Cross-Validation in Cancer QSAR: Mastering LOO, LMO, and Advanced Validation for Predictive Drug Discovery Models
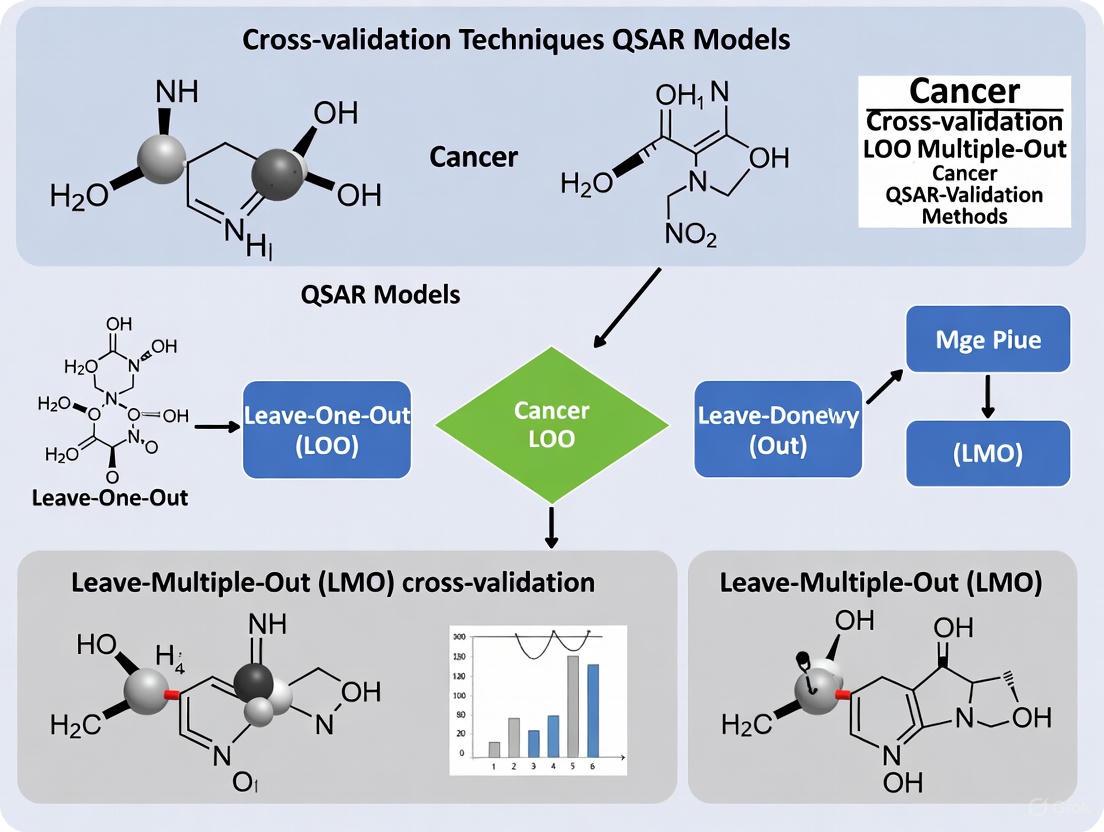
This article provides a comprehensive guide to cross-validation techniques for Quantitative Structure-Activity Relationship (QSAR) models in cancer research.
Cross-Validation in Cancer QSAR: Mastering LOO, LMO, and Advanced Validation for Predictive Drug Discovery Models
Abstract
This article provides a comprehensive guide to cross-validation techniques for Quantitative Structure-Activity Relationship (QSAR) models in cancer research. Tailored for researchers, scientists, and drug development professionals, it covers foundational principles of Leave-One-Out (LOO) and Leave-Many-Out (LMO) validation, their practical implementation in anti-cancer model development, common pitfalls and optimization strategies, and advanced validation frameworks including double cross-validation and external validation. By synthesizing current methodologies and addressing critical challenges like model selection bias, this resource aims to enhance the reliability and predictive power of QSAR models in the discovery of novel oncology therapeutics.
Understanding QSAR and Cross-Validation Fundamentals in Cancer Research
The Role of QSAR in Modern Anti-Cancer Drug Discovery
Quantitative Structure-Activity Relationship (QSAR) modeling represents a cornerstone of modern computational drug discovery, establishing statistically significant correlations between chemical structures and biological activities to predict compound behavior. In anti-cancer drug development, QSAR methodologies have evolved from traditional linear regression models to sophisticated machine learning (ML) and artificial intelligence (AI) approaches capable of navigating complex chemical spaces to identify novel therapeutic candidates [1]. These models serve as powerful virtual screening tools that accelerate the identification of potential cancer therapeutics by prioritizing compounds with the highest likelihood of efficacy, thereby reducing reliance on costly and time-consuming experimental screening [2].
The predictive power of QSAR models in oncology hinges on rigorous validation techniques, particularly cross-validation procedures that ensure model robustness and reliability. As chemical databases expand exponentially, with modern libraries containing billions of compounds, proper validation becomes increasingly critical for distinguishing true therapeutic potential from false hits [3]. This review examines current QSAR methodologies, their validation frameworks, and practical applications in cancer drug discovery, with a specific focus on how cross-validation techniques enhance predictive accuracy in identifying novel oncology therapeutics.
Foundational QSAR Methodologies and Validation Frameworks
Molecular Descriptors and Model Architectures
QSAR models utilize quantitative descriptors to capture key aspects of molecular structure that influence biological activity. These descriptors span multiple dimensions of complexity:
- 1D descriptors: Elemental composition and molecular weight
- 2D descriptors: Structural fingerprints and topological indices derived from molecular graphs
- 3D descriptors: Geometrical and surface properties
- 4D descriptors: Incorporation of molecular dynamics and conformational ensembles [4]
In anti-cancer drug discovery, 2D descriptors have proven particularly valuable for large datasets with significant chemical diversity, as they eliminate conformational uncertainty while providing sufficient structural information for meaningful activity predictions [4]. Machine learning algorithms commonly employed in modern QSAR development include support vector machines (SVM), random forests (RF), gradient boosting, and deep neural networks (DNN), each offering distinct advantages for specific dataset characteristics and prediction tasks [4] [5].
Critical Validation Paradigms: From LOO to Nested Cross-Validation
Robust validation is essential for generating reliable QSAR models, with cross-validation techniques serving as the gold standard for assessing predictive performance:
- Leave-One-Out (LOO) Cross-Validation: Iteratively removes one compound, builds the model on the remaining compounds, and predicts the omitted compound. This approach uses data efficiently but may produce higher variance in error estimates [6].
- Leave-Many-Out (LMO) Cross-Validation: Also known as k-fold cross-validation, this method removes a subset of compounds (typically 10-20%) during each iteration, offering a balance between bias and variance in error estimation [6].
- Nested (Double) Cross-Validation: Employs two layers of cross-validation, with an inner loop for model selection and parameter tuning and an outer loop for unbiased performance estimation. This approach provides the most reliable assessment of model performance on new data and effectively controls overfitting [4] [7].
Table 1: Comparison of Cross-Validation Techniques in QSAR Modeling
| Validation Method | Key Characteristics | Advantages | Limitations |
|---|---|---|---|
| Leave-One-Out (LOO) | Single compound omitted in each cycle | Maximizes training data usage | Can overestimate performance for small datasets |
| Leave-Many-Out (LMO) | Multiple compounds omitted in each cycle | More reliable error estimation | Requires larger datasets for stable results |
| Nested Cross-Validation | Separate loops for model selection & assessment | Unbiased performance estimation | Computationally intensive |
| Hold-Out Validation | Single split into training and test sets | Simple implementation | High variance based on split composition |
Traditional validation approaches have emphasized balanced accuracy as the primary performance metric. However, contemporary research demonstrates that for virtual screening of highly imbalanced chemical libraries (where inactive compounds vastly outnumber actives), positive predictive value (PPV) provides a more relevant metric for assessing model utility in early drug discovery [3]. Models with high PPV identify a greater proportion of true active compounds within the limited number of candidates that can be practically tested experimentally, making them particularly valuable for anti-cancer drug screening campaigns.
Experimental Protocols and Case Studies in Cancer Therapeutics
QSAR-Driven Discovery of PD-L1 Immune Checkpoint Inhibitors
Immunotherapy targeting the PD-1/PD-L1 axis has revolutionized cancer treatment, but existing therapeutics face limitations including high cost and drug resistance. A recent study applied multi-step structure-based virtual screening coupled with QSAR modeling to identify novel PD-L1 inhibitors from natural products [8].
Experimental Protocol:
- Receptor Preparation: The 3D crystal structure of human PD-L1 co-crystallized with a JQT inhibitor (PDB ID: 6R3K) was retrieved and prepared using protein preparation tools
- Library Curation: 32,552 natural compounds were obtained from the Natural Product Atlas database and prepared using LigPrep module
- Virtual Screening Workflow:
- Step 1: High-throughput virtual screening (HTVS) filtered compounds using ADME and drug-likeness criteria
- Step 2: Standard precision (SP) docking further refined candidate compounds
- Step 3: Extra precision (XP) screening identified top candidates
- Binding Affinity Assessment: Post-process binding free energy calculations using Molecular Mechanics Generalized Born Surface Area (MM/GBSA) method
- Validation: Explicit 100 ns molecular dynamics simulations assessed complex stability [8]
This workflow identified five natural compounds with substantial stability with PD-L1 through intermolecular interactions with essential residues. The calculated results indicated these natural compounds as putative potent PD-L1 inhibitors worthy of further development in cancer immunotherapy [8].
Nanoparticle QSAR Models for Tumor Delivery Optimization
Nanoparticles represent promising drug delivery systems in oncology, but achieving efficient tumor delivery remains challenging. Recent research has developed QSAR models to predict tissue distribution and tumor delivery efficiency of nanoparticles based on their physicochemical properties [5].
Experimental Protocol:
- Dataset Compilation: Data on nanoparticle physicochemical properties and in vivo distribution were obtained from the Nano-Tumor Database
- Model Development: Multiple ML algorithms were trained and validated:
- Linear regression
- Support vector machines
- Random forest
- Gradient boosting
- Deep neural networks (DNN)
- Model Validation: Rigorous cross-validation assessed prediction accuracy for delivery efficiency to tumors and major tissues
- Feature Importance Analysis: Identified core nanoparticle materials as critical determinants of distribution patterns [5]
The DNN model demonstrated superior performance, with determination coefficients (R²) for test datasets of 0.41, 0.42, 0.45, 0.79, 0.87, and 0.83 for delivery efficiency in tumor, heart, liver, spleen, lung, and kidney, respectively [5]. This model successfully identified multiple nanoparticle formulations with enhanced tumor delivery efficiency and was converted to a user-friendly web dashboard to support nanomedicine design.
Diagram 1: Nested Cross-Validation Workflow for QSAR Model Development. This diagram illustrates the double-layered validation approach that provides unbiased performance estimation.
Comparative Performance Analysis of QSAR Approaches
Validation Metrics and Model Performance
The predictive accuracy of QSAR models varies significantly based on the biological endpoint, descriptor types, and modeling algorithms employed. The following table summarizes performance metrics for recently published QSAR models with relevance to anti-cancer drug discovery.
Table 2: Performance Metrics of QSAR Models in Drug Discovery Applications
| Application Domain | Model Type | Dataset Size | Validation Method | Performance Metrics | Reference |
|---|---|---|---|---|---|
| HMG-CoA Reductase Inhibition | Multiple ML Algorithms | 300 models | Nested Cross-Validation | R² ≥ 0.70, CCC ≥ 0.85 | [4] |
| Nanoparticle Tumor Delivery | Deep Neural Network | Nano-Tumor Database | 5-Fold Cross-Validation | R² = 0.41 (tumor), 0.87 (lung) | [5] |
| Repeat Dose Toxicity Prediction | Random Forest | 3,592 chemicals | External Test Set | R² = 0.53, RMSE = 0.71 log10-mg/kg/day | [9] |
| 5-HT2B Receptor Binding | Binary Classification | 754 compounds | External Validation | 90% Experimental Hit Rate | [2] |
Impact of Data Set Characteristics on Model Performance
The size and composition of training datasets significantly influence QSAR model reliability. While traditional QSAR development often emphasized dataset balancing, contemporary research indicates that models trained on imbalanced datasets (reflecting the true distribution of active versus inactive compounds in chemical space) can achieve higher positive predictive value (PPV) – a critical metric for virtual screening applications [3]. In practical anti-cancer drug discovery, this translates to higher hit rates within the limited number of compounds that can be experimentally tested.
Comparative studies demonstrate that training on imbalanced datasets achieves hit rates at least 30% higher than using balanced datasets when screening ultra-large chemical libraries [3]. This paradigm shift acknowledges that modern virtual screening campaigns typically evaluate billions of compounds but can only experimentally validate a minute fraction (e.g., 128 compounds corresponding to a single 1536-well plate), making early enrichment of true actives more valuable than global classification accuracy.
Table 3: Key Research Reagents and Computational Tools for QSAR Modeling
| Resource Category | Specific Tools/Databases | Primary Function | Application in Anti-Cancer QSAR |
|---|---|---|---|
| Chemical Databases | ZINC15, ChEMBL, PubChem, Natural Product Atlas | Source of chemical structures and bioactivity data | Provides training data and virtual screening libraries [4] [8] |
| Descriptor Calculation | MOE, Dragon, PaDEL | Compute molecular descriptors and fingerprints | Generates quantitative features for model building [6] |
| Modeling Platforms | scikit-learn, WEKA, mlr3, Schrödinger | Machine learning algorithm implementation | Develops and validates QSAR models [4] |
| Validation Frameworks | Double Cross-Validation, Bootstrapping | Model performance assessment | Ensures model robustness and predictive capability [7] |
| Specialized Tools | ADMETLab 3.0, EPI Suite, VEGA | Predicts absorption, distribution, metabolism, excretion, toxicity | Assesses drug-like properties and safety profiles [10] |
Diagram 2: Integrated QSAR Workflow in Anti-Cancer Drug Discovery. This diagram shows the sequential process from data collection to experimental validation, with integrated ADMET assessment.
QSAR modeling continues to evolve as an indispensable tool in anti-cancer drug discovery, with advanced machine learning algorithms and rigorous validation frameworks enhancing predictive accuracy. The adoption of nested cross-validation techniques represents a significant advancement in model reliability, providing unbiased performance estimates that better reflect real-world screening utility. As chemical libraries expand into the billions of compounds, the emphasis on positive predictive value rather than balanced accuracy aligns model development with practical screening constraints, where only a minute fraction of predicted actives can undergo experimental validation.
Future directions in QSAR development for oncology applications will likely incorporate more sophisticated deep learning architectures, multi-task learning approaches that simultaneously model multiple cancer targets, and enhanced integration with structural biology information through hybrid structure-based and ligand-based methods. Furthermore, the growing availability of high-quality bioactivity data from public repositories will enable the development of increasingly accurate models capable of navigating the complex chemical space of potential anti-cancer therapeutics. As these computational approaches mature, their integration with experimental validation will continue to accelerate the discovery of novel cancer therapies while optimizing resource allocation in the drug development pipeline.
Quantitative Structure-Activity Relationship (QSAR) modeling is a fundamental computational approach in modern drug discovery, particularly in the development of anti-cancer agents. These models mathematically correlate the chemical structure of compounds with their biological activity, enabling the prediction of new therapeutic candidates against targets like breast cancer cell lines, tubulin, and dihydrofolate reductase [11] [12] [13]. The core assumption of QSAR is that structurally similar molecules exhibit similar biological properties, a principle that underpins the use of molecular descriptors to quantify chemical features and predict bioactivity [14] [13].
The predictive performance and reliability of any QSAR model are critically dependent on rigorous validation techniques. Without proper validation, models risk being overfitted to their training data, rendering them useless for predicting new, unseen compounds. Cross-validation stands as the primary statistical method for internally validating QSAR models and estimating their predictive capability. It operates by repeatedly partitioning the available dataset into training and validation subsets to simulate how the model will perform on external data [7]. Among cross-validation methods, Leave-One-Out (LOO) and Leave-Many-Out (LMO) are two pivotal approaches with distinct characteristics, advantages, and limitations. Their strategic application is essential for developing robust QSAR models in cancer research, where accurate prediction of compound activity can significantly accelerate the identification of novel therapeutics [15] [11] [12].
Theoretical Foundations of LOO and LMO
Leave-One-Out (LOO) Cross-Validation
Leave-One-Out cross-validation is an exhaustive method where each compound in the dataset takes a turn being the sole test subject. For a dataset containing N compounds, LOO involves N separate learning experiments. In each iteration, N-1 compounds are used to train the model, and the single remaining compound is used to test its predictive accuracy. The process repeats until every molecule has been the test object once, and the overall predictive performance is summarized by averaging the results from all N iterations [7]. The primary advantage of LOO is its efficient use of data; since each training set contains nearly all available compounds, the model is built on a near-complete representation of the chemical space. This characteristic makes LOO particularly valuable when working with small datasets, a common scenario in early-stage anticancer drug discovery where synthesizing and testing numerous compounds is costly and time-consuming [11]. However, LOO is computationally intensive for large datasets and can yield high-variance error estimates because each test set consists of only one compound, potentially making the results sensitive to small changes in the data.
Leave-Many-Out (LMO) Cross-Validation
Leave-Many-Out cross-validation, also known as k-fold cross-validation, takes a different approach by partitioning the dataset into k subsets (folds) of approximately equal size. Typically, k values of 5 or 10 are used, though this can vary based on dataset size and characteristics. In each iteration, k-1 folds are combined to form the training set, while the remaining single fold serves as the test set. This process repeats k times, with each fold getting exactly one turn as the test set. The final predictive performance metric is the average across all k iterations [7]. LMO's strength lies in its ability to provide a more stable and reliable estimate of prediction error, particularly for larger datasets. By testing the model on multiple compounds simultaneously, it better represents how the model will perform when faced with entirely new sets of compounds. Additionally, LMO is less computationally demanding than LOO for larger datasets. The main disadvantage of LMO is that each training set contains substantially fewer samples than the full dataset (e.g., 80-90% for k=5 or k=10), which might lead to models that don't fully capture the underlying chemical space, especially when the total number of available compounds is limited.
Table 1: Core Characteristics of LOO and LMO Cross-Validation
| Feature | Leave-One-Out (LOO) | Leave-Many-Out (LMO) |
|---|---|---|
| Basic Principle | Iteratively removes one compound as test set, uses all others for training | Partitions data into k folds; uses k-1 folds for training, one fold for testing |
| Number of Iterations | Equal to number of compounds (N) | Typically 5 or 10 (user-defined) |
| Training Set Size | N-1 compounds | Approximately (k-1)/k * N compounds |
| Test Set Size | 1 compound | Approximately N/k compounds |
| Computational Demand | High for large N | Lower than LOO for large N |
| Variance of Error Estimate | Higher | Lower |
| Preferred Context | Small datasets | Medium to large datasets |
Comparative Analysis in Cancer QSAR Research
The choice between LOO and LMO cross-validation significantly impacts the validation outcomes of QSAR models designed for anticancer activity prediction. A review of recent literature reveals how both methods are applied in practice and highlights their performance characteristics across different research contexts.
In breast cancer research, a QSAR study on pyrimidine-coumarin-triazole conjugates against MCF-7 cell lines utilized LOO cross-validation, reporting a high Q²LOO value of 0.9495, indicating strong predictive capability [11]. Similarly, research on 1,2,4-triazine-3(2H)-one derivatives as tubulin inhibitors for breast cancer therapy relied on LOO validation to confirm model robustness [12]. These applications demonstrate LOO's prevalence in studies with limited compound libraries, where maximizing training data is crucial.
For leukemia research, a QSAR study on 112 anticancer compounds tested against MOLT-4 and P388 leukemia cell lines implemented both LOO and external validation. The models achieved high Q²LOO values (0.881 and 0.856, respectively) alongside respectable external prediction accuracy (R²pred = 0.635 and 0.670) [15]. This dual-validation approach provides a more comprehensive assessment of model performance, with LOO offering internal consistency and external validation testing true generalizability.
The critical importance of proper validation parameterization was highlighted in a systematic study on double cross-validation, which emphasized that the parameters for the inner loop of double cross-validation mainly influence bias and variance of the resulting models [7]. This finding underscores why the choice between LOO and LMO directly impacts the reliability of the validated QSAR model, especially under model uncertainty when the optimal QSAR model isn't known a priori.
Table 2: Application of LOO and LMO in Published Cancer QSAR Studies
| Study Focus | Dataset Size | Validation Method | Reported Metric | Performance |
|---|---|---|---|---|
| Anti-breast cancer agents (MCF-7) [11] | 28 compounds | LOO | Q²LOO | 0.9495 |
| Anti-leukemia agents (MOLT-4) [15] | 112 compounds | LOO | Q²LOO | 0.881 |
| Anti-leukemia agents (P388) [15] | 112 compounds | LOO | Q²LOO | 0.856 |
| Tubulin inhibitors [12] | 32 compounds | LOO | Q²LOO | Not specified |
| c-Met inhibitors [16] | 48 compounds | LOO | Q²LOO | Not specified |
Experimental Protocols and Best Practices
Standard Implementation Protocol
Implementing proper cross-validation requires a systematic approach to ensure reliable and reproducible results. The following protocol outlines the key steps for both LOO and LMO cross-validation in cancer QSAR studies:
Dataset Preparation: Begin with a curated dataset of compounds with experimentally determined biological activities (e.g., IC₅₀ or pIC₅₀ values). For anticancer QSAR studies, this typically involves 20-100 compounds, depending on synthetic and testing capacity [11] [12] [16]. Ensure structural diversity within the dataset to adequately represent the chemical space under investigation.
Descriptor Calculation and Preprocessing: Compute molecular descriptors using appropriate software such as PaDEL, DRAGON, or quantum chemical calculations with Gaussian [15] [12] [17]. Reduce descriptor dimensionality using methods like Principal Component Analysis (PCA) or variable selection techniques to avoid overfitting [13].
Data Splitting:
- For LOO: No explicit splitting is needed as the algorithm automatically creates N partitions where each partition has one test compound and N-1 training compounds.
- For LMO: Randomly partition the dataset into k folds of approximately equal size, ensuring each fold represents the overall distribution of activity values. Stratified sampling is recommended to maintain similar activity distributions across folds.
Model Training and Validation:
- For each iteration, train the QSAR model (e.g., MLR, PLS, Random Forest) on the training set.
- Predict the activity of compounds in the validation set.
- Record the prediction error metrics (e.g., MSE, RMSE, R²) for each iteration.
Performance Assessment: Calculate the average performance metrics across all iterations. The most commonly reported metric is Q² (cross-validated R²), which indicates the model's predictive capability [15] [11].
External Validation (Recommended): For a more rigorous assessment, further validate the model using a completely external test set that wasn't involved in any cross-validation process [15] [7].
Workflow Diagram
The following diagram illustrates the comparative workflows for LOO and LMO cross-validation in the context of QSAR model development:
Cross-Validation Workflow: LOO vs. LMO
Decision Framework and Best Practices
Selecting the appropriate cross-validation method requires consideration of multiple factors. The following decision framework incorporates established best practices from the literature:
Dataset Size Considerations: Use LOO for small datasets (N < 50) commonly encountered in preliminary anticancer studies, as it maximizes training data usage. For medium to large datasets (N > 100), prefer LMO (typically 5-fold or 10-fold) for more stable error estimates and reduced computation time [15] [11] [7].
Model Stability Assessment: Implement multiple runs of LMO with different random seeds to assess model stability, as the specific partitioning can influence results. For LOO, this isn't necessary as the partitions are deterministic.
Comprehensive Validation Strategy: Employ double cross-validation (nested cross-validation) when performing both model selection and model assessment to obtain unbiased error estimates [7]. Always supplement internal cross-validation with external validation on a completely hold-out test set when data permits [15].
Reporting Standards: Clearly specify the cross-validation method (LOO or LMO with k value) and report all relevant metrics (Q², RMSE, etc.) in publications. For LMO, indicate the number of folds and whether the partitioning was stratified.
Applicability Domain Integration: Combine cross-validation with applicability domain assessment to identify when predictions for new compounds fall outside the model's reliable prediction space [15] [16].
Table 3: Essential Computational Tools for QSAR Cross-Validation
| Tool/Resource | Type | Primary Function in QSAR/CV | Application Example |
|---|---|---|---|
| QSARINS [11] [17] | Software | QSAR model development with comprehensive cross-validation features | 2D-QSAR analysis of pyrimidine-coumarin-triazole conjugates |
| PaDEL-Descriptor [15] | Software | Calculation of molecular descriptors for QSAR modeling | Descriptor calculation for anti-leukemia QSAR models |
| Gaussian 09/16 [12] [16] | Software | Quantum chemical calculations for electronic structure descriptors | Computing HOMO/LUMO energies for tubulin inhibitor models |
| R/Python with scikit-learn [17] [7] | Programming Libraries | Implementing custom cross-validation and machine learning algorithms | Building double cross-validation workflows for model uncertainty assessment |
| DRAGON [14] | Software | Calculation of a wide range of molecular descriptors (>3,300) | Molecular descriptor calculation for predictive toxicology models |
Leave-One-Out and Leave-Many-Out cross-validation represent two fundamental approaches with complementary strengths in validating QSAR models for cancer research. LOO's exhaustive nature makes it particularly valuable for small datasets typical in early-stage anticancer drug discovery, where maximizing training data is paramount. In contrast, LMO provides more stable error estimates for larger compound libraries and is computationally more efficient. The choice between these methods should be guided by dataset size, computational resources, and the required stability of the error estimate. As QSAR methodology continues to evolve with integration of artificial intelligence and multi-omics data [14] [17], proper cross-validation remains the bedrock of developing reliable models that can genuinely accelerate the discovery of novel anticancer therapeutics. A thoughtful validation strategy, potentially incorporating both LOO and LMO in a double cross-validation framework, provides the rigorous assessment necessary to advance promising compounds from in silico predictions to experimental validation.
In the field of oncology drug discovery, Quantitative Structure-Activity Relationship (QSAR) models are indispensable computational tools that connect chemical structures to biological activity, dramatically accelerating the identification of potential therapeutic compounds [13]. However, the predictive power and real-world utility of these models are entirely dependent on the rigor of their validation. Without proper validation, models may suffer from overfitting and model selection bias, producing deceptively optimistic results that fail to generalize to new compounds [18]. This guide examines the critical validation methodologies that ensure oncology QSAR models generate reliable, clinically-relevant predictions for researchers, scientists, and drug development professionals.
Key Validation Concepts and Their Importance
The Fundamental Distinction: Internal vs. External Validation
Robust QSAR modeling requires both internal and external validation approaches, each serving distinct purposes in establishing model reliability:
Internal Validation assesses model stability using only the training data, typically through techniques like Leave-One-Out (LOO) and Leave-Many-Out (LMO) cross-validation [19]. These methods evaluate how well the model performs on different subsets of the training data, providing initial indicators of potential overfitting.
External Validation represents the gold standard for evaluating predictive power, where the model is tested on completely independent compounds that were not involved in model building or selection [18] [19]. This approach provides the most realistic estimate of how the model will perform in actual drug discovery applications when predicting activities of novel compounds.
The Perils of Inadequate Validation: Model Selection Bias and Overfitting
When validation is insufficient, several critical pitfalls can compromise model utility:
Model Selection Bias occurs when the same data is used for both model selection and validation, causing overly optimistic performance estimates [18]. This bias arises because suboptimal models may appear superior by chance when their errors are underestimated on specific data splits.
Overfitting happens when models become excessively complex, adapting to noise in the training data rather than capturing the underlying structure-activity relationship [18]. Such models demonstrate excellent performance on training compounds but fail dramatically when applied to new chemical entities.
Cross-Validation Techniques: Methodologies and Protocols
Core Cross-Validation Protocols
Table 1: Comparison of Key Cross-Validation Techniques in Oncology QSAR
| Technique | Key Methodology | Primary Application | Advantages | Limitations |
|---|---|---|---|---|
| Leave-One-Out (LOO) | Iteratively removes one compound, builds model on remaining n-1 compounds, and predicts the omitted compound [19] | Internal validation for small datasets | Maximizes training data usage; Low computational cost for small n | High variance in error estimate; Can overestimate predictive ability |
| Leave-Many-Out (LMO) | Removes a subset of compounds (typically 20-30%) repeatedly, building models on reduced training sets [19] | Internal validation for datasets of various sizes | More reliable error estimate than LOO; Better assessment of model stability | Requires larger datasets; Higher computational cost |
| Double (Nested) Cross-Validation | Features external loop for model assessment and internal loop for model selection [18] | Both model selection and error estimation for final assessment | Provides nearly unbiased performance estimates; Uses data efficiently | Complex implementation; Computationally intensive |
Advanced Validation: Double Cross-Validation Methodology
For the most reliable validation, double cross-validation (also called nested cross-validation) offers a sophisticated approach that addresses model selection bias:
Workflow Overview:
Experimental Protocol:
- Outer Loop Configuration: Partition the entire dataset into k-folds (typically 5-10), reserving one fold as the test set and remaining folds as the training set [18]
- Inner Loop Execution: On the training set, perform additional cross-validation to optimize model parameters and select the best-performing configuration [18]
- Model Assessment: Apply the selected model to the held-out test set from the outer loop to obtain unbiased performance estimates [18]
- Iteration and Averaging: Repeat the process across all outer loop partitions and average the results for stable performance metrics [18]
Compared to single validation approaches, double cross-validation provides more realistic performance estimates and should be preferred over single test set validation [18].
Quantitative Validation Metrics and Benchmarking
Essential Statistical Parameters for QSAR Validation
Table 2: Key Validation Metrics and Their Interpretation in Oncology QSAR
| Validation Metric | Acceptance Threshold | Interpretation | Example from Literature |
|---|---|---|---|
| R² (Coefficient of Determination) | > 0.6 [20] | Goodness of fit for training set | QSAR model for photodynamic therapy showed R² = 0.87 [20] |
| Q² (LOO Cross-Validated R²) | > 0.5 [20] | Internal predictive ability | Photodynamic therapy model achieved Q² = 0.71 [20] |
| R²pred (External Validation R²) | > 0.5 [20] [21] | True predictive power for new compounds | CoMSIA model for breast cancer inhibitors showed strong external prediction [21] |
| RMSE (Root Mean Square Error) | Lower values preferred | Average prediction error | Used in 3D-QSAR studies of thioquinazolinone derivatives [21] |
Performance Benchmarks from Oncology QSAR Studies
Recent studies demonstrate how proper validation separates reliable from unreliable models:
- Photodynamic Therapy Application: A porphyrin-based QSAR model achieved excellent internal validation (R² = 0.87, Q² = 0.71) and respectable external predictive ability (R²pred = 0.52) [20]
- Anti-Breast Cancer Models: A CoMSIA model for thioquinazolinone derivatives exhibited significant external prediction performance, confirming the value of rigorous validation [21]
- Multi-Model Analysis: Examination of 44 published QSAR models revealed that relying solely on R² cannot adequately indicate model validity, emphasizing the need for multiple validation metrics [19]
Table 3: Research Reagent Solutions for QSAR Validation
| Tool/Resource | Type | Primary Function | Application in Validation |
|---|---|---|---|
| DRAGON Software [22] | Descriptor Calculation | Computes molecular descriptors (0D-2D) | Generates structural parameters for model building and validation |
| QSARINS [22] | Modeling Software | Develops MLR models with validation features | Facilitates variable selection and model validation processes |
| Cross-Validation Algorithms [18] | Statistical Method | Data splitting and resampling | Implements LOO, LMO, and double cross-validation protocols |
| Statistical Metrics Package [19] | Validation Metrics | Calculates R², Q², R²pred, etc. | Quantifies model performance and predictive power |
Implementation Guidelines and Best Practices
Recommended Validation Workflow
For comprehensive QSAR validation in oncology applications, researchers should implement this integrated approach:
Data Preparation Phase:
- Curate high-quality, diverse compound sets with reliable activity measurements
- Apply appropriate division algorithms to create representative training and test sets
Internal Validation Stage:
- Implement LOO cross-validation for initial assessment of model stability
- Conduct LMO cross-validation with multiple data splits (e.g., 5-fold, 10-fold)
- Calculate Q² and internal performance metrics
External Validation Stage:
- Completely hold out the test set during model building and parameter optimization
- Evaluate the final model on the external test set to calculate R²pred
- Assess predictive performance using multiple statistical measures
Advanced Validation (When Feasible):
- Implement double cross-validation to obtain nearly unbiased error estimates
- Compare performance across different validation approaches
- Conduct applicability domain analysis to define model boundaries
Interpretation of Validation Results
Proper interpretation of validation outcomes is crucial for model acceptance:
- Models meeting all thresholds (R² > 0.6, Q² > 0.5, R²pred > 0.5) can be considered predictively reliable for the defined chemical space [20]
- Models with strong internal but weak external validation likely suffer from overfitting and require simplification or better applicability domain definition [18]
- Consistently poor performance across validation methods indicates fundamental issues with descriptor selection or the underlying structure-activity hypothesis
Robust validation is not merely a statistical formality but the fundamental determinant of real-world predictive power in oncology QSAR models. Through the systematic application of cross-validation techniques, particularly LOO, LMO, and double cross-validation, researchers can develop models that genuinely accelerate oncology drug discovery rather than producing misleading results. The integration of both internal and external validation, coupled with appropriate performance metrics, provides the comprehensive assessment needed to translate computational predictions into successful experimental candidates. As QSAR methodologies continue to evolve, maintaining rigorous validation standards will remain essential for building trust in computational approaches and ultimately developing more effective cancer therapeutics.
Common Molecular Descriptors and Datasets in Cancer QSAR Studies
Quantitative Structure-Activity Relationship (QSAR) modeling represents a cornerstone of modern computational drug discovery, enabling researchers to predict the biological activity and physicochemical properties of compounds based on their molecular structures. In oncology research, QSAR models provide an invaluable tool for prioritizing synthetic efforts, understanding structure-activity relationships, and identifying potential anticancer agents with desired efficacy profiles. These computational approaches have gained significant importance in recent years due to their ability to reduce reliance on animal testing through New Approach Methodologies (NAMs), offering faster, less expensive alternatives for early-stage drug screening while maintaining ethical standards [23].
The predictive power of QSAR models hinges on two fundamental components: molecular descriptors that numerically represent structural features, and robust datasets containing reliable bioactivity measurements. Molecular descriptors quantify diverse aspects of molecular structure, from simple atomic properties to complex quantum chemical calculations, while datasets provide the experimental foundation upon which models are built and validated. Understanding the interplay between these components, particularly within the context of proper validation techniques like Leave-One-Out (LOO) and Leave-Many-Out (LMO) cross-validation, is essential for developing reliable predictive models in cancer drug discovery [7].
Common Molecular Descriptors in Cancer QSAR Studies
Molecular descriptors serve as the mathematical representation of molecular structures and properties, forming the independent variables in QSAR models. The selection of appropriate descriptors is critical for model interpretability and predictive performance, with different descriptor classes offering distinct advantages for specific applications in cancer research.
Quantum Chemical Descriptors
Quantum chemical descriptors derived from computational chemistry methods provide insights into electronic structure and reactivity properties that influence biological activity. Studies on anti-colorectal cancer agents have identified several significant quantum chemical descriptors, including total electronic energy (E~T~), charge of the most positive atom (Q~max~), and electrophilicity (ω) [24]. These descriptors validate the importance of electronic properties in modeling anti-cancer activity and can be obtained through gaseous-state Gaussian optimization at HF/3-21G level in a vacuum, providing robust yet computationally accessible parameters for QSAR modeling.
Two-Dimensional (2D) Descriptors
Two-dimensional descriptors remain widely used due to their computational efficiency and clear structural interpretability. Research on triple-negative breast cancer (TNBC) inhibitors has identified several key 2D descriptors that correlate with cytotoxicity against MDA-MB231 cells, including electronegativity (Epsilon-3), carbon atoms separated through five bond distances (TCC_5), electrotopological state indices of -CH~2~ groups (SssCH2count), z-coordinate dipole moment (Zcomp Dipole), and the distance between highest positive and negative electrostatic potential on van der Waals surface area [25]. These descriptors capture essential electronic, topological, and steric properties that influence compound binding and biological activity.
Topological Descriptors
Topological descriptors encode molecular connectivity patterns and have demonstrated significant utility in breast cancer QSAR studies. Recent research has explored novel entire neighborhood topological indices, which provide comprehensive characterization of atomic environments and bonding patterns [26]. These indices include first, second, and modified entire neighborhood indices, as well as newly developed entire neighborhood forgotten and modified entire neighborhood forgotten indices. Such descriptors have shown strong correlations with physicochemical properties of breast cancer drugs, enabling predictive modeling of their behavior.
SMILES-Based Descriptors
SMILES (Simplified Molecular Input Line Entry System) notation provides an alternative approach to molecular representation through string-based descriptors. Studies on anti-colon cancer chalcone analogues have demonstrated that hybrid optimal descriptors combining SMILES notation with hydrogen-suppressed molecular graphs (HSG) can achieve excellent predictive performance, with validation R² values reaching 0.90 [27]. The SMILES-based approach allows for efficient representation of complex molecular structures while maintaining interpretability through identified structural promoters.
Table 1: Common Molecular Descriptors in Cancer QSAR Studies
| Descriptor Category | Specific Examples | Cancer Type Applications | Key Insights |
|---|---|---|---|
| Quantum Chemical | Total electronic energy (E~T~), Most positive atomic charge (Q~max~), Electrophilicity (ω) | Colorectal cancer [24] | Describe electronic structure and reactivity; Computed at HF/3-21G level |
| 2D Descriptors | Electronegativity (Epsilon-3), TCC_5, SssCH2count, Zcomp Dipole | Triple-negative breast cancer [25] | Capture electronic, topological, and steric properties |
| Topological Indices | Entire neighborhood indices, Entire forgotten index, Modified entire neighborhood indices | Breast cancer [26] | Encode molecular connectivity and atomic environments |
| SMILES-Based | Hybrid optimal descriptors (SMILES + Graph) | Colon cancer [27] | String-based representations with high predictive power |
Datasets for Cancer QSAR Modeling
The development of robust QSAR models requires high-quality, well-curated datasets containing reliable bioactivity measurements. These datasets vary in size, composition, and source, with each offering distinct advantages and limitations for different cancer types and research objectives.
Colon Cancer Datasets
Colon cancer research has benefited from carefully constructed datasets focusing on specific compound classes. Studies on chalcone derivatives have utilized datasets of 193 compounds tested against HT-29 human colon adenocarcinoma cell lines, with activity measurements expressed as pIC~50~ values ranging from 3.58 to 7.00 [27]. These datasets are typically compiled from multiple published sources and standardized using rigorous curation protocols to ensure consistency in structural representation and activity measurements.
Breast Cancer Datasets
Breast cancer QSAR studies employ diverse datasets reflecting the heterogeneity of this disease. Research on triple-negative breast cancer has utilized datasets comprising 99 known MDA-MB-231 inhibitors sourced from the ChEMBL database and published literature [25]. These datasets focus specifically on the aggressive TNBC subtype and include structurally diverse chemical series, particularly terpene derivatives and analogs with measured IC~50~ values. Additionally, studies on breast cancer drugs more broadly have examined 16 established therapeutic agents, including Azacitidine, Cytarabine, Daunorubicin, Docetaxel, Doxorubicin, and Paclitaxel, focusing on their physicochemical properties [26].
Genotoxicity and Carcinogenicity Datasets
Beyond direct anticancer activity, QSAR models also address genotoxicity and carcinogenicity endpoints crucial for safety assessment. Research in this area has led to the development of consolidated micronucleus assay datasets, including 981 chemicals for in vitro micronucleus testing and 1,309 chemicals for in vivo mouse micronucleus assays [28]. These datasets are constructed through extensive literature mining using advanced natural language processing approaches, specifically the BioBERT large language model fine-tuned for biomedical text mining, followed by expert curation to ensure data quality and relevance.
Public Databases and Repositories
Several public databases serve as valuable resources for QSAR model development in cancer research. The ChEMBL database provides extensively curated bioactivity data, including drug-target interactions and inhibitory concentrations, with version 34 containing over 2.4 million compounds and 15,598 targets [29]. The DBAASP database offers specialized collections of anticancer peptides, while the EFSA Genotoxicity Pesticides Database provides curated information relevant to carcinogenicity assessment [23] [30]. These repositories enable researchers to access standardized, annotated bioactivity data for model building and validation.
Table 2: Representative Datasets in Cancer QSAR Research
| Cancer Type/Endpoint | Dataset Size | Activity Measure | Data Sources |
|---|---|---|---|
| Colon Cancer (Chalcones) | 193 compounds | pIC~50~ against HT-29 cells | Multiple published studies [27] |
| Triple-Negative Breast Cancer | 99 inhibitors | IC~50~ against MDA-MB-231 cells | ChEMBL database & literature [25] |
| Breast Cancer Drugs | 16 drugs | Physicochemical properties | Established therapeutics [26] |
| In Vitro Micronucleus | 981 chemicals | Binary (positive/negative) | PubMed, ISSMIC, EURL ECVAM [28] |
| In Vivo Micronucleus (Mouse) | 1,309 chemicals | Binary (positive/negative) | Multiple databases & literature [28] |
Experimental Protocols and Methodologies
QSAR Model Development Workflow
The development of validated QSAR models follows a systematic workflow encompassing data preparation, model building, validation, and application. The diagram below illustrates this process, highlighting critical steps for ensuring model reliability and predictive power.
Data Curation Protocols
Robust data curation is essential for developing reliable QSAR models. For micronucleus assay datasets, researchers implement comprehensive curation protocols including: standardization of chemical structures using tools like RDKit; removal of mixtures, polymers, and inorganic compounds; neutralization of salts to parent structures; and duplicate removal through InChiKeys comparison [28]. Additionally, experimental results are carefully reviewed for compliance with OECD test guidelines (e.g., OECD 487 for in vitro micronucleus, OECD 474 for in vivo micronucleus), with technically compromised studies excluded from final datasets.
Model Validation Techniques
Proper validation is crucial for assessing model predictive power and avoiding overoptimistic performance estimates. Double cross-validation (also called nested cross-validation) provides a robust framework for both model selection and assessment [7]. This approach consists of two nested loops: an inner loop for model selection and parameter optimization, and an outer loop for unbiased error estimation. The inner loop typically employs LOO or LMO cross-validation to select optimal model parameters, while the outer loop assesses the final model performance on independent test sets, effectively eliminating model selection bias that can occur with single-level validation approaches.
Performance Metrics
QSAR model quality is assessed using multiple statistical metrics, including: coefficient of determination (R²) for goodness of fit; cross-validated R² (Q²) for internal predictive ability; index of ideality correlation (IIC) for model robustness; and accuracy/sensitivity/specificity for classification models [27] [7] [25]. These metrics collectively provide a comprehensive picture of model performance, with acceptable QSAR models typically demonstrating Q² > 0.5 and R² > 0.6, though higher thresholds are preferred for reliable predictions.
Successful QSAR modeling in cancer research relies on a diverse toolkit of software, databases, and computational resources that facilitate data curation, descriptor calculation, model building, and validation.
Table 3: Essential Resources for Cancer QSAR Research
| Resource Category | Specific Tools | Primary Function | Application Examples |
|---|---|---|---|
| QSAR Software | CORAL, QSARINS, V-Life MDS | Model development & validation | Monte Carlo optimization, descriptor selection [27] |
| Descriptor Calculation | RDKit, ChemBioDraw, Dragon | Molecular descriptor computation | 2D/3D descriptor calculation [31] [28] |
| Chemical Databases | ChEMBL, PubChem, DrugBank | Bioactivity data source | Compound sourcing, activity data [29] |
| Text Mining | BioBERT, PubMed | Data extraction from literature | Automated dataset construction [28] |
| Docking & Dynamics | PyRx, AutoDock Vina, GROMACS | Structure-based modeling | Binding mode analysis, stability assessment [31] [30] |
The landscape of cancer QSAR research is characterized by diverse molecular descriptors tailored to specific cancer types and endpoints, complemented by increasingly sophisticated datasets constructed through both manual curation and automated text mining approaches. Quantum chemical descriptors offer fundamental insights into electronic properties governing anti-cancer activity, while 2D, topological, and SMILES-based descriptors provide computationally efficient alternatives with strong predictive power. The reliability of resulting models hinges critically on rigorous validation protocols, particularly double cross-validation approaches that provide unbiased performance estimates under model uncertainty. As the field advances, integration of QSAR predictions with experimental validation through molecular docking, dynamics simulations, and in vitro testing will continue to enhance the efficiency of anti-cancer drug discovery, ultimately contributing to the development of more effective and selective cancer therapeutics.
In the field of cancer research, Quantitative Structure-Activity Relationship (QSAR) models have become indispensable tools for accelerating drug discovery. These computational models predict the biological activity of chemical compounds against specific cancer targets, guiding researchers toward promising therapeutic candidates [32] [33]. The reliability of these models depends critically on rigorous validation practices, with cross-validation being a fundamental technique for assessing predictive performance and minimizing overfitting [34] [35].
Among cross-validation methods, Leave-One-Out cross-validation (LOO CV) has been widely adopted, particularly in QSAR studies featuring limited compound datasets. The LOO q² statistic (or Q²) has traditionally served as a primary metric for judging model quality, with higher values generally interpreted as indicating better predictive capability [33] [36]. However, within the context of cancer QSAR research—where model failures can misdirect precious resources in drug development—this article demonstrates that while LOO q² represents a necessary condition for model acceptability, it is far from sufficient as a standalone validation measure.
Understanding LOO Cross-Validation and Its Statistical Appeal
The LOO CV Methodology
Leave-One-Out Cross-Validation (LOO CV) is a resampling technique that systematically excludes each compound from the dataset once, using the remaining compounds to build a model that predicts the omitted observation [34]. For a dataset containing N compounds, this process involves N separate model building and prediction cycles. The LOO q² statistic is then calculated as:
[ q² = 1 - \frac{\sum{(y{i} - ŷ{i})^2}{\sum{(y_{i} - \bar{y})^2} ]
where (y{i}) represents the observed activity value, (ŷ{i}) is the predicted activity value when the ith compound is excluded from model building, and (\bar{y}) is the mean of all observed activity values [36].
Why LOO CV Gained Prominence in Cancer QSAR
LOO CV offers particular appeal for cancer QSAR studies, which often face limited compound availability due to the cost and complexity of synthetic and biological testing [37]. The method's advantages include:
- Maximized Training Data: Each model training iteration utilizes N-1 compounds, minimizing bias in small datasets [34]
- Comprehensive Usage: Every compound serves in both training and testing capacities across the validation process
- Theoretical Appeal: The approach appears to provide a thorough assessment of predictive capability
These attributes have led to LOO q² becoming a standard reporting requirement in many QSAR publications, with models often judged primarily on this metric [33] [36].
The "Necessary But Not Sufficient" Principle in Model Validation
Logical Foundation of the Principle
The concept of a condition being "necessary but not sufficient" has a precise meaning in logical reasoning. A necessary condition (A) for an outcome (B) must be present for B to occur, but its presence alone does not guarantee B [38]. In the context of QSAR validation:
- LOO q² as Necessary Condition: A sufficiently high q² value is required for a model to be considered predictive
- Insufficiency Demonstrated: High q² alone does not ensure reliable predictions for novel compounds
This logical fallacy occurs when researchers treat the necessary condition (good LOO q²) as sufficient for establishing model validity [38] [39].
Mathematical and Practical Limitations of LOO q²
Despite its widespread use, LOO CV exhibits several critical limitations that undermine its reliability as a sole validation metric:
- High Variance: The method can produce unstable estimates, particularly with small datasets or outliers [34]
- Insufficient Stress Testing: Models are not adequately tested on structurally diverse compounds simultaneously
- Ambiguity in Thresholds: Arbitrary q² cutoff values (e.g., 0.5) provide false security without complementary metrics [36]
The fundamental issue is that LOO CV primarily assesses interpolative capability within the chemical space of the training set, while QSAR models are most valuable for their extrapolative power to truly novel chemotypes [40].
Comparative Analysis of Cross-Validation Techniques in Cancer QSAR
Beyond LOO: Alternative Validation Methods
Robust QSAR model validation requires multiple approaches that complement LOO CV's limitations:
- Leave-Many-Out Cross-Validation (LMO CV): Also known as k-fold cross-validation, this method excludes multiple compounds (typically 10-30%) during each validation cycle, providing a more challenging test of model robustness [33]
- External Validation: The most rigorous approach uses a completely independent compound set not involved in model development, directly simulating real-world prediction scenarios [32] [40]
- Y-Randomization: This technique scrambles activity values to ensure models cannot achieve good statistics by chance alone, testing for chance correlation [33] [36]
Table 1: Comparison of Cross-Validation Methods in Cancer QSAR Research
| Validation Method | Key Characteristics | Advantages | Limitations | Reported Usage in Cancer QSAR |
|---|---|---|---|---|
| LOO CV | Each compound omitted once; N iterations | Maximizes training data; Low bias | High variance; Optimistic estimates | Widely used (e.g., [33] [36]) |
| LMO CV | Multiple compounds omitted; k folds (k=5-10) | Better variance estimation; More challenging test | Smaller training sets; Computational cost | Increasing adoption (e.g., [33]) |
| External Validation | Completely independent compound set | Real-world simulation; Most reliable assessment | Requires additional experimental data | Gold standard (e.g., [32] [40]) |
Case Studies: LOO q² Limitations in Practical Cancer Research
Recent cancer QSAR studies demonstrate the insufficiency of LOO q² alone:
- In a breast cancer QSAR model developing combinational therapy, Deep Neural Networks achieved impressive LOO q² values (0.94) but required external validation on separate cell lines to confirm practical utility [32]
- A study on aurora kinase inhibitors for breast cancer reported both LOO q² (0.7875) and LMO q² (0.7624), with the divergence between values indicating potential overfitting had only LOO been considered [33]
- Research on anti-colorectal cancer agents combined cross-validation with multiple metrics including R², RMSE, and interaction terms to provide comprehensive model assessment beyond single q² values [24]
Table 2: Representative Validation Approaches in Recent Cancer QSAR Studies
| Research Focus | LOO q² Reported | Additional Validation | Key Findings | Reference |
|---|---|---|---|---|
| Breast Cancer Combinational Therapy | R²=0.94 (DNN) | External test set validation | Model generalized well to novel drug combinations | [32] |
| Aurora Kinase Inhibitors | Q²LOO=0.7875 | LMO (Q²LMO=0.7624); External set (R²ext=0.8735) | Discrepancy highlighted need for multiple metrics | [33] |
| Lung Surfactant Inhibition | 5-fold CV accuracy=96% | 10 random seeds; Multiple metrics (F1 score=0.97) | Comprehensive protocol revealed true performance | [40] |
Implementing Robust Validation Protocols: A Practical Guide
Essential Components of QSAR Validation
Based on analysis of successful cancer QSAR studies, robust validation should incorporate these elements:
- Multiple Resampling Methods: Combine LOO with LMO (k-fold) cross-validation [33]
- External Test Set: Reserve 20-30% of compounds for final validation [32] [40]
- Diverse Statistical Metrics: Include R², RMSE, MAE, and domain-specific metrics [32] [40]
- Y-Randomization: Verify models outperform random chance [33] [36]
- Applicability Domain Assessment: Define chemical space where predictions are reliable [40]
Recommended Workflow for Cancer QSAR Validation
The following diagram illustrates a comprehensive validation protocol that positions LOO q² as one component within a multifaceted validation strategy:
Diagram 1: Comprehensive QSAR Validation Workflow (Title: QSAR Validation Protocol)
Table 3: Key Research Reagent Solutions for QSAR Validation
| Tool/Category | Specific Examples | Function in Validation | Implementation Notes |
|---|---|---|---|
| Cheminformatics Libraries | RDKit, PaDEL-Descriptor, Mordred | Molecular descriptor calculation | Generate structural features for modeling [40] |
| Machine Learning Frameworks | scikit-learn, DTC-Lab, PyTorch | Model building and validation | Implement cross-validation protocols [32] [40] |
| Specialized QSAR Software | QSARINS, Material Studio | Dedicated QSAR analysis | Built-in validation statistics [33] |
| Data Processing Tools | Scikit-learn preprocessing, DTC-Lab pretreatment | Data standardization and splitting | Ensure proper train/test separation [32] [40] |
The LOO q² statistic remains a valuable initial screening tool in QSAR model development—a necessary first hurdle that models must clear. However, treating this metric as a sufficient condition for model validity represents a critical methodological error with potentially significant consequences in cancer drug discovery. Robust validation requires a multifaceted approach that combines LOO with LMO cross-validation, external validation, and complementary statistical measures.
As cancer QSAR research increasingly incorporates complex machine learning algorithms and tackles more challenging therapeutic targets, the validation standards must evolve accordingly. By recognizing LOO q² as necessary but insufficient, researchers can implement more rigorous validation protocols that ultimately yield more reliable, predictive models—accelerating the discovery of urgently needed cancer therapeutics.
Implementing LOO and LMO Cross-Validation in Anti-Cancer QSAR Workflows
Step-by-Step Protocol for LOO Cross-Validation Implementation
Quantitative Structure-Activity Relationship (QSAR) modeling is essential in drug discovery for predicting the biological activity of chemical compounds based on their structural features [41]. In cancer research, reliable QSAR models help prioritize compounds for synthesis and testing. Cross-validation (CV) is a fundamental procedure for estimating the predictive performance of these models, with Leave-One-Out (LOO) and Leave-Many-Out (LMO) being two pivotal techniques [42] [43]. This guide provides a detailed, step-by-step protocol for implementing LOO cross-validation, objectively compares it with LMO, and presents experimental data within cancer QSAR research.
Conceptual Foundations of LOO and LMO
Leave-One-Out (LOO) Cross-Validation
LOO-CV is an exhaustive cross-validation technique where each compound in the dataset is systematically held out once as the test set, while the remaining n-1 compounds form the training set [44] [45]. This process repeats for all n compounds in the dataset. The final performance metric is the average of all n individual evaluations [46]. The core advantage of LOO is that it maximizes the data used for training, resulting in a less biased estimate, which is particularly valuable with small datasets [45] [46].
Leave-Many-Out (LMO) Cross-Validation
LMO-CV, also known as k-fold cross-validation, involves partitioning the dataset into k subsets (folds) of approximately equal size [45]. In each iteration, one fold is held out as the test set, and the remaining k-1 folds are used for model training. This process repeats k times until each fold has served as the test set once [35]. Typical values for k are 5 or 10 [45]. LMO introduces more randomness in the data splitting compared to the deterministic LOO, but is computationally more efficient for larger datasets [43].
The workflow below illustrates the fundamental difference in how datasets are partitioned for LOO-CV versus LMO-CV.
Comparative Analysis: LOO vs. LMO in Practice
Theoretical and Practical Comparison
The choice between LOO and LMO involves trade-offs between bias, variance, and computational cost [45]. LOO-CV tends to have lower bias because each training set contains n-1 samples, making it nearly identical to the full dataset. However, since the test sets of LOO are highly similar (overlapping), the performance estimates can have higher variance [46]. Conversely, LMO-CV (e.g., 5-fold or 10-fold) has slightly higher bias but lower variance in its estimates due to more independent test sets [45]. Computationally, LOO requires fitting n models, which becomes prohibitive for large n or complex models, whereas LMO only requires fitting k models [45].
Performance Comparison in Cancer QSAR Studies
Empirical studies, particularly in cancer research, provide concrete performance data. The table below summarizes a comparison from a QSAR study on melanoma cell line SK-MEL-5, which utilized various machine learning classifiers [41].
Table 1: Comparison of LOO and 5-Fold LMO Performance in a Melanoma QSAR Study [41]
| Machine Learning Classifier | Average LOOCV Accuracy (%) | Average 5-Fold LMO Accuracy (%) | Optimal Descriptor Set |
|---|---|---|---|
| Random Forest (RF) | 88.5 | 86.2 | Topological descriptors, Information indices |
| Gradient Boosting (BST) | 85.1 | 83.7 | 2D-Autocorrelation descriptors |
| Support Vector Machine (SVM) | 86.8 | 85.5 | P-VSA-like descriptors, Edge-adjacency indices |
| k-Nearest Neighbors (KNN) | 82.3 | 80.9 | 2D-Autocorrelation descriptors |
A separate multi-level analysis of QSAR modeling methods further compared validation protocols across different case studies, providing general insights into the consistency of these methods [43].
Table 2: General Comparison of CV Methods Based on Multi-Level QSAR Analysis [43]
| Validation Aspect | LOO-CV | 5-Fold LMO (Random) | 5-Fold LMO (Contiguous) | 5-Fold LMO (Venetian Blind) |
|---|---|---|---|---|
| Bias of Estimate | Low | Medium | Medium | Medium |
| Variance of Estimate | High | Medium | High | Medium |
| Computational Cost | High | Low | Low | Low |
| Stability/Determinism | High (Deterministic) | Low (Randomized) | Medium | Medium |
| Resistance to Data Ordering | High | Medium | Low | High |
Step-by-Step LOO-CV Protocol for Cancer QSAR
This protocol is designed for researchers implementing LOO-CV in a Python environment, using standard QSAR data structures.
Prerequisites and Data Preparation
- Environment Setup: Ensure Python (v3.7+) is installed with the following core libraries:
scikit-learn(for model building and CV),pandas(for data handling),numpy(for numerical operations), andrdkitordragon(for calculating molecular descriptors if needed). - Dataset Curation: The dataset should consist of a matrix where rows represent unique chemical compounds and columns represent molecular descriptors and a biological activity endpoint (e.g., GI50, IC50 for cytotoxicity) [41]. For classification models, discretize the activity (e.g., 'active' if GI50 < 1 µM, 'inactive' otherwise) [41].
- Data Pre-processing:
- Descriptor Filtering: Remove descriptors with constant or near-constant values.
- Handling Missing Values: Remove descriptors or impute missing values.
- Reducing Correlarity: Remove highly correlated descriptors (e.g., correlation coefficient > 0.80) to mitigate multicollinearity [41].
- Feature Selection: Apply feature selection methods (e.g., Random Forest importance, symmetrical uncertainty) to reduce dimensionality. Select a manageable number of top descriptors (e.g., 7-15) [41].
Detailed LOO-CV Implementation Code
The following Python code demonstrates the LOO-CV procedure for a Random Forest classifier, a common and robust algorithm in QSAR studies [41].
Performance Evaluation and Model Validation
After completing the LOO-CV procedure, a comprehensive evaluation is necessary.
- Calculate Performance Metrics: Beyond accuracy, calculate metrics relevant to your research question. For classification, report Precision, Recall, Specificity, and F1-Score. For regression, use Root Mean Square Error (RMSE) and the Coefficient of Determination (R²) [42] [47].
- External Validation: The OECD principles for QSAR validation stress the importance of external validation. After finalizing a model using LOO-CV internally, its predictive power must be confirmed on a truly external test set of compounds that were never used in any model-building or CV step [47] [6].
- Assess Model Applicability Domain: Define the chemical space area where the model's predictions are reliable. This can be assessed using leverage, distance-based methods, or ranges of descriptor values [41].
The Scientist's Toolkit: Essential Research Reagents & Solutions
Building and validating a robust cancer QSAR model requires a suite of computational tools and data resources. The table below lists key components.
Table 3: Essential Research Reagent Solutions for Cancer QSAR Modeling
| Item Name | Function / Purpose | Example / Note |
|---|---|---|
| Bioactivity Database | Source of experimental biological activity data for model training and testing. | PubChem BioAssay (source of SK-MEL-5 GI50 data) [41] |
| Chemical Standardization Tool | Standardizes molecular structures into a consistent representation for descriptor calculation. | ChemAxon Standardizer [41] |
| Descriptor Calculation Software | Computes numerical representations of molecular structures from 1D to 3D. | Dragon software [41] |
| Machine Learning Framework | Provides algorithms for building classification/regression models and validation procedures. | Scikit-learn (Python) [35] [45] |
| Statistical Analysis Environment | Used for data pre-processing, statistical analysis, and visualization. | R programming language [41] |
Experimental Protocol & Workflow from a Cited Study
To ground this guide in practical research, the following diagram and summary detail the protocol from a published QSAR study on SK-MEL-5 melanoma cell line cytotoxicity [41].
Summary of Key Experimental Details [41]:
- Dataset: 422 unique compounds after duplicate removal, with 174 active and 248 inactive on SK-MEL-5.
- Descriptors: 13 blocks of molecular descriptors were computed (e.g., topological indices, 2D-autocorrelations, edge-adjacency indices) and pre-processed.
- Modeling: Four machine learning classifiers (RF, BST, SVM, KNN) were used. LOO-CV was performed on the training set (n=316) for model selection and evaluation.
- Results: The best models (all Random Forests) achieved a LOO-CV accuracy of ~88.5% and a positive predictive value (PPV) higher than 0.85 upon external validation.
LOO-CV is a powerful validation technique for QSAR models, especially when working with small, precious datasets common in early-stage cancer drug discovery. It provides a nearly unbiased estimate of model performance by maximizing the use of available data. While LMO-CV (e.g., 5-fold) offers a computationally cheaper and potentially less variable alternative, LOO-CV remains a gold standard for rigorous internal validation [6] [43]. The optimal choice depends on the dataset size, computational resources, and the specific requirement for bias-variance trade-off. Ultimately, a well-validated QSAR model should employ rigorous internal validation like LOO-CV and must be confirmed by a strong external validation test to ensure its reliability for predicting the activity of new, untested compounds.
Quantitative Structure-Activity Relationship (QSAR) modeling represents a cornerstone methodology in modern computational drug discovery, enabling researchers to predict the biological activity of compounds based on their chemical structures [13]. These statistical models correlate molecular descriptors—numerical representations of chemical properties—with biological responses, providing invaluable insights for lead optimization and virtual screening in anticancer drug development [17]. The reliability and predictive power of QSAR models hinge critically on rigorous validation techniques, with cross-validation standing as an indispensable component for assessing model robustness and preventing overfitting [1].
Within the landscape of cross-validation methods, Leave-One-Out (LOO) and Leave-Many-Out (LMO) strategies represent two fundamentally different approaches to model validation. LOO cross-validation, a more traditional approach, involves iteratively removing a single compound from the training set, building a model with the remaining compounds, and predicting the activity of the omitted compound [48]. This process repeats until every compound has been left out once. While computationally intensive, LOO provides a nearly unbiased estimate of model performance but may overestimate predictive accuracy for small datasets and fail to adequately assess model stability [49].
LMO cross-validation, alternatively known as k-fold cross-validation, addresses several limitations of LOO by systematically excluding multiple compounds simultaneously—typically between 10-30% of the dataset—during each validation iteration [49] [48]. This approach more effectively evaluates model stability against data fluctuations and provides a more realistic assessment of predictive performance on external compounds, making it particularly valuable for cancer QSAR models where dataset diversity and model applicability are paramount concerns [50]. The strategic implementation of LMO validation directly supports the development of more reliable predictive models for identifying novel anticancer therapeutics, ultimately accelerating the drug discovery pipeline while reducing resource-intensive experimental screening.
Theoretical Foundations of LMO Validation
Mathematical Framework and Algorithmic Implementation
The Leave-Many-Out cross-validation technique operates on a robust mathematical foundation designed to thoroughly evaluate QSAR model performance. The core algorithm partitions the complete dataset of N compounds into k distinct subsets of approximately equal size through random selection, though stratified sampling based on chemical structural features or activity ranges may be employed for cancer-related targets to ensure representative distribution [48]. The LMO procedure iteratively designates one subset (approximately N/k compounds) as the temporary validation set while using the remaining k-1 subsets (approximately N×(k-1)/k compounds) for model training. This process repeats k times until each subset has served as the validation set exactly once [49].
The predictive performance of LMO cross-validation is quantified using the cross-validated correlation coefficient (Q²), calculated as follows:
Q² = 1 - [Σ(yobserved - ypredicted)² / Σ(yobserved - ymean)²]
where yobserved represents the experimental biological activity values, ypredicted denotes the predicted activities from the LMO validation, and y_mean signifies the mean observed activity of the training set [48]. This metric directly measures the model's predictive capability, with values approaching 1.0 indicating excellent predictive power. Additional statistical parameters frequently reported alongside Q² include Root Mean Square Error (RMSE) values for both training and validation sets, which provide insights into prediction accuracy, and the Concordance Correlation Coefficient (CCC), which evaluates the agreement between observed and predicted values [51].
The critical distinction between LMO and LOO validation emerges from their respective approaches to dataset partitioning. While LOO represents an extreme case of LMO where k equals the number of compounds (N), this approach tends to yield higher variance in prediction error estimates for smaller datasets common in early-stage anticancer drug discovery [49]. The LMO method, with its intentional grouping of compounds, provides a more stringent assessment of model robustness by simulating how the model performs when predicting multiple structurally diverse compounds simultaneously, thus better approximating real-world virtual screening scenarios where models must predict activities for entirely new chemical classes [1].
OECD Guidelines for LMO Validation
The Organisation for Economic Co-operation and Development (OECD) has established definitive guidelines for QSAR model validation, with Principle 4 explicitly addressing the necessity of appropriate validation methods [52] [51]. These internationally recognized guidelines mandate that LMO validation must demonstrate acceptable statistical quality through multiple metrics including Q², RMSE, and CCC values to establish scientific validity for regulatory purposes in drug development [51]. The OECD guidelines further recommend that the number of LMO groups (k) and their composition be carefully selected based on dataset size and diversity, with specific emphasis on ensuring that each group represents the structural and activity space of the entire dataset [49].
For QSAR models targeting cancer therapeutics, adherence to these guidelines becomes particularly crucial given the potential clinical implications of model predictions. The OECD framework emphasizes that LMO validation should assess both internal predictability (through the Q² metric) and external predictability (through validation with truly external compounds not included in any model development), with the latter being especially important for establishing model utility in prospective virtual screening [51]. Recent research in anti-breast cancer QSAR models has further refined these guidelines by recommending that LMO group composition should account for chemical clustering based on molecular scaffolds to prevent overoptimistic performance estimates when structurally similar compounds are grouped together [13] [52].
Comparative Analysis: LMO vs. LOO Cross-Validation
Performance Metrics and Statistical Robustness
Table 1: Comparative Performance Metrics of LMO and LOO Cross-Validation in Cancer QSAR Studies
| Validation Metric | LMO Cross-Validation | LOO Cross-Validation | Statistical Significance & Implications |
|---|---|---|---|
| Q² Value Range | 0.7865 - 0.8558 [51] | Typically 0.05-0.15 higher than LMO for same dataset [48] | LMO provides more conservative, realistic estimate of external predictivity |
| Variance in Error Estimation | Lower variance due to compound grouping [49] | Higher variance, especially with small datasets [48] | LMO offers more stable performance estimates across different data partitions |
| Computational Intensity | Moderate (k iterations) [48] | High (N iterations for dataset size N) [48] | LMO more practical for large virtual screening libraries in cancer drug discovery |
| Sensitivity to Activity Cliffs | Better detection through grouped compound removal [1] | May miss activity cliffs if single compounds removed [1] | LMO superior for identifying robust structure-activity relationships in anticancer agents |
| Regulatory Acceptance (OECD) | Explicitly recommended for model validation [51] | Considered insufficient as sole validation method [49] | LMO required for OECD-compliant QSAR models in pharmaceutical development |
The comparative analysis reveals fundamental differences in how LMO and LOO cross-validation assess model performance. LOO cross-validation typically produces artificially inflated Q² values compared to LMO, as demonstrated in studies of urokinase-type plasminogen activator inhibitors where LMO Q² values ranged between 0.7865-0.8558 while corresponding LOO values were significantly higher [51]. This inflation stems from the high similarity between training sets in LOO validation, where models are built on nearly identical chemical spaces during each iteration. In contrast, LMO validation introduces more substantial chemical diversity between training and validation sets during each iteration, providing a more realistic assessment of how models will perform when predicting truly novel compounds in anti-cancer drug discovery pipelines [49].
The ability to detect activity cliffs—where small structural changes cause dramatic activity shifts—represents another critical distinction between these methodologies. LMO validation excels at identifying such phenomena because removing groups of compounds creates more substantial gaps in chemical space, potentially excluding entire structural classes during model building [1]. This capability is particularly valuable in cancer QSAR studies where small molecular modifications can significantly alter binding affinity to oncology targets such as estrogen receptors or tyrosine kinases [52] [53]. The grouped exclusion approach of LMO more effectively tests model robustness against such structural-activity discontinuities, ensuring developed models maintain predictive power across diverse chemical scaffolds.
Impact on Model Applicability Domain and Generalizability
The applicability domain (AD) of a QSAR model defines the chemical space within which reliable predictions can be expected, a concept particularly crucial for cancer therapeutic development where prediction errors can have significant resource implications [1] [48]. LMO cross-validation provides a more comprehensive assessment of a model's applicability domain by testing predictions for multiple simultaneously excluded compounds, effectively evaluating how the model performs when presented with combinations of structures that may collectively differ substantially from the training set [48]. This grouped exclusion approach better simulates real-world virtual screening scenarios where researchers typically predict activity for batches of novel compounds rather than individual molecules.
The composition and size of LMO groups directly influence applicability domain assessment. When LMO groups are constructed to represent diverse chemical scaffolds present in the complete dataset, the validation process more rigorously tests the model's ability to handle structural diversity—a key requirement for robust virtual screening in anti-cancer compound libraries [13]. Recent research on estrogen receptor beta binders for hormone-dependent breast cancer demonstrated that LMO validation with strategically grouped compounds provided superior insights into model generalizability compared to LOO, correctly identifying limitations in predicting structurally distinct chemotypes [52]. This capacity to reveal model boundaries makes LMO an indispensable component of QSAR development for molecular targets with diverse binding motifs, such as kinase inhibitors in oncology.
Strategic Implementation of LMO in Cancer QSAR Research
Optimal Group Size Selection and Composition
Table 2: Recommended LMO Grouping Strategies for Different Cancer QSAR Scenarios
| Dataset Size | Recommended Group Number (k) | Recommended Group Size (%) | Composition Strategy | Typical Q² Range |
|---|---|---|---|---|
| Small (<50 compounds) | 5-7 groups [48] | 14-20% per group [49] | Scaffold-based stratification | 0.75-0.85 [51] |
| Medium (50-200 compounds) | 7-10 groups [49] | 10-14% per group [48] | Activity-based binning + structural diversity | 0.80-0.90 [52] |
| Large (>200 compounds) | 10-15 groups [1] | 7-10% per group | Random stratified sampling | 0.85-0.95 [13] |
| Imbalanced Activities | 5-8 groups [48] | Varies to maintain activity representation | Oversampling of minority class | 0.70-0.85 [1] |
| Diverse Scaffolds | 6-9 groups [52] | 11-16% per group | Maximum dissimilarity partitioning | 0.75-0.88 [51] |
Determining the optimal group size and composition for LMO cross-validation requires careful consideration of dataset characteristics and research objectives. For typical cancer QSAR datasets containing 50-200 compounds, such as those developing estrogen receptor beta binders for breast cancer, research indicates that 7-10 groups with each containing 10-14% of the total compounds provides the best balance between computational efficiency and validation rigor [49] [52]. This grouping strategy creates substantial enough validation sets to properly challenge model predictivity while maintaining sufficiently large training sets for stable model building during each iteration.
The composition of LMO groups significantly influences validation outcomes and should be strategically designed rather than randomly assigned. For cancer QSAR models targeting specific molecular pathways, group composition should ensure that each partition represents the structural diversity of the entire dataset, particularly when dealing with chemically diverse screening libraries [13]. Advanced approaches incorporate maximum dissimilarity sampling or scaffold-based stratification to guarantee that each LMO group contains structurally representative compounds, thus providing a more challenging and informative validation process [52] [51]. This approach is particularly valuable when modeling complex molecular targets like tyrosine kinases or histone deacetylases in oncology, where compound scaffolds may exhibit distinct binding modes.
For smaller datasets common in early-stage anti-cancer drug discovery, studies on tetrahydronaphthalene derivatives as antitubercular agents (methodologically relevant to cancer QSAR) demonstrate that 5-7 groups provide more reliable validation than LOO, with each group containing 14-20% of the total compounds [48]. This approach maintains reasonable training set sizes while creating meaningful validation challenges. Similarly, for datasets with imbalanced activity distributions—frequently encountered when studying potent inhibitors versus moderately active compounds—group composition should ensure proportional representation of activity classes across all partitions to prevent biased performance estimates [1].
Integration with Complementary Validation Techniques
While LMO cross-validation provides robust internal validation, comprehensive QSAR model assessment for cancer drug discovery requires integration with additional validation techniques. External validation with completely excluded compounds remains the gold standard for establishing predictive power, with LMO serving as an effective precursor to this final validation step [1] [48]. The OECD guidelines explicitly recommend this hierarchical validation approach, emphasizing that LMO demonstrates internal predictivity while external validation confirms true generalizability to novel chemical entities [51].
Recent advances in anti-breast cancer QSAR research have demonstrated the effectiveness of combining LMO validation with Y-randomization testing, which assesses model robustness by confirming that observed predictivity stems from genuine structure-activity relationships rather than chance correlations [52]. The integration protocol involves performing LMO cross-validation on datasets with randomly scrambled activity values, with valid models demonstrating significantly higher Q² values for the original data versus randomized versions [48]. This combined approach is particularly valuable for cancer QSAR models based on complex machine learning algorithms where overfitting risks are elevated.
The application domain assessment represents another critical complement to LMO validation, establishing the boundaries within which models provide reliable predictions [48]. For cancer therapeutic development, this typically involves calculating leverage values and determining critical thresholds (h) using the formula h = 3(p+1)/n, where p represents the number of model descriptors and n the training set size [48]. Compounds falling outside this applicability domain should be identified during LMO validation, providing additional insights into model limitations for specific chemical classes—information particularly valuable when prioritizing compounds for experimental evaluation in resource-constrained drug discovery programs.
Experimental Protocols and Case Studies
Detailed Methodological Framework for LMO Implementation
Implementing robust LMO cross-validation requires systematic execution of well-defined procedural steps, as demonstrated in successful QSAR studies on urokinase-type plasminogen activator inhibitors and anti-breast cancer compounds [52] [51]. The following protocol outlines a comprehensive methodology tailored to cancer QSAR research:
Step 1: Dataset Curation and Preprocessing Begin with rigorous dataset preparation, including structural standardization, descriptor calculation, and biological activity verification. For cancer targets such as tyrosine kinases or apoptosis regulators, ensure activity data (IC₅₀, Ki, or % inhibition) originates from consistent experimental assays [53]. Calculate molecular descriptors using established software like PaDEL Descriptor or DRAGON, generating an initial matrix of 1,000-3,000 descriptors per compound [17] [48]. Apply preprocessing to reduce dimensionality through variance filtering and correlation analysis, typically retaining 150-300 relevant descriptors to mitigate overfitting while capturing essential chemical information [48].
Step 2: Strategic Dataset Partitioning Divide the curated dataset into k groups for LMO validation using stratified sampling rather than random assignment. For cancer QSAR models, stratification should consider both structural similarity (using molecular fingerprints or scaffold analysis) and activity distribution to ensure each group represents the full chemical and biological diversity of the dataset [52] [51]. Utilize chemoinformatic tools such as RDKit or KNIME to implement maximum dissimilarity algorithms that optimize group composition, particularly important when working with structurally diverse anticancer compound libraries [17].
Step 3: Iterative Model Building and Validation For each of the k iterations, retain k-1 groups as the training set and use the excluded group for validation. Build QSAR models using the selected algorithm (e.g., Partial Least Squares for linear relationships or Random Forests for complex non-linear patterns) [17]. Record prediction statistics for each validation set compound, including observed versus predicted activities and residual errors. For cancer QSAR models specifically, document any notable prediction failures for structurally unique compounds or activity cliffs, as these highlight potential model limitations for specific chemical classes [1].
Step 4: Comprehensive Performance Assessment Following all k iterations, consolidate prediction results and calculate overall validation metrics including Q², RMSE, and CCC values [48] [51]. Perform additional statistical tests to confirm significance, including Y-randomization to verify model robustness (with scrambled activity models showing substantially lower performance) and residual analysis to identify systematic prediction errors [48]. For cancer therapeutic applications, particularly analyze performance for highly active compounds (e.g., IC₅₀ < 100 nM) to ensure accurate prediction of promising leads.
Step 5: Applicability Domain Characterization Define the model's applicability domain using leverage approaches (Williams plot) and distance-based methods [48]. Calculate the critical leverage value h* = 3(p+1)/n, where p represents descriptor count and n training set size, to identify compounds outside the reliable prediction space [48]. This step is crucial for cancer QSAR models to establish boundaries for reliable virtual screening and identify chemical regions requiring model refinement or additional training data.
Case Study: Estrogen Receptor Beta Binders for Breast Cancer
A recent investigation of estrogen receptor beta (ERβ) binders for hormone-dependent breast cancer provides an exemplary case study of strategic LMO implementation [52]. Researchers developed QSAR models using a diverse set of ERβ inhibitors with pIC₅₀ values ranging from 4.0-9.0, implementing LMO validation with k=8 groups (12.5% exclusion each iteration) based on scaffold-stratified partitioning to ensure each group contained representative structural diversity [52].
The LMO validation demonstrated exceptional performance with Q²LMO = 0.792 and CCCex = 0.886, significantly higher than corresponding LOO values which typically overestimate predictivity by 0.05-0.15 units [52]. Critically, the strategic group composition revealed model limitations for specific indole-based scaffolds that random partitioning might have masked, enabling researchers to refine descriptors related to hydrogen bond donors and lipophilic atoms specifically for these chemotypes [52]. The LMO results further informed applicability domain definition, correctly identifying 89% of external validation compounds that would fall within reliable prediction boundaries during subsequent prospective screening.
This case study highlights how tailored LMO group composition based on chemical structure, rather than random partitioning, provides deeper insights into model strengths and limitations across diverse chemotypes—particularly valuable for molecular targets like ERβ that accommodate multiple binding motifs [52]. The implementation successfully balanced predictive accuracy (Q²) with mechanistic interpretability, identifying that sp²-hybridized carbon and nitrogen atoms alongside specific hydrogen bond donor/acceptor patterns critically influenced binding affinity [52].
Table 3: Essential Research Resources for LMO Implementation in Cancer QSAR
| Resource Category | Specific Tools & Software | Key Functionality | Application in Cancer QSAR |
|---|---|---|---|
| Descriptor Calculation | PaDEL-Descriptor [48], DRAGON [17], RDKit [17] | Generates molecular descriptors from chemical structures | Calculates 1D-3D molecular features for structure-activity modeling |
| Model Building & Validation | QSARINS [48], scikit-learn [17], KNIME [17] | Implements machine learning algorithms and validation protocols | Develops predictive models with LMO cross-validation capabilities |
| Chemical Diversity Analysis | RDKit [17], ChemAxon | Assesses structural similarity and scaffold diversity | Optimizes LMO group composition through stratified sampling |
| Statistical Analysis | R Statistics, Python SciPy | Computes validation metrics and statistical significance | Calculates Q², RMSE, CCC and performs Y-randomization tests |
| Data Visualization | MATLAB, Python Matplotlib | Generates Williams plots and performance graphics | Visualizes applicability domains and model performance |
| Chemical Databases | ChEMBL, PubChem, ZINC [1] | Provides bioactivity data and compound structures | Sources experimental data for model training and validation |
The effective implementation of LMO cross-validation requires specialized computational tools and curated chemical databases. QSARINS software has emerged as particularly valuable for cancer QSAR applications, providing integrated genetic algorithm-based descriptor selection coupled with comprehensive LMO validation capabilities [48]. For larger datasets or complex machine learning approaches, open-source platforms like KNIME and scikit-learn offer flexible environments for implementing custom LMO protocols with various algorithms including Support Vector Machines and Random Forests [17].
Chemical descriptor calculation represents another critical component, with tools like PaDEL-Descriptor and DRAGON capable of generating thousands of molecular descriptors encompassing topological, electronic, and geometric features [17] [48]. For cancer QSAR models targeting specific protein families such as kinases or nuclear receptors, incorporating target-specific descriptors like molecular fingerprints or pharmacophore features may enhance model performance and biological relevance [52]. These computational resources collectively enable researchers to implement the sophisticated LMO strategies necessary for developing robust, predictive QSAR models in anticancer drug discovery.
The strategic implementation of Leave-Many-Out cross-validation represents a critical methodological advancement in QSAR modeling for cancer therapeutics. By moving beyond traditional Leave-One-Out approaches, LMO validation provides more realistic assessments of model performance, enhances detection of activity cliffs, and establishes more reliable applicability domains—all essential factors for successful virtual screening in anti-cancer drug discovery [49] [1]. The optimal group size and composition strategies discussed, particularly scaffold-stratified partitioning for structurally diverse datasets, directly address the unique challenges of cancer-related QSAR models where chemical diversity and prediction reliability are paramount concerns [52] [51].
Future developments in LMO methodology will likely integrate artificial intelligence and deep learning approaches to further enhance validation rigor [17]. Graph neural networks and transformer-based architectures offer potential for automatically learning molecular representations that capture subtle structure-activity relationships, potentially complementing traditional descriptor-based QSAR models [17]. Additionally, the growing availability of large-scale cancer cell line screening data and multi-omics datasets presents opportunities for developing multi-task LMO validation approaches that simultaneously assess predictivity across multiple cancer types or molecular targets [50] [17].
The consistent demonstration of LMO's superiority over LOO in recent cancer QSAR studies, particularly those following OECD guidelines, underscores the importance of adopting these advanced validation techniques as standard practice [52] [51]. As QSAR models continue to play increasingly prominent roles in early-stage anticancer drug discovery, the rigorous validation provided by well-designed LMO strategies will be essential for building stakeholder confidence in computational predictions and efficiently prioritizing compounds for experimental evaluation. Through continued refinement of group size optimization and composition strategies, the cancer research community can further enhance the reliability and impact of QSAR modeling in the ongoing development of novel therapeutic agents.
Quantitative Structure-Activity Relationship (QSAR) modeling represents a pivotal computational approach in modern drug discovery, enabling researchers to predict the biological activity of compounds based on their chemical structures. For complex diseases like colorectal cancer (CRC)—the fourth leading cause of cancer mortality worldwide—QSAR models offer promising pathways for accelerating the identification of novel therapeutic agents [54]. The reliability of these models, however, critically depends on the validation techniques employed during their development. This guide provides a comprehensive comparison of QSAR modeling approaches for anti-CRC agents, with particular emphasis on cross-validation methodologies including Leave-One-Out (LOO) and Leave-Many-Out (LMO) techniques, which are essential for establishing model robustness and predictive capability.
QSAR Modeling Approaches for Anti-CRC Agents: A Comparative Analysis
QSAR studies for anti-colorectal cancer agents have utilized diverse molecular descriptors and statistical approaches, each with distinct advantages and validation requirements.
Table 1: Comparison of QSAR Approaches for Anti-Colorectal Cancer Agent Discovery
| Modeling Approach | Descriptor Type | Key Predictors | Validation Methods | Reported Performance | Applications |
|---|---|---|---|---|---|
| Quantum Chemical QSAR [24] | Quantum chemical | Total electronic energy (ET), Most positive atomic charge (Qmax), Electrophilicity (ω) | Logistic regression, 95% confidence intervals for interaction terms | Classification accuracy for active compounds | Prediction of anti-CRC activity using Gaussian optimization data |
| 3D-QSAR (CoMFA) [54] | 3D steric and electrostatic fields | Molecular field contours | LOO, LMO, external test set | r² = 0.99, q² = 0.625 | Design of naphthoquinone derivatives with 2-fold higher theoretical activity |
| Hybrid QSAR/Docking [55] | Quantum chemical descriptors | Not specified | Internal validation (R² = 0.9407, adjusted R² = 0.9329), external test set (R² = 0.9012) | MAE = 1.3313, CCC = 0.9229 | Integrated workflow with molecular docking and dynamics |
Experimental Data and Anti-Proliferative Activity
Recent QSAR investigations have leveraged experimental data from compound screening against colorectal cancer cell lines. A study evaluating 36 naphthoquinone derivatives against HT-29 cells identified 15 compounds as active (1.73 < IC₅₀ < 18.11 μM), with naphtho[2,3-b]thiophene-4,9-dione analogs demonstrating particularly potent cytotoxicity [54]. The most active compound, 8-hydroxy-2-(thiophen-2-ylcarbonyl)naphtho[2,3-b]thiophene-4,9-dione, showed high potency and selectivity, suggesting tricyclic systems with electron-withdrawing groups enhance toxicity against CRC cells.
Cross-Validation Techniques in QSAR Modeling
Fundamental Validation Frameworks
Robust validation is paramount in QSAR modeling to ensure predictive reliability for novel compounds. The primary validation strategies include:
- Internal Validation: Assesses model stability using only the training dataset, primarily through LOO and LMO cross-validation.
- External Validation: Evaluates model performance on completely independent test compounds not used in model development.
- Double Cross-Validation: A nested approach that provides reliable estimation of prediction errors under model uncertainty [7].
Comparative Analysis of LOO vs. LMO Validation
Table 2: Comparison of Cross-Validation Techniques in QSAR Modeling
| Validation Aspect | Leave-One-Out (LOO) | Leave-Many-Out (LMO) | Double Cross-Validation |
|---|---|---|---|
| Procedure | Iteratively removes one compound, builds model on remaining n-1 compounds | Removes a subset of compounds (often 20-30%) repeatedly | Nested loops with internal model selection and external assessment |
| Advantages | Maximizes training data usage, low bias | Better balance of bias-variance, more realistic error estimation | Unbiased error estimation, handles model uncertainty effectively |
| Disadvantages | High computational cost, potentially high variance, optimistic error estimates | Fewer iterations possible, depends on subset selection | Complex implementation, computationally intensive |
| Recommended Use | Small datasets (<30 compounds) [19] | Medium to large datasets, standard practice | Critical applications requiring reliable error estimates [7] |
Implementation Protocols for Cross-Validation
LOO Cross-Validation Protocol:
- Begin with a dataset of N compounds with known structures and biological activities
- Remove one compound from the dataset to serve as the validation sample
- Build the QSAR model using the remaining N-1 compounds
- Predict the activity of the excluded compound using the developed model
- Repeat steps 2-4 until each compound has been excluded exactly once
- Calculate the cross-validated correlation coefficient (q²) and predictive error metrics
LMO Cross-Validation Protocol:
- Randomly divide the dataset into k subsets (typically k=5 or k=10)
- Remove one subset (approximately 20% of data) to serve as the validation set
- Build the QSAR model using the remaining compounds (approximately 80% of data)
- Predict the activities of compounds in the validation set
- Repeat steps 2-4 until each subset has been used as a validation set
- Calculate overall cross-validation statistics across all iterations
Advanced Validation Methodologies
Double Cross-Validation for Enhanced Reliability
Double cross-validation (also known as nested cross-validation) addresses a critical limitation of standard validation techniques: model selection bias. This approach employs two nested loops:
- Inner Loop: Performs model selection and optimization using the training data only
- Outer Loop: Provides unbiased assessment of the model's predictive performance [7]
This method is particularly valuable when dealing with high-dimensional descriptor spaces and multiple modeling algorithms, as it prevents overoptimistic performance estimates that can occur when the same data is used for both model selection and validation.
Validation Workflow Visualization
Figure 1: Comprehensive QSAR Validation Workflow Integrating LOO, LMO, and External Validation
Statistical Metrics for Model Validation
Table 3: Key Statistical Parameters for QSAR Model Validation
| Metric | Formula | Acceptance Criteria | Interpretation |
|---|---|---|---|
| q² (LOO/LMO) | q² = 1 - Σ(yₚᵣₑd - yₐcₜ)² / Σ(yₐcₜ - ȳ)² | > 0.5 (acceptable) > 0.6 (good) | Internal predictive ability |
| R² | R² = 1 - Σ(yₚᵣₑd - yₐcₜ)² / Σ(yₐcₜ - ȳ)² | > 0.8 (good fit) | Goodness of fit for training set |
| R²ₜₑₛₜ | Same as R² for test set | > 0.6 (acceptable) | External predictive ability |
| CCC | CCC = 2rσₓσᵧ/(σₓ² + σᵧ² + (μₓ - μᵧ)²) | > 0.85 (good) [4] | Agreement between observed and predicted values |
| MAE | MAE = Σ|yₚᵣₑd - yₐcₜ|/n | Lower values indicate better performance | Average magnitude of prediction errors |
Table 4: Essential Research Reagents and Computational Tools for Anti-CRC QSAR Studies
| Tool/Resource | Type | Function | Application Examples |
|---|---|---|---|
| Gaussian [24] | Quantum Chemical Software | Molecular structure optimization and descriptor calculation | Calculation of total electronic energy (ET) and atomic charges at HF/3-21G level |
| Spartan [55] | Molecular Modeling Software | Molecular mechanics and quantum chemical calculations | Generation of quantum chemical descriptors for QSAR modeling |
| PyRx [55] | Docking Software | Virtual screening and molecular docking | Prediction of protein-ligand interactions and binding affinities |
| SwissADME [55] | Web Tool | Pharmacokinetic property prediction | Assessment of drug-likeness, absorption, distribution, metabolism, and excretion |
| Desmond [55] | Molecular Dynamics Software | Simulation of molecular trajectories | Analysis of protein-ligand complex stability and interaction dynamics |
| Dragon [19] | Molecular Descriptor Software | Calculation of 2D/3D molecular descriptors | Generation of structural parameters for QSAR model development |
This comparison guide demonstrates that effective QSAR modeling for anti-colorectal cancer agents requires careful selection of both molecular descriptors and validation protocols. While quantum chemical descriptors and 3D-field parameters provide valuable structural insights, the reliability of resulting models fundamentally depends on rigorous validation using LOO, LMO, and external test sets. Double cross-validation emerges as a particularly robust approach for estimating prediction errors under model uncertainty, addressing the critical issue of model selection bias that often plagues single-validation approaches. As QSAR methodologies continue to evolve, integrating these validation best practices with experimental verification will remain essential for accelerating the discovery of novel anti-CRC therapeutics with improved efficacy and selectivity profiles.
The pursuit of effective and safe cancer treatments has positioned Photodynamic Therapy (PDT) as a promising minimally invasive modality. PDT's effectiveness relies on three core components: a photosensitizer (PS) that accumulates in tumor tissue, light of a specific wavelength to activate the PS, and molecular oxygen to generate reactive oxygen species (ROS) that eradicate cancer cells [56]. Among various PS candidates, porphyrins and their derivatives have been extensively studied due to their excellent photosensitizing properties, biodegradability, and high singlet oxygen quantum yields [20] [56]. A significant challenge in porphyrin-based drug development is the optimization of their photodynamic activity, which is influenced by complex molecular properties including lipophilicity, steric factors, and electronic characteristics [20] [57].
Quantitative Structure-Activity Relationship (QSAR) modeling has emerged as a powerful computational approach to navigate this complexity, enabling researchers to correlate the structural features of porphyrins with their biological activity, specifically their half-maximal inhibitory concentration (IC~50~) [20] [58]. The reliability and predictive power of these models are critically dependent on rigorous validation techniques, with Leave-One-Out (LOO) and Leave-Many-Out (LMO) cross-validation standing as gold standards for assessing model robustness and predictive capability in cancer therapeutic research [59]. This case study examines the application of these cross-validation techniques in developing predictive QSAR models for porphyrin-based PDT agents, providing a framework for future drug development efforts.
Cross-Validation in QSAR: A Theoretical Framework
The Essential Role of Validation
In computational drug discovery, a QSAR model's value is determined not merely by its fit to existing data but by its ability to make accurate predictions for new, unseen compounds. Without proper validation, there is a high risk of developing models that are over-fitted to the training data, capturing noise rather than underlying structure-activity relationships, and consequently failing in prospective compound screening [59]. Cross-validation techniques provide a systematic methodology to estimate a model's predictive performance and ensure its applicability for chemical space exploration.
Leave-One-Out (LOO) and Leave-Many-Out (LMO) Techniques
LOO cross-validation involves iteratively removing one compound from the dataset, training the model on the remaining compounds, and then predicting the activity of the omitted compound. This process repeats until every compound in the dataset has been left out once. The predicted activities are then compared with the experimental values to calculate predictive metrics, most commonly Q² (QLOO²) [59].
LMO cross-validation, also known as k-fold cross-validation, extends this principle by leaving out a larger subset (or fold) of compounds at each iteration. This approach provides a more robust assessment of model stability, particularly for larger datasets, as it tests the model's performance on multiple, independent test sets [59]. For a QSAR model to be considered reliable and predictive, both LOO and LMO validation metrics should generally yield Q² values exceeding 0.5, with higher values indicating superior predictive capability [20] [59].
The following diagram illustrates the workflow for building and validating a robust QSAR model, integrating both LOO and LMO cross-validation techniques.
Case Study: QSAR Model for Cyclic Tetrapyrrole-Based Photosensitizers
Model Development and Validation Metrics
A seminal QSAR investigation developed a model to correlate the structural features of 36 porphyrin derivatives with their photodynamic therapy activity, expressed as Log(1/IC~50~) [20]. The dataset was partitioned into a training set of 24 compounds for model development and a test set of 12 compounds for initial internal validation. The model was constructed using Multiple Linear Regression Analysis (MLRA) and incorporated key molecular descriptors such as Verloop's steric parameter (B2), inertia moment, and VAMP octupole ZZY representing electronic properties [20].
The model's validation represents a textbook application of cross-validation protocols. The process and results are summarized in the table below.
Table 1: QSAR Model Validation Metrics for Porphyrin-Based Photosensitizers [20]
| Validation Metric | Value | Interpretation | Validation Type |
|---|---|---|---|
| Non-cross-validated r² | 0.87 | Excellent goodness-of-fit | Internal (Goodness-of-fit) |
| LOO cross-validated r² (CV) | 0.71 | Good internal predictive power | Internal (LOO-CV) |
| r² prediction (test set) | 0.70 | Consistent with LOO-CV result | Internal (Test set) |
| F-value | 37.85 | High statistical significance | Internal (Statistical test) |
| r² prediction (external test set) | 0.52 | Moderate external predictive ability | External (True validation) |
The LOO Q² value of 0.71 significantly exceeded the acceptability threshold of 0.5, providing strong evidence of the model's robustness and internal predictive power [20]. This was further corroborated by the test set prediction r² of 0.70. Finally, the model was challenged with an external test set of 20 porphyrin-based compounds with experimental IC~50~ values ranging from 0.39 μM to 7.04 μM, yielding a predictive correlation coefficient (r²) of 0.52 [20]. This external validation, while lower than the internal metrics, confirmed the model's practical utility for predicting the activity of new porphyrin analogs, successfully identifying new lead photosensitizers.
Key Structural Descriptors and Their Interpretation
The final QSAR model equation was expressed as: Log(1/IC~50~) = 0.96 × Verloop B2(subst.1) + 6.43 × inertia moment3length - 1.63 × VAMPoctupole ZZY + 0.72 [20]
Table 2: Key Molecular Descriptors in the Porphyrin QSAR Model [20]
| Molecular Descriptor | Descriptor Type | Correlation with Activity | Structural & Mechanistic Interpretation |
|---|---|---|---|
| Verloop B2 (subst.1) | Steric | Positive | Characterizes substituent width; bulkier groups may improve interaction with biological targets. |
| Inertia moment3 length | Shape-based | Positive | Related to molecular asymmetry; longer dimensions may favor cellular uptake or receptor binding. |
| VAMP octupole ZZY | Electronic | Negative | Represents electron distribution; specific electrostatic potentials may hinder photon absorption/ROS generation. |
Advanced Applications: Machine Learning and Metal Complexes
Machine Learning-Based Bioactivity Prediction
Advancements in computational power and algorithms have enabled the application of machine learning (ML) to larger and more complex datasets. A recent study compiled a dataset of 317 porphyrin derivatives from the ChEMBL database, calculating over 200 molecular descriptors to predict pIC~50~ (negative logarithm of IC~50~) [58]. The study emphasized the importance of data preprocessing, including the removal of duplicates and entries with missing values, to ensure model quality. After rigorous comparison of multiple algorithms, Logistic Regression emerged as the best-performing model, achieving 83% accuracy in classifying porphyrins as active or inactive [58]. This demonstrates the potent synergy between traditional QSAR descriptor analysis and modern machine learning classification techniques for rapid virtual screening of photosensitizers.
QSAR Modeling for Au(III) Porphyrin Complexes
QSAR approaches extend beyond organic porphyrins to include metalloporphyrins. A computational investigation into Au(III) porphyrin complexes as inhibitors for MCF-7 human breast cancer combined QSAR analysis with molecular docking and molecular dynamics simulations [60]. The study revealed that these complexes exhibited a strong binding affinity to specific cancer-related receptors (2JFR, 3HB5, and 4YTO), with the gold atom facilitating crucial hydrophobic interactions [60]. This integrated methodology highlights how QSAR models can provide insights into the mechanism of action, guiding the rational design of metal-based porphyrin therapeutics.
Experimental Protocols for Key Methodologies
Protocol 1: QSAR Model Development and Cross-Validation
This protocol outlines the core steps for building a validated porphyrin QSAR model, as applied in the featured case study [20] [59].
- Dataset Curation: Assemble a set of porphyrin derivatives (e.g., 36 compounds) with experimentally determined IC~50~ values for PDT activity.
- Data Division: Split the dataset into a training set (e.g., 2/3 of compounds) for model building and a test set (e.g., 1/3 of compounds) for initial internal validation.
- Descriptor Calculation: Compute a wide range of molecular descriptors (e.g., steric, electronic, topological) for all compounds using computational chemistry software.
- Feature Selection: Employ feature selection algorithms (e.g., Objective Feature Selection) to reduce the descriptor pool by removing constant and highly correlated descriptors.
- Model Building: Use a regression method (e.g., Multiple Linear Regression) on the training set to establish a mathematical relationship between selected descriptors and biological activity (Log(1/IC~50~)).
- Internal Validation:
- Perform Leave-One-Out (LOO) Cross-Validation: Iteratively remove one compound, rebuild the model, and predict its activity. Calculate the cross-validated correlation coefficient, r² (CV) or Q².
- Perform Leave-Many-Out (LMO) Cross-Validation: Repeat the process, leaving out a larger subset (e.g., 20-30% of compounds) in each iteration.
- Model Acceptance: Accept the model if both LOO and LMO Q² values are > 0.5, indicating good internal predictive power.
- External Validation: Use a completely independent external test set of porphyrins (e.g., 20 compounds) to evaluate the model's real-world predictive ability.
Protocol 2: Machine Learning-based Bioactivity Classification
This protocol describes the workflow for an ML-driven classification approach, suitable for larger datasets [58].
- Data Acquisition: Compile a large dataset of porphyrin-related molecules and their bioactivity data from public databases like ChEMBL.
- Data Preprocessing:
- Filter data to retain only entries with IC~50~ values in nM.
- Remove duplicate entries based on Molecule ChEMBL ID and Document ChEMBL ID.
- Drop entries with missing values in critical columns (e.g., SMILES).
- Classify molecules as "active" or "inactive" based on a defined IC~50~ threshold (e.g., 10,000 nM).
- Descriptor Calculation & Feature Analysis: Calculate molecular descriptors (e.g., using RDKit). Perform statistical analysis (e.g., correlation matrices) to identify the most impactful descriptors for bioactivity.
- Model Training & Evaluation:
- Split the preprocessed dataset into training and test sets.
- Train multiple machine learning classifiers (e.g., Logistic Regression, Random Forest, Support Vector Machines).
- Evaluate models based on accuracy, precision, recall, and other classification metrics to identify the best performer.
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Reagents and Computational Tools for Porphyrin QSAR Research
| Item Name | Function/Application | Example/Specification |
|---|---|---|
| Porphyrin Derivatives | Core molecules for building structure-activity models. | Tetraphenylporphyrin (TPP), Aminophenyl-TPP (ATPP), and their metal complexes (e.g., Au(III)) [20] [60]. |
| Computational Descriptors | Quantify structural features to correlate with activity. | Steric (Verloop parameters), Electronic (VAMP octupole), Topological (HallKierAlpha), and Drug-likeness (QED) descriptors [20] [58]. |
| QSAR/ML Software | Platform for descriptor calculation, model building, and validation. | RDKit (molecular manipulation), QSARINS (QSAR modeling), Scikit-Learn (machine learning algorithms) [58] [59]. |
| Validation Algorithms | Critical for assessing model predictability and robustness. | Leave-One-Out (LOO) and Leave-Many-Out (LMO) cross-validation scripts/modules [59]. |
| Public Bioactivity Databases | Source of experimental data for model training and testing. | ChEMBL database (provides IC~50~ values and molecular structures for porphyrins) [58]. |
This case study demonstrates that robust cross-validation is the cornerstone of reliable QSAR models for predicting the PDT activity of porphyrin-based therapeutics. The examined model, validated through LOO, LMO, and external testing, successfully established a quantitative link between key structural descriptors (steric, shape-based, and electronic) and photodynamic efficacy [20]. The transition to machine learning frameworks handling larger datasets further enhances the ability to classify and prioritize novel porphyrin structures efficiently [58]. The integration of QSAR with complementary computational techniques like molecular docking provides a more holistic understanding of the mechanistic interactions at play [60]. As the field advances, these rigorously validated computational models will continue to be indispensable tools for accelerating the rational design of next-generation, high-efficacy porphyrin photosensitizers for cancer therapy.
Integrating Cross-Validation with Machine Learning Algorithms (kNN, RF, SVM)
In the field of cancer research, Quantitative Structure-Activity Relationship (QSAR) modeling serves as a pivotal computational technique for predicting the biological activity and toxicity of chemical compounds based on their molecular structures. The primary goal is to accelerate the discovery of novel anticancer agents while reducing reliance on costly and time-consuming laboratory experiments. The central challenge in QSAR modeling lies in ensuring that developed models possess strong predictive power for new, unseen compounds, rather than simply memorizing the training data—a phenomenon known as overfitting. This is where robust validation techniques become indispensable.
Cross-validation represents a fundamental statistical approach for assessing how the results of a predictive model will generalize to an independent dataset. Within cancer QSAR research, proper validation is not merely a technical formality but a critical determinant of model reliability and translational potential. Model uncertainty is an inherent challenge in QSAR studies, as researchers often lack a priori knowledge about the optimal model configuration. The process requires both model selection (choosing the best-performing model from alternatives) and model assessment (evaluating its predictive performance on new data). Prediction errors are frequently used for both selecting and assessing models, but their reliable estimation requires independent test objects that play no role in model building or selection [7].
This guide provides a comprehensive comparison of how different machine learning algorithms—k-Nearest Neighbors (kNN), Random Forest (RF), and Support Vector Machines (SVM)—integrate with various cross-validation techniques, with a specific focus on their application in cancer QSAR research. We examine experimental protocols, performance metrics, and practical considerations for researchers developing reliable predictive models in oncological drug discovery.
Cross-Validation Techniques: LOO, LMO, and Double Cross-Validation
Core Cross-Validation Methods
Leave-One-Out (LOO) Cross-Validation involves iteratively using a single observation as the validation data and the remaining observations as training data. This process repeats such that each observation in the dataset serves as the validation sample exactly once. The primary advantage of LOO is its minimal bias in parameter estimation, as it maximizes training data usage. However, it tends to have high variance in prediction error estimation because the training sets are extremely similar across iterations. LOO is particularly suitable for small datasets where data conservation is critical [4].
Leave-Many-Out (LMO) Cross-Validation, more commonly known as k-fold cross-validation, partitions the original dataset into k equally sized subsets (folds). In each iteration, one fold is retained as validation data while the remaining k-1 folds form the training set. This process repeats k times, with each fold used exactly once as validation. Compared to LOO, LMO offers a better bias-variance trade-off, with typical k values ranging from 5 to 10. The k-fold method has demonstrated superior performance in cancer prediction tasks, providing a minimal mean absolute error score of 0.015 in oral cancer survival prediction compared to the hold-out method [61].
Advanced Validation: Double Cross-Vaidation
Double cross-validation (also called nested cross-validation) represents a more sophisticated approach that addresses model selection bias. This technique employs two nested cross-validation loops: an outer loop for model assessment and an inner loop for model selection [7].
The process works as follows:
- In the outer loop, data is repeatedly split into training and test sets
- The test set is exclusively used for final model assessment
- The training set enters the inner loop, where it is further split into construction and validation sets
- The construction sets build different models by varying tuning parameters
- The validation sets estimate model errors to select the optimal configuration
- The final model performance is assessed using the completely independent test set from the outer loop
Double cross-validation reliably and unbiasedly estimates prediction errors under model uncertainty for regression models. Compared to a single test set approach, it provides a more realistic picture of model quality and should be preferred [7]. This method has been successfully applied in QSAR modeling of HMG-CoA reductase inhibitors, where it provided better control of overfitting [4].
Table 1: Comparison of Cross-Validation Techniques in Cancer QSAR Research
| Technique | Key Advantages | Limitations | Typical Applications in Cancer QSAR |
|---|---|---|---|
| LOO | Maximizes training data, low bias | High computational cost, high variance | Small datasets (<100 compounds) |
| LMO (k-fold) | Better bias-variance trade-off | Requires sufficient data for folding | Medium to large datasets |
| Double CV | Unbiased error estimation, handles model selection | Computationally intensive | Complex models with parameter tuning |
| Hold-out | Simple implementation, fast | High variance, inefficient data use | Preliminary model screening |
Machine Learning Algorithms: Comparative Analysis
k-Nearest Neighbors (kNN) for Cancer Prediction
The kNN algorithm operates on the principle that similar compounds (neighbors) in chemical space exhibit similar biological activities. In cancer research, kNN has been successfully applied for both classification (e.g., categorizing cancer stages) and regression (e.g., predicting survival time) tasks [61].
A study predicting oral cancer patient survival time and stage classification demonstrated kNN's effectiveness when combined with k-fold cross-validation. The model achieved impressive performance metrics, with accuracy of 0.84, recall of 0.85, precision of 0.85, and F-measure of 0.84. Of 429 patient records, the model correctly classified 97 (out of 106), 99 (out of 119), 95 (out of 113), and 77 (out of 91) into their correct cancer stages 1, 2, 3, and 4, respectively [61].
kNN's performance is highly dependent on the choice of the distance metric and the value of k (number of neighbors). Comparative studies have shown that the Hassanat distance metric demonstrates superiority over traditional Manhattan and Euclidean distances, proving more invariant to data scale, noise, and outliers [62]. For optimal performance, researchers should employ ensemble approaches to determine the k parameter rather than relying on a fixed value [62].
Random Forest (RF) for QSAR Modeling
Random Forest is an ensemble learning method that constructs multiple decision trees during training and outputs the mode of classes (classification) or mean prediction (regression) of individual trees. RF excels in QSAR modeling due to its ability to handle high-dimensional descriptor spaces and capture non-linear relationships.
In anticancer QSAR modeling, RF has consistently demonstrated superior performance. A study developing QSAR models for flavone derivatives as anticancer agents found that the RF model achieved R² values of 0.820 for MCF-7 (breast cancer) and 0.835 for HepG2 (liver cancer) cell lines. The cross-validated R² (R²cv) values were 0.744 and 0.770, respectively. When validated using 27 test compounds, the model yielded root mean square error test values of 0.573 (MCF-7) and 0.563 (HepG2) [63].
Another QSAR study on benzoquinone derivatives as 5-lipoxygenase inhibitors (relevant to certain cancers) found that the RF model outperformed SVM and MLR approaches, showing excellent R², Q² (LMO), and R²pred values [64]. RF's built-in feature importance ranking also provides valuable insights into which molecular descriptors most significantly contribute to anticancer activity, aiding in rational drug design.
Support Vector Machines (SVM) in Cancer Research
SVM works by finding the optimal hyperplane that separates classes in a high-dimensional feature space. For non-linear separation, SVM employs kernel functions to transform data into higher dimensions. In cancer research, SVMs have been extensively used for classification tasks, including cancer type identification and compound activity prediction.
An optimized SVM approach for lung cancer classification, utilizing chameleon swarm optimization (CS-SVM), demonstrated remarkable performance with enhanced recognition accuracy, sensitivity, and specificity compared to conventional SVM [65]. Another study comparing multiple classifiers for lung cancer prediction found that SVM achieved 85% accuracy in classifying lung nodules, outperforming probabilistic neural networks (82%) and k-means clustering (81%) [65].
However, SVM performance is highly dependent on proper parameter selection, particularly the choice of kernel function and regularization parameters. Studies have shown that Bayesian optimization of SVM parameters is more effective than random search for lung nodule classification in computer-aided diagnosis systems [65]. When comparing SVM to other algorithms for diabetes prediction (as a proxy for disease prediction tasks), Random Forest delivered better performance, suggesting that SVM may be outperformed by ensemble methods in some biological applications [62].
Table 2: Performance Comparison of ML Algorithms in Cancer-Related Prediction Tasks
| Algorithm | Best Reported Accuracy | Key Strengths | Optimal CV Strategy |
|---|---|---|---|
| kNN | 84-85% (oral cancer staging) [61] | Simple, interpretable, no training phase | k-fold cross-validation |
| Random Forest | 82-83.5% R² (anticancer flavones) [63] | Handles high dimensions, feature importance | Double cross-validation |
| SVM | 85-97% (lung cancer classification) [65] | Effective in high-dimensional spaces | Nested CV with parameter optimization |
Experimental Protocols and Methodologies
Data Preprocessing and Feature Selection
The foundation of reliable QSAR models begins with rigorous data preprocessing and thoughtful feature selection. Molecular structures typically undergo standardization procedures including neutralization, removal of explicit hydrogens, and tautomerization to ensure consistency [66]. Subsequently, molecular descriptors or fingerprints are generated to numerically represent structural characteristics.
In a comprehensive target identification model comprising 1,121 target SAR models built using Random Forest, researchers employed extended-connectivity fingerprints (ECFP_4) with a 2,048-bit length string to represent molecular structures [66]. To address class imbalance between active and inactive compounds—a common challenge in chemical databases—they applied both negative-undersampling (randomly selecting a subset of inactive ligands) and positive-oversampling (by imposing larger weights on active ligands during training) [66].
Feature selection techniques are crucial for enhancing model interpretability and performance. Recursive feature elimination and feature importance ranking based on tree-based models have proven effective. One study incorporating both structural and biological information found that using only the five most relevant molecular descriptors combined with one key gene expression marker (metallothionein) yielded optimal predictive performance for non-genotoxic carcinogenicity [67].
Implementation of Cross-Validation Protocols
The implementation details of cross-validation significantly impact model performance estimates. For double cross-validation, parameters in the inner loop mainly influence the bias and variance of resulting models, while parameters in the outer loop mainly affect the variability of prediction error estimates [7].
A recommended protocol for cancer QSAR models includes:
- Outer loop: 10-fold cross-validation for model assessment
- Inner loop: 5-fold cross-validation for model selection
- Multiple repetitions with different random seeds to assess stability
- Stratified sampling to maintain class distribution in each fold
For the HMG-CoA reductase inhibitor QSAR models, researchers created 300 models using nested cross-validation as the primary validation method, selecting 21 that demonstrated good performance (R² ≥ 0.70 or concordance correlation coefficient ≥ 0.85) [4]. This rigorous approach ensured robust performance estimation and minimized overfitting.
Performance Evaluation Metrics
Comprehensive model evaluation requires multiple metrics to assess different aspects of predictive performance:
- Regression tasks: R², Q² (cross-validated R²), mean absolute error (MAE), root mean square error (RMSE)
- Classification tasks: Accuracy, sensitivity, specificity, precision, F-measure, AUC-ROC
- Model robustness: Y-randomization test (to confirm model isn't fitting to noise)
In cancer survival prediction, one study reported MAE scores as low as 0.015 using k-fold cross-validation with kNN [61]. For classification of lung cancer nodules, performance metrics included sensitivity (92%), specificity (97.3%), and accuracy (97%) using optimized SVM [65].
Comparative Performance Analysis
Direct Algorithm Comparisons
Direct comparisons of kNN, RF, and SVM in disease prediction tasks provide valuable insights for researchers selecting algorithms for cancer QSAR models. A comprehensive comparative performance analysis of kNN and its variants for disease prediction found that the optimal kNN implementation can compete with more complex algorithms, particularly when using advanced distance metrics and optimized k values [62].
Another study comparing machine learning approaches for diabetes prediction found that Random Forest delivered the best performance, with an accuracy of 96%, surpassing both kNN and SVM [62]. This aligns with findings from anticancer QSAR modeling, where RF consistently demonstrates superior predictive ability and robustness [63] [64].
However, algorithm performance is highly context-dependent. For lung cancer classification, one study found that a chameleon swarm-optimized SVM achieved superior performance compared to other approaches [65]. Similarly, another study comparing multiple classifiers found that an artificial neural network achieved the highest accuracy (96%) for lung cancer prediction, followed by SVM [65].
Impact of Cross-Validation on Model Performance
The choice of cross-validation technique significantly impacts performance estimates and model selection. One study systematically investigating regression models with variable selection found that prediction errors of QSAR models depend largely on the parameterization of double cross-validation [7].
The same study demonstrated that double cross-validation provides more realistic performance estimates compared to single test set validation. While the hold-out method may provide optimistically biased performance estimates, double cross-validation offers unbiased estimation of prediction errors under model uncertainty [7].
In practical applications, the k-fold cross-validation method has been shown to outperform the hold-out method for kNN in cancer prediction, providing the least mean absolute error score of 0.015 [61]. For complex models with extensive parameter tuning, nested cross-validation is essential to avoid model selection bias and obtain reliable performance estimates for new compounds.
Table 3: Experimental Protocols for Cross-Validation in Cancer QSAR Studies
| Protocol Step | kNN Recommendations | RF Recommendations | SVM Recommendations |
|---|---|---|---|
| Data Preprocessing | Feature scaling, distance metric selection | Handle missing values, imbalance correction | Feature scaling, kernel selection |
| Validation Scheme | k-fold CV (k=5-10) | Double CV with feature importance | Nested CV with parameter optimization |
| Key Parameters | k neighbors, distance metric | Number of trees, tree depth | Kernel type, C, gamma |
| Performance Metrics | Accuracy, F-measure, MAE | R², RMSE, feature importance | Sensitivity, specificity, AUC |
Research Toolkit and Experimental Workflows
Essential Research Reagents and Computational Tools
Successful implementation of QSAR models in cancer research requires both computational tools and experimental resources:
Table 4: Essential Research Toolkit for Cancer QSAR Modeling
| Tool/Resource | Function | Example Applications |
|---|---|---|
| Chemical Databases | Source of bioactive compounds | ChEMBL, PubChem, ZINC [66] |
| Descriptor Calculation | Molecular representation | DRAGON, RDKit, PaDEL [67] |
| Machine Learning Libraries | Model implementation | scikit-learn, MLR3, WEKA [4] |
| Validation Frameworks | Performance estimation | Double CV implementation, Y-randomization [7] |
| Visualization Tools | Results interpretation | Matplotlib, Plotly, Chemical space maps [4] |
Integrated Workflow for Cancer QSAR Modeling
The following workflow diagram illustrates a robust methodology integrating cross-validation with machine learning algorithms for cancer QSAR models:
Cancer QSAR Modeling with Double Cross-Validation
This workflow emphasizes the critical importance of keeping test data completely separate from model selection processes to obtain unbiased performance estimates—a key advantage of the double cross-validation approach [7].
Integrating appropriate cross-validation strategies with machine learning algorithms is fundamental to developing reliable QSAR models in cancer research. Our comparative analysis demonstrates that each algorithm—kNN, RF, and SVM—has distinct strengths and optimal application scenarios in oncological informatics.
Random Forest consistently demonstrates superior performance in many anticancer QSAR tasks, particularly with its robust handling of high-dimensional descriptors and built-in feature importance metrics [63] [64]. However, kNN remains competitive for specific applications, especially when using optimized distance metrics and ensemble approaches for parameter selection [62]. SVM excels in classification tasks with clear margins of separation but requires careful parameter tuning [65].
The cross-validation technique should be selected based on dataset size and model complexity. While k-fold cross-validation generally outperforms simple hold-out validation [61], double cross-validation represents the gold standard for complex models with parameter optimization, providing unbiased error estimation under model uncertainty [7].
Future directions in cancer QSAR modeling include increased integration of biological data beyond chemical structures [67], application of deep learning architectures [68], and development of automated machine learning pipelines to streamline model development and validation. As AI continues transforming drug discovery [68], robust validation practices will become increasingly critical for translating computational predictions into clinically effective cancer therapeutics.
Researchers should prioritize implementation of rigorous validation protocols, particularly double cross-validation, to ensure their QSAR models generate reliable predictions that can genuinely accelerate anticancer drug discovery and development.
Addressing Pitfalls and Optimizing Cross-Validation Strategies for Robust Cancer Models
The Model Selection Bias Problem and Overfitting in LOO Validation
Quantitative Structure-Activity Relationship (QSAR) modeling represents a cornerstone approach in modern computational drug discovery, establishing quantitative relationships between structural features of molecules and their biological activities [7] [6]. These models are particularly valuable in cancer research for predicting the efficacy of potential therapeutic compounds, prioritizing synthesis candidates, and reducing experimental costs [69] [12]. The fundamental challenge in QSAR modeling lies in ensuring that developed models possess true predictive power for new, unseen compounds rather than merely fitting the existing data [7] [1].
Cross-validation techniques serve as essential tools for estimating the predictive performance of QSAR models, with Leave-One-Out (LOO) and Leave-Many-Out (LMO) representing two predominant approaches [6]. While LOO cross-validation uses nearly all available data for training and provides low-variance error estimates, it faces significant criticism regarding potential overfitting and model selection bias, especially when dealing with complex models and large descriptor pools [7] [6]. This comprehensive analysis examines these critical limitations within the context of cancer QSAR research and evaluates advanced validation methodologies that address these fundamental challenges.
The Theoretical Framework of Model Selection Bias
Understanding Model Selection Bias
Model selection bias represents a fundamental pitfall in QSAR validation that occurs when the same data guides both model selection and error estimation [7] [18]. This phenomenon arises because validation objects, while independent of model building, are not independent of the model selection process [7]. The predictions of these validation objects collectively influence the search for an optimal model, creating an inherent bias in the resulting error estimates [7] [18].
In technical terms, model selection bias frequently causes overly optimistic internal validation results while yielding poor generalization performance on truly external datasets [7]. This discrepancy stems from the tendency to select models that capitalize on chance correlations within the specific dataset rather than capturing true structure-activity relationships [7] [1]. The bias is particularly pronounced in high-dimensional descriptor spaces where the ratio of descriptors to compounds is unfavorable, a common scenario in QSAR modeling [6] [70].
Overfitting in LOO Validation
Leave-One-Out cross-validation suffers from specific vulnerabilities to overfitting, especially when dealing with complex models and large descriptor pools [7] [6]. The core issue lies in LOO's tendency to select overly complex models that include irrelevant variables while providing deceptively favorable validation metrics [7]. These models adapt to noise in the training data, resulting in poor performance when applied to genuine external compounds [7] [14].
The overfitting problem exacerbates when researchers employ multiple model types and descriptor combinations without proper validation safeguards [7] [1]. Each additional model variant increases the probability of identifying a seemingly high-performing model by chance alone, especially when validation lacks true independence from the selection process [7]. This scenario commonly occurs in cancer QSAR studies where researchers explore diverse molecular descriptors ranging from topological indices to quantum chemical parameters [24] [12].
Comparative Analysis of Validation Techniques
Methodological Approaches
Table 1: Comparison of Cross-Validation Techniques in QSAR Modeling
| Validation Method | Key Characteristics | Advantages | Limitations | Typical Applications |
|---|---|---|---|---|
| Leave-One-Out (LOO) | Iteratively removes one compound; uses remaining n-1 compounds for training | Uses maximum data for training; low variance estimate | High computational cost; prone to overfitting; model selection bias | Small datasets (<50 compounds); initial screening models |
| Leave-Many-Out (LMO) | Removes a subset (20-30%) of compounds each iteration | More realistic error estimate; reduced overfitting | Higher variance; multiple iterations needed | Medium to large datasets; model optimization |
| Double Cross-Validation | Nested loops: outer for assessment, inner for model selection | Unbiased error estimation; handles model uncertainty | Computationally intensive; complex implementation | Final model validation; high-stakes predictions |
| Hold-Out Validation | Single split into training/test sets (typically 80/20) | Simple implementation; computationally fast | High variability; inefficient data use | Very large datasets; preliminary assessment |
Quantitative Performance Comparison
Table 2: Empirical Performance Metrics of Validation Methods in Cancer QSAR Studies
| Research Context | Validation Method | Reported R² | Q²/Internal Validation | External Prediction Accuracy | Reference |
|---|---|---|---|---|---|
| Anti-colorectal cancer agents | LOO-CV | 0.849 (training) | Not specified | Not reported | [24] |
| PI3Kγ inhibitors (245 compounds) | LOO with variable selection | 0.623-0.642 | Q²LOO = 0.600 | RMSE = 0.464-0.473 | [70] |
| Tubulin inhibitors for breast cancer | LOO on training set | 0.849 | Not specified | R²test = 0.81 (limited test set) | [12] |
| Juvenile hormone activity modeling | Double Cross-Validation | Less variable estimates | More reliable than single split | Superior to hold-out sample | [6] |
The experimental data reveals a critical pattern: while LOO validation often generates favorable internal metrics (R² > 0.8 in multiple studies), these results frequently overstate real-world predictive performance [12] [6]. The PI3Kγ inhibitor study exemplifies this discrepancy, where robust internal validation (Q²LOO = 0.600) nonetheless resulted in moderate external prediction accuracy (RMSE = 0.464-0.473) [70]. This consistent observation across multiple cancer QSAR domains underscores the necessity of more rigorous validation approaches.
Double Cross-Validation: A Robust Alternative
Theoretical Foundation and Workflow
Double cross-validation, also termed nested cross-validation, provides a sophisticated framework that directly addresses model selection bias [7] [18]. This methodology employs two nested validation loops: an inner loop for model selection and parameter tuning, and an outer loop exclusively for model assessment [7] [18]. This strict separation ensures that test data in the outer loop remains completely independent of both model building and selection processes, yielding unbiased error estimates [7].
The fundamental strength of double cross-validation lies in its efficient data utilization while maintaining statistical integrity [7]. Unlike single-split validation methods that sacrifice substantial data for testing, double cross-validation leverages the entire dataset for both model development and validation through systematic partitioning [7] [6]. This approach becomes particularly valuable in cancer QSAR research where compound data is often limited and costly to obtain [69] [12].
Diagram Title: Double Cross-Validation Workflow
Implementation Protocol
The standard implementation protocol for double cross-validation in cancer QSAR studies involves these critical stages:
Outer Loop Configuration: Partition the complete dataset into k-folds (typically 5-10), reserving each fold iteratively as the test set [7]. This outer loop provides the definitive assessment of model performance on truly independent data [7] [18].
Inner Loop Optimization: For each outer training set, implement a separate cross-validation cycle to optimize model parameters and select the best-performing configuration [7]. This inner loop typically employs LOO or LMO validation but confines the selection process exclusively to the training partition [7].
Performance Aggregation: After completing all outer iterations, aggregate the prediction errors from each test set to compute comprehensive performance metrics [7] [18]. This aggregated estimate accurately reflects expected performance on new compounds [7].
Final Model Construction: Using the optimal parameters identified through the double cross-validation process, construct the final model using the entire dataset [7]. This model benefits from both robust parameter selection and maximum data utilization [7] [6].
Experimental Case Studies in Cancer Research
Tubulin Inhibitors for Breast Cancer Therapy
A recent QSAR study on 1,2,4-triazine-3(2H)-one derivatives as tubulin inhibitors for breast cancer therapy demonstrated both the prevalence and implications of validation limitations [12]. Researchers developed QSAR models using multiple linear regression (MLR) with 24 molecular descriptors, reporting a training correlation coefficient of R² = 0.849 [12]. While the authors employed an 80:20 train-test split, the limited test set size (approximately 6 compounds) raises concerns about validation reliability [12].
The study's molecular descriptors included quantum chemical parameters (EHOMO, ELUMO, electronegativity) and topological descriptors (Wiener index, polar surface area) [12]. Despite favorable internal metrics, the external predictive power remains uncertain without larger validation cohorts [12] [1]. This case exemplifies how cancer QSAR studies with promising internal validation may benefit from more rigorous double cross-validation approaches [7].
Selective Survivin Inhibitors Design
Research on survivin inhibitors for breast cancer therapy employed 2D-QSAR methods on 31 hydroxyquinoline-derived compounds [69]. The study developed multivariate linear regression models incorporating steric, electronic, and topological descriptors to predict inhibitory activity (pIC50) [69]. While the authors complemented QSAR with molecular docking and dynamics simulations, the internal validation methodology leaves potential for model selection bias [69] [1].
Notably, this research designed nine novel compounds predicted to exhibit enhanced survivin inhibitory activity based on the QSAR models [69]. Such predictive applications underscore the critical importance of reliable validation, as flawed models directly impact experimental resource allocation and drug development decisions [69] [1].
PI3Kγ Inhibitors Modeling
A comprehensive QSAR analysis on 245 potent PI3Kγ inhibitors addressed validation challenges through sophisticated methodology [70]. Researchers implemented both multiple linear regression (MLR) and artificial neural network (ANN) approaches, validating models through external and internal validation methods [70]. The reported metrics (R² = 0.623-0.642, Q²LOO = 0.600) reflect moderate predictive capability, while y-randomization testing (R²y-random = 0.011) confirmed model robustness [70].
This large-scale study demonstrates appropriate validation practices, including external verification using structurally diverse compounds outside the training set [70]. The authors noted that ANN models demonstrated superior performance to MLR, highlighting how model selection itself represents a source of potential bias requiring careful validation [70].
The Researcher's Toolkit: Essential Methodological Solutions
Table 3: Essential Research Reagents and Computational Tools for Robust QSAR Validation
| Resource/Tool | Category | Specific Function | Validation Application | Representative Examples |
|---|---|---|---|---|
| QSARINS Software | Statistical Analysis | MLR-based QSAR model development with advanced validation | Implements double cross-validation; calculates consensus metrics | Tuberculosis drug discovery [71] |
| Double Cross-Validation | Validation Protocol | Nested validation for unbiased error estimation | Addresses model selection bias; provides realistic performance estimates | Juvenile hormone activity modeling [6] |
| Y-Randomization Test | Statistical Test | Assesses chance correlation risk | Validates model robustness; ensures structural basis of activity | PI3Kγ inhibitor modeling [70] |
| Applicability Domain | Validation Framework | Defines chemical space for reliable predictions | Identifies extrapolation risks; flags unreliable predictions | SARS-CoV-2 Mpro inhibitors [1] |
| Molecular Descriptors | Input Variables | Quantifies structural and chemical properties | Topological, electronic, quantum chemical parameters | Anti-colorectal cancer agents [24] |
Implementation Guidelines for Cancer QSAR Studies
Based on empirical evidence across multiple studies, researchers should adopt these essential practices to mitigate overfitting and selection bias:
Implement Double Cross-Validation: For definitive model assessment, employ double cross-validation with appropriate partitioning (typically 5-10 folds in outer loop) [7] [18]. This approach provides the most reliable estimate of real-world performance while using data efficiently [7] [6].
Apply Y-Randomization: Routinely perform y-randomization tests to verify that models capture true structure-activity relationships rather than chance correlations [70] [1]. Significant degradation in randomized models confirms meaningful relationships [70].
Define Applicability Domain: Explicitly characterize the chemical space where models provide reliable predictions [1]. This practice identifies compounds requiring special caution and improves decision-making in virtual screening [1].
Utilize Multiple Validation Splits: When using single-split validation, implement multiple random splits to assess result stability [7] [6]. This approach reduces the influence of fortuitous partitioning on performance estimates [7].
Report Comprehensive Metrics: Provide both internal (Q²LOO) and external (R²test, RMSE) validation metrics with complete methodological transparency [70] [12]. This practice enables proper evaluation and comparison across studies [70].
Diagram Title: Robust QSAR Validation Strategy
The model selection bias problem and overfitting in LOO validation represent significant methodological challenges in cancer QSAR research. Empirical evidence consistently demonstrates that conventional LOO validation often produces overly optimistic performance estimates that fail to generalize to external compounds [7] [6] [70]. This discrepancy directly impacts drug discovery efficiency by misleading resource allocation and compound prioritization [69] [1].
Double cross-validation emerges as the methodologically superior approach, providing unbiased error estimates while efficiently utilizing available data [7] [18] [6]. Despite its computational intensity, this nested validation framework directly addresses the fundamental limitations of single-level validation by strictly separating model selection from assessment [7] [18]. The technique proves particularly valuable in cancer QSAR applications where dataset sizes are frequently limited and model reliability critically impacts experimental decisions [69] [12].
Future methodological developments should focus on integrating multiple validation perspectives, combining rigorous statistical approaches with mechanistic understanding [14] [1]. Additionally, standardized reporting of validation methodologies and comprehensive performance metrics will enhance comparability and reliability across cancer QSAR studies [70] [1]. As QSAR applications expand in cancer drug discovery, addressing these fundamental validation challenges remains essential for translating computational predictions into therapeutic advances.
In the field of Quantitative Structure-Activity Relationship (QSAR) modeling, particularly within cancer research, the leave-one-out (LOO) cross-validation statistic (q²) has been traditionally hailed as a gold standard for estimating model predictive ability. A q² value greater than 0.5 is frequently considered indicative of a robust model. However, a growing body of evidence reveals that a high q² can be a dangerously misleading metric, offering an over-optimistic view of model performance due to inherent biases and its inability to fully capture model uncertainty. This article delves into the statistical underpinnings of this phenomenon, contrasts LOO with more rigorous validation techniques like leave-many-out (LMO) and double cross-validation, and provides a structured guide for researchers to adopt more reliable practices in developing QSAR models for anti-cancer drug discovery.
The Deception of the High q² Value
The Allure and the Trap
The widespread adoption of the LOO q² value is rooted in its intuitive appeal. It provides a single, seemingly robust number that appears to validate a model's predictive power using all available data. In LOO, a model is built repeatedly, each time using all data points except one, which is then predicted. The q² is calculated from these predictions. However, this process is susceptible to model selection bias and overfitting, especially under model uncertainty where the optimal model structure is not known a priori [7].
The core of the problem lies in the fact that the LOO procedure uses nearly the entire dataset for both model building and validation in each cycle. This minimal perturbation between training and validation sets can lead to an over-optimistic estimation of predictive error because the model is never truly tested on a substantially independent dataset. Consequently, a model with a high q² may perform poorly when confronted with genuinely new external compounds [19] [7].
The Critical Gap: Internal vs. External Predictivity
A fundamental distinction in QSAR validation is between internal and external predictivity. The q² is a measure of internal predictivity. Research has consistently demonstrated a weak correlation between high internal q² values and a model's performance on an external test set [19]. A study analyzing 44 reported QSAR models found that relying on the coefficient of determination (r² or q²) alone is insufficient to indicate the validity of a QSAR model [19]. Some models with satisfactory q² values exhibited poor external predictivity, as evidenced by low values for external validation parameters like R²ext and Q²-Fn [19]. This disconnect underscores that a high q² does not guarantee a model's utility in practical drug discovery scenarios, such as predicting the activity of newly designed anti-cancer agents.
Superior Validation Paradigms: LMO and Double Cross-Validation
To overcome the limitations of LOO, the QSAR field has moved towards more robust validation protocols that provide a more realistic assessment of model performance on unseen data.
Leave-Many-Out (LMO) Cross-Validation
LMO, also known as k-fold cross-validation, involves repeatedly splitting the data into a training set and a larger, held-out test set (e.g., leaving out 20-30% of the data in each iteration). This approach provides a better simulation of how a model will perform on truly external data.
Experimental Protocol for LMO:
- Randomly partition the dataset of N compounds into k roughly equal-sized folds.
- For each fold i (i=1 to k):
- Retain fold i as the temporary validation set.
- Use the remaining k-1 folds as the training set.
- Build the QSAR model using the training set.
- Predict the compounds in the validation set.
- Collect all predictions and calculate the LMO cross-validated correlation coefficient (Q²LMO) and other error metrics (e.g., RMSEcv).
The value of LMO is evident in modern QSAR studies. For instance, in a model developed for 219 MDA-MB-231 triple-negative breast cancer cell antagonists, the reported Q²LMO values (0.76–0.77) were notably close to the Q²LOO value (0.77) [72]. This consistency strengthens the credibility of the model's internal predictive ability, a reassurance that is often missing when only LOO is reported.
Double Cross-Validation
Double cross-validation (or nested cross-validation) is a comprehensive technique that integrates model selection and model assessment in a single, rigorous workflow [7]. It is considered one of the most reliable methods for estimating prediction errors under model uncertainty.
Experimental Protocol for Double Cross-Validation: The process consists of two nested loops:
- Outer Loop (Model Assessment): The data is split into training and test sets. The test set is used exclusively for the final evaluation and is never involved in model building or selection.
- Inner Loop (Model Selection): The training set from the outer loop is further split into construction and validation sets. This inner loop performs a full cross-validation (e.g., LMO) to tune model parameters and select the optimal model. The model with the best performance in the inner loop is then passed to the outer loop.
- The selected model is used to predict the untouched test set from the outer loop. This process is repeated many times with different splits.
The power of double cross-validation is that it provides an almost unbiased estimate of the prediction error because the data used for final assessment (the outer test set) are completely independent of the model selection process [7]. A systematic study confirmed that double cross-validation "reliably and unbiasedly estimates prediction errors under model uncertainty for regression models" and "should be preferred over a single test set" as it provides a more realistic picture of model quality [7].
Table 1: Comparison of QSAR Cross-Validation Techniques
| Validation Method | Procedure | Key Advantage | Key Limitation | Typical Use Case |
|---|---|---|---|---|
| Leave-One-Out (LOO) | Iteratively removes one compound, models the rest, and predicts the omitted one. | Efficient with very small datasets. | High risk of over-optimism; poor estimator of external predictivity. | Initial, quick internal check (with caution). |
| Leave-Many-Out (LMO) | Iteratively removes a substantial fraction (e.g., 20%) of data for validation. | Better simulation of external prediction; more reliable error estimate. | Higher computational cost than LOO. | Standard for robust internal validation. |
| Double (Nested) CV | Uses an outer loop for assessment and an inner loop for model selection. | Unbiased error estimation under model uncertainty; validates the modeling process. | Computationally intensive; complex to implement. | Gold standard for reliable error estimation and model selection. |
The following diagram illustrates the logical workflow for selecting a validation strategy, emphasizing the superiority of double cross-validation for reliable error estimation.
Figure 1: A decision workflow for selecting appropriate QSAR validation strategies, leading to the most reliable practices.
Case Studies in Cancer Research
TNBC QSAR Models Setting a Robust Example
A 2021 QSAR study on 219 Triple-Negative Breast Cancer (TNBC) cell antagonists exemplifies rigorous validation [72]. The researchers employed GA-MLR (Genetic Algorithm-Multi Linear Regression) and adhered to OECD guidelines, moving beyond a single q² metric.
Table 2: Statistical Parameters from a Validated TNBC QSAR Model [72]
| Statistical Parameter | Model 1.1 Value | Model 1.2 Value | Interpretation |
|---|---|---|---|
| R² | 0.79 | 0.79 | Good fit to the training data. |
| Q²LOO | 0.77 | 0.77 | High internal LOO predictivity. |
| Q²LMO | 0.77 | 0.76 | Confirms robustness, similar to Q²LOO. |
| R²ext | 0.72 | 0.76 | Good external predictivity - the true test. |
| Q²-F1 | 0.72 | 0.76 | Further confirmation of external predictive power. |
This case demonstrates a model where a high Q²LOO was corroborated by high Q²LMO and, most importantly, strong external validation metrics (R²ext, Q²-Fn). The key takeaway is not to dismiss a high q², but to demand accompanying evidence from LMO and external validation.
Machine Learning and Double Cross-Validation in Colorectal Cancer
A 2025 study aimed at identifying Tankyrase inhibitors for colon adenocarcinoma integrated machine learning with QSAR [73]. The authors built a Random Forest classification model using a dataset of 1100 inhibitors. To ensure high predictive performance and avoid overfitting, they rigorously validated their model using internal (cross-validation) and external test sets, achieving a high predictive performance (ROC-AUC of 0.98) [73]. This use of a held-out external test set is a direct application of the principle underlying double cross-validation and provides a credible assessment of the model's real-world utility.
The Scientist's Toolkit: Essential Reagents for Robust QSAR
Table 3: Key Research Reagent Solutions for QSAR Modeling
| Reagent / Software Category | Example | Function in QSAR Modeling |
|---|---|---|
| Descriptor Calculation Software | Dragon Software | Calculates thousands of molecular descriptors (2D/3D) and fingerprints from molecular structure [19]. |
| Chemical Databases | ChEMBL | Provides curated, publicly available bioactivity data for diverse targets (e.g., TNKS2 inhibitors) to build training sets [73]. |
| Machine Learning & Statistical Modeling | R, Python (scikit-learn) | Provides environments for implementing ML algorithms, variable selection (e.g., Genetic Algorithm), and cross-validation [72] [73]. |
| Validation & Benchmarking Tools | Double Cross-Validation Scripts | Custom scripts (e.g., in R/Python) to implement nested validation protocols for reliable error estimation [7]. |
The pursuit of a high q² > 0.5 is not inherently flawed, but treating it as a standalone measure of model quality is a critical error in scientific judgment. For QSAR models in cancer research, where accurate prediction of new anti-cancer agents is paramount, reliance on LOO can lead to costly failures in subsequent experimental validation.
A robust QSAR validation protocol must be multi-faceted:
- Use LOO with Caution: Treat Q²LOO as an initial, but not definitive, internal check.
- Mandate LMO Cross-Validation: Always report Q²LMO. A model is more trustworthy when Q²LOO and Q²LMO values are consistent.
- Prioritize External Validation: The most critical step is to test the final model on a completely independent, blinded external test set and report metrics like R²ext and Q²-Fn.
- Embrace Double Cross-Validation: For the most reliable estimate of a model's future performance, especially when model selection is involved, implement double cross-validation.
- Adhere to OECD Principles: Follow established guidelines, which emphasize the need for a defined endpoint, an unambiguous algorithm, and appropriate measures of goodness-of-fit, robustness, and predictivity.
By moving beyond the deceptive comfort of a high q² and adopting these rigorous validation practices, researchers in drug development can build more reliable and predictive QSAR models, ultimately accelerating the discovery of effective cancer therapeutics.
Quantitative Structure-Activity Relationship (QSAR) modeling is a computational technique that establishes correlations between chemical structures and biological activities, widely employed in rational drug design and toxicity prediction [74]. In cancer research, particularly for modeling compounds against cell lines like MDA-MB-231 (triple-negative breast cancer) and SK-MEL-5 (melanoma), model uncertainty is a significant challenge due to the vast number of molecular descriptors and relatively limited biological testing data [41] [75]. Double cross-validation (DCV), also termed nested cross-validation, offers a robust solution to this problem by providing reliable estimation of prediction errors under model uncertainty [18] [7].
The fundamental principle behind DCV is its two-layered validation structure that strictly separates model selection from model assessment. This separation is critical because using the same data for both selecting optimal hyperparameters and evaluating final model performance leads to optimistically biased results, a phenomenon known as model selection bias [18] [7]. For cancer QSAR models, where selecting relevant molecular descriptors from thousands of possibilities is inherent to model development, this bias can be substantial, leading to models that perform well during development but fail in prospective prediction of new anti-cancer compounds [18] [41].
Compared to single test-set validation (hold-out method), DCV uses data more efficiently—a crucial advantage when working with limited cancer screening data. While the hold-out method requires large test sets for reliable error estimates, DCV provides more precise estimates through repeated sampling, making it particularly suitable for typical QSAR datasets in cancer research [18] [7]. As noted in studies of anti-melanoma compounds, DCV provides "a more realistic picture of model quality and should be preferred over a single test set" [7].
The Mechanism of Double Cross-Validation
Architectural Framework
Double cross-validation consists of two nested loops: an inner loop for model building and parameter tuning, and an outer loop for model assessment. This structure ensures complete separation between the model selection process and the final evaluation, preventing information leakage that would artificially inflate performance metrics [18] [76] [7].
In the outer loop, the entire dataset is repeatedly split into training and test sets. The test sets are exclusively used for final model assessment and play no role in model selection. For each training-test split in the outer loop, the inner loop performs another round of cross-validation on the training data only. This inner CV is responsible for model building and hyperparameter optimization through variable selection, descriptor weighting, or algorithm parameter tuning [18] [74].
The model with the best performance in the inner loop is selected and then evaluated on the test set from the outer loop. This process repeats for multiple splits in the outer loop, with the final performance estimate calculated as the average across all test sets [76] [7]. This approach "validates the process to arrive at a final model rather than a final model itself" [7].
Workflow Visualization
The following diagram illustrates the complete double cross-validation process as applied to QSAR model development:
Diagram 1: Double Cross-Validation Workflow for QSAR Modeling. This illustrates the nested structure with separate inner and outer loops for model selection and assessment, respectively.
Comparison with Single Cross-Validation
The critical difference between single (non-nested) and double cross-validation lies in their handling of model selection bias. In single CV, the same data guides both parameter tuning and performance estimation, leading to overoptimistic results. A scikit-learn example demonstrated this bias clearly, showing "an average difference of 0.007581 between non-nested and nested CV scores" [76]. While this difference may seem small, in cancer QSAR contexts where models prioritize compounds for costly synthesis and testing, even minor biases can significantly impact resource allocation and decision-making.
Application in Cancer QSAR Research
Implementation in Anti-Cancer Drug Discovery
Double cross-validation has been successfully implemented across various cancer QSAR studies, particularly in models predicting anti-proliferative activity against specific cancer cell lines. For SK-MEL-5 melanoma cell line antagonists, researchers developed 186 QSAR models using multiple machine learning classifiers, with double cross-validation ensuring reliable performance estimates [41]. The models incorporated 13 blocks of molecular descriptors, from topological indices to edge-adjacency indices, with rigorous preprocessing to remove constant, near-constant, and highly correlated variables [41].
In triple-negative breast cancer research, DCV was employed for QSAR modeling of 219 MDA-MB-231 cell antagonists. The models achieved impressive validation statistics (R² = 0.79, Q²LOO = 0.77, Q²LMO = 0.76-0.77), demonstrating the robustness attainable through proper validation [75]. Similarly, in optimizing antiproliferative activity of substituted phenyl benzenesulfonates against skin melanoma M-21 cells, multiple QSAR models were built and validated according to OECD principles using thorough internal and external validation with Y-randomization [77].
Experimental Protocols and Methodologies
Data Preparation and Preprocessing:
- Dataset Curation: Collect bioactivity data from reliable sources like PubChem, with cytotoxicity expressed as GI50 or IC50 values converted to pIC50 (-log10 IC50) for modeling [41] [77].
- Structure Standardization: Standardize molecular structures using tools like ChemAxon Standardizer, remove duplicates, and convert to 2D chemical structures [41].
- Descriptor Calculation: Compute multiple blocks of molecular descriptors using software like Dragon, encompassing constitutional descriptors, topological indices, information indices, 2D-autocorrelations, and edge adjacency indices [41].
- Descriptor Preprocessing: Remove variables with constant/near-constant values, features containing missing values, and highly correlated descriptors using a correlation coefficient threshold (e.g., 0.80) [41] [75].
Model Building and Validation Protocol:
- Data Splitting: Randomly divide data into training (typically 80%) and test sets (20%) [75].
- Outer Loop Configuration: Implement k-fold cross-validation (commonly 4-5 folds) for overall performance estimation [76].
- Inner Loop Configuration: Apply cross-validation (commonly 4-fold) on training data for model selection and hyperparameter optimization [18] [76].
- Variable Selection: Employ genetic algorithm multi-linear regression (GA-MLR) or stepwise MLR for descriptor selection [74] [75].
- Model Validation: Apply Y-scrambling to confirm non-random character and define applicability domain through leverage calculation [41] [77].
Comparative Performance Data
Table 1: Comparison of Validation Methods in QSAR Studies
| Validation Method | Advantages | Limitations | Typical Application Context |
|---|---|---|---|
| Single Test Set | Simple implementation; Clear separation of training/test data | Requires large test sets for reliability; Single split may be fortuitous; Less efficient data usage | Initial screening with very large datasets; When ample data available for hold-out |
| Single Cross-Validation | More efficient data usage; Provides performance distribution | Model selection bias when used for both parameter tuning and performance estimation; Overly optimistic error estimates | Preliminary model development; When model complexity is low |
| Double Cross-Validation | Unbiased error estimates under model uncertainty; Efficient data use; Reliable for model selection | Computationally intensive; More complex implementation | Cancer QSAR with limited data; Model uncertainty present; High-stakes predictions |
| Repeated k-Fold | Reduces variance of performance estimate; More stable than single k-fold | Does not address model selection bias; Can be computationally intensive | When dataset variability is high; Supplement to nested CV in outer loop |
Table 2: Performance Metrics from Cancer QSAR Studies Using Double Cross-Validation
| Study Focus | Cell Line | Dataset Size | Model Type | Key Validation Metrics | Reference |
|---|---|---|---|---|---|
| Anti-melanoma compounds | SK-MEL-5 | 422 compounds | Random Forest, SVM, kNN | PPV > 0.85 in both nested CV and external testing | [41] |
| TNBC antagonists | MDA-MB-231 | 219 compounds | GA-MLR | R² = 0.79, Q²LOO = 0.77, Q²LMO = 0.76-0.77 | [75] |
| Anti-melanoma benzenesulfonates | M-21 | 97 compounds | MLR, CoMFA | R² = 0.91, R²ex = 0.89, CCCex = 0.94 | [77] |
| Pyridinium bromides | Not specified | 126 compounds | MLR, PLS | Improved predictive performance vs hold-out method | [74] |
Table 3: Essential Software Tools for Double Cross-Validation in QSAR
| Tool/Resource | Function | Application in Cancer QSAR | Availability |
|---|---|---|---|
| Double Cross-Validation Software Tool | Dedicated DCV implementation for MLR and PLS models | Finding optimal predictive QSAR models; Comparing hold-out vs DCV performance | Freely available [74] |
| QSARINS | Genetic algorithm for descriptor selection; Model validation | Building statistically robust MLR models; Y-randomization testing | Academic license [77] |
| Dragon | Molecular descriptor calculation | Computing 13+ blocks of molecular descriptors for structure-activity modeling | Commercial [41] |
| R with mlr package | Machine learning pipeline implementation | Preprocessing, feature selection, and model building with multiple classifiers | Open source [41] |
| Scikit-learn | Machine learning with nested CV implementation | Comparing nested vs non-nested CV; SVM parameter optimization | Open source [76] |
| ChemAxon Standardizer | Molecular structure standardization | Preparing consistent molecular representations before descriptor calculation | Commercial [41] |
Comparative Analysis with Alternative Methods
Performance Advantages in Model Selection
Double cross-validation demonstrates clear advantages over alternative validation approaches, particularly in addressing model selection bias. When comparing DCV with the conventional hold-out method for multiple linear regression QSAR models, studies found DCV to be "a better technique compared to the hold-out method for obtaining predictive MLR and PLS models" [74]. This superiority stems from DCV's ability to generate diverse training set compositions through its nested structure, increasing the likelihood of identifying truly optimal models rather than those that happen to perform well on a single fixed training set [74].
The problem of model selection bias is particularly pronounced when comparing models with different numbers of hyperparameters. As noted in research on classifier selection, "if some models have more hyper-parameters than others, the model choice will be biased towards the models with the most hyper-parameters" [78]. This bias can lead to selection of overly complex models that appear to perform well during development but generalize poorly to new data. DCV mitigates this risk through its strict separation of model selection and assessment [18] [78].
Limitations and Practical Considerations
Despite its statistical advantages, double cross-validation presents practical challenges, primarily computational intensity. The nested structure substantially increases the number of models that must be built and validated—for k1 outer folds and k2 inner folds, approximately k1×k2 models are developed. This can be prohibitive for large datasets or complex algorithms, though this is less concerning for typical QSAR datasets in cancer research which are often moderate in size [75].
Another consideration is that DCV validates the modeling process rather than a specific final model. As explicitly noted in research on prediction error estimation, "the process to arrive at a final model is validated rather than a final model" [7]. When the entire dataset is used to build a production model after DCV, that specific model's performance is only indirectly validated through the process. Some practitioners address this by maintaining a completely independent validation set, though this reduces data available for model development [7].
Implementation Guidelines for Cancer QSAR
Parameterization Considerations
Successful implementation of double cross-validation requires careful parameterization, as "the prediction errors of QSAR/QSPR regression models in combination with variable selection depend to a large degree on the parameterization of double cross-validation" [18]. The inner loop parameters primarily influence bias and variance of resulting models, while outer loop parameters mainly affect variability of the prediction error estimate [18] [7].
For the inner loop, more folds generally reduce bias in model selection but increase computation time. For the outer loop, increasing the number of folds reduces the variance of the performance estimate. In practice, 4-5 folds for the inner loop and 5-10 folds for the outer loop typically provide good compromises between statistical reliability and computational feasibility for cancer QSAR datasets [18] [76].
Integration with OECD QSAR Validation Principles
Double cross-validation aligns strongly with OECD principles for QSAR validation, particularly regarding robust internal and external validation. The process directly addresses the requirement for "a measure of goodness-of-fit, robustness, and predictivity" through its comprehensive evaluation framework [77] [75]. When combined with Y-scrambling (to confirm non-random models) and applicability domain assessment (through Williams plots and leverage calculation), DCV provides a statistically rigorous foundation for cancer QSAR models intended for regulatory decision-making or prioritizing compounds for synthesis [77] [75].
The integration of DCV with these additional validation techniques creates a comprehensive framework for QSAR development in cancer research. As demonstrated in studies of MDA-MB-231 antagonists, this approach yields models with high external predictivity (R²ext = 0.72-0.76) while maintaining interpretability through selected molecular descriptors that provide insight into structural features governing anti-tumor activity [75].
Double cross-validation represents a statistically rigorous solution to the challenge of model uncertainty in cancer QSAR research. By strictly separating model selection from model assessment through its nested structure, DCV provides unbiased estimation of prediction errors—a critical consideration when models guide resource-intensive synthesis and biological testing of potential anti-cancer compounds. While computationally more demanding than simpler validation approaches, its efficient data use makes it particularly valuable for typical cancer QSAR datasets where biological testing data is limited. As cancer research increasingly relies on computational approaches to prioritize compounds against specific cell lines like triple-negative breast cancer and melanoma, proper validation methodologies like double cross-validation ensure that predictive models deliver reliable performance in prospective applications, ultimately accelerating the discovery of novel therapeutic agents.
Applicability Domain Assessment for Reliable Predictions
Quantitative Structure-Activity Relationship (QSAR) modeling represents a pivotal computational approach in modern cancer drug discovery and toxicological risk assessment. These models mathematically correlate chemical structural features with biological activity, enabling researchers to predict the potency, toxicity, or carcinogenic potential of novel compounds prior to costly laboratory synthesis and biological testing. The reliability of any QSAR model, however, is intrinsically constrained by its Applicability Domain (AD)—the chemically meaningful region defined by the properties of the compounds used to develop the model [79].
Defining a model's AD is essential because QSAR predictions are only reliable for compounds structurally similar to those in the training set [79]. The Organization for Economic Cooperation and Development (OECD) explicitly mandates the definition of the Applicability Domain as one of its five key principles for QSAR model validation, highlighting its regulatory importance [79]. This requirement is particularly crucial in cancer research, where models predict critical endpoints like carcinogenicity or anti-cancer activity, and erroneous predictions can have significant consequences for drug development and safety assessment [23] [13].
The central challenge is that real-world chemical space is vast, while QSAR training sets are inherently limited. When a model is applied to a query compound outside its AD, its predictions become unreliable, a form of extrapolation risk [80] [79]. Consequently, robust AD assessment acts as an early warning system, alerting researchers to potential model over-extension and preventing misguided decisions based on untrustworthy predictions. This guide compares the primary methodologies for AD assessment, providing cancer researchers with the knowledge to select and implement appropriate domain characterization techniques, thereby enhancing the reliability of their QSAR-based predictions.
Methodologies for Defining the Applicability Domain
Several distinct methodological approaches have been developed to define and characterize the Applicability Domain of QSAR models. These approaches differ in their underlying algorithms, computational complexity, and how they conceptualize the interpolation space of the training set.
Range-Based and Geometric Approaches
These are among the simplest methods for characterizing a model's interpolation space.
- Bounding Box: This approach defines the AD based on the maximum and minimum values of each molecular descriptor used in the model. The resulting domain is a p-dimensional hyper-rectangle. Its main limitation is that it cannot identify empty regions within the defined hyper-rectangle and does not account for correlations between descriptors [79].
- PCA Bounding Box: To overcome descriptor correlation issues, this method performs Principal Component Analysis (PCA) on the original descriptors. The AD is then defined as a hyper-rectangle in the space of the significant principal components. This approach corrects for descriptor correlation but may still include empty regions within the convex hull of the training data [79].
- Convex Hull: This geometric method defines the AD as the smallest convex shape that contains all training compounds in the descriptor space. While intuitive, determining the convex hull becomes computationally challenging as the dimensionality of the descriptor space increases. Like the bounding box methods, it cannot detect internal empty regions where no training data exists [79].
Distance-Based and Density-Based Approaches
These methods focus on the proximity of a query compound to the distribution of the training set.
- Leverage and Mahalanobis Distance: Leverage, derived from the model's hat matrix, is proportional to the Mahalanobis distance from the query compound to the centroid of the training data. The Mahalanobis distance is particularly useful as it accounts for correlations between descriptors by incorporating the covariance matrix. A common rule is that a compound with leverage greater than ( 3p/n ) (where p is the number of model descriptors and n is the number of training compounds) may be influential or an outlier [79].
- Euclidean and City-Block Distance: These are simpler distance measures that do not inherently account for descriptor correlations. Their utility can be improved by applying them within a PCA-transformed space to correct for correlated axes [79].
- Kernel Density Estimation (KDE): KDE is a powerful non-parametric method for estimating the probability density function of the training data in the feature space. A query compound is considered within the AD if it lies in a region of feature space with a density above a predefined threshold. KDE naturally accounts for data sparsity and can handle arbitrarily complex geometries of data regions, making it superior to methods that assume a single, connected region for the AD [80].
Table 1: Comparison of Major Applicability Domain Assessment Methods
| Method | Underlying Principle | Advantages | Limitations | Suitability for Cancer QSAR |
|---|---|---|---|---|
| Bounding Box [79] | Descriptor value ranges | Simple, fast computation | Ignores correlation and empty spaces | Low; too simplistic for complex endpoints |
| Convex Hull [79] | Smallest convex geometry | Intuitive visualization | Computationally intense in high dimensions | Medium; useful for low-dimensional projects |
| Leverage [79] | Mahalanobis distance to centroid | Accounts for descriptor correlations | Defines a single, ellipsoidal domain | High; recommended for regression-based models |
| k-NN Distance [80] | Mean distance to k-nearest neighbors | Simple, does not assume data shape | Requires defining k and a distance threshold | High; flexible for diverse chemical data |
| KDE [80] | Probability density of training set | Handles complex, disjointed domains | Choice of kernel and bandwidth can affect results | Very High; state-of-the-art for complex models |
Integrating AD Assessment with Model Validation in Cancer Research
Robust AD assessment is inextricably linked to rigorous model validation, particularly in the high-stakes context of cancer research. The reliability of a QSAR model is not a single value but a function of how it is validated and where it is applied.
The Imperative of Double Cross-Validation
Under conditions of model uncertainty, especially when variable selection is involved, double cross-validation (double CV) is a highly recommended technique for obtaining reliable estimates of prediction errors [7]. This method consists of two nested loops:
- The outer loop is used for model assessment, providing an unbiased estimate of the prediction error on held-out test data.
- The inner loop is applied to the training set from the outer loop and is used for all model building and optimization steps, including variable selection.
This process is repeated with multiple splits to average the results. Double CV validates the entire model-building process, not just a final model, and is crucial for generating realistic performance estimates that are not overly optimistic due to model selection bias [7]. For cancer QSAR models predicting endpoints like carcinogenicity or compound potency, this provides a more trustworthy foundation for decision-making.
Advanced Validation: Y-Randomization and External Testing
Beyond cross-validation, additional techniques are essential for establishing model credibility:
- Y-Randomization: This test involves scrambling the activity values (Y-response) of the training set and re-building the model. A significant drop in performance for the randomized models confirms that the original model captured a real structure-activity relationship rather than chance correlations [14].
- External Validation: The gold standard for assessing predictive performance is testing the model on a completely independent set of compounds that were not used in any model building or selection steps [7]. The model's performance on this external set provides the most realistic estimate of its predictive power on new data.
Table 2: Experimental Validation Protocols for Robust Cancer QSAR Models
| Validation Technique | Primary Function | Key Outcome Metrics | Interpretation for Model Reliability |
|---|---|---|---|
| Internal Validation (e.g., LOO, LMO) [81] | Assess model stability on training data | ( Q^2{LOO} ), ( Q^2{LMO} ), ( CCC_{cv} ) | High values (( Q^2 > 0.7 ), ( CCC_{cv} > 0.85 )) indicate a stable model [81]. |
| Double Cross-Validation [7] | Unbiased error estimation under model uncertainty | ( RMSE{cv} ), ( R^2{ext} ) | A small gap between internal and double CV error suggests minimal overfitting. |
| Y-Randomization [14] | Verify model is not based on chance | ( R^2 ), ( ACC. ) of randomized models | Performance should drastically fall (e.g., ( ACC. \approx 0.5 ) for classification) [14]. |
| External Validation [81] [7] | Estimate true predictive power on new data | ( R^2{ext} ), ( Q^2{F1} ), ( Q^2{F2} ), ( CCC{ex} ) | ( R^2{ext} > 0.7 ) and ( CCC{ex} > 0.85 ) indicate strong external predictivity [81]. |
A Practical Workflow for Reliable Predictions in Cancer QSAR
Integrating AD assessment with rigorous validation creates a powerful workflow for ensuring reliable predictions in cancer research. The following diagram and explanation outline this integrated process.
Integrated Workflow for QSAR Modeling and AD Assessment
The workflow for building and applying a reliable QSAR model in cancer research involves several critical, interconnected stages:
- Model Building & Internal Validation: A QSAR model is developed using a training set of compounds with known biological activities. Internal validation techniques, such as Leave-One-Out (LOO) and Leave-Many-Out (LMO) cross-validation, are employed to assess the model's internal stability and robustness. Key metrics include ( Q^2{LOO} ) and ( Q^2{LMO} ), with values above 0.7 generally indicating good internal predictive ability [81].
- Define Applicability Domain (AD): Concurrently, the model's Applicability Domain is defined using one or more of the methods described in Table 1 (e.g., Leverage, k-NN, KDE). This step characterizes the chemical space where the model is expected to make reliable predictions.
- External & Double Cross-Validation: The model's generalizability is tested on a completely independent external test set. Double cross-validation should be used to obtain a realistic error estimate that accounts for model selection, ensuring the model is not overfitted to the training data [7].
- Apply Model to New Query Compound: The finalized and validated model is used to predict the activity of a new, unknown compound.
- AD Check for Query Compound: The new compound's position relative to the pre-defined AD is assessed.
- 5a. Compound WITHIN AD: The compound is sufficiently similar to the training set. Proceed with confidence.
- 5b. Compound OUTSIDE AD: The compound is structurally dissimilar or an extrapolation. Proceed with extreme caution.
- Assign Reliability to Prediction:
- 6a. Prediction is RELIABLE: Predictions for in-domain compounds can be trusted for subsequent analysis.
- 6b. Prediction is UNRELIABLE: Predictions for out-of-domain compounds should be flagged as untrustworthy.
- Final Decision:
- 7a. Use Prediction: Reliable predictions can inform hypothesis generation and research decisions.
- 7b. Seek Alternatives: Unreliable predictions should not be used. Instead, seek alternative models (e.g., from different software) or revert to experimental testing.
Implementing a rigorous AD assessment requires a combination of software tools, databases, and computational protocols. The following table details key resources referenced in the literature.
Table 3: Essential Research Reagent Solutions for QSAR and AD Assessment
| Tool / Resource | Type | Primary Function | Relevance to AD Assessment |
|---|---|---|---|
| OECD QSAR Toolbox [23] | Software | Profiling chemicals for potential hazards, grouping, and (Q)SAR model application. | Provides built-in functionality for assessing a compound's position relative to a model's training set, crucial for regulatory acceptance. |
| Danish (Q)SAR Platform [23] | Online Software | A free resource containing a database of predictions from hundreds of (Q)SAR models for toxicity endpoints. | Offers "battery calls" based on predictions from multiple models within their applicability domains, demonstrating integrated AD assessment. |
| DRAGON / E-Dragon [82] | Descriptor Calculator | Software for calculating thousands of molecular descriptors from chemical structures. | Generating a comprehensive set of molecular descriptors is the foundational step for any subsequent domain characterization. |
| Gaussian 09W [82] | Quantum Chemistry | Software for performing quantum mechanical calculations (e.g., DFT with B3LYP functional). | Used to compute high-level quantum chemical descriptors that can provide a more accurate basis for defining the chemical space and AD. |
| Double Cross-Validation [7] | Statistical Protocol | A validation method with nested loops for unbiased error estimation under model uncertainty. | Not a commercial tool, but an essential protocol to use in conjunction with AD to ensure reported model performance is realistic. |
The rigorous assessment of the Applicability Domain is not an optional step but a fundamental requirement for the reliable application of QSAR models in cancer research and toxicology. As evidenced by recent studies, inconsistencies in predictions across different models can often be traced back to differences in their respective applicability domains and the strategies used to define them [23]. No single AD method is universally superior; the choice depends on the model's complexity, the descriptor types, and the specific application.
The most robust strategy involves a multi-faceted approach: leveraging more advanced methods like Kernel Density Estimation for complex models, integrating AD assessment with double cross-validation to combat model selection bias, and always providing transparent documentation of the AD definition method used [23] [80] [7]. By systematically implementing these practices, researchers in drug development and safety assessment can significantly enhance the credibility of their computational predictions, leading to more efficient and successful translation of QSAR models from a theoretical tool to a practical asset in the fight against cancer.
Quantitative Structure-Activity Relationship (QSAR) modeling represents a cornerstone computational approach in modern drug discovery, enabling researchers to predict the biological activity of chemical compounds from their molecular structure [13]. In cancer research specifically, QSAR models have been successfully applied to discover novel anti-melanoma agents, anti-colorectal cancer compounds, and inhibitors targeting specific kinases like c-src, which is implicated in multiple malignancies [41] [24] [83]. The reliability of these models hinges on rigorous validation techniques, particularly through proper parameter optimization using cross-validation methods.
The Organization for Economic and Co-operation and Development (OECD) principles for QSAR validation explicitly recommend assessing both robustness and predictivity, which are typically evaluated through internal and external validation procedures [84]. Leave-One-Out (LOO) and Leave-Many-Out (LMO) cross-validation techniques represent two fundamental approaches for this internal validation, each with distinct advantages and limitations in the context of parameter optimization for cancer QSAR models. These methods function within a nested configuration of inner and outer loops, where the inner loop optimizes model parameters while the outer loop provides unbiased performance estimates [84].
Theoretical Foundations of LOO and LMO Cross-Validation
Leave-One-Out Cross-Validation (LOO-CV)
Leave-One-Out Cross-Validation operates by systematically removing one observation from the dataset, building the model on the remaining n-1 samples, and predicting the held-out observation. This process repeats until every observation has been excluded once. The LOO-CV error is calculated as the average of these prediction errors, providing an estimate of model performance [85]. The mathematical formulation of LOO-CV error is expressed as:
LOO-CVerror = 1/n ∑(yj - ŷ(-j))²
Where yj is the true response at xj, and ŷ(-j) is the prediction at xj calculated using all training points except the j-th observation [85]. For large datasets, computational efficiency becomes a concern, leading to approximations like Pareto-smoothed importance sampling (PSIS-LOO) to reduce computational burden while maintaining accuracy [86].
Leave-Many-Out Cross-Validation (LMO-CV)
Leave-Many-Out Cross-Validation, also known as k-fold cross-validation, extends this concept by removing multiple observations simultaneously. The dataset is partitioned into k subsets (folds), with each fold serving as the validation set while the remaining k-1 folds form the training set. This process repeats k times, with each fold used exactly once as validation data. The LMO-CV error represents the average prediction error across all folds [84]. Research has demonstrated that with appropriate rescaling, LOO and LMO validation parameters can be directly compared, and the computationally feasible method should be chosen depending on the model type and sample size [84].
Comparative Analysis of LOO and LMO Performance Characteristics
Table 1: Theoretical Comparison of LOO and LMO Cross-Validation Methods
| Characteristic | LOO-CV | LMO-CV |
|---|---|---|
| Bias | Lower bias | Higher bias |
| Variance | Higher variance | Lower variance |
| Computational Cost | High (n models) | Lower (k models, where k < n) |
| Optimal Scenario | Small datasets | Large datasets |
| Stability | Less stable with high variance | More stable with lower variance |
Inner and Outer Loop Configuration for Parameter Optimization
Nested Cross-Validation Architecture
The parameter optimization process in QSAR modeling employs a nested cross-validation structure consisting of inner and outer loops. The outer loop provides an unbiased assessment of model performance, while the inner loop performs hyperparameter tuning and feature selection. In this configuration, the dataset is initially divided into training and testing sets, with the training set further partitioned for the inner validation procedure [41] [83].
For cancer QSAR models, this approach ensures that the model's predictive capability is assessed on completely independent data not used during parameter optimization. A study developing QSAR models for SK-MEL-5 melanoma cell line cytotoxicity employed nested cross-validation with over 350 models, selecting only those with both balanced accuracy and positive predictive value higher than 70% [41]. This rigorous approach prevents overfitting and provides more reliable performance estimates for virtual screening applications in oncology drug discovery.
Implementation Protocols
Standard LOO-CV Implementation Protocol
The following workflow details the standard implementation of LOO-CV for parameter optimization in cancer QSAR models:
Dataset Preparation: Standardize molecular structures, calculate molecular descriptors, and divide data into activity classes. For example, in anti-melanoma QSAR models, compounds are typically classified as "active" if GI₅₀ < 1 µM and "inactive" if GI₅₀ ≥ 1 µM [41].
Outer Loop Configuration: Iterate through each observation in the dataset (i = 1 to n), where at each iteration:
- Set aside observation i as the validation sample
- Use remaining n-1 observations as the training set
Inner Loop Operations: For each training set (n-1 observations):
- Perform feature selection using methods like random forest importance or symmetrical uncertainty [41]
- Optimize model hyperparameters through grid search or Bayesian optimization
- Train the model with selected features and optimized parameters
Validation and Aggregation:
- Predict the held-out observation i using the trained model
- Calculate prediction error for observation i
- Aggregate errors across all n iterations to compute overall LOO-CV error
Model Selection: Choose the model configuration with minimal LOO-CV error for final training on the complete dataset [85].
Advanced LMO-CV Implementation Protocol
For LMO-CV implementation in cancer QSAR studies:
Dataset Stratification: Partition data into k folds (typically 5-10) while maintaining activity class distributions. For c-src tyrosine kinase inhibitor models, this ensures representative sampling of active and inactive compounds across folds [83].
Outer Loop Configuration: Iterate through each fold (j = 1 to k), where at each iteration:
- Set aside fold j as the validation set
- Use remaining k-1 folds as the training set
Inner Loop Operations: For each training set (k-1 folds):
- Perform k-fold cross-validation or bootstrap resampling on the training set
- Optimize hyperparameters through performance monitoring on validation folds
- Select optimal parameter set based on cross-validation performance
Validation and Aggregation:
- Predict all observations in the held-out fold j using the trained model
- Calculate prediction errors for fold j
- Aggregate errors across all k folds to compute overall LMO-CV error
Model Assessment: Evaluate model stability and select optimal configuration based on LMO-CV performance metrics [84].
Experimental Comparison in Cancer QSAR Applications
Performance Metrics and Evaluation Criteria
The comparative evaluation of LOO and LMO cross-validation techniques in cancer QSAR modeling employs multiple performance metrics to assess model quality. These include:
- Goodness-of-fit: Measured by R² (coefficient of determination) between predicted and observed activities [84]
- Robustness: Evaluated through Q²LOO (LOO cross-validated R²) and Q²LMO (LMO cross-validated R²) [84]
- Predictivity: Assessed via external validation metrics such as Q²F2 on independent test sets [84]
- Model Stability: Monitored through standard deviation of performance metrics across multiple iterations
For cancer QSAR models, additional domain-specific metrics include balanced accuracy and positive predictive value (PPV), particularly important when dealing with imbalanced datasets common in anticancer compound screening [41].
Case Study: Anti-Colorectal Cancer Agent QSAR Models
A QSAR study on anti-colorectal cancer agents utilizing quantum chemical predictors demonstrated the application of these validation techniques. The research developed models with robust statistical performance, though specific cross-validation parameters were not detailed in the available excerpt [24]. This highlights the critical importance of proper validation in models intended for predicting activity against specific cancer cell lines.
Case Study: c-src Tyrosine Kinase Inhibitor Models
In developing QSAR models for c-src tyrosine kinase inhibitors, researchers employed stacked classification models with nested cross-validation. From over 350 initial models, 49 with acceptable performance (balanced accuracy >70% and PPV >70%) were selected for virtual screening of over 100,000 compounds [83]. This large-scale application demonstrates the practical implications of cross-validation choice in identifying promising anticancer candidates.
Case Study: Dopamine Transporter-Targeted Compounds
A QSAR study on dopamine active transporter (DAT) ligands demonstrated robust model performance using LOO-CV, with reported statistics of R² = 0.7554, Q²LOO = 0.6800, and external R² = 0.7090 [22]. This example illustrates successful LOO-CV implementation on a moderately sized dataset (57 compounds) relevant to neurological targets, with methodologies applicable to cancer-related targets.
Table 2: Experimental Performance Comparison of LOO and LMO in Cancer QSAR Studies
| Study Focus | Sample Size | LOO-CV Performance | LMO-CV Performance | Optimal Method |
|---|---|---|---|---|
| SK-MEL-5 Melanoma [41] | 422 compounds | ~70-85% PPV in nested CV | Not specified | LOO with feature selection |
| c-src Tyrosine Kinase [83] | 1038 compounds | Used in model selection | Not specified | LOO with multiple algorithms |
| DAT Inhibitors [22] | 57 compounds | Q² = 0.6800 | Not specified | LOO-CV |
| General QSAR Validation [84] | Multiple datasets | Equivalent to LMO after rescaling | Equivalent to LOO after rescaling | Method-dependent |
Table 3: Essential Research Reagents and Computational Resources for Cross-Validation in Cancer QSAR
| Resource Category | Specific Tools/Solutions | Function in Cross-Validation |
|---|---|---|
| QSAR Software | QSARINS [71] [22] | MLR-based QSAR modeling with built-in validation |
| Molecular Descriptors | Dragon Software [41] [22] | Calculation of 0D-2D molecular descriptors |
| Machine Learning Libraries | R miner package [41] | Implementation of RF, SVM, BST, KNN algorithms |
| Cross-Validation Implementations | SAS Survival LOOCV Macro [87] | Specialized LOO-CV for survival analysis |
| Model Validation | Python scikit-learn, R mlr package [41] | Nested cross-validation implementation |
| Chemical Standardization | ChemAxon Standardizer [41] | Molecular structure preprocessing |
| Descriptor Pre-processing | R FSelector package [41] | Feature selection for model optimization |
The comparative analysis of LOO and LMO cross-validation techniques for parameter optimization in cancer QSAR modeling reveals a complex landscape with no universally superior approach. The optimal configuration depends on multiple factors including dataset size, computational resources, and specific research objectives.
For small to moderate-sized datasets (n < 1000), LOO-CV often provides less biased estimates and is particularly valuable in early-stage cancer drug discovery where sample sizes are limited. This is evidenced by its successful application in melanoma QSAR models with 422 compounds and DAT inhibitor models with just 57 compounds [41] [22]. However, LOO-CV's computational intensity and potential for high variance must be considered, with approximations like PSIS-LOO offering practical alternatives for larger datasets [86].
For larger cancer compound datasets (n > 1000), LMO-CV provides more practical implementation with reduced computational burden while maintaining reliable performance estimates. The rescaling equivalence between LOO and LMO parameters noted in validation studies suggests that choice may be based primarily on computational feasibility rather than fundamental performance differences [84].
The nested cross-validation architecture, with inner loops handling parameter optimization and outer loops providing performance estimation, represents the gold standard for developing robust, predictive cancer QSAR models. This approach ensures reliable virtual screening outcomes while maintaining the statistical rigor demanded by modern computational oncology and drug discovery pipelines.
Advanced Validation Frameworks and Comparative Analysis of QSAR Techniques in Oncology
In the field of cancer research, particularly in quantitative structure-activity relationship (QSAR) studies for anti-breast cancer drug discovery, the ability to reliably predict compound activity is paramount [13]. While internal validation techniques provide initial assessments of model quality, external validation stands as the unequivocal gold standard for evaluating a model's true predictive power for new, untested chemicals [18] [88]. This distinction is crucial because a model that fits existing data well may still fail catastrophically when presented with novel chemical structures, a phenomenon known as overfitting [18]. The Organisation for Economic Cooperation and Development (OECD) has formally recognized this principle, emphasizing that validation must demonstrate both internal robustness and external predictivity for regulatory acceptance of QSAR models [88]. In the high-stakes domain of cancer drug development, where mispredictions can divert research resources significantly, establishing rigorous validation protocols is not merely academic—it is a practical necessity for efficient therapeutic discovery.
Methodological Framework: Understanding Validation Hierarchies
The Spectrum of QSAR Validation Techniques
QSAR validation strategies exist along a spectrum of stringency, with external validation providing the most rigorous assessment of real-world predictive utility [88]. Internal validation techniques, such as leave-one-out (LOO) cross-validation, use only the training set molecules to assess model performance by systematically holding out subsets of data during model building and predicting their activities [88]. While valuable for initial model development, these methods can produce overoptimistic estimates of predictive ability because the entire dataset influences the model selection process [18]. In contrast, external validation employs a completely independent test set of compounds that are never used during model building or selection, providing an unbiased assessment of how the model will perform on genuinely new chemicals [18] [88]. A third approach, double cross-validation (also called nested cross-validation), combines elements of both strategies by creating an outer loop for model assessment and an inner loop for model selection, offering a more efficient use of data while maintaining statistical rigor [18] [7].
Technical Implementation of External Validation
The implementation of proper external validation requires careful experimental design. The fundamental protocol involves splitting the available chemical dataset into two distinct subsets before model development begins [88]. The training set (typically 70-80% of compounds) is used exclusively for model building and parameter optimization, while the test set (the remaining 20-30%) is held back completely and used only once for final model assessment [18]. This strict separation ensures the test set provides a genuinely independent assessment of predictive performance. For reliable results, the test set must be sufficiently large and representative of the chemical space covered by the training set [18]. The division should ideally use strategic approaches such as balanced random selection or experimental designs on the dependent or independent variables rather than simple random splits, which can produce fortuitous results [18]. When implementing double cross-validation, the process involves repeated partitioning of data in both inner and outer loops to average performance estimates across multiple splits, reducing variability in error estimation [18] [7].
Table 1: Comparison of QSAR Validation Methods
| Validation Type | Key Principle | Advantages | Limitations |
|---|---|---|---|
| Internal Validation (e.g., LOO-CV) | Uses only training data with iterative hold-out samples | Computationally efficient; good for model development | Risk of overoptimistic estimates; model selection bias |
| External Validation (Hold-out method) | Completely independent test set never used in model development | Unbiased estimate of real predictive performance | Requires larger datasets; single split may be fortuitous |
| Double Cross-Validation (Nested CV) | Combines internal and external validation through nested loops | More efficient data usage; multiple performance estimates | Computationally intensive; validates process rather than final model |
Quantitative Assessment: Validation Metrics and Standards
Established Metrics for External Validation
The scientific community has developed multiple quantitative metrics to evaluate external predictive performance, with ongoing debate about optimal criteria [89]. The predictive squared correlation coefficient (Q²F1) has been proposed in OECD guidelines as a standard measure [89] [90]. Alternative metrics include the Golbraikh-Tropsha method, r²m (Roy), Q²F2 (Schüürmann et al.), and Q²F3 (Consonni et al.) [89]. A comparative study of these measures revealed that while they generally produce concordant results, contradictions can occur, creating uncertainty about model acceptability [89]. To address this challenge, the concordance correlation coefficient (CCC) has been proposed as a more restrictive and stable alternative that helps resolve conflicts between differing validation metrics [89]. The CCC evaluates both precision and accuracy by measuring how far observations deviate from the line of perfect concordance (45° line), providing a comprehensive assessment of predictive performance [89].
Experimental Evidence of Superior Predictive Assessment
Empirical studies consistently demonstrate that external validation provides more realistic performance estimates compared to internal methods alone. Research on QSAR/QSPR regression models with variable selection has shown that prediction errors estimated through external validation are consistently higher but more realistic than internally cross-validated estimates [18]. This phenomenon occurs because internal cross-validation errors can be underestimated due to model selection bias, where the same data influences both model selection and error estimation [18] [7]. The bias is particularly pronounced when models include irrelevant variables or when truly relevant but weak variables are poorly estimated [18]. External validation circumvents this issue by providing completely independent assessment, making it indispensable for evaluating true generalization capability [18].
Table 2: Key Validation Metrics for QSAR Model Assessment
| Metric | Calculation Principle | Acceptance Threshold | Key Advantage |
|---|---|---|---|
| Q²F1 (Predictive squared correlation coefficient) | Sum of squares of test set referring to training set mean | >0.5 | Recommended in OECD guidelines |
| Concordance Correlation Coefficient (CCC) | Deviation from line of perfect concordance | >0.85 | Measures both precision and accuracy |
| r²m | Modified correlation coefficient considering mean activity | >0.5 | Accounts for activity distribution |
| Q²F2 | Sum of squares referring to test set mean | >0.5 | Uses test set reference point |
| Q²F3 | Based on mean deviations over training set | >0.5 | Training set reference |
Advanced Applications: External Validation in Cancer Research
Case Study: Anti-Breast Cancer Agent Development
The critical importance of external validation is particularly evident in QSAR models developed for anti-breast cancer applications [13]. In a recent study of dihydropyrimidinone derivatives evaluated against breast cancer cell lines, researchers developed a QSAR model with impressive internal validation statistics (R²=0.98) [31]. However, the model's true utility was established through external validation, which confirmed its predictive capability with a Q² value of 0.97 [31]. This external validation provided the necessary confidence to proceed with experimental testing, which confirmed significant anticancer activity for the lead compound (IC50 2.15 μM) compared to tamoxifen (IC50 1.88 μM) [31]. Without rigorous external validation, the risk of overfitting would have remained substantial, potentially leading to wasted resources on false leads. This case exemplifies how proper validation protocols directly contribute to efficient drug discovery in oncology.
Defining Applicability Domains for Reliable Predictions
A crucial aspect of external validation is defining the applicability domain (AD) of QSAR models, as specified in OECD Principle 3 [91] [88]. The AD represents the chemical space defined by the training set structures and properties, within which the model can generate reliable predictions [91] [88]. When external test compounds fall within this domain, predictions are considered interpolations with higher confidence; predictions outside this domain represent extrapolations with higher uncertainty [88]. Research on estrogen receptor binding models has demonstrated that prediction accuracy is inversely proportional to the degree of domain extrapolation, with high confidence domains providing significantly more reliable predictions [91]. Methods for characterizing AD include ranges of descriptor spaces, leverage approaches, and PCA-based methods [91]. The incorporation of AD assessment complements external validation by quantifying the uncertainty of individual predictions, creating a more comprehensive validation framework.
Diagram 1: Comprehensive QSAR Validation Workflow integrating internal validation, external validation, and applicability domain assessment as sequential checkpoints for model acceptance.
Practical Implementation: The Researcher's Toolkit
Implementing robust external validation requires specialized software tools and computational resources. QSARINS is a standalone software specifically designed for QSAR model development with advanced validation capabilities, including data partitioning, model validation, and applicability domain determination [31]. For molecular docking studies integrated with QSAR validation, PyRx with AutoDock Vina provides open-source docking capabilities for target identification and binding analysis [31]. Molecular descriptor calculation is facilitated by tools like Dragon, Molconn-Z, and CODESSA, which generate thousands of molecular descriptors for QSAR modeling [91] [92]. ADMET prediction can be performed using online tools like pkCSM to assess pharmacokinetic properties and drug-likeness of candidate compounds [31]. For consensus modeling approaches like Decision Forest, custom implementations in R or Python are typically employed to combine multiple decision trees and assess prediction confidence [91].
Experimental Protocols for Validation Studies
A standardized protocol for external validation in cancer QSAR studies includes several critical steps. First, data collection and curation involves compiling a structurally diverse set of compounds with reliable experimental biological activities, preferably from public databases like EDKB (Endocrine Disruptor Knowledge Base) for endocrine disruptors [91] [92]. Second, rational data splitting ensures the external test set adequately represents the structural and activity space of the training set, using methods such as Kennard-Stone or sphere exclusion algorithms [92]. Third, model development with internal validation employs techniques like genetic algorithm-partial least squares (GA-PLS) or multiple linear regression (MLR) with leave-multiple-out cross-validation (LMOCV) to select optimal descriptors [92]. Fourth, external prediction and validation applies the finalized model to the completely independent test set and calculates multiple validation metrics (Q²F1, CCC, r²m) [89]. Finally, applicability domain characterization uses leverage approaches, PCA-based methods, or distance-based metrics to define the chemical space of reliable predictions [91] [88].
Table 3: Research Reagent Solutions for QSAR Validation
| Tool/Category | Specific Examples | Primary Function | Relevance to Validation |
|---|---|---|---|
| QSAR Software | QSARINS, CORAL, Ezqsar | Model development and validation | Specialized in validation statistics and applicability domain |
| Descriptor Calculators | Dragon, Molconn-Z, CODESSA | Molecular descriptor generation | Provides structural parameters for modeling |
| Docking Tools | PyRx (AutoDock Vina), Open3DQSAR | Target-ligand interaction analysis | Supports mechanistic interpretation (OECD Principle 5) |
| ADMET Predictors | pkCSM, Data Warrior | Pharmacokinetic and toxicity profiling | Assesses drug-likeness and therapeutic potential |
| Consensus Models | Decision Forest, R/Python scripts | Combines multiple models for improved accuracy | Enhances prediction confidence through ensemble approaches |
External validation remains the definitive method for assessing the true predictive power of QSAR models in cancer research and drug discovery. While internal validation techniques serve important roles in model development and refinement, only external validation with completely independent test sets can provide unbiased estimates of real-world performance [18] [88]. The integration of external validation with applicability domain assessment creates a robust framework for evaluating model reliability and establishing boundaries for appropriate use [91] [88]. As QSAR applications expand in pharmaceutical development and regulatory decision-making, adherence to OECD principles—particularly the demonstration of external predictivity—becomes increasingly critical [88]. For researchers developing anti-cancer compounds, embracing rigorous external validation protocols is not merely a statistical formality but an essential practice that separates truly predictive models from those that merely fit existing data, ultimately accelerating the discovery of effective therapeutics.
In the field of cancer research, particularly in quantitative structure-activity relationship (QSAR) modeling for drug discovery, the validation of predictive models is not merely a statistical formality but a crucial determinant of real-world applicability. Predictive models in oncology aim to forecast critical outcomes such as compound cytotoxicity against specific cancer cell lines or carcinogenic potential of chemicals, guiding expensive and time-consuming experimental research. The choice between single and double cross-validation methodologies can significantly impact the reliability of these predictions, potentially determining whether a promising therapeutic candidate advances in the development pipeline or not.
Single cross-validation, while widely used, risks overoptimistic performance estimates because the same data is often used for both model selection and evaluation. This problem is particularly acute in high-dimensional QSAR studies where the number of molecular descriptors frequently exceeds the number of compounds, creating ample opportunity for overfitting. Double cross-validation, also known as nested cross-validation, addresses this fundamental limitation by establishing two layers of data separation: an inner loop for model selection and parameter tuning, and an outer loop for unbiased performance estimation. This structured approach validates the entire model-building process rather than just a final model, providing researchers with a more realistic assessment of how their models will perform on truly independent data.
Theoretical Foundations: Understanding the Validation Mechanisms
Single Cross-Validation: Conceptual Framework and Limitations
Single cross-validation operates on a straightforward principle of data partitioning. The dataset is divided into k subsets or "folds," with k-1 folds used for training and the remaining fold for testing. This process rotates across all folds, with the average performance across all iterations representing the model's estimated predictive capability. Common implementations include k-fold cross-validation (typically with k=5 or k=10) and leave-one-out cross-validation (where k equals the number of samples).
The fundamental vulnerability of this approach emerges when model selection occurs within this process. When researchers try multiple algorithms or hyperparameters and select the best performer based on cross-validation results, they introduce model selection bias or "overfitting to the test set." The selected model appears optimal for that specific data partitioning but may not generalize well to truly independent data because the test folds have indirectly influenced model selection [18]. This bias is particularly problematic in cancer research using QSAR models, where the goal is often to predict the biological activity of novel compounds not yet synthesized or tested.
Double Cross-Visualization: A More Robust Architecture
Double cross-validation introduces a hierarchical structure to the validation process, formally separating model selection from performance estimation. The methodology consists of two nested loops:
- Outer Loop: Functions as an external validation layer, repeatedly splitting data into training and test sets. The test sets in this loop are completely withheld from any model development activities and provide the final performance estimates.
- Inner Loop: Operates exclusively on the training set from the outer loop, performing model selection and parameter tuning through an internal cross-validation process. This ensures that the test data in the outer loop remains completely untouched during model optimization.
This structure effectively eliminates the model selection bias inherent in single cross-validation by guaranteeing that the data used for final performance assessment never participates in any aspect of model building or selection [18] [7]. The following diagram illustrates this hierarchical data separation:
Quantitative Performance Comparison: Empirical Evidence from Cancer Studies
Comparative Analysis Across Multiple Research Contexts
Multiple studies across different cancer research domains have systematically compared the performance estimates generated by single versus double cross-validation approaches. The consistent finding across these diverse contexts is that single cross-validation tends to produce overoptimistic performance metrics, while double cross-validation provides more realistic, generalizable estimates of model performance.
Table 1: Performance Comparison Between Single and Double Cross-Validation in Cancer Studies
| Research Context | Single CV Performance | Double CV Performance | Performance Gap | Reference |
|---|---|---|---|---|
| Genomic Prediction Models (8 breast cancer microarray datasets) | Inflated discrimination accuracy across all algorithms | Substantially lower, more realistic accuracy estimates | Significant inflation in single CV estimates | [93] |
| QSAR Regression Models (with variable selection) | Biased estimates due to model selection bias | Reliable and unbiased prediction error estimates | Single CV produced untrustworthy error estimates | [18] [7] |
| MLR QSAR Models (three different datasets) | Lower predictive performance on external test sets | Superior external predictive performance | DCV provided better generalization to new compounds | [74] |
| SERS Spectral Classification (hepatocellular carcinoma detection) | Risk of overfitting with arbitrary parameter choices | 81% average accuracy with confidence intervals | RDCV enabled uncertainty estimation and minimized overfitting | [94] |
Cross-Study Validation: Revealing the True Generalization Gap
A particularly revealing investigation examined prediction models for distant metastasis-free survival (DMFS) in estrogen receptor-positive breast cancer using eight microarray datasets. Researchers implemented what they termed "cross-study validation" (CSV), where models trained on one dataset were validated on completely independent datasets. This approach mirrors the philosophy of double cross-validation by using truly independent data for assessment.
The findings were striking: "standard cross-validation produces inflated discrimination accuracy for all algorithms considered, when compared to cross-study validation" [93]. Furthermore, the ranking of learning algorithms differed between the methods, suggesting that "algorithms performing best in cross-validation may be suboptimal when evaluated through independent validation" [93]. This has profound implications for cancer research, as it indicates that model selection based on single cross-validation may lead researchers to choose suboptimal algorithms for real-world applications where models must generalize across different patient populations and experimental conditions.
Experimental Protocols and Implementation Guidelines
Standard Double Cross-Validation Protocol for QSAR Studies
Implementing double cross-validation correctly requires careful attention to experimental design. The following protocol outlines the key steps for proper implementation in cancer QSAR studies:
Data Preparation: Begin with appropriate data preprocessing, including removal of constant or near-constant descriptors, handling of missing values, and elimination of highly correlated variables (using a threshold such as R² > 0.80) [41]. For QSAR models based on PubChem data, this may involve standardizing molecular structures using tools like ChemAxon Standardizer and calculating molecular descriptors with software such as Dragon.
Outer Loop Configuration: Split the entire dataset into k folds (typically k=5 or k=10) for the outer loop. For each iteration:
- Reserve one fold as the test set
- Use the remaining k-1 folds as the training set for the inner loop
Inner Loop Configuration: Within each training set, implement another cross-validation (typically with the same k value as the outer loop) to optimize model parameters and select the best-performing model configuration. For machine learning methods like Random Forests or Support Vector Machines, this includes tuning hyperparameters such as the number of trees, maximum depth, or kernel parameters.
Model Assessment: Apply the optimally selected and trained model from the inner loop to the reserved test set from the outer loop to obtain performance metrics.
Repetition and Averaging: Repeat the process multiple times with different random splits (repeated double cross-validation) to obtain stable performance estimates and calculate confidence intervals for figures of merit [94].
Case Study: QSAR Model Development for Melanoma Cell Line Cytotoxicity
A specific implementation of this protocol was demonstrated in the development of QSAR models to predict compound cytotoxicity against the SK-MEL-5 human melanoma cell line. Researchers used 422 compounds with known GI50 values from PubChem, represented by 13 blocks of molecular descriptors calculated with Dragon software [41].
The experimental workflow followed these specific steps:
Data Curation: Standardized molecular structures, removed duplicates, and defined binary activity classes (active: GI50 < 1 µM; inactive: GI50 > 1 µM)
Descriptor Preprocessing: Removed constant, near-constant, and highly correlated descriptors within each block, then selected a maximum of 7 features using Random Forest importance or symmetrical uncertainty
Model Building with Double CV: Implemented double cross-validation with four different machine learning classifiers: Random Forest, gradient boosting, Support Vector Machines, and k-Nearest Neighbors
Model Validation: Assessed model robustness using y-scrambling tests and evaluated applicability domain using three different methods
This rigorous approach resulted in 7 models with positive predictive values higher than 0.85 in both nested cross-validation and external testing, all utilizing the Random Forest algorithm with specific descriptor sets including topological descriptors, information indices, and 2D-autocorrelation descriptors [41].
Table 2: Key Research Reagents and Computational Tools for Cross-Validation in Cancer QSAR Studies
| Tool/Resource | Type | Primary Function | Application Context |
|---|---|---|---|
| Double Cross-Validation Software Tool | Software | MLR and PLS model development using DCV | Open-access tool for building predictive QSAR models with proper validation [74] |
| Dragon Software | Descriptor Calculator | Molecular descriptor calculation | Generates 13+ blocks of molecular descriptors for QSAR modeling [41] |
| R Statistical Environment | Programming Platform | Data preprocessing and machine learning implementation | Hosts 'mlr', 'randomForest', and 'rminer' packages for model development [41] |
| ChemAxon Standardizer | Chemical Informatics | Molecular structure standardization | Prepares consistent molecular representations from SMILES strings [41] |
| PMC Database | Literature Resource | Access to scientific literature on validation methods | Source of validated methodologies and comparative studies [18] [93] [41] |
Implications for Cancer Research and Drug Development
The consistent demonstration of performance inflation in single cross-validation across multiple cancer research domains carries significant implications for predictive modeling in oncology. In practical terms, the overoptimistic performance estimates from single cross-validation could lead to:
- Misallocation of Research Resources: Advancement of compound candidates with poor actual efficacy
- Reduced Reproducibility: Models that perform well in validation but fail in external applications
- Inefficient Algorithm Selection: Preference for methods that overfit the specific dataset rather than generalize well
The implementation of double cross-validation addresses these concerns by providing a more rigorous framework for model evaluation, ultimately leading to more reliable predictions and better decision-making in cancer drug discovery. As noted in one comprehensive analysis, "as compared to a single test set, double cross-validation provided a more realistic picture of model quality and should be preferred over a single test set" [18] [7].
This validation rigor is particularly crucial in contexts where models will be applied across diverse experimental conditions or patient populations. The cross-study validation approach demonstrates that true generalizability requires assessment on completely independent datasets, a principle that double cross-validation incorporates by design through its strict separation of model selection and performance assessment [93].
The comparative evidence from cancer studies consistently demonstrates the superiority of double cross-validation over single cross-validation for providing realistic estimates of model performance. While single cross-validation remains useful for initial model development due to its computational efficiency, its tendency toward optimistic bias makes it unsuitable for final model assessment, particularly in high-dimensional QSAR problems common in cancer research.
Double cross-validation, through its nested structure that strictly separates model selection from performance estimation, provides a more rigorous validation framework that better approximates how models will perform on truly independent data. The implementation of this method, potentially enhanced through repetition to generate confidence intervals for performance metrics, represents a best practice for cancer QSAR studies where reliable generalization to novel compounds is essential for advancing therapeutic discovery.
As the field moves toward increasingly complex models and datasets, the adoption of robust validation methodologies like double cross-validation will be crucial for maintaining scientific rigor and generating clinically relevant predictions in oncology research.
In the field of cancer research, Quantitative Structure-Activity Relationship (QSAR) modeling serves as a pivotal computational technique for linking the chemical structures of compounds to their biological activity, thereby accelerating the discovery of new anticancer drugs [13]. The core objective of a QSAR model is to predict the activity of new, untested compounds reliably. Since these models are used for virtual screening and prioritizing compounds for synthesis, establishing their predictive reliability is paramount [19]. This is achieved through rigorous validation, a process that moves beyond simply fitting data to assessing how well the model will perform in a real-world discovery setting [7]. Among the various validation strategies, internal validation (e.g., Leave-One-Out (LOO) and Leave-Many-Out (LMO) cross-validation), external validation, and the use of specific metrics like the coefficient of determination (r²), cross-validated correlation coefficient (q²), and external predictive correlation coefficient (r²pred) form the cornerstone of model assessment [20] [7]. This guide provides a comparative analysis of these key metrics, framed within the context of cross-validation techniques for cancer QSAR models, to aid researchers in evaluating model robustness and predictive power.
Defining the Key Validation Metrics
The Coefficient of Determination (r²)
The r² metric, also known as the squared correlation coefficient, is a fundamental statistic that defines the goodness-of-fit of a QSAR model. It quantifies the proportion of variance in the dependent variable (biological activity) that is predictable from the independent variables (molecular descriptors) within the training set [20]. An r² value close to 1.0 indicates that the model successfully explains most of the variance in the training data. For instance, in a QSAR study on porphyrin-based photosensitizers for cancer therapy, a model with an r² value of 0.87 was considered acceptable, demonstrating a strong fit to the training data [20]. However, a high r² alone is insufficient to confirm a model's predictive capability, as it can be artificially inflated by overfitting, especially when the model uses too many descriptors for a small set of compounds [19] [7].
The Cross-Validated Correlation Coefficient (q²)
The q² statistic, derived from internal cross-validation methods like Leave-One-Out (LOO) or Leave-Many-Out (LMO), is a primary indicator of a model's internal predictive ability [20] [7]. In LOO cross-validation, one compound is repeatedly removed from the training set, the model is rebuilt with the remaining compounds, and the activity of the left-out compound is predicted. The q² value is calculated based on the sum of squared differences between the actual and predicted activities of all left-out compounds [20]. This process helps assess the model's stability and its ability to make predictions for compounds not included in the model building phase, thereby providing a guard against overfitting. A q² value greater than 0.5 is generally considered acceptable, indicating reasonable internal predictability [20]. For example, a 3D-QSAR model for phenylindole derivatives as breast cancer inhibitors reported a high q² of 0.814, demonstrating robust internal predictive power [95].
The External Predictive Correlation Coefficient (r²pred)
The r²pred metric is the gold standard for evaluating a model's true external predictive power [19] [7]. This assessment involves splitting the available data into a training set, used exclusively to build the model, and a test set, used solely for validation. The final model, built on the training set, is used to predict the activities of the test set compounds. The r²pred is then calculated similarly to r² but using the test set's experimental versus predicted values [20]. This method provides an unbiased estimate of how the model will perform on genuinely new data. A study on anti-breast cancer combinational QSAR models emphasized the importance of external validation, using a hold-out test set to calculate performance metrics like R² and RMSE for the final model assessment [96]. The value of r²pred is critical for confirming that a model is not just a self-consistent mathematical construct but a tool with practical utility in forecasting the activity of not-yet-synthesized compounds [19].
Table 1: Core Definitions and Characteristics of Key QSAR Validation Metrics
| Metric | Full Name | Validation Type | Primary Purpose | Interpretation (Typical Threshold) |
|---|---|---|---|---|
| r² | Coefficient of Determination | Goodness-of-Fit | Measures how well the model fits the training data | > 0.6 (Acceptable fit) [20] |
| q² | Cross-validated Correlation Coefficient | Internal Validation | Estimates internal predictability and model stability | > 0.5 (Acceptable predictability) [20] |
| r²pred | External Predictive Correlation Coefficient | External Validation | Assesses true, unbiased predictive power on new data | > 0.5 (Acceptable external predictivity) [20] |
Comparative Analysis of r², q², and r²(pred)
A comprehensive understanding of QSAR model validity requires a comparative analysis of r², q², and r²pred. These metrics offer complementary insights, and their collective interpretation is essential for a holistic model assessment.
Interrelationships and Comparative Insights
The relationship between these metrics often reveals the model's nature. A high r² coupled with a low q² is a classic symptom of overfitting, where the model has memorized the training data noise instead of learning the underlying structure [7]. Conversely, a high q² but a low r²pred suggests that the model, while stable internally, may fail to generalize to external data sets due to factors like an unrepresentative training set or data inconsistency [97]. Therefore, a reliable and predictive QSAR model should ideally exhibit high values for all three metrics—r², q², and r²pred—though r²pred is ultimately the most critical for practical application [19] [7]. Research has shown that relying on r² alone is inadequate for confirming model validity, and the established criteria for external validation, including r²pred, have their own advantages and disadvantages that must be considered [19].
Limitations and Best Practices
Each metric has limitations. The r² metric is highly sensitive to the training set composition and descriptor number. The q² metric can sometimes provide an over-optimistic view of predictability, particularly with small datasets or inappropriate validation designs [7]. The r²pred's reliability is contingent on a representative and sufficiently large test set. To mitigate these limitations, double cross-validation has been recommended as a robust method [7]. This nested procedure involves an outer loop for model assessment (estimating an overall predictive error) and an inner loop for model selection (tuning parameters), ensuring a more reliable and unbiased estimation of prediction errors under model uncertainty compared to a single train-test split [7].
Table 2: Comparative Strengths, Weaknesses, and Data Requirements
| Metric | Key Strengths | Key Weaknesses & Pitfalls | Data Splitting Requirement |
|---|---|---|---|
| r² | Simple, intuitive measure of model fit. | Highly susceptible to overfitting; does not indicate predictive ability. | None (uses entire training set). |
| q² | Guards against overfitting; estimates internal robustness. | Can be overly optimistic; value depends on cross-validation design. | Training set is partitioned internally (e.g., LOO, LMO). |
| r²pred | Provides the most realistic estimate of practical utility. | Requires withholding data; value can be sensitive to test set selection. | Data must be split into independent training and test sets. |
Experimental Protocols for Validation
Implementing robust experimental protocols for validation is as important as understanding the metrics themselves. Below are detailed methodologies for key validation experiments cited in cancer QSAR research.
Protocol for Leave-One-Out (LOO) Cross-Validation
LOO cross-validation is a widely used method for estimating q², particularly effective with small datasets [20].
- Model Training: For a dataset with n compounds, remove one compound to serve as the validation sample.
- Model Rebuilding: Use the remaining n-1 compounds to rebuild the QSAR model using the same modeling procedure (e.g., MLR, PLS).
- Prediction: Predict the biological activity of the removed compound using the newly built model.
- Iteration: Repeat steps 1-3 until every compound in the dataset has been left out and predicted exactly once.
- Calculation: Calculate the Predictive Sum of Squares (PRESS) as the sum of the squared differences between the actual and predicted activities for all n compounds.
PRESS = Σ(y_actual - y_predicted)² - Derive q²: Calculate the q² (or r²cv) using the following formula, where SSY is the total sum of squares of the experimental activities relative to their mean:
q² = 1 - (PRESS / SSY)
This protocol was used in a study on porphyrin derivatives, where a model with a q² value of 0.71 was deemed to have good internal predictive power [20].
Protocol for External Validation with r²pred
External validation is the definitive method for establishing a model's utility for virtual screening [19] [7].
- Data Splitting: Randomly divide the full dataset into a training set (typically 70-80%) and an external test set (20-30%). The test set must be held out and never used in any model building or descriptor selection steps [12].
- Model Development: Develop the final QSAR model using only the compounds in the training set. This includes all steps of descriptor calculation, selection, and model training.
- Prediction of Test Set: Use the finalized model from Step 2 to predict the biological activities of the compounds in the external test set.
- Calculation of r²pred: Calculate r²pred using the formula below, where yobs(test) and ypred(test) are the observed and predicted activities for the test set, and y_train is the mean activity of the training set [20].
r²pred = 1 - [ Σ(y_obs(test) - y_pred(test))² / Σ(y_obs(test) - y_train)² ]A study on 1,2,4-triazine-3(2H)-one derivatives for breast cancer employed an 80:20 training-to-test ratio, achieving a model with a high R² of 0.849, validated by this external prediction [12].
Protocol for Double Cross-Validation
Double cross-validation provides a rigorous framework for both model selection and error estimation, minimizing the risk of overfitting and model selection bias [7].
- Outer Loop (Model Assessment): Split the data into k folds (e.g., 5-fold). For each fold:
- Designate the fold as the temporary test set, and the remaining k-1 folds as the temporary training set.
- Inner Loop (Model Selection):
- Within the temporary training set, perform another cross-validation (e.g., LOO or 5-fold).
- Use this inner loop to optimize model parameters (e.g., select the best descriptor subset or number of components in PLS).
- Select the optimal model parameters based on the best performance in the inner loop.
- Final Model and Prediction:
- Rebuild a model on the entire temporary training set using the optimal parameters identified in the inner loop.
- Use this model to predict the temporary test set from the outer loop.
- Iteration and Final Error Estimate: Repeat steps for all k folds in the outer loop. The collection of predictions from all temporary test sets provides a reliable estimate of the model's prediction error [7].
Diagram: Double Cross-Validation Workflow. This illustrates the nested process for reliable error estimation.
The Scientist's Toolkit: Research Reagent Solutions
Building and validating robust cancer QSAR models requires a suite of computational tools and databases. The following table details essential "research reagents" for this field.
Table 3: Essential Computational Tools and Databases for Cancer QSAR Research
| Tool/Resource Name | Type | Primary Function in QSAR | Relevance to Cancer Research |
|---|---|---|---|
| Dragon Software | Descriptor Calculation | Calculates a wide array of molecular descriptors (e.g., topological, constitutional, functional groups) [19]. | Provides quantitative inputs for linking chemical structure to anticancer activity. |
| Gaussian 09W | Quantum Chemistry Software | Computes electronic structure and quantum chemical descriptors (e.g., EHOMO, ELUMO, electronegativity) [12]. | Used in studies on triazine derivatives to derive electronic descriptors critical for activity [12]. |
| ChEMBL | Public Bioactivity Database | Source of curated quantitative biological activity data for drug-like molecules [97] [13]. | Provides experimental bioactivity data (e.g., IC50) against cancer targets for model building. |
| GDSC2 Database | Cancer-Specific Database | Provides drug sensitivity data and combinational screening results across cancer cell lines [96]. | Used to build combinational QSAR models for breast cancer therapy [96]. |
| SYBYL | Molecular Modeling Suite | Used for 3D-QSAR analyses (e.g., CoMFA, CoMSIA), molecular alignment, and docking [95]. | Employed in developing 3D-QSAR models for phenylindole derivatives as MCF7 inhibitors [95]. |
| Scikit-learn (Python) | Machine Learning Library | Provides algorithms for regression (RF, XGBoost, SVR), data preprocessing, and cross-validation [96]. | Enables the application of ML/DL for developing modern, predictive combinational QSAR models [96]. |
The comparative analysis of r², q², and r²pred underscores a fundamental principle in QSAR modeling: a good fit does not guarantee a good prediction. While r² confirms the model is grounded in the training data, and q² checks for internal consistency and guards against overfitting, the r²pred metric is the ultimate arbiter of a model's practical value in a cancer drug discovery pipeline. Relying on any single metric is insufficient; a holistic validation strategy incorporating internal cross-validation and, crucially, external validation is non-negotiable for developing trustworthy QSAR models. Furthermore, advanced procedures like double cross-validation offer a more robust framework for obtaining reliable error estimates under model uncertainty. As QSAR continues to evolve with machine learning and complex data structures, adhering to these rigorous validation standards will be essential for translating computational predictions into successful experimental outcomes in oncology.
Benchmarking Target Prediction Methods for Cancer Drug Repurposing
The high failure rates and exorbitant costs associated with traditional oncology drug development have accelerated interest in computational drug repurposing, which identifies new therapeutic uses for existing drugs [98] [99]. This strategy leverages existing safety and efficacy data, potentially reducing development time from the typical 12-16 years to approximately 6 years and cutting costs from $1-2 billion to around $300 million [98]. Within this domain, accurate target prediction—identifying the specific molecular entities that drugs interact with—is fundamental for understanding mechanisms of action and unlocking new therapeutic applications [100].
Computational oncology faces a significant challenge: the "zero-shot" drug repurposing problem, where models must predict treatments for diseases that have sparse molecular data or no existing therapies [101]. This is particularly relevant for rare cancers and specific subtypes of common cancers where treatment options remain limited. Rigorous benchmarking of prediction methods using appropriate cross-validation techniques is therefore essential to assess model generalizability and reliability before clinical application [98].
This guide provides a systematic comparison of computational target prediction methods, focusing on their performance evaluation through cross-validation frameworks like Leave-One-Out (LOO) and Leave-Multiple-Out (LMO). We synthesize quantitative performance data, detail experimental protocols from key studies, and provide resources to facilitate method selection and implementation in cancer drug repurposing research.
Methodological Landscape of Prediction Approaches
Target prediction methods for drug repurposing can be broadly categorized into three algorithmic families: network-based, machine learning, and integrated approaches [102]. Network-based methods construct heterogeneous networks representing relationships among biomedical entities (drugs, diseases, proteins, etc.) and apply graph-theoretic algorithms to infer new associations [103] [102]. These methods operate on the "guilt-by-association" principle, assuming that similar drugs treat similar diseases [103]. Machine learning methods use known drug-target interactions and features of drugs and targets to build predictive models [102]. With advances in computational power, deep learning techniques have become increasingly prevalent for their ability to handle large, complex datasets [99] [104]. Integrated methods combine network and machine learning approaches, often using network-derived similarities as features in machine learning models [102].
A 2022 comparative analysis of drug-target interaction prediction methods found that integrated approaches generally outperform single-method categories, demonstrating superior prediction accuracy across multiple benchmarks [102]. This synergy between methodological paradigms highlights the value of hybrid frameworks in computational drug repurposing.
Table 1: Categories of Target Prediction Methods for Drug Repurposing
| Method Category | Underlying Principle | Key Algorithms | Strengths | Limitations |
|---|---|---|---|---|
| Network-Based | Infers associations based on topology of biological networks | Network propagation, random walks, matrix completion [103] | Provides systematic view of interaction patterns; captures complex relationships [102] | Performance depends on network completeness and quality [103] |
| Machine Learning | Learns patterns from known drug-target pairs to predict new interactions | Deep learning, matrix factorization, supervised classification [102] | High accuracy with sufficient training data; handles diverse feature types [102] | Risk of overfitting; limited performance on novel targets ("cold start" problem) [102] |
| Integrated | Combines network topology with machine learning prediction | Graph neural networks, similarity-based feature integration [101] [102] | Superior overall accuracy; leverages complementary information [102] | Increased computational complexity; more challenging interpretation [101] |
Benchmarking Frameworks and Cross-Validation Protocols
The Critical Role of Cross-Validation
In computational drug repurposing, cross-validation techniques are indispensable for evaluating model performance and generalizability. Leave-One-Out (LOO) and Leave-Multiple-Out (LMO) cross-validation provide robust frameworks for assessing how well models predict novel drug-disease associations not encountered during training [98].
LOO validation involves iteratively holding out a single drug-disease pair as a test case while training the model on all remaining pairs. This approach is particularly valuable for estimating performance on sparse datasets where positive examples are limited. LMO (also called k-fold cross-validation) withholds multiple pairs simultaneously, providing a more efficient validation strategy for larger datasets and enabling assessment of model performance on multiple unknown interactions [98].
These techniques are especially crucial for evaluating "zero-shot" prediction capabilities—a model's ability to identify therapeutic candidates for diseases with no known treatments [101]. TxGNN, a graph foundation model, addresses this challenge through metric learning that transfers knowledge from well-annotated diseases to those with limited treatment options, demonstrating a 49.2% improvement in indication prediction accuracy under stringent zero-shot evaluation compared to eight benchmark methods [101].
Standardized Evaluation Frameworks
The heterogeneity in evaluation methodologies across drug repurposing studies has complicated direct comparison of different approaches. To address this challenge, researchers have developed standardized benchmarking frameworks. HN-DREP provides a comprehensive evaluation of 28 heterogeneous network-based drug repositioning methods across 11 datasets, assessing performance, scalability, and usability [103]. This systematic approach revealed that methods relying on matrix completion or factorization (HGIMC, ITRPCA, BNNR) generally exhibit the best overall performance, while neural network-based approaches (HINGRL, MLMC) also demonstrate strong predictive capability [103].
For molecular target prediction specifically, a 2025 systematic comparison established a shared benchmark dataset of FDA-approved drugs to evaluate seven prediction methods (MolTarPred, PPB2, RF-QSAR, TargetNet, ChEMBL, CMTNN, and SuperPred) [100]. This study implemented rigorous cross-validation protocols and found that MolTarPred achieved superior performance, with optimization strategies such as high-confidence filtering further enhancing prediction reliability, though at the cost of reduced recall [100].
Performance Comparison of Prediction Methods
Quantitative Benchmarking Results
Table 2: Performance Comparison of Heterogeneous Network-Based Drug Repositioning Methods [103]
| Method Name | Algorithm Category | Performance Rank | Scalability Rank | Usability Rank | Key Strengths |
|---|---|---|---|---|---|
| HGIMC | Matrix Completion | 1 | - | 1 | Best overall performance and usability |
| ITRPCA | Matrix Completion | 2 | - | - | Strong overall performance |
| BNNR | Matrix Completion | 3 | - | 3 | Excellent performance and usability |
| HINGRL | Network Propagation | 4 | - | - | Top performance |
| MLMC | Matrix Completion | 5 | - | - | Strong performance |
| NMFDR | Matrix Factorization | - | 1 | - | Superior scalability |
| GROBMC | Matrix Completion | - | 2 | - | Excellent scalability |
| SCPMF | Matrix Factorization | - | 3 | - | Strong scalability |
| DRHGCN | Machine Learning (GCN) | - | - | 2 | High usability |
Table 3: Molecular Target Prediction Method Performance [100]
| Method | Type | Overall Performance | Recall | Key Findings |
|---|---|---|---|---|
| MolTarPred | Stand-alone code | Most effective | Varies with filtering | Morgan fingerprints with Tanimoto scores outperform MACCS with Dice scores |
| PPB2 | Web server | Competitive | - | - |
| RF-QSAR | QSAR-based | Competitive | - | - |
| TargetNet | Web server | Moderate | - | - |
| ChEMBL | Database-derived | Moderate | - | - |
| CMTNN | Neural network | Moderate | - | - |
| SuperPred | Web server | Moderate | - | - |
Integrated Methods Performance
The comparative analysis of drug-target interaction prediction methods revealed that integrated approaches consistently outperform single-method categories [102]. Methods like DTiGEMS+, which combine network-based features with supervised learning, achieved higher AUC values and F-scores compared to purely network-based (NetLapRLS, BLM-NII) or matrix factorization approaches (MSCMF, NRLMF) across multiple benchmark datasets [102].
This performance advantage stems from the ability of integrated methods to leverage both the topological information from biological networks and the pattern recognition capabilities of machine learning algorithms. However, the study also noted that prediction accuracy substantially decreases for "unknown drugs" not present in the training data, highlighting a persistent challenge in computational drug repurposing [102].
Experimental Protocols and Workflows
Systematic Benchmarking Methodology
The HN-DRES workflow provides a standardized Snakemake pipeline for benchmarking heterogeneous network-based drug repositioning methods [103]. This protocol encompasses several critical stages, beginning with data preparation from 11 diverse datasets, followed by method configuration and execution, and comprehensive evaluation across performance, scalability, and usability metrics.
Performance evaluation typically employs cross-validation techniques (LOO and LMO) with standard metrics including area under the receiver operating characteristic curve (AUROC), area under the precision-recall curve (AUPR), F1-score, and precision-recall break-even point (PRBEP) [103]. Scalability assessment measures computational time and memory usage across increasing dataset sizes, while usability evaluation considers code availability, documentation quality, and ease of implementation [103].
The following diagram illustrates the generalized experimental workflow for benchmarking target prediction methods:
Case Study: Fenofibric Acid Repurposing
A practical application of these benchmarking protocols is illustrated in a 2025 case study on fenofibric acid repurposing for thyroid cancer [100]. The study implemented a programmatic pipeline for target prediction and mechanism of action hypothesis generation, beginning with chemical similarity searching against approved drugs, followed by multi-method target prediction (with MolTarPred as the primary method), and culminating in experimental validation through binding assays and functional tests in thyroid cancer models [100].
This case study demonstrated how benchmarking results directly inform repurposing hypotheses, with the top-performing MolTarPred method correctly identifying thyroid hormone receptor beta (THRB) as a potential target of fenofibric acid, suggesting its repurposing potential for thyroid cancer treatment [100].
Research Reagent Solutions
Table 4: Essential Research Reagents and Resources for Experimental Validation
| Resource Category | Specific Examples | Function in Drug Repurposing Research |
|---|---|---|
| Knowledge Bases | DrugBank [102], KEGG [102], ClinicalTrials.gov [98] | Provide structured information on drugs, targets, pathways, and clinical trials |
| Interaction Databases | BindingDB [102], STITCH [102], SuperTarget [102] | Offer known drug-target interactions for benchmarking and validation |
| Computational Tools | HN-DRES [103], TxGNN [101], MolTarPred [100] | Provide standardized workflows and pretrained models for prediction |
| Compound Resources | FDA-approved drug libraries [100], Natural compound collections | Source of repurposing candidates for experimental screening |
| Validation Assays | In vitro binding assays, Cell-based viability tests, Animal disease models | Experimental confirmation of computational predictions |
Benchmarking studies consistently demonstrate that integrated computational methods—particularly those combining network-based and machine learning approaches—generally achieve superior performance in target prediction for cancer drug repurposing [103] [102]. Methods based on matrix completion (HGIMC, ITRPCA, BNNR) and graph neural networks (TxGNN) have shown exceptional capability in both general and zero-shot prediction scenarios [103] [101].
The implementation of rigorous cross-validation protocols such as LOO and LMO remains essential for proper method evaluation, particularly for assessing performance on novel drug-disease associations [98]. Standardized benchmarking frameworks like HN-DREP provide valuable resources for comparing method performance across multiple dimensions beyond simple accuracy, including scalability and usability [103].
As computational drug repurposing continues to evolve, the integration of more diverse data types, the development of improved zero-shot prediction capabilities, and the adoption of rigorous validation standards will be crucial for translating computational predictions into clinical applications. The methods and frameworks described in this guide provide a foundation for researchers to select appropriate prediction approaches based on their specific research context and requirements.
Regulatory Considerations and Best Practices for Validated Cancer QSAR Models
Quantitative Structure-Activity Relationship (QSAR) modeling represents a crucial computational methodology within New Approach Methodologies (NAMs) for predicting the carcinogenic potential of chemicals. These models mathematically correlate molecular structure descriptors with biological activity, enabling toxicity estimation based solely on chemical structural information and leveraging toxicity profiles of previously tested chemicals [23]. In regulatory science, QSAR applications for carcinogenicity assessment have gained significant importance for hazard identification of chemicals, particularly pesticides, pharmaceuticals, and environmental contaminants, with the potential to reduce reliance on traditional animal testing while ensuring thorough chemical risk evaluation [23] [105].
The regulatory acceptance of QSAR models for carcinogenicity assessment presents both opportunities and challenges. Although these alternative methods are foreseen in many regulatory frameworks, their acceptance by regulatory agencies to meet substance information requirements faces implementation hurdles [23]. The critical importance of proper validation and regulatory consideration stems from the profound implications of carcinogenicity assessments for public health decisions, chemical regulation, and drug development processes. This guide examines current regulatory expectations, validation methodologies, and comparative performance of established QSAR frameworks specifically for cancer endpoint prediction.
Regulatory Framework and Acceptance Criteria
Foundational Regulatory Principles
QSAR models intended for regulatory use must adhere to established principles set forth by international organizations. The Organization for Economic Co-operation and Development (OECD) principles for QSAR validation provide the foundational framework, requiring that models have: (1) a defined endpoint, (2) an unambiguous algorithm, (3) a defined domain of applicability, (4) appropriate measures of goodness-of-fit, robustness, and predictivity, and (5) a mechanistic interpretation, when possible [105] [106]. These principles ensure that models produce reliable, reproducible results suitable for regulatory decision-making.
Regulatory agencies worldwide increasingly recognize QSAR approaches in various legislative contexts. The European Chemicals Agency (ECHA) incorporates QSAR methodologies under REACH regulations to fill information gaps, while the European Food Safety Authority (EFSA) utilizes QSAR for pesticide risk assessment [23]. In the United States, the Environmental Protection Agency (EPA) employs QSAR models for chemical prioritization and risk assessment. The growing regulatory adoption stems from the need to evaluate carcinogenic potential for thousands of chemicals while minimizing animal testing and reducing assessment timelines [105].
Applicability Domain Considerations
The concept of Applicability Domain (AD) represents a critical component in regulatory QSAR acceptance. The AD defines the chemical space where the model's predictions are considered reliable, based on the structural and response similarity between the target chemical and compounds used in model training [23]. Regulatory applications require transparent definition and assessment of the applicability domain, as predictions for chemicals outside this domain carry higher uncertainty [23] [107]. Various approaches exist for defining applicability domains, including range-based methods (e.g., leverage method), distance-based methods, and structural fragment-based approaches, each with distinct advantages for regulatory implementation [108] [19].
Table 1: Key Regulatory Considerations for Cancer QSAR Models
| Regulatory Aspect | Implementation Requirement | Common Challenges |
|---|---|---|
| Applicability Domain | Transparent definition using standardized approaches | Inconsistent definitions across models; domain boundary quantification |
| Documentation | Complete model description per OECD principles | Proprietary algorithm limitations; insufficient mechanistic interpretation |
| Validation | Internal and external validation with appropriate metrics | Inadequate external test sets; overreliance on single metrics |
| Uncertainty Characterization | Quantitative or qualitative uncertainty estimates | Lack of standardized uncertainty reporting formats |
| Mechanistic Basis | Biological plausibility and alert identification | Complex carcinogenesis mechanisms; multiple pathways |
Validation Methodologies for Cancer QSAR Models
Cross-Validation Techniques
Cross-validation represents an essential internal validation procedure for assessing model robustness and predicting internal predictive performance. Leave-One-Out (LOO) and Leave-Many-Out (LMO, also known as k-fold cross-validation) are the most widely employed techniques in QSAR development [19] [109].
Leave-One-Out (LOO) Cross-Validation: This approach systematically removes one compound from the training set, builds the model with the remaining compounds, and predicts the omitted compound. The process repeats until each compound in the dataset has been excluded once. The predicted residual sum of squares (PRESS) is calculated and compared to the total sum of squares to derive cross-validated R² (Q²) [19]. While computationally intensive, LOO provides maximum usage of limited datasets, which is particularly valuable in cancer QSAR modeling where experimental carcinogenicity data is often scarce.
Leave-Many-Out (LMO) Cross-Validation: Also implemented as k-fold cross-validation, LMO removes a subset of compounds (typically 10-20% of the dataset) repeatedly until all compounds have been in the test set. This approach better simulates model performance on external compounds and provides a more realistic assessment of predictive ability [19] [109]. For optimal results in cancer QSAR, repeated k-fold cross-validation with multiple randomizations is recommended to account for dataset partitioning variability.
External Validation Protocols
External validation represents the gold standard for assessing model predictive power, utilizing compounds completely excluded from model development. Proper external validation requires careful dataset division, with typical splits allocating 70-80% of compounds for training and 20-30% for external testing [19] [105]. The external test set must represent structural diversity and activity ranges present in the training set while remaining strictly independent from model development and parameter optimization.
Multiple statistical metrics provide comprehensive assessment of model predictivity. The coefficient of determination for external prediction (r²ext) alone is insufficient for model validity assessment [19]. Additional metrics including root mean square error of prediction (RMSEP), mean absolute error (MAE), and concordance correlation coefficient (CCC) provide complementary assessment of predictive performance. For classification models, sensitivity, specificity, accuracy, and Matthews Correlation Coefficient (MCC) offer robust evaluation of categorical predictivity [105].
Table 2: Statistical Metrics for QSAR Model Validation
| Validation Type | Key Metrics | Acceptance Thresholds | Regulatory Relevance |
|---|---|---|---|
| Internal Validation | Q² (LOO/LMO) > 0.5; RMSECV | Q² > 0.5 (moderate)Q² > 0.7 (good)Q² > 0.9 (excellent) | Indicates model robustness; required for OECD compliance |
| External Validation | r²ext, RMSEP, MAE, CCC | r²ext > 0.6; CCC > 0.85 | Demonstrates predictive ability; regulatory expectation for adoption |
| Classification Performance | Sensitivity, Specificity, Accuracy, MCC | Balanced accuracy > 0.7; MCC > 0.3 | Critical for categorical carcinogenicity prediction |
| Applicability Domain | Leverage (h), Distance (D) | h ≤ h; D ≤ D | Defines model scope; regulatory requirement for appropriate use |
Advanced Validation: Conformal Prediction
Conformal prediction (CP) represents an advanced framework that provides confidence estimates alongside predictions, addressing a significant limitation of traditional QSAR approaches [107]. Unlike conventional models that output point estimates, CP generates prediction intervals with associated confidence levels, allowing users to quantify prediction uncertainty. This approach is particularly valuable for regulatory applications where understanding prediction reliability is essential. Mondrian Conformal Prediction (MCP) further extends this framework by ensuring validity within specific classes, making it suitable for imbalanced datasets common in carcinogenicity modeling [107].
Comparative studies between traditional QSAR and conformal prediction demonstrate distinct advantages for each approach. While traditional QSAR models often show slightly higher raw accuracy for high-confidence predictions, conformal prediction provides calibrated confidence measures that improve decision-making reliability [107]. Implementation of CP in regulatory settings enhances transparency by explicitly acknowledging and quantifying prediction uncertainty, facilitating more appropriate use of model outputs in weight-of-evidence assessments.
Comparative Analysis of Cancer QSAR Platforms
Established Software Tools
Several QSAR platforms have gained recognition for carcinogenicity prediction in regulatory and research contexts. The OECD QSAR Toolbox represents a comprehensive framework supporting chemical hazard assessment through data collection, trend analysis, and QSAR prediction [23] [106]. Its extensive database incorporates over 155,000 chemicals with approximately 3.3 million experimental data points, providing a robust foundation for carcinogenicity assessment. The Toolbox emphasizes mechanistic profiling through structural alerts and metabolic simulators, enhancing biological relevance of predictions [106].
The Danish (Q)SAR Platform offers specialized modules for toxicity endpoints, including carcinogenicity, with both database and model components [23]. This platform employs "battery calls" that aggregate predictions from multiple models (commercial, free, and DTU-developed) to enhance reliability through consensus approaches. The platform's transparent documentation and adherence to OECD principles support its regulatory application, particularly for pesticide assessment [23].
VEGA (Virtual models for property Evaluation of chemicals within a Global Architecture) provides freely available QSAR models specifically developed for carcinogenicity assessment, including innovative models for slope factor prediction [105]. These models demonstrate how hybrid approaches combining classification and regression can address both qualitative and quantitative carcinogenicity assessment needs. The platform's implementation of both Classification and Regression Tree (CART) models and artificial neural networks (ANNs) provides multiple approaches suitable for different regulatory contexts [105].
Performance Benchmarking
Comparative performance assessment reveals the relative strengths and limitations of different modeling approaches. Traditional linear methods like Multiple Linear Regression (MLR) provide interpretability but may lack predictive power for complex endpoints like carcinogenicity [108] [110]. Non-linear methods including Artificial Neural Networks (ANNs) and Support Vector Machines (SVMs) often demonstrate superior predictive performance but require larger datasets and careful validation to avoid overfitting [108].
In a comprehensive comparison spanning 550 human protein targets, both traditional QSAR and conformal prediction approaches demonstrated utility, with performance variations across different targets and confidence levels [107]. This large-scale evaluation highlighted that model performance is highly dependent on data quality, endpoint definition, and applicability domain considerations rather than algorithmic sophistication alone.
Table 3: Comparative Performance of Cancer QSAR Modeling Approaches
| Model/Platform | Endpoint Type | Reported Performance | Regulatory Application |
|---|---|---|---|
| VEGA CART Models [105] | Classification (Oral Carcinogenicity) | Accuracy: 0.76-0.81Sensitivity: 0.76-0.82Specificity: 0.76-0.79 | Chemical prioritization; evidence weighting |
| VEGA ANN Models [105] | Regression (Slope Factor) | r²: 0.57-0.65 (external)MAE: 0.85-0.95 | Quantitative risk assessment; potency estimation |
| Danish QSAR [23] | Battery Consensus | Variable by endpoint; leverages multiple models | Regulatory acceptance in EU for pesticides |
| 3D-QSAR (CoMSIA) [110] | Specific Target (PLK1 Inhibition) | q²: 0.628r²: 0.928 | Drug discovery; lead optimization |
| Conformal Prediction [107] | Multi-Target | Varies by confidence level; valid confidence calibration | Risk-based decision making |
Best Practices in Experimental Protocol Implementation
Data Curation and Preparation
Robust QSAR model development begins with comprehensive data curation. High-quality datasets must be compiled from reliable sources such as the Carcinogenic Potency Database (CPDB), ISSCAN, ECHA, and other validated repositories [23] [105]. Data preprocessing should address critical quality elements including duplicate removal, structural standardization, activity verification, and outlier detection. For carcinogenicity data specifically, careful attention to dose-response relationships, experimental protocols, and species-specific effects is essential for developing predictive models [105].
Activity data should represent consistent experimental protocols, preferably following OECD Test Guidelines 451 (Carcinogenicity Studies) and 453 (Combined Chronic Toxicity/Carcinogenicity Studies) when utilizing animal data [105]. For specific cancer targets, half-maximal inhibitory concentration (IC₅₀) values should be obtained through standardized assays with documented protocols [110]. The use of pChEMBL values (-logIC₅₀) standardizes activity measurements across different experimental systems and facilitates model development [107].
Model Development Workflow
A systematic workflow ensures development of robust, regulatory-compliant QSAR models. The process initiates with explicit endpoint definition, progressing through descriptor calculation, model training, validation, and applicability domain characterization [108] [109]. Feature selection represents a critical step, with appropriate methods (filter, wrapper, or embedded approaches) identifying optimal descriptor subsets that balance predictive performance and interpretability [108] [110].
For cancer QSAR specifically, incorporation of mechanistic understanding enhances regulatory acceptance. This includes identification of structural alerts associated with known carcinogenesis mechanisms such as DNA reactivity, endocrine disruption, or receptor-mediated effects [23] [105]. The integration of metabolic activation pathways further improves biological relevance, as implemented in tools like the OECD QSAR Toolbox's metabolism simulators [106].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Resources for Cancer QSAR Research
| Resource Category | Specific Tools | Application in Cancer QSAR |
|---|---|---|
| Software Platforms | OECD QSAR Toolbox, Danish QSAR, VEGA, Dragon, RDKit | Chemical profiling, descriptor calculation, model development |
| Data Resources | CPDB, ISSCAN, ChEMBL, PubChem, RAIS Database | Experimental carcinogenicity data for model training/validation |
| Descriptor Software | PaDEL-Descriptor, Dragon, RDKit, Mordred | Molecular descriptor calculation for structure-activity modeling |
| Modeling Algorithms | Multiple Linear Regression (MLR), Partial Least Squares (PLS), Artificial Neural Networks (ANN), Support Vector Machines (SVM) | Model development with varying complexity and interpretability |
| Validation Tools | Custom scripts, R/Python packages, KNIME, Orange | Performance assessment and model validation |
Regulatory-quality cancer QSAR models require rigorous validation through both internal (LOO, LMO) and external procedures, transparent definition of applicability domains, and comprehensive performance characterization. The integration of traditional QSAR with emerging approaches like conformal prediction represents a promising direction for enhancing regulatory decision-making through uncertainty quantification [107]. As regulatory agencies continue to advance NAM adoption, standardized validation protocols and performance benchmarks will further strengthen the role of QSAR in carcinogenicity assessment. Future developments will likely focus on integrating diverse data streams (in vitro, in chemico, in silico) within weight-of-evidence frameworks, enhancing model reliability and regulatory acceptance for cancer risk assessment [23] [105].
Conclusion
Effective cross-validation is paramount for developing reliable QSAR models in cancer drug discovery. While LOO and LMO provide essential internal validation, they represent just the beginning of a comprehensive validation strategy. The critical insight from recent research is that a high LOO q² value is necessary but insufficient to guarantee model predictive power, necessitating external validation as the definitive assessment. The adoption of advanced frameworks like double cross-validation addresses model uncertainty and selection bias, providing more realistic error estimates. Future directions should focus on integrating AI and machine learning with robust validation protocols, expanding applicability domain characterization, and developing standardized validation benchmarks specific to oncology applications. By implementing these comprehensive validation strategies, researchers can significantly enhance the translation of computational predictions into successful cancer therapeutics, ultimately accelerating the drug discovery pipeline while reducing costly late-stage failures.
References
- 1. The importance of good practices and false hits for QSAR ... [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2023.1237655/full]
- 2. The Development, Validation, and Use of Quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3438292/]
- 3. One size does not fit all: revising traditional paradigms for ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-00948-y]
- 4. QSAR Regression Models for Predicting HMG-CoA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11597356/]
- 5. Predicting tissue distribution and tumor delivery of ... [https://www.sciencedirect.com/science/article/pii/S0168365924005546]
- 6. Quantitative Structure–Activity Relationship (QSAR) ... [https://www.sciencedirect.com/science/article/abs/pii/S016974390600061X]
- 7. Reliable estimation of prediction errors for QSAR models ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-014-0047-1]
- 8. Computational Investigations on the Natural Small ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145275/]
- 9. Structure-based QSAR Models to Predict Repeat Dose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8128699/]
- 10. Comparative Study of (Q)SAR Models for Predicting the ... [https://www.sciencedirect.com/science/article/pii/S3050620425000491]
- 11. QSAR and Molecular Docking Studies of Pyrimidine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8955476/]
- 12. one derivatives as tubulin inhibitors for breast cancer therapy [https://www.nature.com/articles/s41598-024-66877-2]
- 13. A (Comprehensive) Review of the Application ... [https://www.mdpi.com/2076-3417/15/3/1206]
- 14. Enhanced QSAR Model Performance by Integrating ... [https://www.mdpi.com/1420-3049/18/9/10789]
- 15. Quantitative structure–activity relationship study on potent ... [https://www.sciencedirect.com/science/article/pii/S2090123216300121]
- 16. QSAR, molecular docking and ADMET properties in silico ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8282965/]
- 17. AI-Integrated QSAR Modeling for Enhanced Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525248/]
- 18. Reliable estimation of prediction errors for QSAR models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4260165/]
- 19. Comparison of various methods for validity evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9396839/]
- 20. Validation of Quantitative Structure-Activity Relationship ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3257093/]
- 21. 3D-QSAR, molecular docking and ADMET studies of ... [https://www.sciencedirect.com/science/article/abs/pii/S0019452222003375]
- 22. Combining QSAR and Molecular Docking for the ... [https://www.mdpi.com/2076-3417/15/15/8134]
- 23. A Statistical Exploration of QSAR Models in Cancer Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030765/]
- 24. Quantitative Structure-Activity Relationship (QSAR) ... [https://www.sciencedirect.com/science/article/pii/S2211715623001273]
- 25. Machine learning-based QSAR modeling, molecular ... [https://www.sciencedirect.com/science/article/abs/pii/S0022286024013267]
- 26. Exploring QSPR in breast cancer drugs via entire ... [https://www.nature.com/articles/s41598-025-12179-0]
- 27. SMILES-based QSAR and molecular docking studies of ... [https://www.nature.com/articles/s41598-025-91338-9]
- 28. Datasets Construction and Development of QSAR Models ... [https://www.mdpi.com/2305-6304/11/9/785]
- 29. A precise comparison of molecular target prediction methods [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d5dd00199d]
- 30. Machine learning-driven QSAR modeling combined with ... [https://www.sciencedirect.com/science/article/abs/pii/S0968089625002731]
- 31. Cytotoxic Evaluation, Molecular Docking, and 2D-QSAR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9061032/]
- 32. A breast cancer-specific combinational QSAR model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10822965/]
- 33. 2-Amino Thiazole Derivatives as Prospective Aurora Kinase Inhibitors... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10666282/]
- 34. Cross Validation in Machine Learning [https://www.geeksforgeeks.org/machine-learning/cross-validation-machine-learning/]
- 35. 3.1. Cross-validation: evaluating estimator performance [https://scikit-learn.org/stable/modules/cross_validation.html]
- 36. A combined 2-D and 3-D QSAR , molecular docking study... modeling [https://bnrc.springeropen.com/articles/10.1186/s42269-022-00874-1]
- 37. Analogue-based approaches in anti- cancer compound modelling : the... [https://link.springer.com/article/10.1186/2191-2858-1-3]
- 38. discrete mathematics - Necessary but not sufficient [https://math.stackexchange.com/questions/3889176/necessary-but-not-sufficient]
- 39. Confusing Necessary for Sufficient - LSAT Discussion Forum [https://forum.powerscore.com/viewtopic.php?t=10242]
- 40. Evaluation of Machine Learning Based QSAR Models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11667287/]
- 41. Development of QSAR machine learning-based models to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6466999/]
- 42. Cross-validation FAQ • loo - Stan [https://mc-stan.org/loo/articles/online-only/faq.html]
- 43. Modelling methods and cross-validation variants in QSAR [https://pubmed.ncbi.nlm.nih.gov/30160175/]
- 44. A Quick Intro to Leave-One-Out Cross-Validation (LOOCV) [https://www.statology.org/leave-one-out-cross-validation/]
- 45. LOOCV for Evaluating Machine Learning Algorithms [https://www.machinelearningmastery.com/loocv-for-evaluating-machine-learning-algorithms/]
- 46. Leave-One-Out Cross-Validation Explained [https://medium.com/@pacosun/one-out-all-in-leave-one-out-cross-validation-explained-409df5ff6385]
- 47. Comparison of various methods for validity evaluation of ... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-022-00856-4]
- 48. QSAR modeling, molecular docking, dynamic simulation and ... [https://bjbas.springeropen.com/articles/10.1186/s43088-023-00451-z]
- 49. A Review of Quantitative Structure–Activity Relationship ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474327/]
- 50. Strategies for the drug development of cancer therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518319/]
- 51. QSAR modelling to predict structural features of certain ... [https://www.sciencedirect.com/science/article/pii/S2667022424000884]
- 52. Identification of pharmacophore synergism for optimization ... [https://www.sciencedirect.com/science/article/pii/S266702242500060X]
- 53. Design, synthesis, QSAR modelling and molecular ... [https://www.nature.com/articles/s41598-024-75100-1]
- 54. Synthesis, Anti-Proliferative Activity Evaluation and 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6017957/]
- 55. Potential anti-colon cancer agents: Molecular modelling, ... [https://www.sciencedirect.com/science/article/pii/S2707368824000487]
- 56. Enhanced photodynamic therapy of cancer using porphyrin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403052/]
- 57. Evaluation of the correlation between porphyrin ... [https://www.nature.com/articles/s41598-021-81725-3]
- 58. Machine learning-based bioactivity prediction of porphyrin ... [https://link.springer.com/article/10.1007/s43630-025-00733-8]
- 59. QSAR, pharmacophore modeling and molecular docking ... [https://fjps.springeropen.com/articles/10.1186/s43094-021-00380-7]
- 60. Data Article Computational investigation of structural- ... [https://www.sciencedirect.com/science/article/abs/pii/S2405830023001052]
- 61. K-nearest-neighbor algorithm to predict the survival time and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10690040/]
- 62. Comparative performance analysis of K-nearest neighbour ... [https://www.semanticscholar.org/paper/Comparative-performance-analysis-of-K-nearest-(KNN)-Uddin-Haque/19b42746abd48048ad04c8ebad3e24753ffaccc2]
- 63. Machine Learning-Driven QSAR Modeling of Anticancer ... [https://pubmed.ncbi.nlm.nih.gov/40447459/]
- 64. QSAR modeling of benzoquinone derivatives as 5- ... [https://www.sciencedirect.com/science/article/pii/S2213453018301241]
- 65. An optimized support vector machine for lung cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11700792/]
- 66. Utilizing random Forest QSAR models with optimized ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-017-1960-x]
- 67. Enhanced QSAR Model Performance by Integrating Structural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6270197/]
- 68. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 69. Design of novel potent selective survivin inhibitors using 2D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11467593/]
- 70. QSAR analysis on a large and diverse set of potent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9005662/]
- 71. insights from QSAR modeling, ADMET, molecular docking ... [https://www.sciencedirect.com/science/article/pii/S2590093525000578]
- 72. Quantitative Structure–Activity Relationship Evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8401583/]
- 73. A machine learning-Assisted QSAR and integrative ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525014209]
- 74. The “double cross-validation” software tool for MLR QSAR ... [https://www.sciencedirect.com/science/article/abs/pii/S0169743916303987]
- 75. Quantitative Structure–Activity Relationship Evaluation of ... [https://www.mdpi.com/1420-3049/26/16/4795]
- 76. Nested versus non-nested cross-validation [https://scikit-learn.org/stable/auto_examples/model_selection/plot_nested_cross_validation_iris.html]
- 77. QSAR and CoMFA analyses [https://www.sciencedirect.com/science/article/abs/pii/S0928098715002961]
- 78. Nested cross validation vs repeated k-fold [https://stats.stackexchange.com/questions/283303/nested-cross-validation-vs-repeated-k-fold]
- 79. Comparison of Different Approaches to Define the ... [https://www.mdpi.com/1420-3049/17/5/4791]
- 80. A general approach for determining applicability domain of ... [https://www.nature.com/articles/s41524-025-01573-x]
- 81. QSAR Evaluations to Unravel the Structural Features in Lysine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9332886/]
- 82. Combined interaction of fungicides binary mixtures [https://pmc.ncbi.nlm.nih.gov/articles/PMC11639718/]
- 83. Use of QSAR Global Models and Molecular Docking for ... [https://www.mdpi.com/1422-0067/21/1/19]
- 84. The Relevance of Goodness‐of‐fit, Robustness and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9787734/]
- 85. Modify Leave-One-Out Cross Validation by Moving ... [https://www.mdpi.com/2076-3417/10/7/2448]
- 86. Using Leave-one-out cross-validation for large data • loo - Stan [https://mc-stan.org/loo/articles/loo2-large-data.html]
- 87. A leave-one-out cross validation SAS macro for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4306627/]
- 88. Validation of QSAR Models | Basicmedical Key [https://basicmedicalkey.com/validation-of-qsar-models/]
- 89. Real external predictivity of QSAR models: how to evaluate it? Comparison of different validation criteria and proposal of using the concordance correlation coefficient - PubMed [https://pubmed.ncbi.nlm.nih.gov/21800825/]
- 90. Comments on the definition of the Q2 parameter for QSAR validation - PubMed [https://pubmed.ncbi.nlm.nih.gov/19527034/]
- 91. Assessment of Prediction Confidence and Domain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1277118/]
- 92. A QSAR Study of Environmental Estrogens Based on a ... [https://www.mdpi.com/1420-3049/17/5/6126]
- 93. Cross-study validation for the assessment of prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4058929/]
- 94. Repeated double cross-validation applied to the PCA-LDA ... [https://link.springer.com/article/10.1007/s00216-020-03093-7]
- 95. Insights from 3D-QSAR, molecular docking, and dynamics for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0326245]
- 96. A breast cancer-specific combinational QSAR model ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2023.1328262/full]
- 97. Case Study for HIV-1 Reverse Transcriptase Inhibitors [https://pmc.ncbi.nlm.nih.gov/articles/PMC7738000/]
- 98. Validation approaches for computational drug repurposing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10785886/]
- 99. Exploring Artificial Intelligence's Potential to Enhance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582507/]
- 100. A precise comparison of molecular target prediction methods [https://pubs.rsc.org/en/content/articlelanding/2025/dd/d5dd00199d]
- 101. A foundation model for clinician-centered drug repurposing [https://www.nature.com/articles/s41591-024-03233-x]
- 102. Comparative analysis of network-based approaches and ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202321002474]
- 103. A comparative benchmarking and evaluation framework for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11033846/]
- 104. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 105. QSAR Models for Human Carcinogenicity: An Assessment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7796303/]
- 106. QSAR Toolbox [https://qsartoolbox.org/]
- 107. Large scale comparison of QSAR and conformal prediction ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-018-0325-4]
- 108. Advancing QSAR models in drug discovery for best ... [https://www.sciencedirect.com/science/article/abs/pii/S0169743925002291]
- 109. A Beginner's Guide to QSAR Modeling in Cheminformatics ... [https://neovarsity.org/blogs/cheminformatics-qsar-beginner-guides]
- 110. Exploration of 2D and 3D-QSAR analysis and docking studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10501407/]