Benchmarking Virtual Screening for Breast Cancer Subtypes: Methods, Challenges, and AI-Driven Advances
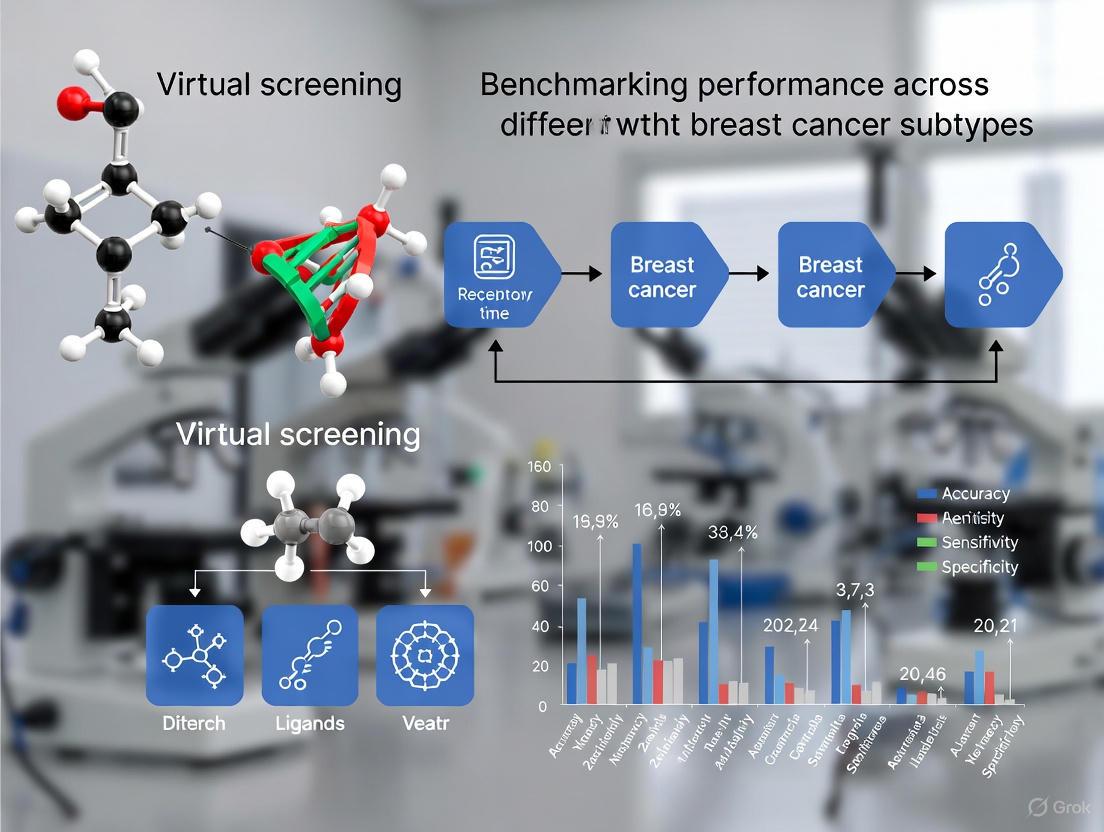
This article provides a comprehensive analysis of benchmarking virtual screening (VS) performance across the major molecular subtypes of breast cancer—Luminal, HER2-positive, and Triple-Negative Breast Cancer (TNBC).
Benchmarking Virtual Screening for Breast Cancer Subtypes: Methods, Challenges, and AI-Driven Advances
Abstract
This article provides a comprehensive analysis of benchmarking virtual screening (VS) performance across the major molecular subtypes of breast cancer—Luminal, HER2-positive, and Triple-Negative Breast Cancer (TNBC). It explores the foundational need for subtype-specific VS strategies due to distinct therapeutic vulnerabilities and target landscapes. The content details the application of core computational methodologies, including molecular docking, pharmacophore modeling, AI-accelerated platforms, and molecular dynamics, highlighting their use in discovering subtype-specific inhibitors. Significant challenges such as tumor heterogeneity, data leakage in benchmarks, and scoring function inaccuracies are addressed, alongside optimization strategies like flexible receptor docking and active learning. The article further examines validation protocols, from retrospective benchmarks like DUD and CASF to experimental confirmation via X-ray crystallography and cell-based assays. Aimed at researchers and drug development professionals, this review synthesizes current best practices and future directions for developing more precise and effective computational drug discovery pipelines in oncology.
The Imperative for Subtype-Specific Virtual Screening in Breast Cancer
Breast cancer is not a single disease but a collection of malignancies with distinct molecular features, clinical behaviors, and therapeutic responses. This heterogeneity has profound implications for prognosis and treatment selection, necessitating robust classification systems that guide clinical decision-making and drug development. The most widely recognized framework categorizes breast cancer into four principal molecular subtypes—Luminal A, Luminal B, HER2-positive (HER2-enriched), and Triple-Negative Breast Cancer (TNBC)—based on the expression of hormone receptors (estrogen receptor [ER] and progesterone receptor [PR]), human epidermal growth factor receptor 2 (HER2), and the proliferation marker Ki-67 [1] [2] [3]. This guide provides a comparative analysis of these subtypes, detailing their pathological characteristics, associated signaling pathways, and standard treatment modalities. Furthermore, it situates this biological overview within the context of modern computational drug discovery, illustrating how virtual screening and computer-aided drug design (CADD) are being leveraged to target subtype-specific vulnerabilities.
Molecular and Clinical Characteristics of Breast Cancer Subtypes
The classification of breast cancer into intrinsic molecular subtypes has revolutionized both prognostic assessment and therapeutic strategies. The table below summarizes the defining Pathological and Clinical Characteristics of each major subtype.
Table 1: Pathological and Clinical Characteristics of Major Breast Cancer Subtypes
| Characteristic | Luminal A | Luminal B | HER2-Positive | Triple-Negative (TNBC) |
|---|---|---|---|---|
| ER Status | Positive [1] [2] | Positive (often lower levels) [1] [3] | Usually Negative [1] [4] | Negative [1] [5] |
| PR Status | Positive [1] [2] | Negative or Low [1] [2] | Negative [1] | Negative [1] [5] |
| HER2 Status | Negative [1] [2] | Positive or Negative [2] [3] | Positive (Overexpression/Amplification) [1] [4] | Negative [1] [5] |
| Ki-67 Level | Low (<20%) [1] | High (≥20%) [1] | Variable, often high [1] | High [2] [5] |
| Approx. Prevalence | 50-60% [2] [3] | 15-20% [2] [3] | 10-15% [1] [2] | 10-20% [1] [3] |
| Common Treatments | Endocrine Therapy (e.g., Tamoxifen, AIs) [1] [6] | Endocrine Therapy + Chemotherapy ± Anti-HER2 [1] [3] | Chemotherapy + Anti-HER2 Therapy (e.g., Trastuzumab) [1] [2] | Chemotherapy ± Immunotherapy [6] [5] |
| Prognosis | Best prognosis [1] [2] | Intermediate prognosis [1] [3] | Good prognosis with targeted therapy [2] [4] | Poor prognosis, more aggressive [1] [5] |
Subtype-Specific Signaling Pathways and Therapeutic Targets
The clinical behavior of each subtype is driven by distinct underlying molecular pathways. Targeting these pathways is the cornerstone of precision oncology in breast cancer. The following diagram illustrates the core signaling pathways and associated targeted therapies for the major subtypes.
Computational Approaches for Subtype-Specific Drug Discovery
The heterogeneity of breast cancer demands tailored therapeutic development. Computational methods, particularly virtual screening and computer-aided drug design (CADD), have emerged as powerful tools for efficiently identifying and optimizing subtype-specific drugs.
Key Methodologies and Workflows
Virtual screening employs structure-based or ligand-based approaches to computationally screen large libraries of compounds for potential activity against a specific target [6] [7]. A standard structure-based workflow for identifying novel HER2 inhibitors, as exemplified by a study screening natural products, is outlined below [8].
Table 2: Key Virtual Screening and CADD Methodologies
| Method Category | Description | Application Example |
|---|---|---|
| Structure-Based Virtual Screening | Docking compounds from large libraries into the 3D structure of a target protein to predict binding affinity and pose [8] [7]. | Screening 638,960 natural products against the HER2 tyrosine kinase domain [8]. |
| Molecular Dynamics (MD) Simulations | Simulating the physical movements of atoms and molecules over time to assess the stability of protein-ligand complexes and refine binding models [8] [7]. | Validating the binding stability of the natural product liquiritin to HER2 [8]. |
| Pharmacophore Modeling | Identifying the essential 3D arrangement of molecular features (e.g., hydrogen bond donors/acceptors, hydrophobic regions) necessary for biological activity [7]. | Used in CADD campaigns for luminal breast cancer to design novel ER-targeting agents [7]. |
| AI/Machine Learning in Drug Design | Using predictive models to triage chemical space, forecast drug-target interactions, and optimize pharmacokinetic properties [6] [7]. | Predicting novel drug candidates and biomarkers by integrating multi-omics data across breast cancer subtypes [6]. |
Successful execution of computational and experimental research on breast cancer subtypes relies on a suite of key reagents, databases, and software tools.
Table 3: Essential Research Reagents and Resources for Breast Cancer Subtype Research
| Resource Category | Specific Example | Function and Application |
|---|---|---|
| Protein Structure Database | RCSB Protein Data Bank (PDB) | Source of 3D protein structures (e.g., PDB ID 3RCD for HER2) for structure-based virtual screening and molecular docking [8]. |
| Compound Libraries | COCONUT, ZINC Natural Products | Large-scale, commercially available libraries of small molecules or natural products used for virtual screening campaigns [8]. |
| Computational Software | Schrödinger Suite (Maestro) | Integrated software platform for protein preparation (Protein Prep Wizard), molecular docking (Glide), and ADMET prediction (QikProp) [8] [7]. |
| Cell Line Models | HER2+ Cell Lines (e.g., SK-BR-3) | Preclinical in vitro models representing specific subtypes (e.g., HER2-overexpressing) for validating the anti-proliferative effects of computationally identified hits [8]. |
| Clinical Biomarker Assays | Immunohistochemistry (IHC) for ER, PR, HER2, Ki-67 | Standard clinical methods for defining breast cancer subtypes by measuring protein expression levels in tumor tissue [1] [5]. |
Benchmarking Virtual Screening Performance Across Subtypes
The application and performance of virtual screening can vary significantly across different breast cancer subtypes, primarily due to differences in target availability and characterization.
Subtype-Specific CADD Applications and Experimental Protocols
Luminal A & B (ER-Positive): The primary target is the estrogen receptor (ER). CADD efforts have been highly successful in developing Selective Estrogen Receptor Modulators (SERMs) and Degraders (SERDs). A common protocol involves docking compounds into the ligand-binding domain of ERα to identify novel antagonists or degraders. For instance, virtual screening of colchicine-based compounds followed by Molecular Mechanics/Generalized Born Surface Area (MM/GBSA) calculations identified candidates with higher predicted binding affinity than tamoxifen [9] [7]. Subsequent molecular dynamics simulations (e.g., 100-200 ns) are used to confirm the thermodynamic stability of the ligand-ER complex [9].
HER2-Positive (HER2-Enriched): The HER2 tyrosine kinase is a well-defined, druggable target. The standard protocol, as detailed in a study discovering natural HER2 inhibitors, involves a hierarchical docking workflow [8]. First, a large compound library is screened using High-Throughput Virtual Screening (HTVS). Top hits are refined with Standard Precision (SP) docking, and the best are subjected to more computationally intensive Extra Precision (XP) docking. The final top-ranking compounds undergo molecular dynamics simulations (e.g., 100 ns) to validate binding mode stability, followed by MM-GBSA calculations to estimate binding free energy [8]. Successful hits are then tested in biochemical kinase inhibition assays and cellular proliferation assays using HER2-overexpressing cell lines.
Triple-Negative Breast Cancer (TNBC): The lack of classic targets makes TNBC a challenge. Research often focuses on targeting non-classical vulnerabilities, such as:
- Androgen Receptor (AR) in the LAR subtype: Using virtual screening to identify AR antagonists [5] [7].
- DNA Damage Response Pathways: Targeting BRCAness and homologous recombination deficiency (HRD) with PARP inhibitors, which can be identified and optimized using CADD [5] [7].
- Immunomodulatory Targets: AI and network-based methods analyze multi-omics data to identify immune checkpoints or other immunomodulatory targets for combination therapies [6] [5]. The experimental protocol often includes network pharmacology to map compound-gene-disease interactions, followed by validation in TNBC cell line panels representing different transcriptomic subsets (e.g., basal-like 1, mesenchymal, LAR) [5].
Comparative Analysis of Computational Challenges
Table 4: Benchmarking Virtual Screening Across Breast Cancer Subtypes
| Subtype | Prominent CADD Targets | Strengths of CADD Approach | Key Challenges & Research Gaps |
|---|---|---|---|
| Luminal (A/B) | Estrogen Receptor (ERα), CDK4/6, ESR1 mutants [7]. | Well-characterized, structured ligand-binding domain highly amenable to docking; Success in developing clinical-grade SERDs [9] [7]. | Overcoming therapy resistance due to ESR1 mutations and pathway rewiring requires modeling receptor plasticity [7]. |
| HER2-Positive | HER2 Tyrosine Kinase domain, extracellular domain [8] [4]. | High-resolution crystal structures available; Clear definition of ATP-binding site enables successful structure-based screening [8] [7]. | Tumor heterogeneity and brain metastases; Need for inhibitors overcoming resistance via alternative pathways (e.g., PI3K) [4] [7]. |
| TNBC | AR (LAR), PARP1/2, PI3K, PD-L1, various kinases [5] [7]. | Opportunity for novel target discovery; Network-based and AI methods can uncover hidden vulnerabilities from multi-omics data [6] [5]. | Target scarcity and high heterogeneity; Lack of a single dominant driver complicates target selection; Limited clinical success of candidates [5] [7]. |
Breast cancer remains a leading cause of cancer-related mortality among women worldwide, with therapeutic resistance representing a fundamental barrier to improving patient outcomes [10] [11]. Despite significant advances in targeted therapies and treatment modalities, resistance mechanisms enable cancer cells to evade destruction, leading to disease progression and recurrence [12]. This challenge is particularly acute in triple-negative breast cancer (TNBC), where target scarcity—the lack of defined molecular targets such as hormone receptors or HER2—severely limits treatment options [10] [7]. The complex interplay of genetic, epigenetic, metabolic, and microenvironmental factors drives resistance through dynamic adaptations that allow cancer cells to survive therapeutic assaults [13] [11].
Computational approaches, particularly virtual screening and artificial intelligence (AI), have emerged as powerful strategies to address these challenges [7] [11]. By leveraging molecular modeling, machine learning, and multi-omics data integration, researchers can identify novel therapeutic vulnerabilities and predict resistance mechanisms before they manifest clinically [14] [7]. This review benchmarks current computational methodologies across breast cancer subtypes, evaluating their performance in overcoming resistance and identifying new targets in traditionally challenging contexts like TNBC.
Molecular Mechanisms of Resistance Across Breast Cancer Subtypes
Genetic and Epigenetic Alterations
Therapeutic resistance in breast cancer arises through complex genetic and epigenetic reprogramming. Key driver mutations include ESR1 mutations in luminal subtypes, which confer resistance to endocrine therapies by enabling ligand-independent activation of estrogen receptor signaling [15] [7]. In HER2-positive disease, PIK3CA mutations activate alternative signaling pathways that bypass HER2 blockade, while TNBC frequently exhibits TP53 mutations and germline BRCA deficiencies that promote genomic instability and adaptive resistance [14] [10] [7]. Beyond genetic changes, epigenetic modifications such as DNA methylation, histone alterations, and non-coding RNA dysregulation reprogram gene expression patterns to support survival under therapeutic pressure [12].
Cancer Stem Cells and Tumor Microenvironment
Cancer stem cells (CSCs) represent a functionally resilient subpopulation capable of driving tumor initiation, progression, and therapy resistance [13]. These cells demonstrate enhanced DNA repair capacity, efficient drug efflux mechanisms, and metabolic plasticity that collectively enable survival after conventional treatments [13]. The tumor microenvironment (TME) further reinforces resistance through stromal cell interactions, immune evasion, and metabolic symbiosis [10] [16]. Nutrient competition, hypoxia-driven signaling, and lactate accumulation within the TME create protective niches that shield resistant cells from therapeutic effects [16] [11].
Metabolic Reprogramming
Metabolic adaptation represents a cornerstone of resistance across breast cancer subtypes [16]. Hormone receptor-positive tumors exhibit dependencies on fatty acid oxidation and mitochondrial biogenesis, while HER2-positive cancers leverage enhanced glycolytic flux and HER2-mediated metabolic signaling [16]. TNBC demonstrates remarkable metabolic plasticity, dynamically shifting between glycolysis, oxidative phosphorylation, and glutamine metabolism to survive under diverse conditions [13] [16]. These subtype-specific metabolic dependencies represent promising therapeutic targets for overcoming resistance.
Computational Strategies for Overcoming Resistance
Virtual Screening and Computer-Aided Drug Design
Computer-aided drug design (CADD) has emerged as a transformative approach for addressing resistance across breast cancer subtypes [7]. Structure-based methods including molecular docking, virtual screening, and molecular dynamics simulations enable rational drug design against resistance-conferring mutations [7]. For luminal breast cancer, CADD has facilitated development of next-generation selective estrogen receptor degraders (SERDs) effective against ESR1-mutant tumors [7]. In HER2-positive disease, computational approaches guide antibody engineering and kinase inhibitor optimization to overcome pathway reactivation [7]. For TNBC, virtual screening identifies compounds targeting DNA repair pathways and epigenetic regulators to address target scarcity [7].
AI-enabled workflows represent a recent advancement, with deep learning models rapidly triaging chemical space while physics-based simulations provide mechanistic validation [7]. Generative models propose novel chemical entities aligned with pharmacological requirements, feeding candidates into refinement loops for optimized therapeutic efficacy [7].
Deep Learning for Diagnostic and Predictive Biomarkers
Deep learning approaches applied to medical imaging and digital pathology demonstrate growing capability for non-invasive resistance prediction [17] [18]. The DenseNet121-CBAM model achieves area under curve (AUC) values of 0.759 for distinguishing Luminal versus non-Luminal subtypes and 0.668 for identifying triple-negative breast cancer directly from mammography images [17]. For multiclass classification across five molecular subtypes, the system shows superior performance in detecting HER2+/HR− (AUC = 0.78) and triple-negative (AUC = 0.72) subtypes [17]. These imaging-based predictors offer non-invasive alternatives to biopsy for monitoring tumor evolution and detecting emerging resistance.
Virtual staining represents another computational breakthrough, using deep generative models to create immunohistochemistry (IHC) images directly from hematoxylin and eosin (H&E) stained samples [18]. This approach preserves tissue specimens while reducing turnaround time and resource requirements for biomarker assessment [18]. Generative adversarial networks (GANs) and contrastive learning approaches have demonstrated particular effectiveness for this image-to-image translation task [18].
Liquid Biopsy and Circulating Tumor DNA Analysis
Liquid biopsy approaches leveraging circulating tumor DNA (ctDNA) enable real-time monitoring of resistance evolution [14] [15]. The SERENA-6 trial demonstrated that ctDNA analysis can detect emerging ESR1 mutations in hormone receptor-positive breast cancer months before standard imaging shows progression [15]. This early detection enables timely intervention with targeted therapies like camizestrant, potentially delaying resistance emergence [15]. In TNBC, the PREDICT-DNA trial established that ctDNA-negative status after neoadjuvant therapy correlates with excellent prognosis, suggesting utility for risk stratification and adjuvant therapy guidance [15].
Table 1: Performance Benchmarking of Computational Methods Across Breast Cancer Subtypes
| Method Category | Specific Approach | Luminal Performance | HER2+ Performance | TNBC Performance | Primary Application |
|---|---|---|---|---|---|
| Deep Learning Imaging | DenseNet121-CBAM (Mammography) | AUC: 0.759 (Luminal vs non-Luminal) | AUC: 0.658 (HER2 status) | AUC: 0.668 (TN vs non-TN) | Molecular subtype prediction |
| Virtual Staining | H&E to IHC Translation | High accuracy for ER/PR prediction | HER2 virtual staining under validation | Emerging for Ki-67 assessment | Biomarker preservation |
| Liquid Biopsy | ctDNA mutation detection | ESR1 mutations: 5.3 months lead time | HER2 mutations: Detectable pre-progression | Limited validation | Early resistance detection |
| CADD | Molecular docking & dynamics | SERDs development (elacestrant, camizestrant) | HER2 degraders & kinase inhibitors | PARP inhibitors & novel targets | Overcoming target scarcity |
Experimental Protocols for Key Methodologies
Deep Learning Model Development for Subtype Prediction
The DenseNet121-CBAM architecture provides a validated protocol for predicting molecular subtypes from mammography images [17]. This approach integrates Convolutional Block Attention Modules (CBAM) with DenseNet121 backbone for enhanced feature extraction [17].
Data Preprocessing Workflow:
- Image Acquisition: Full-field digital mammography images acquired with spatial resolution of 7 lp/mm, stored in DICOM format [17]
- Region of Interest Annotation: Two qualified radiologists independently annotate tumor areas using ITK-SNAP software, with inter-observer variability assessment [17]
- ROI Expansion: Annotated tumor regions expanded outward by specified pixel values to capture peritumoral features, then resized to square dimensions (224×224 pixels) [17]
- Class Imbalance Handling: Simple random oversampling applied with subtype-specific rates (Luminal: 1.3×, TNBC: 1.7×, HER2: 1.5×) [17]
- Data Augmentation: Geometric transformations including random horizontal flipping (50% probability), vertical flipping (50% probability), random rotation (±20°), and horizontal shearing (±10°) [17]
Model Architecture Details:
- Backbone Selection: DenseNet121 selected through comparative analysis of multiple CNN architectures (Simple CNN, ResNet101, MobileNetV2, ViT-B/16) [17]
- Channel Adaptation: Pretrained ImageNet weights adapted to single-channel mammography images by averaging across three input channels [17]
- Attention Mechanism: CBAM modules integrated to enhance feature discriminability, with Grad-CAM visualization for interpretability [17]
- Training Protocol: Five-fold cross-validation with binary (Luminal vs non-Luminal, HER2-positive vs negative, TN vs non-TN) and multiclass classification tasks [17]
Virtual Staining Implementation
Virtual staining techniques generate immunohistochemistry images directly from H&E-stained tissue sections using deep generative models [18].
Benchmarking Framework:
- Model Architectures: CycleGAN, conditional GAN, and contrastive unpaired translation (CUT) models evaluated on public datasets [18]
- Performance Metrics: Structural similarity index measure (SSIM), peak signal-to-noise ratio (PSNR), and Fréchet Inception Distance (FID) for image quality assessment [18]
- Clinical Validation: Concordance with ground truth IHC staining assessed for ER, PR, HER2, and Ki-67 biomarkers [18]
- Dataset Requirements: Training typically requires paired H&E and IHC whole slide images from consecutive tissue sections [18]
Circulating Tumor DNA Analysis Protocol
Liquid biopsy methodologies enable detection of resistance mutations in real-time [15].
SERENA-6 Trial Methodology:
- Blood Collection: Serial blood samples collected at baseline and every 4-8 weeks during treatment [15]
- ctDNA Extraction: Plasma separation followed by cell-free DNA extraction using commercial kits [15]
- Mutation Detection: Next-generation sequencing panels targeting known resistance mutations (ESR1, PIK3CA, etc.) with high sensitivity (0.1% variant allele frequency) [15]
- Intervention Threshold: Protocol-specified therapy switch upon detection of emerging ESR1 mutations with clinical correlation [15]
Signaling Pathways in Breast Cancer Resistance
The following diagram illustrates key resistance pathways and their interactions across breast cancer subtypes, highlighting potential intervention points for computational targeting.
Breast Cancer Resistance Signaling Network: This diagram illustrates key molecular pathways contributing to therapy resistance across breast cancer subtypes, highlighting potential targets for computational intervention.
Table 2: Key Research Reagent Solutions for Breast Cancer Resistance Studies
| Reagent Category | Specific Product/Platform | Primary Research Application | Subtype Specificity |
|---|---|---|---|
| Cell Line Panels | MD Anderson Breast Cancer Cell Panel, ATCC Breast Cancer Portfolio | In vitro drug screening & resistance modeling | All subtypes (Luminal, HER2+, TNBC) |
| ctDNA Detection Kits | MSK-ACCESS, Guardant360, FoundationOne Liquid CDx | Liquid biopsy analysis for resistance mutation detection | Luminal (ESR1), HER2+ (PIK3CA), TNBC (TP53) |
| IHC Antibodies | ER (SP1), PR (1E2), HER2 (4B5), Ki-67 (30-9) | Biomarker validation & molecular subtyping | Subtype-defining markers |
| Virtual Staining Datasets | TCGA-BRCA, Camelyon17, Internal institutional datasets | Training & validation of generative models | All subtypes |
| CADD Software | AutoDock, Schrödinger Suite, OpenEye Toolkits | Molecular docking & dynamics simulations | Target-specific applications |
| AI/ML Frameworks | PyTorch, TensorFlow, MONAI for medical imaging | Development of predictive models for resistance | Subtype-agnostic |
| 3D Culture Systems | Matrigel, Organoid culture media | Tumor microenvironment modeling & CSC studies | All subtypes |
| Animal Models | PDX collections (Jackson Laboratory, EurOPDX) | In vivo validation of resistance mechanisms | Subtype-characterized models |
The growing arsenal of computational approaches for addressing breast cancer resistance demonstrates promising performance across subtypes, though significant challenges remain [7] [11]. Virtual screening and AI-driven drug design show particular potential for overcoming target scarcity in TNBC by identifying novel vulnerabilities [7]. Deep learning applications in medical imaging enable non-invasive resistance monitoring, while liquid biopsy approaches provide real-time molecular intelligence on evolving tumor dynamics [17] [15].
Future progress will require enhanced integration of multi-omics data, refined in silico models of tumor heterogeneity, and robust validation through prospective clinical trials [7]. The convergence of computational prediction with experimental validation offers a pathway toward personalized therapeutic strategies that proactively address resistance mechanisms rather than reacting to their emergence [14]. As these technologies mature, they hold potential to transform breast cancer management by anticipating resistance and deploying countermeasures before treatment failure occurs.
Computer-Aided Drug Design (CADD) as a Strategic Response
Breast cancer is a highly heterogeneous malignancy with distinct molecular subtypes—Luminal, HER2-positive (HER2+), and triple-negative breast cancer (TNBC)—each presenting unique therapeutic challenges and vulnerabilities [19]. This molecular diversity complicates the development of effective therapies, as traditional drug discovery methods face constraints from high costs and extended development timelines [19]. Computer-Aided Drug Design (CADD) has emerged as a transformative strategy to accelerate therapeutic discovery by leveraging computational power to identify and optimize drug candidates with enhanced precision [19]. CADD integrates a suite of computational techniques, including molecular docking, virtual screening (VS), pharmacophore modeling, and molecular dynamics (MD) simulations, enabling researchers to efficiently explore chemical space and predict drug-target interactions [19] [20]. The strategic application of CADD is particularly valuable for developing subtype-specific therapies, overcoming drug resistance mechanisms, and streamlining the drug discovery pipeline from initial target identification to lead optimization [19].
Benchmarking Virtual Screening Performance: A Subtype-Centric Analysis
Virtual screening (VS) stands as a cornerstone technique within CADD, functioning as a computational counterpart to experimental high-throughput screening [21]. Its performance is critical for the efficient identification of hit compounds. Benchmarking studies reveal that VS effectiveness varies considerably across breast cancer subtypes due to their distinct molecular pathologies and target characteristics. The integration of multiple computational techniques significantly enhances VS outcomes, with structure-based virtual screening (SBVS) emerging as the most prominently used approach, accounting for an average of 57.6% of applications [21].
Table 1: Benchmarking Virtual Screening Software Preferences and Performance
| Software/Resource | Average Usage % | Primary Application | Notable Advantages |
|---|---|---|---|
| AutoDock | 41.8% | Structure-based Virtual Screening, Molecular Docking | Open-source; well-validated; extensive community support [21] |
| ZINC Database | 31.2% | Compound Library Source | Extensive catalog of commercially available compounds [21] |
| GROMACS | 39.3% | Molecular Dynamics Simulations | Open-source; high performance for biomolecular systems [21] |
| AlphaFold | N/A | Protein Structure Prediction | High-accuracy predictions when experimental structures unavailable [19] |
The selection of specific VS protocols is often guided by the target class prevalent in each breast cancer subtype. For instance, in Luminal cancers targeting the Estrogen Receptor (ER), VS workflows frequently incorporate pharmacophore modeling and quantitative structure-activity relationship (QSAR) analyses to identify novel Selective Estrogen Receptor Degraders (SERDs) [19]. For HER2+ subtypes, structure-based approaches leveraging high-resolution HER2 kinase domain structures enable the optimization of selective inhibitors and antibody-drug conjugates [19]. The particularly challenging TNBC subtype, characterized by a scarcity of well-defined targets, often benefits from hybrid workflows that combine ligand-based screening for targets like PARP with structure-based methods for emerging targets in DNA repair pathways [19].
Table 2: Subtype-Specific Virtual Screening Applications and Outcomes
| Breast Cancer Subtype | Primary Targets | Preferred VS Approaches | Representative Successes |
|---|---|---|---|
| Luminal (ER/PR+) | Estrogen Receptor (ESR1) | SBVS, Pharmacophore Modeling, QSAR | Next-generation oral SERDs (elacestrant, camizestrant) [19] |
| HER2-Positive | HER2 receptor, kinase domain | SBVS, Molecular Docking, MD Simulations | Optimized kinase inhibitors, antibody engineering [19] |
| Triple-Negative (TNBC) | PARP, epigenetic regulators, immune checkpoints | Hybrid Screening, Multi-omics Guided VS | PARP inhibitors, immune modulators [19] |
Post-docking refinement through Molecular Dynamics (MD) simulations has become a standard practice for validating VS results, employed in approximately 38.5% of studies [21]. This step is crucial for assessing binding stability, accounting for protein flexibility, and calculating more reliable binding free energies, thereby reducing false positives identified from docking alone [21].
Experimental Protocols for Benchmarking CADD Performance
Standard Protocol for Structure-Based Virtual Screening
A robust, benchmarked workflow for SBVS integrates multiple computational techniques to maximize the likelihood of identifying true active compounds [21]. The following protocol outlines the key steps:
- Target Selection and Preparation: Obtain the three-dimensional structure of the target protein from the Protein Data Bank (PDB) or generate a high-confidence model using predictive tools like AlphaFold [19] [20]. Prepare the protein structure by adding hydrogen atoms, assigning protonation states, and removing water molecules, except those involved in key binding interactions.
- Compound Library Preparation: Select a diverse chemical library, such as ZINC or Enamine REAL Database [22] [21]. Prepare ligands by generating 3D conformations, optimizing geometry, and assigning correct tautomeric and ionization states at physiological pH.
- Molecular Docking: Define the binding site coordinates based on experimental data or known active sites. Perform docking simulations using software like AutoDock to generate multiple binding poses for each compound. Score each pose using the software's native scoring function to estimate binding affinity [21].
- Post-Docking Analysis and Refinement: Visually inspect the top-ranked poses to evaluate critical interaction patterns (e.g., hydrogen bonds, hydrophobic contacts). Subject the most promising complexes to Molecular Dynamics (MD) simulations using software like GROMACS to assess binding stability and account for protein flexibility [21].
- Consensus Scoring and Hit Selection: Apply consensus scoring strategies by re-evaluating top poses with alternative scoring functions or machine learning-based predictors to improve hit rates. Prioritize compounds for experimental validation based on a combination of docking scores, interaction quality, and stability in MD simulations [21].
Protocol for AI-Enhanced Virtual Screening
The integration of Artificial Intelligence (AI) and Machine Learning (ML) introduces a paradigm shift in VS efficiency [19] [22].
- Data Curation and Featurization: Compile a dataset of known active and inactive compounds against the target. Featurize the compounds using molecular descriptors or fingerprint representations that encode structural and physicochemical properties [22].
- Model Training and Validation: Train a machine learning classifier (e.g., deep neural networks, random forest) on the curated dataset to distinguish between active and inactive molecules. Validate model performance using rigorous cross-validation or a held-out test set to ensure predictive robustness and avoid overfitting [22].
- AI-Driven Triage: Apply the trained model to rapidly screen ultra-large chemical libraries, effectively triaging millions of compounds and generating a manageable shortlist of high-probability hits [19].
- Physics-Based Validation: Subject the AI-prioritized compounds to physics-based methods, such as molecular docking and MD simulations, to provide mechanistic insights and validate the AI predictions [19]. This hybrid approach leverages the speed of AI with the mechanistic detail of physics-based simulations.
Visualizing Key Pathways and Workflows
CADD Workflow in Breast Cancer Drug Discovery
Key Signaling Pathways in Breast Cancer Subtypes
The Scientist's Toolkit: Essential Research Reagent Solutions
The effective application of CADD requires a suite of computational tools and data resources. The following table details key reagents and platforms essential for conducting cutting-edge virtual screening and drug design research in breast cancer.
Table 3: Essential Research Reagent Solutions for CADD
| Tool/Resource | Type | Primary Function in CADD | Relevance to Breast Cancer |
|---|---|---|---|
| AlphaFold [19] [20] | Structure Prediction | Provides high-accuracy 3D protein models when experimental structures are unavailable. | Crucial for modeling mutant forms of ER (ESR1) in Luminal BC and other targets with limited structural data. |
| AutoDock [21] | Docking Software | Predicts ligand binding modes and scores binding affinity. | Workhorse for SBVS against targets like HER2 kinase domain and ER. |
| GROMACS [21] | MD Simulation Software | Simulates protein-ligand dynamics and refines binding poses. | Used to validate stability of potential inhibitors and study resistance mechanisms. |
| ZINC/Enamine [22] [21] | Compound Database | Provides libraries of commercially available compounds for virtual screening. | Source of chemical matter for screening campaigns across all subtypes. |
| ChEMBL/PubChem [22] | Bioactivity Database | Curates bioactivity data for model training and validation. | Source of data for building QSAR and ML models specific to breast cancer targets. |
| PyMOL/Maestro | Visualization & Platform | Enables visualization of complexes and integrated workflow management. | Used for analyzing docking poses and communicating results; commercial platforms offer end-to-end workflows. |
The strategic implementation of CADD, particularly through rigorously benchmarked virtual screening protocols, provides a powerful response to the challenges of drug discovery in heterogeneous diseases like breast cancer. The continued evolution of this field is being driven by the deeper integration of AI and ML for accelerated compound triage, the rise of more accurate protein structure prediction tools like AlphaFold, and the increasing emphasis on hybrid workflows that marry the speed of learning-based models with the mechanistic validation of physics-based simulations [19] [22]. Furthermore, the growing availability of large-scale, high-quality biological data (big data) and its multi-omics integration is paving the way for more holistic, systems-level approaches to target identification and drug design [22]. As these technologies mature and overcome current challenges—such as the need for robust experimental validation and better modeling of complex phenomena like drug resistance—CADD is poised to enable the design of ever more precise, subtype-informed, and personalized therapeutic strategies for breast cancer patients [19].
This guide objectively compares the performance of two modern artificial intelligence frameworks designed for breast cancer subtype classification, a critical task in oncological research and drug development. Benchmarking such tools reveals significant performance variations, underscoring the necessity for context-specific model selection.
Experimental Protocols & Performance Benchmarking
The following section details the methodologies of two distinct deep-learning approaches and quantitatively compares their performance.
Detailed Experimental Protocols
1. DenseNet121-CBAM Model Protocol
This protocol utilized a retrospective analysis of 390 patients with pathologically confirmed invasive breast cancer [17]. The model was designed to predict molecular subtypes from conventional mammography images, offering a non-invasive diagnostic alternative [17].
- Data Preprocessing: Mammographic images were acquired via a Hologic full-field digital mammography system. Two radiologists independently annotated tumor areas to create Regions of Interest (ROIs). These ROIs were expanded outward to include peritumoral background, resized to 224x224 pixels, and processed with a channel-adaptive strategy to adapt ImageNet's 3-channel pre-trained weights to single-channel mammograms [17].
- Model Architecture: The proposed model integrated Convolutional Block Attention Modules (CBAM) with a DenseNet121 backbone. This enhancement aimed to improve feature extraction by focusing on spatially informative regions, visualized via Grad-CAM heatmaps [17].
- Training Strategy: The study involved three binary classification tasks (Luminal vs. non-Luminal, HER2-positive vs. HER2-negative, triple-negative vs. non-TN) and one multiclass task (Luminal A, Luminal B, HER2+/HR+, HER2+/HR−, TNBC). To address class imbalance, simple random oversampling was applied with rates between 1.3 and 1.7. Data augmentation included random horizontal/vertical flipping, rotation (±20°), and shearing (±10°) [17].
2. TransBreastNet Model Protocol
This protocol introduced BreastXploreAI, a multimodal and multitask framework for breast cancer diagnosis. Its backbone, TransBreastNet, is a hybrid CNN-Transformer architecture designed to classify subtypes and predict disease stages simultaneously, incorporating temporal lesion progression and clinical metadata [23].
- Data Preprocessing and Modeling: The framework processes longitudinal mammogram sequences to model temporal lesion evolution. A key innovation is the generation of synthetic temporal lesion sequences to compensate for scarce real longitudinal data. It also fuses imaging features with structured clinical metadata (e.g., hormone receptor status, tumor size) for context-aware predictions [23].
- Model Architecture: The hybrid model uses CNNs for spatial feature encoding from lesions and Transformers for temporal encoding of lesion sequences. A dense network fuses the clinical metadata, and a dual-head classifier performs the joint subtype and stage prediction [23].
- Training Strategy: The model was trained for multi-task learning, which helps avoid bias towards a primary class in imbalanced datasets. Explainability is built-in through Grad-CAM and attention rollout to elucidate the model's decision-making process [23].
Performance Data Comparison
The table below summarizes the quantitative performance of the two models, highlighting their different strengths.
Table 1: Benchmarking performance of AI models for breast cancer subtype classification.
| Model | Primary Classification Task | Key Performance Metric | Score | Dataset & Notes |
|---|---|---|---|---|
| DenseNet121-CBAM [17] | Binary (Luminal vs. non-Luminal) | AUC | 0.759 | Internal test set of 390 patients. |
| Binary (HER2-positive vs. HER2-negative) | AUC | 0.658 | ||
| Binary (Triple-negative vs. non-TN) | AUC | 0.668 | ||
| Multiclass (5 subtypes) | AUC | 0.649 | ||
| TransBreastNet [23] | Multiclass (Subtype & Stage) | Macro Accuracy (Subtype) | 95.2% | Public mammogram dataset; performs joint stage prediction. |
| Macro Accuracy (Stage) | 93.8% |
The Scientist's Toolkit: Research Reagent Solutions
For researchers seeking to implement or benchmark similar AI frameworks, the following computational "reagents" are essential.
Table 2: Key computational components and their functions in deep learning for medical imaging.
| Research Reagent | Function in the Experimental Pipeline |
|---|---|
| DenseNet121 Backbone | A Convolutional Neural Network (CNN) that is highly effective for extracting complex spatial features from medical images like mammograms [17]. |
| Convolutional Block Attention Module (CBAM) | An attention mechanism that enhances a CNN's ability to focus on diagnostically significant regions within an image, such as specific lesion areas [17]. |
| Transformer Encoder | A neural network architecture adept at modeling long-range dependencies and temporal sequences, crucial for analyzing the progression of lesions over time [23]. |
| Grad-CAM & Attention Rollout | Explainable AI (XAI) techniques that generate visual heatmaps, illustrating which parts of the input image most influenced the model's prediction. This builds clinical trust and aids in validation [17] [23]. |
| Clinical Metadata Encoder | A component (often a dense neural network) that processes non-imaging patient data (e.g., hormone receptor status), fusing it with image features for a holistic diagnosis [23]. |
Workflow Visualization
The diagrams below illustrate the logical structure and data flow of the two benchmarked AI frameworks.
DenseNet121-CBAM Workflow
TransBreastNet Hybrid Workflow
The benchmarking data reveals a clear trade-off: the DenseNet121-CBAM model provides a strong, interpretable baseline for subtype prediction from single images, while the TransBreastNet framework offers a more holistic, clinically nuanced approach by integrating temporal and metadata context, achieving higher accuracy at the cost of increased complexity. The choice for virtual screening and research depends on the specific experimental goals, data availability, and the need for joint pathological staging.
Core Methodologies and Subtype-Tailored Virtual Screening Applications
Structure-based virtual screening (SBVS) has become an indispensable cornerstone of modern drug discovery, providing a computationally driven methodology to identify novel hit compounds by leveraging the three-dimensional structure of a biological target. The core premise involves computationally "docking" large libraries of small molecules into a target's binding site to predict interaction poses and evaluate binding affinity. From its origins in traditional molecular docking, the field is now experiencing a paradigm shift, propelled by the integration of artificial intelligence (AI). AI acceleration is enhancing nearly every aspect of the SBVS pipeline, from improved scoring functions to the management of target flexibility, thereby offering unprecedented gains in speed, accuracy, and cost-efficiency [24] [25] [26]. This evolution is particularly critical in complex areas like breast cancer research, where understanding the subtle differences in binding sites across molecular subtypes (e.g., Luminal A, HER2-positive, Triple-Negative) can inform the development of more targeted and effective therapeutics [27].
This guide provides a comparative analysis of mainstream and emerging SBVS tools, benchmarking their performance and outlining detailed experimental protocols. It is framed within the context of breast cancer research, a field that stands to benefit immensely from these advanced computational methodologies.
Benchmarking Docking and AI-Accelerated Tools
The selection of a docking engine is a fundamental decision in any SBVS workflow. The following table summarizes the key characteristics and performance metrics of widely used and next-generation tools.
Table 1: Benchmarking Traditional and AI-Accelerated Docking Tools
| Tool Name | Type / Core Algorithm | Key Features | Performance Highlights | Considerations |
|---|---|---|---|---|
| AutoDock Vina [24] [28] | Traditional / Gradient-Optimization | Open-source, fast, widely used. | Good pose reproduction; scoring can be less accurate for certain target classes. | A good baseline tool; scoring function is generic. |
| GNINA [28] | AI-Accelerated / CNN-based Scoring | Uses Convolutional Neural Networks (CNNs) for scoring and pose refinement. | Superior performance in pose reproduction and active ligand enrichment vs. Vina; better at distinguishing true/false positives. | Higher computational demand than Vina; requires more specialized setup. |
| Glide [24] [29] | Traditional / Hierarchical Filtering | High accuracy in pose prediction, robust scoring function. | Often used in high-performance screening workflows; integrates with active learning (e.g., Glide-MolPAL). | Commercial software; can be computationally intensive. |
| SILCS-MC [29] | Physics-Based / Monte Carlo Docking with Fragments | Incorporates explicit solvation and membrane effects via Fragmap technology. | Excellent for membrane-embedded targets (e.g., GPCRs); provides realistic environmental description. | Highly specialized; computationally demanding for very large libraries. |
| Active Learning Protocols (e.g., MolPAL) [29] | AI-Driven / Iterative Surrogate Modeling | Iteratively trains models to prioritize promising compounds, reducing docking calculations. | Vina-MolPAL: Highest top-1% recovery. SILCS-MolPAL: Comparable accuracy at larger batch sizes. | Requires careful parameter tuning (batch size, acquisition function). |
A recent 2025 benchmark study across ten heterogeneous protein targets, including kinases and GPCRs, provides compelling quantitative data on the performance gains offered by AI-driven tools [28]. The study compared AutoDock Vina with GNINA, evaluating their ability to distinguish active ligands from decoys in a virtual screen.
Table 2: Virtual Screening Performance Metrics (GNINA vs. AutoDock Vina) [28]
| Metric | AutoDock Vina | GNINA | Interpretation |
|---|---|---|---|
| AUC-ROC | Variable, lower on average | Consistently higher | GNINA shows better overall classification performance. |
| Enrichment Factor (EF) at 1% | Lower | Significantly Higher | GNINA is more effective at identifying true hits early in the ranked list. |
| Pose Reproduction Accuracy | Good | Excellent | GNINA's CNN scoring more accurately replicates crystallographic poses. |
Experimental Protocols for Benchmarking VS Workflows
To ensure reproducible and meaningful results in virtual screening, a structured experimental protocol is essential. The following workflow is adapted from established methodologies in the literature [24] [29] [28].
Workflow Diagram: AI-Accelerated Virtual Screening
Protocol Details
Target and Library Preparation
- Target Preparation: Obtain a high-resolution crystal structure (e.g., from PDB) or a high-quality homology model. For breast cancer targets like HER2 or estrogen receptor, special attention should be paid to the protonation states of key residues, the management of structurally important water molecules, and the treatment of metal ions if present. For flexibility, consider using an ensemble of conformations generated by molecular dynamics (MD) simulations [24].
- Compound Library Curation: Select a diverse and relevant chemical library (e.g., ZINC, PubChem). Prepare compounds by generating relevant tautomeric and stereoisomeric states at a physiological pH (e.g., 7.4). Apply pre-filters, such as physicochemical property filters (e.g., Lipinski's Rule of Five) or structure-based pharmacophore models, to enrich the library for drug-like compounds and reduce the screening burden [24] [30].
Docking and AI-Driven Prioritization
- Molecular Docking: Perform docking calculations using the chosen tool(s) (e.g., GNINA, Vina, Glide). Ensure the docking box is large enough to encompass the entire binding site of interest. It is good practice to validate the docking protocol first by re-docking a known co-crystallized ligand and confirming that the root-mean-square deviation (RMSD) of the top pose is less than 2.0 Å from the experimental pose [24] [28].
- AI-Enhanced Scoring & Active Learning: After initial docking, re-score the generated poses using an AI-based scoring function. For example, in GNINA, this involves using its built-in CNN models. For ultra-large libraries, implement an active learning protocol like MolPAL, which iteratively selects the most informative compounds for docking based on a surrogate model, dramatically reducing the number of full docking calculations required [29] [28].
Post-Processing and Hit Analysis
- Consensus Ranking & Visual Inspection: Combine scores from different methods (e.g., traditional and CNN scoring) to create a consensus ranking, which can improve the robustness of hit selection. Crucially, the top-ranked compounds should be visually inspected to verify that they form sensible interactions (e.g., hydrogen bonds, hydrophobic contacts) with key residues in the binding site [30].
- Experimental Validation: The final shortlist of virtual hits should proceed to in vitro experimental validation, such as binding affinity assays (e.g., SPR) or functional cell-based assays, to confirm biological activity.
The Scientist's Toolkit: Essential Research Reagents and Solutions
A successful SBVS campaign relies on a foundation of high-quality data and software tools. The following table details key resources mentioned in the featured research.
Table 3: Key Research Reagent Solutions for SBVS Workflows
| Category / Item | Function in SBVS Workflow | Relevant Context / Example |
|---|---|---|
| Protein Data Bank (PDB) | Primary source for experimentally determined 3D structures of target proteins. | Essential for obtaining reliable starting structures for docking (e.g., HER2 kinase domain). |
| Chemical Libraries (ZINC, PubChem) | Provide vast collections of purchasable or synthesizable small molecules for virtual screening. | ZINC database contains over 13 million compounds for screening [24]. |
| AutoDock Vina | Open-source docking program for initial pose generation and baseline scoring. | Serves as a benchmark and is integrated into active learning pipelines (Vina-MolPAL) [29]. |
| GNINA | AI-powered docking suite that uses CNNs for superior pose scoring and ranking. | Demonstrated to outperform Vina in virtual screening enrichment and pose accuracy [28]. |
| MolPAL | Active learning framework that optimizes the screening of ultra-large chemical libraries. | Can be coupled with Vina, Glide, or SILCS to improve screening efficiency [29]. |
| Convolutional Block Attention Module (CBAM) | Deep learning component that improves model interpretability by highlighting relevant image regions. | Used in DenseNet121-CBAM models for analyzing mammograms, analogous to identifying key binding features in a protein pocket [17]. |
The field of structure-based virtual screening is undergoing a rapid transformation, moving from reliance on traditional physics-based docking algorithms toward hybrid and fully AI-accelerated workflows. As benchmark studies have shown, tools like GNINA that integrate deep learning offer tangible improvements in both pose prediction accuracy and, most critically, the enrichment of truly active compounds in virtual screens. When combined with strategic active learning protocols, these AI-powered methods enable researchers to navigate the vastness of chemical space with unprecedented efficiency and precision. For scientists working on challenging targets in breast cancer and beyond, adopting these advanced SBVS workflows promises to significantly accelerate the journey from a protein structure to a promising therapeutic hit.
Within modern oncology drug discovery, ligand-based computational approaches provide powerful methods for identifying novel chemical scaffolds when structural information for the primary target is limited or unavailable. In the context of breast cancer research—a disease characterized by significant molecular heterogeneity across subtypes such as Luminal, HER2-positive, and triple-negative breast cancer (TNBC)—these approaches enable researchers to leverage existing bioactivity data to accelerate the discovery of new therapeutic candidates [7]. This guide objectively compares the performance and application of two fundamental ligand-based methods: Quantitative Structure-Activity Relationship (QSAR) modeling and pharmacophore modeling, with a specific focus on their utility in scaffold identification for virtual screening campaigns targeting breast cancer subtypes.
Core Methodologies and Comparative Performance
Quantitative Structure-Activity Relationship (QSAR) Modeling
QSAR modeling establishes a mathematical relationship between the chemical structure of compounds and their biological activity [31]. It operates on the principle that structurally similar compounds exhibit similar biological activities, and uses molecular descriptors to quantify these structural properties.
Key Experimental Protocols:
- Data Collection and Curation: A set of compounds with known biological activities (e.g., IC₅₀) against a specific breast cancer target or cell line is assembled. For combinational therapy QSAR, this includes data on anchor and library drugs and their combined biological activity (Combo IC₅₀) [32].
- Molecular Descriptor Calculation: Software tools like PaDEL or PaDELPy are used to compute numerical descriptors representing the molecules' structural, topological, geometric, electronic, and physicochemical properties [32] [31].
- Model Building and Validation: The dataset is split into training and test sets. Machine Learning (ML) and Deep Learning (DL) algorithms—such as Random Forest, Deep Neural Networks (DNN), and Support Vector Regressor (SVR)—build the predictive model using the training set [32]. The model is rigorously validated using statistical parameters like the coefficient of determination (R²) and Root Mean Square Error (RMSE). For instance, a DNN model achieved an R² of 0.94 and an RMSE of 0.255 in predicting the combinational biological activity of drug pairs in breast cancer cell lines [32].
Pharmacophore Modeling
A pharmacophore is defined as "the ensemble of steric and electronic features that is necessary to ensure the optimal supra-molecular interactions with a specific biological target structure and to trigger (or to block) its biological response" [33]. Ligand-based pharmacophore modeling extracts common chemical features from a set of known active ligands, arranged in a specific 3D orientation, which are critical for biological activity [33] [34].
Key Experimental Protocols:
- Ligand Selection and Conformation Generation: A set of active compounds with diverse structures but common activity against a target (e.g., aromatase in breast cancer) is selected. Their 3D structures are generated, and conformational models are created to account for flexibility [35] [34].
- Feature Identification and Model Generation: Software such as PharmaGist or the 3D QSAR Pharmacophore Generation module in Discovery Studio is used to identify common pharmacophore features from the aligned active ligands. These features include Hydrogen Bond Acceptors (HBA), Hydrogen Bond Donors (HBD), Hydrophobic areas (H), and Aromatic rings (AR) [33] [31] [34].
- Model Validation: The model is validated using a test set of compounds and sometimes through Fisher randomization to ensure its predictive power is not due to chance [34]. The model's ability to distinguish active compounds from inactive decoys is assessed using metrics like the Enrichment Factor (EF) and the Area Under the Curve (AUC) of a Receiver Operating Characteristic (ROC) plot [36].
Performance Comparison in Virtual Screening
The table below summarizes the comparative performance of QSAR and pharmacophore modeling in key aspects relevant to scaffold identification and virtual screening.
Table 1: Performance and Application Comparison of Ligand-Based Approaches
| Aspect | QSAR Modeling | Pharmacophore Modeling |
|---|---|---|
| Primary Strength | Quantitative activity prediction; excellent for lead optimization [35] | Identification of novel chemotypes via "scaffold hopping" [35] |
| Data Requirement | Requires a sufficiently large and congeneric set of compounds with known activity data [32] | Can be generated from a relatively small set of known active ligands [33] |
| Scaffold Identification | Identifies scaffolds based on descriptor-activity relationships; less intuitive for direct scaffold design | Directly defines the essential steric and electronic features for activity, enabling search for diverse scaffolds possessing these features [33] |
| Handling of Cancer Heterogeneity | Can build subtype-specific models (e.g., for Luminal or TNBC) by using relevant cell line or target data [32] [7] | A single model can screen for compounds active against a specific target across subtypes; subtype-specificity depends on the ligands used for modeling |
| Key Limitation | Predictive capability is limited to the chemical space defined by the training set; poor extrapolation | Lacks quantitative activity prediction unless combined with QSAR (3D-QSAR pharmacophore) [34] |
| Typical Output | Predictive model for biological activity (e.g., pIC₅₀) | 3D spatial query for database screening |
Integrated Workflows for Enhanced Performance
Benchmarking studies reveal that integrating QSAR and pharmacophore modeling into a single workflow significantly enhances virtual screening performance. The sequential application of these methods allows researchers to leverage the strengths of each approach.
Protocol for an Integrated QSAR-Pharmacophore Screening Workflow:
- 3D-QSAR Pharmacophore Generation: A pharmacophore model is built based on the QSAR of training set compounds, correlating the spatial arrangement of features with biological activity levels [34].
- Virtual Screening: The validated pharmacophore model is used as a 3D query to screen large chemical databases (e.g., ZINC, NCI) to retrieve potential hit compounds with novel scaffolds [35] [34].
- Activity Prediction and Prioritization: The retrieved hits are then passed through a previously developed and validated QSAR model to predict their biological activity and prioritize the most promising candidates for further study [35] [37].
- Experimental Validation: Top-ranked compounds are subjected to in vitro and in vivo testing to confirm computational predictions [7].
This workflow was successfully applied to identify novel steroidal aromatase inhibitors for breast cancer. A pharmacophore model containing two acceptor atoms and four hydrophobic centers was used to screen the NCI2000 database, and the retrieved hits' activities were predicted using CoMFA and CoMSIA models, leading to the identification of six promising hit compounds [35].
Figure 1: Integrated ligand-based virtual screening workflow, combining pharmacophore and QSAR approaches for identifying and prioritizing novel scaffolds.
The Scientist's Toolkit: Essential Research Reagents and Software
Successful implementation of ligand-based approaches relies on a suite of computational tools and data resources. The table below details key solutions used in the featured experiments and the broader field.
Table 2: Key Research Reagent Solutions for Ligand-Based Modeling
| Tool / Resource | Type | Primary Function in Research | Example Application |
|---|---|---|---|
| PaDEL / PaDELPy [32] [31] | Software Descriptor | Calculates molecular descriptors and fingerprints for QSAR. | Generating structural descriptors for training a combinational QSAR model on breast cancer cell lines [32]. |
| ZINC Database [36] [31] | Chemical Database | A curated collection of commercially available compounds for virtual screening. | Source of natural products for pharmacophore-based screening against dengue virus NS3 protease [31]. |
| PharmaGist [31] | Software Pharmacophore | Generates ligand-based pharmacophore models from a set of active molecules. | Creating a pharmacophore hypothesis from top-active 4-Benzyloxy Phenyl Glycine derivatives [31]. |
| ZINCPharmer [31] | Online Tool | Screens the ZINC database using a pharmacophore model as a query. | Identifying compounds with features similar to known active ligands [31]. |
| LigandScout [36] | Software Pharmacophore | Creates structure-based and ligand-based pharmacophore models and performs virtual screening. | Generating a structure-based pharmacophore model for XIAP protein from a protein-ligand complex [36]. |
| BuildQSAR [31] | Software QSAR | Develops QSAR models using selected descriptors and the Multiple Linear Regression (MLR) method. | Building a 2D QSAR model to predict the IC₅₀ of dengue virus protease inhibitors [31]. |
| GDSC Database [32] | Bioactivity Database | Provides drug sensitivity data for a wide range of cancer cell lines, including combinational drug screening data. | Source of data for building a combinational QSAR model for breast cancer therapy [32]. |
Ligand-based approaches, namely QSAR and pharmacophore modeling, are indispensable for scaffold identification in breast cancer drug discovery. While QSAR excels at providing quantitative activity predictions for lead optimization, pharmacophore modeling is superior for scaffold hopping and identifying novel chemotypes. Benchmarking studies and experimental data confirm that the integration of these methods into a cohesive workflow, often supplemented with molecular docking and dynamics simulations, provides a powerful strategy for navigating the complex chemical and biological space of breast cancer subtypes. This integrated approach enhances the efficiency of virtual screening campaigns, ultimately accelerating the discovery of new therapeutic agents to address the critical challenge of tumor heterogeneity and drug resistance.
Integrating AI and Machine Learning for Sensitivity Prediction and Biomarker Discovery
The integration of artificial intelligence (AI) and machine learning (ML) is fundamentally reshaping the landscape of breast cancer research, particularly in the critical areas of sensitivity prediction and biomarker discovery. This transformation is most evident in the benchmarking of virtual screening performance across different breast cancer subtypes. AI systems are increasingly being validated against, and integrated with, traditional biological assays to stratify patient risk, predict treatment response, and identify novel molecular signatures directly from standard clinical images and data [38] [39] [40]. The emerging paradigm leverages deep learning models to extract subtle, sub-visual patterns from mammography, histopathology slides, and multi-omics data, establishing imaging-derived biomarkers as non-invasive proxies for complex molecular phenotypes [39] [41]. This guide provides a systematic comparison of AI/ML performance against conventional methods, detailing experimental protocols and offering a toolkit for researchers aiming to implement these technologies in their drug discovery and development pipelines for breast cancer.
Performance Benchmarking: AI vs. Conventional Workflows
The performance of AI/ML models is benchmarked across several key clinical tasks. The following tables synthesize quantitative results from recent studies, allowing for direct comparison between emerging computational approaches and established diagnostic and predictive methods.
Table 1: Performance of AI Models in Breast Cancer Subtype Classification
| Clinical Task | AI Model / Approach | Performance Metric | Conventional Method (for context) | Citation |
|---|---|---|---|---|
| TNBC Identification (from H&E images) | TRIP System (Deep Learning) | AUC: 0.980 (Internal), 0.916 (External) | Immunohistochemistry (IHC) & FISH (Gold Standard, costly/time-consuming) | [41] |
| Molecular Subtyping (from Mammography) | DenseNet121-CBAM | AUC: 0.759 (Luminal), 0.668 (TN), 0.649 (Multiclass) | Needle Biopsy & IHC (Invasive, risk of sampling error) | [42] |
| HER2 Status Prediction | Vision Transformer (ViT) | Accuracy up to 99.92% reported in mammography | IHC & FISH (Tissue-based, requires specialized equipment) | [38] |
| Biomarker Status Prediction | End-to-End CNN on CEM | AUC: 0.67 for HER2 status | IHC on biopsy sample | [42] |
Table 2: AI Performance in Screening, Prognosis, and Workflow Efficiency
| Application Area | AI Model / Workflow | Performance Outcome | Comparison Baseline | Citation |
|---|---|---|---|---|
| Population Screening | AI-supported double reading (Vara MG) | Detection Rate: 6.7/1000 (vs. 5.7/1000); Recall rate non-inferior | Standard Double Reading (without AI) | [43] |
| TNBC Prognosis (Disease-Free Survival) | TRIP System | C-index: 0.747 (Internal), 0.731 (External) | Traditional clinicopathological features (e.g., TNM stage) | [41] |
| Workflow Triage | AI Normal Triage + Safety Net | 56.7% of exams auto-triaged as normal; Safety Net triggered for 1.5% of exams, contributing to 204 cancer diagnoses | Full manual review by radiologists | [43] |
| Risk Stratification | AI-based Mammographic Risk Models | Improved discrimination vs. classical models (e.g., Gail, Tyrer-Cuzick); AUCs often >0.70 | Classical Clinical Risk Models (AUC often <0.65-0.70) | [40] |
Experimental Protocols for Key AI Applications
Protocol 1: Predicting Molecular Subtypes from Mammography Images
This protocol is based on the study by Luo et al. (2025) that developed a deep learning model for predicting molecular subtypes from conventional mammography [42].
- Objective: To develop and validate a deep learning model for non-invasive prediction of breast cancer molecular subtypes (Luminal A, Luminal B, HER2+/HR+, HER2+/HR-, TNBC) using standard mammography images.
- Data Curation:
- Cohort: Retrospective dataset of 390 patients with pathologically confirmed invasive breast cancer and preoperative mammography.
- Inclusion Criteria: Primary invasive breast cancer with mammographically visible tumor mass, molecular subtype determined by postoperative pathology (gold standard).
- Exclusion Criteria: Inflammatory breast cancer, bilateral/pathologically heterogeneous lesions, prior radiotherapy/chemotherapy, or invasive procedures within a week before mammography.
- Image Annotation: Two qualified radiologists independently annotated all identifiable tumor areas on craniocaudal (CC) and mediolateral oblique (MLO) views using ITK-SNAP software.
- Preprocessing & Augmentation:
- ROI Extraction: Annotated tumor regions were extracted and expanded outward by a specified pixel bound to include peritumoral background, then resized to 224x224 pixels.
- Class Imbalance Handling: Simple random oversampling was applied (e.g., oversampling rate of 1.7 for TNBC class).
- Data Augmentation: Geometric transformations included random horizontal flipping (50% probability), vertical flipping (50% probability), random rotation (±20°), and horizontal shearing (±10°).
- Model Architecture & Training:
- Backbone: DenseNet121 was selected as the backbone after comparative experiments with ResNet101, MobileNetV2, and Vision Transformers.
- Innovation: Integration of Convolutional Block Attention Modules (CBAM) to enhance feature learning.
- Input Adaptation: A channel-adaptive pretrained weight allocation strategy was used to adapt ImageNet (3-channel) pretrained weights to single-channel mammography images.
- Tasks: The model was trained for binary (Luminal vs. non-Luminal, HER2-positive vs. HER2-negative, TN vs. non-TN) and multiclass classification tasks.
- Validation & Interpretation:
- Validation: Performance was evaluated on an independent test set using AUC, accuracy, sensitivity, and specificity.
- Interpretability: Gradient-weighted Class Activation Mapping (Grad-CAM) was used to generate heatmaps, highlighting that the model focused on peritumoral regions as critical discriminative features [42].
Protocol 2: Developing an AI System for TNBC Diagnosis and Prognosis
This protocol is based on the development and validation of the TRIP system, a deep learning model for identifying Triple-Negative Breast Cancer (TNBC) and predicting its prognosis from histopathology images [41].
- Objective: To create a unified, end-to-end AI system for accurate TNBC identification and prognosis prediction (disease-free and overall survival) using haematoxylin and eosin (H&E)-stained whole slide images (WSIs).
- Data Sourcing and Cohort Design:
- Development Cohort: 2045 patients with breast cancer from The First Affiliated Hospital, Zhejiang University School of Medicine (FAH), including 451 TNBC patients with follow-up outcomes.
- External Validation: Independent retrospective cohorts from four tertiary hospitals in China (SDPH, SRRS, YWCH, WHCH) and The Cancer Genome Atlas (TCGA) dataset, totaling 2793 cases for identification and 463 for prognosis.
- Exclusion Criteria: Patients with other synchronous malignant neoplasms within five years or those who had received neoadjuvant chemotherapy.
- AI Model Development:
- System Architecture: The TRIP system integrates a pathology foundation model with effective long-sequence modelling to process giga-pixel WSIs.
- Outputs: A single pipeline capable of both classifying TNBC versus other subtypes and predicting continuous survival outcomes.
- Performance Evaluation:
- TNBC Identification: Evaluated using the Area Under the Receiver Operating Characteristic Curve (AUC) on internal and external cohorts.
- Prognosis Prediction: Evaluated using the Concordance Index (C-index) for disease-free survival (DFS) and overall survival (OS) predictions.
- Interpretability and Biological Validation:
- Heatmaps: Generated to visualize key histologic features learned by the model, revealing associations with nuclear atypia, necrosis, lymphoplasmacytic infiltration, and immune-cold microenvironments.
- Multi-Omics Analysis: Conducted to explore TNBC heterogeneity and identify molecular subtypes with distinct immune and pro-tumour signalling profiles, providing biological plausibility for the model's prognostic accuracy [41].
Visualizing the AI-Driven Biomarker Discovery Workflow
The following diagram illustrates the logical workflow and data relationships in an AI-driven pipeline for sensitivity prediction and biomarker discovery, integrating elements from the experimental protocols above.
AI-Driven Biomarker Discovery Workflow
This workflow visualizes the end-to-end pipeline, from multi-modal data input to clinical validation, highlighting the key stages and components required for robust AI-driven biomarker discovery and sensitivity prediction in breast cancer research.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Computational Tools for AI-Driven Breast Cancer Research
| Item / Resource | Function / Application | Relevance to AI Benchmarking |
|---|---|---|
| H&E-Stained Whole Slide Images (WSIs) | Digital pathology slides used as primary input for deep learning models predicting subtype and prognosis. | The TRIP system demonstrated that standard H&E slides contain latent information for accurate TNBC identification (AUC 0.98) and survival prediction [41]. |
| Annotated Mammography Datasets (CC & MLO views) | Curated imaging datasets with radiologist-annotated regions of interest (ROIs) for model training. | Essential for developing models like DenseNet121-CBAM for non-invasive molecular subtyping; annotations enable supervised learning [42]. |
| Immunohistochemistry (IHC) Kits (ER, PR, HER2) | Gold standard for determining molecular subtype and providing ground truth labels for AI model training and validation. | Critical for validating AI predictions against biological truth; necessary for creating labeled datasets [42] [41]. |
| Multi-Omics Datasets (Genomics, Transcriptomics) | Data used for biological validation and to explore correlations between AI-derived image features and molecular pathways. | Multi-omics analysis supported the TRIP system's prognostic accuracy by revealing distinct molecular subtypes underlying the AI-predicted risk groups [41]. |
| Pre-Trained Deep Learning Models (e.g., DenseNet, Vision Transformers on ImageNet) | Foundational models that can be adapted for medical image tasks via transfer learning, mitigating data scarcity. | A channel-adaptive strategy was used to adapt ImageNet-pretrained DenseNet121 weights for single-channel mammography, improving performance [42]. |
| AI Explainability Tools (Grad-CAM, Attention Heatmaps) | Software libraries to generate visual explanations of model predictions, fostering trust and providing biological insight. | Grad-CAM heatmaps revealed that the DenseNet121-CBAM model focused on peritumoral regions, offering interpretability [42]. |
The benchmarking data and experimental protocols presented herein demonstrate that AI and ML models are achieving performance levels that suggest their potential as valuable supplements, and in some cases alternatives, to more invasive or costly conventional methods for sensitivity prediction and biomarker discovery in breast cancer. Key findings indicate strong capabilities in TNBC identification, molecular subtyping from mammography, and prognostic risk stratification.
However, the field must address critical challenges before widespread clinical adoption. Generalizability remains a concern, as model performance can diminish on external datasets from different institutions due to variations in imaging equipment, protocols, and patient populations [38] [39]. Furthermore, prospective clinical trials demonstrating improvement in patient outcomes are still needed for many of these AI systems [40] [41]. The future of this field lies in the development of robust, multimodal AI models that integrate imaging, clinical, and genomic data within validated frameworks, ensuring that these powerful tools can be translated safely and effectively into routine research and clinical practice to advance personalized breast cancer therapy [38] [40] [44].
Clinical Context: Breast Cancer Molecular Subtypes
Breast cancer is not a single disease but a collection of molecularly distinct subtypes that dictate prognosis, therapeutic strategies, and drug development approaches. The classification is primarily based on the expression of hormone receptors (HR)—estrogen receptor (ER) and progesterone receptor (PR)—and human epidermal growth factor receptor 2 (HER2). These biomarkers define four principal subtypes with dramatically different clinical behaviors and therapeutic responses [6] [45].
Table: Epidemiology and Survival Profiles of Major Breast Cancer Subtypes
| Molecular Subtype | Approximate Prevalence | 5-Year Relative Survival | Key Clinical Characteristics |
|---|---|---|---|
| HR+/HER2- (Luminal A/B) | ~70% [46] | 95.6% [46] | Hormone-driven; best prognosis; treated with endocrine therapy (e.g., Tamoxifen, AIs) ± CDK4/6 inhibitors [6] [47]. |
| HR+/HER2+ (Luminal B) | ~9% [46] | 91.8% [46] | Aggressive; responsive to both endocrine and HER2-targeted therapies (e.g., Trastuzumab, T-DXd) [6] [47]. |
| HR-/HER2+ (HER2-Enriched) | ~4% [46] | 86.5% [46] | Very aggressive; highly responsive to modern HER2-targeted therapies and Antibody-Drug Conjugates (ADCs) [47] [48]. |
| Triple-Negative (TNBC) | ~10% [46] | 78.4% [46] | Most aggressive subtype; lacks targeted receptors; chemotherapy and immunotherapy are mainstays; poor prognosis [6] [49]. |
These subtypes also exhibit distinct metastatic patterns, a critical consideration for late-stage drug development. HR+/HER2- tumors show a propensity for bone metastasis, while HER2-positive and TNBC subtypes are more likely to involve visceral organs and the brain [50]. Multi-organ metastases, particularly combinations involving the brain, are associated with the poorest prognosis, underscoring the need for subtype-specific therapeutic strategies [50].
Current Therapeutic Landscape and Challenges
The treatment paradigm for advanced breast cancer is rapidly evolving, marked by the rise of targeted therapies and antibody-drug conjugates (ADCs). Recent phase III trials are redefining standards of care, particularly for HER2-positive and TNBC subtypes [47].
HER2-Positive Breast Cancer
The DESTINY-Breast09 trial established a new first-line benchmark for HER2-positive metastatic breast cancer. It demonstrated that Trastuzumab Deruxtecan (T-DXd) plus Pertuzumab significantly outperformed the previous standard (taxane + trastuzumab + pertuzumab), reducing the risk of disease progression or death by 44% and achieving a median progression-free survival (PFS) of 40.7 months [47]. Despite its efficacy, toxicity management remains crucial, with interstitial lung disease (ILD) observed in approximately 12% of patients in the experimental arm [47] [48].
Hormone Receptor-Positive (HR+), HER2-Negative Breast Cancer
A key challenge in this subtype is overcoming resistance to endocrine therapy. The SERENA-6 trial addressed this by using liquid biopsy to identify emerging ESR1 mutations in patients on aromatase inhibitor therapy. Switching these patients to camizestrant (a next-generation oral SERD) significantly prolonged PFS to 16.0 months compared to 9.2 months with continued AI therapy [47]. This trial highlights the importance of real-time biomarker monitoring for optimizing treatment sequencing.
Triple-Negative Breast Cancer (TNBC)
The ASCENT-04/KEYNOTE-D19 trial showed that the combination of sacituzumab govitecan (SG), a TROP2-directed ADC, and pembrolizumab improved outcomes over chemotherapy plus pembrolizumab in PD-L1-positive advanced TNBC [47]. Furthermore, research is refining the TNBC classification, revealing that HER2-low TNBC (a subset with minimal HER2 expression) has distinct molecular features, including activated androgen receptor pathways and higher PIK3CA mutation rates, which may inform future targeted strategies [49].
Computational Virtual Screening: Methodologies and Workflows
Computational drug repositioning offers a powerful, cost-effective strategy to identify new therapeutic candidates for breast cancer subtypes, bypassing the high costs and extended timelines of de novo drug discovery [6]. The following workflow outlines a standard pipeline for benchmarking virtual screening performance.
Detailed Experimental Protocols
Network-Based Pharmacology and AI Methods
Objective: To identify repurposable drug candidates by analyzing complex biological networks and multi-omics data. Workflow:
- Network Construction: Create a comprehensive network where nodes represent biological entities (e.g., drugs, genes, proteins, diseases) and edges represent interactions or relationships (e.g., protein-protein interactions, drug-target binding) [6].
- Subtype-Specific Model Mapping: Overlay subtype-specific genomic, transcriptomic, and proteomic data onto the network to identify disease modules and key pathogenic hubs for TNBC, HER2+, or Luminal cancers [6] [49].
- Candidate Prioritization: Use network proximity measures and centrality algorithms (e.g., degree, betweenness) to rank existing drugs based on their predicted ability to perturb the identified subtype-specific disease modules [6].
- Multi-Omics Integration: Corroborate findings by integrating data from whole exome sequencing, RNA sequencing, and transcriptomic signatures to confirm pathway activation and drug mechanism-of-action [6] [49].
Computer-Aided Drug Design (CADD) and Molecular Docking
Objective: To predict the binding affinity and interaction模式 of a small molecule with a specific protein target critical to a breast cancer subtype. Workflow:
- Target Selection: Choose a well-validated, structurally characterized target (e.g., HER2 receptor in HER2+ cancer, androgen receptor in the Luminal Androgen Receptor (LAR) subset of TNBC) [49].
- Structure Preparation: Obtain the 3D structure of the target protein from the Protein Data Bank (PDB) and prepare it by adding hydrogen atoms, correcting residues, and defining binding sites.
- Ligand Preparation: Prepare a library of small molecule compounds from drug databases, optimizing their 3D structures and assigning correct charges.
- Molecular Docking: Perform computational docking simulations to predict the binding pose and affinity (scoring function) of each compound against the target.
- Hit Identification: Prioritize compounds with the most favorable binding scores and stable interaction profiles for further experimental testing [6].
Benchmarking Performance Across Subtypes
The performance of virtual screening is highly dependent on the molecular context of each breast cancer subtype. The table below summarizes key metrics and considerations for benchmarking.
Table: Benchmarking Virtual Screening Performance Across Subtypes
| Subtype | Promising Targets & Pathways | Computational Approach | Validation Case Study / Metric | Key Challenges |
|---|---|---|---|---|
| TNBC | AR signaling [49], PI3K/AKT pathway [49], Fatty acid metabolism [49] | Multi-omics analysis (WES, RNA-seq) to define HER2-low vs HER2-0 subgroups and their unique vulnerabilities [49]. | HER2-low TNBC within LAR subtype shows distinct prognosis and molecular features (PFS, RFS) [49]. | High tumor heterogeneity; lack of druggable targets; defining predictive biomarkers beyond HR/HER2. |
| HER2+ | HER2 receptor, PI3K/mTOR pathway | Network-based proximity & CADD for novel HER2 inhibitor discovery or ADC payload optimization. | Phase III trial of trastuzumab botidotin vs T-DM1: mPFS 11.1 vs 4.4 mos (HR=0.39) [48]. | Managing toxicity (e.g., ILD from ADCs); understanding mechanisms of resistance to ADCs. |
| HR+/HER2- (Luminal) | ESR1 mutations [47], CDK4/6, AKT | AI/ML models trained on clinical trial data (e.g., SERENA-6) to predict response to oral SERDs and combination therapies [6] [47]. | SERENA-6: Camizestrant in ESR1-mutants: mPFS 16.0 vs 9.2 mos (HR=0.44) [47]. | Tackling endocrine therapy resistance; intrinsic and acquired tumor heterogeneity. |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful execution of the described experimental protocols requires a suite of specialized reagents, databases, and software platforms.
Table: Key Research Reagent Solutions for Virtual Screening in Breast Cancer
| Tool Category | Specific Examples | Function in Workflow |
|---|---|---|
| Biological Databases | SEER database [46] [50] [51], The Cancer Genome Atlas (TCGA), Protein Data Bank (PDB), DrugBank | Provides population-level incidence, survival, and metastatic pattern data for hypothesis generation and model validation [46] [50]. Source for protein structures and drug information. |
| Bioinformatics Software | R, SPSS, SEER*Stat [45] [50] [51] | Statistical analysis of clinical and omics data; survival analysis; logistic regression for metastatic risk assessment. |
| AI/Deep Learning Platforms | PyTorch, TensorFlow, DenseNet121-CBAM [42] | Development of custom deep learning models for tasks such as predicting molecular subtypes from mammography images [42]. |
| Molecular Modeling Suites | AutoDock Vina, Schrödinger Suite, GROMACS | Performing molecular docking simulations and molecular dynamics to study drug-target interactions and stability. |
| Pathology & IHC Reagents | Anti-ER, Anti-PR, Anti-HER2 antibodies, Ki-67 assay | Gold-standard determination of molecular subtypes from patient tissue samples [45] [52]. |
| Imaging & Analysis | Contrast-Enhanced Ultrasound (CEUS), Superb Microvascular Imaging (SMI) [52] | Non-invasive assessment of tumor vascularity and perfusion, providing features for ML-based subtype classification [52]. |
Addressing Critical Challenges and Optimizing VS Performance
Overcoming Data Biases and Ensuring Generalizability
In the field of breast cancer research, the accurate classification of molecular subtypes is a critical determinant for guiding therapeutic decisions and developing new drugs. Virtual screening, powered by artificial intelligence (AI), promises to non-invasively predict subtypes from medical images like mammograms, potentially bypassing the limitations of invasive biopsies [53] [54]. However, the real-world performance of these AI models is highly contingent on overcoming significant data biases and ensuring their generalizability across diverse clinical settings. Biases arising from imbalanced datasets, varying imaging protocols, and heterogeneous patient populations can severely limit a model's clinical applicability [54] [42]. This guide objectively compares the performance of contemporary AI approaches for breast cancer subtyping, with a focus on their methodological rigor in mitigating bias and fostering generalizability. By benchmarking these approaches, we provide researchers and drug development professionals with a framework for evaluating the trustworthiness and translational potential of virtual screening tools.
Performance Benchmarking of AI Approaches
The performance of AI models in classifying breast cancer molecular subtypes varies significantly based on their architecture, the data modalities used, and the specific classification task. The following tables summarize key quantitative findings from recent studies.
Table 1: Performance Metrics for Multiclass Subtype Classification
| Study (Year) | Model Architecture | Dataset | Key Performance Metric | Reported Value |
|---|---|---|---|---|
| Luo et al. (2025) [42] | DenseNet121-CBAM | In-house (390 patients) | Multiclass AUC | 0.649 |
| Multimodal DL (2025) [53] | Multimodal (Xception-based) | CMMD (1,775 patients) | Multiclass AUC | 88.87% |
| MDL-IIA (2023) [55] | Multi-ResNet50 with Attention | Multi-modal (3,360 cases) | Matthews Correlation Coefficient (MCC) | 0.837 |
Table 2: Performance in Binary Classification Tasks
| Classification Task | Study (Year) | Model Architecture | AUC |
|---|---|---|---|
| Luminal vs. Non-Luminal | Luo et al. (2025) [42] | DenseNet121-CBAM | 0.759 |
| MDL-IIA (2023) [55] | Multi-ResNet50 with Attention | 0.929 | |
| HER2-positive vs. HER2-negative | Luo et al. (2025) [42] | DenseNet121-CBAM | 0.658 |
| Breast Cancer Subtype Prediction (2024) [54] | ResNet-101 | 0.733 | |
| Triple-Negative vs. Non-TN | Luo et al. (2025) [42] | DenseNet121-CBAM | 0.668 |
Key Performance Insights
- Multimodal Integration Enhances Performance: The model by [53], which integrated mammography images with clinical metadata (e.g., age, tumor class), achieved a markedly higher multiclass AUC (88.87%) compared to its image-only counterpart (61.3%). This underscores the value of combining data types to overcome the limitations of any single modality.
- Attention Mechanisms Improve Discriminative Power: The MDL-IIA model [55], which employed intra- and inter-modality attention, achieved a superior MCC of 0.837 for 4-category classification and an AUC of 0.929 for distinguishing Luminal from Non-Luminal disease. Attention mechanisms allow the model to focus on more discriminative image regions.
- Binary vs. Multiclass Complexity: Consistently, models perform better in binary classification tasks than in multiclass scenarios [54] [42]. This highlights the inherent challenge of capturing the subtle and complex imaging patterns that distinguish between all five major subtypes simultaneously.
Detailed Experimental Protocols and Methodologies
A critical step in benchmarking is understanding the experimental design and data handling procedures that underpin model performance.
Data Curation and Preprocessing Protocols
- Data Sourcing and Inclusion Criteria: Studies utilized retrospective data from patients with pathologically confirmed breast cancer. Standard inclusion criteria involved the availability of preoperative mammography and a confirmed molecular subtype from postoperative histopathology [42]. The CMMD and OPTIMAM are two large public databases frequently used [53] [54].
- Region of Interest (ROI) Extraction: To reduce heterogeneity and focus the model on relevant features, radiologists often manually annotate tumor areas on mammograms. These ROIs are then extracted, sometimes with an expanded boundary to include peritumoral tissue, which can provide additional discriminative information [42].
- Class Imbalance Mitigation: A common challenge is the natural imbalance in subtype prevalence (e.g., more Luminal A cases than HER2-enriched). To prevent model bias toward majority classes, researchers employ techniques like:
- Inverse Class Weighting: Adjusting the loss function to penalize misclassifications of rare classes more heavily [53].
- Oversampling: Randomly duplicating samples from minority classes [54] [42].
- Data Augmentation: Artificially expanding the dataset through random geometric transformations like flipping, rotation, and shearing [42].
Model Architectures and Training Procedures
- Backbone Selection and Transfer Learning: Common practice involves using a pre-trained convolutional neural network (CNN)—such as Xception, DenseNet121, or ResNet101—as a feature extractor [53] [54] [42]. These models, initially trained on large natural image datasets like ImageNet, are fine-tuned on medical images, often using a channel-adaptive strategy to adapt their weights to single-channel mammograms [42].
- Multimodal Fusion Architectures: Advanced models go beyond single-image analysis. The multimodal approach in [53] uses two encoders: one (CNN1) processes the mammography image, while another (CNN2) processes clinical metadata. The features from both are then fused into a unified representation before the final classification.
- Attention Mechanisms: The MDL-IIA model [55] incorporates two attention modules. The intra-modality attention module identifies salient features within a single image (e.g., a mammogram), while the inter-modality attention module dynamically identifies and weighs relevant features across different imaging modalities (e.g., between mammography and ultrasound).
Diagram: Workflow of a Multimodal Deep Learning Model for Subtype Classification
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Computational Tools for AI-based Breast Cancer Subtyping
| Item/Reagent | Function/Description | Exemplar in Use |
|---|---|---|
| Public Mammography Databases | Provides large, annotated datasets for training and validating models. Essential for reproducibility and benchmarking. | CMMD [53], OPTIMAM [54] |
| Pre-trained CNN Models | Serves as a robust starting point for feature extraction, mitigating the need for massive, private datasets. | Xception [53], ResNet-101 [54], DenseNet121 [42] |
| Class Imbalance Algorithms | Computational methods to correct for uneven class distribution, preventing model bias. | Inverse Class Weighting [53], Random Oversampling [54] [42] |
| Attention Modules | Neural network components that boost model performance and interpretability by focusing on salient image regions. | Convolutional Block Attention Module (CBAM) [42], Intra- & Inter-modality Attention [55] |
| Data Augmentation Pipelines | Software tools that apply transformations to expand training data diversity and improve model generalizability. | Geometric transforms (flips, rotations, shears) [42] |
Pathway to Robust and Generalizable Models
The logical progression from raw data to a clinically generalizable model involves systematic steps to address bias at every stage.
Diagram: Logical Pathway for Developing Generalizable AI Models
Overcoming data biases and ensuring generalizability requires a multi-faceted strategy:
- Diverse Data Curation: The foundation of a generalizable model is a dataset that reflects population diversity in terms of genetics, demographics, and imaging equipment. Relying on multi-institutional data, as seen in larger studies [55], is crucial.
- Bias-Aware Preprocessing: Proactively addressing class imbalance through the techniques detailed in Section 3.1 is not an optional step but a core requirement for unbiased learning [53] [54].
- Advanced Model Design: Moving from simple, unimodal models to architectures that integrate multiple data types (images + clinical data) [53] or multiple imaging modalities (MG + US) [55] provides a more comprehensive view of the tumor, enhancing predictive accuracy and robustness.
- Rigorous Validation: True performance is measured not on the training data, but on held-out test sets and, more importantly, external validation cohorts from entirely separate institutions. This is the ultimate test of a model's ability to generalize.
Improving Scoring Functions and Managing Ultra-Large Libraries
The application of virtual screening in breast cancer research represents a paradigm shift in early drug discovery, enabling researchers to efficiently navigate the vast chemical space to identify potential therapeutic candidates. Breast cancer's clinical management is strongly influenced by molecular heterogeneity, with major subtypes including hormone receptor-positive Luminal, HER2-positive (HER2+), and triple-negative breast cancer (TNBC), each exhibiting distinct therapeutic vulnerabilities and resistance mechanisms [7]. The growing availability of make-on-demand compound libraries, which now contain billions of readily available compounds, presents both unprecedented opportunities and significant computational challenges for researchers targeting these breast cancer subtypes [56].
Traditional virtual screening methods have struggled to maintain efficiency when applied to ultra-large libraries, necessitating innovative approaches that combine advanced scoring functions with intelligent library management strategies. This comparison guide examines three pioneering methodologies that address these challenges: an evolutionary algorithm (REvoLd), a machine learning-guided docking screen utilizing conformal prediction, and a hierarchical structure-based virtual screening protocol specifically applied to HER2 inhibitors. Each approach demonstrates unique strengths in balancing computational efficiency with predictive accuracy, offering researchers multiple pathways for advancing breast cancer drug discovery.
Experimental Protocols and Methodologies
Evolutionary Algorithm Screening (REvoLd)
The REvoLd protocol employs an evolutionary algorithm to efficiently explore combinatorial make-on-demand chemical space without exhaustive enumeration of all molecules [56]. The methodology exploits the structural feature of make-on-demand libraries being constructed from lists of substrates and chemical reactions.
Key Experimental Parameters:
- Library: Enamine REAL space (over 20 billion molecules)
- Docking Method: RosettaLigand flexible docking protocol
- Initial Population: 200 randomly created ligands
- Generations: 30 generations of optimization
- Selection: 50 individuals advanced to next generation
- Reproduction Mechanics: Crossovers between fit molecules, fragment switching mutations, and reaction-changing mutations
The algorithm initiates with a diverse random population, then iteratively applies selection pressure and genetic operators to evolve promising candidates. Multiple independent runs (typically 20 per target) are recommended to explore different regions of chemical space, with each run docking between 49,000-76,000 unique molecules per target [56].
Machine Learning-Guided Docking with Conformal Prediction
This workflow combines machine learning classification with molecular docking to enable rapid virtual screening of billion-compound libraries [57]. The approach uses Mondrian conformal predictors to make statistically valid selections from ultra-large libraries.
Experimental Protocol:
- Initial Docking: 1 million compounds docked to target protein
- Classifier Training: CatBoost algorithm trained on Morgan2 fingerprints
- Conformal Prediction: Application of CP framework with significance level (ε)
- Virtual Active Set: Reduced compound library for explicit docking
- Experimental Validation: Testing predictions against G protein-coupled receptors
The method was optimized using docking scores for 235 million compounds from the ZINC15 library against A2A adenosine (A2AR) and D2 dopamine (D2R) receptors [57]. The significance level was set to achieve maximal efficiency (A2AR εopt = 0.12 and D2R εopt = 0.08), ensuring the percentage of incorrectly classified compounds did not exceed these thresholds.
Hierarchical Virtual Screening for HER2 Inhibitors
This structure-based protocol implements a multi-stage docking approach to identify natural product-derived HER2 inhibitors [8]. The method was specifically applied to breast cancer targeting the HER2 tyrosine kinase domain.
Screening Workflow:
- Library Preparation: 638,960 natural products from nine commercial databases
- HTVS Docking: High-throughput virtual screening (Glide HTVS)
- SP Docking: Standard precision docking of top 10,000 compounds
- XP Docking: Extra precision docking of top 500 compounds
- ADME Prediction: Schrödinger's QikProp module for pharmacokinetic properties
- Experimental Validation: Biochemical, cellular, and molecular dynamics analyses
The binding site was defined using a 20×20×20 Å grid around the co-crystallized ligand (TAK-285) centroid in the HER2 tyrosine kinase domain (PDB ID: 3RCD) [8]. The protocol was validated using a training set of 18 standard HER2 kinase inhibitors including lapatinib and neratinib.
Performance Comparison and Experimental Data
Quantitative Performance Metrics
Table 1: Performance Comparison Across Virtual Screening Methods
| Method | Library Size | Screening Efficiency | Hit Rate Improvement | Computational Reduction |
|---|---|---|---|---|
| REvoLd (Evolutionary Algorithm) | 20 billion molecules | 49,000-76,000 molecules docked per target | 869-1622x over random selection | Not explicitly quantified |
| ML-Guided Docking (Conformal Prediction) | 3.5 billion compounds | ~10% of library requiring explicit docking | Sensitivity: 0.87-0.88 | 1000-fold reduction in computational cost |
| Hierarchical HER2 Screening | 638,960 natural products | 500 compounds reaching XP stage | 4 biochemically validated hits | Not explicitly quantified |
Table 2: Application to Breast Cancer Subtypes
| Method | Molecular Targets | Breast Cancer Relevance | Experimental Validation |
|---|---|---|---|
| REvoLd | 5 drug targets | Benchmark included cancer-relevant targets | Experimental testing confirmed ligand discovery |
| ML-Guided Docking | A2AR, D2R receptors | GPCRs relevant to cancer signaling | Identified multi-target ligands for therapeutic effect |
| Hierarchical HER2 Screening | HER2 tyrosine kinase | Direct targeting of HER2+ breast cancer | Biochemical suppression of HER2 with nanomolar potency |
Method-Specific Performance Insights
The REvoLd evolutionary algorithm demonstrated remarkable efficiency in hit discovery, improving hit rates by factors between 869 and 1622 compared to random selections [56]. This approach consistently identified promising compounds with just a few thousand docking calculations while maintaining high synthetic accessibility through its exploitation of make-on-demand library structures.
The machine learning-guided approach achieved sensitivity values of 0.87-0.88, meaning it could identify close to 90% of virtual actives by docking only approximately 10% of the ultra-large library [57]. The conformal prediction framework guaranteed that the percentage of incorrectly classified compounds did not exceed the predefined significance levels (8-12%), providing statistical confidence in the predictions.
The hierarchical HER2 screening identified four natural products (oroxin B, liquiritin, ligustroflavone, and mulberroside A) that suppressed HER2 catalysis with nanomolar potency [8]. Cellular assays revealed preferential anti-proliferative effects toward HER2-overexpressing breast cancer cells, with liquiritin emerging as a particularly promising pan-HER inhibitor candidate with notable selectivity indices.
Visual Workflows and Signaling Pathways
Evolutionary Algorithm Screening Workflow
Machine Learning-Guided Screening Pipeline
HER2 Signaling and Inhibition Pathway
Research Reagent Solutions
Table 3: Essential Research Tools for Virtual Screening
| Reagent/Tool | Function | Application Context |
|---|---|---|
| Enamine REAL Library | Make-on-demand compound source | Provides >20 billion synthetically accessible compounds for screening [56] |
| RosettaLigand | Flexible molecular docking | Accounts for full ligand and receptor flexibility during docking [56] |
| CatBoost Classifier | Machine learning algorithm | Rapid prediction of top-scoring compounds based on molecular fingerprints [57] |
| Conformal Prediction | Statistical framework | Provides valid confidence measures for classifier predictions [57] |
| Schrödinger Suite | Molecular modeling platform | Protein preparation, grid generation, and hierarchical docking [8] |
| Morgan2 Fingerprints | Molecular representation | Substructure-based descriptors for machine learning [57] |
| HER2 Tyrosine Kinase (3RCD) | Crystal structure | Defines binding site for HER2-targeted virtual screening [8] |
| QikProp Module | ADME prediction | Computational assessment of pharmacokinetic properties [8] |
Comparative Analysis and Research Implications
Each virtual screening approach offers distinct advantages for breast cancer drug discovery. The REvoLd evolutionary algorithm provides exceptional efficiency for exploring ultra-large make-on-demand libraries, particularly valuable when prior structural knowledge is limited. Its ability to improve hit rates by several orders of magnitude while maintaining synthetic accessibility makes it ideal for initial discovery campaigns across multiple breast cancer subtypes.
The machine learning-guided docking approach delivers unprecedented computational efficiency for screening trillion-compound libraries, reducing resource requirements by 1000-fold while maintaining high sensitivity [57]. This method is particularly suited for targets where sufficient training data exists and when researchers require statistical confidence in their predictions.
The hierarchical HER2 screening protocol demonstrates exceptional specificity for targeting particular breast cancer subtypes, successfully identifying natural product-derived HER2 inhibitors with nanomolar potency [8]. This approach is invaluable for focused discovery efforts against well-characterized targets like HER2, especially when combined with experimental validation.
For researchers working across breast cancer subtypes, the choice of virtual screening methodology should consider the target characterization, library size, computational resources, and required confidence levels. The integration of these approaches represents the future of virtual screening, potentially enabling efficient navigation of chemical space while delivering subtype-specific therapeutic candidates for breast cancer treatment.
Accounting for Tumor Heterogeneity and Protein Flexibility
In the pursuit of effective therapeutics for breast cancer, computational drug discovery faces two paramount challenges: the profound molecular heterogeneity of tumors and the dynamic flexibility of protein targets. Breast cancer is not a single disease but a collection of subtypes, each driven by distinct genetic, epigenetic, and transcriptomic profiles that influence drug response and resistance [58] [59]. Simultaneously, the proteins targeted by drugs are not static; their conformational changes and binding site dynamics are crucial for accurate ligand docking in virtual screening (VS) [60]. This guide objectively compares the performance of current virtual screening methodologies, focusing on their capacity to integrate multi-omics data for addressing tumor heterogeneity and incorporate sophisticated molecular dynamics for modeling protein flexibility. We frame this evaluation within a broader benchmarking thesis to aid researchers in selecting optimal tools for subtype-specific breast cancer drug discovery.
Understanding the Biological Complexities
The Multifaceted Nature of Breast Tumor Heterogeneity
Breast cancer heterogeneity operates across multiple molecular layers:
- Genetic Alterations: Driver mutations in genes such as
TP53,BRCA1/2, andPIK3CAinitiate and propel tumor evolution. These mutations are associated with varied clinical outcomes and therapeutic sensitivities [59]. For instance,TP53mutations are linked to poor prognosis and altered immune infiltration [59]. - Immune Microenvironment: The tumor immune microenvironment (TIME) is highly heterogeneous, comprising tumor-infiltrating lymphocytes (TILs) and tertiary lymphoid structures (TLSs). Mechanisms of immune evasion, including downregulation of antigen presentation and recruitment of immunosuppressive cells, differ significantly across molecular subtypes [59].
- Molecular Subtypes: Classifications such as luminal A, triple-negative, and HER2-positive present distinct therapeutic targets and vulnerabilities. Multi-omics integration—combining genomics, transcriptomics, and epigenomics—is essential to identify robust biomarkers that capture this complexity [58].
The Critical Role of Protein Flexibility
Protein flexibility is a fundamental physical property that impacts drug binding:
- Induced Fit: Ligand binding often induces conformational changes in the receptor's binding site. Physics-based docking methods that model flexible side chains and limited backbone movement can more accurately predict binding poses and affinities compared to rigid protocols [60].
- Allosteric Regulation: The influence of binding at one site on the function of a distant site is a key mechanism that requires an understanding of protein dynamics.
Comparative Analysis of Virtual Screening Platforms
The table below compares the performance of selected virtual screening methods, with a focus on their approaches to protein flexibility and applicability to heterogeneous cancer targets.
Table 1: Benchmarking Virtual Screening Platforms for Complex Cancer Targets
| Platform/Method | Core Approach | Handling of Protein Flexibility | Reported Performance Metrics | Applicability to Breast Cancer Heterogeneity |
|---|---|---|---|---|
| RosettaVS [60] | Physics-based force field (RosettaGenFF-VS) with AI-accelerated active learning. | Models full side-chain and limited backbone flexibility in high-precision mode. | Docking Power: Top performer on CASF-2016 benchmark.Screening Power: EF1% = 16.72; identifies best binder in top 1% [60]. | High; demonstrated on unrelated biological targets; flexible protocol suitable for diverse mutant proteins. |
| Machine Learning (NB, kNN, SVM, RF, ANN) [61] | Ligand- or structure-based screening using classical ML algorithms. | Typically relies on a single, rigid protein conformation for structure-based approaches. | Success varies; dependent on training data quality and diversity. ANN/CNN are noted as the future direction [61]. | Moderate; requires extensive, subtype-specific training data to implicitly capture heterogeneity. |
| Deep Learning (e.g., DeepMO, moBRCA-net) [58] | Deep neural networks for multi-omics integration and subtype classification. | Not primarily designed for atomic-level protein flexibility; focuses on molecular patterns. | Binary Classification Accuracy: ~78.2% for breast cancer subtypes [58]. | Very High; explicitly designed to integrate genomics, transcriptomics, and epigenomics for subtype analysis. |
| Multi-Modal Deep Learning with XAI [62] | Integration of genomics, histopathology, imaging, and clinical data with explainable AI (SHAP, LIME). | Flexibility is not a primary feature of the high-level integration framework. | Immunotherapy Response Prediction: AUC up to 0.80 in NSCLC [62]. | Very High; captures cross-scale dependencies and provides biological explanations for predictions. |
Experimental Protocols and Workflows
Protocol for Flexible Protein Virtual Screening with RosettaVS
This protocol is adapted from the OpenVS platform for ultra-large library screening [60].
System Preparation:
- Obtain the 3D structure of the target protein (e.g., from PDB). Define the binding site coordinates.
- Prepare the ligand library in a specified format (e.g., SDF), applying filters like Lipinski's Rule of Five and PAINS removal.
VS Express (VSX) Mode - Initial Triage:
- Run the VSX protocol, which uses a faster, less flexible docking model.
- The integrated active learning component trains a target-specific neural network in real-time to triage compounds for further analysis.
VS High-Precision (VSH) Mode - Refinement:
- Take the top-ranking compounds from VSX and subject them to the VSH protocol.
- VSH allows for full receptor side-chain flexibility and limited backbone movement to model induced fit.
- Binding affinities are ranked using the improved
RosettaGenFF-VSscoring function, which combines enthalpy (ΔH) and entropy (ΔS) terms.
Validation:
- Select top-ranked compounds for in vitro binding affinity assays (e.g., IC50 determination).
- Where possible, validate predicted binding poses using X-ray crystallography [60].
Protocol for Multi-Omics Subtype Stratification
This protocol outlines the workflow for incorporating tumor heterogeneity into research design, using methods like adaptive multi-omics integration [58].
Data Acquisition and Preprocessing:
- Collect multi-omics data (e.g., DNA sequencing, RNA expression, DNA methylation) from sources like The Cancer Genome Atlas (TCGA).
- Perform quality control, normalization, and batch effect correction (e.g., using Nested ComBat) [62].
Feature Selection and Integration:
- Employ genetic programming or other AI-driven methods to adaptively select the most informative features from each omics dataset [58].
- Fuse the selected features into a unified model. This can be early, intermediate, or late integration, with attention mechanisms dynamically weighting modality importance [62].
Model Training and Validation:
- Train a deep learning model (e.g., a transformer or graph neural network) for tasks like subtype classification or survival prediction.
- Validate the model using multi-cohort external validation to ensure generalizability across diverse populations [62].
- Apply Explainable AI (XAI) techniques like SHAP to interpret predictions and link them to biological mechanisms [62].
The following workflow diagram illustrates the parallel pathways for handling protein flexibility and tumor heterogeneity in a coordinated virtual screening campaign.
Virtual Screening Workflow Integrating Two Key Pathways
Successful virtual screening campaigns against heterogeneous breast cancers require a suite of computational and biological resources.
Table 2: Key Research Reagent Solutions for Virtual Screening in Breast Cancer
| Resource Category | Example | Function in Research |
|---|---|---|
| Computational Platforms | OpenVS Platform [60] | An open-source, AI-accelerated platform for high-performance virtual screening of ultra-large compound libraries. |
| Multi-Omics Data Repositories | The Cancer Genome Atlas (TCGA) [58] [62] | Provides comprehensive, publicly available genomic, epigenomic, and transcriptomic data from thousands of tumor samples for model training and validation. |
| Chemical Compound Libraries | ZINC, PubChem [61] | Curated databases of purchasable chemical compounds, providing the starting point for virtual screening campaigns. |
| Explainable AI (XAI) Tools | SHAP, LIME [62] | Provides post-hoc interpretability for complex AI models, linking predictions to input features (e.g., specific mutations or expression levels) for biological insight. |
| Validation Assays | Patient-Derived Organoids & Breast Cancer-on-a-Chip (BCOC) [59] | Advanced in vitro models that recapitulate the 3D tumor microenvironment and patient-specific heterogeneity for experimental validation of computational hits. |
Integrated Signaling Pathways in Breast Cancer Subtypes
The complex interplay of signaling pathways varies significantly across breast cancer subtypes, influencing virtual screening target selection. The diagram below maps key pathways and their interactions.
Key Signaling Pathways and Breast Cancer Subtypes
Benchmarking virtual screening performance in breast cancer research necessitates a dual focus on atomic-level protein dynamics and system-level tumor heterogeneity. Platforms like RosettaVS demonstrate that explicitly modeling protein flexibility through advanced physics-based force fields is critical for achieving high docking accuracy and lead enrichment [60]. Concurrently, multi-omics AI frameworks are indispensable for deconvoluting breast cancer heterogeneity, enabling subtype-specific biomarker discovery and patient stratification with proven improvements in predictive performance [58] [62]. The future of effective therapeutic discovery lies in the tighter integration of these two paradigms, creating workflows where flexible target screening is directly informed by deep molecular subtyping, all validated within physiologically relevant models like BCOCs [59]. This integrated approach provides a robust benchmark for accelerating personalized oncology.
Best Practices for Model Training and Avoiding Data Leakage
In the field of medical artificial intelligence (AI), particularly in high-stakes domains like breast cancer screening, the integrity of model training is paramount. Data leakage—the use of information during model training that would not be available in real-world prediction scenarios—represents a critical vulnerability that can compromise model validity and clinical utility. Within breast cancer research, where AI systems are increasingly deployed for tasks ranging from mammogram interpretation to malignancy classification, preventing data leakage is essential for developing models that generalize across diverse populations and clinical settings. This guide examines established protocols for leakage prevention and benchmarks performance across breast cancer subtypes, providing researchers with methodologies to ensure model robustness and reliability.
Understanding Data Leakage in Medical AI
Data leakage occurs when a model inadvertently gains access to information during training that it wouldn't have when deployed in actual clinical practice. This phenomenon undermines a model's ability to generalize and leads to misleading performance metrics that don't translate to real-world effectiveness [63] [64].
Primary Types and Causes of Data Leakage
| Leakage Type | Definition | Common Causes in Medical Research |
|---|---|---|
| Target Leakage | Using features that would not be available at prediction time [63] [64]. | Including post-diagnosis test results in predictive models; using "discharge status" to predict hospital readmission [63]. |
| Train-Test Contamination | When evaluation data influences the training process [63] [64]. | Applying preprocessing (normalization, imputation) to entire dataset before splitting; including test data in preprocessing steps [63] [64]. |
| Improper Data Splitting | Failing to maintain independence between training and test sets [63]. | Random splitting of time-series or patient data, allowing same patient in both sets; not using chronological splits for temporal data [63] [64]. |
| Preprocessing Leakage | Applying global transformations across full dataset before splitting [63]. | Calculating normalization statistics on full dataset; using future information for imputation during training [63] [64]. |
The consequences of data leakage are particularly severe in healthcare contexts. A review across 17 scientific fields found at least 294 papers affected by data leakage, leading to overly optimistic performance claims that don't hold up in real-world implementation [64]. In breast cancer detection, this can translate to models that appear highly accurate during testing but fail to generalize across diverse patient populations and clinical settings.
Data Leakage Prevention Framework
Proper Data Handling Protocols
Implementing rigorous data handling procedures forms the foundation of leakage prevention:
Temporal Data Splitting: For medical time-series data, split datasets chronologically to ensure models are trained on past data and tested on future data [64]. This mimics real-world deployment where models predict future outcomes based on historical information.
Group-Aware Splitting: When working with patient data, use grouped splits by patient ID to prevent the same patient from appearing in both training and test sets [63]. This maintains the independence assumption critical for valid evaluation.
Pipeline Automation: Implement automated data processing pipelines that apply preprocessing separately to training and test sets [65]. This reduces human error and ensures consistent data handling.
Preprocessing Isolation: Perform all preprocessing steps—including scaling, normalization, and imputation—only on the training data, then apply the derived parameters to the test set [63] [64].
Feature Engineering and Selection Guardrails
Feature selection requires careful consideration to avoid target leakage:
Temporal Validation: Audit every feature to verify it would be available at prediction time in clinical practice [63]. Use domain knowledge and data lineage tracking to ensure temporal validity.
Causal Relationship Analysis: Prioritize features with clear causal relationships to outcomes rather than those merely correlated [64]. In breast cancer prediction, this means distinguishing between genuine risk factors and incidental associations.
Cross-Validation Adaptation: Use time-series cross-validation or grouped cross-validation instead of standard k-fold approaches when dealing with medical data containing temporal or patient-specific dependencies [63].
Benchmarking AI Performance in Breast Cancer Detection
Performance Metrics Across Screening Modalities
Robust evaluation frameworks are essential for comparing AI systems in breast cancer detection. The following table summarizes key performance metrics from recent studies and consortium data:
| Screening Method | Cancer Detection Rate (per 1000) | Sensitivity | Specificity | Abnormal Interpretation Rate | Source |
|---|---|---|---|---|---|
| Digital Mammography (BCSC) | 4.1 | 86.9% | 88.9% | 11.6% | [66] |
| Digital Breast Tomosynthesis (Pre-AI) | 3.7 | - | - | 8.2% | [67] |
| Digital Breast Tomosynthesis (With AI) | 6.1 | - | - | 6.5% | [67] |
| RSNA AI Challenge (Top Algorithm) | - | 48.6% | 99.5% | 1.5% | [68] |
| RSNA AI Challenge (Top 10 Ensemble) | - | 67.8% | 97.8% | 3.5% | [68] |
The Breast Cancer Surveillance Consortium (BCSC) has established comprehensive performance benchmarks for screening mammography based on large-scale community practice data. Their studies highlight that while most radiologists surpass cancer detection recommendations, abnormal interpretation rates remain higher than recommended for almost half of practitioners [66]. These benchmarks provide critical baselines against which AI systems can be evaluated.
Performance Across Cancer Subtypes and Demographics
Understanding how AI performance varies across breast cancer subtypes and demographic groups is crucial for clinical implementation:
| Stratification Factor | Performance Variation | Study |
|---|---|---|
| Cancer Type | Higher sensitivity for invasive cancers (68.0%) vs. non-invasive (43.8%) | [68] |
| Geographic Location | Lower sensitivity in U.S. datasets (52.0%) vs. Australian (68.1%) | [68] |
| Breast Density | Higher interval cancer rates for women with extremely dense breasts | [69] |
| Dataset Diversity | Performance degradation when models trained on Caucasian populations are applied to Asian populations | [70] |
Recent research has revealed significant performance disparities across demographic groups. Models trained predominantly on Caucasian populations demonstrate limited generalizability to Asian populations, who typically have higher breast density and earlier cancer onset [70]. This highlights the critical need for diverse, representative training datasets and stratified performance reporting.
Experimental Protocols for Benchmarking Studies
Performance Metric Definitions and Calculations
Standardized metrics are essential for comparing screening performance across studies:
Cancer Detection Rate (CDR): Calculated as the number of cancers detected per 1000 screening examinations [66] [67]. Cancers are typically defined as those diagnosed within 365 days of screening and before the next screening examination.
Sensitivity: The proportion of true-positive cancers among all cancers present in the screened population [66]. The BCSC defines sensitivity as the percentage of screening mammograms with cancer diagnosed within 1 year that were correctly interpreted as positive.
Specificity: The proportion of true-negative examinations among all cancer-free screening examinations [66]. Calculated as the percentage of screening mammograms without cancer that were correctly interpreted as negative.
Abnormal Interpretation Rate (AIR): The percentage of screening examinations interpreted as positive (BI-RADS 0, 3, 4, or 5) [66] [67].
Positive Predictive Values: PPV1 represents the percentage of screening examinations with abnormal interpretation that resulted in cancer diagnosis; PPV3 represents the percentage of biopsies that resulted in cancer diagnosis [67].
Final Assessment Metrics Protocol
The BCSC has developed enhanced performance metrics based on the final assessment of the entire screening episode rather than just the initial assessment [69]. This approach includes:
Episode Definition: A screening episode includes the initial screening mammogram and all subsequent diagnostic imaging within 90 days following abnormal screens (BI-RADS 0 assessment) and prior to biopsy [69].
Final Assessment Classification: Positive screening episodes are defined as those with final BI-RADS assessment categories 3, 4, or 5, acknowledging that category 3 assessments often lead to cancer diagnosis through short-interval follow-up [69].
Outcome Tracking: Cancer status is determined based on standard 365-day follow-up, with interval cancers defined as those diagnosed within 1 year after a negative screening episode but before the next scheduled screen [69].
Data Leakage Prevention Tools and Techniques
| Tool/Technique | Function | Implementation Example |
|---|---|---|
| Differential Privacy | Adds mathematical noise to protect individual data points while maintaining statistical utility [65]. | Applying noise injection to training data for breast cancer models while preserving diagnostic patterns. |
| Synthetic Data Generation | Creates artificial datasets with similar statistical properties to real data without containing actual patient information [63]. | Generating synthetic mammography data to augment training sets while protecting patient privacy. |
| Automated Pipeline Tools | Implements consistent, reproducible data preprocessing and splitting protocols [63] [65]. | Using tools like Tonic.ai or custom scripts to ensure proper data segregation throughout model development. |
| Feature Importance Analysis | Identifies features with disproportionate influence on model predictions that may indicate leakage [64]. | Using SHAP analysis to detect if models are relying on temporally invalid features in breast cancer prediction. |
| Data Lineage Tracking | Monitors data provenance throughout the machine learning lifecycle [63]. | Implementing version control for datasets and preprocessing steps to trace potential leakage sources. |
| Resource | Application | Key Features |
|---|---|---|
| BCSC Performance Benchmarks | Reference standards for screening mammography performance [66] [69]. | Community practice data from multiple registries; metrics for digital mammography and tomosynthesis. |
| RSNA AI Challenge Dataset | Standardized evaluation for AI algorithms in mammography [68]. | Curated dataset with cancer cases confirmed by pathology and non-cancer cases with 1-year follow-up. |
| Explainable AI (XAI) Frameworks | Model interpretability for clinical validation [71]. | SHAP analysis; decision tree visualization; feature contribution mapping. |
| Cross-Validation Methodologies | Robust performance estimation while preventing leakage [64]. | Time-series cross-validation; grouped cross-validation by patient; nested cross-validation. |
Implementing rigorous data leakage prevention strategies is fundamental to developing valid, generalizable AI models for breast cancer detection. The practices outlined—proper data splitting, temporal validation of features, preprocessing isolation, and diverse dataset curation—form essential safeguards against misleading performance metrics. As AI systems increasingly integrate into breast cancer screening pathways, maintaining methodological rigor in model development and adopting comprehensive benchmarking approaches will be critical for ensuring equitable performance across diverse populations and breast cancer subtypes. The research community must prioritize transparency in reporting methodologies and validation results to advance the field responsibly and earn the trust of clinicians and patients alike.
Benchmarking, Validation, and Cross-Method Comparison
This guide provides a comparative analysis of three established benchmarks for Virtual Screening (VS)—DUD-E, CASF, and LIT-PCBA—framed within the context of breast cancer research. For computational drug discovery scientists, the choice of benchmark is critical for reliably evaluating the performance of VS models in identifying novel therapeutics, particularly for complex and heterogeneous diseases like breast cancer.
Virtual screening benchmarks provide a standardized set of targets, active compounds, and decoy molecules to assess a model's ability to prioritize true binders. The core characteristics of the three benchmarks are summarized below.
Table 1: Core Characteristics of VS Benchmarks
| Feature | DUD-E | LIT-PCBA | CASF |
|---|---|---|---|
| Full Name | Directory of Useful Decoys, Enhanced | Literature-Powered Primary Screening Benchmark | Comparative Assessment of Scoring Functions |
| Primary Focus | Assessing ligand enrichment with property-matched decoys [72] [73] | Evaluating performance with experimentally validated negatives [74] [75] | Evaluating scoring functions for docking & scoring [74] |
| Active Compounds | 22,886 active compounds across 102 targets [72] | Actives and inactives from PubChem bioassays [74] [75] | Not specified in search results |
| Decoy/Inactive Source | 50 property-matched, topologically dissimilar computational decoys per active [72] [73] | Experimentally confirmed inactives from high-throughput screens [74] [75] | Not specified in search results |
| Key Advantage | Large target diversity; challenging decoys [73] | High fidelity due to experimental inactives; reduces false negative risk [74] [75] | Standardized for scoring function comparison |
Performance Metrics and Methodologies
A critical step in benchmarking is the use of appropriate metrics to measure the success of a virtual screen.
Traditional and Novel Enrichment Metrics
The Enrichment Factor (EF) is a standard metric that measures the ratio of actives found in a top fraction of a screened library compared to a random selection [74] [75]. A significant limitation of the traditional EF is that its maximum achievable value is capped by the ratio of inactives to actives in the benchmark set. For example, in DUD-E, this ratio is about 61:1, which is much lower than the ratios of 1000:1 or more encountered in real-life virtual screens of large compound libraries. This makes it impossible for the standard EF to measure the very high enrichments required for a model to be useful in practice [74] [75].
The Bayes Enrichment Factor (EFB) is a recently proposed metric designed to overcome this limitation [74] [75]. It is calculated as the fraction of actives scoring above a threshold divided by the fraction of random molecules scoring above the same threshold. The EFB does not depend on the inactive-to-active ratio and can, therefore, estimate much higher enrichments, providing a better indication of real-world performance [74] [75].
Experimental Protocol for Benchmarking
A typical workflow for evaluating a VS model using these benchmarks involves:
- Target Selection: Select a protein target of interest from the benchmark (e.g., a breast cancer-related protein like HER2 or HSP90).
- Data Preparation: Prepare the benchmark's structure file, active compounds, and decoy/inactive molecules for the chosen target.
- Molecular Docking: Perform docking of all active and decoy/inactive molecules against the target structure using the VS model to be evaluated.
- Score and Rank: Generate a docking score for each molecule and rank the entire library from best-scoring to worst-scoring.
- Performance Calculation: Calculate evaluation metrics like EF or EFB by analyzing the distribution of known actives within the ranked list [74] [75].
Diagram: Virtual Screening Benchmark Workflow. This flowchart outlines the standard experimental protocol for evaluating a VS model using established benchmarks.
Benchmarking Data and Comparative Performance
The choice of benchmark can significantly influence the perceived performance of a VS method.
Table 2: Representative Performance Data on DUD-E
| VS Model | Median EF1% | Median EF0.1% | Median EFmaxB |
|---|---|---|---|
| Vina | 7.0 | 11 | 32 |
| Vinardo | 11 | 20 | 48 |
| Dense (Pose) | 21 | 42 | 160 |
Note: Data presented is median values across all DUD-E targets. EFmaxB is the maximum Bayes Enrichment Factor achievable over the measurable χ interval. Adapted from [74] [75].
Performance varies widely across different models and benchmarks. For instance, on DUD-E, traditional scoring functions like Vina show modest enrichment, while more advanced machine-learning-based models can achieve significantly higher performance [74] [75]. Furthermore, a model's high performance on a benchmark like DUD-E does not guarantee success in prospective screens, especially if the benchmark has issues like data leakage between training and test sets, which can lead to over-optimistic results. Newer benchmarks like BayesBind have been created with rigorous splits specifically to address this issue for machine learning models [74] [75].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents and Resources
| Item Name | Function in VS Benchmarking |
|---|---|
| DUD-E Database | Provides targets, active ligands, and property-matched decoys to test a model's ability to avoid false positives [72] [73]. |
| LIT-PCBA Dataset | Supplies experimentally validated active and inactive compounds, offering a high-fidelity benchmark to reduce the risk of false negatives [74] [75]. |
| AutoDock Vina | A widely used molecular docking program that serves as a common baseline for comparing the performance of novel VS methods [76]. |
| PDB (Protein Data Bank) | The source for high-resolution 3D protein structures (e.g., EGFR: 1M17; HSP90: 3TUH) essential for structure-based virtual screening [76]. |
| ChEMBL Database | A repository of bioactive molecules with curated binding data, used as a source for active ligands in benchmarks like DUD-E [73]. |
Application in Breast Cancer Research
The application of these benchmarks in breast cancer research is vital for developing reliable computational models. Key breast cancer targets include:
- Human Epidermal Growth Factor Receptor 2 (HER2): Overexpressed in 15-30% of invasive breast cancers and a critical prognostic and predictive marker [76] [55].
- Epidermal Growth Factor Receptor (EGFR): Often amplified in specific phenotypes like metaplastic triple-negative breast cancer (TNBC) [76].
- Heat Shock Protein 90 (HSP90): Overexpressed in breast ductal carcinomas and crucial for the stability of many oncogenic proteins [76].
Diagram: Key Breast Cancer VS Targets. This diagram illustrates three high-priority protein targets for virtual screening in breast cancer and their primary oncogenic roles [76] [55].
Breast cancer's heterogeneity, with distinct molecular subtypes (Luminal A, Luminal B, HER2-enriched, Triple-negative), further complicates drug discovery [55] [77]. Benchmarks that account for this diversity are essential. For example, a VS model could be rigorously tested on a benchmark's HER2 target to evaluate its potential for discovering drugs for the HER2-enriched subtype.
In the field of breast cancer research, virtual screening has emerged as a powerful computational approach for identifying potential therapeutic compounds by rapidly evaluating large chemical libraries against specific molecular targets. The reliability of these screening campaigns depends critically on the metrics used to evaluate their performance. For researchers, scientists, and drug development professionals, understanding the proper application and interpretation of key metrics—including Enrichment Factors (EF), Area Under the Curve (AUC), and Hit Rates (HR)—is fundamental to accurately assessing virtual screening methodologies and comparing their effectiveness across different breast cancer subtypes.
Breast cancer's molecular heterogeneity, with distinct subtypes such as Luminal A, Luminal B, HER2-positive, and triple-negative, presents unique challenges for virtual screening. Each subtype involves different signaling pathways and molecular drivers, requiring tailored screening approaches and careful benchmarking of results. This guide provides a comprehensive comparison of virtual screening performance metrics within this context, supported by experimental data and methodological protocols to ensure rigorous evaluation across breast cancer subtypes.
Core Metrics for Virtual Screening Performance
Definition and Calculation of Key Metrics
Virtual screening performance is quantified through several standardized metrics that provide complementary insights into a method's ability to identify true active compounds. The Enrichment Factor (EF) measures the concentration of active compounds found early in a ranked list compared to a random selection, typically calculated at specific percentiles of the screened library (e.g., EF1%, EF5%). A higher EF indicates better early recognition performance, which is particularly valuable when computational resources for further investigation are limited.
The Area Under the Curve (AUC) of the Receiver Operating Characteristic (ROC) curve provides an aggregate measure of performance across all possible classification thresholds. The ROC curve plots the true positive rate against the false positive rate, and the AUC represents the probability that a classifier will rank a randomly chosen positive instance higher than a randomly chosen negative one. Values range from 0 to 1, with 0.5 indicating random performance and 1.0 representing perfect separation.
Hit Rate (HR), sometimes referred to as yield, represents the proportion of truly active compounds identified within a selected subset of the screened library. It is typically calculated as the number of confirmed active compounds divided by the total number of compounds selected for testing. This metric is particularly useful for estimating the practical efficiency of a virtual screening campaign in terms of experimental follow-up requirements.
Comparative Analysis of Metric Performance
Table 1: Comparative Performance of Virtual Screening Metrics Across Methodologies
| Screening Method | AUC Range | Early Enrichment (EF1%) | Hit Rate (%) | Optimal Use Case |
|---|---|---|---|---|
| Molecular Docking | 0.6-0.8 | 5-15 | 10-25 | Structure-based screening with known protein structures |
| MM-GBSA | 0.7-0.9 | 10-30 | 15-35 | Binding affinity refinement and ranking |
| Ensemble Docking | 0.7-0.85 | 15-35 | 20-40 | Flexible receptor screening |
| Machine Learning | 0.65-0.95 | 20-50 | 25-60 | Large library pre-screening with sufficient training data |
The table above demonstrates that methods incorporating binding affinity calculations like MM-GBSA and Ensemble Docking generally achieve higher early enrichment and hit rates, though molecular docking remains widely used for its balance of performance and computational efficiency [78]. The variation in metric performance highlights the importance of selecting virtual screening approaches based on specific research objectives, available structural information, and computational resources.
Experimental Protocols for Method Evaluation
Structure-Based Virtual Screening Workflow
A comprehensive structure-based virtual screening protocol for breast cancer targets involves multiple stages of increasing computational complexity. The initial phase typically employs molecular docking against relevant breast cancer targets such as estrogen receptor alpha (ERα) for hormone receptor-positive subtypes or HER2 for HER2-positive breast cancer. Docking calculations employ scoring functions to predict binding poses and affinities, generating an initial ranked list of compounds.
Advanced protocols often incorporate induced-fit docking (IFD) to account for receptor flexibility, which is particularly important for targets with known conformational changes upon ligand binding. For even greater accuracy, quantum-polarized ligand docking (QPLD) can be implemented to more precisely model electronic interactions during binding. The most computationally intensive approaches apply molecular mechanics/generalized Born surface area (MM-GBSA) calculations to refine binding affinity predictions by estimating solvation effects and explicit binding energies [78].
Validation of these protocols requires benchmarking against known active and inactive compounds for each specific breast cancer target. Performance is evaluated using the metrics described in Section 2, with careful attention to the statistical significance of differences between methodologies. This is particularly important when comparing performance across different breast cancer subtypes, as target properties can significantly influence metric values.
Data Fusion and Pose Selection Strategies
The statistical analysis of virtual screening results requires careful consideration of data fusion techniques and pose selection strategies. Research has demonstrated that the method of combining results from multiple screening approaches significantly impacts performance metrics. Minimum fusion approaches have shown particular robustness across varying conditions, consistently outperforming arithmetic, geometric, and Euclidean averaging methods in compound ranking accuracy [78].
The number of docking poses considered also substantially influences metric performance. Studies evaluating pose counts ranging from 1 to 100 have demonstrated that increasing pose numbers generally reduces predictive accuracy for early enrichment metrics, highlighting the importance of optimal pose selection rather than exhaustive consideration [78]. These findings suggest that virtual screening protocols should prioritize quality over quantity in pose selection to maximize enrichment factors and hit rates.
When using experimental reference values for validation, studies indicate that pIC50 values (negative logarithm of IC50) provide higher Pearson correlations with predicted binding affinities compared to raw IC50 values, while both metrics perform similarly in non-parametric Spearman rankings [78]. This distinction is important for researchers designing validation protocols for breast cancer target screens.
Virtual Screening Workflow for Breast Cancer Targets
Breast Cancer Subtype Considerations in Virtual Screening
Molecular Subtype-Specific Screening Strategies
Breast cancer heterogeneity necessitates subtype-specific virtual screening approaches. For hormone receptor-positive (HR+) breast cancers, which constitute approximately 70% of cases, virtual screening typically focuses on targets like the estrogen receptor (ERα). Studies have successfully identified colchicine-based inhibitors demonstrating superior binding affinities (ΔGB values of -40.37 to -40.26 kcal/mol) compared to standard tamoxifen therapy (ΔGB = -38.66 kcal/mol) [9]. These findings highlight the potential of virtual screening to identify improved therapeutic options for the most common breast cancer subtype.
For HER2-positive breast cancer, virtual screening approaches target the HER2 receptor or downstream signaling components. The clinical success of antibody-drug conjugates like trastuzumab deruxtecan (T-DXd) in recent trials underscores the importance of targeting this pathway [79] [80]. Virtual screening for triple-negative breast cancer (TNBC), the most aggressive subtype with limited treatment options, often focuses on alternative targets such as cell cycle regulators, immune checkpoints, or metabolic enzymes identified through CRISPR-cas9 screening as essential for cancer cell survival [81].
Multi-Omics Integration for Enhanced Screening
Advanced virtual screening approaches increasingly incorporate multi-omics data to improve specificity across breast cancer subtypes. Methods like Differential Sparse Canonical Correlation Analysis (DSCCN) integrate mRNA expression and DNA methylation data to identify highly correlated molecular features that distinguish breast cancer subtypes [82]. This approach effectively addresses the "large p, small n" problem (many features, few samples) common in genomics data by selecting differentially expressed genes prior to correlation analysis.
Deep learning models represent another frontier in subtype-specific screening, with architectures like DenseNet121-CBAM achieving AUC values of 0.759 for distinguishing Luminal versus non-Luminal subtypes and 0.72 for identifying triple-negative breast cancer directly from mammography images [17]. While these approaches currently focus on diagnostic classification, their principles can be adapted to virtual screening by linking molecular features with compound sensitivity profiles.
Table 2: Breast Cancer Subtype-Specific Screening Targets and Metrics
| Breast Cancer Subtype | Primary Molecular Targets | Characteristic Metrics | Special Considerations |
|---|---|---|---|
| Luminal A (HR+/HER2-) | ERα, PR, CDK4/6 | High AUC (>0.8), Moderate EF | Endocrine resistance mechanisms |
| Luminal B (HR+/HER2+) | ERα, HER2, CDK4/6 | Variable EF, High specificity | Dual targeting approaches |
| HER2-positive (HR-/HER2+) | HER2, PI3K, mTOR | High early enrichment | Binding site conformational flexibility |
| Triple-Negative (HR-/HER2-) | Cell cycle regulators, PARP, Immune checkpoints | Moderate AUC, High hit rate | Limited target options |
Pathway Visualization and Analytical Frameworks
Key Signaling Pathways in Breast Cancer
Understanding the key signaling pathways in breast cancer provides essential context for target selection in virtual screening campaigns. The cell cycle pathway has been identified as particularly significant, with CRISPR-cas9 screening revealing essential genes in this pathway that represent vulnerable points for therapeutic intervention across multiple breast cancer subtypes [81]. This finding aligns with the clinical success of CDK4/6 inhibitors in HR+ breast cancer and supports continued focus on cell cycle regulators in virtual screening.
For HR+ breast cancers, the estrogen receptor signaling pathway remains a primary focus, with virtual screening identifying novel approaches to overcome resistance mechanisms such as ESR1 mutations [80] [9]. The PI3K/AKT/mTOR pathway represents another key signaling network frequently altered in breast cancer, with the FINER trial demonstrating that adding the AKT inhibitor ipatasertib to fulvestrant improved progression-free survival from 1.94 to 5.32 months in patients who had progressed on prior CDK4/6 inhibitor therapy [80].
Breast Cancer Pathways and Screening Targets
Essential Research Reagents and Computational Tools
Research Reagent Solutions for Virtual Screening
Table 3: Essential Research Reagents and Computational Tools
| Resource Category | Specific Tools/Resources | Application in Virtual Screening | Performance Considerations |
|---|---|---|---|
| Protein Structure Databases | PDB, AlphaFold DB | Source of 3D structures for docking | Resolution, completeness, and validation status critical |
| Compound Libraries | ZINC, ChEMBL, PubChem | Source of small molecules for screening | Diversity, drug-likeness, and lead-likeness properties |
| Computational Docking Software | AutoDock, Glide, GOLD | Pose prediction and scoring | Scoring function accuracy and computational efficiency |
| Molecular Dynamics Packages | AMBER, GROMACS, NAMD | Binding affinity refinement and stability assessment | Force field accuracy and sampling efficiency |
| Breast Cancer Cell Line Models | MCF-7, MDA-MB-231, BT-474 | Experimental validation of screening hits | Representativeness of specific breast cancer subtypes |
| Multi-omics Data Resources | TCGA, METABRIC, DepMap | Contextualizing targets within subtype biology | Sample size, data quality, and clinical annotations |
The resources listed in Table 3 represent essential components of a comprehensive virtual screening pipeline for breast cancer drug discovery. The Protein Data Bank (PDB) provides experimentally determined structures of key breast cancer targets, with studies typically employing multiple structures (e.g., four distinct urease structures in one benchmarking study) to assess methodological robustness [78]. For targets lacking experimental structures, AlphaFold DB offers high-accuracy predicted structures.
Compound libraries like ZINC and ChEMBL provide curated collections of screening compounds with associated properties. The Cancer Dependency Map (DepMap) offers functional genomics data from CRISPR-cas9 screens across breast cancer cell lines, identifying essential genes that represent potential vulnerabilities [81]. Integration of these diverse data sources enhances the contextual relevance of virtual screening for specific breast cancer subtypes.
The benchmarking of virtual screening performance through metrics like Enrichment Factors, AUC, and Hit Rates provides critical guidance for method selection and optimization in breast cancer research. Current evidence indicates that MM-GBSA and ensemble docking approaches consistently outperform simpler methods in compound ranking, though optimal methodology depends on the specific breast cancer target and screening context [78]. The integration of multi-omics data and machine learning approaches represents a promising direction for enhancing subtype-specific screening performance.
Future developments in virtual screening for breast cancer will likely focus on adaptive scoring frameworks that dynamically adjust weighting based on target properties and screening objectives [78]. Additionally, the integration of real-world clinical response data with virtual screening results, as exemplified by trials such as DESTINY-Breast09, SERENA-6, and ASCENT-04/KEYNOTE-D19 [80], will further refine screening approaches and validation protocols. As virtual screening methodologies continue to evolve, maintaining rigorous benchmarking against standardized metrics will remain essential for advancing breast cancer drug discovery across diverse molecular subtypes.
Comparative Analysis of Physics-Based vs. Deep Learning Scoring Functions
Virtual screening has become an indispensable tool in early drug discovery, with its success crucially dependent on the accuracy of the scoring functions used to predict protein-ligand binding [60] [83]. These computational methods help narrow down billions of potential compounds to a manageable number of promising candidates for experimental testing. The emergence of ultra-large chemical libraries containing billions of make-on-demand compounds has intensified the need for reliable and efficient scoring functions [84]. Within breast cancer research, where molecular subtypes such as Luminal A, Luminal B, HER2-positive, and triple-negative require different therapeutic strategies, accurate virtual screening is particularly valuable for identifying subtype-specific treatments [17].
The current landscape of scoring functions is primarily divided between two paradigms: traditional physics-based methods and increasingly popular deep learning approaches. Physics-based functions rely on mathematical representations of physical and chemical forces governing molecular interactions, while deep learning methods leverage pattern recognition from large datasets of protein-ligand complexes [83]. This review provides a comprehensive comparative analysis of these approaches, examining their underlying principles, performance benchmarks, and practical applications in breast cancer drug discovery. We focus specifically on their performance in structure-based virtual screening, where the three-dimensional structure of the target protein is known and used to predict ligand binding.
Fundamental Approaches and Methodologies
Physics-Based Scoring Functions
Physics-based scoring functions calculate binding affinity based on principles of molecular mechanics, typically incorporating terms for van der Waals interactions, hydrogen bonding, electrostatics, and desolvation effects. These methods explicitly model the physical forces that govern molecular recognition, with parameters often derived from theoretical principles or experimental data [83].
A representative state-of-the-art physics-based approach is RosettaVS, which incorporates an improved force field (RosettaGenFF-VS) that combines enthalpy calculations (ΔH) with entropy estimates (ΔS) upon ligand binding [60] [84]. This platform employs two distinct docking modes: Virtual Screening Express (VSX) for rapid initial screening and Virtual Screening High-precision (VSH) for final ranking of top hits, with the key difference being the inclusion of full receptor flexibility in VSH. Notably, RosettaVS accommodates substantial receptor flexibility, enabling modeling of flexible sidechains and limited backbone movement, which proves critical for targets requiring induced conformational changes upon ligand binding [84].
Deep Learning Scoring Functions
Deep learning scoring functions represent a paradigm shift from physics-based modeling to data-driven pattern recognition. These approaches utilize neural networks that learn complex relationships between protein-ligand structural features and binding affinities without relying on pre-defined physical equations [83].
These methods can be categorized as:
- Structure-Based Deep Learning (SBDL): Uses 3D structural information of protein-ligand complexes as input
- Ligand-Based Deep Learning (LBDL): Utilizes chemical structure information of ligands alone
SBDL models often employ convolutional neural networks (CNNs) that automatically extract relevant features from 3D complex structures, eliminating the need for manual feature engineering [83]. Popular architectures include CNN-based models like KDeep, Pafnucy, and DeepDTA, which have demonstrated competitive performance in binding affinity prediction [83]. These models typically use structural databases such as PDBBind, CSAR, CASF, and the Astex diverse set for training and validation [83].
Table 1: Key Characteristics of Scoring Function Approaches
| Characteristic | Physics-Based | Deep Learning |
|---|---|---|
| Theoretical Basis | Molecular mechanics principles | Pattern recognition from data |
| Input Data | Protein-ligand coordinates | Structural features or raw complex data |
| Receptor Flexibility | Explicitly modeled (e.g., RosettaVS) | Limited by training data |
| Training Data Requirements | Minimal (parameterization) | Large datasets (thousands of complexes) |
| Interpretability | High (specific interaction terms) | Low ("black box" nature) |
| Computational Demand | High for flexible docking | Lower after training |
Performance Benchmarking
Established Benchmarking Datasets and Protocols
Standardized datasets and evaluation protocols enable direct comparison between different scoring functions. Key benchmarks include:
CASF-2016 Benchmark: Consists of 285 diverse protein-ligand complexes specifically designed for scoring function evaluation [60] [84]. This benchmark provides small molecule structures as decoys, effectively decoupling the scoring process from conformational sampling. Standard tests include:
- Docking Power: Ability to identify native binding poses among decoys
- Screening Power: Capability to identify true binders among negative molecules, measured via enrichment factors (EF) and success rates at top 1%, 5%, and 10% cutoffs
DUD Dataset: Contains 40 pharmaceutically relevant protein targets with over 100,000 small molecules, used to evaluate virtual screening performance through AUC and ROC enrichment metrics [60].
For QSAR models used in virtual screening, recent research recommends prioritizing Positive Predictive Value (PPV) over traditional balanced accuracy, especially when screening ultra-large libraries where only a small fraction of top-ranked compounds can be experimentally tested [85]. This reflects the practical constraint of experimental follow-up, typically limited to 128 compounds corresponding to a single 1536-well plate format [85].
Comparative Performance Data
In rigorous benchmarking, physics-based methods like RosettaGenFF-VS have demonstrated top-tier performance. On the CASF-2016 benchmark, RosettaGenFF-VS achieved a top 1% enrichment factor (EF1%) of 16.72, significantly outperforming the second-best method (EF1% = 11.9) [60] [84]. The method also excelled in identifying the best binding small molecule within the top 1%, 5%, and 10% ranking molecules, surpassing all other physics-based methods in the comparison [84].
Deep learning methods have shown promising but mixed results. While some SBDL models report Pearson correlation coefficients (Rp) of 0.59-0.89 on binding affinity prediction tasks, their performance in real virtual screening scenarios is less consistently documented [83]. The DEELIG model currently leads with Rp = 0.89, followed by BgN-score (Rp = 0.86) and PerSPECT-ML (Rp = 0.84) [83].
Table 2: Quantitative Performance Comparison of Scoring Functions
| Method | Type | CASF-2016 EF1% | Binding Affinity Rp | Key Strengths |
|---|---|---|---|---|
| RosettaGenFF-VS | Physics-based | 16.72 | N/A | Receptor flexibility, pose accuracy |
| DEELIG | Deep Learning | N/A | 0.89 | Feature comprehension |
| BgN-score | Deep Learning | N/A | 0.86 | Binding affinity prediction |
| PerSPECT-ML | Deep Learning | N/A | 0.84 | Multi-task learning |
| TNet-BP | Deep Learning | N/A | 0.83 | Target-specific prediction |
Analysis across different protein pocket types reveals that physics-based methods show significant improvements in more polar, shallower, and smaller pockets compared to other approaches [84]. However, deep learning methods generally outperform physics-based functions in standard binding affinity prediction benchmarks when trained and tested on similar complexes [83].
Experimental Validation in Breast Cancer Research
Practical Applications and Case Studies
Experimental validation is the ultimate test of virtual screening performance. Both physics-based and deep learning approaches have demonstrated success in identifying novel ligands for therapeutic targets.
The physics-based RosettaVS platform was used to screen multi-billion compound libraries against two unrelated targets: KLHDC2 (a ubiquitin ligase) and the human voltage-gated sodium channel NaV1.7 [60] [84]. For KLHDC2, researchers discovered seven hit compounds (14% hit rate), while for NaV1.7, they identified four hits (44% hit rate), all with single-digit micromolar binding affinities [84]. Crucially, an X-ray crystallographic structure validated the predicted docking pose for a KLHDC2 ligand complex, demonstrating the method's effectiveness in lead discovery [60]. The entire screening process was completed in less than seven days using a high-performance computing cluster [84].
Deep learning methods have also shown promising results in breast cancer research applications. QSAR models with high PPV have been successfully employed for virtual screening campaigns, though specific hit rates for breast cancer targets are less frequently documented in the literature surveyed [85]. DL models have found significant utility in related areas such as predicting molecular subtypes from mammography images, with one DenseNet121-CBAM model achieving AUCs of 0.759 (Luminal vs. non-Luminal), 0.658 (HER2 status), and 0.668 (TN vs. non-TN) [17].
Performance in Real-World Virtual Screening
The ultimate validation of any virtual screening method comes from experimental confirmation of predicted hits. The high hit rates observed with RosettaVS (14-44%) [84] demonstrate the practical utility of physics-based approaches, particularly when combined with high-performance computing resources.
For deep learning models, the Positive Predictive Value (PPV) has emerged as a critical metric, especially when dealing with ultra-large chemical libraries [85]. Studies show that training on imbalanced datasets achieves a hit rate at least 30% higher than using balanced datasets, and the PPV metric captures this performance difference without parameter tuning [85]. This highlights the importance of selecting appropriate metrics aligned with the practical constraints of virtual screening campaigns, where typically only a few hundred compounds can be experimentally tested regardless of library size.
Integrated Workflow and Research Toolkit
Virtual Screening Workflow
The typical virtual screening process integrates multiple steps from target preparation to experimental validation. The following diagram illustrates a comprehensive workflow incorporating both physics-based and deep learning approaches:
Virtual Screening Workflow Integrating Physics-Based and ML Approaches. This diagram illustrates the comprehensive process of structure-based virtual screening, highlighting where physics-based (blue) and machine learning (red) scoring functions integrate into the workflow.
Research Reagent Solutions
Table 3: Essential Research Tools for Virtual Screening
| Tool/Resource | Type | Function | Access |
|---|---|---|---|
| RosettaVS | Physics-based platform | Flexible receptor docking & scoring | Open-source |
| Autodock Vina | Physics-based docking | Rigid receptor docking | Open-source |
| PDBBind | Database | Protein-ligand structures & affinities | Public |
| CASF-2016 | Benchmark set | Scoring function evaluation | Public |
| ChEMBL | Database | Bioactivity data for QSAR | Public |
| BINANA | Feature tool | Protein-ligand interaction descriptors | Open-source |
| PaDEL | Descriptor tool | Molecular descriptor calculation | Open-source |
Discussion and Future Perspectives
The comparative analysis reveals that both physics-based and deep learning scoring functions offer distinct advantages and face particular challenges. Physics-based methods like RosettaVS provide high interpretability and explicitly model receptor flexibility, which is crucial for certain protein targets [84]. Their demonstrated success in real-world virtual screening campaigns with high hit rates [84] makes them valuable for practical drug discovery applications.
Deep learning approaches excel at binding affinity prediction when sufficient training data is available, with some models achieving correlation coefficients up to 0.89 with experimental measurements [83]. However, their "black box" nature and limited generalizability to unseen complexes remain significant challenges [60] [84]. The performance advantage of deep learning methods appears most pronounced when the virtual screening target shares high similarity with complexes in the training data.
For breast cancer research specifically, where molecular subtypes dictate treatment strategies, both approaches offer complementary strengths. Physics-based methods may prove more reliable for novel targets with limited structural or bioactivity data, while deep learning models could provide advantages for well-characterized targets like hormone receptors or HER2.
Future developments will likely focus on hybrid approaches that combine the physical interpretability of traditional methods with the pattern recognition power of deep learning. As chemical libraries continue to grow into the billions of compounds, scoring functions with high positive predictive value will become increasingly essential for identifying promising therapeutic candidates [85]. The integration of these advanced computational methods holds significant promise for accelerating the discovery of novel treatments for breast cancer subtypes.
In the field of breast cancer research, the integration of computational predictions with experimental validation has become a cornerstone for advancing diagnostic and therapeutic strategies. This synergy is particularly critical in benchmarking virtual screening performance and developing AI-driven diagnostic tools for diverse breast cancer subtypes. Computational models, including deep learning and molecular docking simulations, provide high-throughput capabilities for identifying potential drug candidates and predicting molecular subtypes from medical imagery. However, their true utility and reliability are only established through rigorous correlation with experimental gold standards. This guide objectively compares the performance of various computational approaches, highlighting the essential role of experimental validation in ensuring their translational relevance for researchers, scientists, and drug development professionals.
Performance Benchmarking of Computational Tools
Virtual Screening Benchmarks for Drug Discovery
Structure-based virtual screening (SBVS) is a key computational approach in drug discovery. Benchmarking studies evaluate the performance of docking tools and machine learning (ML) scoring functions by measuring their ability to prioritize known bioactive molecules over inactive decoys. Performance is quantified using metrics such as Enrichment Factor at 1% (EF 1%), Area Under the Precision-Recall Curve (pROC-AUC), and Coefficient of Determination (R²) [86].
Table 1: Benchmarking Performance of Docking and ML Re-scoring for PfDHFR Variants
| Target Protein | Docking Tool | ML Re-scoring Function | Performance Metric | Value | Interpretation |
|---|---|---|---|---|---|
| Wild-Type (WT) PfDHFR | PLANTS | CNN-Score | EF 1% | 28 [86] | Best enrichment for WT variant |
| Quadruple-Mutant (Q) PfDHFR | FRED | CNN-Score | EF 1% | 31 [86] | Best enrichment for resistant Q variant |
| WT PfDHFR | AutoDock Vina | None (Default Scoring) | pROC-AUC | Worse-than-random [86] | Poor screening performance |
| WT PfDHFR | AutoDock Vina | RF-Score-VS v2 / CNN-Score | pROC-AUC | Better-than-random [86] | ML re-scoring significantly improves performance |
The data reveals that re-scoring docking outcomes with ML scoring functions like CNN-Score consistently augments SBVS performance, enriching diverse and high-affinity binders for both wild-type and resistant variants [86]. This benchmarking approach is directly applicable to breast cancer targets, such as mutant kinases or resistance-implicated receptors.
Deep Learning for Molecular Subtype Prediction from Mammography
Predicting the molecular subtype of breast cancer non-invasively is a major research focus. Deep learning models trained on conventional mammography images demonstrate promising but variable performance across subtypes.
Table 2: Deep Learning Model Performance for Predicting Molecular Subtypes
| Prediction Task | Model Architecture | Performance Metric | Value | Key Insight |
|---|---|---|---|---|
| Luminal vs. Non-Luminal | DenseNet121-CBAM | AUC | 0.759 [42] | Best binary classification performance |
| Triple-Negative vs. Non-TNBC | DenseNet121-CBAM | AUC | 0.668 [42] | Moderate predictive capability |
| HER2-positive vs. HER2-negative | DenseNet121-CBAM | AUC | 0.658 [42] | Most challenging binary prediction |
| Multiclass Subtype Classification | DenseNet121-CBAM | AUC | 0.649 [42] | Distinguishing all five subtypes is complex |
| HER2+/HR- Subtype | DenseNet121-CBAM | AUC | 0.78 [42] | Best performance in multiclass setting |
The model's interpretability, provided by Grad-CAM heatmaps, offers crucial validation by highlighting discriminative image regions, often corresponding to peritumoral tissue, which aligns with known pathological features [42].
Experimental Protocols for Validation
Validation Workflow for Computational Predictions
A robust validation workflow is essential to correlate computational predictions with biological reality. The process is iterative, involving both computational and experimental phases.
Detailed Methodologies for Key Experiments
Virtual Screening and Experimental Corroboration
The benchmarking protocol for virtual screening involves specific steps for both computational and experimental validation [86].
Computational Benchmarking Protocol:
- Protein Preparation: Crystal structures from the Protein Data Bank are prepared by removing water molecules, unnecessary ions, and redundant chains. Hydrogen atoms are added and optimized using tools like OpenEye's "Make Receptor".
- Ligand/Decoy Set Preparation: Known bioactive molecules and structurally similar but physiochemically matched inactive decoys are compiled from databases like DEKOIS 2.0. Ligands are prepared using tools like Omega to generate multiple conformations.
- Docking and Re-scoring: Docking simulations are performed using tools like AutoDock Vina, FRED, or PLANTS. The resulting poses are often re-scored with ML scoring functions like CNN-Score or RF-Score-VS v2 to improve enrichment.
- Performance Analysis: Enrichment is evaluated using EF 1% and pROC-AUC to quantify the tool's ability to rank active compounds above decoys.
Experimental Corroboration:
- Gold Standard Assays: The top-ranked compounds from virtual screening are progressed to in vitro binding assays (e.g., Surface Plasmon Resonance) and cell-based viability assays (e.g., MTT assays on breast cancer cell lines) to confirm target engagement and biological activity.
- Orthogonal Validation: For drug targets like kinase receptors, functional assays such as kinase activity inhibition and Western blotting to assess downstream signaling pathway modulation (e.g., MAPK/ERK) are used for orthogonal validation [87].
AI-Based Subtype Prediction and Pathological Validation
For AI models predicting breast cancer subtypes from mammography, validation follows a distinct pathway [42].
Model Development and Internal Validation:
- Data Curation: A retrospective cohort of patients with pathologically confirmed breast cancer and preoperative mammography is assembled. Regions of interest (ROIs) around tumors are annotated by qualified radiologists.
- Model Training: A deep learning architecture (e.g., DenseNet121 integrated with Convolutional Block Attention Modules) is trained on the ROIs. The model performs binary or multiclass classification tasks to predict molecular subtypes.
- Internal Performance Assessment: Model performance is evaluated via cross-validation on a held-out test set, using metrics like AUC, accuracy, sensitivity, and specificity. Interpretability heatmaps (Grad-CAM) are generated to visualize salient regions.
Pathological Validation:
- Gold Standard: The definitive molecular subtype is determined by postoperative histopathological examination of surgical specimens according to international consensus criteria (e.g., St. Gallen 2023). This involves Immunohistochemistry (IHC) testing for Estrogen Receptor (ER), Progesterone Receptor (PR), HER2, and Ki-67 [42].
- Correlation: The model's predictions are directly correlated against the IHC results. Statistical analysis determines the strength of association, and the Grad-CAM heatmaps are reviewed by pathologists to assess if the model's focus aligns with known radiological-pathological correlates, such as peritumoral regions for specific subtypes [42].
The Scientist's Toolkit: Research Reagent Solutions
Successful correlation of computational and experimental data relies on key reagents and tools.
Table 3: Essential Research Reagents and Tools for Validation
| Category | Item | Function in Validation |
|---|---|---|
| Computational Tools | AutoDock Vina, FRED, PLANTS [86] | Docking software for predicting ligand binding poses and affinities in virtual screening. |
| CNN-Score, RF-Score-VS v2 [86] | Machine Learning Scoring Functions for re-scoring docking outputs to improve enrichment of active compounds. | |
| DenseNet, Vision Transformers (ViTs), ResNet [38] [42] | Deep learning architectures for analyzing medical images (e.g., mammography) to predict cancer subtypes or detect lesions. | |
| Experimental Assays | Immunohistochemistry (IHC) Kits [42] | Gold standard for determining protein expression of ER, PR, HER2, and Ki-67 to define molecular subtypes from tissue. |
| Fluorescence In Situ Hybridization (FISH) [87] | Validates gene amplification status (e.g., HER2) and copy number alterations, offering orthogonal validation to IHC and sequencing. | |
| Cell-Based Viability Assays (e.g., MTT) | Measures the cytotoxic effect of potential drug candidates identified through virtual screening on breast cancer cell lines. | |
| Data & Benchmarks | DEKOIS 2.0 Benchmark Sets [86] | Provides curated sets of known active molecules and decoys for fair and rigorous benchmarking of virtual screening pipelines. |
| Public Repositories (TCIA, TCGA) [88] | Sources for linked radiology (e.g., MRI, mammography) and pathology data, essential for training and validating AI models. | |
| Specialized Reagents | Primary Antibodies (anti-ER, anti-PR, anti-HER2) [42] | Critical reagents for IHC to specifically detect and quantify biomarker expression in patient tissue sections. |
| Pathway-Specific Inhibitors/Activators | Used in functional assays to experimentally probe computational predictions about signaling pathways involved in breast cancer subtypes. |
Conclusion
Benchmarking virtual screening across breast cancer subtypes is not a mere technical exercise but a fundamental requirement for advancing personalized oncology. The key takeaway is that the distinct molecular landscapes of Luminal, HER2+, and TNBC subtypes demand tailored computational strategies. Success hinges on integrating AI and physics-based methods within robust, subtype-aware workflows that rigorously address challenges of data bias, tumor heterogeneity, and scoring function accuracy. Future progress will be driven by the development of more specialized benchmarks, the integration of multi-omics data for target triage, and the adoption of federated learning to leverage diverse, multi-institutional datasets while preserving privacy. Ultimately, the rigorous benchmarking and optimization of VS pipelines outlined here are poised to significantly accelerate the discovery of novel, subtype-specific therapeutics, moving us closer to truly personalized treatment for breast cancer patients.
References
- 1. Subtypes of Breast Cancer - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK583808/]
- 2. Understanding the Molecular Subtypes of Breast Cancer [https://www.bcrf.org/about-breast-cancer/molecular-subtypes-breast-cancer/]
- 3. The Molecular Subtypes of Breast Cancer [https://www.breastcancer.org/types/molecular-subtypes]
- 4. Dissecting the biological heterogeneity of HER2-positive ... [https://www.sciencedirect.com/science/article/pii/S0960977621004276]
- 5. Heterogeneity of triple negative breast cancer: Current ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-022-02476-1]
- 6. Redefining Breast Cancer Care by Harnessing Computational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471285/]
- 7. Computer-Aided Drug Design Across Breast Cancer ... [https://www.mdpi.com/1422-0067/26/21/10744]
- 8. Discovery of natural scaffolds as HER2 inhibitors for breast ... [https://www.nature.com/articles/s41598-025-11177-6]
- 9. Virtual screening, in silico pharmacokinetic and toxicity ... [https://www.sciencedirect.com/science/article/pii/S2214750025000447]
- 10. The Underlying Mechanisms and Emerging Strategies to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428164/]
- 11. The Underlying Mechanisms and Emerging Strategies to ... [https://www.mdpi.com/2072-6694/17/17/2938]
- 12. Decoding breast cancer treatment resistance through ... [https://pubmed.ncbi.nlm.nih.gov/40843360/]
- 13. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 14. Latest Research Into Overcoming Resistance to Breast ... [https://www.mskcc.org/news/latest-research-into-overcoming-resistance-to-breast-cancer-targeted-therapies]
- 15. 5 Breast Cancer Highlights to Know About From ASCO 2025 [https://www.bcrf.org/blog/asco-2025-breast-cancer-highlights/]
- 16. Metabolic reprogramming in breast cancer: Pathways ... [https://www.sciencedirect.com/science/article/pii/S0304419X25001386]
- 17. Predicting molecular subtype in breast cancer using deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479247/]
- 18. H&E to IHC virtual staining methods in breast cancer [https://www.nature.com/articles/s41746-025-01741-9]
- 19. Computer-Aided Drug Design Across Breast Cancer Subtypes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608970/]
- 20. Computational-aided drug design strategies for drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634332/]
- 21. Current trends in computer aided drug design and a ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523421005547]
- 22. Advancing computer-aided drug discovery (CADD) by big ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7572559/]
- 23. TransBreastNet a CNN transformer hybrid deep learning ... [https://www.nature.com/articles/s41598-025-19173-6]
- 24. Structure-Based Virtual Screening for Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC3282008/]
- 25. From Molecules to Medicines: The Role of AI-Driven Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300675/]
- 26. Revolutionizing pharmacology: AI-powered approaches in ... [https://www.sciencedirect.com/science/article/pii/S259009862500020X]
- 27. Advancements in breast cancer therapy: Integrating AI ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525014192]
- 28. Benchmarking GNINA and AutoDock Vina for Precision ... [https://pubmed.ncbi.nlm.nih.gov/40871514/]
- 29. Benchmarking Active Learning Virtual Screening across ... [https://chemrxiv.org/engage/chemrxiv/article-details/691a1736a10c9f5ca1edf1f1]
- 30. Combining Ligand- and Structure-Based Methods for More ... [https://www.genengnews.com/topics/drug-discovery/combining-ligand-and-structure-based-methods-for-more-effective-virtual-screening/]
- 31. Ligand-based pharmacophore modeling and QSAR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9996041/]
- 32. A breast cancer-specific combinational QSAR model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10822965/]
- 33. Drug Design by Pharmacophore and Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145410/]
- 34. 3D-QSAR-Based Pharmacophore Modeling, Virtual ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2022.909111/full]
- 35. 3D QSAR Studies, Pharmacophore Modeling and Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4264204/]
- 36. Structure based pharmacophore modeling, virtual ... [https://www.nature.com/articles/s41598-021-83626-x]
- 37. QSAR-based virtual screening, molecular docking, ADMET ... [https://link.springer.com/article/10.1007/s40203-024-00266-5]
- 38. Exploring AI Approaches for Breast Cancer Detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553387/]
- 39. AI-Based Characterization of Breast Cancer in Mammography ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564584/]
- 40. Artificial Intelligence-Driven Personalization in Breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428423/]
- 41. Development and validation of an artificial intelligence system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547159/]
- 42. Predicting molecular subtype in breast cancer using deep ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1638212/full]
- 43. Nationwide real-world implementation of AI for cancer ... [https://www.nature.com/articles/s41591-024-03408-6]
- 44. AI and the future of biomarker analysis in early R&D [https://www.drugtargetreview.com/article/190428/ai-and-the-future-of-biomarker-analysis-in-early-rd/]
- 45. Molecular Subtypes and Survival Patterns in Female ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566443/]
- 46. Cancer Stat Facts: Female Breast Cancer Subtypes - SEER [https://seer.cancer.gov/statfacts/html/breast-subtypes.html]
- 47. Key breast cancer highlights from the 2025 American Society ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12314680/]
- 48. New ADC Data Underscore Progress and Highlight ... [https://www.onclive.com/view/new-adc-data-underscore-progress-and-highlight-challenges-in-her2-breast-cancer-and-tnbc-management]
- 49. Clinical and molecular characteristics of HER2-low triple ... [https://www.sciencedirect.com/science/article/pii/S0960977625006010]
- 50. Patterns and prognostic implications of distant metastasis ... [https://www.nature.com/articles/s41598-025-12883-x]
- 51. Molecule subtypes play important roles for second primary ... [https://www.nature.com/articles/s41598-025-96716-x]
- 52. Classification of breast cancer molecular subtypes based on ... [https://gs.amegroups.org/article/view/143672/html]
- 53. A Multimodal Deep Learning Model for the Classification of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025686/]
- 54. Breast Cancer Molecular Subtype Prediction [https://pmc.ncbi.nlm.nih.gov/articles/PMC11201998/]
- 55. Predicting breast cancer types on and beyond molecular ... [https://www.nature.com/articles/s41523-023-00517-2]
- 56. Ultra-large library screening with an evolutionary algorithm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12594993/]
- 57. Rapid traversal of vast chemical space using machine ... [https://www.nature.com/articles/s43588-025-00777-x]
- 58. Adaptive multi-omics integration framework for breast ... [https://www.nature.com/articles/s41598-025-22202-z]
- 59. Microengineered Breast Cancer Models: Shaping the Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523347/]
- 60. An artificial intelligence accelerated virtual screening ... [https://www.nature.com/articles/s41467-024-52061-7]
- 61. Machine Learning-based Virtual Screening and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6327115/]
- 62. Explainable Artificial Intelligence for Multi-Modal Cancer ... [https://www.sciencedirect.com/science/article/pii/S1040842825004287]
- 63. Preventing Training Data Leakage in AI Systems | Blog [https://www.tonic.ai/blog/prevent-training-data-leakage-ai]
- 64. What is Data Leakage in Machine Learning? [https://www.ibm.com/think/topics/data-leakage-machine-learning]
- 65. Data Leakage Prevention in AI [https://blog.qualys.com/product-tech/2025/04/18/data-leakage-prevention-in-ai]
- 66. National Performance Benchmarks for Modern Screening Digital Mammography: Update from the Breast Cancer Surveillance Consortium - PubMed [https://pubmed.ncbi.nlm.nih.gov/27918707/]
- 67. Improved Breast Cancer Detection with Artificial ... [https://www.sciencedirect.com/science/article/abs/pii/S152682092500120X]
- 68. Performance of Algorithms Submitted in the 2023 RSNA Screening Mammography Breast Cancer Detection AI Challenge - PubMed [https://pubmed.ncbi.nlm.nih.gov/40793948/]
- 69. New mammography screening performance metrics based on the entire screening episode - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7319901/]
- 70. A systematic literature review on mammography: deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542462/]
- 71. A simple and fast explainable artificial intelligence-based ... [https://www.nature.com/articles/s41598-025-16842-4]
- 72. DUD-E: A Database of Useful (Docking) Decoys — Enhanced [https://dude.docking.org/]
- 73. Directory of Useful Decoys, Enhanced (DUD-E) [https://pmc.ncbi.nlm.nih.gov/articles/PMC3405771/]
- 74. An Improved Metric and Benchmark for Assessing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10980085/]
- 75. An Improved Metric and Benchmark for Assessing the ... [https://arxiv.org/html/2403.10478v1]
- 76. Structure-based virtual screening and molecular docking for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5476443/]
- 77. 昆明医科大学陈策实团队从肿瘤起源角度揭示乳腺癌异质性 [https://www.kmmc.cn/Pages_1284_51510.aspx]
- 78. Comparative Data Analysis of Virtual Screening ... [https://pubmed.ncbi.nlm.nih.gov/41179155/]
- 79. ESMO 2025 Breast Cancer Data May Redefine Treatment ... [https://www.onclive.com/view/esmo-2025-breast-cancer-data-may-redefine-treatment-standards-across-patient-subgroups]
- 80. Key breast cancer highlights from the 2025 American Society ... [https://tbcr.amegroups.org/article/view/103086/html]
- 81. CRISPR-cas9 Screening Identified Lethal Genes Enriched ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.646774/full]
- 82. Classifying breast cancer subtypes on multi-omics data via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10967155/]
- 83. Artificial intelligence in virtual screening: Models versus ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622002033]
- 84. An artificial intelligence accelerated virtual screening platform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11377542/]
- 85. One size does not fit all: revising traditional paradigms for ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-00948-y]
- 86. Benchmarking the Structure-Based Virtual Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12363558/]
- 87. Re-evaluating experimental validation in the Big Data Era [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02292-4]
- 88. Machine learning-based classification of histological ... [https://www.nature.com/articles/s41598-025-23498-7]