2].
- Hit Selection: Select a diverse set of top-ranking compounds that meet the predefined criteria for biological activity and drug-like properties as putative hits for experimental validation.
Protocol 2: Hit-to-Lead Optimization via Scaffold Hopping and Decoratio n
Objective: To optimize a confirmed hit into a lead compound by improving its potency, selectivity, and overall drug-like profile. Application: Optimization of a confirmed hit with suboptimal properties.
Materials and Reagents:
- Confirmed Hit Compound: Chemically characterized and biologically tested molecule.
- Generative AI Platform with Scaffold-Hopping Capability: Software capable of suggesting novel core scaffolds while preserving bioactivity [18].
- Medicinal Chemistry Tools: Applications for visualizing and analyzing structure-activity relationships (SAR).
Procedure:
- SAR Analysis: Analyze existing data to identify key pharmacophoric features essential for the hit's biological activity.
- Scaffold Identification: Define the core molecular scaffold of the hit compound.
- AI-Guided Scaffold Hopping: Use the AI platform to generate novel, structurally distinct scaffolds that maintain the critical pharmacophoric features. This explores new intellectual property space and can improve properties [18] [19].
- Scaffold Decoration: For the original or a newly identified scaffold, use the AI model to suggest optimal substituents at various attachment points. This fine-tunes the molecule's interaction with the target and its physical properties [18].
- In Silico Lead Profiling: Rank the optimized compounds based on a weighted score of predicted potency, selectivity over anti-targets, and ADMET properties.
- Synthesis and Testing: Synthesize the top-ranked proposed leads and subject them to in vitro biological testing to confirm improved efficacy and selectivity.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table details key reagents, computational tools, and data resources essential for executing de novo design campaigns in oncology.
Table 3: Key Research Reagents and Solutions for De Novo Design
| Item Name | Function/Application | Specific Use Case in Oncology |
|---|---|---|
| Generative AI Software | Generates novel molecular structures optimized for specific parameters [1] [19]. | De novo design of inhibitors for specific oncology targets like kinases or mutant proteins. |
| Protein Structure Data | Provides the 3D atomic coordinates of a biological target. | Enables structure-based de novo design for targets such as EGFR or KRAS. |
| Curated Compound Libraries | Serves as training data for AI models and source for virtual screening. | Libraries enriched with known oncology drugs and tool compounds improve model predictions for cancer targets. |
| ADMET Prediction Tools | Computationally predicts absorption, distribution, metabolism, excretion, and toxicity. | Early filtering of compounds with potential cardiotoxicity or poor blood-brain barrier penetration for CNS cancers. |
| Molecular Docking Software | Predicts the preferred orientation and binding affinity of a molecule to a target protein. | Validating the binding mode of AI-generated hits to the active site of an oncology target. |
Workflow and Pathway Visualizations
The following diagrams illustrate the logical workflow of the integrated AI-driven de novo design process and a key signaling pathway often targeted in oncology.
AI De Novo Workflow
STK33 Signaling in Cancer
This application note details a standardized protocol for implementing an integrated, artificial intelligence (AI)-driven workflow for de novo drug design, with a specific focus on novel oncology therapeutics. The documented methodology accelerates the early discovery pipeline—from target identification and validation to the generation of novel, optimized molecular entities. By leveraging machine learning (ML) and deep learning (DL), this workflow significantly compresses discovery timelines, reduces reliance on costly empirical screening, and enhances the probability of clinical success for oncology drugs [1] [5]. The protocols below provide a framework for researchers and drug development professionals to adopt and adapt these technologies in their discovery campaigns.
Quantitative Foundations of AI in Drug Discovery
The adoption of AI-driven platforms is supported by compelling quantitative metrics that demonstrate increased efficiency and cost-effectiveness in the drug discovery process.
Table 1: Performance Metrics of AI-Driven vs. Traditional Drug Discovery in Oncology
| Metric | Traditional Discovery | AI-Driven Discovery | Key Supporting Evidence |
|---|---|---|---|
| Early Discovery Timeline | ~3-6 years | 12-18 months | Insilico Medicine developed a preclinical candidate for idiopathic pulmonary fibrosis in under 18 months [1]. |
| Compounds Synthesized | Thousands | Hundreds | Exscientia's CDK7 inhibitor program achieved a clinical candidate after synthesizing only 136 compounds [5]. |
| Design Cycle Efficiency | Baseline | ~70% faster | Exscientia reports AI-driven design cycles that are substantially faster and require 10x fewer synthesized compounds [5]. |
| Target Identification | Several months | Days to weeks | A Top Ten pharmaceutical company reported saving four months in the discovery phase, identifying the right research target faster [20]. |
| Cost Impact | High | Significant reduction | Life sciences researchers report AI is reducing operational costs; one project saved an estimated $42M by cutting research timelines by 90% [20]. |
Table 2: Key AI Platforms and Their Clinical-Stage Contributions (2025 Landscape)
| AI Platform / Company | Core AI Technology | Oncology-Relevant Clinical Candidate(s) | Development Stage (as of 2025) |
|---|---|---|---|
| Exscientia | Generative AI, Centaur Chemist | EXS-21546 (A2A antagonist for IO), GTAEXS-617 (CDK7 inhibitor) | Phase I/II trials; Pipeline prioritized post-Recursion acquisition [5]. |
| Insilico Medicine | Generative Adversarial Networks (GANs) | Novel inhibitors for QPCTL (tumor immune evasion) | Advancing into oncology pipelines [1]. |
| BenevolentAI | Knowledge Graphs, ML | Novel targets in Glioblastoma | Preclinical validation [1]. |
| Recursion | Phenotypic Screening, CNNs | Pipeline enhanced by integration with Exscientia's generative chemistry | Multiple programs in clinical trials [5]. |
Experimental Protocols
Protocol 1: AI-Driven Target Identification and Validation
Objective: To systematically identify and prioritize novel, druggable oncology targets from integrated multi-omics data.
Materials: High-performance computing (HPC) cluster or cloud instance (GPU-accelerated recommended); Access to a purpose-built scientific AI platform (e.g., Causaly) or in-house pipeline; Curated biological databases (e.g., The Cancer Genome Atlas (TCGA), COSMIC, Human Protein Atlas, PubMed, ClinicalTrials.gov).
Procedure:
- Data Aggregation and Curation:
- Compile and pre-process multimodal data, including genomic (DNA sequencing), transcriptomic (RNA-seq), proteomic (mass spectrometry), and epigenomic datasets relevant to the cancer type of interest.
- Incorporate structured and unstructured data from scientific literature and clinical trial reports using Natural Language Processing (NLP) to build a comprehensive knowledge graph [20].
Target Hypothesis Generation:
- Utilize the AI platform to query the integrated data for genes or proteins associated with the desired disease phenotype (e.g., "cell proliferation in glioblastoma").
- Apply network analysis algorithms to identify key nodes (potential targets) within disease-associated biological pathways. BenevolentAI used this approach to predict novel targets in glioblastoma [1].
- Filter generated hypotheses based on genetic evidence (e.g., overexpression, mutation frequency), "druggability" predictions, and novelty relative to the competitive landscape.
Target Prioritization and Rationale:
- The platform should generate a ranked list of targets with fully traceable evidence for each association, linking back to source literature and data [20].
- Manually review the top candidates, focusing on the strength of causal versus correlative relationships, the potential for resistance mechanisms, and the feasibility of developing a high-throughput assay for downstream screening.
Validation Workflow Diagram:
Protocol 2: Generative AI forDe NovoMolecule Design with Active Learning
Objective: To generate novel, synthetically accessible, and target-specific small molecules using a generative AI model refined by iterative active learning cycles.
Materials: A dataset of known active and inactive molecules for the target of interest (e.g., ChEMBL, internal libraries); Cheminformatics software suite (e.g., RDKit); Molecular docking software (e.g., AutoDock Vina, Glide); High-performance computing resources for molecular dynamics simulations; Access to a generative AI framework (e.g., Variational Autoencoder (VAE)).
Procedure:
- Model Initialization and Training:
- Represent molecules in a machine-readable format, typically SMILES (Simplified Molecular-Input Line-Entry System). Tokenize and convert them into one-hot encoding vectors.
- Pre-train a VAE on a large, general molecular dataset (e.g., ZINC) to learn fundamental chemical rules and structures.
- Fine-tune the pre-trained VAE on a target-specific training set to bias the model towards relevant chemical space [21].
Nested Active Learning (AL) Cycles:
- Inner AL Cycle (Chemical Optimization):
- Generate: Sample the fine-tuned VAE to produce a set of novel molecular structures.
- Evaluate: Filter generated molecules using chemoinformatic oracles for drug-likeness (e.g., Lipinski's Rule of Five), synthetic accessibility (SA) score, and structural dissimilarity from the training set.
- Learn: Add molecules that pass the filters to a "temporal-specific set." Use this set to further fine-tune the VAE, reinforcing the generation of molecules with desired chemical properties. Repeat for a predefined number of iterations [21].
- Outer AL Cycle (Affinity Optimization):
- Evaluate: Subject the accumulated molecules from the inner cycles to molecular docking against the target's 3D structure, using the docking score as an affinity oracle.
- Learn: Transfer molecules with favorable docking scores to a "permanent-specific set." Use this high-quality set to fine-tune the VAE, directly steering the generative process towards high-affinity chemical space [21].
- Iterate between inner and outer AL cycles to progressively optimize for both chemical excellence and target engagement.
- Inner AL Cycle (Chemical Optimization):
Candidate Selection and In Silico Validation:
- Apply stringent filters to the final "permanent-specific set," selecting molecules with the best docking scores, SA, and novelty.
- Perform advanced molecular modeling, such as absolute binding free energy (ABFE) simulations or Monte Carlo methods (e.g., PELE), to refine the selection of the most promising candidates for synthesis and in vitro testing [21].
Active Learning Workflow Diagram:
Key Signaling Pathways in Oncology for AI-Driven Discovery
PD-1/PD-L1 Immune Checkpoint Pathway: A primary target for cancer immunotherapy. AI can design small molecules to disrupt the PD-1/PD-L1 protein-protein interaction, a strategy complementary to monoclonal antibodies [4]. These small molecules can inhibit PD-L1 dimerization or promote its degradation, potentially offering improved tissue penetration and oral bioavailability [4].
Tumor Microenvironment (TME) Metabolic Pathways: Targets like the IDO1 (Indoleamine 2,3-dioxygenase 1) enzyme, which catalyzes tryptophan degradation, creating an immunosuppressive TME. AI-driven models are used to design novel IDO1 inhibitors to reverse this suppression and reinvigorate T-cell responses [4].
Oncogenic Signaling (e.g., KRAS): Once considered "undruggable," KRAS is now a high-priority target. AI-generative models have been successfully tested to design novel inhibitors for KRAS, exploring scaffolds distinct from known ones, even in sparsely populated chemical spaces [21].
Pathway Diagram for PD-1/PD-L1 and IDO1:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for AI-Driven Oncology Drug Discovery
| Research Reagent / Resource | Function in the Workflow | Specific Application Example |
|---|---|---|
| Multi-omics Databases (e.g., TCGA) | Provides comprehensive molecular profiling data for human tumors. | Used as primary input data for AI-driven target identification and patient stratification [1] [10]. |
| Scientific AI Platform (e.g., Causaly, BenevolentAI) | Aggregates and structures public and private biomedical evidence using NLP and knowledge graphs. | Accelerates target identification and validation by uncovering causal biological relationships from vast literature [20]. |
| Generative AI Model (e.g., VAE, GAN) | Learns the structure of chemical space and generates novel molecular entities from scratch. | Core engine for de novo molecule design, as in the VAE-Active Learning workflow [21]. |
| Cheminformatics Suite (e.g., RDKit) | Provides computational tools for analyzing and manipulating chemical structures. | Used to calculate molecular properties, filter for drug-likeness, and assess synthetic accessibility [21]. |
| Molecular Docking Software (e.g., AutoDock Vina) | Predicts the preferred orientation and binding affinity of a small molecule to a protein target. | Serves as the "affinity oracle" in the active learning cycle to prioritize molecules for synthesis [21]. |
| Patient-Derived Organoids / Ex Vivo Models | Provides biologically relevant, human-derived systems for testing compound efficacy. | Used to validate AI-designed compounds in a more translational context, as exemplified by Exscientia's acquisition of Allcyte [5]. |
Generative AI in Action: Core Methodologies for Designing Novel Cancer Drugs
The advent of artificial intelligence (AI) has catalyzed a paradigm shift in computational chemistry and drug discovery, transitioning the field from reliance on manually engineered descriptors to the automated extraction of molecular features using deep learning [22]. Central to this transformation is the choice of molecular representation—the method of encoding chemical structures into a computationally tractable format [23]. The representation serves as the foundational layer upon which models learn, directly influencing their ability to predict molecular properties, generate novel compounds, and ultimately accelerate the discovery of new oncology therapeutics.
Within the context of de novo drug design for novel oncology research, selecting an appropriate molecular representation is crucial for creating effective AI-driven workflows. This document provides detailed Application Notes and Protocols for the three predominant molecular representations: SMILES (Simplified Molecular Input Line Entry System), SELFIES (SELF-referencing Embedded String), and Molecular Graphs. We summarize their comparative performance, provide protocols for their implementation, and visualize their roles in an integrated drug discovery pipeline.
String-Based Representations: SMILES and SELFIES
SMILES (Simplified Molecular Input Line Entry System) is a linear notation system that represents a molecule's structure using ASCII strings, describing atoms, bonds, and ring structures [23] [24]. Despite its widespread use, SMILES has inherent limitations, including non-uniqueness (a single molecule can have multiple valid SMILES strings) and semantic fragility, where small string mutations can lead to invalid molecules [25] [26].
SELFIES (SELF-referencing Embedded String) is a more robust string-based representation developed to guarantee 100% syntactic and semantic validity [25] [27]. Every possible SELFIES string corresponds to a valid molecule, making it particularly advantageous for generative models in de novo design [26]. This robustness has enabled its successful application in platforms like DeLA-DrugSelf for multi-objective optimization of bioactive molecules [26].
Graph-Based Representations: Molecular Graphs
Molecular Graphs explicitly represent a molecule's structure as a mathematical graph ( G = (V, E) ), where atoms are nodes (V) and bonds are edges (E) [23]. This representation naturally captures the topological structure of molecules and can be enriched with node and edge features (e.g., atom type, formal charge, bond type) [23]. Molecular graphs are the backbone of Graph Neural Networks (GNNs), which have demonstrated superior performance in many molecular property prediction tasks [22] [28]. Furthermore, graph-based crossover operators in genetic algorithms have shown high performance in generating diverse and plausible candidate molecules for drug discovery [29].
Quantitative Comparison of Representation Performance
The table below summarizes a quantitative comparison of SMILES-, SELFIES-, and Graph-based models on benchmark molecular generation tasks, as reported in recent literature. Performance is measured by the Wasserstein distance (lower is better) between property distributions of generated and test molecules, indicating how well the model learns the target distribution [24].
Table 1: Performance Comparison of Molecular Representations on Complex Generation Tasks (Wasserstein Distance). Lower values indicate better performance.
| Representation | Model Type | Penalized LogP Task | Multimodal Distribution Task | Large Molecules Task | Validity (%) | Uniqueness (%) |
|---|---|---|---|---|---|---|
| SMILES | RNN (SM-RNN) | 0.095 | 0.109 | 3.482 | >99% [24] | High [24] |
| SELFIES | RNN (SF-RNN) | 0.177 | 0.132 | 4.789 | ~100% [25] | High [24] |
| Molecular Graph | JTVAE | 0.536 | 0.245 | 18.16 | ~100% [24] | Moderate [24] |
| Molecular Graph | CGVAE | 1.000 | 0.426 | 22.69 | ~100% [24] | Moderate [24] |
| Hybrid (Multi-View) | MoL-MoE [28] | - | - | - | - | - |
Table 2: Qualitative Comparison of Molecular Representation Characteristics.
| Representation | Robustness | Interpretability | Ease of Generation | Information Captured |
|---|---|---|---|---|
| SMILES | Low: Sensitive to small changes [25] | Medium: Readable but non-unique | High: Simple string-based models | 2D molecular structure |
| SELFIES | High: Every string is valid [27] | Low: Less human-readable | High: Simple string-based models | 2D molecular structure |
| Molecular Graph | High: Inherently structured | High: Direct structural mapping | Medium: Requires complex GNN architectures | 2D/3D topology and features |
Application Notes forDe NovoDrug Design
Selecting a Representation for Oncology Drug Discovery
The choice of molecular representation should be guided by the specific goals and constraints of the oncology research project:
- For goal-directed optimization of known scaffolds, where exploring a constrained chemical space around a lead compound is key, SELFIES-based models are highly recommended. Their robustness ensures a high yield of valid molecules during optimization, as demonstrated in the DeLA-DrugSelf platform for CB2R ligand optimization [26].
- For exploring vast chemical spaces or generating entirely novel scaffolds, graph-based representations and genetic algorithms with cut-and-join crossover operators can produce highly diverse and synthesizable molecules [29]. The REvoLd system successfully utilized this approach to find candidate molecules with binding constants exceeding known binders for several target proteins [29].
- For multi-task property prediction or when data is limited, hybrid models that integrate multiple representations (SMILES, SELFIES, graphs) can leverage complementary strengths. The MoL-MoE framework demonstrated superior performance on various MoleculeNet benchmarks by dynamically weighting experts from different modalities [28].
- For structure-based design, where explicit 3D protein binding site information is required, 3D graph-based approaches are essential. The DRAGONFLY framework successfully integrated 3D protein binding site graphs with ligand information for the de novo design of potent PPARγ partial agonists, with crystal structures confirming the anticipated binding modes [30].
Integrated Workflow forDe NovoDesign
The following diagram illustrates a recommended protocol integrating multiple molecular representations within a de novo drug design cycle for oncology therapeutics.
Protocols
Protocol 1: Implementing a SELFIES-Based Generative Model for Scaffold Optimization
This protocol outlines the steps for using a SELFIES-based generative model, like DeLA-DrugSelf, to optimize a starting bioactive molecule for an oncology target [26].
Research Reagent Solutions Table 3: Essential reagents and computational tools for Protocol 1.
| Item | Function/Description | Example/Source |
|---|---|---|
| Starting Query Molecule | The known bioactive molecule to be optimized. | e.g., a known inhibitor from corporate or public databases (ChEMBL). |
| SELFIES Encoder | Converts the molecular structure into a SELFIES string. | Open-source libraries: selfies (Python). |
| DeLA-DrugSelf Algorithm | The generative algorithm performing mutations (substitutions, insertions, deletions). | https://www.ba.ic.cnr.it/softwareic/delaself/ [26] |
| Fitness Function | Multi-objective function evaluating generated compounds (e.g., binding affinity, solubility, synthetic accessibility). | User-defined based on project goals; can use Pareto dominance. |
| Filtering Pipeline | Removes SELFIES-related collapse issues and applies drug-likeness rules (e.g., Lipinski's Rule of Five). | Integrated in DeLA-DrugSelf; can be customized with RDKit. |
Procedure
- Input Preparation: Select a starting query molecule with known activity against the oncology target of interest. Convert this molecule into its SELFIES representation using a SELFIES encoder.
- Algorithm Initialization: Configure the DeLA-DrugSelf algorithm with the initial SELFIES string and set the parameters for the genetic operations (mutation and crossover rates).
- Generation Loop: Execute the algorithm. In each iteration, DeLA-DrugSelf will generate new SELFIES strings by applying substitutions, insertions, and deletions to the parent string(s).
- Collapse Check and Validation: Decode all newly generated SELFIES strings to molecular structures. Explicitly check for and discard any compounds that encounter SELFIES-related collapse issues, retaining only collapse-free structures [26].
- Fitness Evaluation: Evaluate the validated compounds using the multi-objective fitness function. This function should incorporate predictions for key properties relevant to oncology drugs, such as target binding affinity (from a QSAR model), permeability, and metabolic stability.
- Selection and Iteration: Select the top-performing compounds based on the fitness score to serve as parents for the next generation. Repeat steps 3-5 for a predefined number of generations or until convergence criteria are met.
- Output: The final output is a library of optimized, novel compounds prioritized for further computational analysis and experimental validation.
Protocol 2: Structure-BasedDe NovoDesign with 3D Molecular Graphs (DRAGONFLY Framework)
This protocol describes the methodology for using the DRAGONFLY framework, which utilizes deep interactome learning on 3D graphs for structure-based molecular generation [30].
Research Reagent Solutions Table 4: Essential reagents and computational tools for Protocol 2.
| Item | Function/Description | Example/Source |
|---|---|---|
| Target Protein Structure | 3D structure of the oncology target's binding site. | Protein Data Bank (PDB), homology model. |
| Drug-Target Interactome | A graph database of known ligand-target interactions for pre-training. | Curated from ChEMBL [30]. |
| Graph Transformer Neural Network (GTNN) | Encodes the 3D protein binding site graph into a latent representation. | Core component of DRAGONFLY [30]. |
| Chemical Language Model (LSTM) | Decodes the latent representation into a SMILES string of a novel ligand. | Core component of DRAGONFLY [30]. |
| QSAR Models | Predicts pIC50 values for generated molecules against the target. | Kernel Ridge Regression (KRR) models with ECFP4, CATS, USRCAT descriptors [30]. |
| Synthesizability Filter | Assesses the feasibility of synthesizing the generated molecule. | Retrosynthetic Accessibility Score (RAScore) [30]. |
Procedure
- Data Curation and Interactome Construction: Compile a structure-based interactome comprising macromolecular targets with known 3D structures and their associated ligands (with binding affinity ≤ 200 nM). This serves as the pre-training dataset [30].
- Target Binding Site Representation: For the target protein of interest, represent the 3D binding site as a graph. Nodes represent key residues or pharmacophore features, and edges represent spatial relationships or interactions.
- Model Inference ("Zero-Shot" Generation): Input the target binding site graph into the pre-trained DRAGONFLY model. The model, which combines a GTNN and an LSTM, will process the graph and generate novel, drug-like molecules predicted to bind the site, without requiring application-specific fine-tuning [30].
- Computational Validation: Screen the generated molecules using the following steps: a. On-Target Bioactivity Prediction: Use pre-trained QSAR models (e.g., KRR with ECFP4 descriptors) to predict pIC50 values for the generated molecules against the target [30]. b. Synthesizability Assessment: Calculate the RAScore for each molecule to prioritize synthetically accessible compounds [30]. c. Selectivity and Off-Target Profiling: Use similar QSAR models to predict activity against related anti-targets (e.g., other nuclear receptors) to assess selectivity.
- Hit Prioritization and Experimental Validation: Chemically synthesize the top-ranking computational designs. Characterize them biophysically (e.g., Surface Plasmon Resonance) and biochemically to confirm binding and functional activity. Determine the crystal structure of the ligand-receptor complex to validate the predicted binding mode [30].
The workflow for this structure-based protocol is visualized below.
Application Notes
Generative artificial intelligence (AI) has transitioned from a proof-of-concept technology to a central pillar of modern de novo drug design, particularly for oncology therapeutics. Faced with rising research and development costs, multi-year timelines, and high attrition rates, the pharmaceutical industry is increasingly adopting AI-driven approaches to explore the vast theoretical chemical space (estimated at 10³³–10⁶³ drug-like molecules) efficiently [31]. Among the most impactful architectures are Variational Autoencoders (VAEs), Generative Adversarial Networks (GANs), and Transformers. These models enhance the "design–make–test–analyze" (DMTA) cycle by generating novel, optimized molecular structures with desired pharmacological properties, thereby accelerating the journey from target identification to clinical candidates [31] [4]. In oncology, this is critical for designing novel immunomodulators, kinase inhibitors, and therapies against drug-resistant cancers.
Quantitative Performance Comparison of Generative Models
The following table summarizes key performance metrics for different generative model architectures as reported in recent literature and benchmarks.
Table 1: Performance Metrics of Generative Model Architectures in De Novo Drug Design
| Model Architecture | Reported Validity (%) | Novelty (%) | Uniqueness (%) | Internal Diversity (intDiv2, %) | Key Application Strengths |
|---|---|---|---|---|---|
| PCF-VAE (Posterior Collapse Free VAE) [32] | 95.01 - 98.01 | 93.77 - 95.01 | 100 | 85.87 - 86.33 | Mitigates posterior collapse; high diversity and validity. |
| ScafVAE (Scaffold-Aware VAE) [33] | High (Model-specific) | High (Model-specific) | High (Model-specific) | High (Model-specific) | Multi-objective optimization; scaffold-based generation. |
| VGAN-DTI (VGAE + GAN for DTI) [34] | High (Model-specific) | High (Model-specific) | High (Model-specific) | N/R | High DTI prediction accuracy (96% accuracy, 94% F1-score). |
| Transformer-Based Models [31] | High | High | High | N/R | Scaffold hopping; molecular optimization via NLP-inspired edits. |
| GAN-Based Models (e.g., MolGAN) [31] [35] | Variable (Can suffer from mode collapse) | High | High | N/R | Generation of structurally diverse compounds. |
N/R: Not explicitly reported in the summarized search results. Metrics for VAE models like PCF-VAE can vary based on the diversity level (D) parameter and training setup [32].
Oncology-Focused Applications
Targeting Immune Checkpoints and the Tumor Microenvironment (TME)
Generative models are pivotal for designing small-molecule immunomodulators, which offer advantages over biologics like monoclonal antibodies, including oral bioavailability and better penetration into solid tumors [4].
- VAEs and GANs are used to generate inhibitors for intracellular targets like IDO1 (Indoleamine 2,3-dioxygenase 1), an enzyme that contributes to immunosuppression in the TME [4].
- Transformers and VAEs help design small molecules that disrupt the PD-1/PD-L1 interaction, a critical immune checkpoint, by promoting PD-L1 degradation or inhibiting its dimerization [4].
Overcoming Drug Resistance in Cancer Therapy
A key application is the de novo design of dual-target drug candidates to combat drug resistance through various mechanisms, such as synthetic lethality [33].
- Scaffold-aware VAEs (ScafVAE) have been successfully employed to generate molecules with strong binding affinity for two distinct target proteins involved in cancer resistance pathways. This is achieved while simultaneously optimizing other properties like drug-likeness (QED) and synthetic accessibility (SA) [33].
Scaffold Hopping and Lead Optimization
Generative models enable scaffold hopping—creating novel molecular cores that retain biological activity but offer improved properties.
- Transformers, trained on vast molecular corpora, can suggest chemist-like edits and novel scaffolds, escaping existing intellectual property or improving selectivity [31].
- VAEs with Bayesian optimization in their latent space can efficiently explore and optimize known scaffolds to improve potency, selectivity, and ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) profiles [31] [33].
Experimental Protocols
Protocol 1: De Novo Molecule Generation using a Scaffold-Aware VAE (ScafVAE)
Principle
This protocol outlines the procedure for generating novel, multi-objective drug candidates using ScafVAE, a graph-based variational autoencoder. Its bond scaffold-based generation approach expands the accessible chemical space while ensuring high chemical validity and synthetic accessibility, making it particularly suitable for designing oncology therapeutics [33].
Reagents and Materials
Table 2: Research Reagent Solutions for ScafVAE Protocol
| Item | Function/Description | Example/Note |
|---|---|---|
| Molecular Dataset | Provides training data for the model. | ZINC, ChEMBL, QM9, or proprietary corporate libraries. |
| Protein Structures | For structure-based validation via docking. | From Protein Data Bank (PDB) or AlphaFold2 predictions. |
| Surrogate Model Datasets | Train property prediction models on the latent space. | ADMET, QED, SA scores, or experimental binding affinity data. |
| High-Performance Computing (HPC) Cluster | Provides computational resources for training and inference. | Equipped with multiple GPUs (e.g., NVIDIA A100/V100). |
| Molecular Dynamics (MD) Simulation Software | Validates binding stability of generated molecules. | GROMACS, AMBER, or Desmond. |
| Docking Software | Computationally assesses binding affinity. | AutoDock Vina, Glide, or GOLD. |
Workflow Diagram
Diagram Title: ScafVAE Multi-Objective Molecule Generation Workflow
Step-by-Step Procedure
Data Preprocessing and Perplexity-Inspired Fragmentation
- Input: A large dataset of molecules (e.g., from ZINC or ChEMBL) in SMILES or graph format.
- Action: A pre-trained masked graph model (the "perplexity estimator") calculates a perplexity score for each bond in a molecule, which reflects the bond's predictability and uncertainty. Bonds with high perplexity are prioritized as potential breakpoints for fragmentation. This data-driven approach generates a comprehensive set of molecular fragments and "bond scaffolds" (scaffolds where atom types are unspecified) [33].
Model Training: Encoder and Decoder
- Encoder: A Graph Neural Network (GNN) combined with a Recurrent GNN (RGNN) encodes each molecular graph into a low-dimensional, continuous latent vector (z) following a Gaussian distribution. This maps the molecule into a probabilistic latent space [33].
- Decoder: The decoder network performs bond scaffold-based generation. It first assembles fragments into a complete bond scaffold by specifying connected bonds, then decorates the scaffold with specific atom types to produce a valid molecular structure. This process preserves the benefits of fragment-based approaches while accessing a wider chemical space [33].
- Training Objective: The model is trained to minimize the reconstruction loss (difference between original and reconstructed molecule) and the Kullback-Leibler (KL) divergence, which regularizes the latent space [34] [33].
Surrogate Model Augmentation
- Input: The latent vectors (z) from the trained encoder.
- Action: Shallow Multilayer Perceptrons (MLPs) are applied to the latent vectors, followed by task-specific machine learning modules, to predict molecular properties. The model is augmented using contrastive learning and molecular fingerprint reconstruction to improve prediction accuracy, especially for scarce experimental data (e.g., ADMET properties) [33].
Multi-Objective Optimization and Sampling
- Input: Desired property profiles (e.g., strong binding to two oncology targets, high QED, low toxicity).
- Action: Using the trained surrogate models, an optimization algorithm (e.g., Bayesian optimization) navigates the latent space to find vectors (z) that maximize the desired multi-objective function. This allows for the targeted generation of dual-target drug candidates or molecules with other optimized property combinations [33].
Generation and Validation
- Action: The optimized latent vectors are decoded by the ScafVAE decoder to generate novel molecular structures.
- Validation:
- Computational: Assess generated molecules with docking simulations, ADMET prediction tools, and synthetic accessibility (SA) scores [31] [33].
- Experimental: Promising candidates proceed to in vitro biochemical/biophysical assays and cell-based assays for functional validation in a relevant biological context [31].
Protocol 2: Predicting Drug-Target Interactions (DTI) using a Hybrid VAE-GAN Framework
Principle
This protocol describes a framework (VGAN-DTI) that combines VAEs, GANs, and MLPs to accurately predict drug-target interactions, a critical step in early-stage drug discovery for identifying potential oncology therapeutics [34].
Workflow Diagram
Diagram Title: Hybrid VAE-GAN Framework for DTI Prediction
Step-by-Step Procedure
Data Preparation
- Input: Gather datasets of known drug-target interactions (e.g., from BindingDB). Represent drug molecules as feature vectors (e.g., molecular fingerprints or SMILES strings) and target proteins as sequences or structural features [34].
Feature Refinement with VAE
- Action: The VAE's encoder network (
f_θ) maps the input molecular features (x) to a latent space distribution, characterized by a mean (μ) and log-variance (log σ²). A latent vector (z) is sampled from this distribution:z ~ N(μ, σ²). - The VAE's decoder network (
g_φ) then reconstructs the molecular features from (z). The VAE is trained by minimizing a loss function that combines reconstruction loss and the KL divergence to ensure a smooth, well-structured latent space [34].
- Action: The VAE's encoder network (
Diverse Molecule Generation with GAN
- Action: In parallel, a GAN's generator network (G) takes a random noise vector and generates novel molecular feature vectors. The discriminator network (D) is trained to distinguish between real molecules from the dataset and synthetic molecules generated by (G).
- The generator and discriminator are trained adversarially, leading to the generation of diverse and realistic molecular structures [34].
Feature Integration and MLP Prediction
- Action: The refined features from the VAE pathway and the diverse molecules from the GAN pathway are combined with target protein features.
- This combined feature set is fed into a Multilayer Perceptron (MLP) classifier/regressor. The MLP, typically composed of multiple fully connected layers with non-linear activation functions (e.g., ReLU), is trained to predict the probability of interaction or the binding affinity between the drug and the target [34].
Model Evaluation and Validation
- Action: The VGAN-DTI framework is evaluated on held-out test sets from BindingDB. Performance is measured using accuracy, precision, recall, F1-score, and other relevant metrics. The model has been shown to achieve high performance (e.g., 96% accuracy, 95% precision) [34].
- Ablation Studies: Conduct rigorous ablation studies to validate the contribution of each component (VAE, GAN, MLP) to the overall predictive robustness [34].
Ligand-Based vs. Structure-Based De Novo Design Approaches
De novo drug design encompasses computational methods to generate novel molecular entities from scratch, offering a powerful strategy to explore vast regions of the chemical space inaccessible to conventional screening techniques. Within modern oncology drug discovery, two dominant computational paradigms have emerged: ligand-based and structure-based de novo design [36] [37]. The ligand-based approach relies on the known bioactive properties of existing compounds to generate new molecules with similar activities, without requiring direct knowledge of the target's three-dimensional structure. In contrast, the structure-based approach utilizes the atomic-level details of a target protein's binding site to design molecules with complementary steric and chemical features [36] [38]. As the number of determined and predicted protein structures grows exponentially, particularly with advancements like AlphaFold, structure-based methods are gaining unprecedented traction [36]. However, both methodologies offer distinct advantages and face unique challenges. This application note provides a detailed comparison of these approaches, supplemented with experimental protocols and resource guidelines, framed within the context of developing novel oncology therapeutics.
Conceptual Foundations and Comparative Analysis
Ligand-Based De Novo Design
Ligand-based design operates on the principle of "molecular similarity," which posits that structurally similar molecules are likely to exhibit similar biological activities. This approach is particularly valuable when the three-dimensional structure of the target protein is unknown, but a set of active ligands has been identified through experimental assays.
Core Methodology: The process typically begins with the compilation of a training set of known active molecules. Chemical language models (CLMs), a subset of deep learning models, are then pre-trained on large libraries of drug-like molecules to learn the underlying "grammar" of chemistry [37]. These models, often using Simplified Molecular Input Line Entry System (SMILES) strings or molecular graphs as input, can be fine-tuned on the specific set of active ligands. Once trained, they generate novel molecular structures that inhabit the same chemical space as the training actives but possess novel scaffolds [37]. Advanced implementations, such as the DRAGONFLY framework, leverage drug-target interactome data, capturing connections between ligands and their macromolecular targets to guide the generation process [37].
Key Advantages: Its primary strength is the ability to propose novel bioactive molecules in the absence of a protein structure. Furthermore, it can rapidly generate large, diverse virtual libraries tailored to possess specific physicochemical properties like molecular weight, lipophilicity, and polar surface area, which are crucial for drug-likeness and synthesizability [37].
Structure-Based De Novo Design
Structure-based design directly leverages the 3D structure of a biological target to design molecules that fit precisely within a binding pocket. This is the computational equivalent of crafting a key for a specific lock.
Core Methodology: This approach often starts with the 3D coordinates of a protein's binding site, obtained from X-ray crystallography, cryo-electron microscopy, or computational prediction [36]. A plethora of sampling algorithms are then employed:
- Fragment-Based Methods: These include growing (building a molecule from an initial anchor fragment), linking (connecting two fragments that bind to proximal sites), and merging (combining features of overlapping fragments) [36]. Tools like LigBuilder and OpenGrowth implement these strategies [36].
- Deep Generative Models: Modern AI methods, such as RFdiffusion for antibodies and CMD-GEN for small molecules, generate binder structures or pharmacophore point clouds conditioned on the protein pocket [39] [38]. For instance, CMD-GEN uses a coarse-grained pharmacophore sampling module to propose critical interaction points within the pocket, which are subsequently translated into full molecular structures [38].
- Evolutionary Algorithms and Monte Carlo Methods: These heuristics iteratively generate and score populations of molecules, optimizing them for high binding affinity and favorable properties [36].
Scoring and Validation: Proposed molecules are evaluated using scoring functions that estimate binding affinity. These can be physics-based force fields, empirical potentials, or knowledge-based functions [36]. The designs are often filtered using structure prediction tools; for example, a fine-tuned RoseTTAFold2 can validate designed antibody-antigen complexes by recapitulating the intended binding mode [39].
Table 1: Comparative Analysis of De Novo Design Approaches
| Feature | Ligand-Based Design | Structure-Based Design |
|---|---|---|
| Prerequisite | Set of known active ligands | 3D structure of the target protein |
| Underlying Principle | Molecular similarity & QSAR | Molecular complementarity & docking |
| Chemical Space Exploration | Explores space similar to known actives; can be limited by training data | Can access entirely novel scaffolds and binding modes |
| Handling Novel Targets | Not applicable without known actives | Directly applicable, especially with AlphaFold models |
| Primary Challenge | Scaffold hopping beyond the training data; no direct control over binding mode | Accurate prediction of binding affinity and solvation effects |
| Synthetic Accessibility | Can be explicitly optimized during generation (e.g., using RAScore) [37] | Often a historical challenge; addressed by reaction-rule based methods [36] |
| Example Tools/Platforms | DRAGONFLY (CLM), alvaBuilder [37] [40] | RFdiffusion (Antibodies), CMD-GEN, LigBuilder, de novoDOCK [39] [38] [36] |
Quantitative Benchmarking of Generated Libraries
The performance of de novo design methods is quantitatively assessed using a suite of computational metrics that evaluate the quality, utility, and novelty of the generated molecular libraries.
Table 2: Key Performance Metrics for De Novo Design Outputs
| Metric | Description | Interpretation in Drug Discovery |
|---|---|---|
| Validity | Percentage of generated molecules that are chemically plausible [38]. | High validity indicates a robust generative model. |
| Uniqueness | Percentage of unique molecules within the generated library [38]. | Low uniqueness suggests model collapse and lack of diversity. |
| Novelty | Measure of structural dissimilarity from known training set molecules [38] [37]. | High novelty is key for intellectual property and discovering new scaffolds. |
| Synthetic Accessibility (SA) | Score predicting the ease of synthesis (e.g., SAscore, RAScore) [40] [37]. | Critical for ensuring that designs can be physically made and tested. |
| Drug-Likeness (QED) | Quantitative Estimate of Drug-likeness [40]. | Filters out molecules with undesirable physicochemical properties. |
| Self-Consistency | For structure-based designs, the similarity between the designed structure and the structure predicted for its sequence (e.g., by AlphaFold) [39]. | A high score correlates with a higher probability of experimental success. |
Experimental Protocols and Workflows
Protocol 1: Ligand-BasedDe NovoDesign Using a Chemical Language Model
This protocol outlines the steps for generating novel inhibitors for a cancer target (e.g., IDO1) using a ligand-based approach, assuming a set of known active compounds is available but a protein structure is not.
Workflow Diagram: Ligand-Based Design with a CLM
Step-by-Step Procedure:
Data Curation and Preparation
- Source a set of known active molecules (e.g., IC50 ≤ 10 µM) from public databases like ChEMBL for your specific oncology target (e.g., IDO1) [40] [37].
- Curate the data by standardizing structures, removing duplicates, and neutralizing charges using toolkits like RDKit.
- Compute molecular descriptors (e.g., Molecular Weight, HBD, HBA, LogP, TPSA) for the active set to define the property ranges for the scoring function [40].
Model Setup and Training
- Select a CLM architecture, such as a Recurrent Neural Network (RNN) with Long Short-Term Memory (LSTM) or a Transformer model, capable of processing SMILES strings [37].
- Pre-train the model on a large, general database of drug-like molecules (e.g., ChEMBL) to learn fundamental chemical rules [37].
- Fine-tune the pre-trained model on the curated set of target-specific active molecules. This step biases the model's generation toward the relevant chemical space.
Library Generation and Filtering
- Generate a virtual library of 10,000-100,000 molecules using the fine-tuned model. Frameworks like DRAGONFLY can perform this in a "zero-shot" manner, conditioned on the desired bioactivity and properties without further fine-tuning [37].
- Filter the generated library based on:
- Assess novelty by comparing generated molecules against the training set and public databases to ensure scaffold innovation.
In Silico Validation
- Develop a validated QSAR model using the known actives and inactives. Use kernel ridge regression (KRR) with molecular descriptors like ECFP4 and CATS for robust prediction [37].
- Predict the pIC50 of the top-filtered designs using the QSAR model to prioritize the most promising candidates for synthesis.
Protocol 2: Structure-BasedDe NovoDesign for a Selective Inhibitor
This protocol details the design of a selective inhibitor for a kinase target (e.g., PARP1) using a structure-based generative model, requiring a 3D structure of the target protein.
Workflow Diagram: Structure-Based Design with a Generative Model
Step-by-Step Procedure:
Protein Structure Preparation
- Obtain the high-resolution 3D structure of the target (e.g., PARP1, PDB ID: 7ONS) and any related anti-targets (e.g., PARP2) for selectivity assessment [38].
- Prepare the structure using molecular modeling software: add hydrogens, assign partial charges, and optimize side-chain orientations for unresolved residues.
- Define the binding pocket coordinates based on the location of a co-crystallized native ligand or a known catalytic site.
Conditional Molecular Generation
- Employ a structure-based generative model like CMD-GEN [38].
- Sample coarse-grained pharmacophore points within the defined binding pocket. The model learns to generate combinations of interaction features (e.g., hydrogen bond donors, acceptors, hydrophobic regions) that complement the pocket's topography and chemistry.
- Generate full molecular structures from the sampled pharmacophore point clouds. The model's GCPG (Gating Condition Mechanism and Pharmacophore Constraints) module translates these points into chemically valid structures with optimized properties.
In-Silico Validation and Selectivity Analysis
- Perform molecular docking of the top-generated designs into the target (PARP1) and anti-target (PARP2) binding sites using programs like AutoDock Vina or LeDock [40].
- Analyze binding poses to confirm the designed molecular conformation is maintained and key interactions are formed.
- Calculate binding affinity. Use more computationally intensive methods like MM/GBSA or scoring functions in Rosetta to calculate the estimated change in binding free energy (ddG) [39]. Designs with a significantly higher predicted affinity for the target over the anti-target are prioritized.
- Predict structural self-consistency. For the final candidates, run the designed sequence through a structure predictor like AlphaFold2 or a fine-tuned RoseTTAFold2 to check if the predicted unbound structure is consistent with the design intent [39].
Successful implementation of de novo design relies on a suite of computational tools, databases, and finally, experimental reagents for validation.
Table 3: Key Research Reagent Solutions for De Novo Design and Validation
| Category | Item / Resource | Function and Application |
|---|---|---|
| Software & Platforms | alvaBuilder [40] | Ligand-based de novo design using a training set of active molecules. |
| LigBuilder [36] [40] | Structure-based de novo design implementing fragment growing/linking strategies. | |
| RFdiffusion [39] | A deep learning (diffusion) model for de novo protein and antibody design. | |
| CMD-GEN [38] | A deep learning framework for structure-based generation of small molecules. | |
| DRAGONFLY [37] | An interactome-based deep learning model for ligand- and structure-based design. | |
| Databases | ChEMBL [40] [37] | A manually curated database of bioactive molecules with drug-like properties. |
| Protein Data Bank (PDB) | A repository for the 3D structural data of proteins and nucleic acids. | |
| ZINC | A free database of commercially available compounds for virtual screening. | |
| Experimental Validation Reagents | Purified Target Protein | Required for in vitro binding affinity assays (e.g., SPR) and enzymatic inhibition assays. |
| Cell Lines | Engineered cell lines (e.g., overexpressing the target oncogene) for cellular efficacy and cytotoxicity assays (e.g., MTT assay). | |
| Antibodies for Western Blot | To analyze downstream signaling pathway modulation (e.g., p-STAT3 levels) upon treatment [2]. | |
| In Vivo Model | Patient-derived xenograft (PDX) or cell-line-derived xenograft (CDX) mouse models for in vivo efficacy studies [2]. |
Both ligand-based and structure-based de novo design are indispensable pillars of modern computational oncology. The choice between them is dictated by the available information: ligand-based methods excel when active compounds are known but structural data is lacking, while structure-based methods provide a rational, mechanism-driven path to novel chemotypes, especially for well-characterized targets. The future lies in the intelligent integration of these approaches, leveraging the power of deep learning and multi-dimensional data to accelerate the discovery of next-generation, personalized cancer therapeutics.
The discovery of novel oncology therapeutics is increasingly reliant on sophisticated de novo drug design strategies that efficiently navigate complex chemical and biological space. Among the most impactful approaches are fragment-based drug discovery (FBDD), scaffold hopping, and structure-based molecular decoration. These methodologies enable researchers to address historically "undruggable" targets and overcome resistance mechanisms that limit conventional therapies [41] [42]. The integration of these strategies with advanced computational techniques, including artificial intelligence and deep learning, has accelerated the identification and optimization of lead compounds against challenging oncological targets such as mutant IDH1, FGFR1, and RAS family proteins [43] [44] [42].
Fragment-based approaches have demonstrated particular value for targeting the growing number of medically relevant 'featureless' or 'flat' protein-protein interaction (PPI) interfaces [45]. The fundamental premise involves identifying low molecular weight fragments (typically 150-300 Da) with weak but efficient binding to target proteins, followed by systematic optimization into potent lead compounds [45]. Concurrently, scaffold hopping and decoration strategies leverage known active compounds to generate novel chemical entities with improved properties, while maintaining or enhancing target engagement [44]. This integrated methodological framework provides a powerful toolkit for addressing the persistent challenges in oncology drug development, including tumor heterogeneity, drug resistance, and therapeutic index optimization [41] [46].
Core Methodologies and Quantitative Comparisons
Fragment-Based Drug Discovery (FBDD)
Fragment-based lead discovery begins with screening low molecular weight compounds (<300 Da) against therapeutic targets using sensitive biophysical techniques. The approach capitalizes on the superior binding efficiency of fragments compared to larger compounds, enabling coverage of greater chemical space with smaller libraries [45]. Success in FBDD depends on robust fragment library design, sensitive detection methods, and effective strategies for fragment-to-lead optimization.
Table 1: Key Platforms for Fragment Screening and Hit Validation
| Technique | Application in FBDD | Key Advantages | Representative Providers |
|---|---|---|---|
| Surface Plasmon Resonance (SPR) | High-throughput fragment screening on target arrays | Parallel detection across multiple targets; reveals selectivity patterns | Genentech, Cytiva (Biacore) [45] |
| Spectral Shift Assays | Fragment binding detection | Label-free measurement of binding events | WuXi AppTec [47] |
| X-ray Crystallography | Structural validation of fragment hits | Atomic-resolution binding mode determination | Astex Pharmaceuticals, WuXi AppTec [47] [45] |
| Nuclear Magnetic Resonance (NMR) | Fragment binding confirmation and characterization | Detects weak interactions; provides structural information | Multiple academic and industry platforms [45] |
| Microscale Thermophoresis (MST) | Fragment affinity measurement | Low sample consumption; rapid analysis | WuXi AppTec [47] |
Recent innovations in FBDD include parallel SPR detection on large target arrays, enabling "ligandability testing" and "general pocket finding" across multiple targets simultaneously [45]. This transformative approach allows researchers to complete fragment screening over large target panels in days rather than years, facilitating rapid identification of selective fragments with favorable enthalpic contributions that possess superior development potential [45].
Scaffold Hopping and Molecular Decoration
Scaffold hopping involves the structural modification of lead compounds through substitution of core ring systems or key structural elements, while molecular decoration focuses on optimizing side chains and functional groups to enhance binding affinity and drug-like properties [44]. These strategies aim to generate novel chemical entities with improved potency, selectivity, and pharmacokinetic profiles while maintaining target engagement.
Advanced computational methods have significantly enhanced scaffold hopping efficiency. The DRAGONFLY computational approach utilizes interactome-based deep learning for ligand- and structure-based generation of drug-like molecules, capitalizing on both graph neural networks and chemical language models [30]. This method enables "zero-shot" construction of compound libraries tailored to possess specific bioactivity, synthesizability, and structural novelty without requiring application-specific reinforcement, transfer, or few-shot learning [30].
Table 2: Performance Comparison of Molecular Design Approaches
| Method | Novelty | Synthesizability (RAScore) | Predicted Bioactivity | Key Applications |
|---|---|---|---|---|
| DRAGONFLY (Interactome-based) | Superior scaffold and structural novelty | High synthesizability scores | Accurate pIC50 prediction (MAE ≤0.6) | PPARγ partial agonists; broad applicability [30] |
| Bidirectional RNN (BRNN) | Enhanced molecular diversity | Favorable synthetic accessibility | Superior docking scores vs. scaffold hopping | mIDH1 inhibitor design [44] |
| Scaffold Hopping | Moderate novelty (focused on electron isomer principle) | Moderate synthesizability | Variable docking performance | Fragment substitution in mIDH1 inhibitors [44] |
| Fine-tuned RNNs | Limited novelty | Lower synthesizability scores | Less accurate bioactivity prediction | Benchmark comparison [30] |
In a direct comparison study for mIDH1 inhibitor design, molecules generated by the BRNN model demonstrated superior performance in molecular diversity, druggability, synthetic accessibility, and docking scores compared to those created through conventional scaffold hopping approaches [44]. From 3,890 compounds generated by BRNN, researchers identified 10 structurally diverse drug candidates, with four (M1, M2, M3, and M6) exhibiting optimal binding properties in molecular dynamics simulations [44].
Experimental Protocols and Application Notes
Protocol 1: Integrated Fragment-to-Lead Optimization
Objective: Identify and optimize fragment hits against oncology targets using biophysical screening and structure-based design.
Materials and Reagents:
- Fragment library (500-1,500 compounds, MW <300, ClogP <3)
- Purified target protein (>95% purity, confirmed activity)
- SPR microarrays (e.g., Genentech parallel screening platform) [45]
- Crystallization screening kits (commercial sparse matrix screens)
- Cell lines expressing target of interest (validation of cellular activity)
Procedure:
- Primary Screening: Perform fragment screening using parallel SPR detection at 100-500 µM fragment concentration in PBS buffer with 1-5% DMSO. Identify hits with significant response units (>10 RU) and steady-state binding [45].
- Hit Validation: Confirm binding using orthogonal methods (MST, NMR, or thermal shift). Determine preliminary IC50 values for validated hits.
- Structural Characterization: Soak promising fragments into protein crystals or co-crystallize fragment-protein complexes. Collect X-ray diffraction data to 2.0 Å resolution or better [47] [45].
- Fragment Growing/Linking: Design synthetic analogues using structure-based design. Prioritize vectors that extend into adjacent subpockets while maintaining favorable physicochemical properties.
- Potency Optimization: Iteratively synthesize and test analogues using biochemical and cellular assays. Monitor ligand efficiency (>0.3 kcal/mol/heavy atom) and lipophilic ligand efficiency (>5) throughout optimization [45].
- Selectivity Profiling: Screen advanced compounds against related target family members (e.g., kinome panel for kinase targets) to assess selectivity.
Application Note: This protocol successfully identified novel allosteric binders for Werner Syndrome helicase (WRN) using fragment-based screening, enabling targeting of mismatch repair deficiency in cancer cells [45]. The approach revealed a previously unknown allosteric binding pocket through careful structural characterization of fragment hits.
Protocol 2: AI-Guided de novo Design for Challenging Targets
Objective: Generate novel chemotypes for difficult-to-drug oncology targets using deep learning approaches.
Materials and Reagents:
- Known active compounds for target of interest (10+ molecules for model training)
- Target structure (experimental or high-quality homology model)
- DRAGONFLY or BRNN computational platform [30] [44]
- Molecular docking software (Schrödinger, AutoDock, etc.)
- ADMET prediction tools (QikProp, ADMET Predictor)
Procedure:
- Data Curation: Compile known active compounds and their bioactivity data from public databases (ChEMBL, PubChem). Curate SMILES strings and standardize activity measurements [44].
- Model Training: Implement DRAGONFLY interactome-based deep learning or BRNN model using known actives as input. For DRAGONFLY, the interactome consists of ~360,000 ligands, 2,989 targets, and approximately 500,000 bioactivities [30].
- Molecular Generation: Generate novel compounds using ligand-based or structure-based constraints. Incorporate desired properties including molecular weight (300-500 Da), lipophilicity (LogP 2-4), and polar surface area (60-120 Ų).
- Virtual Screening: Dock generated compounds into target binding site. Prioritize molecules with superior predicted binding affinity compared to reference compounds.
- ADMET Profiling: Predict pharmacokinetic properties including aqueous solubility, CYP inhibition, and human ether-a-go-go-related gene (hERG) liability.
- Synthetic Prioritization: Evaluate synthetic accessibility using RAScore or similar metrics. Select 10-20 top candidates for chemical synthesis and experimental validation [30].
- Experimental Validation: Synthesize prioritized compounds and evaluate biological activity in biochemical and cellular assays.
Application Note: This approach successfully generated potent PPARγ partial agonists with favorable activity and selectivity profiles through prospective de novo design. Crystal structure determination of the ligand-receptor complex confirmed the anticipated binding mode, validating the computational predictions [30].
Protocol 3: Scaffold Hopping for Overcoming Resistance
Objective: Generate novel chemotypes to overcome resistance mutations in oncology targets.
Materials and Reagents:
- Parent compound with resistance limitations
- Structural data on resistance mechanisms (co-crystal structures preferred)
- Scaffold hopping software (Schrödinger, MOE, or custom implementations)
- Molecular dynamics simulation platform (GROMACS, AMBER)
- Resistance cell lines (engineered or clinically derived)
Procedure:
- Resistance Analysis: Identify key resistance mutations through clinical data or directed evolution studies. Obtain or generate structural models of mutated targets.
- Scaffold Identification: Deconstruct parent compound into core scaffold and functional groups. Identify isosteric replacements with similar shape and electronic properties.
- Molecular Design: Generate novel scaffolds using deep learning approaches (BRNN) or rule-based methods. The BRNN model employs an encoder-decoder architecture with attention mechanism for fragment prediction [44].
- Binding Assessment: Dock proposed scaffolds into wild-type and mutated target structures. Prioritize scaffolds maintaining interactions with conserved binding site residues.
- Dynamics Validation: Perform molecular dynamics simulations (150 ns) to assess binding stability and conformational flexibility of complexes [43].
- ADME Optimization: Decorate selected scaffolds with functional groups to optimize potency while maintaining favorable pharmacokinetic properties.
- Resistance Testing: Evaluate compounds against panel of resistance mutants in cellular assays. Confirm mechanism of action through downstream pathway analysis.
Application Note: In FGFR1 inhibitor development for cancer, researchers applied fragment-based de novo design guided by virtual screening to identify novel pyrido[2,3-d]pyrimidine-based inhibitors. The approach yielded compounds with enhanced binding affinity, superior conformational stability, and favorable pharmacokinetic profiles compared to the reference drug derazantinib [43].
Visualization of Experimental Workflows
Integrated Drug Design Workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for De Novo Drug Design
| Reagent/Platform | Function | Application Notes | Key Providers |
|---|---|---|---|
| Parallel SPR Arrays | High-throughput fragment binding assessment | Enables screening across target families; reveals selectivity patterns | Genentech [45] |
| Biacore Insight Software 6.0 | Automated SPR data analysis | AI-powered analysis reduces processing time by >80% with enhanced reproducibility | Cytiva [45] |
| F-SAPT (Functional-group SAPT) | Quantum chemistry analysis of protein-ligand interactions | Quantifies interaction components; explains structural basis of binding | QC Ware [45] |
| Covalent Fragment Libraries | Targeted screening for cysteine and other nucleophilic residues | Expands druggable space; enables targeting of shallow binding sites | Frontier Medicines [45] |
| Photoaffinity Probe Libraries | Cellular target identification and engagement monitoring | Enables mapping of ligandable sites directly in cells | Belharra Therapeutics, Scripps Research [45] |
| Targeted Protein Degradation Platforms | PROteolysis-TArgeting Chimeras (PROTACs) and molecular glues | Enables targeted degradation of disease-causing proteins | Multiple (Academia/Industry) [41] |
| DRAGONFLY Computational Platform | Interactome-based de novo molecular design | Combines graph neural networks with chemical language models | Academic/Research Implementation [30] |
| BRNN Models | Bidirectional recurrent neural networks for molecular generation | Generates molecules with enhanced diversity and drug-likeness | ETH ModLab Implementation [44] |
The integrated application of scaffold hopping, molecular decoration, and fragment-based design represents a powerful framework for addressing the persistent challenges in oncology drug discovery. These strategies are particularly valuable for targeting historically "undruggable" targets such as KRAS, which have witnessed remarkable breakthroughs after decades of failed attempts [42]. The continued evolution of these approaches, particularly through integration with artificial intelligence and advanced structural biology, promises to further accelerate the development of novel oncology therapeutics.
Future directions in the field include increased incorporation of covalent targeting strategies to expand the druggable proteome, enhanced prediction of resistance mechanisms during early design phases, and more sophisticated integration of cellular permeability considerations into molecular design workflows [45] [42]. Additionally, the growing application of targeted protein degradation approaches, including molecular glues and PROTACs, provides new avenues for addressing targets that have proven recalcitrant to conventional inhibition strategies [41] [42]. As these methodologies continue to mature and integrate, they will undoubtedly yield transformative new therapies for cancer patients, ultimately improving outcomes in this challenging therapeutic area.
The discovery of novel oncology therapeutics is being transformed by artificial intelligence (AI)-enabled de novo drug design. This computational approach generates novel molecular structures from scratch, optimizing them for specific biological targets and drug-like properties from the beginning [48]. Conventional methods rely heavily on known molecular templates, but AI methods, including deep learning and chemical language models, can explore the vast chemical space more efficiently to create innovative intellectual property [48] [49] [30]. This case study examines the application of these principles through the development of two AI-designed inhibitors, REC-617 (targeting CDK7) and REC-4539 (targeting LSD1), tracing their journey from preclinical discovery to clinical evaluation.
Case Study 1: REC-617, an AI-Designed CDK7 Inhibitor
2.1. Compound Overview and Therapeutic Rationale REC-617 is a reversible, non-covalent small molecule inhibitor of Cyclin-Dependent Kinase 7 (CDK7) [50]. CDK7 is a key regulatory protein that plays a dual role in cell cycle progression and transcription. It is a validated oncology target, but achieving selectivity to minimize off-target toxicities has been a challenge. REC-617 was precision-designed using an AI-driven approach to achieve high selectivity and an optimized half-life, aiming to manage potential toxicities while maximizing on-target efficacy in advanced solid tumors [51] [50].
2.2. AI Design and Experimental Protocols The Recursion Operating System (OS), an AI-powered platform, was central to the identification and optimization of REC-617. This platform leverages large-scale, multimodal biological data to infer relationships and generate novel chemical matter.
- AI Design Workflow: The process likely involved a structure- or ligand-based de novo design approach. The AI model would have been trained on a vast drug-target interactome, learning the complex relationships between chemical structures and their biological activities against kinase targets [30]. The model then generates novel molecular structures predicted to inhibit CDK7 potently and selectively. Key properties like synthesizability and favorable ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) profiles are integrated into the generation process [48] [30].
- Key Experimental Protocol: Biochemical Potency and Selectivity Assay
- Objective: To determine the half-maximal inhibitory concentration (IC50) of REC-617 against CDK7 and a panel of related kinases to establish potency and selectivity.
- Methodology: A kinase activity assay is performed using recombinant CDK7/Cyclin H/MAT1 complex. The assay measures the incorporation of radioactive phosphate or a fluorescent signal from a substrate peptide. REC-617 is tested in a dose-response manner. The same assay is run against other CDKs (e.g., CDK1, CDK2, CDK9) and kinases to generate a selectivity profile.
- Data Analysis: IC50 values are calculated by fitting the dose-response data to a non-linear regression model. Selectivity is expressed as the fold-change in IC50 relative to CDK7.
2.3. Key Preclinical and Clinical Data REC-617 is currently in Phase I/II clinical trials (ELUCIDATE trial, NCT05985655) [51] [50]. Initial clinical data announced in December 2024 showed a confirmed partial response in a patient with platinum-resistant ovarian cancer, with a tumor burden reduction of over 30%. Four additional patients exhibited stable disease for up to six months [51]. Combination therapy studies are planned.
Table 1: Key Data for REC-617 (CDK7 Inhibitor)
| Parameter | Preclinical/Clinical Findings | Source/Context |
|---|---|---|
| Target | CDK7 (Cyclin-Dependent Kinase 7) | [51] [50] |
| Designated Name | REC-617 | [50] |
| AI Design Platform | Recursion Operating System (OS) | [51] |
| Key Differentiator | High selectivity & optimized half-life | [50] |
| Development Status | Phase I/II (NCT05985655) | [51] [50] |
| Reported Clinical Activity | Partial response and stable disease in advanced solid tumors | [51] |
| Clinical Trial Combination | Planned with other agents | [51] |
Case Study 2: REC-4539, an AI-Designed LSD1 Inhibitor
3.1. Compound Overview and Therapeutic Rationale REC-4539 is a small molecule inhibitor of Lysine-Specific Demethylase 1 (LSD1/KDM1A), an epigenetic regulator [50]. LSD1 is overexpressed in various cancers and promotes tumor progression by altering gene expression networks. It has been identified as a crucial promoter of oral squamous cell carcinoma (OSCC) progression from preneoplastic lesions [52] [53]. REC-4539 was designed to be the first reversible and central nervous system (CNS)-penetrant LSD1 inhibitor, potentially reducing adverse events (e.g., on-target platelet effects) associated with other LSD1 inhibitors and allowing it to treat CNS-involved cancers [51] [50].
3.2. AI Design and Signaling Pathway The target was likely identified and the compound optimized using phenotypic insights from the Recursion OS. The integration with Exscientia's precision design capabilities further enhanced the compound's properties [51]. The mechanistic pathway regulated by LSD1 inhibition involves key oncogenic signaling networks.
Diagram: LSD1 Inhibition in the STAT3 Signaling Pathway
Diagram Title: LSD1 Inhibition Disrupts Oncogenic Signaling
As shown in the diagram, LSD1 promotes OSCC progression by activating STAT3 signaling [53]. This leads to the phosphorylation of cell cycle mediators like CDK7 and the upregulation of immunosuppressive checkpoints like CTLA4. LSD1 inhibition disrupts this axis, reducing STAT3 activity, CDK7 phosphorylation, and CTLA4 expression, thereby arresting the cell cycle and promoting anti-tumor immunity [53].
3.3. Key Preclinical and Clinical Status An IND application for REC-4539 was cleared by the FDA in early 2025 [51]. However, as of late 2025, its development is on a "strategic pause" due to the competitive landscape [50]. Preclinical data supported its progression to clinical trials. Independent research on other LSD1 inhibitors like Seclidemstat (SP2577) has demonstrated safety and efficacy in inhibiting the STAT3 network in spontaneous OSCC models, validating LSD1 as a target [53].
Table 2: Key Data for REC-4539 (LSD1 Inhibitor)
| Parameter | Preclinical/Clinical Findings | Source/Context |
|---|---|---|
| Target | LSD1 (Lysine-Specific Demethylase 1) | [51] [50] |
| Designated Name | REC-4539 | [50] |
| AI Design Platform | Recursion OS & Exscientia precision design | [51] |
| Key Differentiator | First reversible & CNS-penetrant LSD1 inhibitor | [51] [50] |
| Development Status | Strategic Pause (Preclinical) | [50] |
| Mechanistic Insight | Disrupts LSD1/STAT3/CDK7/CTLA4 axis | [53] |
| Therapeutic Indication | Small-cell lung cancer (SCLC), Acute Myeloid Leukemia (AML) | [50] |
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key reagents and their applications in the experimental workflows relevant to characterizing AI-designed inhibitors like REC-617 and REC-4539.
Table 3: Research Reagent Solutions for Characterizing Novel Inhibitors
| Research Reagent / Tool | Function in Experimental Protocols |
|---|---|
| Recombinant Kinase (e.g., CDK7 complex) | Essential for biochemical assays to determine inhibitor IC50 and selectivity against off-target kinases [30]. |
| Cell Viability Assay (e.g., MTT, CellTiter-Glo) | Used in cell-based experiments to measure the reduction in cell proliferation or viability after compound treatment [53]. |
| Phospho-Specific Antibodies (e.g., pCDK7 Tyr170) | Critical for western blotting or immunofluorescence to detect and quantify changes in target phosphorylation in cells or tissue lysates upon treatment [53]. |
| Flow Cytometry Antibody Panel (e.g., CD45, CD4, CD8, CTLA4) | Enables immunophenotyping of tumor microenvironment in syngeneic mouse models to assess changes in immune cell infiltration and activation after LSD1 inhibition [53]. |
| LSD1 Inhibitor (e.g., SP2509) | A tool compound used in in vitro and in vivo mechanistic studies to validate the pharmacological effects of LSD1 inhibition before testing clinical candidates [53]. |
Discussion & Future Perspectives
The development of REC-617 and REC-4539 exemplifies the industrial application of AI in de novo drug design. Platforms like Recursion OS and methods like the deep interactome learning framework DRAGONFLY enable the "zero-shot" generation of novel bioactive molecules tailored for specific targets, with consideration for synthesizability and optimal physicochemical properties from the outset [51] [30]. A significant trend is the expansion of AI from discovery into clinical development ("ClinTech"), where it is used to optimize trial design, accelerate patient enrollment, and enhance evidence generation [51].
The main challenges remain the synthetic accessibility of generated structures and the successful integration of wet- and dry-lab data cycles [48] [11]. However, as AI models evolve and more biological data becomes available, AI-driven de novo design is poised to become a cornerstone of oncology drug discovery, potentially increasing success rates and delivering more effective, targeted therapies to patients faster.
The discovery and development of biologic therapeutics, particularly monoclonal antibodies, have traditionally been laborious processes constrained by high-throughput screening limitations and extensive optimization cycles. The emergence of generative artificial intelligence (AI) is fundamentally reshaping this landscape, enabling the de novo design of antibodies and other complex biologics from scratch [54]. This paradigm shift is particularly transformative for oncology research, where the ability to target previously "undruggable" pathways and create highly selective therapeutics offers unprecedented opportunities for novel cancer therapeutics [54].
Generative AI moves beyond conventional discovery by employing algorithms that can learn the complex language of protein structures and functions. These models can propose novel antibody sequences optimized for specific targets, with desired pharmacological properties, and with precision that often exceeds what natural immune systems or display technologies can achieve [55]. For oncology researchers, this means accelerated timelines, reduced development costs, and access to previously inaccessible target classes, including complex membrane proteins and intracellular oncogenic drivers [54]. The integration of these AI-driven approaches is poised to become a cornerstone in the next generation of precision cancer immunotherapies.
Key Application Areas in Oncology-Focused Biologics Discovery
De Novo Antibody Design for Novel Epitope Targeting
The most significant advancement enabled by generative AI in biologics discovery is the capacity for true de novo antibody design. Unlike traditional methods that rely on existing antibody repertoires, AI systems can generate entirely novel antibody sequences that bind to specific epitopes on oncology targets with high affinity and selectivity [54]. This capability is particularly valuable for targeting conserved regions on rapidly mutating oncology targets or engaging epitopes that are poorly immunogenic through conventional approaches.
Several companies have demonstrated successful applications of this technology. Nabla Bio has reported designing antibodies against eight challenging targets, including the first binders to engage with cancer-linked membrane-bound targets CLDN4 and CXCR7 [54]. Similarly, Absci, in collaboration with researchers at California Institute of Technology, designed an antibody targeting the conserved "caldera" region of the HIV virus, an area where traditional approaches had previously failed due to the natural immune system's inability to generate antibodies that could bind to this particular region [54]. These successes highlight AI's potential to access biologically relevant but previously inaccessible binding sites.
Multi-specific Antibody Engineering with Reduced Toxicity
Generative AI is revolutionizing the design of complex multi-specific antibodies, particularly for cancer immunotherapy applications. These engineered molecules can simultaneously engage tumor antigens and immune cells, potentially enhancing anti-tumor efficacy. However, their development has been hampered by the challenge of optimizing multiple binding domains while maintaining favorable drug-like properties [54].
LabGenius exemplifies this application with its platform that employs generative AI to design T-cell engager antibodies for solid tumors [54]. The platform uses a closed-loop cycle of AI design and automated experimental testing to co-optimize for all desired properties simultaneously. This approach has produced highly selective T-cell engagers that minimize off-tumor toxicity – a significant challenge with conventional immunotherapies that can cause serious neurological issues, infections, and cytopenias [54]. As one executive noted, designing such complex molecules with the required selectivity "would be impossible without machine learning... these are such rare molecules that you would never have found them unless you deployed these methods" [54].
Targeting the "Undruggable" Oncology Landscape
A substantial portion of clinically validated oncology targets, including G protein-coupled receptors (GPCRs) and ion channels, have remained largely inaccessible to conventional antibody therapeutics due to technical challenges in generating effective binders [54]. These targets represent approximately 60% of drug targets but have proven difficult to drug with biologics [54].
Generative AI approaches are overcoming these limitations by designing antibodies with properties that go beyond what natural immune systems can produce. As Debbie Law, Chief Scientific Officer of Xaira Therapeutics, explains, "We will be able to make molecules that, for example, recognize very small 'real estate' on a protein" [54]. This precision enables targeting of specific protein conformations or mutant variants present exclusively on cancer cells. Galux, for instance, has successfully generated an antibody targeting the epidermal growth factor receptor (EGFR) with single-amino acid specificity, designing the molecule to bind only to mutated EGFR found on cancer cells while sparing healthy cells [54].
Table 1: Key Advances in AI-Driven Biologics Discovery for Oncology
| Application Area | Key Advancement | Representative Companies | Oncology Relevance |
|---|---|---|---|
| De Novo Antibody Design | Generation of novel antibody sequences without known binders | Nabla Bio, Absci, Xaira Therapeutics | Accessing novel epitopes on validated oncology targets |
| Multi-specific Engineering | Simultaneous optimization of multiple binding domains and properties | LabGenius, Nabla Bio | Creating safer T-cell engagers with reduced off-tumor toxicity |
| "Undruggable" Target Engagement | Designing antibodies for GPCRs, ion channels, and other challenging targets | Galux, Nabla Bio | Expanding the druggable genome to include previously inaccessible cancer targets |
| Property Optimization | Enhancing developability, half-life, and manufacturability | Generate:Biomedicines | Improving therapeutic profiles of oncology biologics |
Experimental Protocols for AI-Driven Biologics Discovery
Protocol: Closed-Loop Design-Make-Test Cycle for Antibody Optimization
This protocol outlines the iterative process for optimizing antibody candidates using generative AI and automated laboratory validation, adapted from methodologies successfully implemented by companies including LabGenius and Xaira Therapeutics [54].
Materials and Equipment:
- High-performance computing cluster with AI modeling capabilities
- Automated molecular biology workstation
- High-throughput surface plasmon resonance (SPR) or bio-layer interferometry (BLI) system
- Mammalian expression system for antibody production
- Cell-based functional assay relevant to target biology
Procedure:
- Initial Design Generation: Input target specifications (e.g., binding epitope, affinity range, structural constraints) into the generative AI platform to produce an initial library of 1,000-10,000 candidate sequences.
- In Silico Filtering: Apply machine learning models to predict developability, immunogenicity, and expression levels, reducing the candidate pool to 100-200 sequences.
- Gene Synthesis and Expression: Utilize automated gene synthesis and mammalian expression systems to produce antibody variants.
- High-Throughput Characterization: Measure binding affinity (SPR/BLI), specificity, and thermal stability using automated systems.
- Functional Assessment: Evaluate candidates in cell-based assays measuring target engagement and functional activity.
- Data Integration and Model Retraining: Feed experimental results back into the AI system to refine subsequent design generations.
- Iteration: Repeat steps 1-6 for 3-5 cycles or until candidates meet predefined success criteria.
Typical Timeline: Each cycle requires approximately 6 weeks, with 4 cycles typically needed to identify a development candidate [54].
Protocol: De Novo Binder Generation Against Novel Oncology Targets
This protocol describes the process for generating entirely novel antibody binders against targets with no known binders, based on approaches used by Nabla Bio and Absci for challenging targets including GPCRs and viral epitopes [54].
Materials and Equipment:
- Protein structure prediction software (AlphaFold2 or similar)
- Generative AI platform for antibody design (Diffusion models, EvoDiff, or similar)
- Mammalian display technology or yeast display platform
- High-content imaging system for functional characterization
- Target protein (purified or in cell membrane format)
Procedure:
- Target Characterization: Generate or obtain high-confidence structural models of the target protein, identifying potential binding sites.
- Paratope-Conditioned Generation: Use diffusion-based generative models (e.g., EvoDiff, DiffAb) to create antibody sequences optimized for specific structural features of the target binding site.
- Library Design and Synthesis: Generate a library of 500-1,000 sequences focusing on structural diversity within the predicted binding regions.
- Display Screening: Screen the library using mammalian or yeast display against the target protein under conditions favoring the desired affinity (typically 1-100 nM).
- Hit Characterization: Express and purify top 50-100 hits from display screening for quantitative affinity measurement and specificity profiling.
- Functional Validation: Test binding in relevant cellular contexts; for membrane proteins, use cell-based binding assays with wild-type and target-knockout cells.
- Lead Optimization: Apply the closed-loop design process from Protocol 3.1 to optimize the top 5-10 candidates.
Success Metrics: Current AI platforms demonstrate hit rates of 1-10% for de novo designs, compared to <0.1% with conventional approaches [54].
Table 2: Key Performance Metrics for AI-Driven Biologics Discovery
| Performance Metric | Traditional Methods | AI-Driven Approaches | Improvement Factor |
|---|---|---|---|
| Hit Rate (de novo designs) | <0.1% | 1-10% | 10-100x |
| Timeline to Clinical Candidate | 5.5 years (average) | 2 years (demonstrated) | ~2.75x faster |
| Compounds Synthesized (lead optimization) | Thousands | Hundreds | 10x reduction |
| Success Rate for Challenging Targets (GPCRs, etc.) | Low | Demonstrated for multiple targets | Significant expansion of druggable genome |
Workflow Visualization: AI-Driven Biologics Discovery
The following diagram illustrates the integrated computational and experimental workflow for generative AI-driven biologics discovery:
AI-Driven Biologics Discovery Workflow: This diagram illustrates the iterative cycle of computational design and experimental validation that enables rapid optimization of therapeutic biologics. The process integrates generative AI with high-throughput experimentation, creating a closed-loop system that continuously improves based on experimental feedback [54].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for AI-Driven Biologics Discovery
| Research Tool | Function | Application in Workflow |
|---|---|---|
| Generative AI Platforms (Nabla Bio, Xaira, Absci) | De novo antibody sequence generation with target-conditioned design | Computational design phase: creates initial candidate sequences based on target specifications |
| Structure Prediction Tools (AlphaFold2, RoseTTAFold) | High-accuracy protein structure prediction from sequence | Target characterization: provides structural information for binding site identification and epitope selection |
| Automated Gene Synthesis (Twist Bioscience, etc.) | Rapid, high-fidelity DNA synthesis for candidate sequences | Experimental validation: enables quick transition from digital designs to physical molecules for testing |
| Mammalian Display Systems | Library screening technology with post-translational modifications | Candidate screening: allows functional screening of antibody libraries in mammalian cell environment |
| High-Throughput SPR/BLI | Label-free binding affinity and kinetics measurement | Characterization: provides quantitative binding data for hundreds of candidates |
| Developability Assessment Platforms | In silico and experimental analysis of manufacturability | Candidate selection: predicts expression, stability, and immunogenicity risks |
The application of generative AI to antibodies and other biologics represents a fundamental shift in oncology therapeutic discovery. The protocols and applications outlined in this document demonstrate tangible progress in addressing long-standing challenges in biologic drug development, particularly for oncology targets that have remained recalcitrant to conventional approaches. As these technologies mature, we anticipate further acceleration of discovery timelines, increased success rates in clinical development, and expansion of the druggable genome to include currently untreatable oncogenic drivers.
The integration of AI-driven biologics discovery with other emerging technologies, including single-cell multi-omics and spatial biology, will further enhance our ability to design precision therapeutics matched to specific cancer subtypes and resistance mechanisms. For oncology researchers, embracing these tools and methodologies will be essential for maintaining leadership in the increasingly competitive and technologically advanced landscape of cancer drug development.
Navigating the Oddysey: Overcoming Challenges in AI-Driven Molecule Design
In the field of de novo drug design for novel oncology therapeutics, artificial intelligence (AI) has emerged as a transformative force, accelerating target identification, compound design, and lead optimization [1] [5]. However, the performance and reliability of these AI models are fundamentally constrained by the quality, scale, and diversity of the data on which they are trained [56] [13]. Biased or incomplete datasets can lead to skewed predictions, perpetuating healthcare disparities and producing therapies with unequal efficacy across patient populations [56]. This application note details standardized protocols for oncology research teams to critically assess data quality, identify and mitigate bias, and implement strategies for expanding dataset diversity, thereby ensuring the development of robust and equitable AI-driven cancer therapeutics.
Application Notes: Data Quality and Bias in Oncology AI
The "garbage in, garbage out" paradigm is critically applicable to AI in drug discovery. In oncology, the stakes are elevated due to the high degree of tumor heterogeneity and the urgent need for effective treatments [1].
- Impact of Data Quality: AI models trained on incomplete, noisy, or incorrectly annotated data are prone to generating false leads, incorrectly predicting binding affinities, or overlooking critical safety profiles, which contributes to the high attrition rates in oncology drug development [1] [13].
- Consequences of Bias: A primary challenge is dataset bias, where training data inadequately represent the full spectrum of the patient population [56]. For instance, if genomic or clinical trial datasets underrepresent women, ethnic minorities, or specific cancer subtypes, the resulting AI models may poorly predict drug efficacy or toxicity in these groups [56]. This can lead to therapies that are less effective for underrepresented populations, thereby widening existing health disparities.
The emerging regulatory landscape, including the EU AI Act, classifies AI systems in healthcare as "high-risk," mandating strict requirements for transparency and accountability [56]. This makes the implementation of robust data governance protocols not merely a scientific best practice but a regulatory necessity.
Protocol for Data Quality Verification and Bias Assessment
Objective
To establish a standardized workflow for evaluating the integrity, completeness, and representativeness of datasets used in AI-driven de novo drug design for oncology.
Materials and Reagents
Table 1: Key Research Reagent Solutions for Data Management and Analysis
| Item Name | Function/Description |
|---|---|
| Data Curation Software | Tools for parsing, cleaning, and standardizing raw data from disparate sources (e.g., genomic sequencers, EHRs, scientific literature). |
| Federated Learning Framework | A privacy-preserving distributed AI approach that allows model training across multiple institutions without sharing raw data [1]. |
| Explainable AI (xAI) Tools | Software libraries that provide insights into AI model decision-making, highlighting which data features most influenced a prediction [56]. |
| Algorithmic Auditing Suite | A set of tools and metrics to proactively test trained models for performance disparities across different demographic or clinical subgroups [56]. |
Experimental Workflow
The following diagram outlines the core procedural workflow for data quality and bias assessment.
Step-by-Step Procedure
Step 1: Data Acquisition and Provenance Logging
- Action: Collect multi-modal data from relevant sources, including genomic databases (e.g., TCGA), electronic health records (EHRs), high-throughput screening results, and scientific literature [1] [13].
- Documentation: Create a complete data provenance log detailing the origin, collection methods, and any transformations applied to the raw data.
Step 2: Data Integrity and Completeness Check
- Action: Execute automated checks for missing values, duplicate entries, and inconsistent formatting. Validate biological annotations against controlled vocabularies and ontologies.
- Quantitative Metrics: Calculate and report the metrics in Table 2 for each dataset. Table 2: Key Quantitative Metrics for Data Quality Assessment
| Metric | Target Value | Measurement Method |
|---|---|---|
| Data Completeness | >95% for critical fields | Percentage of non-null values per key data field. |
| Annotation Accuracy | >98% | Random manual audit of a subset of automated annotations. |
| Batch Effect Score | Z-score < 2 | Statistical tests (e.g., PCA, DESeq2) to identify technical variation. |
Step 3: Bias and Representativeness Assessment
- Action: Analyze the demographic and clinical distribution of the dataset.
- Protocol:
- Stratification: Stratify the dataset by key demographic (sex, ethnicity, age) and clinical (cancer stage, subtype, prior treatments) variables.
- Comparison: Compare the distribution of these strata against the known distribution in the broader patient population (e.g., using public health data).
- Gap Analysis: Identify over- and under-represented groups. A significant gender data gap, for example, is common and can lead to models that perform poorly for one sex [56].
Step 4: Explainable AI (xAI) Model Interrogation
- Action: Use xAI techniques on preliminary models to understand decision drivers [56].
- Protocol:
- Train a baseline model on the dataset.
- Apply xAI methods (e.g., SHAP, LIME) to determine the features most influential in the model's predictions.
- Analysis: If the model's decisions are disproportionately driven by features correlated with a demographic factor (like sex) rather than purely biological drivers, this indicates embedded bias that must be mitigated.
Step 5: Data Augmentation and Bias Mitigation
- Action: Address identified quality issues and biases.
- Protocol:
- For missing data, use imputation techniques or, if pervasive, exclude the incomplete entries.
- For underrepresented groups, employ strategies like targeted data augmentation (oversampling) or the generation of synthetic data to create balanced datasets without compromising patient privacy [56].
- Implement algorithmic re-weighting to adjust the model's learning process to compensate for dataset imbalances.
Protocol for Expanding Diverse Datasets
Objective
To provide a methodology for actively expanding datasets to include underrepresented populations and cancer subtypes, enhancing the generalizability of AI models.
Strategic Workflow
The strategy for dataset expansion involves multiple parallel approaches, as visualized below.
Step-by-Step Procedure
Step 1: Establish Multi-Institutional Consortia
- Action: Form partnerships with research hospitals and institutes across different geographic and demographic regions to access a more diverse patient population [1].
- Documentation: Develop standardized data-sharing agreements and common data models to ensure interoperability.
Step 2: Implement Federated Learning Networks
- Action: Adopt a federated learning approach to train AI models across consortium institutions [1].
- Protocol:
- A global model is trained by aggregating model updates (e.g., gradients) from each institution's local data.
- The raw data never leaves the original institution, preserving privacy and complying with regulations while leveraging diverse data sources.
Step 3: Mine Public Data Repositories
- Action: Systematically query public repositories like The Cancer Genome Atlas (TCGA) and ClinicalTrials.gov to identify and fill specific data gaps related to underrepresented cohorts [1].
Step 4: Generate Synthetic Data
- Action: Use generative AI models to create synthetic patient data for underrepresented groups.
- Protocol: Ensure synthetic data preserves the statistical properties and clinical relationships of the original data while fully anonymizing individual patient information. This synthetic data can then be used to rebalance training sets [56].
Navigating the data hurdle is a prerequisite for realizing the full potential of AI in de novo design of oncology therapeutics. By rigorously applying the protocols outlined herein—for quality verification, bias assessment, and strategic dataset expansion—research teams can build more reliable, equitable, and generalizable AI models. This disciplined approach to data management is foundational for developing novel cancer drugs that are effective for all patient populations.
The development of novel oncology therapeutics via de novo drug design represents a complex multi-parameter optimization challenge. Research indicates that a narrow focus on ultra-high in vitro potency often introduces suboptimal physicochemical properties, ultimately undermining a compound's therapeutic potential [57]. Analyses of comprehensive drug databases reveal that successful oral drugs, including those in oncology, seldom possess nanomolar potency, with an average IC₅₀ of 50 nM, and show no strong correlation between high in vitro potency and low therapeutic dose [57]. This paradox highlights the critical need for balanced molecular design strategies that simultaneously address potency, selectivity, synthesizability, and ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties from the earliest stages of discovery.
Quantitative Foundations: Establishing Property Relationships
A data-driven approach is essential for understanding the interplay between conflicting molecular properties. Analysis of large compound datasets enables the establishment of quantitative relationships to guide design decisions.
Table 1: Property Relationships in Successful Oral Drugs (Including Oncology Therapeutics)
| Property Category | Typical Range/Observation | Impact on Drug Profile | Data Source |
|---|---|---|---|
| In Vitro Potency | Average IC₅₀ ~50 nM; seldom sub-nanomolar | Weak correlation with therapeutic dose; reduces risk of physicochemical property bias [57] | ChEMBL Database Analysis |
| Selectivity | Many oral drugs show considerable off-target activity | Requires careful profiling against anti-targets (e.g., hERG) [57] | ChEMBL Database Analysis |
| Molecular Mass | Gradual increase over time in drug development | Higher mass often correlates with decreased ligand efficiency and solubility [57] | Historical Drug Analysis |
| Lipophilicity (LogP) | Critical parameter for multiple ADMET endpoints | Directly impacts permeability, metabolic clearance, and solubility [57] | ADMET-PhysChem Relationship Studies |
| Oncology ADMET Tolerance | Potentially more forgiving than other therapeutic areas [58] | Allows exploration of broader chemical space while maintaining efficacy focus [58] | Comparative Drug Analysis |
Table 2: Machine Learning Model Performance for ADMET Prediction
| Prediction Method | Key Features/Descriptors | Reported Performance | Application Context |
|---|---|---|---|
| Light Gradient Boosting Machine (LGBM) | Molecular descriptors from structure | Accuracy >0.87, Precision >0.72, Recall >0.73, F1-score >0.73 for key ADMET properties [59] | Anti-breast cancer compound screening |
| Kernel Ridge Regression (KRR) | ECFP4, CATS, USRCAT descriptors | Mean Absolute Error (MAE) ≤0.6 for pIC₅₀ prediction across 1,265 targets [30] | Target affinity prediction in de novo design |
| Graph Neural Networks | Molecular graph representations | Superior performance for binding affinity and ADMET endpoints in prospective validation [30] | Structure-based and ligand-based design |
| Random Forest | RDKit descriptors, FCFP4 fingerprints | Robust performance in benchmark studies; less prone to overfitting [60] | General-purpose ADMET QSAR |
Strategic Framework for Multi-Parameter Optimization
Successful de novo design requires a holistic framework that integrates multiple optimization parameters throughout the drug discovery process. The "beauty" of a molecule in drug discovery is context-dependent, reflecting the optimal balance of therapeutically aligned properties for a specific program [61].
Computational Design Workflow
The following diagram illustrates the integrated workflow for balancing conflicting properties in de novo drug design:
Diagram 1: Integrated De Novo Design Workflow. This workflow depicts the systematic approach to balancing conflicting properties from initial design through experimental validation.
Key Strategic Considerations for Oncology
Efficacy-Driven Tolerance: Unlike most therapeutic areas, oncology may be more forgiving of certain ADMET shortcomings when compelling efficacy is demonstrated, particularly for life-threatening conditions with limited treatment options [58].
Administration Route Flexibility: The historical acceptance of intravenous administration in oncology provides formulation flexibility, though oral bioavailability remains highly desirable for chronic dosing and patient convenience [58].
Therapeutic Index Focus: The primary goal is achieving sufficient exposure at the tumor site while managing toxicity profiles, which may differ from the requirements of chronic medications for non-life-threatening conditions.
Experimental Protocols and Methodologies
Protocol: Machine Learning-Driven ADMET Prediction for Compound Prioritization
Purpose: To predict key ADMET properties early in the design process using validated machine learning models, enabling prioritization of virtual compounds for synthesis.
Materials:
- Compound structures in SMILES or SD file format
- Computing infrastructure with Python/R environment
- Curated ADMET datasets for model training/validation
Procedure:
- Data Preparation and Cleaning
- Standardize molecular representations using tools like the standardisation tool by Atkinson et al. [60]
- Remove inorganic salts and organometallic compounds
- Extract organic parent compounds from salt forms
- Adjust tautomers to consistent functional group representation
- Canonicalize SMILES strings and remove duplicates with inconsistent measurements
Feature Generation
- Calculate molecular descriptors (e.g., RDKit descriptors)
- Generate molecular fingerprints (e.g., Morgan fingerprints, ECFP4)
- Produce learned representations (e.g., graph embeddings) where applicable
- Implement structured feature selection combining filter and wrapper methods to identify most relevant descriptors [62]
Model Training and Validation
Prediction and Interpretation
- Apply trained models to virtual compounds
- Generate confidence estimates for predictions
- Interpret results in context of applicable domains
- Integrate predictions with other compound properties for multi-parameter optimization
Validation: Benchmark model performance against known internal or public datasets using accuracy, precision, recall, F1-score for classification tasks, and MAE/R² for regression tasks [59].
Protocol: Generative AI with Embedded Property Optimization
Purpose: To generate novel molecular structures with inherently balanced properties using advanced generative AI models.
Materials:
- Pre-trained chemical language models or graph-based generative models
- Target product profile specifying property constraints
- Computational resources for model inference
Procedure:
- Model Selection and Configuration
- For ligand-based design: Utilize models like DRAGONFLY that leverage drug-target interactome information [30]
- For structure-based design: Employ models capable of processing 3D protein binding site information
- Configure property constraints based on target profile:
- Molecular weight (range: 300-500 Da)
- Lipophilicity (LogP range: 1-3)
- Polar surface area (range: 60-120 Ų)
- Structural novelty requirements
Molecular Generation
- Input target constraints and/or template molecules
- Generate diverse compound libraries (typically 10,000-100,000 molecules)
- Apply filters for synthetic accessibility early in the process
- Implement reinforcement learning with human feedback (RLHF) where possible to incorporate medicinal chemistry expertise [61]
Multi-Parameter Optimization
- Score generated molecules using weighted desirability functions
- Prioritize compounds balancing potency predictions with ADMET profiles
- Assess synthetic accessibility using retrosynthetic analysis tools
- Select top candidates (typically 100-1000) for further evaluation
Experimental Validation
- Synthesize top-ranking designs (typically 10-50 compounds)
- Evaluate in vitro potency against primary oncology target
- Assess selectivity against related targets and anti-targets (e.g., kinases, hERG)
- Profile ADMET properties using in vitro assays
- Iterate design based on experimental results
Validation: In prospective applications, this approach has yielded potent PPARγ partial agonists with desired activity and selectivity profiles, confirmed by crystal structure determination [30].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Computational Tools for De Novo Design and ADMET Prediction
| Tool/Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Generative AI Platforms | DRAGONFLY, Chemical Language Models (CLMs) | De novo molecule generation with tailored properties | Ligand- and structure-based design [30] |
| ADMET Prediction Software | ADMETlab 2.0, admetSAR 2.0 | Web-based prediction of ADMET properties | Early-stage compound prioritization [59] |
| Molecular Descriptor Calculators | RDKit, PaDEL, Dragon | Calculation of molecular descriptors from structure | Feature generation for QSAR models [62] |
| Machine Learning Libraries | Scikit-learn, LightGBM, Chemprop | Implementation of ML algorithms for property prediction | Building custom predictive models [59] [60] |
| Synthetic Accessibility Tools | RAScore, SYNOPSIS | Assessment of compound synthesizability | Prioritization of readily accessible compounds [30] |
| Docking & Structure-Based Design | Molecular docking software, Free Energy Perturbation | Prediction of binding affinity and mode | Structure-based optimization [48] |
Table 4: Experimental Assays for ADMET Profiling in Oncology
| Assay Endpoint | Standardized Methods | Key Parameters Measured | Significance in Oncology |
|---|---|---|---|
| Permeability | Caco-2 assay | Intestinal epithelial cell permeability | Predicts oral bioavailability potential [59] |
| Metabolic Stability | CYP450 inhibition (e.g., CYP3A4) | Metabolic susceptibility | Impacts dosing regimen and drug interactions [59] |
| Cardiotoxicity | hERG binding/inhibition | Potassium channel blockade | Critical safety assessment [59] |
| Genotoxicity | Micronucleus (MN) test | Chromosomal damage potential | Long-term safety evaluation [59] |
| Plasma Protein Binding | Equilibrium dialysis | Fraction unbound in plasma | Affects volume of distribution and efficacy [58] |
| Transporter Interactions | P-glycoprotein assays | Efflux transporter susceptibility | Impacts tumor penetration and resistance [58] |
The future of de novo design for oncology therapeutics lies in sophisticated multi-parameter optimization frameworks that seamlessly integrate generative AI, predictive modeling, and experimental validation. By adopting a holistic approach that balances potency with synthesizability and ADMET properties from the outset, researchers can increase the probability of clinical success while reducing late-stage attrition. The continued advancement of computational methods, particularly deep learning approaches that leverage large-scale interactome data [30], promises to further democratize and accelerate the discovery of innovative oncology therapeutics with optimal property profiles.
The application of Artificial Intelligence (AI) in de novo drug design for oncology represents a paradigm shift in therapeutic development. While AI models, particularly deep learning and generative models, have demonstrated remarkable capabilities in accelerating target identification, molecular design, and response prediction, their complex architecture often renders them as "black boxes" [1]. This opacity presents a significant barrier to clinical adoption and regulatory approval, as understanding the rationale behind model predictions is crucial for validating biological plausibility, ensuring safety, and building trust among researchers and clinicians [4] [63]. Model interpretability refers to the degree to which a human can understand the cause of a decision from a model, while explainability is the ability to explain and provide meaning in understandable terms to a human [64]. In the high-stakes context of oncology drug discovery, where decisions impact patient safety and therapeutic efficacy, moving beyond the black box is not merely an academic exercise but a fundamental requirement for translating AI innovations into clinically actionable insights [2].
The regulatory landscape is increasingly emphasizing the need for transparent AI. The U.S. Food and Drug Administration (FDA) has initiated pilot programs and issued guidance documents that explore the use of AI in clinical trials and medical products, underscoring the need for transparency and contextual validation [63]. Furthermore, the FDA Modernization Act 3.0 positions computational modeling and AI-driven in silico approaches as viable substitutes for traditional animal testing, provided they meet qualification standards that inherently require a degree of explainability [4]. This review details practical strategies and experimental protocols to enhance the interpretability and explainability of AI models, specifically tailored for de novo design of novel oncology therapeutics.
Foundational Concepts and Terminology
Interpretability is the ability to comprehend the model's internal mechanics and the causal pathways that lead to a specific output. It is often associated with simpler, inherently transparent models.
Explainability involves post-hoc analysis to articulate the reasoning behind a model's decision in human-understandable terms, typically for complex models where intrinsic interpretability is low.
Global Interpretability aims to explain the overall model behavior and logic based on the entire dataset, answering the question: "How does the model make decisions overall?"
Local Interpretability focuses on explaining individual predictions, answering the question: "Why did the model make this specific decision for this single instance?"
Table 1: Key Categories of Interpretable and Explainable AI (XAI) Techniques
| Category | Description | Common Methods | Primary Use Case in Drug Discovery |
|---|---|---|---|
| Intrinsic Interpretability | Models that are inherently transparent due to their simple structure. | Linear/Logistic Regression, Decision Trees, Rule-Based Learners [4]. | Preliminary screening, establishing baseline models with clear feature importance. |
| Post-hoc Explainability | Techniques applied after model training to explain complex models. | SHAP (SHapley Additive exPlanations), LIME (Local Interpretable Model-agnostic Explanations), Partial Dependence Plots (PDPs) [63]. | Explaining predictions of deep learning models for target identification and compound efficacy. |
| Model-Specific | Explanations that are tied to the architecture of a specific model type. | Feature Importance in Random Forests, Attention Mechanisms in Transformers [4] [64]. | Interpreting graph neural networks for molecular property prediction; NLP models for literature mining. |
| Model-Agnostic | Methods that can be applied to any machine learning model. | SHAP, LIME, Counterfactual Explanations, Surrogate Models [63]. | Providing unified explanations across diverse AI platforms in a drug discovery pipeline. |
Interpretability Strategies forDe NovoDrug Design
Leveraging Inherently Interpretable Models for Initial Screening
For specific tasks in the early stages of drug discovery, using simpler, intrinsically interpretable models can provide a transparent baseline. Models like Decision Trees and Random Forests can uncover complex, non-linear relationships while still offering insights into feature importance [4]. For instance, a Random Forest model can rank molecular descriptors or genomic features based on their contribution to predicting a compound's binding affinity, providing a clear, actionable list for medicinal chemists to prioritize structural motifs [2].
Experimental Protocol 1: Feature Importance Analysis using Random Forests
Objective: To identify and rank the most influential molecular descriptors predicting inhibition of a specific oncology target (e.g., PD-L1).
- Data Collection: Curate a dataset of small molecules with known experimental IC₅₀ values against the target. Sources can include ChEMBL or BindingDB.
- Feature Calculation: Compute a comprehensive set of molecular descriptors (e.g., molecular weight, logP, topological surface area, number of hydrogen bond donors/acceptors) and fingerprints (e.g., ECFP4) for each compound.
- Model Training: Train a Random Forest regressor to predict pIC₅₀ (-log₁₀IC₅₀) from the molecular features.
- Interpretation Analysis:
- Global Interpretation: Calculate and plot mean decrease in impurity (Gini importance) or permutation importance for all features.
- Local Interpretation: For a specific prediction on a new compound, use TreeSHAP (a variant of SHAP integrated for tree-based models) to generate a force plot illustrating how each feature contributed to shifting the prediction from the baseline average.
- Validation: Correlate the top-ranked molecular features with known structural activity relationships (SAR) from the medicinal chemistry literature. Synthesize and test analogs designed to modulate the top features to experimentally validate their impact.
Post-hoc Explainability for Complex Deep Learning Models
For advanced tasks such as de novo molecular generation using variational autoencoders (VAEs) or generative adversarial networks (GANs), or predicting drug-target interactions (DTIs) with deep neural networks like DeepDTA, post-hoc explanation methods are indispensable [4] [63].
SHAP is a unified approach based on cooperative game theory that assigns each feature an importance value for a particular prediction. It connects local explainability with global model behavior.
Experimental Protocol 2: Explaining a Deep Learning-Based DTI Predictor using SHAP
Objective: To explain the predictions of a convolutional neural network (CNN) like DeepDTA, which predicts binding affinity based on the amino acid sequence of a target protein and the SMILES string of a compound.
- Model Setup: Train a DeepDTA model on a benchmark dataset like KIBA.
- Background Selection: Select a representative sample (typically 100-1000 instances) from the training data to serve as a background distribution.
- Explanation Generation:
- For a prediction of interest, use a model-agnostic explainer like KernelSHAP or a model-specific one like DeepSHAP.
- The explainer calculates the SHAP values for the input features—in this case, segments of the protein sequence and the compound's SMILES string.
- Visualization and Analysis:
- Local: Generate a SHAP force plot for a single high-affinity prediction. This will highlight which specific amino acids in the protein and which substructures in the compound contributed most positively to the predicted strong binding.
- Global: Create a summary plot of SHAP values for many predictions to identify which molecular fragments and protein domains are consistently associated with high-affinity interactions across the dataset.
- Biological Validation: Cross-reference the highlighted protein domains with known functional domains from databases like UniProt. For the key molecular substructures, search for similar pharmacophores in known active compounds.
The workflow below illustrates the integration of these interpretability techniques within a standard AI-driven de novo design pipeline.
Diagram 1: Integrated XAI Workflow for De Novo Drug Design. This workflow illustrates the pathway from data input to validated insight, highlighting key points for applying Explainable AI (XAI) techniques.
Attention Mechanisms and Counterfactual Explanations
Attention Mechanisms in transformer-based models and large language models (LLMs) provide a built-in mechanism for interpretability. When an LLM is used to mine biomedical literature for novel drug targets, the attention weights can indicate which words or phrases in the input text were most influential in the model's decision to classify a protein as a promising target [63] [64].
Experimental Protocol 3: Visualizing Attention in a Target Identification LLM
Objective: To identify key scientific rationale from text for a model's suggestion of a novel cancer target.
- Model & Input: Use a fine-tuned BioBERT or similar model. Input a sentence from a scientific abstract: e.g., "CRISPR knockout of gene X significantly reduced proliferation in triple-negative breast cancer cell lines."
- Extract Attention: For the output prediction "gene X is a high-priority target," extract the attention weights from the relevant transformer layer.
- Visualize: Create a heatmap overlay on the input text, where higher attention scores are represented by more intense colors. This will visually emphasize words like "CRISPR knockout," "proliferation," and "triple-negative breast cancer."
- Analysis: The heatmap allows researchers to quickly verify that the model's decision aligns with biologically plausible evidence, increasing confidence in the target nomination.
Counterfactual Explanations answer the question, "What would need to change in the input for the model to give a different output?" In molecular design, a counterfactual explanation could specify the minimal structural change required to turn a predicted toxic compound into a predicted safe one.
Experimental Protocol 4: Generating Counterfactuals for a Toxicity Predictor
Objective: To find a minimal modification that reduces the predicted toxicity of a novel AI-generated compound.
- Query: Input a compound (A) predicted to be toxic by a deep learning model.
- Generation: Use a counterfactual generation algorithm (e.g., utilizing a generative model or a genetic algorithm) to produce a set of similar compounds (A', A'') that are structurally close to A but are predicted to be non-toxic.
- Comparison: Analyze the structural differences between A and the closest non-toxic counterfactual A'. The difference (e.g., removal of a specific functional group, addition of a methyl group) is the counterfactual explanation.
- Actionable Insight: This precise, minimal change provides a direct hypothesis for a medicinal chemist to test in the next cycle of compound synthesis and experimental validation.
Quantitative Benchmarking of XAI Methods
Evaluating the quality of explanations is critical for adopting XAI methods. The following metrics provide a framework for comparison.
Table 2: Quantitative Metrics for Evaluating XAI Method Performance
| Metric | Description | Interpretation | Ideal Value |
|---|---|---|---|
| Faithfulness | Measures how well the explanation reflects the model's true reasoning process. Computes correlation between feature importance and prediction drop upon removal. | Higher correlation indicates a more faithful explanation. | +1.0 |
| Stability (Robustness) | Measures how consistent the explanation is for similar inputs. If two instances are nearly identical, their explanations should be similar. | Higher stability is desired; low stability indicates unreliable explanations. | > 0.8 |
| Complexity | Measures the conciseness of an explanation (e.g., number of features used). | Simpler explanations with fewer features are generally more interpretable. | Context-dependent |
| AUC on Faithfulness Curve | Evaluates the ability of the explanation to identify features most important to the model's prediction. | A higher AUC indicates a better ability to identify critical features. | 1.0 |
The Scientist's Toolkit: Research Reagent Solutions for XAI
Implementing the protocols above requires a suite of software tools and computational resources.
Table 3: Essential Research Reagents and Software for XAI Implementation
| Tool/Reagent | Type | Primary Function | Application in Protocol |
|---|---|---|---|
| SHAP Library | Software Library (Python) | Unified framework for explaining model outputs using game theory. | Core of Protocol 2 for global and local explanations. |
| LIME | Software Library (Python) | Creates local, interpretable surrogate models to explain individual predictions. | Alternative to SHAP in Protocol 2, especially for text or image data. |
| ALEPlot | Software Library (R/Python) | Calculates Accumulated Local Effects plots, a robust alternative to Partial Dependence Plots. | Visualizing the relationship between a feature and the prediction. |
| Captum | Software Library (Python) | Model interpretability library for PyTorch, including integrated gradients and deep lift. | Explaining deep learning models like DeepDTA in Protocol 2. |
| RDKit | Software Library (Python) | Open-source toolkit for Cheminformatics and Machine Learning. | Calculating molecular descriptors and fingerprints in Protocol 1. |
| ChemBERTa | Pre-trained Model | Transformer model for molecular property prediction. | Model for Protocol 3; its attention mechanisms can be visualized. |
| DeepChem | Software Library (Python) | Deep learning framework for drug discovery and quantum chemistry. | Provides end-to-end pipelines for training DTI models and others. |
| High-Performance Computing (HPC) Cluster | Hardware | Provides the computational power for training large models and running resource-intensive XAI analyses. | Essential for all protocols, particularly with large datasets. |
Integrating robust interpretability and explainability strategies is no longer optional for AI-driven de novo drug design in oncology; it is a core component of a credible and translatable research pipeline. By systematically applying the protocols for intrinsic interpretability, post-hoc analysis with SHAP, attention visualization, and counterfactual generation, researchers can transform opaque AI models into collaborative partners. This transition empowers scientists to generate biologically plausible hypotheses, prioritize experiments with greater confidence, and ultimately accelerate the development of novel, effective, and safe oncology therapeutics. The future of AI in drug discovery hinges not only on its predictive power but also on our ability to understand and trust its decisions.
The application of generative artificial intelligence (AI) in de novo drug design represents a paradigm shift in the search for novel oncology therapeutics. This process involves the computational generation of novel molecular structures from scratch, aiming to explore the vast chemical space—estimated to contain up to 10^60 drug-like molecules—more efficiently than traditional experimental methods [18] [65]. However, the proliferation of generative models, including chemical language models and graph-based approaches, has created an urgent need for standardized evaluation frameworks. Without consistent benchmarks, comparing the performance, strengths, and limitations of different molecular generation strategies becomes problematic, hindering methodological advancement and reliable integration into drug discovery pipelines [66] [67]. In response to this challenge, the MOSES (Molecular Sets) and GuacaMol benchmarks have emerged as cornerstone platforms for the rigorous, reproducible, and comparative assessment of generative models for de novo drug design, particularly in the high-stakes field of oncology research [66] [67].
MOSES and GuacaMol provide complementary yet distinct approaches to evaluating generative models. Their core characteristics, objectives, and underlying data are summarized in Table 1.
Table 1: Core Characteristics of MOSES and GuacaMol Benchmarks
| Feature | MOSES | GuacaMol |
|---|---|---|
| Primary Focus | Distribution-learning tasks [67] | Goal-directed and distribution-learning tasks [66] |
| Core Objective | Approximating the chemical distribution of the training set [67] | Optimizing molecules for specific, predefined property profiles [66] |
| Training Data | Standardized dataset based on ZINC Clean Leads, containing ~1.9 million molecules [67] [68] | Dataset derived from ChEMBL, containing ~1.6 million bioactive molecules [66] [68] |
| Typical Application | Building representative virtual libraries; data augmentation [67] | Hit identification and lead optimization for specific therapeutic targets [66] |
| Key Reference | Polykovskiy et al., 2020 (Front. Pharmacol.) [67] | Brown et al., 2019 [66] |
The choice between these benchmarks depends on the research objective. MOSES is ideal for evaluating a model's ability to produce a chemically realistic and diverse set of drug-like compounds, which is valuable for initial library generation. In contrast, GuacaMol is tailored for assessing a model's capacity to solve specific medicinal chemistry challenges, such as designing molecules with high affinity for a particular oncology target or favorable ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties [66] [18].
Evaluation Metrics and Scoring
A comprehensive understanding of the evaluation metrics is crucial for interpreting benchmark results. These metrics are designed to assess different dimensions of generative model performance, from basic chemical validity to the ability to explore chemical space effectively.
Table 2: Core Evaluation Metrics in MOSES and GuacaMol
| Metric Category | Metric Name | Definition | Interpretation in an Oncology Context |
|---|---|---|---|
| Chemical Plausibility | Validity | Fraction of generated strings that correspond to chemically plausible molecules [66] [67]. | Ensures generated candidates are synthetically feasible. |
| Uniqueness | Fraction of unique molecules among the valid generated structures [66] [67]. | Penalizes low-diversity libraries, which is critical for scaffold hopping in oncology. | |
| Novelty | Fraction of unique, valid molecules not present in the training set [66] [67]. | Measures potential to design novel chemotypes against cancer targets. | |
| Distribution Similarity | Fréchet ChemNet Distance (FCD) | Measures similarity between generated and test set distributions using activations from the ChemNet network [66]. | Low FCD indicates generated molecules are drug-like and similar to known bioactive compounds. |
| KL Divergence | Measures the divergence in distributions of key physicochemical properties (e.g., LogP, TPSA) [66]. | Ensures generated oncology candidates have properties aligned with known drugs. | |
| Goal-Directed Performance | Similarity & Rediscovery | Ability to generate a specific target molecule (e.g., a known inhibitor) or one highly similar to it [66]. | Tests the model's ability to rediscover a known drug or propose close analogs. |
| Multi-Property Optimization (MPO) | Balances and optimizes multiple, often competing, property objectives simultaneously [66]. | Mimics the real-world challenge of optimizing potency, selectivity, and ADMET. |
These metrics collectively provide a multi-faceted view of model performance. For instance, a model ideal for oncology drug discovery must not only score highly on goal-directed tasks (e.g., generating molecules with high predicted affinity for EGFR) but also maintain strong performance on distribution-learning metrics to ensure the chemical realism and diversity of its proposals [66] [68].
Detailed Experimental Protocols
Protocol for Distribution-Learning Benchmark (MOSES-Centric)
This protocol evaluates how well a model learns and reproduces the chemical space of a reference dataset.
- Data Preparation: Utilize the standardized training set provided by the MOSES platform, which is pre-filtered for drug-like molecules.
- Model Training: Train the generative model (e.g., LSTM, GPT, S4, VAE) on the canonical SMILES strings from the training set.
- Molecule Generation: Use the trained model to generate a large set of molecules (typically 30,000 as used in MOSES assessments).
- Post-processing and Deduplication: Canonicalize the generated SMILES and remove duplicates.
- Metric Calculation:
- Validity: Calculate the fraction of generated strings that RDKit can successfully parse into valid molecules.
- Uniqueness: Determine the fraction of unique molecules among the valid ones.
- Novelty: Calculate the fraction of unique, valid molecules that are not found in the training set.
- FCD and KL Divergence: Compare the distributions of the generated set and a held-out test set using the respective metrics.
Protocol for Goal-Directed Benchmark (GuacaMol-Centric)
This protocol tests a model's ability to optimize molecules against a specific objective, highly relevant for targeting oncology pathways.
- Task Selection: Choose a specific goal-directed task from the GuacaMol suite (e.g., "Perindopril MPO," "Amlodipine Rediscovery").
- Objective Function Definition: The benchmark provides a pre-defined scoring function that quantifies how well a molecule meets the task's objective (e.g., similarity to a target + desirable properties).
- Model Optimization: The generative model is optimized, often using reinforcement learning or fine-tuning, to maximize the objective function score.
- Candidate Generation: The optimized model generates a set of candidate molecules.
- Performance Scoring: The benchmark evaluates the set of generated molecules and reports a final score for the task (e.g., between 0 and 1), based on the success in achieving the objective.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of these benchmarks requires a suite of software tools and chemical resources.
Table 3: Essential Research Reagents and Tools for Benchmarking
| Tool/Reagent | Type | Primary Function in Benchmarking | Access Information |
|---|---|---|---|
| MOSES Platform | Software Platform | Provides standardized data, baseline models, and the full suite of evaluation metrics for distribution-learning tasks. [67] | https://github.com/molecularsets/moses |
| GuacaMol Benchmark | Software Platform | Offers a suite of goal-directed and distribution-learning tasks for rigorous model comparison. [66] | https://github.com/BenevolentAI/guacamol |
| MolScore | Unified Framework | Unifies scoring and benchmarking, re-implementing GuacaMol and MOSES tasks while allowing for easy creation of custom, drug-design-relevant objectives. [69] | https://github.com/MorganCThomas/MolScore |
| RDKit | Cheminformatics Library | Handles fundamental cheminformatics operations: SMILES parsing, canonicalization, and descriptor calculation (e.g., LogP, TPSA). Essential for metric computation. [69] | Open-source, available via PyPI. |
| ChEMBL Database | Chemical Database | A large-scale, open-source database of bioactive molecules. Serves as the primary data source for GuacaMol's training set, providing a real-world context for bioactivity. [66] [68] | https://www.ebi.ac.uk/chembl/ |
| ZINC Database | Chemical Database | A curated collection of commercially available compounds. The MOSES benchmark uses a subset of ZINC to ensure drug-like starting points. [67] | http://zinc.docking.org/ |
Application in Oncology Drug Discovery
The practical value of these benchmarks is demonstrated by their application in the de novo design of oncology therapeutics. For example, a recent study applied the Structured State Space Sequence (S4) model, benchmarked on both MOSES and GuacaMol, to the prospective design of kinase inhibitors [68]. The S4 model, which showed superior performance on the benchmarks by effectively capturing global molecular properties, was then used to design novel molecules targeting MAPK1—a key protein in cancer signaling pathways. This led to the in silico design of molecules, eight out of ten of which were predicted as highly active by molecular dynamics simulations, showcasing a direct pipeline from rigorous benchmark validation to prospective drug design [68].
Furthermore, the GuacaMol benchmark's goal-directed tasks, such as multi-property optimization (MPO), directly mirror the challenges in oncology lead optimization. A model can be tasked with generating molecules that are simultaneously similar to a known active compound but with improved solubility and reduced predicted toxicity [66] [18]. This ability to balance multiple, conflicting objectives is critical for developing viable clinical candidates, making these benchmarks an indispensable component of the modern computational oncologist's toolkit.
The discovery of novel oncology therapeutics is being transformed by the integration of artificial intelligence (AI), robotic synthesis, and high-throughput screening (HTS) into a unified, iterative workflow. This convergence creates a closed-loop system that accelerates the design-make-test-analyze (DMTA) cycle for de novo drug design [18]. AI-driven generative models design novel molecular structures with desired anti-tumor properties, which are then synthesized using automated robotic platforms and subsequently tested in high-throughput biological assays [70]. The resulting data feedback into AI models to refine subsequent design cycles, creating a continuous optimization process that dramatically reduces the time and cost required to identify promising drug candidates [5].
In oncology research, where tumor heterogeneity and resistance mechanisms present significant challenges, this integrated approach enables rapid exploration of chemical space to discover compounds targeting specific cancer pathways, immune checkpoints, and tumor microenvironment modulators [4]. The ability to quickly generate, synthesize, and validate novel chemical entities is particularly valuable for addressing undrugged oncology targets and overcoming existing therapeutic resistance [2]. This application note details the protocols and methodologies for implementing such an integrated platform specifically for oncology drug discovery.
The seamless integration of computational design, automated synthesis, and high-throughput testing forms a continuous cycle for accelerating oncology drug discovery. This workflow transforms AI-generated molecular structures into physically validated drug candidates through an optimized, iterative process.
The following diagram illustrates the core closed-loop workflow, highlighting the continuous feedback mechanism that connects computational design with experimental validation:
Figure 1. Closed-Loop Drug Discovery Workflow. This continuous cycle integrates AI design with experimental validation, creating an iterative optimization process for oncology drug discovery.
AI-Driven De Novo Molecular Design
Molecular Generation Platforms
AI-driven de novo molecular design employs advanced computational architectures to generate novel compound structures with optimized properties for oncology therapeutics. These platforms leverage deep learning models trained on extensive chemical and biological datasets to design molecules targeting specific cancer mechanisms [48] [18].
Table 1. AI Platforms for De Novo Drug Design in Oncology
| Platform/Algorithm | AI Architecture | Oncology Application | Key Features |
|---|---|---|---|
| DRAGONFLY [30] | Graph Transformer + LSTM | PPARγ partial agonists | Interactome-based learning; zero-shot design |
| Generative Adversarial Networks (GANs) [48] [4] | Generator + Discriminator networks | Immunomodulatory small molecules | High chemical diversity; property optimization |
| Variational Autoencoders (VAEs) [48] [4] | Encoder-decoder architecture | Kinase inhibitors | Continuous latent space exploration |
| Reinforcement Learning (RL) [48] [4] | Agent-environment interaction | Anti-tumor agents | Multi-parameter optimization (potency, ADMET) |
| Chemical Language Models (CLMs) [30] | Sequence-based models (SMILES) | Targeted protein degraders | Transfer learning from large compound libraries |
Protocol: AI-Driven Molecular Generation for Oncology Targets
Objective: Generate novel small molecule inhibitors for a specific oncology target (e.g., kinase, immune checkpoint) with optimized binding affinity, selectivity, and drug-like properties.
Materials and Reagents:
- Target protein structure (PDB format) or known active ligands
- Chemical databases (ChEMBL, ZINC, etc.)
- Computational resources (GPU clusters)
- AI software platforms (DRAGONFLY, REINVENT, etc.)
Procedure:
- Target Preparation (Day 1)
- Obtain 3D structure of target protein from Protein Data Bank or generate via homology modeling
- Define binding site coordinates through structural analysis or known ligand interactions
- For ligand-based design, curate known active compounds (>50 molecules) with binding affinity data
Model Training and Configuration (Days 1-2)
- Pre-process training data from chemical databases (>100,000 compounds)
- Configure AI model parameters based on design objectives:
- Molecular weight: 300-500 Da
- LogP: 2-4
- Hydrogen bond donors/acceptors: Based on Lipinski's Rule of Five
- Target-specific properties (e.g., kinase hinge-binding motifs)
- Implement multi-parameter optimization using reinforcement learning or transfer learning
Molecular Generation (Day 3)
- Generate initial library of 10,000-100,000 virtual compounds
- Filter based on drug-likeness, synthetic accessibility, and structural novelty
- Apply docking simulations or QSAR predictions to prioritize top 100-500 candidates
- Cluster compounds by structural scaffolds to ensure diversity
Output and Prioritization (Day 4)
- Select top 20-50 candidates for synthesis based on comprehensive scoring
- Export structures in standard formats (SMILES, SDF) for robotic synthesis
Robotic Synthesis and Automated Platforms
High-Throughput Synthesis Technologies
Automated robotic platforms enable rapid translation of AI-designed molecules into physical compounds for biological testing. These systems significantly accelerate synthesis while reducing human error and variability [70].
Table 2. Automated Synthesis Platforms for Oncology Compound Production
| Platform Component | Function | Throughput | Key Features |
|---|---|---|---|
| iChemFoundry [70] | Automated compound synthesis | 100-1000 reactions/day | Integrated reaction optimization & purification |
| Automated Solid-Phase Synthesis | Peptide/nucleotide synthesis | 50-200 compounds/batch | Sequential building block addition |
| Flow Chemistry Systems | Continuous compound production | 10-100x faster than batch | Improved heat/mass transfer; safer operations |
| Automated Purification Systems | HPLC, flash chromatography | 50-200 samples/day | Integrated with synthesis platforms |
| Reaction Planning Software | Route selection and optimization | N/A | Retrosynthetic analysis; condition recommendation |
Protocol: Automated Synthesis of AI-Designed Compounds
Objective: Synthesize and characterize AI-designed small molecules using automated robotic platforms.
Materials and Reagents:
- Building block libraries (diverse chemical scaffolds)
- Solvents (DMF, DMSO, dichloromethane, etc.)
- Catalysts (palladium, copper, etc.)
- Protecting group reagents
- Purification materials (HPLC columns, silica gel)
Procedure:
- Reaction Planning and Preparation (Day 1)
- Analyze AI-generated structures for synthetic feasibility using retrosynthetic analysis software
- Select appropriate building blocks from available chemical libraries
- Program robotic synthesis platform with reaction sequences and conditions
- Prepare reagent solutions at specified concentrations in compatible solvents
Automated Synthesis Execution (Days 1-2)
- Load building blocks, solvents, and catalysts into designated platform reservoirs
- Execute programmed synthesis protocol:
- Reaction vessel heating/cooling to specified temperatures
- Precise reagent addition with liquid handling systems
- Inert atmosphere maintenance for air-sensitive reactions
- Real-time reaction monitoring via inline spectroscopy
- Perform parallel synthesis of multiple analogs (10-50 compounds per run)
Workup and Purification (Days 2-3)
- Transfer reaction mixtures to automated workup stations
- Execute standard workup procedures (extraction, washing, concentration)
- Perform automated purification via flash chromatography or HPLC
- Analyze compound purity (>90% by LC-MS) before proceeding to screening
Compound Characterization (Day 3)
- Confirm structural identity via NMR and mass spectrometry
- Determine purity through analytical HPLC/UV
- Prepare standardized stock solutions (10 mM in DMSO) for HTS
- Log compounds into electronic laboratory notebook with metadata
High-Throughput Screening in Oncology
Screening Technologies for Cancer Targets
High-throughput screening provides the critical experimental validation component in the integrated discovery loop, assessing the biological activity of synthesized compounds against relevant oncology targets [1] [2].
Table 3. HTS Assays for Oncology Drug Discovery
| Assay Type | Target Class | Throughput | Detection Method |
|---|---|---|---|
| Cell Viability Assays | Broad anti-tumor activity | 10,000-100,000 compounds/week | ATP content, resazurin reduction |
| - Target-Based Biochemical Assays: Kinase activity, protein-protein interactions | 50,000-200,000 compounds/week | Fluorescence polarization, TR-FRET | |
| - Phenotypic Screening: Tumor cell migration, invasion, stemness | 5,000-20,000 compounds/week | High-content imaging, label-free detection | |
| - Immuno-oncology Assays: T-cell activation, checkpoint inhibition | 10,000-50,000 compounds/week | Reporter gene assays, cytokine secretion |
Protocol: Oncology-Focused HTS Campaign
Objective: Evaluate synthesized compounds in relevant oncology assays to identify hits for further optimization.
Materials and Reagents:
- Cancer cell lines (appropriate to target biology)
- Assay kits (viability, apoptosis, pathway activation)
- Antibodies for specific target detection
- Cell culture media and supplements
- Microplates (96, 384, or 1536-well format)
Procedure:
- Assay Development and Validation (Days 1-3)
- Select appropriate cancer models (cell lines, patient-derived organoids)
- Optimize assay conditions (cell density, reagent concentrations, incubation times)
- Establish robustness parameters (Z' factor >0.5, CV <10%)
- Validate with reference compounds (positive and negative controls)
Screening Execution (Days 4-7)
- Dispense cells/reagents into microplates using automated liquid handlers
- Transfer compound libraries using pin tools or acoustic dispensers
- Incubate under appropriate conditions (37°C, 5% CO₂)
- Measure endpoint using plate readers (fluorescence, luminescence, absorbance)
- Include quality control plates throughout screening run
Data Analysis and Hit Identification (Days 7-10)
- Process raw data using specialized software (e.g., CBIS, Genedata Screener)
- Normalize signals to positive and negative controls
- Apply statistical methods to identify significant activity (≥3σ from mean)
- Apply multi-parameter scoring including potency, efficacy, and data quality
- Select confirmed hits for dose-response validation
Hit Validation and Characterization (Days 10-14)
- Confirm activity in dose-response format (8-12 point curves)
- Assess selectivity in counter-screens against related targets
- Evaluate preliminary ADMET properties (solubility, metabolic stability)
- Select 5-20 lead compounds for further optimization cycles
The Scientist's Toolkit: Research Reagent Solutions
Table 4. Essential Research Reagents for Integrated Oncology Drug Discovery
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Building Block Libraries | Chemical starting materials for robotic synthesis | Diverse scaffold generation for structure-activity relationship studies |
| Cell Line Panels | Disease models for phenotypic screening | Patient-derived cancer cells for target identification and validation |
| Assay Kits | Target engagement and pathway modulation detection | Kinase activity, protein-protein interaction, and cell viability assays |
| Protein Targets | Structural and biochemical studies | Recombinant kinases, nuclear receptors, immune checkpoints for binding assays |
| Specialized Chemical Reagents | Enabling specific synthetic transformations | Cross-coupling catalysts, asymmetric synthesis reagents, protecting groups |
Pathway Visualization
The following diagram illustrates key oncology signaling pathways targeted by AI-designed small molecules, highlighting intervention points for novel therapeutics:
Figure 2. Oncology Signaling Pathways. Key therapeutic targets for AI-designed small molecules in cancer, including growth factor signaling and immune checkpoint pathways.
The integration of AI-driven de novo design with robotic synthesis and high-throughput screening creates a powerful, closed-loop system that significantly accelerates oncology drug discovery. This approach compresses the traditional drug discovery timeline from years to months while increasing the quality of resulting clinical candidates [5]. As these technologies continue to mature, they promise to deliver more effective and targeted therapies for cancer patients by enabling rapid exploration of chemical space and efficient optimization of drug candidates. The protocols outlined in this application note provide a framework for implementing this integrated approach in oncology research settings.
The application of de novo drug design for novel oncology therapeutics represents a paradigm shift in drug discovery, offering the potential to generate innovative chemical entities targeting specific cancer pathways from scratch [18]. This computational approach utilizes artificial intelligence (AI) and deep learning to design molecules with predefined optimal characteristics, including biological activity, target selectivity, and favorable ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) profiles [48]. However, the practical implementation of these computationally generated designs faces two significant interconnected limitations: ensuring the synthetic feasibility of proposed molecules and their effective integration into the established Design-Make-Test-Analyze (DMTA) cycle [18]. These challenges are particularly acute in oncology, where the urgency for novel therapeutic agents is high, and the biological targets are often complex [18]. This document outlines the core limitations and provides detailed protocols to overcome them, specifically framed for researchers, scientists, and drug development professionals working in oncology drug discovery.
Core Challenges and Quantitative Assessment
A primary challenge in de novo drug design is the frequent proposal of molecules that are difficult or impossible to synthesize with current chemical methods [48]. Furthermore, integrating these computational tools into the iterative DMTA cycle requires careful planning to ensure that the generated data is meaningful and accelerates development rather than creating bottlenecks [18]. The quantitative assessment of these challenges is crucial for project planning and resource allocation.
Table 1: Key Challenges in Integrating De Novo Design into Oncology Drug Discovery
| Challenge Domain | Specific Limitation | Impact on Oncology Drug Discovery | Common Quantitative Metrics |
|---|---|---|---|
| Synthetic Feasibility | High complexity of AI-generated structures [48] | Delays in obtaining physical samples for biological testing; requires specialized synthetic expertise. | Retrosynthetic Accessibility Score (RAScore) [30], number of synthetic steps, complexity scores. |
| Poor alignment with available building blocks [18] | Increases cost and time of chemical synthesis. | Number of rare/unavailable fragments, similarity to known synthetic pathways. | |
| DMTA Cycle Integration | Computational validation not predictive of real-world performance [18] | Failed cycles due to poor activity/ADMET in experimental models (cell lines, animal models). | Discrepancy between predicted vs. measured pIC50/EC50; false positive/negative rates [30]. |
| Lack of automation between digital design and chemical synthesis [18] | Slow iteration between idea generation and experimental validation. | Time from digital design to synthesized compound (weeks); degree of manual intervention required. | |
| Data & Model Limitations | Limited scope of training data (e.g., for novel oncology targets) [18] | Poor generation performance for entirely novel target classes (e.g., undrugged transcription factors). | Mean Absolute Error (MAE) of bioactivity predictions on novel targets [30]. |
| Exploration of a narrow chemical space despite vast theoretical possibilities [18] | Missed opportunities for novel chemotypes with unique resistance profiles. | Molecular novelty scores, scaffold diversity metrics [30]. |
Experimental Protocols for Validation and Integration
To overcome these challenges, a structured experimental approach is required. The following protocols detail methodologies for validating the synthetic feasibility of de novo generated compounds and for their rigorous experimental testing within a DMTA framework.
Protocol 1: Assessing Synthetic Feasibility and Planning Synthesis
This protocol aims to triage computationally generated molecules based on synthetic tractability and to devise a practical synthesis route.
I. Materials and Reagents
- Software for Retrosynthetic Analysis: (e.g., CAS SciFinder, Reaxys) for literature-based route planning.
- Synthetic Feasibility Scoring Algorithm: (e.g., RAScore) [30] for rapid computational assessment.
- Compound Database: (e.g., ChEMBL, ZINC) for identifying analogous synthetic pathways.
- Standard Laboratory Equipment & Reagents: For organic synthesis, including fume hoods, glassware, and a library of common chemical building blocks.
II. Methodology
- Computational Triage: a. Calculate the Retrosynthetic Accessibility Score (RAScore) for all de novo generated molecules. A higher RAScore indicates greater synthetic feasibility [30]. b. Filter the virtual library, prioritizing molecules with a RAScore above a predefined threshold (e.g., >0.7, based on internal validation). c. Apply additional functional group filters to remove molecules with known instability, toxicity, or reactivity issues.
Retrosynthetic Analysis: a. For the top-ranked candidates, perform a computer-assisted retrosynthetic analysis using dedicated software. b. Identify key disconnections and potential synthons. Prioritize routes that utilize commercially available or readily synthesizable building blocks. c. Evaluate the proposed routes based on the number of steps, projected yields, and the use of hazardous or costly reagents.
Route Selection and Analogue Identification: a. Select the most practical synthetic route for initial efforts. b. Identify simpler, closely related analogues from the generated library that can be synthesized more rapidly to provide early structure-activity relationship (SAR) data.
III. Analysis and Output The output is a prioritized list of compounds for synthesis, each accompanied by a proposed synthetic route and an assessment of confidence level (high, medium, low) based on the above criteria.
Protocol 2: Experimental Validation within the DMTA Cycle
This protocol describes the experimental testing of synthesized de novo compounds to close the DMTA loop, specifically for an oncology target.
I. Materials and Reagents
- Test Compounds: Synthesized from Protocol 1, dissolved in DMSO or suitable solvent.
- Cell Lines: Relevant cancer cell lines (e.g., MCF-7 for breast cancer, A549 for lung cancer) and a non-malignant control cell line.
- Assay Kits: Cell viability (e.g., MTT, CellTiter-Glo), apoptosis (e.g., Caspase-Glo), and other pathway-specific assays.
- Protein Purification System: For target protein expression and purification if biophysical assays are required.
- Microscopy and Flow Cytometry: For phenotypic analysis.
II. Methodology
- Primary In Vitro Screening: a. Treat a panel of cancer cell lines with a range of compound concentrations (typically 0.1 nM - 100 µM) for 72 hours. b. Assess cell viability using a validated assay (e.g., CellTiter-Glo). Calculate IC₅₀ values. c. Counter-screen against non-malignant cells to assess selective toxicity.
Target Engagement and Mechanism of Action (MoA): a. Biochemical Assay: If applicable, perform a direct binding or enzymatic inhibition assay with the purified target protein (e.g., kinase assay for an oncology kinase target) to determine biochemical IC₅₀. b. Cellular Pathway Analysis: Use Western blotting or immunofluorescence to monitor modulation of the intended signaling pathway (e.g., phosphorylation status of downstream effectors). c. Phenotypic Profiling: Utilize high-content imaging to capture complex morphological changes indicative of a specific MoA (e.g., mitotic arrest).
Early ADMET Profiling: a. Metabolic Stability: Incubate compounds with human or mouse liver microsomes and measure parent compound depletion over time. b. CYP Inhibition: Screen for inhibition of major cytochrome P450 enzymes. c. Plasma Protein Binding: Determine the fraction of compound bound to plasma proteins.
III. Analysis and Feedback to Design The generated experimental data (IC₅₀, selectivity indices, ADMET parameters) are analyzed and used as the "Analyze" component of the DMTA cycle. This data is then fed back to inform the next iteration of the computational de novo design, creating a learning loop for the AI models [18]. For instance, compounds with poor metabolic stability can be used as negative examples to fine-tune the generative model.
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 2: Key Research Reagents for Experimental Validation in Oncology
| Reagent / Material | Function / Explanation |
|---|---|
| ChEMBL Database | A manually curated database of bioactive molecules with drug-like properties. Used for training AI models and understanding SAR of related targets [48]. |
| Relevant Cancer Cell Line Panel | A collection of cell lines representing different cancer types and genetic backgrounds. Essential for assessing the potency and selectivity of novel compounds [18]. |
| Cell Viability Assay Kits (e.g., MTT) | Colorimetric or luminescent assays to quantitatively measure the number of viable cells after compound treatment, determining cytotoxic effects [18]. |
| Human Liver Microsomes | Subcellular fractions used in in vitro assays to predict metabolic stability and potential drug-drug interactions of new chemical entities [18]. |
| Target Protein (Purified) | The purified recombinant oncology target protein (e.g., kinase, nuclear receptor) is required for biochemical assays to confirm direct target engagement and mechanism of action [30]. |
Visualizing the Integrated Workflow
The following diagram illustrates the fully integrated DMTA cycle, enhanced with specific steps to address synthetic feasibility and experimental validation for de novo generated compounds.
Diagram 1: Integrated DMTA cycle for de novo design.
The DRAGONFLY framework exemplifies a modern AI approach that directly incorporates key design constraints to generate more viable compounds from the outset, as shown in the diagram below.
Diagram 2: DRAGONFLY interactome learning workflow.
From In Silico to In Vivo: Validating and Benchmarking AI-Designed Oncology Candidates
The integration of artificial intelligence (AI) into oncology drug discovery represents a paradigm shift, moving from traditional, labor-intensive processes to computationally driven, precision-focused approaches. De novo drug design, a methodology for creating novel chemical entities from scratch with no a priori relationships, is being revolutionized by AI technologies such as deep learning and reinforcement learning [48] [18]. This application note provides a detailed 2025 landscape of AI-designed oncology drugs currently in clinical trials, framed within the context of a broader thesis on de novo drug design methods for novel oncology therapeutics research. It offers a comprehensive analysis of the clinical pipeline, summarizes quantitative data for comparison, details essential experimental protocols for validation, and visualizes key signaling pathways and workflows to serve the needs of researchers, scientists, and drug development professionals.
The AI-Driven Drug Discovery Paradigm in Oncology
Traditional oncology drug discovery is a time-intensive and resource-heavy process, often requiring over a decade and billions of dollars to bring a single drug to market, with an estimated 90% of oncology drugs failing during clinical development [1]. AI is transforming this pipeline by leveraging machine learning (ML), deep learning (DL), and natural language processing (NLP) to integrate massive, multimodal datasets—from genomic profiles to clinical outcomes—generating predictive models that accelerate the identification of druggable targets, optimize lead compounds, and personalize therapeutic approaches [1] [2].
A paramount application of AI is in de novo drug design, which aims to generate novel molecular structures from atomic building blocks to fit a set of constraints, exploring a broader chemical space and designing compounds that constitute novel intellectual property [48] [18]. Deep generative models, such as variational autoencoders (VAEs) and generative adversarial networks (GANs), can create novel chemical structures with desired pharmacological properties, while reinforcement learning (RL) further optimizes these structures to balance potency, selectivity, solubility, and toxicity [1] [4]. This approach has demonstrated remarkable efficiency, compressing discovery timelines that traditionally took 3–6 years down to under 18 months in reported cases [1] [5].
Table: Core AI Technologies in De Novo Drug Design for Oncology
| AI Technology | Sub-category | Key Function in De Novo Design | Application Example in Oncology |
|---|---|---|---|
| Deep Learning | Generative Adversarial Networks (GANs) | Generate novel molecular structures with drug-like properties | Designing small-molecule inhibitors for immune checkpoints like PD-1/PD-L1 [4] |
| Graph Neural Networks (GNNs) | Model molecular graphs and protein-ligand interactions | Predicting binding affinity for novel kinase inhibitors [30] | |
| Chemical Language Models (CLMs) | Represent and generate molecules as text sequences (e.g., SMILES) | Creating novel compound libraries tailored to specific cancer targets [30] | |
| Reinforcement Learning (RL) | Deep Q-Learning / Actor-Critic | Iteratively propose and optimize molecular structures based on reward signals | Balancing potency, selectivity, and ADMET properties during lead optimization [48] [4] |
| Multimodal AI | Graph Transformer Neural Networks (GTNNs) | Integrate diverse data types (e.g., genomics, imaging, clinical data) | Identifying patient subgroups for targeted therapy and predicting drug response [71] |
2025 Clinical Pipeline of AI-Designed Oncology Drugs
The clinical pipeline for AI-designed oncology drugs has experienced exponential growth, with over 75 AI-derived molecules reaching clinical stages by the end of 2024 [5]. These candidates, primarily in Phase I and II trials, originate from both specialized AI biotechs and large pharmaceutical partnerships. The following section and table provide a detailed landscape of key assets, their AI generation methodologies, and current development status as of 2025.
Table: Selected AI-Designed Oncology Drugs in Clinical Trials (2025 Landscape)
| Drug Candidate | AI Developer / Pharma Partner | AI Generation Methodology | Target / Indication | Key Mechanism of Action | Trial Phase (as of 2025) |
|---|---|---|---|---|---|
| GTAEXS-617 | Exscientia (post-merger with Recursion) [5] | Generative AI & Centaur Chemist platform for iterative design [5] | CDK7 inhibitor / Solid Tumors | Inhibits Cyclin-Dependent Kinase 7, disrupting cell cycle progression [5] | Phase I/II [5] |
| EXS-74539 | Exscientia [5] | Generative AI-driven design | LSD1 inhibitor / Oncology | Inhibits Lysine-Specific Demethylase 1, potentially affecting gene expression in cancer cells [5] | Phase I (IND approval in early 2024) [5] |
| EXS-73565 | Exscientia [5] | Generative AI-driven design | MALT1 inhibitor / Oncology | Next-generation Mucosa-Associated Lymphoid Tissue Lymphoma Translocation Protein 1 inhibitor [5] | IND-enabling studies [5] |
| DSP-0038 | Exscientia/Sumitomo Dainippon Pharma [18] | AI-designed molecule | Not Specified / Oncology | A drug developed using generative algorithms that has reached clinical trials [18] | Phase I (Inferred) |
| Insilico Medicine Compound | Insilico Medicine [1] | Generative AI platform (Generative Tensorial Reinforcement Learning) | QPCTL inhibitor / Oncology | Targets glutaminyl-peptide cyclotransferase-like protein, relevant to tumor immune evasion [1] | Preclinical/Phase I (Pipeline) |
| Z29077885 | AI-driven screening strategy [2] | AI-driven screening of large databases linking compounds and diseases | STK33 / Cancer | Induces apoptosis by deactivation of the STAT3 signaling pathway; causes cell cycle arrest at S phase [2] | Validated in vitro and in vivo (Preclinical) [2] |
Experimental Protocols for Validating AI-Designed Compounds
The transition from in silico design to clinical candidate requires rigorous experimental validation. The following protocols detail key methodologies used to characterize the efficacy, selectivity, and binding mechanisms of AI-generated drug candidates, as exemplified by recent prospective studies [30].
Protocol 1: In Vitro Binding Affinity and Selectivity Profiling
This protocol is used to biophysically confirm target engagement and assess selectivity against related targets.
- Objective: To determine the binding affinity (KD) and selectivity of a novel AI-designed PPARγ partial agonist [30].
- Materials:
- Recombinant Protein: Purified human PPARγ ligand-binding domain (LBD) [30].
- Control Ligands: Known PPARγ agonists (e.g., rosiglitazone) and inactive DMSO control.
- Assay Kit: Commercial fluorescence-based thermal shift assay (TSA) kit.
- Equipment: Real-time PCR system for thermal cycling and fluorescence detection.
- Procedure:
- Sample Preparation: Prepare a 1 µM solution of the PPARγ LBD in assay buffer. Add the AI-designed compound and control ligands at a range of concentrations (e.g., 0.1 nM – 100 µM). Include a SYPRO Orange fluorescent dye.
- Thermal Denaturation: Load samples into a 96-well plate and run a thermal ramp from 25°C to 95°C with a gradual increase (e.g., 1°C/min) on the real-time PCR system while monitoring fluorescence.
- Data Analysis: Calculate the melting temperature (Tm) for each sample from the resulting melt curves. Plot the change in Tm (ΔTm) against compound concentration to determine the apparent KD.
- Validation Criterion: A concentration-dependent increase in Tm indicates stable binding. The AI-designed compound should show a favorable KD (e.g., in the nanomolar range) and a selectivity profile distinct from full agonists in follow-up cellular assays [30].
Protocol 2: Functional Cellular Assay for Target Engagement and Efficacy
This protocol assesses the functional biological activity of the AI-generated compound in a cellular context.
- Objective: To evaluate the functional activity and potency (EC50) of an AI-designed CDK7 inhibitor in a cancer cell line [5].
- Materials:
- Cell Line: Relevant cancer cell line (e.g., MCF-7 breast cancer cells).
- Assay Kit: Commercial luminescent cell viability assay (e.g., CellTiter-Glo) and RNA extraction kit.
- Equipment: Microplate reader for luminescence detection, qPCR system.
- Procedure:
- Cell Treatment: Seed cells in a 96-well plate. The following day, treat with the AI-designed compound and a control inhibitor across a concentration gradient (e.g., 1 nM – 10 µM) for 72 hours.
- Viability Readout: Add CellTiter-Glo reagent to measure ATP levels as a surrogate for cell viability. Calculate the percentage of growth inhibition relative to DMSO-treated controls.
- Gene Expression Analysis: Extract RNA from parallel treated samples after 24 hours. Perform qPCR to measure the expression levels of known CDK7-dependent genes (e.g., MYC). Reduced expression confirms on-target mechanism.
- Validation Criterion: The compound should demonstrate a dose-dependent decrease in cell viability and downregulation of target genes, yielding a calculable EC50 or IC50 value [5].
Protocol 3: Protein-Ligand Co-Crystallography for Binding Mode Confirmation
This high-resolution structural method is the gold standard for confirming the predicted binding mode of an AI-designed molecule.
- Objective: To determine the crystal structure of an AI-designed PPARγ partial agonist in complex with its target protein [30].
- Materials:
- Protein: High-purity, purified PPARγ LBD.
- AI-Designed Ligand: Synthesized and purified compound.
- Crystallization Kit: Commercial sparse matrix crystallization screen.
- Procedure:
- Complex Formation: Incubate the PPARγ LBD with a molar excess of the AI-designed ligand on ice for 1-2 hours.
- Crystallization: Set up crystallization trials using the vapor diffusion method (e.g., sitting drop) with the commercial screen. Optimize promising conditions.
- Data Collection and Structure Solution: Flash-cool the crystal in liquid nitrogen. Collect X-ray diffraction data at a synchrotron source. Solve the structure by molecular replacement using a known PPARγ structure as a model.
- Validation Criterion: The electron density map must unambiguously show the AI-designed ligand bound in the active site, with specific atomic-level interactions (e.g., hydrogen bonds, hydrophobic contacts) matching or rationally differing from computational predictions [30].
Visualization of Pathways and Workflows
AI-Driven De Novo Drug Design Workflow
The following diagram illustrates the integrated "Design-Make-Test-Analyze" (DMTA) cycle, central to modern AI-driven de novo drug discovery.
Key Oncogenic Signaling Pathway
The STAT3 signaling pathway is a clinically relevant target in oncology, which has been successfully engaged by AI-designed molecules like Z29077885 [2].
The Scientist's Toolkit: Essential Research Reagents and Platforms
This section details key reagents, computational platforms, and data resources that form the foundation of AI-driven de novo drug discovery campaigns in oncology.
Table: Key Research Reagent Solutions for AI-Driven Oncology Drug Discovery
| Tool / Resource Name | Type | Primary Function in R&D | Application Example |
|---|---|---|---|
| DRAGONFLY [30] | Deep Learning Software | Ligand- and structure-based de novo molecular generation without need for application-specific fine-tuning. | Generating novel PPARγ partial agonists with confirmed bioactivity and crystallographic validation [30]. |
| Exscientia's Centaur Chemist [5] | Integrated AI Platform | Combines generative AI with automated synthesis and testing for closed-loop DMTA cycles. | Accelerating the design of clinical candidates like CDK7 and LSD1 inhibitors with high efficiency [5]. |
| BEKHealth Platform [72] | Clinical Data & NLP Tool | Analyzes EHRs with NLP to identify eligible patients for clinical trials, accelerating recruitment. | Identifying protocol-eligible patients three times faster with 93% accuracy for oncology trial enrollment [72]. |
| TransNEO / TRIDENT Models [71] | Multimodal AI (MMAI) Model | Integrates radiomics, digital pathology, and genomics to predict treatment response and stratify patients. | Identifying patient signatures for optimal benefit from specific oncology regimens in clinical trial data [71]. |
| ChEMBL Database [30] | Public Bioactivity Database | Curated database of bioactive molecules with drug-like properties, used for training AI models. | Building drug-target interactomes for deep learning models like DRAGONFLY [30]. |
| Allcyte Platform [5] | Phenotypic Screening Platform | Uses patient-derived tumor samples for high-content screening of AI-designed compounds. | Incorporating patient-derived biology into Exscientia's discovery workflow to improve translational relevance [5]. |
This application note provides a detailed comparison of four leading AI-driven drug discovery platforms, with a specific focus on their application in de novo design of novel oncology therapeutics. It summarizes their core technologies, quantitative outputs, and provides actionable experimental protocols for researchers.
The table below summarizes the core AI approaches, technology platforms, and key oncology programs of the four companies.
Table 1: AI Drug Discovery Platform Overview and Oncology Focus
| Company | Core AI Approach | Proprietary Platform Name | Key Differentiator | Representative Oncology Programs & Status (as of 2025) |
|---|---|---|---|---|
| Exscientia | Generative Chemistry, Centaur Chemist (AI + human expertise) [5] | Centaur Chemist, DesignStudio, AutomationStudio [5] | End-to-end automated design-make-test-analyze cycle; patient-derived biology integration [5] | GTAEXS-617 (CDK7i): Phase I/II in solid tumors [5]. EXS-73565 (MALT1i): In IND-enabling studies [5]. |
| Insilico Medicine | End-to-end Generative AI, Foundation Models | Pharma.AI (PandaOmics, Chemistry42, InClinico) [73] [74] | Fully integrated from target discovery to clinical forecasting; rapid de novo design [74] [75] | USP1 Inhibitor: For BRCA-mutant cancer, Phase II [73]. MEN2312 (KAT6i): Licensed to Menarini, Phase I for ER+/HER2- breast cancer [74]. QPCTL Inhibitor: For immuno-oncology, discovery stage [73]. |
| BenevolentAI | Knowledge-Graph & Machine Learning Driven Target Discovery | Benevolent Platform [76] | Unsupervised ML on patient data to discover endotypes and novel targets; precision medicine focus [77] | Discovery programs and target identification in oncology (Specific clinical candidates not listed in results) [77]. Collaboration with Novartis on oncology medicines [77]. |
| Recursion | Phenomics-First, High-Content Cellular Imaging | Recursion OS (Operating System) [78] | Maps trillions of cellular relationships with phenomics; integrated with Exscientia's generative chemistry post-merger [5] [78] | REC-617 (CDK7i): Phase I/2 in advanced solid tumors [78]. REC-7735 (PI3Kα H1047Ri): IND-enabling studies for breast cancer [78]. REC-102 (ENPP1i): Potential Phase 1 initiation in 2H26 [78]. |
Table 2: Quantitative Performance Metrics and Pipeline Strength
| Company | Avg. Discovery Timeline (Target to Candidate) | Estimated Synthesis & Testing Efficiency (vs. Traditional) | Clinical-Stage Pipeline (Total Programs) | Key Oncology-Specific Milestones (2024-2025) |
|---|---|---|---|---|
| Exscientia | "Substantially faster than industry standards" [5] | ~70% faster design cycles; 10x fewer compounds synthesized [5] | 3+ clinical compounds designed (oncology and other areas) [5] | Established MTD for CDK7 inhibitor REC-617; manageable safety profile and preliminary anti-tumor activity observed [78]. |
| Insilico Medicine | ~12-18 months (Average for 20 candidates from 2021-2024) [75] | 60-200 molecules synthesized and tested per program [75] | 10+ programs entered human trials [74] | Licensed a second AI-designed oncology candidate to Menarini ($20M upfront) [74]. USP1 inhibitor for BRCA-mutant cancer in Phase II [73]. |
| BenevolentAI | Information Missing | Information Missing | Information Missing | Investigating new indications and responders for Novartis oncology medicines in clinical development [77]. |
| Recursion | Information Missing | Information Missing | Multiple clinical and preclinical programs [78] | $30M milestone from Roche/Genentech for a microglial cell phenomap (neurology); GI oncology program optioned [78]. Progress in PI3Kα H1047R inhibitor REC-7735, showing tumor regressions in preclinical studies [78]. |
Experimental Protocols for AI-Driven Oncology Discovery
Protocol: Phenomics-Based Target and Hit Identification (Recursion OS Workflow)
This protocol outlines the process of using high-content cellular phenotyping to discover novel oncology targets and hits [5] [78].
I. Research Reagent Solutions
- Cell Lines: Isogenic cancer cell lines (e.g., with/without specific oncogenic mutations like PI3Kα H1047R) [78].
- Perturbagen Library: CRISPR knockouts, siRNA, ORF overexpression constructs, or small-molecule libraries [78].
- Staining Reagents: Multiplexed fluorescent dyes and antibodies for key oncology biomarkers (e.g., γH2AX for DNA damage, Cleaved Caspase-3 for apoptosis, Ki-67 for proliferation).
- Imaging Platform: High-throughput, high-content confocal imaging systems.
- Analysis Software: Recursion OS with customized image analysis pipelines.
II. Methodology
- Phenomap Generation:
- Seed a diverse panel of cancer cell lines relevant to the oncology indication in 384-well plates.
- Treat cells with the perturbagen library using automated liquid handling.
- After incubation, fix and stain cells with multiplexed fluorescent reagents to mark various cellular compartments and processes.
- Image each well using high-content microscopes, generating >100,000 images per experiment [78].
- Image Feature Extraction & Data Ingestion:
- Process images using convolutional neural networks (CNNs) to extract millions of quantitative morphological features (phenotypic features) per sample.
- Ingest feature data and chemical/genetic perturbagen metadata into the Recursion OS data lake.
- AI-Driven Phenomic Analysis:
- Use unsupervised machine learning to cluster perturbations based on their phenotypic profiles, creating a "phenotypic map" (phenomap).
- Identify novel perturbagens that induce a phenotypic signature similar to known oncogene knockouts or tumor suppressor activations but through a novel mechanism.
- Validate hits by correlating phenotypic signatures with known drug mechanisms and functional genomics data.
Protocol: Generative AI forDe NovoSmall Molecule Design (Insilico Medicine/Exscientia Workflow)
This protocol details the use of generative AI models for the de novo design of small molecule inhibitors for a validated oncology target.
I. Research Reagent Solutions
- Target Structure: Atomic-level 3D structure of the target (e.g., from AlphaFold2, X-ray crystallography, or cryo-EM).
- Training Data: Public and proprietary datasets of chemical structures with associated bioactivity (IC50, Ki), ADMET properties, and synthetic accessibility scores.
- Software Platforms: Insilico Medicine's Chemistry42 or Exscientia's DesignStudio.
- Validation Assays: High-throughput biochemical assays (e.g., FRET, TR-FRET) for target inhibition; cell-based viability or pathway activation assays (e.g., Western blot, NanoBRET).
II. Methodology
- Target Profiling and Constraints Definition:
- Define the Target Product Profile (TPP): required potency (e.g., IC50 < 100 nM), selectivity against a panel of kinases, and key ADMET properties (e.g., CYP inhibition, solubility).
- Input the 3D structure of the target's active/allosteric site.
- Generative Molecular Design:
- The generative AI model (e.g., a conditional generative adversarial network or a transformer-based model) proposes novel molecular structures that satisfy the TPP constraints.
- The system performs in silico scoring of generated compounds for binding affinity (via docking or free-energy perturbation), synthetic accessibility, and other properties [5] [74].
- Iterative Optimization & Candidate Selection:
- Select a diverse subset of top-ranking virtual compounds (e.g., 20-50) for synthesis.
- Synthesize compounds and test them in biochemical and cellular assays.
- Feed the experimental results (potency, selectivity, ADMET) back into the AI model to refine the next round of compound generation. This "design-make-test-analyze" loop continues until a preclinical candidate meeting all TPP criteria is identified [5].
Protocol: Knowledge-Graph-Driven Patient Endotyping for Target Discovery (BenevolentAI Workflow)
This protocol describes using AI to analyze patient data to discover distinct disease endotypes and identify novel oncology targets [77].
I. Research Reagent Solutions
- Patient Data: Multi-modal datasets including transcriptomics (RNA-seq), proteomics, genomics (whole exome/genome sequencing), and clinical data from public repositories (e.g., TCGA) and proprietary biobanks.
- Knowledge Graph: A structured, proprietary knowledge base integrating biological entities (genes, proteins, diseases, drugs, pathways) and their relationships from scientific literature, patents, and databases.
- Software: BenevolentAI Platform with machine learning and bioinformatics pipelines.
II. Methodology
- Data Integration and Graph Construction:
- Ingest and harmonize multi-omics and clinical data from a cohort of cancer patients (e.g., 500+ patients).
- This data is integrated into the knowledge graph, connecting patient-specific molecular alterations to established biological pathways and entities.
- Unsupervised Patient Stratification:
- Apply unsupervised machine learning (e.g., clustering algorithms) on the integrated patient data within the knowledge graph to identify distinct patient subgroups (endotypes) based on their underlying molecular drivers, not just clinical presentation.
- Target Hypothesis Generation:
- For a selected endotype of interest (e.g., a subgroup of non-responders to standard therapy), the platform identifies upstream regulators or key dysregulated nodes within the subnetwork that are central to the endotype's biology.
- The platform ranks these potential targets based on novelty, druggability, and causal evidence within the graph.
- In Silico and Experimental Validation:
- Validate target hypotheses by querying their association with patient survival and drug response in external datasets.
- Proceed to in vitro and in vivo experimental validation of the top-ranked targets.
The development of novel oncology therapeutics is a high-stakes endeavor, traditionally characterized by protracted timelines, exorbitant costs, and daunting attrition rates. The conventional drug discovery pipeline often requires 10 to 15 years and exceeds $2 billion per approved therapeutic, with success rates averaging less than 10% from first-in-human trials to market approval [79] [80]. However, the integration of artificial intelligence (AI) and de novo drug design methods is fundamentally reshaping this landscape, particularly in oncology. These computational approaches enable a "predict-then-make" paradigm, shifting the center of gravity from physical experimentation to in silico design and validation [81]. This Application Note provides a structured framework of quantitative metrics, detailed protocols, and essential research tools to benchmark and enhance the success of AI-driven de novo drug discovery campaigns for novel oncology therapeutics.
Quantitative Performance Metrics
To objectively evaluate the impact of AI-driven de novo design, key performance indicators (KPIs) must be tracked across the discovery and development continuum. The following metrics, derived from recent industry and academic reports, serve as critical benchmarks.
Table 1: Benchmarking AI-Driven vs. Traditional Drug Discovery Metrics
| Metric Category | Traditional Discovery | AI-Accelerated Discovery | Data Source/Example |
|---|---|---|---|
| Discovery Timeline | ~5 years to clinical candidate [5] | 18–24 months to clinical candidate [5] | Insilico Medicine (IPF drug): 18 months from target to Phase I [5] |
| Chemistry Efficiency | Requires synthesis of thousands of compounds [5] | 10x fewer compounds synthesized [5] | Exscientia (CDK7 inhibitor): 136 compounds synthesized for clinical candidate [5] |
| Clinical Trial Success Rate (ClinSR) | Average overall success rate: ~7.9% [80] | To be determined (most assets in early trials) [5] | Industry-wide analysis of 20,398 CDPs [80] |
| Oncology Clinical Success Rate | Phase I to Approval: ~5%–10% [80] | To be determined | Dynamic analysis of 21st-century trials [80] |
| R&D Cost per Approved Drug | ~$2.26 billion [81] [79] | Potential for significant reduction (AI streamlines early R&D) [81] | Industry-wide analysis accounting for attrition [81] |
Table 2: Clinical Trial Success Rates (ClinSR) by Phase and Modality
| Development Phase / Modality | Phase Transition Probability | Notes and Context |
|---|---|---|
| Phase I to II | ~50% | High attrition in phase transition [80] |
| Phase II to III | ~25%–30% | Significant drop due to efficacy failures [80] |
| Phase III to Approval | ~60%–70% | High cost of late-stage failure [80] [79] |
| Overall (Phase I to Approval) | ~7.9% (Average across all modalities/therapies) [80] | Calculated from 20,398 clinical development programs [80] |
| Small Molecules | Slightly above industry average | Better-established development pathways [80] |
| Biologics & Novel Modalities | Variable, often below average | e.g., Cell therapies and vaccines may have lower success rates [80] |
Experimental Protocols for AI-DrivenDe NovoDesign
This section details a validated protocol for prospective de novo drug design using deep interactome learning, enabling the generation of novel, bioactive small molecules for oncology targets.
Protocol: ProspectiveDe NovoDesign with Deep Interactome Learning
Principle: The DRAGONFLY (Drug-target interActome-based GeneratiON oF noveL biologicallY active molecules) framework leverages a graph-based drug-target interactome to enable ligand- and structure-based molecular generation without application-specific fine-tuning. It integrates a Graph Transformer Neural Network (GTNN) with a Chemical Language Model (CLM) to translate molecular graphs or protein binding sites into novel, optimized chemical structures [30].
Applications in Oncology: This protocol is particularly suited for generating selective modulators of oncology targets (e.g., nuclear receptors, kinases, immune checkpoints) with tailored properties for potency, selectivity, and synthesizability [30] [4].
Workflow Diagram:
Materials and Reagents:
- Hardware: High-performance computing cluster with multi-core CPUs, modern GPUs (e.g., NVIDIA A100/V100).
- Software: Python 3.8+, PyTorch or TensorFlow, RDKit, DRAGONFLY framework code.
- Data: 3D protein structures (PDB), annotated bioactivity data (ChEMBL), defined target product profile.
Procedure:
- Interactome Construction:
- Compile a structured interactome graph from public databases (e.g., ChEMBL). Nodes represent bioactive ligands and their macromolecular targets. Edges connect ligands to proteins with a binding affinity ≤ 200 nM [30].
- For structure-based design, filter the interactome to include only targets with known 3D structures.
Input Representation:
- For structure-based design: Represent the target's 3D binding site as a graph. Nodes are amino acid residues or key atoms; edges represent spatial relationships or interactions [30].
- For ligand-based design: Represent a known active ligand as a 2D molecular graph.
Model Execution & Molecular Generation:
- Process the input graph through the GTNN to generate a latent representation.
- The LSTM-based CLM decodes this representation into a SMILES string of a novel molecule.
- Constrain the generation by specifying desired physicochemical properties (e.g., molecular weight, lipophilicity) within the model to ensure drug-likeness [30].
In Silico Validation & Ranking:
- Synthesizability: Calculate the Retrosynthetic Accessibility Score (RAScore). Prioritize molecules with RAScore > certain threshold (e.g., >0.7) [30].
- Novelty: Quantify scaffold and structural novelty against known bioactive compounds using a rule-based algorithm (e.g., Tanimoto coefficient on ECFP4 fingerprints < 0.3) [30].
- Bioactivity Prediction: Employ pre-trained QSAR models (e.g., Kernel Ridge Regression with ECFP4/CATS descriptors) to predict pIC50 against the intended target. Mean Absolute Error (MAE) of validated models should be ≤ 0.6 [30].
- Selectivity Screening: Perform in silico profiling against anti-targets and related off-targets (e.g., other nuclear receptors for a PPARγ program) using similar QSAR models [30].
Experimental Validation:
- Chemically synthesize the top-ranking de novo designs.
- Characterize compounds biophysically (e.g., SPR, DSF) and biochemically to determine binding affinity and functional activity.
- Validate the binding mode empirically, ideally via X-ray crystallography of the ligand-receptor complex [30].
The Scientist's Toolkit: Key Research Reagents & Platforms
Successful implementation of AI-driven de novo design relies on a suite of computational and experimental resources.
Table 3: Essential Research Reagents and Platforms for AI-Driven Oncology Drug Discovery
| Tool / Reagent | Type | Function / Application | Example Use Case |
|---|---|---|---|
| DRAGONFLY Framework | Computational Platform | Ligand- and structure-based de novo molecular generation without task-specific fine-tuning. | Generating selective PPARγ partial agonists with validated crystallographic binding modes [30]. |
| Exscientia 'Centaur Chemist' Platform | Integrated AI Platform | End-to-end generative AI for small-molecule design, integrated with automated synthesis and testing. | Designing clinical candidates for oncology (CDK7, LSD1 inhibitors) with ~70% faster design cycles [5]. |
| ChEMBL Database | Public Data Resource | Curated database of bioactive molecules with drug-like properties for model training and validation. | Constructing the drug-target interactome for deep learning models [30]. |
| Retrosynthetic Accessibility Score (RAScore) | Computational Metric | Quantifies the feasibility of synthesizing a given molecule. | Prioritizing de novo-generated compounds for synthesis [30]. |
| Patient-Derived Organoids/Ex Vivo Models | Biological Reagent | High-content phenotypic screening on biologically relevant human tissue models. | Validating efficacy of AI-designed compounds in patient-derived contexts (e.g., Exscientia's Allcyte platform) [5]. |
| Cloud & Robotics Infrastructure | Enabling Infrastructure | Scalable computing (e.g., AWS) linked with automated synthesis ('AutomationStudio') for closed-loop design-make-test-analyze cycles. | Running large-scale generative models and rapidly iterating compound design and testing [5]. |
The quantitative metrics and standardized protocols outlined in this document provide a roadmap for leveraging AI to overcome the historical challenges of drug discovery. By adopting these KPIs for benchmarking, implementing robust de novo design protocols like DRAGONFLY, and utilizing the associated toolkit, researchers can systematically enhance the speed, efficiency, and ultimate success of developing novel oncology therapeutics.
The journey of a novel oncology therapeutic from concept to clinic is a high-stakes endeavor, characterized by substantial costs and a low probability of market approval, which varies between 3.5% and 5% for oncology drugs [82]. Preclinical drug development is the critical gateway designed to improve these odds. Its primary aims are to determine whether a compound is sufficiently effective against a disease target, reasonably safe for initial human testing, and to establish a starting dose for Phase I clinical trials [82]. This process systematically moves through a series of validation stages, beginning with controlled in vitro studies and culminating in complex in vivo models, to build a robust evidence base for transitioning a candidate drug into human testing [82].
In Vitro Screening: The Foundation of Discovery
In vitro models provide the first line of evidence in preclinical validation, enabling high-throughput, controlled investigation of drug activity and resistance mechanisms.
High-Throughput and Quantitative Screening
High-throughput screening (HTS) is a foundational technique for simultaneously analyzing thousands of compounds for biological activity [83]. A screen is considered high throughput when it conducts over 10,000 assays per day [83]. The advent of quantitative HTS (qHTS), which tests compounds across multiple concentrations, has further improved the reliability of these screens by generating concentration-response data, thereby reducing false-positive and false-negative rates [84]. In qHTS, the Hill equation (HEQN) is commonly used to model this data, yielding key parameters such as AC50 (potency) and Emax (efficacy) [84]. However, parameter estimation can be highly variable if the experimental design does not adequately define the upper and lower response asymptotes [84].
Table 1: Key In Vitro Models and Their Applications in Oncology
| Model Type | Key Features | Primary Applications in Oncology |
|---|---|---|
| 2D Cell Lines [82] | Panels of human tumor cell lines (e.g., NCI-60); relatively inexpensive, scalable, and reproducible. | - Large-scale phenotypic screens- Identifying potential anticancer agents- Studying cell biology and drug sensitivity |
| 3D Organoids [82] [85] | Three-dimensional cultures derived from patient samples, PDX models, or murine tissues. | - Retaining tumor morphology and genetic features- Predicting patient drug responses- Studying tumor heterogeneity and validating findings from 2D screens |
| Drug-Induced Resistance Models [85] | Created by exposing cancer cells to therapeutic agents until resistance develops (continuous, pulsed, or high-dose). | - Revealing novel and complex resistance mechanisms- Mimicking the clinical development of resistance over time- Biomarker comparison before and after resistance |
| Engineered Resistance Models [85] | Created using genetic editing (e.g., CRISPR) to introduce specific resistance mutations (Knock-in/Knock-out). | - Rapidly examining the impact of specific genetic alterations- Consistent expression of a desired resistance phenotype- Assessing gene function via targeted deletion |
Protocol: Quantitative High-Throughput Screening (qHTS)
Objective: To identify active compounds ("hits") and quantify their potency and efficacy from a large chemical library. Materials:
- Libraries: Combinatorial chemistry, protein, genomics, or peptide libraries [83].
- Assay Plates: 1536-well plates or similar low-volume plates [84].
- Detection System: High-sensitivity detectors for cellular or biochemical readouts [84].
- Liquid Handling: Automated robotics for efficient and precise sample dispensing [83].
Procedure:
- Target Identification & Assay Design: Focus on a specific biological target (e.g., a protein) involved in a disease mechanism [83].
- Primary Screening: Screen the entire library against the target. Quickly eliminate compounds with no or poor effect [83].
- qHTS Profiling: For the primary hits, perform multiple-concentration testing (e.g., across 15 concentrations) to generate concentration-response curves [84].
- Data Analysis: Fit the response data to the Hill equation to estimate AC50 (potency) and Emax (efficacy) for hit prioritization [84].
- Secondary Screening: Characterize prioritized hits in more refined, often cell-based, assays to confirm activity and begin assessing selectivity [83].
In Vivo Validation: From Model Organisms to Clinical Prediction
Following successful in vitro characterization, drug candidates progress to in vivo models, which are essential for evaluating complex physiological responses, efficacy in a whole-body system, and toxicity.
Model Selection and Efficacy Testing
The choice of in vivo model is critical and depends on the research question. Key models include:
- Human Tumor Xenografts: Immunodeficient mice (e.g., nude mice) implanted with human tumor cell lines. The discovery of T cell-deficient nude mice in the 1980s significantly advanced this model type [82].
- Patient-Derived Xenografts (PDXs): Immunodeficient mice implanted with tumor tissue directly from a patient. PDXs most closely resemble patient genetics and histopathology and are used in tumor inhibition assays for evaluating target-specific inhibitors [82] [86].
- Genetically Engineered Mouse Models (GEMMs): Mice engineered with germline or somatic cell modifications to test the role of potential targets in spontaneous tumorigenesis [86].
- Syngeneic Models: Immunocompetent mice implanted with murine tumor cells, allowing for the study of interactions between the therapy and an intact immune system [87].
The standard efficacy study involves monitoring tumor growth kinetics in treated versus control groups to calculate Tumor Growth Inhibition (TGI) [86] [87]. Advanced in vivo imaging techniques, such as bioluminescence and microPET/CT, are used to non-invasively monitor disease localization, burden, and progression [87].
Table 2: Comparative Analysis of Standard In Vivo Pharmacology Models
| Model | Key Features | Strengths | Limitations |
|---|---|---|---|
| Cell Line-Derived\nXenograft (CDX) [82] | - Human cancer cell lines implanted in immunodeficient mice- Well-characterized | - Highly reproducible- Scalable for high-throughput studies | - Limited tumor heterogeneity- Does not recapitulate human tumor microenvironment (TME) |
| Patient-Derived\nXenograft (PDX) [82] [86] | - Fresh patient tumor tissue implanted in immunodeficient mice | - Retains patient tumor histopathology and genetics- Better predictive value for clinical response | - Requires immunodeficient hosts- Longer engraftment time, higher cost |
| Syngeneic Model [87] | - Mouse tumor cell lines implanted in immunocompetent mice of the same genetic background | - Intact mouse immune system allows for immuno-oncology studies- Relatively fast and inexpensive | - Mouse TME, not human- Limited range of tumor types |
| Genetically Engineered\nMouse Model (GEMM) [86] | - Mice with genetically engineered mutations that drive spontaneous tumor development | - Tumors arise in native tissue context- Ideal for studying tumorigenesis and target validation | - Long development time, high cost- Tumor development can be variable |
Protocol: Efficacy Testing in a Patient-Derived Xenograft (PDX) Model
Objective: To evaluate the in vivo anti-tumor efficacy of a novel oncology therapeutic candidate. Materials:
- Animals: Immunodeficient mice (e.g., NOD-scid IL2Rγnull (NSG)) [82].
- Tumor Tissue: Patient-derived tumor tissue, typically from a pre-established and characterized PDX biobank [82] [86].
- Test Article: The drug candidate, formulated for in vivo administration (e.g., oral gavage, intraperitoneal injection).
- Calipers: For measuring tumor volume [87].
- In Vivo Imaging System (IVIS): For bioluminescence or fluorescence imaging, if tumor cells are engineered with reporters [87].
Procedure:
- Model Development: Implant a small fragment of patient-derived tumor tissue subcutaneously into the flank of an immunodeficient mouse [87].
- Tumor Growth Monitoring: Allow the tumor to engraft and grow. Monitor tumor volume regularly by measuring with calipers (Volume = (length × width²)/2) or via in vivo imaging [87].
- Randomization & Dosing: When tumors reach a predetermined volume (e.g., 100-200 mm³), randomize mice into treatment and control groups. Begin dosing according to the planned schedule [87].
- Efficacy Monitoring: Continue treatment and measure tumor volumes and animal body weights 2-3 times per week for the study duration.
- Endpoint Analysis: At the end of the study, calculate the Tumor Growth Inhibition (TGI) percentage. Collect tumors and key organs for further histopathological and molecular analysis (pharmacodynamics) [87].
Integrated Workflows: Overcoming Drug Resistance
Drug resistance is the leading cause of treatment failure in oncology, necessitating integrated strategies that leverage both in vitro and in vivo models to study and overcome it [85].
Two primary approaches for modeling resistance are:
- Drug-Induced Resistance: Exposing cancer cells in vitro or in vivo to increasing doses of a therapeutic until resistance develops. This can reveal novel, complex mechanisms but can be time-consuming and variable [85].
- Engineered Resistance: Using techniques like CRISPR/Cas9 to introduce specific genetic alterations known to confer resistance in well-characterized models. This allows for focused study but may miss complex, multi-factorial mechanisms [85].
A powerful application involves using matched patient-derived tumor organoids (PDTOs) and PDX-derived organoids (PDXOs) alongside their in vivo PDX counterparts. This integrated system allows for in vitro drug screening on the organoids to rapidly identify candidate therapies, which are then validated in vivo in the matched PDX model, streamlining the discovery pipeline [82].
Protocol: Generating a Drug-Induced Resistance Model
Objective: To mimic the clinical development of resistance by generating a cancer cell population resistant to a targeted therapy. Materials:
- Parental Cell Line: The original, drug-sensitive cancer cell line (e.g., HCC827 for EGFR TKIs) [85].
- Targeted Therapeutic: The drug of interest (e.g., an EGFR TKI like osimertinib) [85].
- Cell Culture Supplies: Standard tissue culture flasks/plates, growth medium, and passaging reagents.
Procedure:
- Initial Exposure: Culture the parental, drug-sensitive cells and expose them to a low, sub-lethal concentration of the drug [85].
- Dose Escalation: Two main strategies can be employed:
- Selection & Expansion: Monitor cell death and proliferation. Once a resistant population emerges that can proliferate at a concentration that would kill the parental line, expand these cells.
- Validation: Confirm the resistant phenotype by comparing the IC~50~ of the resistant line to the parental line using a cell viability assay. The resistant line should have a significantly higher IC~50~.
- Mechanism Investigation: Use the resistant line for downstream -omic analyses (genomics, proteomics) to identify the acquired resistance mechanisms [85].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Experimental Validation
| Reagent / Material | Function / Application |
|---|---|
| CRISPR/Cas9 Gene Editing Systems [85] | Engineered resistance models; creating knock-in/knock-out cell lines to study specific genetic alterations. |
| Patient-Derived Tumor Organoids (PDTOs) [82] | High-throughput in vitro drug screening; maintaining patient-specific tumor heterogeneity for predictive response modeling. |
| Liquid Chromatography (LC) Systems [87] | Preclinical pharmacokinetics (PK); determining drug and metabolite levels in plasma, serum, blood, and tissues over time. |
| Organ-on-a-Chip Platforms [82] | Preclinical toxicology; modeling complex human tissue interfaces and providing a human-relevant system for safety assessment. |
| Combinatorial Chemistry Libraries [83] | HTS; providing vast collections of diverse chemical compounds for primary screening against a biological target. |
| Anti-Apoptosis Assay Kits | Mechanism-of-action studies; determining if a drug candidate induces programmed cell death. |
| Cytokine Profiling Arrays | Immuno-oncology; measuring immune cell activation and cytokine secretion in syngeneic or humanized mouse models. |
The landscape of preclinical oncology drug development is being reshaped by the complementary use of sophisticated in vitro and in vivo models. While traditional models remain valuable, the integration of advanced tools like PDTOs, GEMMs, qHTS, and AI-driven bioinformatics creates a more predictive and human-relevant framework [82]. This iterative, integrated approach to experimental validation, which strategically employs both in vitro and in vivo studies, is critical for de-risking the development of novel oncology therapeutics and enhancing the likelihood of clinical success.
Artificial Intelligence (AI) has rapidly evolved from a theoretical promise to a tangible force in drug discovery, driving a paradigm shift that replaces labor-intensive, human-driven workflows with AI-powered discovery engines capable of compressing timelines and expanding chemical and biological search spaces [5]. By mid-2025, dozens of AI-driven drug candidates had entered clinical trials, a remarkable leap from essentially zero in 2020 [5]. This transition is particularly impactful in oncology, where tumor heterogeneity, resistance mechanisms, and complex microenvironmental factors make effective targeting especially challenging [1]. AI-driven platforms claim to drastically shorten early-stage research and development timelines and cut costs by using machine learning (ML) and generative models to accelerate tasks compared with traditional approaches long reliant on cumbersome trial-and-error [5]. However, a critical question remains: Is AI truly delivering better success, or just faster failures? This Application Note provides a framework for differentiating accelerated discovery from genuine improvements in clinical success rates within de novo drug design for novel oncology therapeutics.
Current Landscape: AI-Driven Clinical Candidates
The growth of AI-designed or AI-identified drug candidates entering human trials has been exponential, with over 75 AI-derived molecules reaching clinical stages by the end of 2024 [5]. These candidates span a spectrum of AI approaches, from generative chemistry and physics-based simulations to phenotypic screening and knowledge-graph-driven target discovery [5]. The table below summarizes prominent examples and their reported efficiency gains.
Table 1: Select AI-Driven Oncology Drug Candidates and Efficiency Metrics
| Company / Platform | Drug Candidate / Program | Indication / Target | Reported Efficiency Gains | Clinical Stage (as of 2025) |
|---|---|---|---|---|
| Exscientia (Generative AI Design) | GTAEXS-617 (CDK7 inhibitor) | Solid Tumors [5] | Clinical candidate achieved after synthesizing only 136 compounds [5] | Phase I/II Trial [5] |
| Exscientia | EXS-21546 (A2A receptor antagonist) | Immuno-Oncology [5] | Program halted due to insufficient therapeutic index prediction [5] | Discontinued (Phase I) [5] |
| Insilico Medicine (Generative AI) | IPF Drug (Target Discovery & Design) | Idiopathic Pulmonary Fibrosis [5] | Target discovery to Phase I in 18 months [5] | Phase I [5] |
| Insilico Medicine | Novel QPCTL Inhibitors | Tumor Immune Evasion [1] | AI-identified novel target and inhibitors [1] | Preclinical/Oncology Pipelines [1] |
| DRAGONFLY (Interactome Learning) | PPARγ Partial Agonists | Nuclear Receptor Target [30] | "Zero-shot" generation of potent, selective agonists with confirmed binding mode [30] | Preclinical (Profiled) [30] |
Analytical Framework: Disentangling Speed from Success
To objectively assess the impact of AI, researchers must distinguish between metrics of acceleration and metrics of success. Acceleration refers to the compression of predefined timelines within the discovery and preclinical phases, while success pertains to the probability that a candidate will successfully transition through clinical development stages to eventual approval.
Quantifying Acceleration Metrics
Acceleration is most readily measured by comparing duration and resource utilization against industry benchmarks.
Table 2: Key Performance Indicators for Discovery Acceleration
| KPI Category | Specific Metric | Traditional Benchmark | AI-Driven Benchmark | Measurement Method |
|---|---|---|---|---|
| Timeline Compression | Target-to-Candidate Time | ~3-6 years [1] | ~18-24 months (e.g., Insilico Medicine) [5] | Project timeline tracking |
| Chemistry Efficiency | Compounds Synthesized | Thousands [5] | Hundreds (e.g., 136 for Exscientia's CDK7 inhibitor) [5] | Design-make-test-learn (DMTL) cycle logs |
| Design Cycle Speed | Design-Make-Test-Analyze Cycle | Industry standard | ~70% faster, 10x fewer compounds (e.g., Exscientia) [5] | Cycle time tracking across iterations |
Assessing Success Rate Indicators
True success is measured by a candidate's performance in rigorous biological and clinical validation. Key indicators include:
Table 3: Indicators of Improved Success Rates in Preclinical and Clinical Development
| Development Stage | Success Indicator | Data Source / Assay | Interpretation |
|---|---|---|---|
| Preclinical | Selectivity Profile & Off-Target Predictions | In vitro panel screening; In silico prediction (e.g., DRAGONFLY) [30] | A favorable profile suggests reduced risk of adverse effects. |
| Preclinical | Efficacy in Complex Biology | Patient-derived organoids/PDX models; High-content phenotypic screening (e.g., Exscientia's Allcyte platform) [5] | Improved translational relevance over simple cell lines. |
| Clinical (Phase I) | Therapeutic Index / Maximum Tolerated Dose (MTD) | First-in-Human Trial Data | A higher MTD and wide therapeutic window indicate a better safety profile. |
| Clinical (Phase II) | Objective Response Rate (ORR) & Biomarker Correlation | Phase II Trial Results; Biomarker analysis (e.g., AI-discovered biomarkers) [1] | Confirmation of hypothesized mechanism and efficacy in patients. |
Experimental Protocols for Outcome Analysis
Protocol: In Silico Target Validation and Hit Identification
This protocol utilizes platforms like the DRAGONFLY framework for de novo design [30].
- I. Define Target Product Profile (TPP): Establish desired potency (IC50/EC50), selectivity against related targets (e.g., kinase panels), ADME properties (e.g., Lipinski's Rule of 5), and synthesizability (e.g., Retrosynthetic Accessibility Score - RAScore) [30].
- II. Configure the AI Model:
- III. Generate and Prioritize Virtual Library: Execute the model to generate a virtual compound library. Rank compounds using a combined scoring function integrating:
Protocol: Experimental Validation of AI-Designed Candidates
This protocol outlines the critical wet-lab experiments to validate AI-generated hits.
- I. Compound Synthesis & Characterization:
- Synthesize top-ranking designs.
- Characterize purity and structure via LC-MS and NMR.
- II. In Vitro Biochemical/Biophysical Assays:
- Primary Potency Assay: Determine IC50/EC50 against the purified target protein.
- Selectivity Panel Screening: Test against a panel of related targets (e.g., kinase family, nuclear receptor subtypes) to establish selectivity profile [30].
- Cellular Efficacy Assay: Measure potency in cell-based assays (e.g., cell viability, reporter gene assays).
- Cytotoxicity Assessment: Test in relevant normal cell lines to gauge initial therapeutic window.
- III. Structural Validation (If Applicable):
- Pursue co-crystallization of the lead compound with the target protein.
- Solve the crystal structure to confirm the predicted binding mode, as demonstrated with DRAGONFLY-designed PPARγ agonists [30].
- IV. Advanced Disease Models:
- Test efficacy in patient-derived organoids or ex vivo patient tissue samples, as enabled by Exscientia's patient-first strategy [5].
- Progress validated hits to in vivo patient-derived xenograft (PDX) models.
The following workflow diagrams the integrated computational and experimental pathway for analyzing AI-derived candidates.
Integrated AI Drug Design and Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
The following reagents and platforms are essential for executing the described analytical protocols.
Table 4: Essential Research Reagents and Platforms for AI-Driven Oncology Discovery
| Item / Solution | Function / Application | Example / Provider Context |
|---|---|---|
| De Novo Design Software | Generates novel molecular structures from scratch based on TPP constraints. | DRAGONFLY (interactome-based) [30], Exscientia's Centaur Chemist [5], Insilico Medicine's Generative Tensorial Reinforcement Learning (GENTRL) [1]. |
| Target Interaction Database | Provides structured bioactivity data for model training and validation. | ChEMBL [30], The Cancer Genome Atlas (TCGA) for oncology target identification [1]. |
| Patient-Derived Biology Models | Provides translational, clinically relevant models for efficacy testing. | Patient-derived organoids (PDOs), patient-derived xenografts (PDXs), Exscientia's Allcyte platform for ex vivo patient tissue screening [5]. |
| High-Content Phenotypic Screening | Multiparametric analysis of compound effects in complex biological systems. | Recursion's phenomics platform [5], Cell painting assays. |
| Automated Synthesis & Testing | Closes the Design-Make-Test-Learn (DMTL) loop with high throughput. | Exscientia's AutomationStudio with robotics-mediated synthesis [5]. |
Differentiating faster discovery from improved success rates requires a multi-faceted approach that combines rigorous in silico design with robust experimental validation across increasingly complex biological systems. While current data demonstrates undeniable acceleration—compressing discovery timelines from years to months and drastically reducing the number of compounds needed—the ultimate validation of improved success rates hinges on clinical outcomes [5]. The analytical frameworks, protocols, and tools detailed in this Application Note empower researchers to move beyond mere efficiency metrics and critically evaluate whether AI-driven de novo design truly yields higher-quality, more effective oncology therapeutics with a greater chance of success in the clinic. As the field matures, the integration of patient-derived data from the earliest stages of discovery will be critical to ensuring that accelerated timelines translate into tangible patient benefit.
Regulatory and Ethical Considerations for AI-Designed Drug Candidates
The integration of artificial intelligence (AI) into drug discovery, particularly for de novo design of oncology therapeutics, represents a paradigm shift in pharmaceutical research. While AI technologies can compress discovery timelines from years to months and identify novel drug candidates with unprecedented efficiency, they also introduce complex regulatory and ethical challenges [5]. This document outlines the essential considerations and protocols for researchers developing AI-designed oncology drug candidates, ensuring compliance with evolving global frameworks while maintaining ethical rigor. The guidance is structured to support the broader thesis that responsible innovation is paramount for the successful translation of AI-derived discoveries into safe, effective cancer therapies.
Current Regulatory Landscape
Global regulatory bodies are developing frameworks to guide the use of AI in drug development, emphasizing a risk-based approach tied to the technology's specific context of use (COU) [88] [89] [90].
United States Food and Drug Administration (FDA) Framework
The FDA's 2025 draft guidance, "Considerations for the Use of Artificial Intelligence to Support Regulatory Decision-Making for Drug and Biological Products," establishes a foundational risk-based credibility assessment framework [88] [89] [90]. The core principles are:
- Context of Use (COU) as a Starting Point: The COU defines the specific role and scope of an AI model in addressing a regulatory question. It is the critical factor for determining risk and necessary validation [90].
- Risk-Based Credibility Assessment: Risk is determined by both the model influence risk (degree of influence on decision-making) and the decision consequence risk (potential impact on patient safety or drug quality) [90]. High-risk AI models, such as those influencing clinical trial endpoints or patient safety, require comprehensive disclosure and validation.
- Seven-Step Credibility Framework: The FDA recommends a structured process to establish model credibility: 1) Define the question of interest; 2) Define the COU; 3) Identify model assumptions; 4) Assess model applicability to the COU; 5) Assess model verification; 6) Assess model validation; and 7) Assess model performance and uncertainty [89].
The following diagram illustrates the FDA's risk-based assessment pathway for an AI model in drug development.
Table 1: Overview of Global Regulatory Approaches to AI in Drug Development
| Regulatory Body | Key Guidance/Document | Core Regulatory Approach | Noteworthy Features |
|---|---|---|---|
| U.S. FDA | Draft Guidance (Jan 2025) [90] | Risk-based credibility assessment tied to Context of Use (COU). | Seven-step credibility framework; Focus on model transparency and data fitness. |
| European Medicines Agency (EMA) | Reflection Paper (Oct 2024) [89] | Structured, cautious approach requiring rigorous upfront validation. | First qualification opinion on an AI methodology for liver disease diagnosis issued in March 2025 [89]. |
| UK MHRA | Principles-based regulation [89] | Apply existing technology-neutral laws (e.g., Medical Device Regulations). | "AI Airlock" regulatory sandbox to foster innovation in a controlled environment [89]. |
| Japan PMDA | PACMP for AI-SaMD (2023) [89] | "Incubation function" to accelerate access; Pro-innovation. | Post-Approval Change Management Protocol (PACMP) allows pre-approved AI model updates post-market. |
International Regulatory Perspectives
Globally, regulatory approaches are converging on core principles but differ in implementation. A comparative overview is provided in Table 1. The European Medicines Agency (EMA) emphasizes rigorous upfront validation and comprehensive documentation [89]. The UK's Medicines and Healthcare products Regulatory Agency (MHRA) favors a principles-based approach, extending existing software regulations to cover "AI as a Medical Device" (AIaMD) [89]. Japan's Pharmaceuticals and Medical Devices Agency (PMDA) has implemented a proactive Post-Approval Change Management Protocol (PACMP) for AI-based software, facilitating continuous algorithm improvement without requiring a full resubmission [89].
Ethical Framework and Implementation
The application of AI in oncology drug development must be guided by a robust ethical framework to ensure patient safety, uphold public trust, and promote equitable outcomes [91].
Core Ethical Principles
A widely adopted framework is based on four core principles: Autonomy, Justice, Non-maleficence, and Beneficence [91]. The practical application of these principles across the drug development lifecycle is critical.
Protocol for Ethical Risk Assessment in AI-Driven Oncology Discovery
This protocol provides a step-by-step methodology for identifying and mitigating ethical risks throughout the AI drug discovery pipeline.
Objective: To systematically evaluate and address ethical risks associated with AI models used in de novo design and development of oncology therapeutics. Materials: AI model specifications, training data documentation, model performance metrics, patient data provenance records, institutional review board (IRB) protocols.
Procedure:
Data Provenance and Consent Audit
- Action: Map the origin of all data used for AI model training (e.g., public genomic databases, hospital EHRs, biobanks). Verify that informed consent covers AI-driven drug discovery applications.
- Documentation: Create a data lineage report. Record specific consent language related to secondary use for AI research [91].
- Mitigation: If consent is ambiguous or insufficient for the planned COU, consult the IRB. Consider data anonymization or seeking re-consent where feasible.
Algorithmic Bias and Fairness Assessment
- Action: Quantitatively assess the training and clinical trial data for representativeness across racial, ethnic, gender, and socioeconomic groups relevant to the cancer indication.
- Documentation: Perform statistical analysis (e.g., χ² test) to identify under-represented groups. Use fairness metrics (e.g., demographic parity, equalized odds) to evaluate model predictions across subgroups [91] [1].
- Mitigation: If bias is detected, employ techniques like re-sampling, re-weighting, or adversarial de-biasing. Proactively recruit from underrepresented populations in subsequent validation studies.
Pre-clinical Dual-Track Verification
- Action: Validate all AI-generated hypotheses (e.g., target identification, compound efficacy) using parallel, independent traditional experimental methods.
- Documentation: For a novel AI-predicted target, the protocol requires:
- AI Track: In silico validation (e.g., molecular dynamics simulation, pathway analysis).
- Traditional Track: In vitro validation (e.g., cell-based assays, CRISPR knockout) and in vivo studies (e.g., patient-derived xenograft models in mice) [91].
- Rationale: This mitigates the risk of "black box" predictions leading to undetected intergenerational toxicity or efficacy failures, as exemplified by historical incidents like thalidomide [91].
Transparency and Explainability (XAI) Analysis
- Action: Implement Explainable AI (XAI) techniques to interpret the AI model's decisions.
- Documentation: For a novel compound, generate reports using methods like SHAP (SHapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) to identify which molecular features most influenced the AI's design decision [1] [90].
- Submission Ready: These reports are crucial for regulatory submissions to the FDA and EMA, demonstrating model credibility and enabling expert review [89] [90].
Protocol for AI Model Lifecycle Management and Regulatory Submission
This protocol outlines the end-to-end process for developing, validating, and maintaining an AI model used in a critical COU, such as analyzing clinical trial endpoints.
Objective: To ensure the AI model remains credible, reliable, and compliant throughout the drug development lifecycle. Materials: AI development platform, version control system (e.g., Git), documented standard operating procedures (SOPs), automated monitoring tools for data drift.
Procedure:
Pre-Submission: Model Development and Internal Validation
- Define COU and Question of Interest: Clearly state the AI's purpose (e.g., "To identify eligible metastatic melanoma patients for trial NCTXXX by analyzing EHR data with NLP").
- Data Curation and Management: Document data sources, cleaning procedures, and any transformations. Address missing data and outliers. Split data into training, validation, and hold-out test sets.
- Model Training and Tuning: Train the model, hyperparameter tune using the validation set, and document all steps to ensure reproducibility.
- Comprehensive Model Evaluation:
- Performance Metrics: Calculate standard metrics (e.g., AUC-ROC, accuracy, precision, recall, F1-score) on the hold-out test set.
- Robustness and Generalizability: Test the model on external datasets or via cross-validation to assess performance stability.
- Bias and Fairness Assessment: As per the ethical protocol, evaluate model performance across patient subgroups.
Regulatory Submission Dossier Preparation
- Compile the following information for regulatory review, with detail commensurate with the determined risk level [90]:
- Model Description: Architecture, input/output definitions, and underlying algorithm.
- Data Description: Sources, pre-processing steps, and representativeness.
- Training Description: Hyperparameters, optimization method, and hardware used.
- Evaluation Results: All performance, robustness, and fairness metrics.
- XAI Analysis: Outputs of interpretability methods.
- Lifecycle Management Plan: A detailed plan for ongoing monitoring and updates (Step 3).
- Compile the following information for regulatory review, with detail commensurate with the determined risk level [90]:
Post-Submission: Lifecycle Maintenance and Monitoring
- Implement Continuous Monitoring: Deploy automated systems to track model performance and detect "model drift" (e.g., data drift, concept drift) in real-time [89] [90].
- Establish a Retraining Protocol: Define triggers for model retraining (e.g., performance decay, significant data drift) and a documented procedure for doing so.
- Manage Model Updates: For substantial changes, follow the FDA's defined process or Japan's PACMP, if applicable, which may require regulatory notification or supplemental submission [89].
The Scientist's Toolkit: Research Reagents and Computational Platforms
Successful implementation of AI-driven oncology discovery relies on a suite of wet-lab and computational tools. The table below details key resources.
Table 2: Essential Research Reagents and Platforms for AI-Driven Oncology Drug Discovery
| Item/Platform Name | Type | Primary Function in AI Drug Discovery | Example Use Case |
|---|---|---|---|
| DeepChem [91] | Software Library | Provides a foundational toolkit for applying deep learning to chemistry and biology. | Predicting molecular bioactivity or toxicity for virtual compound screening. |
| BRENDA Database [91] | Knowledgebase | A comprehensive enzyme resource used to train AI models on enzyme function and kinetics. | Identifying novel enzymatic drug targets in cancer metabolic pathways. |
| Recursion Pharmaceuticals Platform [91] [5] | Integrated AI & Phenomics Platform | Uses ML to analyze high-content cellular imaging data, linking compound-induced phenotypic changes to disease biology. | Discovering new drug mechanisms of action or repurposing opportunities for oncology. |
| Exscientia's Centaur Chemist [5] | AI-Driven Design Platform | Integrates generative AI with human expertise to iteratively design and optimize novel compounds meeting target product profiles. | De novo design of a small-molecule CDK7 inhibitor for solid tumors. |
| BEKHealth AI Platform [72] | Clinical Trial SaaS | Uses NLP to analyze structured/unstructured EHR data for patient recruitment and trial feasibility analytics. | Identifying protocol-eligible oncology patients 3x faster than manual review. |
| PathAI [1] | Digital Pathology Tool | Applies deep learning to histopathology images to identify predictive biomarkers for therapy response. | Discovering morphological biomarkers in tumor biopsies predictive of immunotherapy success. |
The integration of AI into the de novo design of oncology therapeutics offers immense promise but demands a disciplined, principled approach. Success is contingent not only on algorithmic innovation but also on rigorous adherence to an evolving regulatory landscape and a steadfast commitment to ethical principles. By implementing the structured protocols and considerations outlined herein—from the FDA's risk-based credibility framework and dual-track experimental validation to proactive bias mitigation and lifecycle management—researchers can navigate this complex terrain. This will ultimately accelerate the delivery of safe, effective, and equitable AI-designed cancer therapies to patients.
Conclusion
De novo drug design, powered by advanced generative AI, is fundamentally reshaping the oncology therapeutics landscape by compressing discovery timelines and expanding the explorable chemical universe. The integration of these computational methods throughout the drug development continuum—from AI-driven target identification to clinically validated candidates—demonstrates a paradigm shift from serendipity to engineered precision. Future progress hinges on overcoming persistent challenges in data quality, model interpretability, and seamless experimental integration. The ongoing maturation of these technologies, coupled with evolving regulatory frameworks, promises to deliver more effective, personalized, and rapidly developed cancer treatments to patients, ultimately solidifying AI as an indispensable pillar of biomedical research.
References
- 1. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 2. Artificial Intelligence-Driven Innovations in Oncology Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12232943/]
- 3. Drug resistance in cancer: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623568/]
- 4. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 5. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 6. Transforming Cancer Therapy: Insights from 2025 H1 FDA ... [https://blog.crownbio.com/transforming-cancer-therapy-insights-from-2025-h1-fda-approvals-and-preclinical-drug-discovery]
- 7. Reimagining Oncology Preclinical Science | Eureka blog [https://www.criver.com/eureka/reimagining-oncology-preclinical-science-0]
- 8. End to end drug discovery: Revolutionizing 2025 [https://lifebit.ai/blog/end-to-end-drug-discovery/]
- 9. Integrating artificial intelligence in drug discovery and early ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00758-2]
- 10. How AI and multiomics are accelerating drug discovery [https://www.ddw-online.com/how-ai-and-multiomics-are-accelerating-drug-discovery-38345-202510/]
- 11. The future of pharmaceuticals: Artificial intelligence in drug ... [https://www.sciencedirect.com/science/article/pii/S2095177925000656]
- 12. How Machine Learning is Recoding the Future of Drug ... [https://www.drugpatentwatch.com/blog/the-application-of-machine-learning-in-drug-discovery-revolutionizing-pharmaceutical-research/?srsltid=AfmBOoqSyP3p9eQ-qgO1gYNtH2av9nntp_YFMDG5GWZj1iCo8U9VLNFm]
- 13. Exploring Artificial Intelligence's Potential to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582507/]
- 14. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 15. Natural Language Processing in Clinical Research Recruitment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476210/]
- 16. Biomedical Natural Language Processing Workshop (2025) [https://aclanthology.org/events/bionlp-2025/]
- 17. Strategies for the drug development of cancer therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518319/]
- 18. De novo drug design through artificial intelligence [https://www.frontiersin.org/journals/hematology/articles/10.3389/frhem.2024.1305741/full]
- 19. Unlocking Chemical Space Through De Novo Design [https://www.digitalchemistry.ai/resources/white-papers/unlocking-chemical-space-through-de-novo-design/]
- 20. How AI is Transforming Early Drug Discovery [https://globalforum.diaglobal.org/issue/august-2025/how-ai-is-transforming-early-drug-discovery/]
- 21. Optimizing drug design by merging generative AI with a ... [https://www.nature.com/articles/s42004-025-01635-7]
- 22. Molecular representation learning: cross-domain foundations ... [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d5dd00170f]
- 23. Molecular representations in AI-driven drug discovery [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-020-00460-5]
- 24. Language models can learn complex molecular distributions [https://pmc.ncbi.nlm.nih.gov/articles/PMC9174447/]
- 25. Comparing SMILES and SELFIES tokenization for ... [https://www.nature.com/articles/s41598-024-76440-8]
- 26. DeLA-DrugSelf: Empowering multi-objective de novo ... [https://www.sciencedirect.com/science/article/pii/S0010482524005705]
- 27. SELFIES and the future of molecular string representations [https://www.sciencedirect.com/science/article/pii/S2666389922002069]
- 28. Multi-View Mixture-of-Experts for predicting molecular ... [https://research.ibm.com/publications/multi-view-mixture-of-experts-for-predicting-molecular-properties-using-smiles-selfies-and-graph-based-representations--1]
- 29. Crossover operators for molecular graphs with an application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12175394/]
- 30. Prospective de novo drug design with deep interactome ... [https://www.nature.com/articles/s41467-024-47613-w]
- 31. Reinventing Drug Discovery with AI De Novo Design [https://ai.creative-biolabs.com/blog/reinventing-drug-discovery-ai-de-novo-design/]
- 32. PCF-VAE: posterior collapse free variational autoencoder ... [https://www.nature.com/articles/s41598-025-14285-5]
- 33. Multi-objective drug design with a scaffold-aware variational ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d4sc08736d]
- 34. A generative framework for enhancing drug target ... [https://www.nature.com/articles/s41598-025-01589-9]
- 35. Recent advances and application of generative adversarial ... [https://www.sciencedirect.com/science/article/pii/S2667318522000150]
- 36. Recent Advances in Automated Structure-Based De Novo ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10966644/]
- 37. Prospective de drug novo with deep... | Nature Communications design [https://www.nature.com/articles/s41467-024-47613-w?error=cookies_not_supported&code=864d9d6e-dd0c-44b7-aef6-a2f051c4ac02]
- 38. A structure-based framework for selective inhibitor design ... [https://www.nature.com/articles/s42003-025-07840-3]
- 39. Atomically accurate de novo design of antibodies with ... [https://www.nature.com/articles/s41586-025-09721-5]
- 40. of Inhibitors of DNA Methyltransferase 1: A Critical... De Novo Design [https://pmc.ncbi.nlm.nih.gov/articles/PMC11274800/]
- 41. Medicinal chemistry perspectives on anticancer drug design ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra05472a]
- 42. Key oncology trends to watch in 2025 [https://www.labiotech.eu/in-depth/oncology-trends-2025/]
- 43. A fragment-based De novo drug designing guided virtual ... [https://pubmed.ncbi.nlm.nih.gov/41187366/]
- 44. De novo design of mIDH1 inhibitors by integrating deep ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1491699/full]
- 45. Fragment-Based Drug Discovery | April 15-16, 2025 [https://www.drugdiscoverychemistry.com/25/fragment-based-drug-discovery]
- 46. ASCO 2025 Insights: Oncology Clinical Trends You Need ... [https://tfscro.com/resources/asco-2025-recap-oncology-clinical-trial-trends-cros-and-sponsors-need-to-know/]
- 47. Fragment-Based Lead Discovery Conference [https://wuxibiology.com/fragment-based-lead-discovery-conference-2/]
- 48. Advances in De Novo Drug Design: From Conventional to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7915729/]
- 49. Artificial intelligence in drug discovery and development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7577280/]
- 50. Recursion's Drug Discovery Pipeline [https://www.recursion.com/pipeline]
- 51. As Pipeline Advances, Recursion Expands AI Focus to ... [https://www.genengnews.com/topics/artificial-intelligence/as-pipeline-advances-recursion-expands-ai-focus-to-clinical-trials/]
- 52. Lysine-specific demethylase 1 controls key OSCC ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/40246812/]
- 53. Lysine-specific demethylase 1 controls key OSCC ... [https://www.nature.com/articles/s41368-025-00363-x]
- 54. Designed by AI: the future of antibody drugs [https://pharmaceutical-journal.com/article/feature/designed-by-ai-the-future-of-antibody-drugs]
- 55. Artificial intelligence-driven computational methods for ... [https://pubmed.ncbi.nlm.nih.gov/40677216/]
- 56. Making sense of AI: bias, trust and transparency in pharma ... [https://www.drugtargetreview.com/article/183358/making-sense-of-ai-bias-trust-and-transparency-in-pharma-rd/]
- 57. Probing the links between in vitro potency, ADMET and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6317702/]
- 58. Why optimize cancer drugs for ADMET? [https://www.sciencedirect.com/science/article/abs/pii/S1740677305000720]
- 59. Prediction of ADMET Properties of Anti-Breast Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10005249/]
- 60. Benchmarking ML in ADMET predictions: the practical impact ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-01041-0]
- 61. In Search of Beautiful Molecules: A Perspective on Generative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12458704/]
- 62. Leveraging machine learning models in evaluating ADMET ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12205928/]
- 63. Advancing cancer care through artificial intelligence [https://link.springer.com/article/10.1007/s44272-025-00052-0]
- 64. Artificial intelligence in cancer: applications, challenges, and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02450-3]
- 65. De Novo Molecular Design Enabled by Direct Preference ... [https://arxiv.org/html/2504.01389v1]
- 66. GuacaMol Benchmark for Molecular Design [https://www.emergentmind.com/topics/guacamol-benchmark]
- 67. Molecular Sets (MOSES): A Benchmarking Platform for ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.565644/full]
- 68. Chemical language modeling with structured state space ... [https://www.nature.com/articles/s41467-024-50469-9]
- 69. MolScore: a scoring, evaluation and benchmarking framework ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-024-00861-w]
- 70. Automated Intelligent Platforms for High‐Throughput ... [https://www.sciencedirect.com/science/article/pii/S2949747724000150]
- 71. The AI revolution: how multimodal intelligence will reshape ... [https://www.nature.com/articles/s44387-025-00044-4]
- 72. How AI Is Transforming Clinical Trials | AHA [https://www.aha.org/aha-center-health-innovation-market-scan/2025-10-21-how-ai-transforming-clinical-trials]
- 73. Insilico Medicine: Main [https://insilico.com/]
- 74. 14 Biotechs Utilizing AI-based Research Platforms [https://www.biopharmatrend.com/artificial-intelligence/recent-ipos-among-ai-driven-platforms-for-drug-discovery-and-biotech-601/]
- 75. Insilico and Lilly enter a research and licensing ... [https://insilico.com/tpost/e9xm9y0if1-insilico-and-lilly-enter-a-research-and]
- 76. BenevolentAI | AI Drug Discovery | AI Pharma [https://www.benevolent.com/]
- 77. Advancing Oncology Drug Development with Precision ... [https://www.benevolent.com/news-and-media/blog-and-videos/advancing-oncology-drug-development-precision-medicine/]
- 78. Recursion Reports Third Quarter 2025 Financial Results ... [https://ir.recursion.com/news-releases/news-release-details/recursion-reports-third-quarter-2025-financial-results-and]
- 79. The Drug Development Timeline: Why It Takes Over 10 Years [https://intuitionlabs.ai/articles/drug-development-timeline-explained]
- 80. Dynamic clinical trial success rates for drugs in the 21st ... [https://www.nature.com/articles/s41467-025-64552-2]
- 81. How Machine Learning is Recoding the Future of Drug ... [https://www.drugpatentwatch.com/blog/the-application-of-machine-learning-in-drug-discovery-revolutionizing-pharmaceutical-research/?srsltid=AfmBOorx_fcqpfU8vGe71ouK5J4yE-wYeIVAPM_fZ29GhsRfMu54Syh7]
- 82. Advancing oncology drug development: Innovative ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X25002094]
- 83. High throughput screening in modern drug discovery [https://www.drugdiscoverynews.com/high-throughput-screening-in-modern-drug-discovery-16695]
- 84. Quantitative high-throughput screening data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4375054/]
- 85. How to use in vitro models to study and overcome drug ... [https://blog.crownbio.com/how-to-use-in-vitro-models-to-study-and-overcome-drug-resistance-in-oncology]
- 86. In Vivo Pharmacology Models for Cancer Target Research [https://pubmed.ncbi.nlm.nih.gov/30912023/]
- 87. In Vivo Pharmacology | Experimental Therapeutics [https://www.bccrc.ca/dept/et/services/investigational-drug-program/vivo-pharmacology]
- 88. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 89. Regulating the Use of AI in Drug Development: Legal ... [https://www.fdli.org/2025/07/regulating-the-use-of-ai-in-drug-development-legal-challenges-and-compliance-strategies/]
- 90. AI Drug Development: FDA Releases Draft Guidance [https://www.foley.com/insights/publications/2025/01/ai-drug-development-fda-releases-draft-guidance/]
- 91. Exploring the ethical issues posed by AI and big data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581208/]