Advanced Real-Time PCR Protocols for Circulating Tumor DNA: From Foundational Principles to Clinical Applications in Precision Oncology
This comprehensive review details the pivotal role of real-time PCR technologies, particularly digital PCR (dPCR) and droplet digital PCR (ddPCR), in the analysis of circulating tumor DNA (ctDNA) for cancer...
Advanced Real-Time PCR Protocols for Circulating Tumor DNA: From Foundational Principles to Clinical Applications in Precision Oncology
Abstract
This comprehensive review details the pivotal role of real-time PCR technologies, particularly digital PCR (dPCR) and droplet digital PCR (ddPCR), in the analysis of circulating tumor DNA (ctDNA) for cancer research and drug development. It covers foundational principles of ctDNA biology, advanced methodological protocols for ultra-sensitive detection, and strategies for troubleshooting pre-analytical and analytical challenges. The article provides a critical comparison with next-generation sequencing (NGS) and validates ctDNA as a biomarker for treatment monitoring, minimal residual disease (MRD) detection, and early therapeutic response assessment in clinical trials. Aimed at researchers, scientists, and drug development professionals, this resource offers practical insights for implementing robust, reproducible ctDNA PCR assays that meet the evolving demands of precision oncology.
Understanding ctDNA Biology and the Central Role of Real-Time PCR in Liquid Biopsy
Circulating tumor DNA (ctDNA) refers to the fraction of cell-free DNA (cfDNA) in the bloodstream that originates from tumor cells. As a minimally invasive biomarker, ctDNA carries tumor-specific genetic and epigenetic alterations that reflect the entire tumor genome, enabling real-time monitoring of cancer dynamics [1] [2]. The analysis of ctDNA has emerged as a cornerstone of liquid biopsy, providing critical insights for precision oncology through applications in treatment selection, response monitoring, and detection of minimal residual disease (MRD) [1] [3]. Understanding the biological foundations of ctDNA—including its release mechanisms, structural characteristics, and clearance dynamics—is essential for developing robust real-time PCR protocols and other detection methodologies that accurately capture tumor burden and evolution.
Biological Mechanisms of ctDNA Release
Tumor cells release DNA fragments into the circulation through multiple distinct pathways, which can be broadly categorized into passive release (through cell death) and active secretion. The specific mechanism of release significantly influences the structural properties of the resulting ctDNA, including its fragment size and integrity [4] [2] [5].
Passive Release Mechanisms
Apoptosis: Programmed cell death serves as a primary source of ctDNA, particularly through the caspase-dependent cleavage of DNA [4] [2]. During apoptosis, caspase-activated DNase (CAD) and other nucleases systematically cleave DNA at internucleosomal regions, resulting in DNA fragments that are wrapped around nucleosomal structures [4]. This process generates characteristic short DNA fragments of approximately 167 base pairs (bp), which correspond to the length of DNA protected by a single nucleosome core (147 bp) plus linker DNA [4] [2]. These fragments are typically packaged into apoptotic bodies and subsequently cleared by phagocytosis before being released into circulation as soluble debris [4].
Necrosis: In contrast to apoptosis, necrosis represents an unprogrammed form of cell death resulting from pathological conditions such as hypoxia, nutrient deprivation, or therapeutic injury [4] [2]. This process involves uncontrolled release of cellular contents due to plasma membrane rupture, leading to the liberation of larger, more heterogeneous DNA fragments that can extend to many kilobase pairs [4] [2]. However, these large fragments are often subjected to further degradation by circulating nucleases and phagocytic activity, resulting in a mixture of fragment sizes in circulation [4] [2].
Active Secretion Mechanisms
Beyond cell death pathways, viable tumor cells can actively release DNA through extracellular vesicles (EVs) [2]. This secretion represents a regulated communication mechanism rather than a consequence of cellular demise. Different EV subtypes contribute variably to this process:
- Exosomes (30-150 nm diameter) and microvesicles (100-1000 nm diameter) can carry tumor-derived DNA [2].
- Studies have identified DNA within EVs isolated from cancer patients, including fragments containing mutations in key oncogenes such as KRAS and TP53 [2].
- The DNA associated with larger vesicles (e.g., microvesicles, apoptotic bodies) appears enriched with smaller fragments (<200 bp), while nanoscale EVs may offer superior mutation detection capabilities in some early-stage cancers [2].
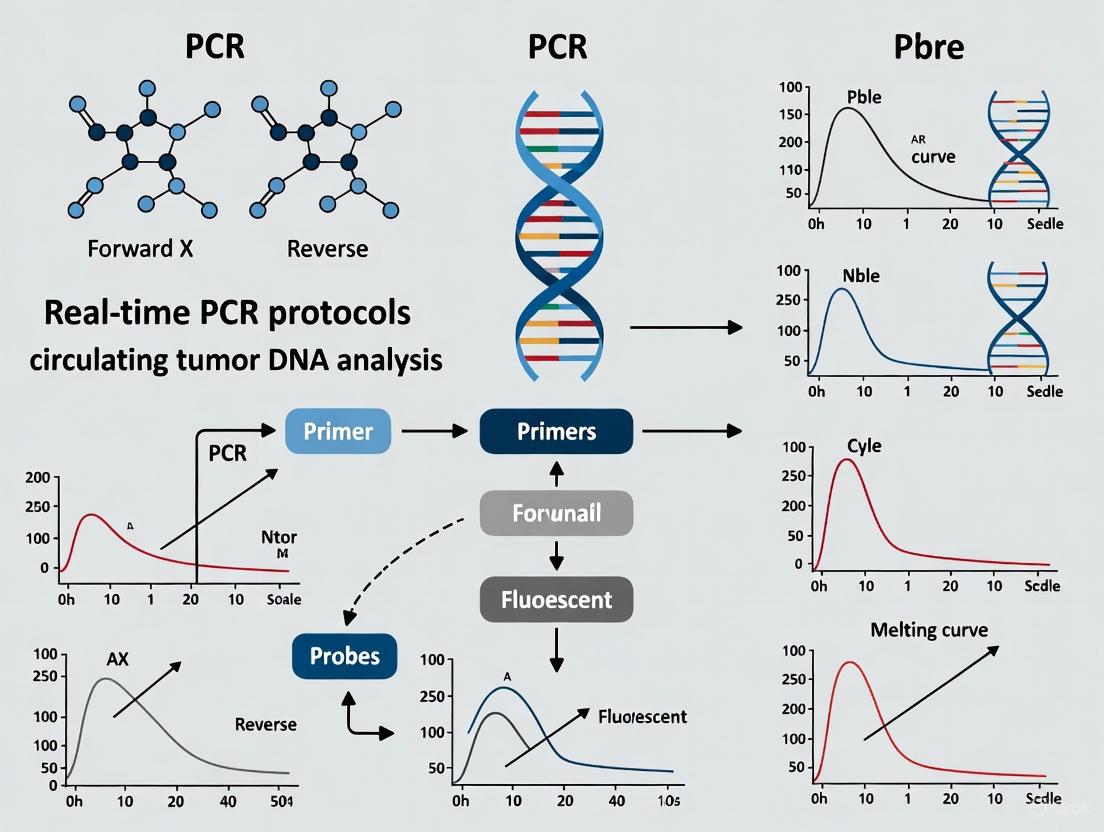
The following diagram illustrates the primary mechanisms of ctDNA release and their characteristic fragment profiles:
Figure 1: ctDNA Release Mechanisms and Resulting Fragment Characteristics. Tumor cells release DNA through passive mechanisms (apoptosis and necrosis) and active secretion via extracellular vesicles, each generating distinct fragment size profiles.
Characteristics and Properties of ctDNA
The mechanism of release directly influences the physical and molecular properties of ctDNA, which has important implications for detection methodology selection and assay design.
Table 1: Key Characteristics of ctDNA by Release Mechanism
| Release Mechanism | Primary Fragment Sizes | DNA Integrity | Distinguishing Features | Contribution to Total ctDNA Pool |
|---|---|---|---|---|
| Apoptosis | ~167 bp (mononucleosomal) with ladder-like pattern | Low integrity; systematic fragmentation | Nucleosome-protected ends; enriched in tumor-derived alterations | Major contributor |
| Necrosis | >200 bp to many kilobases; heterogeneous | Higher integrity; random fragmentation | Longer fragments; may reflect advanced disease or treatment effect | Variable; increased in aggressive tumors |
| Active Secretion | Variable; associated with vesicle size | Protected within lipid bilayers | Mutation-containing DNA in exosomes and microvesicles | Less characterized; potentially significant |
Beyond fragment size, ctDNA possesses several distinguishing biological features:
- Nucleosome Footprints: ctDNA fragments often retain nucleosomal patterning, which protects them from nuclease digestion and informs tissue of origin [4] [2].
- Preferred End Motifs: The cleavage of ctDNA is a non-random process, with certain genomic locations serving as preferential ends [2]. Cancer patients demonstrate greater end motif diversity, which can potentially enhance diagnostic performance [2].
- Fragmentation Patterns: ctDNA exhibits a higher fragmentation pattern compared to non-tumor cfDNA, with shorter fragments (<100 bp) potentially enriched for tumor-derived genomic alterations [2].
Experimental Approaches for ctDNA Analysis
The analysis of ctDNA requires highly sensitive methodologies capable of detecting rare mutant molecules against a background of wild-type DNA, with concentrations that can be below 0.1% of total cfDNA in early-stage disease or MRD settings [3].
Detection Technologies
PCR-based methods, including quantitative PCR (qPCR) and digital PCR (dPCR), offer sensitive detection of known mutations with rapid turnaround times [1] [6]. These techniques are particularly valuable for tracking specific mutations identified through prior tumor tissue testing (tumor-informed approach) [1] [6]. Digital PCR platforms partition samples into thousands of individual reactions, enabling absolute quantification of mutant alleles without the need for standard curves [1].
Next-generation sequencing (NGS) provides a more comprehensive approach for ctDNA analysis, enabling the assessment of multiple genomic alterations simultaneously [1] [3]. Both targeted panels and whole-exome/whole-genome sequencing approaches have been developed, with error-correction methods such as unique molecular identifiers (UMIs) essential for distinguishing true low-frequency variants from sequencing artifacts [1]. Recent technological advances include:
- Structural variant (SV)-based assays that identify tumor-specific rearrangements with high specificity [3].
- Phased variant approaches that target multiple single-nucleotide variants on the same DNA fragment to improve sensitivity [3].
- Fragmentomic analyses that leverage size selection and fragmentation patterns to enrich ctDNA fraction [3].
Pre-analytical Considerations
The reliability of ctDNA analysis depends heavily on appropriate sample collection, processing, and storage:
- Blood Collection: Plasma is preferred over serum for ctDNA analysis due to reduced background DNA from clotting [6].
- Sample Processing: Rapid separation of plasma from blood cells (within 2-6 hours of collection) prevents dilution of ctDNA by genomic DNA from lysed leukocytes [6].
- DNA Extraction: Methods optimized for short-fragment recovery improve ctDNA yield [6] [3].
- Fragment Size Selection: Enrichment of shorter DNA fragments (90-150 bp) can significantly increase the mutant allele fraction by excluding longer wild-type DNA [3].
The following workflow diagram outlines key steps in ctDNA analysis from sample collection to detection:
Figure 2: ctDNA Analysis Workflow. The process from sample collection to data analysis, highlighting critical steps that impact assay performance.
The Scientist's Toolkit: Essential Reagents and Materials
Successful ctDNA research requires carefully selected reagents and methodologies optimized for working with low-abundance, fragmented DNA.
Table 2: Essential Research Reagents and Materials for ctDNA Analysis
| Reagent/Material | Function/Purpose | Technical Considerations |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes | Stabilizes nucleated blood cells to prevent genomic DNA contamination | Critical for extended transport or storage; maintains sample integrity |
| Nucleic Acid Extraction Kits | Isolation of cfDNA from plasma | Select kits optimized for short-fragment recovery; silica membrane or magnetic bead-based |
| DNA Quantification Assays | Measure cfDNA concentration and quality | Fluorometric methods (e.g., Qubit) preferred over UV spectrophotometry |
| PCR Reagents | Amplification of target sequences | Use of high-fidelity polymerases with low error rates essential |
| Digital PCR Master Mixes | Partitioned amplification for absolute quantification | Enables detection down to 0.001% VAF; requires specialized instrumentation |
| NGS Library Prep Kits | Preparation of sequencing libraries | Incorporation of UMIs critical for error correction; size selection enhances sensitivity |
| Targeted Capture Panels | Enrichment of cancer-relevant genes | Commercially available or custom-designed; should cover relevant mutational hotspots |
| Bioinformatic Tools | Variant calling and interpretation | Error-suppression algorithms; fragmentomic analysis capabilities |
Clinical Applications and Research Implications
The biological characteristics of ctDNA directly inform its clinical applications in oncology. The short half-life of ctDNA (estimated between 16 minutes to several hours) enables real-time monitoring of tumor dynamics and treatment response [1]. Key applications include:
Treatment Response Monitoring: Changes in ctDNA levels often precede radiographic evidence of response or progression [1] [3] [7]. Molecular response assessments using ctDNA have demonstrated utility across multiple cancer types, with clearance of ctDNA after treatment initiation correlating with improved outcomes [7]. Quantitative metrics such as variant allele frequency (VAF) dynamics provide sensitive measures of therapeutic efficacy [7].
Minimal Residual Disease Detection: The high sensitivity of modern ctDNA assays enables identification of MRD following curative-intent treatment [1] [6] [3]. Tumor-informed approaches that track patient-specific mutations achieve the highest sensitivity for MRD detection, with ctDNA positivity post-treatment strongly predicting future recurrence [6] [3].
Therapy Selection and Resistance Monitoring: ctDNA profiling can identify targetable mutations and emerging resistance mechanisms without the need for repeated tissue biopsies [1] [3]. For example, in EGFR-mutant non-small cell lung cancer, ctDNA monitoring enables detection of T790M resistance mutations that guide subsequent therapy selection [3].
Understanding the origins and characteristics of ctDNA through apoptosis, necrosis, and active release mechanisms provides the fundamental biological context necessary for developing and optimizing real-time PCR protocols and other detection methodologies. This knowledge enables researchers to select appropriate pre-analytical methods, design assays with optimal sensitivity and specificity, and accurately interpret experimental results in the context of cancer biology and clinical management.
The analysis of circulating tumor DNA (ctDNA) has emerged as a transformative paradigm in precision oncology, enabling real-time, noninvasive assessment of tumor burden, genetic heterogeneity, and therapeutic response [3]. As a subset of cell-free DNA (cfDNA) derived from tumor tissue, ctDNA carries tumor-specific genetic alterations that provide a molecular snapshot of the cancer's dynamic genomic landscape [8]. However, the reliable detection of ctDNA faces three fundamental analytical challenges that constrain its clinical utility, particularly in early-stage disease and minimal residual disease (MRD) monitoring [3] [9].
The first challenge, low abundance, stems from the fact that ctDNA often constitutes less than 0.1% of the total circulating cell-free DNA, creating a significant detection hurdle that demands exceptional analytical sensitivity [3]. In early-stage tumors, the concentration can be vanishingly low—sometimes fewer than 1-100 copies per milliliter of plasma—posing substantial technical challenges for detection systems [9]. The second challenge, short half-life, reflects the rapid clearance of ctDNA from circulation, with estimates ranging from 16 minutes to several hours [1]. This transient presence necessitates careful timing of sample collection and rapid processing to avoid pre-analytical degradation. The third challenge, background wild-type DNA, represents the overwhelming majority of cfDNA derived from non-tumor sources, primarily hematopoietic cells undergoing physiological apoptosis [9] [1]. This background creates a signal-to-noise problem where rare mutant ctDNA fragments must be distinguished from a vast excess of wild-type DNA, requiring exceptional specificity in detection methods.
These interconnected challenges are particularly pronounced in clinical scenarios where ctDNA detection would be most impactful: early cancer detection, assessment of MRD following curative-intent therapy, and early identification of molecular recurrence [3]. This technical guide examines these analytical barriers within the context of real-time PCR protocols and emerging solutions, providing a framework for optimizing ctDNA research in oncology applications.
Technical Analysis of Core Challenges
Challenge 1: Low Abundance of ctDNA
The low fractional abundance of ctDNA represents perhaps the most significant technical hurdle in liquid biopsy applications. Tumor-derived DNA typically constitutes only 0.025-2.5% of total circulating cell-free DNA, with this proportion influenced by tumor biology, disease burden, and treatment-related factors [9]. In practical terms, this means that detection methods must identify a handful of mutant DNA molecules among tens of thousands of wild-type fragments, pushing analytical systems to their limits of detection [3].
The biological basis for low ctDNA abundance is multifactorial. In early-stage tumors, only a tiny fraction of cells undergo apoptosis and shed DNA into circulation [9]. Additionally, ctDNA release is influenced by factors such as tumor vascularity, with ctDNA being more frequently detected in tumors with vascular invasion [9]. The relationship between tumor burden and ctDNA levels is not linear, creating particular difficulties in detecting minimal residual disease where tumor mass may be below current detection thresholds [9].
Table 1: Factors Influencing ctDNA Abundance
| Factor Category | Specific Factors | Impact on ctDNA Levels |
|---|---|---|
| Tumor-Related Factors | Tumor stage and size | Higher stages and larger tumors correlate with increased ctDNA |
| Tumor vascularity | Vascular invasion increases ctDNA release | |
| Tumor location | Anatomical site influences shedding rates | |
| Cellular turnover rate | Higher apoptosis rates increase ctDNA | |
| Patient-Related Factors | Body mass index | Affects background cfDNA levels |
| Renal function | Impacts clearance of cfDNA | |
| Inflammatory conditions | Increase background wild-type cfDNA | |
| Circadian rhythms | ctDNA levels may fluctuate diurnally | |
| Treatment-Related Factors | Radiotherapy | Can transiently increase ctDNA release |
| Chemotherapy | May initially increase then decrease ctDNA | |
| Surgical resection | Rapidly decreases ctDNA post-procedure |
Challenge 2: Short Half-Life of ctDNA
The transient nature of ctDNA in circulation presents significant challenges for sample timing, collection, and processing. Current evidence suggests a half-life ranging from 16 minutes to several hours, significantly shorter than many protein biomarkers traditionally used in oncology [1]. This rapid turnover means that ctDNA levels provide a near real-time snapshot of tumor dynamics but also necessitates careful protocol standardization to avoid pre-analytical degradation.
The clearance mechanisms for ctDNA involve both enzymatic degradation by circulating nucleases and phagocytic uptake by liver macrophages [9]. This rapid elimination contributes to the dynamic range of ctDNA measurements, enabling rapid assessment of treatment response, but also creates vulnerabilities in the pre-analytical phase where delays in processing can profoundly impact results.
Experimental approaches to modulate ctDNA half-life have shown promise in animal models, where interfering with liver macrophages and circulating nucleases can slow physiological ctDNA decay [9]. However, these interventions remain primarily in the research domain and are not yet applicable to clinical practice.
Challenge 3: Background Wild-Type DNA Interference
The presence of abundant wild-type DNA constitutes a significant source of background noise in ctDNA analysis. In healthy individuals and cancer patients alike, the majority of cfDNA originates from hematopoietic cells through physiological apoptosis [1]. This wild-type DNA creates a dilution effect where mutant alleles are present at very low variant allele frequencies (VAF), often below 0.1% in early-stage cancers and MRD settings [3].
The wild-type background not only dilutes the signal but can also introduce analytical artifacts during amplification. In PCR-based methods, the amplification of wild-type sequences can preferentially consume reagents, potentially limiting the amplification of rare mutant templates. Additionally, errors introduced during early amplification cycles can be perpetuated and mistaken for true variants, creating false positives unless robust error-correction methods are implemented.
Table 2: Sources and Characteristics of Background Wild-Type DNA
| Source of Wild-Type DNA | Contribution to Total cfDNA | Factors Increasing Contribution |
|---|---|---|
| Hematopoietic Cells | Primary source (≥90% in many cases) | Hemolysis during blood draw, extended tourniquet use |
| Other Normal Tissues | Variable based on physiological state | Physical exercise, tissue trauma, inflammation |
| Clonal Hematopoiesis | Variable (increases with age) | Advanced age, smoking history |
| Post-Surgical Release | Transiently increased | Recent surgical procedures, tissue injury |
Advanced Methodologies and Experimental Protocols
Ultrasensitive Detection Technologies
Structural Variant-Based ctDNA Assays
Next-generation sequencing assays that focus on somatic structural variants (SVs) rather than single nucleotide variants (SNVs) can mitigate many challenges associated with low VAF detection [3]. SV-based assays identify tumor-specific chromosomal rearrangements with breakpoint sequences unique to the tumor, effectively eliminating concerns about sequencing artifacts affecting SNV calls [3]. These assays can employ multiplexed PCR panels or hybrid-capture probes personalized to individual breakpoints, achieving parts-per-million sensitivity with tumor specificity, as normal cells lack these rearrangement combinations [3].
Experimental Protocol: SV-Based ctDNA Detection
- Tumor Whole Genome Sequencing: Perform 30-60x WGS on tumor tissue and matched normal DNA to identify tumor-specific structural variants.
- Breakpoint Prioritization: Select 10-20 rearrangements with balanced allele frequencies in tumor tissue.
- Probe Design: Design hybrid-capture probes or PCR primers spanning breakpoint junctions.
- Library Preparation: Extract cfDNA from patient plasma and create sequencing libraries with unique molecular identifiers (UMIs).
- Target Enrichment: Enrich for target regions using custom probes.
- Deep Sequencing: Sequence to high coverage (≥10,000x) to detect rare ctDNA molecules.
- Bioinformatic Analysis: Map reads to reference genome, identify chimeric reads spanning breakpoints, and quantify tumor-specific molecules using UMI groups.
In early-stage breast cancer, this approach detected ctDNA in 96% (91/95) of participants at baseline with a median VAF of 0.15% (range: 0.0011%-38.7%), with 10% of cases having VAF <0.01% [3].
Nanomaterial-Enhanced Electrochemical Sensors
Bioelectronic sensors utilize the high surface area and conductive properties of nanomaterials to transduce DNA-binding events into recordable electrical signals, achieving attomolar sensitivity [3]. Magnetic nanoparticles coated with gold and conjugated with complementary DNA probes can capture and enrich target ctDNA fragments in proximity to electrode surfaces, enabling detection within 20 minutes [3]. Graphene or molybdenum disulfide (MoS₂) facilitates label-free sensing methods where ctDNA hybridization is detected through impedance changes or current-voltage characteristics [3].
Experimental Protocol: Magnetic Nano-Electrode System
- Nanoparticle Preparation: Synthesize superparamagnetic Fe₃O₄–Au core–shell particles (10-15 nm diameter).
- Probe Conjugation: Covalently link thiol-modified DNA capture probes to gold surfaces.
- Sample Incubation: Mix nanoparticle probes with plasma cfDNA for 15 minutes with agitation.
- Magnetic Separation: Concentrate nanoparticle-cfDNA complexes using magnetic fields.
- Electrochemical Readout: Transfer complexes to electrode surface and measure current-voltage characteristics.
- Signal Amplification: Apply enzymatic or nanomaterial-based signal amplification if needed.
This approach can achieve detection limits of three attomolar with a signal-to-noise ratio within 7 minutes of PCR amplification [3].
Pre-Analytical Optimization Strategies
Blood Collection and Processing Protocols
Standardized blood collection and processing are critical for reliable ctDNA analysis. Conventional EDTA tubes require processing within 2-6 hours at 4°C to prevent leukocyte lysis and release of genomic DNA [9]. Commercial blood collection tubes containing cell-stabilizing preservatives (e.g., Streck cfDNA, PAXgene Blood ccfDNA) allow for storage and transportation for up to 7 days at room temperature by preventing leukocyte degradation [9].
Experimental Protocol: Optimal Blood Collection and Processing
- Blood Draw: Collect 20-30 mL blood using butterfly needles, avoiding excessively thin needles and prolonged tourniquet use.
- Tube Selection: Use cfDNA-stabilizing tubes for studies requiring shipment or delayed processing.
- Centrifugation: Perform two-step centrifugation:
- First step: 380-3,000 × g for 10 minutes at room temperature
- Second step: 12,000-20,000 × g for 10 minutes at 4°C
- Plasma Storage: Aliquot plasma and store at -80°C (stable for 10 years for mutation detection; 9 months for quantitative analysis).
- DNA Extraction: Use silica membrane-based kits (e.g., QIAamp Circulating Nucleic Acid Kit) for higher yields compared to magnetic bead methods.
Fragment Size Selection
Tumor-derived cfDNA typically fragments to lengths of 90-150 base pairs, while non-tumor cfDNA tends to be longer [3]. Utilizing bead-based or enzymatic size selection to enrich for shorter fragments can increase the fractional abundance of ctDNA in sequencing libraries by several folds [3]. This approach enhances the detection yield of low-frequency variants and can reduce the required sequencing depth for MRD detection, improving cost-effectiveness [3].
Bioinformatic Enhancement Strategies
Error suppression through bioinformatic methods is essential for distinguishing true low-frequency variants from technical artifacts. Unique molecular identifiers (UMIs) tagged onto DNA fragments before PCR amplification enable consensus sequencing to filter out errors introduced during amplification [1]. Advanced methods like Duplex Sequencing tag and sequence both strands of DNA duplexes, allowing true mutations to be identified when present in the same position on both strands [1]. Recent innovations such as CODEC (Concatenating Original Duplex for Error Correction) achieve 1000-fold higher accuracy than conventional NGS while using up to 100-fold fewer reads than duplex sequencing [1].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for ctDNA Research
| Reagent Category | Specific Examples | Primary Function | Technical Notes |
|---|---|---|---|
| Blood Collection Tubes | Streck cfDNA BCT, PAXgene Blood ccfDNA Tube | Cellular stabilization during transport | Enable room temperature storage for ≤7 days |
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit, Cobas ccfDNA Sample Preparation Kit | Isolation of high-quality cfDNA | Silica-membrane methods yield more ctDNA than magnetic beads |
| Library Preparation | KAPA HyperPrep, ThruPLEX Plasma-Seq | Sequencing library construction | Incorporate UMIs for error correction |
| Target Enrichment | IDT xGen Lockdown Probes, Twist Custom Panels | Hybrid-capture-based target enrichment | Enable focused sequencing on relevant regions |
| qPCR/dPCR Master Mixes | ddPCR Supermix, TaqMan Advanced miRNA cDNA | Absolute quantification of mutant alleles | Digital PCR provides single-molecule sensitivity |
| Size Selection Beads | AMPure XP, Circulomics SRE | Enrichment of short cfDNA fragments | Improve tumor fraction by selecting 90-150 bp fragments |
The analytical challenges of low abundance, short half-life, and background wild-type DNA in ctDNA analysis continue to drive innovation in detection technologies and methodological approaches. Emerging strategies include stimulation of ctDNA release through external means such as localized irradiation or ultrasound, which can transiently increase ctDNA concentration 6-24 hours post-procedure [9]. Additionally, interference with physiological clearance mechanisms to prolong ctDNA half-life shows promise in animal models, though clinical applications remain exploratory [9].
The future of ctDNA analysis will likely involve multimodal approaches that combine mutation detection with complementary analytes such as methylation patterns and fragmentomics. Tumor-agnostic hypermethylated gene promoter panels can detect and quantify tumor development in patients with early-stage cancer by analyzing epigenetic modifications in cfDNA [3]. The combination of mutations and methylation signatures in cfDNA may form the foundation for future pan-cancer screening initiatives [3].
For the research community, addressing the current challenges requires continued focus on pre-analytical standardization, analytical validation, and bioinformatic sophistication. As these technical hurdles are overcome, ctDNA analysis promises to become an increasingly powerful tool for precision oncology, enabling earlier detection, more sensitive monitoring of treatment response, and improved management of cancer patients across the disease spectrum.
Diagrams above illustrate the integrated workflow for ctDNA analysis (top) and the relationship between key challenges and technological solutions (bottom).
Digital PCR (dPCR) represents a paradigm shift in nucleic acid quantification, moving beyond the relative measurements of quantitative real-time PCR (qPCR) to provide absolute quantification with single-molecule sensitivity. This transformative technology partitions a sample into thousands of individual reactions, enabling precise enumeration of target molecules through binary endpoint detection and Poisson statistics. Within circulating tumor DNA (ctDNA) research, dPCR's exceptional sensitivity for detecting rare mutations in a background of wild-type DNA has revolutionized liquid biopsy applications, including minimal residual disease monitoring, treatment response assessment, and resistance mutation tracking. This technical guide explores the fundamental principles, methodological frameworks, and cutting-edge applications of dPCR that are advancing precision oncology.
The polymerase chain reaction (PCR), invented by Kary Mullis in 1983, revolutionized molecular biology by enabling exponential amplification of specific DNA sequences [10]. Quantitative real-time PCR (qPCR) advanced this technology by allowing researchers to monitor amplification throughout the reaction cycle using fluorescent probes, establishing itself as the gold standard for nucleic acid quantification [11]. However, qPCR possesses significant limitations: it requires standard curves for quantification, lacks sensitivity for detecting very rare mutations, and is susceptible to amplification efficiency variations between samples [12] [11].
Digital PCR emerged to address these limitations, with the fundamental concept first described in 1988 and the term "digital PCR" formally introduced in 1999 [12]. The technology leverages sample partitioning, endpoint fluorescence detection, and Poisson statistics to achieve absolute quantification without standard curves [10] [12]. This approach has proven particularly valuable in ctDNA research, where detecting rare tumor-derived mutations in circulation requires exceptional sensitivity to identify mutant allele frequencies often below 0.1% amid abundant wild-type DNA [1] [3].
Fundamental Principles of Digital PCR
Core Technological Framework
The fundamental innovation of dPCR lies in its partitioning strategy. A standard PCR reaction mixture containing template DNA, primers, probes, nucleotides, and enzymes is divided into thousands to millions of individual microreactions [12]. These partitions can be created through various physical means including microfluidic chambers, droplet emulsions, or nanoplates [10] [12]. Each partition acts as an independent PCR microreactor where amplification occurs in isolation from other partitions.
Following thermal cycling, each partition is analyzed for fluorescence. Partitions containing the target sequence emit fluorescence (recorded as "1"), while those without the target remain dark (recorded as "0") [12]. This binary detection system gives the technology its "digital" name, analogous to digital computing's binary code [12]. The ratio of positive to total partitions enables absolute quantification of the target nucleic acid through statistical analysis.
Statistical Foundation: Poisson Distribution and Quantification Accuracy
The random distribution of DNA molecules across partitions follows Poisson statistics, which forms the mathematical foundation for dPCR quantification [10] [11]. According to Poisson distribution, the probability of a partition containing k target molecules is given by:
P(k) = (λ^k · e^(-λ)) / k!
Where λ represents the average number of target molecules per partition [11]. For dPCR analysis, the most critical case is k=0 (the fraction of empty partitions), leading to the simplified equation:
λ = -ln(1 - p)
Where p is the proportion of positive partitions [11]. This relationship allows calculation of the absolute target concentration without reference to standards.
The accuracy of dPCR quantification depends heavily on the number of partitions analyzed and their occupancy rate. Precision is optimal when approximately 20% of partitions are positive (λ = 1.6), with accuracy improving as the total number of partitions increases [11]. This statistical framework defines both the dynamic range and detection limits of dPCR systems, with higher partition counts enabling more sensitive detection of rare targets—a critical advantage for ctDNA analysis where mutant allele frequencies can be extremely low [10] [12].
Comparative Analysis: dPCR vs. qPCR
digital PCR vs. Quantitative PCR: Key Technical Differences
| Parameter | Digital PCR (dPCR) | Quantitative PCR (qPCR) |
|---|---|---|
| Quantification Method | Absolute quantification via Poisson statistics | Relative quantification requiring standard curve |
| Detection Principle | End-point fluorescence detection | Real-time fluorescence monitoring during exponential phase |
| Sensitivity | Higher sensitivity for rare alleles (<0.1% VAF) | Limited sensitivity for rare mutations (typically >1% VAF) |
| Precision | Superior precision due to partitioning and binary detection | Moderate precision influenced by amplification efficiency |
| Tolerance to Inhibitors | Higher tolerance due to sample partitioning | More susceptible to PCR inhibitors |
| Dynamic Range | Limited by number of partitions | Broader dynamic range |
| Throughput | Moderate to high | High |
| Cost Considerations | Higher per sample, but becoming more competitive | Established, cost-effective for high-volume testing |
VAF: Variant Allele Frequency [12] [11]
dPCR Workflow and Experimental Design
Core Workflow Implementation
The dPCR process follows a standardized workflow that can be divided into three key phases: preparation, amplification, and analysis [12]. The preparation phase involves assembling the PCR reaction mix and loading it into the dPCR instrument, which then automatically partitions the sample. The partitioning mechanism varies by platform, with common approaches including droplet-based systems (creating water-in-oil emulsions), chip-based arrays (with etched microwells), and nanoplate-based technologies [10] [12].
During the amplification phase, the partitioned sample undergoes conventional PCR thermal cycling. Each partition functions as an individual reaction vessel, with target molecules amplified independently. Following amplification, the system detects fluorescence in each partition, with positive partitions indicating the presence of the target sequence [12]. The final analytical phase applies Poisson statistics to calculate the absolute concentration of the target molecule in the original sample based on the proportion of positive partitions [10] [12].
Research Reagent Solutions for ctDNA Analysis
Essential Research Reagents for dPCR-based ctDNA Analysis
| Reagent/Category | Function in dPCR Workflow | Application Notes for ctDNA |
|---|---|---|
| Blood Collection Tubes with Stabilizers (e.g., cfDNA BCT tubes) | Preserves blood sample integrity, prevents genomic DNA release from blood cells | Critical for accurate ctDNA analysis; enables room temperature transport for up to 7 days [13] |
| cfDNA Extraction Kits | Isolates cell-free DNA from plasma | Size-selection methods can enrich for ctDNA fragments (90-150 bp) over longer hematopoietic DNA [3] |
| dPCR Master Mix | Provides enzymes, nucleotides, buffers for amplification | Should include UDI technology to reduce cross-contamination; inhibitor-resistant formulations preferred [12] |
| Mutation-Specific Assays | Detects tumor-specific mutations | Tumor-informed assays (based on prior sequencing) increase sensitivity; multiplex assays enable parallel detection [1] |
| Unique Molecular Identifiers (UMIs) | Tags individual DNA molecules to distinguish true mutations from PCR errors | Essential for error correction in rare mutation detection; reduces false positives [1] |
| Microfluidic Partitioning Oil/Reagents | Creates stable emulsion for droplet-based dPCR | Partition stability critical for accurate quantification; commercial formulations provide optimal consistency [10] |
dPCR Applications in ctDNA Research
Monitoring Treatment Response and Resistance
The short half-life of ctDNA (approximately 16 minutes to several hours) makes it an ideal biomarker for real-time monitoring of treatment response [1]. dPCR enables serial assessment of mutation-specific ctDNA levels during therapy, with declining concentrations indicating positive treatment response and rising levels suggesting therapeutic resistance [1] [3]. Studies across multiple cancer types have demonstrated that ctDNA changes often precede radiographic evidence of response or progression by several weeks [3]. In EGFR-mutant non-small cell lung cancer, for example, dPCR can detect emerging T790M resistance mutations, guiding timely switches to third-generation EGFR inhibitors without repeated tissue biopsies [3].
Minimal Residual Disease (MRD) Detection
The exceptional sensitivity of dPCR enables detection of molecular residual disease following curative-intent surgery or radiation therapy [1] [14]. MRD assessment represents one of the most promising applications of dPCR in oncology, as it can identify patients at high risk of recurrence who might benefit from additional therapy, while sparing those with undetectable MRD from unnecessary treatment [14]. Clinical studies have demonstrated that ctDNA detection post-treatment predicts recurrence with high sensitivity and specificity, often providing a lead time of several months before clinical or radiographic recurrence [14]. In colorectal cancer, ctDNA-guided approaches have reduced adjuvant chemotherapy use without compromising recurrence-free survival [14].
Clinical Trial Applications and Protocol Implementation
The research applications of dPCR in ctDNA analysis are increasingly being translated into clinical trials frameworks. Ongoing studies are evaluating ctDNA-based endpoints for accelerated drug development and as potential surrogates for traditional survival endpoints [14]. The implementation of dPCR in these settings requires careful attention to pre-analytical variables, assay validation, and analytical standardization to ensure reproducible results across sites [13]. A proposed workflow for implementing dPCR in clinical research captures the comprehensive process from sample collection to clinical decision-making.
Advanced Methodologies and Future Directions
Emerging Technological Innovations
While current dPCR platforms already provide exceptional sensitivity, emerging technologies promise to further advance the field. Approaches such as Concatenating Original Duplex for Error Correction (CODEC) claim to achieve 1000-fold higher accuracy than conventional NGS while using significantly fewer reads [1]. Structural variant-based ctDNA assays that identify tumor-specific chromosomal rearrangements are achieving detection sensitivities in the parts-per-million range [3]. Nanomaterial-based electrochemical sensors using graphene or molybdenum disulfide (MoS₂) can detect ctDNA at attomolar concentrations within minutes, potentially enabling point-of-care applications [3]. Additionally, fragmentation pattern analysis that exploits the characteristic shorter length of ctDNA fragments (90-150 bp) compared to non-tumor cfDNA provides an orthogonal method for improving detection specificity [1] [3].
Addressing Current Limitations and Challenges
Despite its considerable advantages, dPCR faces several technical and implementation challenges. The dynamic range of dPCR is constrained by the number of partitions available in each system, potentially limiting its utility for samples with very high target concentrations [12]. Pre-analytical variables including blood collection methods, processing timelines, and plasma separation protocols can significantly impact ctDNA recovery and assay performance [13]. Standardization across platforms and laboratories remains challenging, with inter-institution harmonization efforts ongoing [13]. Additionally, the tumor-informed approach that provides maximum sensitivity requires prior knowledge of tumor-specific mutations, adding complexity to the testing workflow [1] [14].
Future developments will likely focus on increasing partition densities to enhance sensitivity and dynamic range, improving multiplexing capabilities to simultaneously monitor multiple mutations, and integrating artificial intelligence-based error suppression methods to further improve specificity [3]. As these technological advances mature, dPCR is poised to become an increasingly central tool in both cancer research and clinical oncology, enabling more precise monitoring of treatment response and disease dynamics through non-invasive liquid biopsy approaches.
Digital PCR represents a fundamental advancement in nucleic acid quantification, providing absolute measurement of target sequences with precision that surpasses traditional qPCR, particularly for rare mutation detection. Its unique partitioning approach, combined with Poisson statistical analysis, enables researchers to detect and quantify ctDNA at variant allele frequencies below 0.1%—a critical capability for advancing liquid biopsy applications in oncology. As technological innovations continue to enhance the sensitivity, multiplexing capacity, and accessibility of dPCR platforms, this methodology is establishing new paradigms for cancer monitoring, minimal residual disease detection, and real-time assessment of treatment response. The integration of dPCR into both research and clinical workflows promises to accelerate the development of more personalized, dynamic cancer management strategies based on the molecular signatures captured in circulating tumor DNA.
Liquid biopsy, a revolutionary technique in precision oncology, enables the analysis of tumor-derived components from bodily fluids such as blood. This approach provides a minimally invasive alternative to traditional tissue biopsies, offering dynamic insights into tumor biology through circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and other biomarkers [15] [16]. The clinical adoption of liquid biopsy has transformed cancer management by facilitating real-time monitoring, capturing tumor heterogeneity, and enabling serial sampling with minimal patient risk [17]. This technical guide explores the core advantages of liquid biopsy technologies, with particular emphasis on their application within circulating tumor DNA research frameworks, providing researchers and drug development professionals with detailed methodologies and current evidence supporting their implementation.
Core Advantages of Liquid Biopsy
Real-Time Monitoring and Dynamic Prognostication
Liquid biopsy enables real-time tracking of tumor dynamics and treatment response by detecting changes in circulating biomarker levels, offering a significant advantage over traditional imaging methods.
Superior Prognostic Value: Meta-analyses demonstrate that ctDNA detection consistently predicts poorer survival outcomes across multiple cancer types. In esophageal cancer, for example, ctDNA positivity associates with significantly reduced progression-free survival (PFS) and overall survival (OS) at various treatment timepoints, with hazard ratios increasing from baseline through follow-up monitoring [18].
Early Recurrence Detection: ctDNA testing can identify molecular recurrence months before radiological confirmation. A comprehensive analysis revealed that ctDNA detection anticipates clinical recurrence with an average lead time of 4.53 months (range: 0.98-11.6 months) compared to conventional imaging [18].
Therapy Response Monitoring: Dynamic changes in ctDNA levels closely reflect treatment effectiveness. In metastatic colorectal cancer, a ctDNA increase during systemic therapy strongly correlates with reduced PFS (HR: 2.44, 95% CI: 2.02-2.95) and OS (HR: 2.53, 95% CI: 2.01-3.18) [19]. Rapid ctDNA clearance following treatment initiation often indicates favorable response, while persistent detection may signal resistance [17].
Table 1: Prognostic Value of ctDNA at Different Monitoring Timepoints in Esophageal Cancer
| Timepoint | PFS Hazard Ratio | OS Hazard Ratio | Clinical Implications |
|---|---|---|---|
| Baseline (after diagnosis, before treatment) | HR = 1.64 (95% CI: 1.30-2.07) | HR = 2.02 (95% CI: 1.36-2.99) | Identifies high-risk patients who may benefit from treatment intensification |
| After Neoadjuvant Therapy (before surgery) | HR = 3.97 (95% CI: 2.68-5.88) | HR = 3.41 (95% CI: 2.08-5.59) | Detects minimal residual disease, guides adjuvant therapy decisions |
| During Follow-up (adjuvant therapy or surveillance) | HR = 5.42 (95% CI: 3.97-7.38) | HR = 4.93 (95% CI: 3.31-7.34) | Enables early recurrence detection, allows for preemptive intervention |
Comprehensive Capture of Tumor Heterogeneity
Tumors exhibit substantial spatial and temporal heterogeneity, which traditional biopsies often fail to capture comprehensively. Liquid biopsy addresses this limitation by sampling tumor-derived components released from all tumor sites throughout the body.
Overcoming Sampling Bias: Tissue biopsies provide information only from a specific lesion and may miss molecular alterations present in metastatic sites or different regions of the primary tumor. In contrast, liquid biopsy integrates genetic material from multiple tumor sites, offering a more complete molecular profile [16].
Tracking Clonal Evolution: Serial liquid biopsies enable monitoring of tumor evolution under therapeutic pressure, including the emergence of resistance mechanisms. This capability is crucial for understanding treatment failure and guiding subsequent therapy selection [19].
Complementary Biomarker Classes: Different liquid biopsy components provide unique insights:
- CTCs: Offer intact cellular material for functional studies and protein expression analysis [15]
- ctDNA: Provides genetic information including mutations, copy number alterations, and epigenetic modifications [15]
- Extracellular Vesicles: Contain proteins, RNA species, and other macromolecules that reflect cellular states [16]
The following workflow illustrates how liquid biopsy captures global tumor heterogeneity, unlike traditional tissue biopsy:
Non-Invasive Sampling and Clinical Applications
The minimally invasive nature of liquid biopsy facilitates repeated sampling, enabling longitudinal monitoring that is not feasible with tissue biopsies due to procedural risks and patient discomfort.
Procedural Advantages: Liquid biopsy primarily uses blood draws, which are routine outpatient procedures with minimal risk, unlike surgical biopsies which may require hospitalization and carry risks of bleeding, infection, or organ injury [15] [16].
Serial Monitoring Capability: The ability to perform frequent assessments enables dynamic treatment response evaluation and early detection of resistance mechanisms. This facilitates timely intervention before clinical deterioration [17].
Diverse Clinical Applications:
- Early Cancer Detection: Identifying tumor-specific mutations in blood samples from asymptomatic individuals [15]
- Minimal Residual Disease (MRD) Monitoring: Detecting molecular residual disease after curative-intent treatment [17] [13]
- Treatment Selection: Identifying actionable genomic alterations to guide targeted therapy [20]
- Clinical Trial Endpoints: Providing pharmacodynamic biomarkers for drug development [16]
Table 2: Clinical Impact of Liquid Biopsy in a Real-World Cohort (n=30 Patients)
| Clinical Decision Category | Case Examples | ctDNA Findings | Clinical Action |
|---|---|---|---|
| Treatment Escalation | Stage III sigmoid cancer; Stage IV pancreatic NET | ctDNA positivity after initial therapy | Initiation or intensification of systemic treatment |
| Treatment De-escalation | Metastatic urothelial carcinoma; Oligometastatic colorectal cancer | ctDNA negativity with radiological response | Reduction or discontinuation of toxic therapies |
| Early Relapse Prediction | GE junction carcinoma; Lung adenocarcinoma | ctDNA detection during surveillance | Earlier imaging confirmation and treatment modification |
| Response Monitoring | Colorectal, endometrial, breast cancers | Persistent ctDNA negativity | Continued surveillance or maintenance therapy |
Technical Considerations for ctDNA Analysis
Pre-analytical Factors and Sample Collection
The sensitivity of ctDNA detection depends critically on proper sample collection and processing, as ctDNA typically represents less than 0.025-2.5% of total circulating cell-free DNA [13].
Blood Collection Tubes: Both conventional EDTA tubes and specialized cell-free DNA preservation tubes are used. EDTA tubes require processing within 2-6 hours at 4°C, while specialized tubes (e.g., Streck cfDNA, PAXgene) allow sample stability for up to 7 days at room temperature [13].
Recommended Blood Volume: For single-analyte liquid biopsy, 2 × 10 mL of blood is typically recommended. Larger volumes may be necessary for MRD detection, whole-genome sequencing, or multi-analyte testing [13].
Pre-analytical Variables: Physical activity, circadian rhythms, and concurrent conditions (inflammation, surgery) can influence ctDNA levels. Surgical trauma transiently increases total cell-free DNA for several weeks, potentially confounding interpretation [13].
Analytical Methods and Sensitivity Enhancement
Advanced molecular techniques have dramatically improved the sensitivity of ctDNA detection, enabling applications in minimal residual disease monitoring.
Ultra-Sensitive Detection Platforms: Next-generation sequencing (NGS) and droplet digital PCR (ddPCR) are the primary technologies for ctDNA analysis. Recent assays like Northstar Select demonstrate a limit of detection of 0.15% variant allele frequency for single nucleotide variants and indels, with sensitive detection of copy number variations and gene fusions [20].
Approaches to Enhance Sensitivity:
- Physical Stimulation: Local tumor irradiation can induce transient apoptosis and increase ctDNA release 6-24 hours post-procedure [13]
- Technical Innovations: Modified ultra-deep NGS protocols discriminate true low-frequency mutations from sequencing artifacts [13]
- Biological Interventions: Slowing physiological ctDNA clearance by interfering with liver macrophages and circulating nucleases shows promise in preclinical models [13]
The following diagram illustrates the complete workflow from sample collection to clinical application in ctDNA analysis:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Liquid Biopsy Experiments
| Reagent/Material | Function | Technical Notes |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes (e.g., Streck, PAXgene) | Preserves blood sample integrity during storage and transport | Enables room temperature stability for up to 7 days; prevents genomic DNA contamination from white blood cell lysis |
| Nucleic Acid Extraction Kits | Isolation of high-quality cfDNA from plasma | Magnetic bead-based systems typically provide better yield and reproducibility than column-based methods |
| PCR/Sequencing Reagents | Amplification and detection of tumor-specific alterations | Digital PCR platforms (ddPCR) offer absolute quantification; NGS enables multiplexed analysis of multiple genomic regions |
| Reference Standard Materials | Assay validation and quality control | Commercially available synthetic cfDNA references with predetermined mutation frequencies enable assay calibration |
| Bioinformatic Analysis Pipelines | Variant calling and interpretation | Specialized algorithms (e.g., MuTect, VarScan2) distinguish low-frequency true variants from sequencing artifacts |
Liquid biopsy represents a paradigm shift in cancer management, offering distinct advantages through its non-invasive nature, capacity for real-time monitoring, and comprehensive capture of tumor heterogeneity. Technological advancements continue to enhance the sensitivity of ctDNA detection, expanding applications from early cancer detection to minimal residual disease monitoring. For researchers and drug development professionals, understanding these advantages and the associated technical considerations is essential for leveraging liquid biopsy's full potential in advancing precision oncology and improving patient outcomes.
Implementing Cutting-Edge dPCR and ddPCR Protocols for ctDNA Analysis
Circulating tumor DNA (ctDNA), a subset of cell-free DNA derived from tumor tissue, has emerged as an essential biomarker for the real-time, noninvasive assessment of cancer burden, molecular response, and early evaluation of recurrence in precision oncology [3]. The analysis of ctDNA via liquid biopsy presents a less invasive alternative to tissue biopsy, with lower sampling bias and procedural risk [3]. However, the reliable detection of ctDNA is challenging due to its often very low concentration in blood, sometimes constituting less than 0.1% of the total circulating cell-free DNA, especially in early-stage disease and minimal residual disease (MRD) settings [3]. This technical guide details an optimized, end-to-end workflow from blood collection to data analysis, specifically framed within the context of real-time PCR protocols for ctDNA research, to achieve maximal sensitivity and reproducibility for researchers, scientists, and drug development professionals.
The entire process, from patient blood draw to the generation of a quantitative ctDNA report, involves a series of critical and sequential steps. Each stage must be rigorously controlled to preserve the integrity of the scarce ctDNA analyte and ensure the accuracy of the final result. The following diagram summarizes this optimized workflow and its key decision points.
Phase 1: Pre-Analytical Sample Processing
The pre-analytical phase is arguably the most critical for success in ctDNA analysis, as improper handling can lead to the irreversible loss of the target analyte or the introduction of artifacts that confound subsequent analysis.
Blood Collection and Plasma Separation
- Collection Tube: Collect peripheral blood using cell-stabilizing tubes (e.g., Streck, PAXgene). These tubes prevent the lysis of white blood cells and the subsequent release of genomic DNA, which would dilute the ctDNA fraction [3] [21].
- Processing Timeline: Process blood samples within 4-6 hours of draw to ensure ctDNA stability and prevent degradation [21].
- Centrifugation Protocol: A double-centrifugation method is essential to obtain platelet-poor plasma.
- First Spin: Centrifuge at 1,600 × g for 15 minutes at 4°C to separate plasma from cellular components.
- Second Spin: Transfer the supernatant to a new tube and centrifuge at 16,000 × g for 10 minutes at 4°C to remove any remaining platelets and debris.
- Storage: Aliquot the cleared plasma to avoid freeze-thaw cycles and store at -80°C until cfDNA extraction.
cfDNA Extraction and Quality Control
Extract cfDNA from plasma using a silica membrane or magnetic bead-based kit optimized for low-abundance nucleic acids. The following table outlines key quality control checkpoints and their acceptance criteria.
Table 1: Quality Control Metrics for Extracted cfDNA
| Parameter | Assessment Method | Optimal QC Range | Importance |
|---|---|---|---|
| Concentration | Fluorometry (e.g., Qubit) | >0.5 ng/µL (from 1-4 mL plasma) | Indicates sufficient material for downstream analysis [3]. |
| Fragment Size | Bioanalyzer/TapeStation | Peak ~160-170 bp | Confirms enrichment of mononucleosomal cfDNA; tumor-derived cfDNA is often shorter [3]. |
| Purity (A260/A280) | Spectrophotometry | 1.8 - 2.0 | Suggests minimal protein or solvent contamination. |
Samples failing these QC metrics should not be advanced to library preparation, as they are likely to yield unreliable results.
Phase 2: Analytical Assay and qPCR Setup
This phase involves preparing the extracted cfDNA for amplification and setting up the highly sensitive qPCR reaction.
Library Preparation and Target Enrichment
For ctDNA detection using real-time PCR, a targeted approach is typically used.
- Library Preparation: Convert the extracted cfDNA into a sequencing library. This involves end-repair, adapter ligation, and minimal cycle amplification. Specialized library preparation methods that enrich for short fragments can significantly increase the fractional abundance of ctDNA [3].
- Target Enrichment: Use multiplexed PCR to amplify specific genomic regions harboring mutations of interest (e.g., SNVs, indels). This creates an amplicon library enriched for the targets, increasing the assay's sensitivity for detecting low-frequency variants [3].
qPCR Experimental Design and Plate Setup
Quantitative PCR enables the detection and quantification of mutant alleles with a limit of detection (LOD) approaching 0.1% variant allele frequency (VAF) when using digital PCR (dPCR) technologies, which is often the basis for ultra-sensitive qPCR assays [3] [22].
- Assay Design: Design TaqMan hydrolysis probes or similar, with wild-type and mutation-specific probes.
- Reaction Composition: Optimize the reaction mix with a passive reference dye to correct for variations in master mix volume and optical anomalies, thereby improving precision [22].
- Replicates: Include both technical and biological replicates.
- Technical Replicates: A minimum of triplicate reactions per sample is recommended to account for system variation (pipetting, instrument noise) and allow for outlier detection [22].
- Biological Replicates: Multiple patient or control samples per group are required to account for true biological variation [22].
The following diagram illustrates the logical decision process for setting up and running the qPCR experiment.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for ctDNA qPCR Workflow
| Reagent / Material | Function | Technical Considerations |
|---|---|---|
| Cell-Stabilizing Blood Tubes | Preserves blood sample integrity post-draw. | Prevents gDNA contamination from white blood cell lysis; critical for maintaining low background [3]. |
| cfDNA Extraction Kit | Isolates and purifies cfDNA from plasma. | Select kits designed for low-input, short-fragment DNA to maximize ctDNA recovery. |
| qPCR Master Mix | Provides enzymes, dNTPs, and buffer for amplification. | Use a high-fidelity, robust mix suitable for detecting rare variants. |
| Mutation-Specific Assays | Enables specific detection of target mutations. | Includes primers and probes (e.g., TaqMan) for wild-type and mutant sequences. LNA/DNA primers can enhance specificity. |
| Passive Reference Dye | Normalizes fluorescent signals. | Corrects for well-to-well volume variation and optical anomalies, improving data precision [22]. |
| Quantitative Standards | Enables absolute quantification. | A dilution series of synthetic DNA templates with known mutant allele concentrations to generate a standard curve. |
Phase 3: Data Analysis and Quality Assurance
Rigorous data analysis is required to transform raw fluorescence data into reliable, quantitative ctDNA measurements.
Quantification Methods
- Absolute Quantification: Relates the Cq value of a sample to a standard curve from known concentrations, allowing the determination of the fundamental number of target DNA molecules in a sample. This is essential for reporting ctDNA concentration in plasma [22].
- Relative Quantification: Measures the change in target quantity relative to a reference group (e.g., a housekeeping gene or wild-type allele). The ΔΔCq method is commonly used to calculate fold-changes in mutant allele frequency, though this is less common for direct ctDNA reporting.
Ensuring Precision and Statistical Significance
Precision—the random variation of repeated measurements—is critical for discriminating small, biologically significant differences in ctDNA levels [22].
- Calculate Precision Metrics:
- Coefficient of Variation (CV): A key measure of precision, calculated as (Standard Deviation / Mean) × 100%. CV should be minimized, ideally below 10-15% for technical replicates [22].
- Standard Error (SE): Measures sampling error, providing boundaries for how distant the measured mean is from the true mean [22].
- Statistical Testing: To assess whether an observed fold-change in ctDNA levels between groups (e.g., pre- and post-treatment) is statistically significant, perform a t-test. A significant result (typically p < 0.05) indicates that random chance is an unlikely explanation for the observed change [22].
Table 3: Key Statistical Metrics for qPCR Data Analysis
| Metric | Calculation | Interpretation in ctDNA Context |
|---|---|---|
| Coefficient of Variation (CV%) | (SD / Mean) × 100% | Measures run-to-run and sample-to-sample reproducibility. A high CV reduces the ability to detect true changes in ctDNA levels [22]. |
| Standard Error (SE) | SD / √(n) | Indicates the confidence in the mean estimate. A smaller SE suggests the sample mean is a more reliable estimate of the true population mean [22]. |
| p-value | From t-test or ANOVA | Determines the statistical significance of observed differences in ctDNA levels between patient groups or time points. |
The optimized workflow detailed in this guide—from standardized blood collection and stringent pre-analytical processing to a meticulously controlled qPCR assay and rigorous statistical analysis—provides a robust framework for reliable ctDNA detection and quantification. As the field advances, emerging technologies like fragment-enriched library preparation, nanomaterial-based electrochemical sensors, and AI-based error suppression methods promise to push sensitivity even further, potentially to attomolar concentrations [3]. Adherence to this structured protocol ensures the generation of high-quality, reproducible data, which is foundational for realizing the full potential of ctDNA analysis in cancer research, drug development, and ultimately, clinical practice.
The analysis of circulating tumor DNA (ctDNA) through real-time PCR has emerged as a transformative tool in oncology research and drug development, enabling non-invasive detection of tumor-specific genetic alterations from liquid biopsies. The pre-analytical phase—encompassing sample collection, processing, storage, and preparation—represents the most vulnerable stage in the entire workflow, where improper handling can irrevocably compromise data integrity. Research indicates that pre-analytical variables contribute to up to 70% of errors in laboratory testing, underscoring the critical importance of standardized protocols for reliable ctDNA analysis. This technical guide provides comprehensive, evidence-based methodologies for mastering pre-analytical variables to ensure the accuracy, reproducibility, and sensitivity required for cutting-edge circulating tumor DNA research.
Sample Tubes: Selection and Specifications
The initial choice of blood collection tubes fundamentally influences ctDNA stability and recovery, serving as the foundational step in pre-analytical workflows. Proper selection preserves the integrity of cell-free DNA and prevents genomic DNA contamination from leukocyte lysis.
PCR Tube Specifications and Performance Characteristics
For downstream PCR amplification, tube design directly impacts thermal transfer efficiency and reaction consistency. The following table summarizes key specifications for PCR tubes and strips used in ctDNA analysis:
Table 1: Performance Characteristics of PCR Tubes for ctDNA Analysis
| Feature | Specification | Importance for ctDNA Analysis |
|---|---|---|
| Material | Polypropylene [23] [24] | Chemically inert, prevents biomolecule adsorption |
| Wall Design | Thin-walled [23] [24] | Optimizes thermal transfer for precise temperature cycling |
| Certifications | RNase-, DNase-, DNA-free [23] [24] | Precludes false positives from contaminating nucleases or DNA |
| Profile | Low-profile design [24] | Reduces dead air volume, minimizes evaporation |
| Volume Range | 5-125 µL [24] | Accommodates low-volume reactions (15 µL typical for qPCR) |
| Cap Seal | Attached flat caps or domed strip caps [23] [24] | Ensures leak-proof seal during thermal cycling |
Tube Selection Guidelines
- Thermal Conductivity: Prioritize thin-walled tubes specifically designed for optimal heat transfer in thermal cyclers to ensure uniform temperature distribution across all samples [23] [24].
- Evaporation Prevention: Select tubes with secure, leak-proof caps; for instruments without heated lids, consider a mineral oil overlay to prevent evaporation during cycling [25].
- Sample Identification: Utilize color-coded caps or strips for efficient sample tracking in high-throughput environments [23].
Centrifugation Protocols: Optimal Processing Parameters
Differential centrifugation protocols are critical for separating ctDNA from cellular components in blood samples, preventing contamination from genomic DNA released by lysed blood cells.
Blood Processing Workflow for ctDNA Analysis
The following diagram illustrates the sequential centrifugation approach for optimal plasma and ctDNA recovery:
Centrifugation Parameters
- Initial Centrifugation: Process whole blood within 2 hours of collection at 1,600-2,000 × g for 10-20 minutes at 4°C to separate plasma from cellular components while minimizing cell lysis.
- Secondary Centrifugation: Transfer plasma supernatant to a new tube and centrifuge at 16,000 × g for 10 minutes at 4°C to remove remaining platelets and cellular debris.
- Plasma Storage: Aliquot cleared plasma into low-protein-binding tubes and store at -80°C if cfDNA extraction cannot be performed immediately.
Storage Conditions: Maintaining Sample Integrity
Storage conditions and stability timelines significantly impact ctDNA recovery and the sensitivity of subsequent qPCR detection. Systematic evaluation of reagent stability enables workflow optimization while maintaining analytical fidelity.
DNA and Reagent Stability Parameters
Table 2: Stability of qPCR Reagents and DNA Templates for ctDNA Analysis
| Component | Storage Condition | Stability Duration | Key Considerations |
|---|---|---|---|
| Extracted DNA | -20°C (short-term) [26] | Weeks to months | For long-term storage, purify and resuspend in standard buffer [26] |
| Primer-Probe Mixes | -20°C, protected from light [27] | ≥5 months with monthly freeze-thaw cycles | Aliquot to minimize freeze-thaw cycles [27] |
| Prepared qPCR Plates | 4°C [27] | 3 days before thermocycling | Maintains detection fidelity for low and high DNA copies [27] |
| Synthetic DNA Standards | -20°C with stabilizer (e.g., tRNA) [27] | ≥3 months | Aliquot to reduce freeze-thaw impacts; maintains standard curve linearity [27] |
| Whole Blood | Room temperature | Process within 2-6 hours | Use stabilizer-containing tubes if delayed processing is unavoidable |
Factors Contributing to DNA Degradation
DNA degradation profoundly impacts PCR efficiency and must be minimized throughout storage and handling:
- Temperature Fluctuations: Repeated freezing and thawing introduces strand breaks; aliquot samples to avoid more than 3-5 freeze-thaw cycles [28].
- Nuclease Contamination: Residual nucleases from inefficient purification degrade DNA; use nuclease-free consumables and include EDTA in storage buffers [28].
- Physical Shearing: Vortexing or pipetting generates hydrodynamic shear forces; gently mix by inversion and use wide-bore tips for DNA handling [28].
- Environmental Exposure: UV radiation and elevated temperatures accelerate degradation; store DNA in amber tubes at -20°C or below with consistent temperatures [28].
Experimental Protocols: Validation Methodologies
Protocol: Stability Testing of qPCR Reagents
Objective: Systematically evaluate the effects of storage conditions on qPCR reagent performance for ctDNA detection [27].
Materials:
- Validated qPCR assays (primers, probes)
- Synthetic DNA templates (gBlocks)
- QIAcuity Probe Master Mix (or equivalent)
- Low-protein-binding tubes (e.g., Corning Eppendorf tubes)
- Thermal cycler with real-time detection capability
Methodology:
- Primer-Probe Mix Stability:
- Prepare primer-probe mixes containing 7 µM each of forward and reverse primers and 1 µM TaqMan probe
- Aliquot mixes and subject to freeze-thaw cycles (monthly for 5 months)
- Store at -20°C in manual defrost freezer protected from light
- Compare Cq values and amplification efficiency monthly using synthetic DNA templates
Prepared qPCR Plate Stability:
- Prepare qPCR reactions containing master mix, primer-probe, and DNA template (4-20 copies/reaction)
- Prepare identical plates: one run immediately, another stored at 4°C for 3 days before running
- Use 8 technical replicates per condition to ensure statistical power
- Compare DNA copy estimates between plates using Wilcoxon Signed Rank test
Synthetic DNA Template Stability:
- Prepare gBlocks dilution series (1010 to 0.016 copies/µL) in tRNA stabilizer (10 ng/µL)
- Aliquot and store at -20°C for 0-3 months
- Calculate limits of detection (LOD) and limits of quantification (LOQ) using eLowQuant or equivalent software
- Assess PCR efficiency via linear regression of standard curves
Statistical Analysis:
- Use R Studio or equivalent for statistical analysis
- Test data normality with Shapiro-Wilk test and homogeneity of variance with Levene's test
- Apply non-parametric tests (Wilcoxon Signed Rank, Friedman repeated measures) for copy number comparisons
- Present data as median values with median absolute deviation error
Protocol: Assessment of DNA Degradation
Objective: Determine DNA integrity and its suitability for long-target amplification in ctDNA research [28].
Methodology:
- Agarose Gel Electrophoresis:
- Prepare 1-2% agarose gel in TAE or TBE buffer with ethidium bromide or alternative stain
- Load 100-200 ng DNA alongside high molecular weight ladder
- Electrophorese at 5-6 V/cm for 45-60 minutes
- Visualize under UV transillumination
- Interpretation:
- Intact DNA: Tight band of high molecular weight with minimal smearing
- Degraded DNA: Smearing pattern with reduction in high molecular weight band intensity
- Impact on PCR: As average DNA fragment size approaches target amplicon length, PCR efficiency decreases due to reduced intact templates
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Pre-Analytical ctDNA Workflows
| Item | Function | Technical Specifications |
|---|---|---|
| Stabilized Blood Collection Tubes | Preserves cell-free DNA profile prevents leukocyte lysis during transport | Streck Cell-Free DNA BCT or PAXgene Blood cDNA tubes |
| Polypropylene PCR Tubes | Reaction vessels for qPCR amplification | Thin-walled, DNase/RNase-free, 0.1-0.2 mL capacity [23] [24] |
| Taq DNA Polymerase | Enzyme for PCR amplification | Thermostable, 5'→3' polymerase activity, supplied with optimized buffer [25] |
| dNTPs | Building blocks for DNA synthesis | Purified, nuclease-free, neutral pH, quality verified for PCR |
| Primer-Probe Mixes | Target-specific amplification and detection | HPLC-purified, sequence-verified, optimized concentrations [27] [29] |
| qPCR Master Mix | Provides optimized reaction components | Contains buffer, dNTPs, polymerase, reference dye (e.g., ROX) [27] [29] |
| DNA Quantification Standards | Standard curve generation for absolute quantification | Synthetic DNA (gBlocks) with target sequences, suspended in stabilizer [27] |
| Nuclease-Free Water | Diluent for reagents and reactions | Molecular biology grade, certified free of nucleases and contaminants |
Mastering pre-analytical variables in ctDNA research requires meticulous attention to sample tube selection, centrifugation parameters, and storage conditions. The protocols and stability data presented herein provide evidence-based frameworks for optimizing liquid biopsy workflows, enabling researchers to maintain the integrity of precious samples throughout processing and storage. Implementation of these standardized approaches ensures the reliability, reproducibility, and sensitivity required for robust circulating tumor DNA detection and quantification in both basic research and drug development contexts.
The analysis of circulating tumor DNA (ctDNA) has emerged as a pivotal tool in precision oncology, enabling non-invasive detection of oncogenic mutations that drive cancer progression. This technical guide focuses on assay design strategies for five critical oncogenic targets—EGFR, KRAS, BRAF, PIK3CA, and ESR1—within the context of real-time PCR protocols for ctDNA research. These genes represent frequently mutated drivers in major cancer types, including non-small cell lung cancer (NSCLC), colorectal cancer, melanoma, and breast cancer, making them prime targets for therapeutic development and monitoring.
ctDNA refers to fragmented DNA molecules released into the bloodstream by tumor cells through apoptosis and necrosis, carrying the same genetic alterations present in the tumor tissue. Compared to traditional tissue biopsies, liquid biopsy offers distinct advantages: it is minimally invasive, captures tumor heterogeneity, enables real-time monitoring of treatment response, and facilitates detection of resistance mechanisms. The half-life of ctDNA is remarkably short (approximately 16 minutes to several hours), allowing researchers to monitor dynamic changes in tumor burden almost in real-time [30].
The effective design of assays for ctDNA analysis must account for several technical challenges, primarily the low abundance of ctDNA in plasma, especially in early-stage disease or low-shedding tumors, where it can constitute less than 0.1% of total cell-free DNA. This necessitates highly sensitive detection methods capable of identifying rare mutant alleles against a background of wild-type DNA. Additional considerations include pre-analytical variables (blood collection, processing, and DNA extraction), assay specificity, and standardization across laboratories [30].
Molecular Pathways and Biological Significance
Oncogenic mutations in EGFR, KRAS, BRAF, PIK3CA, and ESR1 converge on a limited number of critical signaling pathways that control cellular proliferation, survival, and differentiation. Understanding these pathways is essential for appropriate assay design and interpretation of results.
The EGFR (Epidermal Growth Factor Receptor) gene encodes a transmembrane receptor tyrosine kinase. Upon ligand binding, EGFR activates downstream signaling cascades, primarily the RAS-RAF-MAPK and PI3K-AKT pathways, which promote cell growth and inhibit apoptosis. Oncogenic EGFR mutations, particularly in NSCLC, often occur in the tyrosine kinase domain (exons 18-21) and lead to constitutive kinase activity independent of ligand binding. The most common sensitizing mutations include exon 19 deletions and the L858R point mutation in exon 21, both predicting response to EGFR tyrosine kinase inhibitors (TKIs). Conversely, the T790M mutation in exon 20 is a well-characterized resistance mechanism to first-generation TKIs [31] [32].
The KRAS (Kirsten Rat Sarcoma Viral Oncogene Homolog) gene encodes a small GTPase that acts as a critical signal transducer between activated cell surface receptors (including EGFR) and intracellular effectors. KRAS alternates between GTP-bound (active) and GDP-bound (inactive) states. Oncogenic mutations, most frequently at codons 12, 13, and 61, impair GTP hydrolysis, resulting in constitutive signaling through effectors like RAF and PI3K. KRAS mutations are prevalent in pancreatic, colorectal, and lung cancers and have historically been difficult to target therapeutically, though recent drugs target specific variants like KRAS G12C [33] [31].
The BRAF (B-Raf Proto-Oncogene, Serine/Threonine Kinase) gene encodes a serine/threonine-protein kinase that is a key component of the MAPK signaling pathway. The most common oncogenic mutation, BRAF V600E, results in constitutive kinase activity and continuous stimulation of MAPK signaling, promoting uncontrolled cell proliferation. BRAF mutations are particularly prevalent in melanoma, where they serve as predictive biomarkers for BRAF inhibitor therapies [33].
The PIK3CA (Phosphatidylinositol-4,5-Bisphosphate 3-Kinase Catalytic Subunit Alpha) gene encodes the catalytic subunit of PI3K. Oncogenic mutations, frequently found in hotspots within the helical (exon 9) and kinase (exon 20) domains, lead to hyperactivation of the PI3K-AKT-mTOR pathway, enhancing cell survival, growth, and metabolism. PIK3CA mutations are common in breast, colorectal, and other solid tumors and have emerged as biomarkers for PI3K inhibitors, such as alpelisib in PIK3CA-mutant breast cancer [34].
The ESR1 (Estrogen Receptor 1) gene encodes the estrogen receptor alpha, a ligand-activated transcription factor that plays a central role in hormone-responsive breast cancer. Mutations in the ligand-binding domain, particularly at residues Y537 and D538, lead to constitutive, estrogen-independent activation of the receptor, driving resistance to endocrine therapies like aromatase inhibitors. ESR1 mutations are rarely found in primary breast cancer but are acquired under the selective pressure of endocrine therapy in advanced disease, making them important biomarkers for monitoring treatment resistance [30].
The following diagram illustrates the key signaling pathways and interactions between these oncogenic targets:
Mutation Profiles and Clinical Prevalence
Understanding the specific mutation profiles and their clinical prevalence across different cancer types is fundamental to designing targeted assays. The following table summarizes key mutations in these oncogenic drivers and their frequencies in major malignancies, based on recent next-generation sequencing studies.
Table 1: Mutation Profiles and Clinical Prevalence of Key Oncogenic Targets
| Gene | Common Mutations | Primary Cancer Types | Approximate Frequency | Clinical Significance |
|---|---|---|---|---|
| EGFR | Exon 19 deletions, L858R, T790M, G719X | Non-small cell lung cancer | 51.8% (in NSCLC study) [31] | Predictive of response to EGFR TKIs; T790M confers resistance |
| KRAS | G12D, G12V, G12C, G13D, Q61H | Colorectal cancer, Pancreatic cancer, NSCLC | 8.9% (in NSCLC study) [31] | Prognostic biomarker; G12C now targetable with specific inhibitors |
| BRAF | V600E, V600K, V600R | Melanoma, Colorectal cancer, NSCLC | 43.8% V600E in melanoma [33] | Predictive biomarker for BRAF/MEK inhibitor combinations |
| PIK3CA | H1047R, E545K, E542K | Breast cancer, Colorectal cancer, Endometrial cancer | 5.4% (in NSCLC study) [31] | Predictive for PI3K inhibitors (e.g., alpelisib) in breast cancer |
| ESR1 | Y537S, Y537N, D538G | Hormone receptor-positive breast cancer | <1% in primary, 15-40% in endocrine-resistant metastatic disease [30] | Biomarker of resistance to aromatase inhibitors |
Recent research has revealed that mutation prevalence can vary significantly based on detection methodology. For instance, a 2025 study on melanoma patients using a sensitive NGS panel covering 1,114 COSMIC mutations found BRAF V600E in 43.8% and NRAS G12D in 36.4% of patients at baseline [33]. This highlights how assay sensitivity and coverage impact mutation detection rates. Furthermore, the same study demonstrated that ctDNA dynamics during treatment have prognostic value, with persistent or re-emerging ctDNA positivity post-therapy correlating with shorter progression-free survival.
The distribution of mutation types also differs among genes. KRAS and EGFR mutations are predominantly single nucleotide variants (SNVs) and small insertions/deletions (indels), while ESR1 mutations are almost exclusively missense mutations in specific hotspots. BRAF mutations are primarily the V600E variant in melanoma but show more diversity in other cancers. PIK3CA mutations cluster in exons 9 and 20, with the specific variant potentially influencing response to targeted therapies [34].
Assay Design Strategies for Real-Time PCR
Core Principles of ctDNA Assay Design
Designing robust real-time PCR assays for ctDNA analysis requires careful consideration of several factors to achieve the necessary sensitivity and specificity for detecting low-frequency mutations. The fundamental challenge lies in discriminating true low-abundance mutations from technical errors introduced during sample preparation, PCR amplification, and detection. The following experimental workflow outlines the key steps in developing and implementing ctDNA assays:
Effective assay design begins with understanding that ctDNA is highly fragmented (typically 160-180 base pairs), corresponding to nucleosome-protected DNA fragments. This fragmentation impacts primer and probe placement, with optimal amplicon sizes typically between 60-120 base pairs to maximize amplification efficiency. Shorter amplicons have higher amplification efficiency and are better suited for the fragmented nature of ctDNA.
Specificity is achieved through several mechanisms. Allele-Specific PCR designs primers with the 3' terminal nucleotide complementary to the mutant sequence, providing preferential amplification of the mutant allele. Mismatches in the penultimate positions can further enhance discrimination. Blocking oligonucleotides (also known as PCR clamps) can be used to suppress wild-type amplification by binding preferentially to wild-type sequences and interfering with polymerase extension. Probe-based detection with hydrolysis (TaqMan) or hybridization (FRET) probes provides an additional layer of specificity through sequence-specific binding and fluorescence reporting.
Sensitivity requirements depend on the clinical application. For monitoring minimal residual disease or early detection, assays need to detect variant allele frequencies (VAF) of 0.01% or lower. For therapy selection in advanced cancers, where VAFs are typically higher, sensitivities of 0.1-1% may be sufficient. Digital PCR platforms naturally provide higher sensitivity than conventional real-time PCR due to partitioning, which enables detection of rare mutants through endpoint amplification of individual molecules.
Advanced Techniques and Methodologies
Several advanced PCR methodologies have been developed specifically to address the challenges of ctDNA analysis:
Digital PCR (dPCR) partitions the reaction into thousands of individual amplifications, allowing absolute quantification without standard curves and enabling detection of rare mutations down to 0.001% VAF in optimal conditions. Droplet Digital PCR (ddPCR) is a widely adopted format that creates water-in-oil emulsion droplets for partitioning [30].
Amplification Refractory Mutation System (ARMS) technology utilizes allele-specific primers that only amplify when the target mutation is present. Commercial kits like the therascreen PIK3CA RGQ PCR Kit employ this principle to detect 11 mutations in the PIK3CA gene with high specificity [34].
BEAMing (Beads, Emulsion, Amplification, and Magnetics) combines emulsion PCR with flow cytometry to detect and quantify mutant alleles with high sensitivity, capable of detecting mutations at frequencies as low as 0.01% [30].
The following table compares the performance characteristics of different PCR-based methods for ctDNA analysis:
Table 2: Comparison of PCR-Based Methodologies for ctDNA Analysis
| Method | Sensitivity | Throughput | Multiplexing Capacity | Quantification | Best Applications |
|---|---|---|---|---|---|
| Real-time PCR | 1-5% VAF | Medium | Low (2-4 plex) | Relative | Therapy selection in high tumor burden |
| ARMS/Scorpions | 0.1-1% VAF | Medium | Low (mutation-specific) | Relative | Targeted mutation detection (e.g., therascreen) |
| Digital PCR (dPCR) | 0.01-0.1% VAF | Low to Medium | Medium (3-6 plex) | Absolute | MRD monitoring, therapy response |
| Droplet Digital PCR (ddPCR) | 0.01-0.05% VAF | Medium | Medium (3-6 plex) | Absolute | Validation of NGS findings, longitudinal monitoring |
| BEAMing | 0.01% VAF | Low | Low | Absolute | Ultra-sensitive detection of known mutations |
Protocol: Real-Time PCR Assay for PIK3CA Mutations in ctDNA
The following detailed protocol adapts principles from commercially available IVD tests, such as the therascreen PIK3CA RGQ PCR Kit, for research use in detecting PIK3CA mutations in plasma-derived ctDNA [34].
Principle: This assay uses allele-specific PCR with Scorpions primers and PCR clamps to selectively amplify and detect 11 mutations in exons 7, 9, and 20 of the PIK3CA gene while suppressing wild-type amplification.
Sample Requirements:
- Plasma: 4-5 mL of peripheral blood collected in K2EDTA tubes
- Process within 2-4 hours of collection with double centrifugation (300 × g for 10 minutes, then 1800 × g for 10 minutes)
- Store plasma at -80°C until extraction
cfDNA Extraction:
- Use the QIAamp DSP Circulating NA Kit or equivalent
- Elute in 50-100 μL of AE buffer
- Quantify using fluorometry (Qubit dsDNA HS Assay)
- Expected yield: 5-30 ng/mL plasma depending on tumor burden
Reaction Setup:
- Prepare six separate reaction mixes: one control reaction targeting exon 15 and five mutation-specific reactions
- Use 5-10 μL of extracted cfDNA per reaction (adjust volume based on concentration)
- Total reaction volume: 25 μL
- Cycling conditions on Rotor-Gene Q or equivalent real-time PCR instrument:
- Initial activation: 95°C for 10 minutes
- 50 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 60 seconds (with fluorescence acquisition)
Data Analysis:
- Analyze amplification curves using instrument software
- Automatic calling with pre-defined thresholds for mutant-positive calls
- A sample is called mutation-positive if the amplification curve crosses the threshold within 50 cycles for any mutation-specific reaction
- Include positive and negative controls in each run
Performance Characteristics:
- Analytical sensitivity: 0.1-1% VAF depending on mutation and input DNA
- Specificity: >97% compared to tissue testing [34]
- Turnaround time: <2 working days
Research Reagent Solutions
Successful implementation of ctDNA assays requires carefully selected reagents and tools. The following table outlines essential research reagent solutions for developing and performing real-time PCR assays for oncogenic targets.
Table 3: Essential Research Reagent Solutions for ctDNA Analysis
| Reagent/Tool | Function | Examples/Specifications | Key Considerations |
|---|---|---|---|
| Blood Collection Tubes | Plasma stabilization for ctDNA analysis | K2EDTA tubes; Cell-free DNA BCT tubes | Process K2EDTA tubes within 2-4 hours; BCT tubes allow longer storage at room temperature |
| cfDNA Extraction Kits | Isolation of cell-free DNA from plasma | QIAamp DSP Circulating NA Kit; Maxwell RSC ccfDNA Plasma Kit | High recovery of short fragments; effective removal of PCR inhibitors |
| DNA Quantification | Measurement of cfDNA concentration and quality | Qubit dsDNA HS Assay; Bioanalyzer HS DNA kit | Fluorometry preferred over spectrophotometry for accuracy with low concentrations |
| PCR Enzymes/Master Mixes | Amplification of target sequences | Hot-start Taq polymerases; dPCR master mixes | Low error rate; high efficiency with short amplicons; minimal allele amplification bias |
| Assay Designs | Mutation-specific detection | Therascreen kits; Custom TaqMan assays; IDT PrimeTime assays | Validation required for LOD, specificity, and reproducibility with fragmented DNA |
| Reference Materials | Assay validation and quality control | Seraseq ctDNA mutation mixes; Horizon Discovery reference standards | Characterized VAFs for sensitivity determination; include in each run as controls |
| Software | Data analysis and interpretation | Rotor-Gene AssayManager; Quantasoft for dPCR; Custom bioinformatics pipelines | Automated calling algorithms reduce inter-operator variability |
Analytical Validation and Quality Control
Rigorous validation is essential before implementing ctDNA assays in research studies. Key performance parameters to establish include:
Analytical Sensitivity (Limit of Detection): Determine the lowest VAF that can be reliably detected with 95% confidence. This requires testing dilution series of mutant DNA in wild-type background at various input amounts. A 2025 melanoma study using a sensitive NGS approach established a detection limit corresponding to 0.07% mutation allele frequency with seven mutant molecules [33].
Analytical Specificity: Assess cross-reactivity with similar mutation sequences and wild-type background. Include samples with known mutations in related genes to evaluate potential false positives.
Precision and Reproducibility: Evaluate repeatability (within-run) and reproducibility (between-run, between-operator, between-instrument) using samples with mutations at low VAFs near the limit of detection.
Linearity and Quantitative Properties: For quantitative assays, establish the dynamic range and correlation between measured and expected VAFs using reference materials with known mutation concentrations.
Robustness: Test performance under varying conditions, including different DNA inputs, reagent lots, and minor protocol modifications.
Routine quality control should include:
- Negative controls (wild-type DNA) in each run to monitor contamination
- Positive controls with mutations at low VAF near the detection limit
- No-template controls to monitor reagent contamination
- Reference materials with known VAF for process monitoring
Well-designed real-time PCR assays for detecting oncogenic mutations in EGFR, KRAS, BRAF, PIK3CA, and ESR1 from ctDNA provide powerful tools for cancer research and drug development. The strategies outlined in this guide emphasize the importance of understanding biological context, mutation profiles, and technical considerations specific to ctDNA analysis. As the field advances, ongoing refinements in assay sensitivity, multiplexing capabilities, and standardization will further enhance the utility of these approaches. The integration of well-validated ctDNA assays into research protocols promises to accelerate our understanding of cancer dynamics and therapeutic resistance mechanisms.
The analysis of circulating tumor DNA (ctDNA) via real-time quantitative PCR (qPCR) represents a transformative approach in modern clinical oncology. This methodology enables non-invasive monitoring of treatment response, detection of Minimal Residual Disease (MRD), and identification of emerging resistance mutations. The core principle hinges on the precise quantification of tumor-specific genetic alterations present in the bloodstream, providing a dynamic snapshot of tumor burden and genomic evolution. When framed within broader real-time PCR protocols for ctDNA research, these applications empower clinicians and drug development professionals to make data-driven decisions, moving beyond traditional and often less sensitive imaging or biopsy-based techniques. The technical foundation for these applications relies on robust nucleic acid extraction, optimized amplification, and rigorous data analysis to ensure that the results accurately reflect the underlying biological reality of the patient's disease state.
Core Principles of Real-Time PCR Data Analysis
The accurate interpretation of real-time PCR data is paramount for deriving meaningful clinical conclusions from ctDNA analysis. The process converts raw fluorescence data into reliable quantitative measures of target nucleic acid concentration.
Key Analytical Metrics
During a real-time PCR run, the accumulation of DNA products is tracked by fluorescence and plotted against amplification cycles, generating an amplification curve. Several critical metrics are derived from this curve [35]:
- Cycle Threshold (Ct): The cycle number at which the fluorescence signal intersects a set threshold. This value is inversely proportional to the starting concentration of the target molecule; a lower Ct indicates a higher initial concentration [35].
- Baseline: The initial cycles (typically 5-15) where fluorescence remains at background levels, establishing the baseline signal against which amplification is measured [35].
- Threshold: A fluorescence level set above the baseline but within the exponential phase of amplification, indicating a significant, detectable signal increase [35].
- Amplification Efficiency (E): A crucial measure of reaction performance, calculated as the proportion of target molecules duplicated in each cycle. Ideal reactions have efficiencies close to 100% (or E=2, representing a doubling). Acceptable efficiency typically ranges from 85% to 110% [35]. Efficiency is calculated using the formula:
Efficiency (%) = (10^(-1/Slope) - 1) * 100, where the slope is derived from a standard curve of serial dilutions [35].
Quantification Methods
Two primary mathematical models are used for quantification:
- Absolute Quantification: Determines the exact copy number of the target sequence by comparing Ct values to a standard curve of known concentrations. This is essential for applications like viral load testing [35].
- Relative Quantification: More common in gene expression studies like ctDNA analysis, this method compares the expression level of a target gene between a test sample and a reference sample (e.g., pre-treatment vs. during treatment). The target quantity is normalized to a reference gene with stable expression [35]. The two main approaches for relative quantification are the Livak method (2^(-ΔΔCt)), which assumes near-perfect amplification efficiency, and the Pfaffl method, which accounts for differences in efficiency between the target and reference genes [35].
Table 1: Key Data Analysis Methods for Real-Time PCR
| Method | Principle | Application Context | Key Assumptions |
|---|---|---|---|
| Comparative Ct (Livak) [35] | Calculates expression ratio via 2^(-ΔΔCt) | Relative quantification when target and reference gene efficiencies are approximately equal and near-perfect (90-100%) [35]. | PCR efficiencies of target and reference genes are similar and close to 100% [35]. |
| Efficiency-Calibrated (Pfaffl) [36] | Uses individual amplification efficiencies for target and reference genes in the ratio calculation [36]. | Relative quantification when amplification efficiencies are known and differ from 100% or between genes [36]. | Accurate pre-determination of individual reaction efficiencies is possible and reliable [36]. |
| Standard Curve [37] | Determines quantity by interpolating Ct values from a standard curve of known concentrations. | Absolute quantification or relative quantification with high accuracy; considered a gold-standard method [37]. | The standard curve is highly precise, and sample amplification efficiency matches that of the standard [37]. |
Experimental Workflow and Protocol Design
A standardized and meticulous experimental protocol is critical for generating reproducible and clinically actionable data from ctDNA analysis.
Sample Processing and Assay Design
The workflow begins with blood sample collection in cell-stabilizing tubes to prevent genomic DNA contamination from lysed white blood cells. Plasma is separated via centrifugation, followed by ctDNA extraction using specialized kits designed for low-concentration, fragmented DNA. The subsequent steps involve assay design and validation [37]:
- Primer/Probe Design: Target tumor-specific mutations (e.g., SNVs, indels, fusions) with primers and probes (e.g., TaqMan) designed for high specificity. A reference gene (e.g., from a housekeeping gene) is simultaneously assayed for normalization.
- Validation of Efficiency: Serial dilutions of a synthetic template or a known positive control are run to generate a standard curve. This curve is used to calculate the amplification efficiency and the dynamic range of the assay. The correlation coefficient (R²) of the standard curve should be >0.98, and the efficiency should be 85-110% [35] [37].
- Determination of Limit of Detection (LOD): The LOD, critical for MRD applications, is established by repeatedly testing serially diluted samples to find the lowest concentration detectable in ≥95% of replicates.
qPCR Run and Data Analysis
The prepared samples, including patient ctDNA, controls, and standards, are run on the qPCR instrument. The resulting data is then processed as follows [35] [36]:
- Assess the quality of the amplification curves and the efficiency of the run.
- Apply the chosen quantification method (see Table 1) to calculate the relative or absolute quantity of the mutant allele in each sample.
- For longitudinal monitoring (e.g., treatment response), normalize the mutant allele signal to the reference gene and plot the relative quantity over time. A decreasing trend indicates a positive response, while a rising trend may signal resistance or progression.
Diagram 1: Core Workflow for ctDNA Analysis
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of ctDNA qPCR assays requires a suite of specialized reagents and instruments.
Table 2: Essential Research Reagents and Materials
| Item | Function/Description | Application Note |
|---|---|---|
| Nucleic Acid Extraction Kit | Silica-membrane or magnetic bead-based kits optimized for recovering fragmented, low-abundance DNA from plasma. | Critical for achieving high-purity, inhibitor-free ctDNA, directly impacting PCR efficiency [35]. |
| qPCR Master Mix | A pre-mixed solution containing thermostable DNA polymerase, dNTPs, MgCl₂, and buffer. For ctDNA, a mix resistant to common plasma inhibitors is ideal. | Often includes a passive reference dye (ROX) for signal normalization. SYBR Green or probe-based (e.g., TaqMan) chemistries are used [35]. |
| Assay Primers & Probes | Oligonucleotides designed to specifically amplify and detect a tumor-derived mutation and a reference genomic sequence. | Specificity is paramount. Probe-based assays (e.g., TaqMan) offer higher specificity for distinguishing mutant from wild-type alleles [36]. |
| Standard Curve Templates | Synthetic oligonucleotides or plasmid controls containing the exact target sequence at known concentrations. | Used to generate a standard curve for determining amplification efficiency and for absolute quantification [35] [37]. |
| Real-Time PCR Instrument | A thermocycler with an integrated optical system for exciting fluorophores and detecting fluorescence in real time. | Must be capable of detecting multiple fluorophores simultaneously (multiplexing) for efficient target and reference amplification in a single well. |
Statistical Considerations and Data Quality Control
Robust statistical analysis is non-negotiable for ensuring the reliability of qPCR data, especially when used for clinical decision-making.
Replication and Quality Thresholds
To account for technical variability, experiments must include replicates. A minimum of three technical replicates per sample is recommended to identify and discount outliers and to calculate a mean Ct with a standard deviation [35]. The coefficient of variation for Ct values should be small. Furthermore, pre-defined quality thresholds for amplification efficiency (85-110%) and standard curve correlation (R² > 0.98) must be established, and runs failing these criteria should be repeated [35] [37].
Statistical Modeling for Significance
For relative quantification, confidence intervals and significance testing (p-values) for the calculated expression ratios are essential to avoid false positive conclusions [36]. Several statistical models can be applied:
- Multiple Regression or ANCOVA: These models can be used to derive ΔΔCt from the estimation of the interaction between gene and treatment effects, providing a framework for calculating confidence intervals [36].
- Randomization Tests: Some dedicated software packages use re-sampling techniques (like bootstrap or permutation tests) to assign statistical significance to expression ratios without assuming a specific data distribution [36].
Diagram 2: Data Quality Control Pathway
The integration of real-time PCR-based ctDNA analysis into clinical research protocols provides an powerful tool for advancing personalized oncology. The ability to monitor treatment response with high sensitivity, detect MRD post-therapy, and dynamically identify resistance mutations offers unprecedented insights into tumor dynamics. The reliability of these applications is contingent upon a rigorous foundation of optimized experimental workflows, precise data analysis adhering to established mathematical models, and stringent statistical quality control. As these methodologies continue to mature and become standardized, they hold the promise of fundamentally reshaping how cancer treatment efficacy is assessed and how therapeutic strategies are adapted in real time.
Solving Common Pitfalls and Enhancing Sensitivity in ctDNA PCR Assays
The reliability of circulating tumor DNA (ctDNA) analysis in cancer research and clinical diagnostics is fundamentally dependent on the quality of the pre-analytical phase. This technical guide provides an in-depth examination of three critical pre-analytical variables—hemolysis, cellular contamination, and sample stability—within the context of real-time PCR protocols for ctDNA research. We summarize the quantitative impacts of these variables, detail robust methodological protocols for their mitigation, and provide visual workflows to guide researchers in ensuring the integrity of liquid biopsy samples from collection to analysis.
Circulating tumor DNA (ctDNA) comprises fragmented DNA released into the bloodstream through tumor cell apoptosis and necrosis, typically exhibiting a short half-life ranging from 16 minutes to 2.5 hours [38]. The analysis of ctDNA via liquid biopsy offers a non-invasive window into tumor genetics, enabling applications in early cancer detection, treatment response monitoring, and identification of resistance mechanisms [39] [38]. However, the low relative abundance of ctDNA within total cell-free DNA (cfDNA) presents a significant analytical challenge, necessitating techniques with exceptional sensitivity and specificity [39].
The journey from sample collection to ctDNA analysis is intricate, involving numerous steps where variables can compromise result integrity. Among these, hemolysis (the rupture of red blood cells), cellular contamination (from improper handling), and sample instability (from improper storage or processing delays) represent the most pervasive threats to pre-analytical quality [40]. These variables can introduce significant analytical noise, including:
- Release of abundant wild-type genomic DNA from blood cells, diluting the mutant allele fraction of ctDNA.
- Introduction of PCR inhibitors that affect amplification efficiency.
- Degradation of true ctDNA targets, reducing detection sensitivity.
For real-time PCR protocols, which are widely used for their sensitivity and speed in detecting predefined mutations, these pre-analytical imperfections can lead to both false-negative and false-positive results, ultimately undermining the validity of research findings and their translation into clinical applications [41] [42]. This guide details the impacts of these variables and provides standardized protocols to navigate these challenges effectively.
Hemolysis: Impact, Detection, and Quantification
Mechanisms of Interference
Hemolysis occurs when red blood cells (RBCs) rupture, releasing their intracellular contents, including hemoglobin and genomic DNA, into the plasma or serum. This process fundamentally alters the sample matrix in ways that interfere with downstream ctDNA analysis [43]. The primary mechanisms of interference include:
- Release of PCR Inhibitors: Hemoglobin and its breakdown products are potent inhibitors of DNA polymerase enzymes, reducing the amplification efficiency critical for real-time PCR assays [42].
- Dilution of ctDNA Fraction: The genomic DNA released from lysed RBCs constitutes a large mass of wild-type DNA. This dilutes the already scarce ctDNA fragments, effectively lowering the mutant allele fraction and making detection of low-frequency variants more challenging [40].
- Alteration of Sample Composition: The profile of cell-free nucleic acids is skewed, as RBCs contain specific microRNAs and other nucleic acid species that are not representative of the tumor-derived material [43].
Quantitative Impact on Quality Metrics
The effect of hemolysis is dose-dependent. Research on non-invasive prenatal testing (NIPT), which similarly relies on the analysis of rare cfDNA fragments, provides quantifiable insights into these impacts. One study categorized plasma samples based on free hemoglobin concentration and observed significant deviations in key quality metrics in severely hemolyzed samples [44].
Table 1: Impact of Hemolysis Severity on NIPT Quality Control Metrics
| Hemolysis Group | Free Hemoglobin (g/L) | Library Concentration | Duplication Rate | Fetal Fraction (Analogous to ctDNA fraction) |
|---|---|---|---|---|
| I (None) | 0 - 1 | Baseline | Baseline | Baseline |
| II (Slight) | 1 - 2 | No significant change | No significant change | No significant change |
| III (Moderate) | 2 - 4 | No significant change | No significant change | No significant change |
| IV (Severe) | > 4 | Decreased | Increased | Increased |
Data adapted from [44]. An increased duplication rate indicates lower library complexity, often resulting from an over-representation of a limited number of original DNA molecules, which can occur when the sample input is compromised. The observed increase in fetal fraction in severely hemolyzed samples may be an analytical artifact.
Detection and Assessment Methods
- Visual Inspection: A simple initial assessment. After centrifugation, the plasma of a hemolyzed sample will have a pink to red hue, whereas non-hemolyzed plasma is typically yellow and clear.
- Spectrophotometry: This is the gold-standard for objective quantification. Hemoglobin has a characteristic absorbance peak at 414 nm (with secondary peaks at 541 and 576 nm) [43] [44]. The optical density at 414 nm (OD414) is used to quantify hemolysis.
- Protocol: Measure the absorbance of the plasma sample against a blank (e.g., water or buffer) across a spectrum from 350 nm to 650 nm. An OD414 value exceeding 0.2 is generally considered indicative of significant hemolysis, though laboratories should establish their own validated thresholds based on downstream applications [43].
- Automated Hematology Analyzers: Clinical-grade instruments can provide highly precise measurements of free hemoglobin concentration in plasma using methods like photometry with sodium lauryl sulfate reagent [44].
Cellular Contamination and Sample Stability
The Threat of Cellular Contamination
Cellular contamination refers to the presence of intact white blood cells (WBCs) in the plasma fraction. This occurs due to incomplete or improper centrifugation, which fails to pellet all cellular components. The stability of cfDNA is also highly time- and temperature-sensitive [40].
- Source of Contamination: The primary source is WBCs that are not fully removed during plasma preparation.
- Consequence: These cells can lyse during storage or freeze-thaw cycles, releasing high-molecular-weight genomic DNA into the plasma. This contaminating DNA is a major confounder for ctDNA analysis, as it dilutes the ctDNA fraction and can lead to false-positive or false-negative results in mutation detection assays [40] [38].
Sample Stability and Processing Timelines
cfDNA is susceptible to degradation by nucleases present in blood, and the risk of cellular lysis increases with time. Therefore, establishing strict processing protocols is essential.
Table 2: Pre-Analytical Stability and Processing Guidelines for Blood Samples
| Variable | Recommended Handling | Rationale |
|---|---|---|
| Time to Processing | Centrifuge within 1-2 hours of blood draw if using standard EDTA tubes; within 3-4 days if using specialized cfDNA stabilization tubes [40] [44]. | Prevents lysis of blood cells and release of genomic DNA; preserves the integrity of cfDNA fragments. |
| Centrifugation Protocol | Two-step protocol: 1. ~1000-1500 × g for 10-20 min to pellet cells. 2. Transfer plasma and re-centrifuge at ~3000-4000 × g for 10-15 min to remove residual cells [40]. | The initial spin separates bulk cells; the second, higher-force "plasma clean-up" spin ensures removal of remaining platelets and cellular debris. |
| Storage Temperature | Store isolated plasma and extracted cfDNA at -80 °C; avoid repeated freeze-thaw cycles [40]. | Halts nuclease activity and preserves nucleic acid integrity for long-term storage. |
| Urine cfDNA | Even more labile than plasma cfDNA; requires immediate stabilization or processing due to sensitivity to temperature and pH [40]. | Direct contact with urinary enzymes and variable pH can lead to rapid degradation of ucfDNA. |
Experimental Protocols for Quality Control
Protocol: Assessment of Hemolysis by Spectrophotometry
This protocol is used to objectively quantify the degree of hemolysis in a plasma sample [43] [44].
- Sample Preparation: Centrifuge the blood sample using a validated two-step protocol to obtain clear plasma.
- Blank Preparation: Use the supernatant from a centrifuged saline solution or distilled water as a blank.
- Measurement:
- Use a spectrophotometer (e.g., NanoPhotometer P300) capable of scanning from 350 nm to 650 nm.
- Blank the instrument with your chosen solution.
- Place the plasma sample in a cuvette and run the absorbance scan.
- Analysis:
- Identify the absorbance peak at or near 414 nm.
- Record the OD414 value. Values above 0.2 suggest significant hemolysis that may interfere with downstream PCR analysis [43].
- Visually inspect the spectrum for the characteristic hemoglobin peaks at 541 nm and 576 nm, which confirm hemolysis.
Protocol: Direct Real-Time PCR from Blood Lysate (A Cost-Effective QC Tool)
This method, adapted from a recent study, allows for rapid genetic analysis without DNA extraction, which can be useful for quick quality checks or specific applications where inhibitor resistance is optimized [42]. The "GG-RT PCR" protocol demonstrates that with a simple heat treatment and dilution, PCR inhibitors in blood can be overcome.
- Lysate Preparation:
- Mix 400 µL of EDTA-treated whole blood with 1.6 mL of distilled water (creating an 80% dilution).
- Vortex the mixture and incubate at 95 °C for 20 minutes. Vortex 2-3 times during incubation.
- Centrifuge at 14,000 rpm for 5 minutes.
- Collect the clear supernatant. This lysate can be used directly as a template or diluted 1:5 or 1:10 for PCR.
- Real-Time PCR Setup:
- Use a robust real-time PCR master mix (e.g., LightCycler 480 SYBR Green I Master mix).
- In a final reaction volume of 10 µL, add 2.5 µL of the 1:10 diluted blood lysate and 5 pmol of each primer.
- Run the PCR with standard cycling conditions: 95°C for 10 min, followed by 40 cycles of 95°C for 15 s and 60-61°C for 30 s.
- Note: While this method is cost-effective, the study notes that PCR efficiency can be lower than with purified DNA, and it may not be suitable for detecting very low-frequency ctDNA mutations without further optimization [42].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Kits for Managing Pre-Analytical Variables
| Item | Function/Benefit |
|---|---|
| Cell-Free DNA Blood Collection Tubes | Specialized tubes (e.g., from Streck, Roche, Geenseek) contain preservatives that stabilize nucleated blood cells, preventing lysis and genomic DNA release for several days, allowing for extended transport [40] [44]. |
| Magnetic Bead-based cfDNA Kits | Kits (e.g., PowerSoil Pro Kit, BGI DNA Extraction Kit) are optimized for efficient isolation of short-fragment cfDNA while removing PCR inhibitors [41] [44]. |
| Droplet Digital PCR (ddPCR) | A highly sensitive detection method suitable for validating low-frequency variants in ctDNA, often used as a gold standard to compare against real-time PCR results [38]. |
| Next-Generation Sequencing (NGS) | Provides a broader, untargeted approach for discovering novel mutations and assessing tumor heterogeneity, complementing targeted real-time PCR assays [39] [38]. |
| Sysmex XN-9000 Analyzer | Automated hematology analyzer capable of precise, photometric quantification of free hemoglobin in plasma, providing an objective measure of hemolysis [44]. |
Workflow and Pathway Visualizations
Sample Processing and Quality Control Workflow
Sample Processing and QC Workflow: This diagram outlines the critical decision points from blood collection to analysis, emphasizing the importance of tube selection and hemolysis assessment.
Impact of Pre-Analytical Variables on ctDNA Analysis
Impact of Pre-Analytical Variables: This diagram illustrates how different pre-analytical failures lead to specific technical problems that compromise the quality and reliability of real-time PCR data.
The path to robust and reproducible real-time PCR-based ctDNA analysis is paved during the pre-analytical phase. Uncontrolled variables like hemolysis, cellular contamination, and sample instability are not merely nuisances but fundamental confounders that can invalidate research findings. By implementing the standardized protocols, quality control checks, and workflows detailed in this guide—including rigorous hemolysis assessment, double-centrifugation plasma preparation, and adherence to strict processing timelines—researchers and drug development professionals can significantly enhance the fidelity of their liquid biopsy data. Mastering these pre-analytical fundamentals is a prerequisite for generating meaningful results that can reliably inform cancer biology and therapeutic development.
In circulating tumor DNA (ctDNA) research, the analysis of tumor-derived genetic material from liquid biopsies has emerged as a powerful, noninvasive paradigm for real-time assessment of tumor burden, therapeutic response, and minimal residual disease (MRD) [3]. The central challenge in this field stems from the exceptionally low concentration of ctDNA in bloodstream, which often constitutes less than 0.1% of total circulating cell-free DNA (cfDNA), and can be as low as 0.001% in early-stage cancers and MRD detection [3]. This vanishingly low variant allele frequency (VAF) creates significant technical hurdles for reliable detection, driving the need for rigorous optimization of every component in the real-time PCR workflow [3] [13].
Within this context, three technical elements form the foundational pillars of assay sensitivity: precise input DNA mass determination, strategic primer and probe design, and effective reaction partitioning. These components collectively determine the ability to distinguish rare mutant alleles from wild-type DNA background while maintaining assay efficiency and reproducibility. This guide provides a comprehensive framework for optimizing these critical parameters specifically for ctDNA research, enabling researchers to achieve the attomolar sensitivity required for meaningful clinical applications in cancer detection and monitoring [3] [13].
Input DNA Mass: Quantification and Quality Control
DNA Quantification and Purity Assessment
Accurate quantification and quality assessment of input DNA are critical first steps in ctDNA analysis. Fluorometric methods using Qubit fluorometers are strongly recommended over spectrophotometric approaches (NanoDrop) due to their superior specificity for double-stranded DNA and reduced susceptibility to common contaminants like RNA, salts, or organic compounds [45]. For ctDNA applications, DNA samples should demonstrate purity ratios of approximately 1.8 for OD 260/280 and 2.0-2.2 for OD 260/230 [45]. Deviations from these ranges indicate potential contaminants: low 260/280 ratios suggest protein or phenol contamination, while low 260/230 ratios indicate salt or solvent residues that can inhibit enzymatic reactions [45].
Table 1: DNA Quality Control Assessment Methods and Specifications
| Parameter | Recommended Method | Acceptable Range | Significance for ctDNA Analysis |
|---|---|---|---|
| Mass Quantification | Qubit fluorometer with dsDNA BR Assay | Variable based on application | Specific for dsDNA; unaffected by RNA contamination [45] |
| Purity (260/280) | NanoDrop spectrophotometer | ~1.8 | Ratios <1.8 indicate protein/phenol contamination [45] |
| Purity (260/230) | NanoDrop spectrophotometer | 2.0-2.2 | Ratios <2.0 indicate salt/solvent contamination [45] |
| Fragment Size | Bioanalyzer (≤10 kb) or pulsed-field gel electrophoresis (>10 kb) | Dependent on sample type | Critical for molar concentration calculations [45] |
Optimal Input Mass Determination
The optimal input DNA mass for PCR reactions varies significantly based on template type and fragment size. For genomic DNA, recommendations range from 5-50 ng per 50 μL reaction, while plasmid DNA requires substantially less (0.1-1 ng) due to lower complexity [46]. For ctDNA applications with fragmented DNA, molar quantification becomes essential. As illustrated in Table 2, the relationship between mass and molarity varies dramatically with fragment size, necessitating careful calculation to ensure optimal template input [45].
Table 2: DNA Mass to Molarity Conversion Guide for Various Fragment Sizes
| Mass (ng) | Molarity (fmol) for 200 bp | Molarity (fmol) for 1 kb | Molarity (fmol) for 8 kb | Molarity (fmol) for 20 kb |
|---|---|---|---|---|
| 2000 | 100 | - | - | - |
| 1000 | 200 | 50 | - | - |
| 500 | 500 | 100 | 25 | - |
| 100 | 950 | 100 | 20 | 5 |
| 50 | 450 | 50 | 10 | 3 |
| 10 | 100 | 10 | 2 | - |
Excessive DNA input increases risk of nonspecific amplification, while insufficient template reduces yield and assay sensitivity [46]. For ctDNA applications where template is limiting, inputs at the lower end of recommended ranges (10-100 fmol for fragments <1 kb) are typically optimal, balancing sensitivity with reaction efficiency [45].
Primer and Probe Design: Principles and Optimization Strategies
Fundamental Design Parameters
Well-designed primers and probes are essential for specific and efficient amplification of ctDNA targets. The following parameters represent consensus recommendations from leading industrial and academic sources [46] [47] [48]:
- Length: 18-30 nucleotides for optimal specificity and binding efficiency [46] [47]
- Melting Temperature (Tm): 55-70°C, with ideally 60-64°C for qPCR applications [46] [47]
- Primer Pair Compatibility: Tm values for forward and reverse primers should differ by no more than 2°C [47]
- GC Content: 40-60% with uniform distribution to minimize secondary structures [46] [47] [48]
- 3' End Design: Inclusion of a G or C base (GC clamp) to enhance priming efficiency, while avoiding runs of more than three G or C bases [46] [48]
- Specificity Checks: Comprehensive BLAST analysis to ensure target specificity, particularly important for avoiding amplification of homologous sequences or pseudogenes [47] [48]
For ctDNA applications, special consideration must be given to the impact of fragmented templates on amplicon design. While standard qPCR amplicons of 70-150 bp are ideal, ctDNA fragments typically range from 90-150 bp, necessitating careful size matching between template and anticipated product [3] [47].
Advanced Design Considerations for ctDNA
Beyond these fundamental parameters, ctDNA applications require additional design sophistication. Structural variant (SV)-based assays that target tumor-specific rearrangements (translocations, insertions, or deletions) can achieve parts-per-million sensitivity by leveraging breakpoint sequences unique to the tumor [3]. Phased variant approaches, which target multiple single-nucleotide variants on the same DNA fragment, further enhance ctDNA detection sensitivity [3].
For probe-based detection systems, the mediator probe should be positioned in close proximity to primers without overlapping their binding sites, with a Tm approximately 5-10°C higher than the associated primers [47] [49]. Statistical design of experiments (DOE) methodologies can systematically optimize multiple probe design factors simultaneously, significantly enhancing assay performance while reducing experimental burden [49].
Experimental Validation and Optimization
Computational design represents only the initial phase of primer and probe development. Experimental validation through stepwise optimization is essential, particularly for ctDNA applications where discrimination of single-nucleotide variants is critical [50]. This process should include:
- Annealing Temperature Optimization: Using temperature gradient PCR to identify the optimal temperature that maximizes specificity and efficiency [47] [50]
- Primer Concentration Titration: Testing concentrations from 0.1-1 μM to identify the concentration that minimizes primer-dimer formation while maintaining robust amplification [46]
- Efficiency Validation: Establishing a standard curve with serial dilutions (minimum 5 logs) to verify amplification efficiency between 90-110% with R² ≥ 0.99 [51] [52]
Reaction Partitioning: Digital PCR and Advanced Detection Platforms
Principles of Reaction Partitioning
Reaction partitioning represents a paradigm shift in ctDNA detection sensitivity, enabling absolute quantification of rare mutant alleles through physical separation of template molecules into thousands of individual reactions. This approach, exemplified by droplet digital PCR (ddPCR), effectively dilutes the wild-type DNA background, allowing sensitive detection of mutant alleles at variant allele frequencies as low as 0.001% [3]. The statistical power of partitioning technologies enables precise quantification without standard curves, making them particularly valuable for ctDNA applications where reference materials may be limited [3] [13].
Partitioning assays fundamentally enhance sensitivity by overcoming the limitations of bulk PCR reactions, where rare mutant templates are overwhelmed by abundant wild-type sequences. For early-stage cancers and minimal residual disease monitoring, where ctDNA concentrations can be exceptionally low, partitioning methods provide the necessary sensitivity to detect molecular recurrence months before clinical manifestation [3].
Emerging Partitioning Technologies
Beyond established ddPCR platforms, several emerging technologies show particular promise for ctDNA analysis:
- Beads, Emulsions, Amplification, and Magnetics (BEAMing): Combines magnetic beads with emulsion PCR to physically separate and amplify individual DNA molecules, achieving exceptional sensitivity for rare variant detection [13]
- Nanomaterial-based Platforms: Utilize magnetic nanoparticles conjugated with complementary DNA probes to capture and enrich target ctDNA fragments, achieving attomolar detection limits within 20 minutes [3]
- CRISPR-Cas Integrated Systems: Leverage the specificity of CRISPR-Cas systems combined with partitioning approaches to detect tumor-specific mutations with single-base resolution [3]
- Microfluidic Point-of-Care Devices: Implement partitioning in miniaturized formats suitable for clinical settings, potentially enabling rapid ctDNA analysis without specialized laboratory infrastructure [3]
Implementation Considerations for Partitioning assays
Successful implementation of partitioning technologies for ctDNA analysis requires careful consideration of several factors:
- Template Input Requirements: Optimal partitioning efficiency typically requires 100-200 fmol of DNA input for fragments <10 kb, with adjustments based on fragment size distribution [45]
- Platform-Specific Optimization: Each partitioning technology requires platform-specific optimization of probe chemistry, partition volume, and amplification conditions [3]
- Data Analysis Frameworks: Appropriate statistical models (particularly Poisson distribution accounting for low template concentrations) are essential for accurate variant frequency quantification [51] [52]
- Quality Control Metrics: Implementation of rigorous QC measures including limit of detection (LOD) and limit of quantification (LOQ) determinations specific to partitioning platforms [3]
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents for ctDNA Optimization
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Blood Collection Tubes with Stabilizers (cfDNA BCT Streck, PAXgene Blood ccfDNA) | Preserve blood sample integrity, prevent genomic DNA release from blood cells | Enable room temperature storage/transport for up to 7 days; critical for multisite trials [13] |
| High-Sensitivity DNA Quantitation Kits (Qubit dsDNA BR Assay) | Fluorometric quantification of input DNA | Specific for dsDNA; unaffected by RNA contamination [45] |
| DNA Polymerase with Proofreading Activity | High-fidelity DNA amplification | Essential for minimizing introduction of artifactual mutations during amplification [46] |
| dNTP Mixtures | Nucleotide substrates for DNA synthesis | Balanced equimolar mixtures (typically 0.2 mM each) recommended; unbalanced concentrations can increase error rates [46] |
| Magnesium Salt Solutions (MgCl₂) | Cofactor for DNA polymerase activity | Optimal concentration typically 1.5-4.0 mM; requires titration for each assay [46] [48] |
| Passive Reference Dyes (ROX) | Normalization of fluorescence signals | Correct for well-to-well variation; concentration optimization critical for assay precision [51] |
| PCR Additives (DMSO, Betaine, BSA) | Enhance amplification efficiency | Reduce secondary structure; particularly valuable for GC-rich targets [48] |
Integrated Workflow and Future Perspectives
The optimization of input DNA mass, primer/probe design, and reaction partitioning represents an interconnected framework rather than isolated technical considerations. Successful ctDNA analysis requires seamless integration of these components, with optimization decisions in one area directly influencing requirements in others. The workflow diagram below illustrates the integrated nature of these optimization processes:
Looking forward, several emerging technologies promise to further enhance ctDNA detection sensitivity. Structural variant-based assays that target tumor-specific rearrangements can achieve parts-per-million sensitivity by leveraging breakpoint sequences unique to the tumor [3]. Nanomaterial-based electrochemical sensors utilizing graphene or molybdenum disulfide (MoS₂) facilitate label-free sensing methods with attomolar detection limits [3]. Additionally, fragmentomic approaches that exploit differences in fragment length between tumor-derived and normal cfDNA (90-150 bp versus longer fragments) can enrich for ctDNA without additional biochemical processing [3].
The integration of artificial intelligence-based error suppression methods and microfluidic point-of-care devices represents the next horizon for ctDNA liquid biopsy technology, potentially enabling routine clinical implementation of these optimized technical approaches [3]. As these technologies mature, the rigorous optimization framework outlined in this guide will provide the foundational principles upon which future ctDNA analysis platforms will be built, ultimately enhancing cancer detection, monitoring, and treatment selection for patients across the disease spectrum.
Clonal hematopoiesis of indeterminate potential (CHIP) represents a significant source of biological noise in circulating tumor DNA (ctDNA) analysis, particularly when using real-time PCR and related amplification technologies. CHIP occurs when hematopoietic stem cells acquire mutations that provide a selective growth advantage, leading to an expanded clone within the blood compartment without an underlying hematologic malignancy. These mutations are detectable in cell-free DNA (cfDNA) and can originate from non-malignant white blood cells, creating false positive results that complicate ctDNA interpretation [53]. The presence of CHIP-associated mutations in blood-derived cfDNA poses a substantial challenge for cancer detection and monitoring, as these age-related mutations can be misclassified as tumor-derived variants, thereby reducing the specificity of liquid biopsy assays [53] [1]. This interference is particularly problematic in real-time PCR protocols for ctDNA research, where distinguishing low-frequency tumor-derived mutations from CHIP-related variants is essential for accurate clinical interpretation.
The challenge is amplified by the fact that CHIP prevalence increases with age, affecting more than 20% of elderly individuals, and involves genes commonly mutated in various cancers [54]. For instance, mutations in genes such as DNMT3A, TET2, and ASXL1 are frequently observed in CHIP but may also be relevant in solid tumors, creating a diagnostic gray area. This overlap necessitates sophisticated strategies to differentiate true tumor-derived signals from CHIP-related biological noise, especially in early cancer detection and minimal residual disease monitoring where ctDNA fraction may be exceptionally low [53] [1].
Technical Strategies for CHIP Mitigation
Wet-Lab Methodological Approaches
Table 1: Experimental Wet-Lab Protocols for CHIP Mitigation
| Method | Protocol Details | Key Applications | Limitations |
|---|---|---|---|
| Paired Granulocyte Sequencing | Sequence DNA from paired granulocyte cell fraction alongside plasma cfDNA; filter mutations present in both samples [1]. | Tumor-informed ctDNA assays; distinguishing somatic tumor variants from CHIP. | Requires additional sample processing; increases cost and complexity. |
| Tumor-Informed Sequencing | Utilize prior knowledge of tumor tissue mutational profile to specifically target tumor-derived variants [53] [1]. | MRD detection; therapy response monitoring. | Dependent on availability of tumor tissue; may miss heteroclonal evolution. |
| Unique Molecular Identifiers (UMIs) | Tag individual DNA molecules with barcodes before amplification to distinguish true mutations from amplification artifacts [1]. | All NGS-based ctDNA assays; error correction. | Does not directly address CHIP; requires specialized bioinformatic processing. |
| Duplex Sequencing | Sequence both strands of DNA duplex; true mutations appear in complementary positions on both strands [1]. | Ultra-sensitive mutation detection; error correction. | Technically challenging; lower efficiency requiring more input material. |
Experimental protocols for CHIP mitigation begin at sample collection. The use of cell-stabilizing blood collection tubes (e.g., cfDNA BCT tubes from Streck) is crucial, as they prevent leukocyte lysis and subsequent release of genomic DNA that could amplify CHIP-derived signals [9]. Plasma processing should follow a double centrifugation protocol (initial 380–3,000 × g for 10 minutes followed by 12,000–20,000 × g for 10 minutes at 4°C) to ensure efficient removal of cellular debris [9].
For DNA extraction, silica membrane-based kits (e.g., QIAamp Circulating Nucleic Acid Kit) generally yield higher quantities of ctDNA than magnetic bead-based methods, improving the detection limit for true tumor-derived variants [9]. When designing PCR assays, prioritize amplification of mutations previously identified in tumor tissue when possible, and avoid known CHIP hotspot regions (e.g., DNMT3A R882) unless these mutations are specifically relevant to the patient's known tumor genotype.
Bioinformatic and Computational Solutions
Table 2: Bioinformatic Strategies for CHIP Identification and Filtering
| Strategy | Implementation | Advantages | Considerations |
|---|---|---|---|
| CHIP Database Filtering | Filter variants against curated CHIP databases (e.g., CDC CHIP Resource, public CHIP repositories) [53]. | Rapid filtering of known CHIP hotspots; easily implementable. | May miss novel CHIP mutations; database completeness varies. |
| Variant Allele Frequency (VAF) Analysis | CHIP variants typically show VAF between 5-30% with subclonal patterns; tumor-derived ctDNA often has lower VAF [1]. | Can identify patterns characteristic of CHIP; uses standard sequencing metrics. | Overlap in VAF ranges limits reliability as standalone method. |
| Fragmentomics Analysis | Leverage differences in DNA fragmentation patterns; CHIP-derived cfDNA fragments resemble non-malignant cfDNA [53] [1]. | Tissue-of-origin information; does not require prior knowledge of mutations. | Requires specialized analysis; still in validation phase. |
| Machine Learning Classification | Train classifiers on multi-feature data (VAF, fragment size, genomic context, methylation) [53]. | High discrimination accuracy; adaptable to new data. | Requires large training datasets; computational intensity. |
Advanced computational approaches integrate multiple features to distinguish CHIP-derived mutations. Machine learning algorithms can be trained on fragmentomic patterns, as ctDNA fragments typically exhibit different size distributions and end motifs compared to non-malignant cfDNA [53]. These algorithms achieve high discrimination accuracy when trained on multi-modal features including VAF, fragment size, genomic context, and nucleosomal positioning patterns.
Implementation of these bioinformatic filters requires careful validation using positive and negative control samples with known CHIP status. The analytical workflow should incorporate stepwise filtering approaches that sequentially apply database matching, VAF thresholds, and fragmentomic patterns before final variant calling.
Figure 1: Integrated Workflow for CHIP Mitigation in ctDNA Analysis
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for CHIP-Resistant ctDNA Analysis
| Reagent/Category | Specific Examples | Function in CHIP Mitigation | Implementation Notes |
|---|---|---|---|
| Cell-Stabilizing Blood Collection Tubes | cfDNA BCT (Streck), PAXgene Blood ccfDNA (Qiagen) | Prevent leukocyte lysis and release of CHIP DNA [9]. | Allow blood storage for up to 7 days at room temperature. |
| Nucleic Acid Extraction Kits | QIAamp Circulating Nucleic Acid Kit (Qiagen), Cobas ccfDNA Sample Preparation Kit | High-quality ctDNA extraction with minimal contamination [9]. | Silica membrane methods yield more ctDNA than magnetic beads. |
| UMI Adapters | Safe-SeqS, Custom UMI adapters | Molecular barcoding for error correction and artifact removal [1]. | Must be incorporated before any amplification steps. |
| Targeted Enrichment Panels | CAPP-Seq, TEC-Seq, Custom panels excluding CHIP hotspots | Selective amplification of tumor-informed mutations [1]. | Avoid genes commonly mutated in CHIP unless tumor-relevant. |
| PCR Enzymes with Proofreading | High-fidelity polymerases | Reduce amplification errors that complicate low-VAF detection [1]. | Essential for accurate detection of true low-frequency variants. |
| Methylation Conversion Reagents | Bisulfite conversion kits | Enable methylation-based tissue origin analysis [53]. | Complementary approach to mutation-based detection. |
Advanced Integrated Approaches
Multi-Modal Sequencing Strategies
The most robust approach to CHIP mitigation involves integrating multiple complementary techniques. The CODEC (Concatenating Original Duplex for Error Correction) method, developed in 2023, represents a significant advancement by enabling 1000-fold higher accuracy than conventional NGS while using up to 100-fold fewer reads than duplex sequencing [1]. This method concatenates both strands of each DNA duplex for single NGS read pairs, allowing exceptional error correction that can distinguish true low-frequency variants.
For real-time PCR applications, which remain widely used for their rapid turnaround and accessibility, tumor-informed approaches are particularly valuable. By focusing amplification on mutations previously identified in tumor tissue, researchers can effectively bypass the CHIP interference problem. When designing PCR assays, researchers should prioritize variants that are unlikely to originate from CHIP based on published databases, and consider incorporating fragment length analysis through microfluidic or capillary electrophoresis systems to add an additional layer of discrimination.
Emerging Computational Frameworks
Artificial intelligence and machine learning frameworks are revolutionizing CHIP identification in ctDNA data. These systems can integrate multiple data types - including mutation profile, VAF, fragmentomics, and epigenetic patterns - to generate a composite likelihood score for CHIP origin [53]. Recent implementations have demonstrated the ability to achieve 0.002% mutant allelic fraction detection while maintaining high specificity by effectively filtering CHIP-derived noise [53].
These computational approaches are particularly powerful when applied to multi-analyte liquid biopsy data, where patterns across different biomarker classes (ctDNA, methylation, fragmentomics) provide orthogonal validation of variant origin. The implementation of these advanced computational methods requires specialized expertise but offers the most promising path forward for robust CHIP mitigation in clinical research settings.
Mitigating CHIP interference in ctDNA analysis requires a multi-faceted approach spanning careful experimental design, sophisticated wet-lab techniques, and advanced computational biology. No single method provides complete resolution, but through the strategic integration of paired granulocyte sequencing, tumor-informed approaches, UMIs, fragmentomics, and machine learning classification, researchers can significantly reduce false positives while maintaining sensitivity for true tumor-derived variants. As these technologies continue to evolve, the research community must prioritize standardization and validation of CHIP mitigation strategies to ensure the continued advancement of liquid biopsy applications in oncology research and drug development.
Circulating tumor DNA (ctDNA) has emerged as a transformative biomarker in precision oncology, enabling non-invasive assessment of tumor burden, genetic heterogeneity, and therapeutic response. However, a significant challenge impedes its broader clinical application: ctDNA can be present at exceptionally low concentrations, sometimes less than 0.1% of the total circulating cell-free DNA (cfDNA) or at attomolar concentrations, particularly in early-stage cancers and minimal residual disease (MRD) [3]. This low abundance necessitates the development of ultra-sensitive detection technologies.
The integration of nanomaterials with magnetic enrichment techniques represents a paradigm shift in addressing this sensitivity bottleneck. These hybrid approaches synergistically combine the efficient pre-concentration of target analytes with signal amplification strategies, pushing detection limits to previously unattainable levels. This technical guide explores the core principles, methodologies, and applications of these integrated platforms, framed within the context of advancing real-time PCR protocols for ctDNA research. For researchers and drug development professionals, mastering these techniques is crucial for unlocking the full potential of liquid biopsies in cancer diagnosis, monitoring, and treatment personalization.
Core Principles and Enabling Technologies
The Role of Magnetic Enrichment
Magnetic enrichment functions as a powerful pre-analytical concentration step, dramatically improving the signal-to-noise ratio by isolating rare targets from complex biological matrices like blood. The process typically involves magnetic nanoparticles (MNPs) functionalized with capture probes, such as antibodies, oligonucleotides, or other ligands specific to the target ctDNA or whole circulating tumor cells (CTCs) [55].
- Mechanism of Capture: The fundamental mechanism relies on superparamagnetic iron oxide nanoparticles (often Fe₃O₄), which can be magnetically separated but do not retain magnetism once the field is removed, preventing clumping. These MNPs are conjugated to capture elements via surface chemistry. In ctDNA detection, complementary DNA probes are used, while for CTC isolation, antibodies against epithelial cell adhesion molecule (EpCAM) are common [55] [56].
- Enrichment Efficiency: The capture efficiency (CE) is a critical performance metric, calculated as CE (%) = [Nc / (Nc + Ns)] × 100%, where Nc is the number of captured targets and Ns is the number remaining in the supernatant [57] [58]. Studies using polyethyleneimine-coated MNPs (PEI-MNPs) for bacterial capture demonstrated efficiencies exceeding 70%, highlighting the effectiveness of charge-based interactions for rapid enrichment [58].
Nanomaterials for Signal Amplification and Transduction
Following enrichment, nanomaterials play a pivotal role in transducing the binding event into a detectable and amplifiable signal, which is essential for achieving attomolar sensitivity.
- Electrochemical Biosensors: Nanomaterials like graphene, molybdenum disulfide (MoS₂), and gold-coated magnetic nanoparticles provide a high surface-area-to-volume ratio, facilitating label-free sensing. When ctDNA hybridization occurs on these surfaces, it induces measurable changes in impedance or current-voltage characteristics [3].
- Magnetic Nano-Electrode Systems: These hybrid systems represent a state-of-the-art integration. They use superparamagnetic Fe₃O₄–Au core–shell particles for both the enrichment of ctDNA and as a substrate for electrochemical readout. The system combines the sensitivity of PCR with rapid electrochemical detection, achieving signals in the attomolar range within minutes of PCR amplification [3].
- Redox Cycling Amplification: Advanced generator-collector electrode configurations, such as those used in evaporation-enhanced redox cycling (E2RC), create a continuous oxidation-reduction cycle of electrochemical labels. This significantly amplifies the signal per binding event, enabling the detection of very low target concentrations, as demonstrated with SARS-CoV-2 virion mimics [59].
Table 1: Key Performance Metrics of Integrated Platforms for Ultra-Sensitive Detection
| Technology Platform | Detection Limit | Key Nanomaterials Used | Assay Time | Target Analyte |
|---|---|---|---|---|
| Magnetic Nano-Electrode [3] | Attomolar (aM) | Fe₃O₄–Au core-shell nanoparticles | ~7 min post-PCR | ctDNA |
| Electrochemical Biosensor [3] | Attomolar (aM) | Graphene, MoS₂, DNA-conjugated Au-MNPs | ~20 minutes | ctDNA |
| MS-RT-qPCR [57] | 10² CFU/mL | Penicillin-functionalized Magnetic Beads | ~45 min enrichment | Group B Streptococcus |
| PEI-MNPs-mPCR [58] | 10¹ CFU/mL | Polyethyleneimine-coated MNPs | 10 min enrichment | Pathogenic Listeria |
Experimental Protocols for Integrated Detection
This section provides a detailed, actionable methodology for implementing a magnetic enrichment and nanomaterial-based detection system, adaptable for ctDNA research.
Protocol 1: Synthesis of Ligand-Functionalized Magnetic Nanoparticles
The following protocol for creating polyethyleneimine (PEI)-coated MNPs [58] can be adapted for nucleic acid capture by substituting PEI with specific DNA probes.
Reagents:
- Carboxylated magnetic beads (e.g., 180 nm, 10 mg/mL)
- N-Hydroxysulfosuccinimide sodium salt (NHSS)
- 1-(3-(dimethylamino) propyl)-3-ethylcarbodiimide hydrochloride (EDC)
- Coupling Ligand (e.g., Polyethyleneimine, PEI; or amino-modified DNA probe)
- Phosphate Buffered Saline (PBS, 0.01 M, pH 7.4)
Procedure:
- Activation: Wash 1 mL of carboxylated MNPs thrice with PBS using magnetic separation. Resuspend the beads in 10 mL of PBS containing 2.9 mg EDC and 3.26 mg NHSS. Activate the carboxyl groups by mixing on a vertical mixer for 1 hour at room temperature.
- Coupling: Remove the activation solution magnetically. Add 7.5 mg of PEI (or a calculated excess of DNA probe) to the activated MNPs. Allow the coupling reaction to proceed for 4 hours with gentle mixing.
- Purification and Storage: Separate the functionalized beads (PEI-MNPs or DNA-MNPs) and wash thoroughly with PBS to remove excess ligand. Resuspend the final product in 10 mL of PBS and store at 4°C.
Protocol 2: Magnetic Enrichment and RT-qPCR Detection
This protocol, inspired by methods for pathogen detection [57] [58], outlines a generic workflow for enriching and detecting low-abundance nucleic acid targets.
Sample Pre-treatment and Enrichment:
- Sample Preparation: Centrifuge 1 mL of plasma (or other sample matrix) at 9600×g for 5 min. Wash and resuspend the pellet or the target solution in 1 mL of sterile PBS.
- Capture Incubation: Add 100 μL of the functionalized MNPs (from Protocol 1) to 900 μL of the prepared sample. Incubate at 37°C with mixing (e.g., 144×g) for 45 minutes to allow target capture.
- Magnetic Separation: Apply an external magnetic field to the tube for 3-6 minutes. Carefully discard the supernatant.
- Wash: Wash the magnetic bead complex (now containing captured targets) twice with 1 mL of PBS.
Nucleic Acid Elution and RT-qPCR:
- Elution: Resuspend the MNP complex in 100 μL of sterile PBS or a suitable elution buffer. Extract the nucleic acid templates using an automated extractor (e.g., Smart32 instrument) or standard phenol-chloroform methods.
- Quantitative Real-Time PCR (RT-qPCR): Set up a 25 μL reaction mixture containing 2 μL Taq/UDG enzyme mix, 18 μL nucleic acid amplification reaction solution (containing Tris, KCl, MgCl₂, nucleotides, primers, and probe), and 5 μL of the extracted template DNA. Run the RT-qPCR with the following cycling conditions: 37°C for 5 min (enzyme treatment); 95°C for 5 min (pre-denaturation); 40 cycles of 95°C for 10 s and 60°C for 30-60 s (annealing/extension). Perform data analysis using the ΔΔCt method relative to a standard curve.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of these sensitive protocols relies on a carefully selected suite of reagents and materials. The following table details key components and their functions in the experimental workflow.
Table 2: Essential Research Reagents and Materials for Integrated Nanomaterial-Magnetic Assays
| Reagent/Material | Function/Application | Technical Notes |
|---|---|---|
| Carboxylated Magnetic Beads (e.g., 180 nm) [57] [58] | Core solid support for functionalization; enables magnetic separation. | Provides activated carboxyl groups for stable amide bond formation with amine-containing ligands. |
| EDC & NHSS [57] [58] | Carbodiimide crosslinkers for activating carboxyl groups on MNPs. | Critical for conjugating antibodies, DNA probes, or polymers (e.g., PEI) to the MNP surface. |
| Capture Ligands (e.g., DNA Probes, Antibodies, PEI) [57] [55] [58] | Provides specificity for target capture (ctDNA, CTCs). | Choice depends on target: DNA probes for ctDNA, Anti-EpCAM for CTCs, charged polymers for broad capture. |
| Gold-coated Magnetic Nanoparticles (Fe₃O₄–Au) [3] | Core-shell nanomaterial for electrochemical detection platforms. | Gold shell facilitates easy conjugation of thiolated DNA probes and enhances electrical conductivity. |
| 2x Specific Taq Master Mix [58] | Pre-mixed solution for efficient and specific PCR amplification. | Contains Taq polymerase, dNTPs, Mg²⁺, and optimized buffers for robust qPCR results. |
| Unique Molecular Identifiers (UMIs) [1] | Short nucleotide barcodes for error correction in NGS. | Tag individual DNA molecules pre-amplification to distinguish true mutations from PCR/sequencing errors. |
Clinical Applications and Validation in ctDNA Research
The drive for attomolar sensitivity is primarily motivated by critical applications in oncology where detecting the faintest molecular signals can dramatically impact patient management.
- Minimal Residual Disease (MRD) and Recurrence Monitoring: The most significant application is in the detection of MRD following curative-intent surgery. Ultrasensitive ctDNA assays can identify molecular relapse months to a year before clinical or radiographic recurrence. In breast cancer, SV-based ctDNA assays have detected MRD with a median variant allele frequency of 0.15%, with some cases as low as 0.0011% [3] [1]. This lead time creates a potential window for early therapeutic intervention.
- Real-Time Treatment Monitoring: Dynamic changes in ctDNA levels can serve as a rapid and accurate indicator of treatment response. A decline in ctDNA concentration often precedes and more accurately predicts radiographic tumor shrinkage than standard imaging. Conversely, the emergence of resistance mutations can be detected in plasma weeks before clinical progression, allowing for timely treatment adaptation [3] [1].
- Overcoming Technical Hurdles in ctDNA Analysis: The integration of magnetic enrichment directly addresses several key challenges in ctDNA analysis. The low abundance of ctDNA, its short fragment size (90-150 bp), and the presence of a massive background of wild-type cfDNA create a significant detection hurdle. Magnetic pre-concentration enriches the mutant allele fraction, making subsequent analysis by digital PCR or error-corrected NGS more reliable and sensitive [3] [1]. Furthermore, specialized library preparation methods that enrich for short cfDNA fragments can work synergistically with these enrichment techniques to further boost the detection of tumor-derived DNA [3].
The integration of magnetic enrichment strategies with functional nanomaterials has decisively pushed the detection limits of bioanalytical assays into the attomolar regime, creating new possibilities for basic research and clinical diagnostics. For ctDNA analysis, this technological evolution is paving the way for the routine detection of MRD and the genuine realization of real-time, non-invasive tumor monitoring.
Future developments in this field are likely to focus on the full automation and miniaturization of these workflows into integrated microfluidic point-of-care devices, leveraging the unique properties of nanomaterials for both capture and signal transduction [3]. Furthermore, the combination of multi-omic approaches—analyzing ctDNA mutations, methylation patterns, and fragmentomics simultaneously—within a single, enriched sample will provide a more comprehensive picture of the tumor's biology from a simple blood draw [3] [1]. As these ultrasensitive platforms continue to mature and undergo rigorous clinical validation, they are poised to become indispensable tools in the oncologist's arsenal, fundamentally advancing the goals of precision oncology.
Benchmarking PCR Performance Against NGS and Establishing Clinical Validity
Circulating tumor DNA (ctDNA) analysis has emerged as a revolutionary non-invasive tool in oncology, enabling real-time monitoring of tumor dynamics, treatment response, and resistance mechanisms. The effective analysis of ctDNA presents significant technical challenges due to its extremely low concentration in plasma, often constituting less than 0.1% of total cell-free DNA against a background of wild-type DNA [60]. This analytical landscape is dominated by three principal technologies: quantitative PCR (qPCR), droplet digital PCR (dPCR), and next-generation sequencing (NGS). Each method offers distinct advantages and limitations in sensitivity, specificity, multiplexing capability, and discovery power. qPCR provides a familiar, accessible workflow for targeted analysis but struggles with very low variant allele frequencies. dPCR achieves exceptional sensitivity for detecting predefined mutations through absolute quantification. NGS enables comprehensive profiling of hundreds to thousands of genomic regions simultaneously but traditionally at lower sensitivity than dPCR. This whitepaper provides a detailed technical comparison of these platforms, focusing on their analytical sensitivity and specificity within the context of ctDNA research, to guide researchers and drug development professionals in selecting appropriate methodologies for their experimental and clinical objectives.
Performance Metrics: Quantitative Comparison of Platforms
The selection of an appropriate detection platform requires careful consideration of performance characteristics relative to experimental needs. The following tables summarize key comparative metrics and clinical performance data.
Table 1: Direct Comparison of Technical Capabilities for ctDNA Analysis
| Parameter | qPCR/ARMS-PCR | Droplet Digital PCR (dPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Theoretical Limit of Detection (LOD) | 0.1% VAF [60] | 0.003%–0.01% VAF [61] [62] | 0.1%–0.5% VAF (standard); <0.1% (with barcodes) [63] [60] |
| Quantification | Relative (Cq values) | Absolute (copies/μL) | Relative (Variant Allele Frequency) |
| Multiplexing Capability | Moderate (up to 4-6 plex in one well) | Low (typically 1-2 plex, up to 4 with optimization) | Very High (hundreds to thousands of targets) |
| Discovery Power | Low (only known, predefined mutations) | Low (only known, predefined mutations) | High (detection of known and novel variants) [64] |
| Best Application | Validating known mutations, expression profiling | Ultrasensitive quantification of low-frequency variants, residual disease monitoring | Comprehensive genomic profiling, novel variant discovery, tumor mutation burden [64] [63] |
| Cost per Sample | Low | Medium (higher for rare mutations) [62] | High (but low cost per base) |
| Throughput | High (96-384 well plates) | Medium | Very High (multiplexed samples per run) |
Table 2: Clinical Performance in Cancer Studies
| Cancer Type | Technology | Reported Sensitivity | Reported Specificity | Concordance with Tissue | Source |
|---|---|---|---|---|---|
| Metastatic NSCLC | 101-gene NGS Panel (ctDNA) | 97.5% (by variant); SNVs: 98.3%; InDels: 100% | 99.9% | 72.2% (for targetable variants) | [63] |
| Localized Rectal Cancer | ddPCR (pre-therapy plasma) | 58.5% detection rate | N/A | N/A | [62] |
| Localized Rectal Cancer | NGS Panel (pre-therapy plasma) | 36.6% detection rate | N/A | N/A | [62] |
| Non-Metastatic Gastric Cancer | ddPCR (baseline) | 21% | N/A | N/A | [65] |
Experimental Protocols for ctDNA Analysis
Ultrasensitive qPCR for KRAS Mutations (PNB-qPCR)
The PNB-qPCR (Pooled, Nested, WT-Blocking qPCR) protocol represents a significant enhancement of traditional qPCR for detecting ultra-rare mutations in ctDNA [61].
Methodology:
- First-Round PCR (Enrichment): The extracted cfDNA is subjected to a first amplification round using primers flanking the KRAS exon 2 region. This reaction incorporates wild-type (WT) specific blocking primers (e.g., peptide nucleic acid clamps or LNA oligonucleotides) that hybridize preferentially to the WT sequence, suppressing its amplification and effectively enriching the sample for mutant alleles.
- Pooling: To reduce variance, multiple (e.g., five) first-round PCR reactions are performed per sample.
- Second-Round qPCR (Detection): Products from the multiple first-round reactions are pooled and used as a template for a second, quantitative PCR. This round employs mutation-specific ARMS primers and short, locked nucleic acid (LNA) probes to further enhance specificity and amplify short amplicons suitable for fragmented ctDNA.
Performance: This nested, blocker-based approach drastically reduces background noise, achieving a limit of detection (LOD) as low as 0.003% (1 mutant copy in 30,000 WT copies) and a limit of quantification (LOQ) of 6.25 copies, significantly outperforming standard qPCR [61].
Targeted NGS Panel for Solid Tumors
A validated protocol for a hybridization-capture-based targeted NGS panel demonstrates the workflow for comprehensive mutation profiling [66].
Methodology:
- Sample Input & Library Preparation: A minimum of 50 ng of DNA extracted from FFPE tissue or plasma is required. Libraries are prepared using an automated system (e.g., MGI SP-100RS) to minimize human error and contamination risk. DNA is end-repaired, phosphorylated, dA-tailed, and adapter-ligated.
- Target Enrichment: Biotinylated oligonucleotide probes designed to capture the exonic regions of 61 cancer-associated genes (e.g., KRAS, EGFR, TP53, PIK3CA) are hybridized to the library. The target-probe complexes are isolated using streptavidin-coated magnetic beads.
- Sequencing: Enriched libraries are sequenced on a platform such as the MGI DNBSEQ-G50RS, which uses combinatorial Probe-Anchor Synthesis (cPAS) technology. A median coverage of >1500x is recommended for robust detection.
- Bioinformatic Analysis: Sequencing data is processed through a customized pipeline (e.g., Sophia DDM software) that includes alignment to a reference genome (hg19) and variant calling using tools like VarDict for SNVs and InDels. Molecular barcodes (unique molecular identifiers, UMIs) are critical for correcting PCR amplification errors and achieving high sensitivity.
Performance: This assay demonstrated a sensitivity of 97.14% and a specificity of 99.99% for variants at a limit of detection of 2.9% VAF, with a rapid turnaround time of 4 days [66].
ddPCR for Mutation Detection in Rectal Cancer
A typical ddPCR protocol for a tumor-informed ctDNA analysis is as follows [62]:
Methodology:
- Tumor Sequencing: First, the primary tumor tissue is sequenced using a panel (e.g., Ion AmpliSeq Cancer Hotspot Panel v2) to identify patient-specific somatic mutations.
- Probe Design: Based on the NGS results, one or two predesigned, mutation-specific fluorescent probe assays for ddPCR are selected to target the mutations with the highest variant allele frequency in the tumor.
- Partitioning and PCR: Extracted cfDNA from patient plasma is partitioned into ~20,000 nanoliter-sized droplets, creating individual reaction chambers. A conventional PCR is then run to endpoint within the droplets.
- Droplet Reading: Each droplet is analyzed in a flow cytometer to read the fluorescence signal. The fraction of positive (mutant) droplets against the total number of analyzed droplets allows for the absolute quantification of the mutant allele frequency without the need for a standard curve.
Performance: In a study on localized rectal cancer, ddPCR showed a significantly higher detection rate (58.5%) in pre-therapy plasma compared to an NGS panel (36.6%), highlighting its superior sensitivity for low-frequency variant detection in a clinical workflow [62].
Technology Selection Workflow
The following diagram illustrates the decision-making process for selecting the most appropriate technology based on research goals and practical constraints.
The Scientist's Toolkit: Essential Reagents and Materials
Successful ctDNA analysis relies on a suite of specialized reagents and kits. The following table details key components for establishing a robust workflow.
Table 3: Essential Research Reagents for ctDNA Analysis
| Reagent / Kit | Function | Application Notes |
|---|---|---|
| Streck Cell-Free DNA BCT Tubes | Stabilizes blood samples to prevent release of genomic DNA from white blood cells, preserving the native cfDNA profile. | Critical for pre-analytical phase; ensures accurate VAF measurement by preventing dilution of ctDNA background [62]. |
| QIAamp Circulating Nucleic Acid Kit | Efficient extraction of low-concentration cfDNA from plasma. | Optimized for short, fragmented DNA; maximizes yield and purity for downstream applications [63]. |
| Ion AmpliSeq Cancer Hotspot Panel v2 | Targeted NGS panel for identifying somatic mutations in hotspot regions of 50 oncogenes and tumor suppressor genes. | Used for initial tumor genotyping to inform selection of patient-specific mutations for dPCR tracking [62]. |
| TaqMan Gene Expression Assays / ddPCR Mutation Assays | Sequence-specific fluorescent probes for detecting and quantifying known mutations or gene expression levels via qPCR/ddPCR. | Ideal for validating NGS findings or for high-throughput, targeted screening of a predefined marker set [67]. |
| Hybridization Capture-Based NGS Panels | Customizable panels (e.g., 61-101 gene oncopanels) using biotinylated probes to enrich for target genes prior to sequencing. | Enables comprehensive profiling of a wide range of mutations, fusions, and copy number variations from limited input [63] [66]. |
| Molecular Barcodes (UMIs) | Short, unique DNA sequences ligated to each DNA fragment prior to PCR amplification in NGS library prep. | Allows bioinformatic correction of PCR errors and deduplication, significantly improving sequencing accuracy and sensitivity for low-frequency variants [60]. |
The choice between dPCR, NGS, and qPCR is not a matter of identifying a single superior technology, but rather of aligning platform capabilities with specific research questions. dPCR stands out for its unparalleled sensitivity and absolute quantification when tracking one or a few known mutations, making it ideal for minimal residual disease detection and therapy monitoring. NGS offers unparalleled breadth, enabling hypothesis-free discovery, comprehensive genomic profiling, and the detection of novel variants across hundreds of genes, albeit at a higher cost and with greater computational demands. qPCR remains a valuable, cost-effective workhorse for high-throughput validation of a moderate number of targets and for labs where equipment accessibility is a primary concern. As the field of liquid biopsy continues to evolve, the integration of these complementary technologies—using NGS for broad discovery and dPCR for deep, sensitive tracking—will provide the most powerful approach for advancing cancer research and personalized drug development.
Assay validation is a critical process in ensuring that diagnostic and research tools produce reliable, accurate, and consistent results. For circulating tumor DNA (ctDNA) research using real-time PCR technologies, defining key validation parameters is particularly crucial due to the analytical challenges inherent in detecting low-frequency variants against a background of wild-type DNA. This technical guide provides an in-depth examination of three core validation parameters—Limit of Detection (LOD), Precision, and Reproducibility—within the context of real-time PCR protocols for ctDNA analysis. The quantification of tumor-derived DNA fragments in patient blood samples enables non-invasive cancer monitoring, treatment selection, and disease surveillance [68] [69]. However, the clinical utility of these assays depends entirely on rigorous validation demonstrating their ability to consistently detect low-abundance targets amid technical and biological variability [70] [71].
Core Principles of ctDNA and Real-Time PCR
Biological and Technical Foundations of ctDNA Analysis
Circulating tumor DNA (ctDNA) represents the fraction of cell-free DNA in blood that originates from tumor cells. Key characteristics make it particularly challenging to detect and quantify:
- Low Abundance: ctDNA typically constitutes less than 1% of total cell-free DNA (cfDNA) in plasma, with concentrations ranging from 1-10 ng/mL in asymptomatic individuals [68] [69].
- Short Half-Life: ctDNA is rapidly cleared from circulation with a half-life of 16 minutes to 2.5 hours, enabling real-time monitoring of disease dynamics [68] [69].
- Pre-analytical Variables: Sample collection tubes, processing methods, plasma storage conditions, and centrifugation protocols significantly impact ctDNA yield and quality [68].
- Fragment Characteristics: ctDNA fragments typically range from 70-200 base pairs, shorter than non-tumor derived cfDNA [69].
These characteristics necessitate exceptionally sensitive detection methods capable of identifying rare variants while maintaining specificity against a high background of wild-type DNA.
Real-Time PCR Fundamentals in ctDNA Context
Real-time PCR (quantitative PCR or qPCR) provides the analytical foundation for many ctDNA detection assays. Understanding its fundamental principles is essential for proper validation:
- Threshold Cycle (Ct): The fractional PCR cycle number at which reporter fluorescence exceeds background levels. Lower Ct values indicate higher starting target concentrations [51] [72].
- Amplification Efficiency: The rate at which target sequences are amplified during the exponential phase. Optimal validation requires efficiency between 90-110% [51].
- Dynamic Range: The range of template concentrations over which accurate quantification occurs, typically spanning 3-5 logs for proper validation [51].
- Probe Chemistry: Hydrolysis probes (e.g., TaqMan) provide sequence-specific detection crucial for distinguishing mutant from wild-type alleles in ctDNA [72].
Table 1: Key Considerations for ctDNA Analysis Using Real-Time PCR
| Parameter | Challenge in ctDNA Context | Impact on Validation |
|---|---|---|
| Input Material | Low ctDNA fraction requires high sensitivity | LOD must be established at low variant allele frequencies |
| Sample Volume | Limited ctDNA concentration per sample | Input amount affects all validation parameters |
| Background DNA | High wild-type DNA background | Specificity validation critical to minimize false positives |
| Pre-analytical Factors | Collection tubes, processing time affect yield | Protocol standardization essential for reproducibility |
Defining and Establishing Validation Parameters
Limit of Detection (LOD)
The Limit of Detection (LOD) represents the lowest concentration of an analyte that can be reliably distinguished from zero. For ctDNA assays, this translates to the minimum variant allele frequency (VAF) that can be consistently detected with high confidence.
Experimental Approach for LOD Determination:
- Dilution Series Preparation: Create reference samples with known VAFs using synthetic mutant DNA spiked into wild-type background at concentrations spanning the expected detection limit (e.g., 2.5%, 1%, 0.5%, 0.1%, 0.05%) [71].
- Replicate Testing: Analyze each dilution level with a minimum of 20-30 replicates to establish statistical confidence [70].
- Probit Analysis: Apply statistical models to determine the concentration at which 95% of positive samples are detected [70].
- Matrix Effects: Validate LOD in relevant biological matrices (e.g., plasma) rather than just purified DNA to account for potential inhibitors [70].
Factors Influencing LOD in ctDNA Assays:
- Input DNA Mass: Lower inputs (<20 ng) demonstrate reduced sensitivity compared to higher inputs (>50 ng) [71].
- Variant Type: Single nucleotide variants (SNVs) are typically detected at lower VAFs than insertions/deletions (InDels) or structural variants [71].
- Technical Platforms: Digital PCR methods generally achieve lower LOD (0.02%-0.1%) than standard real-time PCR (approximately 10%) [69].
Precision
Precision describes the closeness of agreement between independent measurements obtained under specified conditions. For ctDNA assays, precision validation must address multiple levels of variability:
Types of Precision to Evaluate:
- Repeatability (Intra-assay Precision): Agreement under the same operating conditions over a short interval.
Intermediate Precision (Inter-assay Precision): Agreement under varying conditions within the same laboratory.
- Experimental Design: Test the same samples across different days, operators, or instruments.
- Acceptance Criterion: ≤0.5 cycle difference in mean Ct values between runs [70].
Reproducibility (Inter-laboratory Precision): Agreement between results from different laboratories.
- Experimental Design: Collaborative study using identical protocols and reference materials across sites.
- Acceptance Criterion: Statistically equivalent quantitative results (p>0.05) between laboratories [71].
Table 2: Precision Requirements for ctDNA Detection at Different VAF Levels
| VAF Level | Acceptable SD for Ct Values | Minimum Replicates | Key Influencing Factors |
|---|---|---|---|
| >5% VAF | ≤0.33 | 10 | Pipetting accuracy, reaction mix homogeneity |
| 1-5% VAF | ≤0.25 | 20 | Template distribution, amplification efficiency |
| 0.1-1% VAF | ≤0.167 | 30 | Stochastic sampling, partition efficiency |
| <0.1% VAF | ≤0.125 | 40 | Poisson distribution, molecular barcoding efficiency |
Reproducibility
Reproducibility extends beyond precision to encompass the consistency of results when analytical conditions vary, including different reagents, operators, instruments, and laboratories. In genomics, this includes both "methods reproducibility" (same protocols and data) and "genomic reproducibility" (consistent bioinformatics results across technical replicates) [73].
Components of Reproducibility Validation:
- Wet-Lab Reproducibility: Consistency in pre-analytical and analytical phases.
- Sample Collection: Use standardized blood collection tubes (e.g., cell-stabilization tubes for delayed processing) [68].
- Nucleic Acid Extraction: Implement double-centrifugation protocols (800-1600g followed by 10,000-20,000g) to minimize cellular DNA contamination [68].
- Amplification Conditions: Use standardized master mixes with consistent ROX reference dye concentrations to minimize Ct value variations [51].
- Bioinformatics Reproducibility: Consistency in computational analysis.
- Variant Calling: Implement standardized pipelines with defined quality thresholds [73].
- Stochastic Algorithms: Use fixed random seeds for tools with probabilistic components to ensure consistent output [73].
- Data Processing: Apply consistent read alignment parameters and quality filters across analyses [73].
Challenges Specific to ctDNA Reproducibility:
- Tumor Heterogeneity: Spatial and temporal variations in tumor genetics create intrinsic biological variability [68].
- Clonal Hematopoiesis: Age-related expansion of hematopoietic clones with mutations in genes like DNMT3A, TET2, and ASXL1 can create false-positive results [69].
- Analytical Variation: One study comparing ctDNA assays found technical discordance responsible for 68% of all unique variants identified [71].
Experimental Protocols for Validation
Comprehensive LOD Determination Protocol
Materials and Reagents:
- Synthetic reference standards with known mutations
- Wild-type human genomic DNA
- Qubit dsDNA HS Assay Kit or similar quantification method
- Validated real-time PCR master mix with probe chemistry
- Appropriate positive and negative controls
Procedure:
- Prepare a stock solution of mutant DNA at precisely quantified concentration.
- Create a dilution series in wild-type DNA background to generate VAFs of 5%, 2.5%, 1%, 0.5%, 0.25%, 0.1%, and 0.05%.
- For each VAF level, prepare a minimum of 20 replicates using the exact sample volume specified in the test protocol.
- Process all samples through the complete workflow including extraction (if applicable), amplification, and analysis.
- Record detection rates and quantitative values (Ct or copies/μL) for each replicate.
- Apply probit analysis or similar statistical method to determine the VAF at which ≥95% of replicates test positive.
- Confirm the determined LOD with an additional 20-30 replicates at that specific VAF.
Acceptance Criteria:
- ≥95% detection rate at the established LOD
- Coefficient of variation <25% for quantitative measurements at 5x LOD
- No false positives in wild-type-only controls
Precision Assessment Protocol
Materials and Reagents:
- Reference material with known VAF near the clinical decision point
- Validated assay reagents from multiple lots
- Multiple instruments of the same model (if available)
- Documentation forms for recording operator, date/time, reagent lots
Procedure:
- Repeatability Assessment:
- Prepare 20 replicates of the reference material at medium VAF (1-2%)
- Process all replicates in a single run by one operator using one reagent lot
- Calculate mean, standard deviation, and coefficient of variation for quantitative results
Intermediate Precision Assessment:
- Test the same reference material across 5-10 separate runs over different days
- Include at least two different operators and two different reagent lots
- Use the same instrumentation or multiple instruments of the same model
- Perform ANOVA analysis to partition variance components
Data Analysis:
- Calculate within-run, between-run, and total standard deviations
- Determine total allowable imprecision based on biological variation of the analyte
- Compare actual precision to predefined acceptance criteria
Acceptance Criteria:
- Repeatability: CV ≤10% for VAF >1%, ≤15% for VAF 0.1-1%
- Intermediate precision: Total CV ≤15% for VAF >1%, ≤20% for VAF 0.1-1%
- No statistically significant differences between operators or reagent lots (p>0.05)
Reproducibility Evaluation Protocol
Materials and Reagents:
- Commutable reference materials (synthetic cfDNA or contrived plasma)
- Standardized blood collection tubes (e.g., Streck, PAXgene)
- Detailed standard operating procedures for all pre-analytical steps
- Bioinformatics pipelines with version-controlled code
Procedure:
- Wet-Lab Reproducibility:
- Distribute identical reference materials to multiple participating laboratories
- Process samples according to standardized SOPs for:
- Blood collection and plasma separation
- cfDNA extraction and quantification
- Real-time PCR setup and cycling conditions
- Collect raw data (Ct values) and extracted nucleic acids for central analysis
Bioinformatics Reproducibility:
- Provide identical sequencing data or raw fluorescence files to multiple analysts
- Apply standardized but independently implemented analysis pipelines
- Compare variant calls and quantification results
Statistical Analysis:
- Calculate intraclass correlation coefficients for quantitative results
- Determine Cohen's kappa for qualitative (positive/negative) agreement
- Use Bland-Altman plots to assess bias between sites or methods
Acceptance Criteria:
- Interlaboratory CV ≤20% for quantitative measurements
- Qualitative agreement ≥95% with kappa statistic ≥0.8
- No systematic bias between sites or methodologies
Visualization of Validation Workflows and Relationships
ctDNA Assay Validation Workflow
Diagram 1: Comprehensive assay validation workflow showing the relationship between analytical parameters and their outputs in the context of ctDNA detection.
Factors Influencing Reproducibility in ctDNA Analysis
Diagram 2: Key factors affecting reproducibility in ctDNA analysis, spanning pre-analytical, analytical, bioinformatics, and biological domains.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for ctDNA Assay Validation
| Reagent Category | Specific Examples | Function in Validation | Key Considerations |
|---|---|---|---|
| Blood Collection Tubes | Streck Cell-Free DNA BCT, PAXgene Blood ccfDNA Tubes, EDTA tubes | Cellular stabilization and preservation of cfDNA | Stabilization tubes allow processing delays up to 7 days; EDTA requires processing within 6 hours [68] |
| Nucleic Acid Extraction Kits | QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit | Isolation of high-quality cfDNA from plasma | Evaluate extraction efficiency using spike-in controls; aim for >60% recovery [68] |
| Quantification Assays | Qubit dsDNA HS Assay, Bioanalyzer High Sensitivity DNA Kit, TapeStation | Accurate measurement of cfDNA concentration and size distribution | Fluorometric methods preferred over spectrophotometry for fragmented DNA [68] |
| PCR Master Mixes | TaqMan Fast Advanced Master Mix, ddPCR Supermix for Probes | Enzymatic amplification with fluorescent detection | Consistent ROX dye concentration critical for Ct value reproducibility [51] |
| Reference Materials | Seraseq ctDNA Reference Materials, Horizon Multiplex I cfDNA Reference | Positive controls with known VAF for LOD determination | Commutable materials that mimic patient sample behavior essential [71] |
| Bioinformatics Tools | BWA-MEM, Bowtie2, GATK, custom variant callers | Read alignment, variant calling, and quantification | Version control and parameter documentation critical for reproducibility [73] |
Robust validation of real-time PCR assays for ctDNA detection requires meticulous attention to Limit of Detection, Precision, and Reproducibility parameters. The complex nature of ctDNA—with its low abundance, short half-life, and biological variability—demands rigorous experimental designs that address both analytical and biological challenges. By implementing comprehensive validation protocols that include appropriate statistical analyses, standardized materials, and systematic evaluation of variability sources, researchers can ensure their ctDNA assays generate reliable data suitable for both research and clinical applications. As the field advances, continued refinement of validation standards will be essential for realizing the full potential of liquid biopsy approaches in oncology research and patient care.
The standardization of tumor response assessment via Response Evaluation Criteria in Solid Tumors (RECIST) has fundamentally transformed oncology drug development. This whitepaper examines the complex correlation between RECIST-defined endpoints—particularly objective response rate (ORR)—and clinically significant survival outcomes such as progression-free survival (PFS) and overall survival (OS). Within the emerging paradigm of circulating tumor DNA (ctDNA) research, we explore how traditional radiographic assessments intersect with novel liquid biopsy methodologies. Our analysis reveals that while RECIST provides crucial standardized response assessment, its relationship with survival outcomes is nuanced and significantly modulated by factors such as tumor burden, treatment line, and therapeutic mechanism. Understanding these relationships is paramount for researchers and drug development professionals utilizing real-time PCR protocols for ctDNA analysis in clinical trials.
The Response Evaluation Criteria in Solid Tumors (RECIST) provides a standardized framework for assessing tumor response to therapy in clinical trials, serving as a critical tool for objective evaluation of treatment efficacy [74] [75]. First introduced in 2000 and revised to RECIST 1.1 in 2009, these criteria establish precise definitions for classifying tumor response into four categories: complete response (CR), partial response (PR), stable disease (SD), and progressive disease (PD) [75]. The implementation of RECIST is particularly crucial in oncology research because inaccuracies in adherence can jeopardize patient treatment courses, compromise data integrity, negatively impact study endpoint analysis, and ultimately influence future oncology standards of care [74].
RECIST 1.1 employs unidimensional measurements of target lesions, reducing the number of lesions assessed compared to earlier systems and providing clarified guidelines for classifying lymph nodes and defining disease progression [76] [75]. The criteria specify that a partial response corresponds to at least a 30% decrease in the sum of diameters of target lesions, while progressive disease requires at least a 20% increase in the sum of diameters [76]. These thresholds originated from historical studies dating back to 1976 that evaluated measurement error in tumor assessment, highlighting the empirical foundation of these now-standardized cutoffs [76].
For clinical trials, RECIST implementation requires careful planning and standardization. Best practices include assessing protocol-specific requirements before trial activation, assigning designated radiologists trained in RECIST criteria, establishing standard processes for solid tumor evaluations, and clearly delegating RECIST-related tasks on study-specific delegation logs [74]. The criteria have become the gold standard for evaluating response in solid tumors, with specialized imaging Contract Research Organizations (CROs) playing an increasingly important role in ensuring consistent image interpretation and minimizing reader variability [75].
Correlation Between RECIST-Defined Response and Survival Outcomes
Quantitative Relationship Between ORR and Survival Metrics
The relationship between Objective Response Rate (ORR) and survival outcomes presents a complex picture in oncology trials. A comprehensive analysis of 68 immunotherapy trials submitted to the FDA revealed varying degrees of correlation between ORR and survival endpoints across different treatment regimens [77]. The overall regression analysis demonstrated a moderate correlation between ORR and PFS (R² = 0.503), indicating that ORR can serve as a useful predictor of short-term disease control. However, the correlation between ORR and OS was notably weaker (R² = 0.157), suggesting that ORR alone may not reliably predict long-term survival outcomes [77].
Table 1: Correlation Between ORR and Survival Outcomes Across Immunotherapy Regimens
| Treatment Category | ORR-PFS Correlation (R²) | ORR-OS Correlation (R²) | Clinical Implications |
|---|---|---|---|
| IO + IO | 0.495 (first-line) | 0.091 (first-line) | ORR predicts PFS better in first-line setting |
| Anti-PD-(L)1 monotherapy | 0.360 (later-line) | Weaker (later-line) | Reduced predictive value in later treatment lines |
| Anti-PD-(L)1 + Chemotherapy | Moderate | Weak | ORR not a reliable OS predictor in combinations |
| Anti-PD-(L)1 + CTLA-4 | Moderate | Weak | Disconnect between response and survival |
| Anti-PD-(L)1 + TKI | Moderate | Weak | Response not predictive of long-term benefit |
The correlation between ORR and survival outcomes demonstrates significant dependence on treatment line. For first-line treatments, the correlation between ORR and PFS shows a stronger relationship (R² = 0.495) compared to later-line treatments (R² = 0.360) [77]. This pattern underscores the declining utility of ORR as a predictor of survival benefits in advanced disease settings and highlights the context-dependent nature of this relationship across the treatment continuum.
Limitations of RECIST as a Surrogate Endpoint
While RECIST-defined endpoints provide valuable intermediate markers of treatment activity, several limitations affect their reliability as surrogates for overall survival:
Mechanistic Disconnects: The distinct mechanisms of action of immunotherapies can lead to delayed responses and atypical patterns of tumor regression, challenging the conventional reliance on ORR as a predictor of long-term benefit [77].
Tumor Burden Impact: Variations in baseline tumor burden between study arms can create discrepancies where improvements in RECIST-based endpoints do not translate to OS benefits, particularly in trials with small samples or non-randomized designs [78].
Atypical Response Patterns: Immunotherapies may produce pseudoprogression or dissociated responses that conventional RECIST criteria may misinterpret, leading to the development of modified criteria such as iRECIST for immunotherapy trials [77].
These limitations have significant implications for drug development, particularly in early-phase trials where ORR often serves as a primary endpoint for accelerated approval. The FDA has granted several immunotherapy regimens accelerated approval based on significant ORR improvements, despite uncertain effects on overall survival [77].
Tumor Burden as a Modulating Factor
Prognostic and Predictive Value of Tumor Burden
Tumor burden, measured as the sum of the longest diameters of target lesions according to RECIST 1.1, has emerged as a significant factor modulating clinical outcomes across multiple cancer types [78] [79]. Research demonstrates that baseline tumor burden serves primarily as a histology-agnostic prognostic factor rather than an immunotherapy-specific predictive biomarker [78]. Individual patient-level analysis of eight prospective trials revealed that low tumor burden was consistently associated with improved outcomes irrespective of treatment class, showing a dose-dependent effect across cancer types [78].
Table 2: Impact of Tumor Burden on Treatment Outcomes Across Cancer Types
| Cancer Type | ORR with Low TB | ORR with High TB | OS Impact | Treatment Class |
|---|---|---|---|---|
| NSCLC | Higher | Lower | Significant OS improvement with low TB | Atezolizumab & Conventional Therapy |
| HCC | Higher | Lower | Significant OS improvement with low TB | Atezolizumab |
| Bladder Cancer | Higher | Lower | Significant OS improvement with low TB | Atezolizumab & Conventional Therapy |
| RCC | Higher | Lower | Significant OS improvement with low TB | Atezolizumab & Conventional Therapy |
In advanced non-small cell lung cancer (NSCLC), patients with low tumor burden receiving chemoimmunotherapy demonstrated significantly longer progression-free survival (11.60 vs. 7.20 months, HR = 0.625, p = 0.004) and overall survival (28.77 vs. 20.10 months, HR = 0.683, p = 0.020) compared to those with high tumor burden [79]. Conversely, in chemotherapy-only arms, no significant survival differences were observed based on tumor burden levels, suggesting that tumor burden may function as a predictive biomarker specifically for immunotherapy-based regimens rather than a general prognostic factor [79].
Tumor Burden and RECIST Assessment Challenges
The interaction between tumor burden and RECIST assessment presents several methodological challenges:
Measurement Limitations: RECIST measurements as a surrogate for total tumor burden may underestimate disease extent in some patients, particularly those with predominantly non-measurable or diffusely distributed lesions [78].
Stratification Imperative: The significant impact of tumor burden on outcomes highlights the importance of stratification by tumor burden in clinical trial design, especially in diseases with highly variable tumor burden distributions [78].
Endpoint Discordance: Tumor burden may confound the interpretation of early-phase trials when results demonstrate improvements in RECIST-based surrogate endpoints but not OS due to underlying imbalances in tumor burden between study arms [78].
An exception to the consistent association between high tumor burden and poor outcomes was observed in hepatocellular carcinoma (HCC) treated with sorafenib, where high tumor burden was paradoxically associated with improved PFS but worse OS, potentially indicating a sorafenib-specific antitumor mechanism more effective against voluminous disease [78].
Methodologies for Correlative Studies
RECIST Implementation Protocols
Proper implementation of RECIST criteria in clinical trials requires standardized methodologies to ensure consistent and accurate response assessment:
Radiologist Training: Designated radiologists must receive specialized training in RECIST criteria interpretation, with ongoing competency assessments to maintain skill levels [74].
Baseline Lesion Selection: At baseline, designated radiologists and treating principal investigators should agree on specific lesions to follow for each subject enrolled in trials involving RECIST criteria [74].
Source Documentation: RECIST source documents must be established prior to trial activation and utilized consistently throughout the trial, saved electronically and accessible to appropriate study team members [74].
Quality Assurance: Implementation of standardized reading processes with centralized image review helps minimize inter- and intra-reader variability and reduces potential for bias and imaging-related queries [75].
For clinical trials, the minimum size for measurable lesions is defined as ≥10 mm on CT scans or ≥20 mm on magnetic resonance imaging, with a maximum of five measurable lesions (up to two per organ) designated as target lesions for follow-up assessment [76] [75].
Liquid Biopsy-RECIST (LB-RECIST) Protocol
The emergence of liquid biopsy methodologies has created new opportunities for complementary response assessment:
Sample Collection: Collect blood samples at baseline (pre-treatment) and at week 8 of treatment using cell-free DNA collection tubes [80].
ctDNA Extraction and Analysis: Extract circulating tumor DNA (ctDNA) from plasma and analyze using next-generation sequencing (Oncomine Colon cfDNA Assay; Ion Torrent S5) [80].
Molecular Response Categorization: Calculate aggregate variant allele frequency (aggVAF) as the sum of all detected variant allele frequencies in a sample. Categorize molecular response using LB-RECIST criteria:
- ctDNA Complete Response (CCR): Complete clearance of ctDNA
- ctDNA Partial Response (CPR): ≥50% decrease in aggVAF
- ctDNA Progressive Disease (CPD): ≥50% increase in aggVAF [80]
Correlation with Outcomes: Associate LB-RECIST categories with radiographic response and survival outcomes (PFS and OS). Patients with CCR demonstrate superior outcomes (median OS 41.8 months; median PFS not reached) compared to CPR/CPD (median OS 16.4-25.5 months; median PFS 11.9-12.7 months) [80].
Diagram 1: LB-RECIST and RECIST 1.1 Integrated Assessment Workflow
Computational Prediction Models
Advanced computational approaches enable survival prediction using RECIST-derived data:
Virtual Patient Linkage: Link virtual patients from Quantitative Systems Pharmacology (QSP) models to real clinical trial patients based on similarity between tumor growth curves [81].
Tumor Dynamics Feature Extraction: Extract features from longitudinal tumor size data, including:
- Tumor growth kinetics during treatment period
- Tumor shrinkage patterns
- Early tumor size changes
- Time to minimum tumor size [81]
Weakly Supervised Learning: Treat linked survival and censoring data as weak supervision labels to train survival models using only QSP model covariates without clinical covariates [81].
Model Validation: Validate predicted survival hazard ratios against observed outcomes from clinical trials. For example, predicted HR of 0.70 (95% PI 0.55-0.86) closely matched observed HR of 0.79 (95% PI 0.64-0.98) from the IMpower130 trial [81].
The Researcher's Toolkit
Essential Reagents and Materials
Table 3: Essential Research Reagents for RECIST and ctDNA Correlation Studies
| Reagent/Material | Specification | Application | Critical Function |
|---|---|---|---|
| Cell-free DNA Blood Collection Tubes | Streck, PAXgene, or similar | LB-RECIST protocol | Preserves blood sample integrity for ctDNA analysis |
| DNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit or similar | ctDNA isolation | High-sensitivity extraction of circulating tumor DNA |
| NGS Library Prep Kits | Oncomine Colon cfDNA Assay | ctDNA mutation profiling | Target enrichment for cancer-associated mutations |
| Real-time PCR Master Mix | TaqMan, SYBR Green, or similar | ctDNA quantification | Amplification and detection of target sequences |
| CT/MRI Contrast Agents | Iohexol, Gadobutrol, or similar | RECIST imaging | Enhances lesion visualization and measurement accuracy |
| RECIST Annotation Software | MIM Software, Philips IntelliSpace | Tumor measurement | Enables precise lesion tracking and sum calculations |
RECIST Implementation Toolkit
Protocol Templates: Utilize standardized protocol templates (e.g., CTEP Generic Protocol Template) for consistent RECIST implementation across trials [82].
Training Materials: Develop institution-specific RECIST training modules with competency assessment components to ensure research staff proficiency [74].
Source Documentation Systems: Establish electronic RECIST source documents accessible to appropriate study team members prior to trial activation [74].
Quality Control Checklists: Implement audit guidelines review to prevent common RECIST implementation errors, including inaccurate documentation of initial sites of disease and inconsistent scanning methods [74].
The correlation between RECIST criteria and clinical endpoints represents a complex interplay between standardized response assessment and genuine clinical benefit. While RECIST provides an essential standardized framework for tumor response evaluation, its relationship with survival outcomes is significantly modulated by factors including tumor burden, treatment mechanism, and line of therapy. The emergence of liquid biopsy methodologies, particularly ctDNA analysis through real-time PCR and NGS platforms, offers promising complementary approaches to traditional radiographic assessment.
Future developments in this field will likely focus on integrated response assessment frameworks that combine radiographic evaluation with molecular response monitoring. The validation of LB-RECIST in metastatic colorectal cancer demonstrates the potential for liquid biopsy to provide earlier response assessment and improved prognostic stratification [80]. Furthermore, computational approaches linking tumor dynamics to survival outcomes represent a promising avenue for enhancing clinical trial design and personalized treatment strategies.
For researchers utilizing real-time PCR protocols in ctDNA research, these developments highlight the growing importance of correlating molecular response with traditional RECIST endpoints. As the field advances, the integration of multi-modal assessment strategies will be essential for developing more comprehensive and predictive evaluation frameworks in oncology drug development.
The monitoring of circulating tumor DNA (ctDNA) is undergoing a profound transformation, moving beyond simple mutation detection to a sophisticated multi-parametric approach. This whitepaper details the integration of multiplexed assays, fragmentomics, and fragment size analysis within real-time PCR protocols, a synergy that is poised to redefine liquid biopsy. We explore how combining these methodologies provides a more comprehensive, tumor-agnostic view of treatment response, tumor burden, and disease biology. This technical guide provides researchers and drug development professionals with the current state of these technologies, supported by quantitative data and detailed experimental protocols, to advance the field of precision oncology.
The conventional use of real-time PCR (qPCR) and digital PCR (dPCR) in liquid biopsy has primarily focused on detecting specific somatic mutations to quantify ctDNA burden [83]. While powerful, this approach is inherently limited by the need for prior knowledge of tumor genetics and can miss critical biological information encapsulated in the physical characteristics of cell-free DNA (cfDNA). Fragmentomics—the study of these fragmentation patterns—has emerged as a powerful, tumor-agnostic supplement to mutation-based assays [84] [85].
Simultaneously, multiplexed assays have evolved to allow for the simultaneous interrogation of dozens to hundreds of genetic targets from a single sample, overcoming the fluorescent channel limitations of traditional qPCR by coupling amplification with fragment analysis [86]. When these approaches are integrated, they create a powerful framework for monitoring treatment response in solid tumors, offering earlier insights than standard imaging and capturing tumor heterogeneity more effectively than single-biopsy genomic profiling [1].
Core Technologies and Principles
Multiplexed PCR and Fragment Analysis
Multiplex PCR coupled with capillary electrophoresis (CE) is a versatile technique that enables high-level multiplexing without being limited by the number of fluorophores, as in standard qPCR.
- Principle of Operation: This method uses primers designed against various targets to generate amplicons of unique, predetermined lengths. Following amplification, capillary electrophoresis separates these fluorescently-labeled products based on size with up to a 2 bp resolution. The resulting data, displayed as an electropherogram, allows for the simultaneous detection and distinction of multiple targets [86].
- Theoretical Multiplexing Capacity: The practical operating size range is between 100 and 600 nucleotides. This theoretically allows for the detection of approximately 250 distinct targets per fluorescent dye. When multiple dyes are used in a single capillary, the potential multiplexing capability expands significantly, enabling the analysis of a large number of targets from a minimal sample volume [86].
- Applications in Oncology: This approach is widely used to detect specific genetic aberrations such as translocations, screen for mutations across a gene, and identify genetic polymorphisms that predict drug response [86].
Fragmentomics: Mining the Biological Information in cfDNA Patterns
Fragmentomics leverages the non-random fragmentation of DNA released from tumor cells. Key fragmentomic features include:
- Fragment Size Distribution: cfDNA fragments from tumor cells are often shorter than those from healthy cells. The most prevalent fragment size in circulation is ~167 bp, corresponding to DNA wrapped around a single nucleosome. The quantification of specific size fractions (e.g., fragments < 150 bp or ratios of longer fragments) provides rich information about the cell of origin [84] [85].
- DNA Integrity and End Motifs: The DNA Integrity Index and the analysis of fragment end motifs (the short DNA sequences at the ends of cfDNA fragments) are other fragmentomic metrics that can distinguish cancer-derived DNA from normal cfDNA [84] [85].
- Inference of Epigenetics: The placement of nucleosomes and transcription factors on DNA protects it from digestion, leading to unique fragmentation patterns at specific genomic locations. This allows fragmentomics to infer epigenetic and transcriptional information from cfDNA, such as predicting cancer type and subtype [85].
Quantitative Fragmentomics: Performance Data and Metrics
The performance of various fragmentomics metrics has been systematically evaluated in recent studies. The following table summarizes the average Area Under the Receiver Operating Characteristic Curve (AUROC) for predicting cancer presence and type using a 822-gene targeted panel, demonstrating the high discriminatory power of these metrics [85].
Table 1: Performance of Fragmentomics Metrics in Cancer Detection and Classification (UW Cohort)
| Fragmentomics Metric | Average AUROC (Range) | Key Application Notes |
|---|---|---|
| Normalized Depth (All Exons) | 0.943 (0.873 - 0.986) | Best overall performance for predicting cancer types and subtypes. |
| Normalized Depth (First Exon/E1) | 0.930 (0.838 - 0.989) | Strong performance, leveraging epigenetic signals near transcription start sites. |
| Normalized Depth (Full Gene) | 0.919 (0.828 - 0.993) | Combines all exons from one gene into a single feature. |
| End Motif Diversity (All Exons) | Variable by cancer type | Top-performing metric for Small Cell Lung Cancer (AUROC: 0.888). |
Furthermore, research indicates that fragmentomics assays do not necessarily require whole-genome sequencing (WGS) to be effective. The table below shows that targeted commercial panels, which are already in clinical use for variant calling, can be successfully repurposed for fragmentomic analysis with only a minimal decrease in performance [85].
Table 2: Performance of Fragmentomics on Commercial Targeted Panels
| Commercial Panel (Number of Genes) | Relative Performance | Implication |
|---|---|---|
| FoundationOne Liquid CDx (309 genes) | Best among commercial panels | Demonstrates robust phenotyping on a clinically adopted platform. |
| Tempus xF (105 genes) | Intermediate | Maintains high AUROCs for many cancer types. |
| Guardant360 CDx (55 genes) | Good | Even smaller gene sets retain significant predictive value. |
Integrated Experimental Protocols
This section provides a detailed methodology for implementing a fragmentomic assay based on quantitative PCR, as validated in recent studies for monitoring treatment response in metastatic cancer [84].
Protocol: qPCR-Based Progression Score (PS) Assay
1. Sample Collection and Processing
- Collection: Draw 8-10 mL of peripheral blood into Streck Cell-Free DNA BCT tubes.
- Transport: Ship tubes at ambient temperature via overnight courier. Process samples within 120 hours of collection to prevent cfDNA degradation [84].
- Plasma Separation: Use a two-step centrifugation protocol.
- First, centrifuge Streck tubes at 1,600× g for 10 minutes at 15°C to separate plasma.
- Transfer the plasma to a new tube and centrifuge a second time at 16,000× g for 10 minutes at room temperature to remove any remaining cells.
- Aliquot plasma and store at -80°C until cfDNA extraction [84].
2. cfDNA Extraction
- Use the QIAamp Circulating Nucleic Acid Kit.
- Extract cfDNA from 500 µL of plasma, following the manufacturer's protocol for a 1 mL plasma volume with the following modification: omit carrier RNA from the ACL buffer [84].
3. Quantitative PCR (qPCR) Setup
- Targets: Design qPCR assays to target multi-copy retrotransposon elements (e.g., ALU). Amplify fragments of distinct size ranges, for example: >80 bp, >105 bp, and >265 bp. Include an internal control assay [84].
- Reaction Optimization: Critical factors for optimizing this multiplexed qPCR include [87] [88] [89]:
- Primers: Use a final concentration of 0.1–0.5 µM per primer. Design primers with a Tm of 42–65°C and ensure primer pairs have Tms within 5°C of each other.
- MgCl₂ Concentration: A starting concentration of 1.5–2.0 mM is recommended for Taq polymerase. Optimize in 0.5 mM increments up to 4 mM if necessary.
- Template DNA: Use 30–100 ng of total cfDNA as template.
- Polymerase: Use 0.5–2.0 units of a hot-start DNA polymerase per 50 µL reaction.
- Thermal Cycling Conditions:
- Initial Denaturation: 95°C for 2 minutes.
- 40–45 Cycles of:
- Denaturation: 95°C for 15 seconds.
- Annealing: 55–60°C for 15–30 seconds (optimize based on primer Tm).
- Extension: 68°C for 45–60 seconds.
- Final Extension: 68°C for 5 minutes [89].
4. Data Analysis and Progression Score Calculation
- Quantification: Determine the concentration of each amplicon size fraction using standard curves or relative quantification methods.
- Model Integration: Input the quantified values into a pre-validated algorithm that integrates the quantities into a single Progression Score (PS) on a scale of 0–100.
- Interpretation: A high PS (e.g., >90) indicates a high probability of radiographic progression, while a low PS (e.g., <10) suggests the therapy is effective [84].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Fragmentomics and Multiplexed PCR
| Item | Function/Description | Example Products/Brands |
|---|---|---|
| cfDNA Collection Tubes | Preserves blood cells and stabilizes cfDNA concentration for up to 5 days at room temperature. | Streck Cell-Free DNA BCT tubes [84] |
| cfDNA Extraction Kit | Isolves short, fragmented cfDNA from plasma with high purity and yield. | QIAamp Circulating Nucleic Acid Kit (Qiagen) [84] |
| Hot-Start DNA Polymerase | Reduces non-specific amplification and primer-dimers by requiring heat activation. | Taq Hot Start, OneTaq Hot Start [89] |
| Multiplex PCR Master Mix | Pre-optimized buffer system often containing enhancers for robust amplification of multiple targets. | Various commercial master mixes |
| Capillary Electrophoresis System | Separates fluorescently-labeled DNA fragments by size for fragment analysis. | Applied Biosystems Genetic Analyzers [86] |
| Fragment Analysis Software | Automates size calling, peak analysis, and quality assessment of CE data. | GeneMarker, ChimeRMarker [90] |
Future Directions and Challenges
The future integration of these technologies faces several challenges that require concerted effort from the research community.
- Standardization and Workflow Bottlenecks: A key challenge is the lack of technical standardization across platforms and laboratories. Furthermore, data interpretation can become a bottleneck, especially with large batches of fragment data, necessitating automated, intelligent software solutions like GeneMarker to streamline analysis [90].
- Low ctDNA Fraction Sensitivity: The performance of all ctDNA assays, including fragmentomics, is dependent on the tumor fraction in the blood. Enhancing the sensitivity of these assays to detect cancer signals at very low ctDNA fractions (e.g., below 0.1%) is a critical area of ongoing development [85] [1].
- Multi-Omic Integration: The most powerful future applications will likely involve a multi-omic liquid biopsy approach. Combining fragmentomics with mutation-based ctDNA quantification, methylation analysis, and other biomarkers like circulating tumor cells (CTCs) will provide an unparalleled, comprehensive view of tumor dynamics and will be crucial for advancing precision oncology [1].
The convergence of multiplexed assays, fragmentomics, and fragment size analysis represents the next frontier in liquid biopsy. By integrating these approaches with established real-time PCR protocols, researchers and clinicians can move beyond simple variant detection to a more holistic, tumor-agnostic understanding of cancer biology and treatment response. This technical guide outlines the principles, data, and methodologies required to implement these advanced techniques, paving the way for more personalized, dynamic, and effective cancer patient management.
Conclusion
Real-time PCR, especially dPCR and ddPCR, has firmly established itself as a cornerstone technology for ctDNA analysis, offering unparalleled sensitivity, quantitative accuracy, and practical efficiency for clinical and research applications. By mastering foundational biology, implementing robust protocols, and systematically troubleshooting assay performance, researchers can reliably deploy these tools to monitor minimal residual disease, track treatment response, and detect resistance mechanisms. Future directions will focus on standardizing pre-analytical steps, developing ultra-high multiplexing capabilities, and further integrating ctDNA kinetics as a validated surrogate endpoint in clinical trials. The continued refinement of PCR-based ctDNA assays is poised to accelerate drug development and deepen our molecular understanding of cancer dynamics, solidifying its indispensable role in the precision oncology toolkit.
References
- 1. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 2. Circulating Tumor DNA as a Cancer Biomarker [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.943253/full]
- 3. Monitoring and Assessment of Circulating Tumor DNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550271/]
- 4. Circulating tumor nucleic acids: biology, release ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9862574/]
- 5. The main sources of circulating cell-free DNA [https://www.sciencedirect.com/science/article/abs/pii/S1040842820303024]
- 6. Detection and Quantification of ctDNA for Longitudinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9274771/]
- 7. Quantitative and Dynamic ctDNA as a Biomarker of ... [https://www.sciencedirect.com/science/article/pii/S1556086425007518]
- 8. Cell-Free DNA (cfDNA) vs. Circulating Tumor DNA (ctDNA) ... [https://www.thermofisher.com/blog/life-in-the-lab/cfdna-vs-ctdna/]
- 9. Improvement of the sensitivity of circulating tumor DNA-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12332530/]
- 10. Digital PCR Principle, techniques and applications [https://www.stillatechnologies.com/digital-pcr/principle/]
- 11. dPCR: A Technology Review - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5948698/]
- 12. Fundamentals of digital PCR [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/digital-pcr/what-is-digital-pcr]
- 13. Improvement of the sensitivity of circulating tumor DNA- ... [https://www.explorationpub.com/Journals/etat/Article/1002333]
- 14. Surveillance of the Genetic Signature in Circulating Tumor ... [https://www.researchprotocols.org/2025/1/e72597]
- 15. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 16. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 17. Liquid biopsy- A pivotal test to help navigate clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409318/]
- 18. Circulating tumor DNA predicts prognosis at different time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507613/]
- 19. Circulating tumor DNA as prognostic marker in patients ... [https://www.sciencedirect.com/science/article/pii/S0305737225001215]
- 20. Validation of a liquid biopsy assay with increased ... [https://www.sciencedirect.com/science/article/pii/S2950195425000384]
- 21. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 22. Quantitative PCR (qPCR) Data Analysis [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/precision-qpcr.html]
- 23. PCR Tubes | Fisher Scientific [https://www.fishersci.com/us/en/browse/90168092/pcr-tubes?page=1]
- 24. PCR-0108-LP-RT-C | Axygen® 0.1 mL Low Profile Polypropylene Thin Wall PCR Tube Strips and Real Time Strip Caps, 8 Tubes and Caps/Strip, Clear, Nonsterile | Corning [https://ecatalog.corning.com/life-sciences/b2b/US/en/Genomics-&-Molecular-Biology/PCR-Consumables/PCR-Tubes-and-Strip-Tubes/Axygen%C2%AE-PCR-Strip-Tubes/p/PCR-0108-LP-RT-C]
- 25. Standard PCR Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/genomics/pcr/standard-pcr?srsltid=AfmBOorMlaYpr1tyBj0-iZXjF7QH5M766yqZlySN_r7oW75HYKA7ar1R]
- 26. Can the extracted DNA be stored long-term at -20 degrees ... [https://pcrbio.com/resources/faqs/pcrbio-rapid-extract-pcr-kit/can-the-extracted-dna-be-stored-long-term-at-20-degrees-celsius/]
- 27. Effects of storage conditions on the stability of qPCR reagents [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-024-06850-4]
- 28. Your DNA may be degraded [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/real-time-pcr-troubleshooting-tool/snp-genotyping-troubleshooting/trailing-clusters/dna-may-be-degraded.html]
- 29. Ten Tips for Successful qPCR - Behind the Bench [https://www.thermofisher.com/blog/behindthebench/ten-tips-for-successful-qpcr/]
- 30. to monitor treatment response in solid Circulating ... tumor DNA tumors [https://www.nature.com/articles/s41698-025-00876-y?error=cookies_not_supported&code=f4628838-4f57-42ef-8c79-cc00c592e46c]
- 31. Next‑generation sequencing‑based detection of EGFR , KRAS , BRAF ... [https://pubmed.ncbi.nlm.nih.gov/29956783/]
- 32. Next‑generation sequencing‑based detection of EGFR , KRAS , BRAF ... [https://www.spandidos-publications.com/mmr/18/2/2191]
- 33. In-depth assessment of BRAF , NRAS, KRAS , EGFR , and PIK ... 3 CA [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03457-w]
- 34. For detection of 11 mutations in the PIK gene by 3 - CA real time PCR [https://www.qiagen.com/us/products/diagnostics-and-clinical-research/oncology/therascreen-solid-tumor/therascreen-pik3ca-rgq-pcr-kit-us]
- 35. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOor1SXjpdlJqnBcqzV4xjdWVjxSfq2osDrfvekAyHGPIBQ8djAQu]
- 36. Statistical analysis of real-time PCR data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1395339/]
- 37. Relative quantification of mRNA: comparison of methods ... [https://bmcmolbiol.biomedcentral.com/articles/10.1186/1471-2199-8-113]
- 38. Circulating Tumor DNA in Genitourinary Cancers [https://www.mdpi.com/2072-6694/16/12/2280]
- 39. Strategies for improving detection of circulating tumor DNA ... [https://www.sciencedirect.com/science/article/pii/S0305737223000889]
- 40. The impact of preanalytical variables on the analysis of cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1385041/full]
- 41. Development of real-time PCR methods for quality control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12058689/]
- 42. A simple and cost-effective real-time PCR method using ... [https://www.nature.com/articles/s41598-024-78802-8]
- 43. The Impact of Hemolysis on Cell-Free microRNA Biomarkers [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2013.00094/full]
- 44. The effect of hemolysis on quality control metrics for ... [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-022-01280-2]
- 45. Input DNA/RNA QC [https://nanoporetech.com/document/input-dna-rna-qc]
- 46. PCR Setup—Six Critical Components to Consider [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-component-considerations.html]
- 47. Rules and Tips for PCR & qPCR Primer Design | IDT [https://www.idtdna.com/page/support-and-education/decoded-plus/how-to-design-primers-and-probes-for-pcr-and-qpcr/]
- 48. Polymerase Chain Reaction: Basic Protocol Plus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846334/]
- 49. Real-time PCR probe optimization using design of ... [https://www.sciencedirect.com/science/article/pii/S2214753515300139]
- 50. An optimized protocol for stepwise optimization of real-time ... [https://www.nature.com/articles/s41438-021-00616-w]
- 51. Real-Time PCR: Understanding Ct [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/real-time-pcr-understanding-ct.html]
- 52. How To Interpret RT-qPCR Results [https://www.goldbio.com/blogs/articles/how-to-interpret-rt-qpcr-results?srsltid=AfmBOoqjlWehGwMWxpsjBbm5Y-ImF4N_vODq8cPRlpUNhiPRn9SJNImX]
- 53. Integrating artificial intelligence with circulating tumor DNA ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1612376/full]
- 54. TET2-mutant clonal hematopoiesis enhances macrophage ... [https://www.sciencedirect.com/science/article/pii/S1535610825004039]
- 55. Recent Update Roles of Magnetic Nanoparticles in Circulating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10610106/]
- 56. Listing Top 10 Circulating Tumor Cells Companies 2025 [https://www.polarismarketresearch.com/blog/listing-top-10-circulating-tumor-cells-companies-2025]
- 57. Quantitative real-time PCR and magnetic separation strategy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10794924/]
- 58. Rapid-Response Magnetic Enrichment Strategy for ... [https://www.mdpi.com/2076-3417/12/13/6415]
- 59. Evaporation-Enhanced Redox Cycling for Rapid Detection ... [https://pure.psu.edu/en/publications/evaporation-enhanced-redox-cycling-for-rapid-detection-of-attomol]
- 60. a comparison of polymerase chain reaction and sequencing ... [https://pcm.amegroups.org/article/view/5565/html]
- 61. Establishing PNB-qPCR for quantifying minimal ctDNA ... [https://www.nature.com/articles/s41598-017-09137-w]
- 62. Performance Comparison of Droplet Digital PCR and Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062871/]
- 63. Analytical and clinical validation of a NGS panel in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11464656/]
- 64. NGS vs qPCR [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-qpcr.html]
- 65. Limited Sensitivity of Circulating Tumor DNA Detection by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6468548/]
- 66. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 67. Real-Time PCR (qPCR) and Whole-Transcriptome NGS [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/ngs-comparison.html]
- 68. Circulating tumor DNA in colorectal cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC11961841/]
- 69. Clinical Circulating Tumor DNA Testing for Precision Oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC10101787/]
- 70. Validating Real-Time Polymerase Chain Reaction (PCR) Assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC7834634/]
- 71. Analytical evaluation of circulating tumor DNA sequencing ... [https://www.nature.com/articles/s41598-024-54361-w]
- 72. Real-Time Polymerase Chain Reaction: Current Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9778061/]
- 73. Genomic reproducibility in the bioinformatics era - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11312195/]
- 74. RECIST 1.1 Criteria Toolkit: A Resource for Success in ... [https://www.nrgoncology.org/Home/News/Post/recist-11-criteria-toolkit-a-resource-for-success-in-clinical-trials-with-solid-tumor-evaluation-requirements/]
- 75. RECIST Imaging Criteria in Clinical Trials with Infographic [https://www.banook.com/resources/blog/recist-imaging-criteria-in-clinical-trials]
- 76. The legend of the response evaluation criteria in solid tumors [https://pmc.ncbi.nlm.nih.gov/articles/PMC12393182/]
- 77. The Relationship Between Response Rate and Survival ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11815975/]
- 78. Impact of Tumor Burden on Immune Checkpoint and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598540/]
- 79. Baseline tumor burden predicts the efficacy of first-line ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14755-z]
- 80. Clinical validation of liquid biopsy-RECIST (LB- ... [https://pubmed.ncbi.nlm.nih.gov/40907207/]
- 81. Predicting survival in prospective clinical trials using ... [https://www.nature.com/articles/s41698-025-00898-6]
- 82. CTEP Trial Development and Conduct - NCI [https://dctd.cancer.gov/research/ctep-trials/trial-development]
- 83. Techniques of using circulating tumor DNA as a liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6197739/]
- 84. A Novel Cell-Free DNA Fragmentomic Assay and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606779/]
- 85. Analysis of cfDNA fragmentomics metrics and commercial ... [https://www.nature.com/articles/s41467-025-64153-z]
- 86. Multiplex PCR Coupled with Fragment Analysis [https://www.thermofisher.com/blog/behindthebench/multiplex-pcr-coupled-with-fragment-analysis/]
- 87. PCR Optimization: Factors Affecting Reaction Specificity ... [https://www.mybiosource.com/learn/pcr-optimization-factors-affecting-reaction-specificity-and-efficien/]
- 88. Optimizing your PCR [https://www.takarabio.com/learning-centers/pcr/faq/optimization?srsltid=AfmBOooX-RASFo5IkokoCaMLHn8joR2q7y3EcSE6qqhgNqQVYD4EtP3W]
- 89. Guidelines for PCR Optimization with Taq DNA Polymerase [https://www.neb.com/en-us/tools-and-resources/usage-guidelines/guidelines-for-pcr-optimization-with-taq-dna-polymerase?srsltid=AfmBOop0tovFTFRtVsb5h9dNlEYpJ9ZyGjZp_Y-H9WWY1eTrSHUJTA5U]
- 90. What does fragment analysis look like in 2025? [https://go.softgenetics.com/guides/fragment-analysis-in-2025]