Advanced 3D-QSAR and Virtual Screening Strategies for Novel Glioblastoma Therapeutics
This article provides a comprehensive exploration of virtual screening utilizing 3D-QSAR models for the discovery of glioblastoma therapeutics.
Advanced 3D-QSAR and Virtual Screening Strategies for Novel Glioblastoma Therapeutics
Abstract
This article provides a comprehensive exploration of virtual screening utilizing 3D-QSAR models for the discovery of glioblastoma therapeutics. It covers the foundational principles of 3D-QSAR, including CoMFA and CoMSIA, and their application against key glioblastoma targets like PLK1, mIDH1, and FAK. The content details methodological workflows integrating machine learning for enhanced predictive accuracy and addresses common troubleshooting and optimization challenges. Furthermore, it examines rigorous validation protocols involving molecular docking, ADMET analysis, and molecular dynamics simulations to assess binding stability and drug-likeness. Aimed at researchers and drug development professionals, this review synthesizes current computational strategies to accelerate the design of effective, targeted therapies for this aggressive brain cancer.
Glioblastoma's Urgent Challenge and 3D-QSAR's Foundational Role in Target Identification
Glioblastoma (GBM) is the most aggressive and lethal primary malignant brain tumor in adults, presenting significant challenges to patient survival and treatment efficacy [1]. Despite extensive research, the median survival remains a dismal 12 to 15 months, with a five-year survival rate of only 7.2% [1] [2]. The current standard of care includes maximal safe surgical resection followed by radiotherapy with concurrent and adjuvant temozolomide (TMZ) chemotherapy, with or without Tumor Treating Fields (TTFields) [3] [4]. This aggressive multimodal approach provides only modest survival benefits, highlighting the critical need for advanced therapeutic strategies.
GBM's treatment resistance stems from three interconnected biological challenges: intrinsic tumor aggressiveness, pronounced therapeutic resistance, and the restrictive blood-brain barrier (BBB). GBM exhibits remarkable molecular heterogeneity, both between patients and within individual tumors, with distinct transcriptional subtypes (proneural, neural, classical, and mesenchymal) that demonstrate differential therapeutic responses [1] [5]. The tumor microenvironment (TME) fosters immunosuppression through tumor-associated macrophages, myeloid-derived suppressor cells, and regulatory T cells, creating a niche conducive to tumor growth and immune evasion [1]. Additionally, glioma stem-like cells (GSCs) with self-renewal capabilities contribute to tumor persistence, recurrence, and resistance [1] [5].
The BBB represents a fundamental obstacle to effective drug delivery, excluding approximately 98% of small molecules and almost all macromolecular agents from the brain [6] [7]. While GBMs exhibit regions of BBB disruption visible as contrast enhancement on MRI, clinically significant tumor burden persists behind an intact BBB in areas of invasive margins and non-enhancing edema, protecting infiltrating cells from therapeutic exposure [7]. Overcoming these interconnected challenges requires innovative approaches that address GBM's complex biology while ensuring adequate drug delivery to all tumor regions.
Molecular Characterization and Therapeutic Targets
Key Molecular Alterations in Glioblastoma
GBM is characterized by diverse molecular alterations that drive tumorigenesis, progression, and therapeutic resistance. The 2021 WHO classification of CNS tumors recognizes GBM as a grade IV IDH-wildtype glioma with specific molecular features including TERT promoter mutations, EGFR amplification, and the combined gain of chromosome 7 and loss of chromosome 10 [4]. Molecular profiling has identified several critical pathways and alterations that represent promising therapeutic targets, summarized in Table 1.
Table 1: Key Molecular Targets in Glioblastoma and Experimental Therapeutic Approaches
| Target/Pathway | Alteration Frequency | Biological Consequence | Targeted Agents in Development |
|---|---|---|---|
| EGFR | Amplified in ~40-60% of GBMs [1] | Enhanced proliferation, survival, and invasion through RTK/MAPK and PI3K/AKT signaling [1] | Antibody-drug conjugates, CAR-T therapies (e.g., CART-EGFR-IL13Ra2) [8] |
| IDH1 | Mutated in ~10% of GBMs (secondary GBM) [1] | Production of oncometabolite 2-HG, leading to epigenetic dysregulation and blocked differentiation [9] | Ivosidenib, olutasidenib, vorasidenib [9] [8] |
| MGMT | Promoter methylated in ~35-50% of GBMs [3] | Predictive of response to temozolomide; methylated tumors have better survival (18.4 vs. 10.8 months) [3] | - |
| PTEN | Lost in ~25-40% of GBMs [1] | Constitutive PI3K/AKT/mTOR pathway activation, promoting growth and survival [1] | mTOR inhibitors, PI3K/AKT pathway inhibitors |
| PDGFR-α | Amplified/overexpressed in ~15% of GBMs [1] | Enhanced proliferative signaling, particularly in proneural subtype [1] | Receptor tyrosine kinase inhibitors |
| TERT promoter | Mutated in ~60-80% of primary GBMs [4] | Telomerase reactivation and cellular immortalization [4] | - |
Signaling Pathways as Therapeutic Targets
Several oncogenic signaling pathways are recurrently dysregulated in GBM and represent rational targets for therapeutic intervention. The PI3K/AKT/mTOR pathway is a central regulator of tumor growth and survival, frequently activated through EGFR amplification or PTEN loss [1]. Despite being a promising target, clinical trials with mTOR inhibitors have shown limited success, highlighting the need for combination approaches and better patient stratification [1]. The RTK/RAS/MAPK pathway is another critical signaling cascade, often driven by EGFR, PDGFR, or MET alterations, making it a compelling target for multi-RTK inhibition strategies [5].
Metabolic reprogramming represents an emerging targeting opportunity, with mutant IDH1 (mIDH1) being a particularly validated target. mIDH1 acquires a neomorphic activity that converts α-ketoglutarate to the oncometabolite 2-hydroxyglutarate (2-HG), which competitively inhibits α-KG-dependent dioxygenases, leading to histone and DNA hypermethylation and subsequent changes in gene expression that drive tumorigenesis [9]. Targeting this pathway with specific inhibitors such as ivosidenib (AG-120) has shown clinical efficacy, particularly in IDH-mutant secondary GBMs and other IDH-mutant cancers [9].
Computational Approaches: Virtual Screening with 3D-QSAR Models
Foundation of 3D-QSAR in Glioblastoma Drug Discovery
Virtual screening using three-dimensional quantitative structure-activity relationship (3D-QSAR) models represents a powerful computational approach for identifying and optimizing novel therapeutic compounds against glioblastoma targets. This method establishes a mathematical correlation between the three-dimensional structural features of molecules and their biological activity, enabling the rational design of compounds with improved efficacy and selectivity [9] [10]. The primary 3D-QSAR techniques include Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA), which analyze steric, electrostatic, hydrophobic, and hydrogen-bonding fields around aligned molecules [9].
Recent applications of 3D-QSAR in glioblastoma drug discovery have demonstrated promising results. For mIDH1 inhibitors, studies utilizing pyridin-2-one-based compounds have yielded highly predictive CoMFA (R² = 0.980, Q² = 0.765) and CoMSIA (R² = 0.997, Q² = 0.770) models, enabling the design of novel structures with enhanced predicted activity [9]. Similarly, for dihydropteridone derivatives targeting Polo-like kinase 1 (PLK1), 3D-QSAR models have shown excellent predictive power (Q² = 0.628, R² = 0.928), facilitating the identification of critical structural features responsible for anti-glioma activity [10].
Experimental Protocol: 3D-QSAR Model Development and Virtual Screening
Protocol Title: Development and Validation of 3D-QSAR Models for Virtual Screening of Glioblastoma Therapeutics
Objective: To create predictive 3D-QSAR models for identifying novel compounds with potential efficacy against glioblastoma molecular targets.
Materials and Software:
- Chemical structure drawing software (ChemDraw)
- Molecular modeling suite (HyperChem, SYBYL, Schrodinger)
- Statistical analysis software (CODESSA, R, Python)
- High-performance computing resources
Procedure:
Data Set Curation and Preparation
- Collect a structurally diverse set of compounds with known biological activity (IC₅₀ or EC₅₀ values) against the glioblastoma target of interest
- Divide compounds into training set (≈80%) for model development and test set (≈20%) for validation [10]
- Sketch 2D chemical structures using ChemDraw and convert to 3D representations
- Perform geometry optimization using molecular mechanics (MM+ force field) followed by semi-empirical methods (AM1 or PM3) until root mean square gradient reaches <0.01 kcal/mol·Å [10]
Molecular Alignment
- Identify common structural features or pharmacophores for alignment
- Utilize field-fit, database, or receptor-based alignment methods
- Ensure consistent orientation of all molecules in the dataset
3D-QSAR Model Construction
- Calculate interaction fields using CoMFA (steric and electrostatic) and CoMSIA (steric, electrostatic, hydrophobic, hydrogen bond donor/acceptor) [9]
- Set grid spacing to 2.0 Å extending 4.0 Å beyond all molecules
- Apply standard scaling options (e.g., block-centered) to normalize field values
Partial Least Squares (PLS) Analysis
- Perform cross-validated PLS analysis to determine optimal number of components
- Use leave-one-out or bootstrapping methods for internal validation
- Generate final non-cross-validated model using optimal component number
Model Validation and Visualization
- Assess model quality using statistical parameters: R² (goodness of fit), Q² (predictive ability), F-value (statistical significance), standard error of estimate [10]
- Validate model externally using test set compounds not included in training
- Generate coefficient contour maps to visualize regions where specific molecular properties enhance or diminish biological activity
Virtual Screening and Compound Design
- Apply validated model to screen virtual compound libraries
- Design novel compounds by scaffold hopping and structural modification based on contour map insights [9]
- Predict activity of newly designed compounds using the established model
- Select top candidates for synthesis and biological evaluation
Quality Control:
- Ensure chemical diversity in both training and test sets
- Verify absence of chance correlation through Y-scrambling
- Confirm model robustness through multiple validation techniques
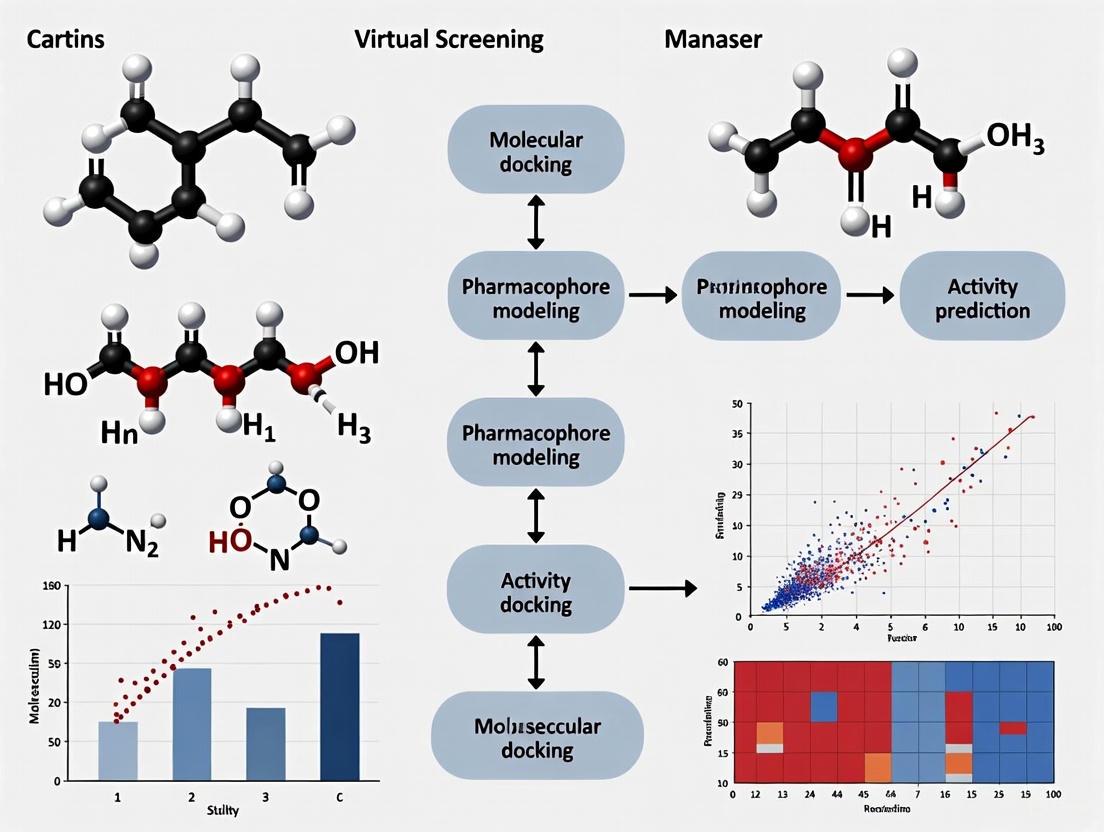
Diagram 1: 3D-QSAR Virtual Screening Workflow. This flowchart illustrates the comprehensive process for developing and applying 3D-QSAR models in glioblastoma drug discovery, from initial data collection to final candidate selection.
Advanced Therapeutic Delivery Strategies
Blood-Brain Barrier Penetration Technologies
The blood-brain barrier (BBB) and blood-brain tumor barrier (BBTB) represent significant obstacles for glioblastoma therapy, restricting delivery of both conventional chemotherapeutics and novel targeted agents to tumor sites [5] [6]. While contrast-enhancing regions of GBM exhibit some BBB disruption, infiltrating tumor cells in non-enhancing regions remain protected by an intact BBB, creating therapeutic sanctuaries that contribute to treatment failure and recurrence [7]. To address this challenge, numerous innovative strategies are being developed to enhance drug delivery across the BBB, as summarized in Table 2.
Table 2: Advanced Strategies for Enhanced Drug Delivery Across the BBB in Glioblastoma
| Strategy Category | Specific Approach | Mechanism of Action | Development Status |
|---|---|---|---|
| Physical Barrier Modulation | Focused Ultrasound with Microbubbles [6] | Temporary BBB disruption through acoustic cavitation | Early-phase clinical trials |
| Optical BBB Modulation (optoBBTB) [6] | Light-activated gold nanoparticles target tight junctions | Preclinical (mouse models) | |
| Hyperosmolar Agents (Mannitol) [6] | Osmotic shrinkage of endothelial cells opens tight junctions | Clinical use | |
| Nanotechnology-Based Delivery | Gold Nanoparticles [6] | Target tight junction proteins (e.g., JAM-A) for reversible BBB opening | Preclinical |
| Polymeric Nanoparticles [3] | Protect payload, enhance circulation time, and enable functionalization | Preclinical to early clinical | |
| Exosome-Mediated Delivery [3] | Exploit natural vesicle trafficking for enhanced brain penetration | Preclinical | |
| Biological Transport Mechanisms | Receptor-Mediated Transcytosis [6] | Utilize endogenous transport systems (e.g., transferrin receptor) | Preclinical to clinical |
| Cell-Penetrating Peptides [5] | Facilitate cellular uptake through membrane interaction | Preclinical | |
| Trojan Bacteria [6] | Engineered bacteria as drug carriers that cross BBB | Preclinical | |
| Localized Delivery Systems | Convection-Enhanced Delivery (CED) [8] | Direct infusion into brain tissue under positive pressure | Clinical trials |
| Implantable Wafers (Gliadel) [5] | Local sustained release of chemotherapeutics | FDA-approved | |
| Intrathecal Administration [5] | Direct administration into cerebrospinal fluid | Clinical use |
Experimental Protocol: Evaluating BBB Penetration Using Advanced Models
Protocol Title: Assessment of Blood-Brain Barrier Penetration in Preclinical Glioblastoma Models
Objective: To evaluate the ability of therapeutic compounds to cross the BBB and reach tumor tissue using physiologically relevant models.
Materials:
- In vitro BBB models (primary human brain endothelial cells, pericytes, astrocytes)
- Transwell culture systems
- Glioblastoma mouse models (genetically engineered, patient-derived xenografts)
- Microdialysis systems
- LC-MS/MS for drug quantification
- Fluorescent or radiolabeled compounds
- MRI with contrast agents
Procedure:
In Vitro BBB Model Establishment
- Culture primary human brain microvascular endothelial cells on Transwell inserts
- Add primary human astrocytes and pericytes to basolateral chamber
- Monitor transendothelial electrical resistance (TEER) daily until >150 Ω·cm²
- Validate barrier integrity with sodium fluorescein (0.3-0.5% leakage acceptable)
Compound Permeability Assessment
- Apply test compound to apical (blood) compartment
- Sample from basolateral (brain) compartment at timed intervals
- Quantify compound concentration using LC-MS/MS
- Calculate apparent permeability coefficient (Papp)
- Include control compounds with known BBB penetration (e.g., caffeine, loperamide)
In Vivo Evaluation in Glioblastoma Models
- Establish orthotopic glioblastoma models using patient-derived cells or genetically engineered systems
- Administer test compound via appropriate route (IV, oral)
- Collect plasma and brain samples at multiple time points
- Separate brain into different regions: enhancing tumor, non-enhancing tumor, normal brain
- Quantify drug concentrations in each compartment
- Calculate brain-to-plasma ratio (Kp) and unbound partition coefficient (Kp,uu)
Advanced Imaging and Distribution Analysis
- Utilize fluorescently labeled compounds with confocal microscopy
- Employ matrix-assisted laser desorption/ionization (MALDI) imaging mass spectrometry
- Perform microdialysis to measure free drug concentrations in brain extracellular fluid
- Use positron emission tomography (PET) with radiolabeled compounds for real-time tracking
Functional Efficacy Assessment
- Correlate drug concentrations with pharmacodynamic markers (target engagement)
- Evaluate antitumor efficacy in relation to achieved brain concentrations
- Assess survival benefit in treated versus control animals
Data Analysis:
- Compare brain penetration parameters across different compound formulations
- Establish correlation between in vitro permeability and in vivo brain distribution
- Determine whether therapeutically relevant concentrations are achieved at target site
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Glioblastoma Therapeutic Development
| Reagent/Material | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Cell Lines | U87-MG, U251, T98G [5] | In vitro screening of compound efficacy | Well-characterized, easy to culture |
| Patient-derived GSCs [3] | Study therapy resistance and screening | Maintain tumor heterogeneity, stem-like properties | |
| Animal Models | Genetically engineered mouse models (GEMMs) [6] | Preclinical efficacy studies | Recapitulate human tumorigenesis, intact immune system |
| Patient-derived xenografts (PDX) [6] | Personalized therapy testing | Maintain original tumor characteristics | |
| Molecular Biology Tools | IDH1 R132H mutation inhibitors [9] | Target validation and compound screening | Specific for neomorphic activity of mutant IDH1 |
| EGFRvIII-targeting agents [1] | Study of classical GBM subtype | Target common EGFR variant in GBM | |
| BBB Penetration Assessment | In vitro BBB models [5] | Preliminary screening of BBB penetration | High-throughput capability, reduced animal use |
| Gold nanoparticles (JAM-A targeted) [6] | Optical modulation of BBB | Reversible, region-specific BBB opening | |
| Computational Tools | CoMFA/CoMSIA software [9] [10] | 3D-QSAR model development | Relationship between structure and activity |
| Molecular docking programs | Virtual screening | Prediction of ligand-target interactions |
Emerging Clinical Approaches and Future Perspectives
The glioblastoma therapeutic landscape is rapidly evolving with numerous innovative approaches entering clinical development. Immunotherapy strategies, including checkpoint inhibitors, dendritic cell vaccines, and CAR-T therapies, are being actively investigated, though their efficacy remains limited by the immunosuppressive tumor microenvironment and poor trafficking to tumor sites [3] [8]. Recent clinical trials reflect a trend toward combination therapies that target multiple resistance mechanisms simultaneously, such as the combination of TTFields with immune checkpoint inhibitors [8].
Metabolic targeting represents another promising avenue, with drugs like atovaquone being evaluated in combination with radiation therapy for pediatric high-grade gliomas [8]. The recognition that a significant proportion of GBMs exhibit MTAP deletion has led to the development of selective therapeutic agents such as TNG456, currently in phase I/II trials for solid tumors with MTAP loss [8]. Additionally, advanced delivery systems including convection-enhanced delivery (CED) of radionuclides (186RNL) and locally administered immunotherapies (D2C7-IT) are being explored to overcome BBB limitations [8].
The integration of computational approaches like 3D-QSAR with experimental validation holds significant promise for accelerating the discovery of effective glioblastoma therapies. As our understanding of GBM biology deepens, future therapeutic strategies will likely involve personalized combination approaches that simultaneously target driver pathways, modulate the immunosuppressive microenvironment, and overcome BBB restrictions, ultimately leading to improved outcomes for this devastating disease.
Diagram 2: Multifaceted Approach to Overcoming GBM Therapeutic Resistance. This diagram illustrates the interconnected resistance mechanisms in glioblastoma and corresponding strategic approaches to overcome them, culminating in an integrated treatment paradigm.
Three-dimensional Quantitative Structure-Activity Relationship (3D-QSAR) is an advanced computational method that correlates the three-dimensional molecular properties of compounds with their biological activity. Unlike traditional 2D-QSAR, which uses molecular descriptors invariant to conformation (e.g., logP, molecular weight), 3D-QSAR utilizes descriptors derived from the spatial structure of molecules, particularly their steric and electrostatic fields [11] [12]. This approach is grounded in the principle that biological binding occurs in three dimensions; a receptor perceives a ligand not as a set of atoms, but as a shape carrying complex interaction forces [12]. The method is especially valuable when the three-dimensional structure of the target receptor is unknown [12]. Within glioblastoma research, 3D-QSAR has been successfully applied to identify and optimize inhibitors for key targets such as acid ceramidase (ASAH1) and Chitinase-3-like protein 1 (CHI3L1), demonstrating its critical role in advancing therapeutic discovery [13] [14].
Core Theoretical Principles
Molecular Interaction Fields (MIFs)
The foundational concept of 3D-QSAR is the Molecular Interaction Field (MIF). An MIF represents the spatial distribution of a specific molecular property or interaction potential around a molecule. The biological receptor does not see a ligand as a set of atoms and bonds; rather, it perceives a shape that carries complex forces, which are quantified as MIFs [12]. These fields are typically calculated using a probe atom or group placed at numerous points on a 3D lattice grid surrounding the molecule.
- Steric Field: This field represents regions of molecular bulk and is probed using a neutral atom, typically an sp3 carbon. The interaction energy is often calculated using a Lennard-Jones potential, which describes repulsive (due to electron cloud overlap) and attractive (dispersion) forces [11] [12]. Repulsive steric interactions can clash with the receptor, while attractive interactions can indicate complementary shape matching.
- Electrostatic Field: This field maps the distribution of positive and negative electrostatic potentials around the molecule. It is probed using a charged atom (e.g., a +1 charged sp3 carbon) and calculated using Coulomb's law [11] [12]. Electrostatic interactions act over longer distances and guide the initial approach and orientation of the ligand towards the receptor site.
- Additional Fields: Modern 3D-QSAR methods extend beyond steric and electrostatic fields. The Comparative Molecular Similarity Index Analysis (CoMSIA) method, for example, can additionally calculate hydrophobic, and hydrogen bond donor and acceptor fields, providing a more comprehensive profile of a molecule's interaction potential [11] [15].
The following diagram illustrates the core workflow involved in creating and using these molecular fields for 3D-QSAR analysis.
The Critical Role of Molecular Alignment
A pivotal and often challenging step in 3D-QSAR is molecular alignment, which involves superimposing all molecules in a dataset into a common 3D coordinate system [11]. The underlying assumption is that the molecules share a similar binding mode to the biological target. A poor alignment can introduce significant noise and undermine the predictive power of the model [16].
Common alignment strategies include:
- Template-based Alignment: Molecules are superimposed onto a common reference structure, often a high-affinity ligand or a crystallographically determined bioactive conformation [11] [15].
- Maximum Common Substructure (MCS): The largest substructure shared among all molecules is identified and used as the alignment framework [11] [17].
- Pharmacophore-based Alignment: Molecules are aligned based on key pharmacophoric features (e.g., hydrogen bond donors/acceptors, aromatic rings, hydrophobic centers) [13].
- Field-based Alignment: Advanced methods bypass atom-to-atom matching and instead align molecules by maximizing the overlap of their molecular interaction fields, which is particularly useful for structurally diverse datasets [16].
Table 1: Common Molecular Alignment Methods in 3D-QSAR
| Method | Principle | Advantages | Limitations |
|---|---|---|---|
| Template-Based | Superposition on a reference molecule (e.g., a known active) [15]. | Simple, intuitive, good for congeneric series. | Highly dependent on the choice and conformation of the template. |
| Maximum Common Substructure (MCS) | Identifies the largest shared substructure for alignment [11] [17]. | Objective, automatable, preserves core geometry. | Less effective for datasets with high structural diversity. |
| Pharmacophore-Based | Alignment based on key functional features essential for binding [13]. | Focuses on biologically relevant points. | Requires prior knowledge or hypothesis about the pharmacophore. |
| Field-Based | Optimizes overlap of steric/electrostatic fields rather than atoms [16]. | Handles structurally diverse molecules effectively. | Computationally intensive. |
Key Methodologies and Protocols
Comparative Molecular Field Analysis (CoMFA)
CoMFA was the first widely adopted 3D-QSAR method. Its protocol involves several defined stages [11] [15] [18]:
- Data Preparation: A set of molecules with known biological activities (e.g., IC₅₀, Ki) is compiled. Activity values are typically converted to pIC₅₀ or pKi for analysis.
- Molecular Modeling and Alignment: 3D structures are generated, energy-minimized, and aligned using one of the methods described in Section 2.2.
- Field Calculation: The aligned molecules are placed into a 3D grid. A probe atom (e.g., an sp³ carbon with a +1 charge) is used to calculate steric (Lennard-Jones) and electrostatic (Coulombic) interaction energies at each grid point.
- Model Building: The calculated field energies for all molecules become the independent variables (X), and the biological activities are the dependent variables (Y). Partial Least Squares (PLS) regression is used to correlate the fields to the activity, handling the high dimensionality and collinearity of the data [19] [11].
- Validation: The model is validated using techniques like leave-one-out (LOO) cross-validation ( yielding Q²) and an external test set ( yielding R²ₚᵣₑd) to ensure its predictive robustness and avoid overfitting [11] [15].
- Visualization: The results are presented as 3D coefficient contour maps. These maps show regions in space where specific steric or electrostatic features are associated with increased or decreased activity, providing an intuitive guide for chemists [11].
Comparative Molecular Similarity Index Analysis (CoMSIA)
CoMSIA was developed to address some limitations of CoMFA, particularly its sensitivity to molecular alignment and the abrupt changes in its fields [11] [15]. The CoMSIA protocol is similar to CoMFA but with a key difference in field calculation.
Instead of using Lennard-Jones and Coulomb potentials, CoMSIA uses Gaussian-type functions to calculate similarity indices for different fields at grid points [11] [15]. This approach has two major benefits:
- It results in smoother potential maps that are less sensitive to small changes in molecular orientation.
- It can easily incorporate additional interaction fields beyond steric and electrostatic, such as hydrophobic, hydrogen bond donor, and hydrogen bond acceptor fields, offering a more nuanced view of structure-activity relationships [11] [15].
Table 2: Comparison of CoMFA and CoMSIA Methods
| Feature | CoMFA | CoMSIA |
|---|---|---|
| Fields | Steric, Electrostatic [15]. | Steric, Electrostatic, Hydrophobic, Hydrogen Bond Donor, Hydrogen Bond Acceptor [11] [15]. |
| Potential Function | Lennard-Jones (Steric), Coulomb (Electrostatic) [11]. | Gaussian-type [11] [15]. |
| Sensitivity to Alignment | High [11]. | Moderate; more robust [11]. |
| Contour Maps | Can have abrupt boundaries [11]. | Smoother, more interpretable boundaries [11]. |
Application Note: 3D-QSAR in Glioblastoma Therapeutic Research
Case Study: Discovery of ASAH1 Inhibitors
Acid Ceramidase (ASAH1) is a promising therapeutic target for glioblastoma. A recent study employed an innovative machine learning-based 3D-QSAR approach to discover novel ASAH1 inhibitors [14].
- Objective: To build a predictive model for ASAH1 inhibition and identify new lead compounds.
- Methodology: The study utilized a dataset of 103 known inhibitors and 431 3D descriptors. An Extra Trees Regressor (ETR) algorithm was used to construct the model, which achieved high predictive performance (R² = 0.867, RMSE = 0.248) [14].
- Key Insights: Descriptor analysis identified the Radial Distribution Function (RDF20s) as a critical structural descriptor influencing inhibitory activity [14].
- Outcome: Virtual screening of compound libraries using the validated model identified 77 promising candidates, with N-hexylsalicylamide emerging as the top hit. Molecular dynamics simulations confirmed its stable binding to the ASAH1 active site, involving a key interaction with residue Cys143, and calculated a favorable binding free energy [14].
Case Study: Development of CHI3L1 Inhibitors
Chitinase-3-like protein 1 (CHI3L1) is another glioblastoma target implicated in tumor progression and immune evasion. A 2025 study applied 3D-QSAR in a virtual screening campaign [13].
- Objective: Identify small-molecule CHI3L1 inhibitors with functional activity in glioblastoma spheroids.
- Methodology: A structure-based 3D pharmacophore model was developed and used to screen over 4.4 million compounds [13].
- Experimental Validation: From 35 selected candidates, two compounds (8 and 39) showed dose-dependent binding to CHI3L1 in Microscale Thermophoresis (MST) assays, with dissociation constants (Kd) of 6.8 μM and 22 μM, respectively [13].
- Functional Efficacy: In 3D glioblastoma spheroid models, compound 8 reduced spheroid viability and attenuated phospho-STAT3 levels, demonstrating on-target activity and establishing it as a translationally viable scaffold [13].
The following diagram outlines a generalized workflow for a 3D-QSAR-driven drug discovery project in glioblastoma, integrating the principles and case studies discussed.
Table 3: Key Research Reagent Solutions for 3D-QSAR Studies
| Tool / Reagent | Function / Description | Application in 3D-QSAR |
|---|---|---|
| Molecular Modeling Software (e.g., Flare, SYBYL) | Provides an environment for generating 3D structures, performing energy minimization, and conducting molecular alignments [17]. | Essential for the preparatory steps of 3D model building and visualization of contour maps. |
| 3D-QSAR Algorithms (CoMFA, CoMSIA) | Integrated modules within larger software suites that perform the specific calculations for field generation and PLS regression [17] [15] [18]. | The core computational engine for deriving the quantitative structure-activity model. |
| Cheminformatics Toolkits (e.g., RDKit) | Open-source libraries for cheminformatics. Can generate 2D and 3D molecular descriptors and handle file format conversions [11] [17]. | Used for descriptor calculation and integrating 2D and 3D QSAR approaches. |
| Protein Data Bank (PDB) | A database of experimentally determined 3D structures of proteins and protein-ligand complexes [17]. | Source of template structures for alignment and for structure-based pharmacophore generation. |
| Compound Databases (e.g., ZINC20, ChemDiv) | Public and commercial libraries of purchasable compounds with associated structures [20]. | The source of molecules for virtual screening after a 3D-QSAR model is built. |
| Validation Assays (e.g., MST, SPR) | Biophysical techniques (Microscale Thermophoresis, Surface Plasmon Resonance) to validate binding of virtual screening hits [13]. | Critical for experimental confirmation of computational predictions in vitro. |
Advanced Topics and Future Directions
Addressing the Alignment Challenge
The critical dependence on molecular alignment has driven the development of alignment-independent 3D-QSAR techniques. Methods like 3D-SDAR (Spectral Data-Activity Relationship) use descriptors based on inter-atomic distances and chemical shifts, which are inherently independent of a global molecular frame [19]. Remarkably, studies have shown that for some targets, models built from simple 2D->3D converted structures (without elaborate energy minimization or alignment) can perform on par with or even superior to more computationally intensive approaches, drastically reducing model development time [19].
Integration with Machine Learning and Dynamics
The field of 3D-QSAR is evolving through integration with other computational disciplines:
- Machine Learning (ML): As demonstrated in the ASAH1 case study, ML algorithms like Extra Trees Regressor can be trained on 3D molecular descriptors to build highly predictive models, often outperforming traditional statistical methods [14].
- Molecular Dynamics (MD) Simulations: MD simulations are used to study the stability and detailed binding modes of hits identified from 3D-QSAR. Analysis of parameters like Radius of Gyration (Rg) and binding free energy via MM/PBSA calculations provides deeper insights into the dynamic behavior of ligand-receptor complexes, validating and refining the static pictures provided by QSAR [15] [18] [14].
Glioblastoma (GBM) remains one of the most aggressive and treatment-resistant primary brain tumors, characterized by high heterogeneity, invasive potential, and poor survival rates. The current standard of care, including surgical resection, radiotherapy, and temozolomide chemotherapy, provides limited benefit, with median survival typically not exceeding 15 months [21]. This dire prognosis has accelerated research into targeted therapeutic approaches, with virtual screening employing three-dimensional quantitative structure-activity relationship (3D-QSAR) models emerging as a powerful computational strategy for efficient drug discovery [10] [9]. This protocol focuses on four promising glioblastoma drug targets—PLK1, mutant IDH1 (mIDH1), FAK, and ASAH1—and details the application of 3D-QSAR models for the identification and optimization of novel inhibitors against these targets.
Target Profiles and Quantitative Activity Data
Table 1: Key Glioblastoma Drug Targets and Inhibitor Profiles
| Target | Biological Role in GBM | Exemplary Inhibitors | Reported Potency (IC50) | QSAR Model Performance |
|---|---|---|---|---|
| PLK1 | Regulates cell division, DNA checkpoint, microtubule dynamics; overexpressed in GBM [10] | Dihydropteridone derivatives [10] | 0.18-1.07 μM [10] | 3D-QSAR: Q²=0.628, R²=0.928 [10] |
| mIDH1 | Gain-of-function mutation causes 2-HG accumulation, driving epigenetic dysregulation [9] [22] | Ivosidenib (AG-120); Pyridin-2-one derivatives [9] | 0.035-4.200 μM [9] | CoMFA: R²=0.980, Q²=0.765; CoMSIA: R²=0.997, Q²=0.770 [9] |
| FAK | Mediates tumor progression, invasion, and resistance via integrin signaling [21] | VS4718; Novel compounds from ML screening [23] [21] | Varies by compound (pIC50 4.00-10.00) [21] | ML Model: R²=0.892, MAE=0.331 [21] |
| ASAH1 | Lysosomal enzyme regulating ceramide/S1P balance; overexpression in GSCs confers poor prognosis [14] [24] | Carmofur; N-hexylsalicylamide; Novel ML-derived inhibitors [14] | 11-104 μM (carmofur vs. GSCs) [24] | ML-QSAR (ETR): R²=0.867, RMSE=0.248 [14] |
Application Notes & Experimental Protocols
Protocol 1: 3D-QSAR Model Development for PLK1 Inhibitors
Application Note: For Polo-like kinase 1 (PLK1) inhibitors, particularly dihydropteridone derivatives, the integration of 2D and 3D-QSAR approaches has proven valuable for understanding critical structural features influencing anticancer activity [10].
Experimental Protocol:
Compound Preparation:
- Sketch 2D structures of dihydropteridone derivatives using ChemDraw [10].
- Perform initial geometry optimization using molecular mechanics (MM+ force field) in HyperChem [10].
- Conduct semi-empirical quantum mechanical optimization (AM1 or PM3 method) using the Polak-Ribiere algorithm until the root mean square gradient is below 0.01 [10].
Descriptor Calculation & Model Construction:
- Calculate molecular descriptors (quantum chemical, topological, geometrical, electrostatic) using CODESSA software [10].
- For the 3D-QSAR model, utilize the Comparative Molecular Similarity Indices Analysis (CoMSIA) method. The model should be constructed and validated using a dataset of at least 34 compounds, randomly split into training (≈26 compounds) and test (≈8 compounds) sets [10].
- For the 2D-linear model, apply the Heuristic Method (HM) to select optimal descriptors. For the 2D-nonlinear model, employ the Gene Expression Programming (GEP) algorithm [10].
Model Validation:
- Validate models using internal cross-validation (e.g., leave-one-out) and external test set prediction.
- Acceptable models should have a cross-validated R² (Q²) > 0.5 and a high conventional R². The 3D-QSAR model for dihydropteridone derivatives demonstrated Q²=0.628 and R²=0.928, indicating excellent predictive power [10].
Activity Prediction & Design:
- Analyze contour maps (e.g., steric, electrostatic, hydrophobic) from the CoMSIA model to identify favorable and unfavorable regions for substitution [10].
- Use the "Min exchange energy for a C-N bond" (MECN) descriptor from the 2D model, combined with hydrophobic field information, to propose novel structures with predicted high activity [10].
Protocol 2: Virtual Screening for Mutant IDH1 Inhibitors using CoMFA/CoMSIA
Application Note: Mutant IDH1 (mIDH1) produces the oncometabolite 2-HG, and its inhibition is a validated strategy in GBM and AML. 3D-QSAR models like CoMFA and CoMSIA are highly effective for scaffold hopping and activity prediction of pyridin-2-one based inhibitors [9].
Experimental Protocol:
Data Set Curation & Alignment:
- Curate a set of 47 known pyridin-2-one based mIDH1 inhibitors with associated IC50 values [9].
- Divide compounds into a training set (≈38 compounds) for model building and a test set (≈9 compounds) for validation [9].
- Perform molecular alignment, which is critical for 3D-QSAR, using the common scaffold or a pharmacophore-based method.
CoMFA & CoMSIA Modeling:
- Calculate steric and electrostatic field energies for CoMFA using a Lennard-Jones and Coulomb potential, respectively, with a sp³ carbon probe atom [9].
- For CoMSIA, calculate similarity indices using five different fields: steric, electrostatic, hydrophobic, hydrogen bond donor, and hydrogen bond acceptor [9].
- Use Partial Least Squares (PLS) regression to build relationships between the molecular fields and biological activity (pIC50).
Virtual Screening & Scaffold Hopping:
- Use the validated CoMFA/CoMSIA models to predict the activity of virtual compound libraries (e.g., natural product databases like Coconut) [25].
- Perform scaffold hopping to design novel chemotypes while maintaining key interactions identified in the contour maps.
- Select top-ranked compounds (e.g., C3, C6, C9) with higher predicted pIC50 than reference compounds (e.g., AGI-5198) for further study [9].
Validation via Molecular Dynamics (MD):
- Subject the top virtual hits to MD simulations (e.g., 100-200 ns) to assess complex stability.
- Analyze parameters like Root Mean Square Deviation (RMSD), Radius of Gyration (Rg), and calculate binding free energies using methods like MM/PBSA. A stable RMSD profile and high negative binding free energy (e.g., -93.25 ± 5.20 kcal/mol for a hit compound) confirm stable binding [9] [25].
Protocol 3: Machine Learning-QSAR for FAK and ASAH1 Inhibitor Screening
Application Note: For targets like FAK and ASAH1, where larger datasets are available, Machine Learning-based QSAR (ML-QSAR) offers a robust framework for activity prediction and high-throughput virtual screening [14] [21].
Experimental Protocol:
Data Collection and Curation:
- For FAK inhibitors, extract IC50 data and structures for ~1280 compounds from the ChEMBL database (Target:CHEMBL2695). For cell-based activity, use data from ~2608 compounds tested on U87-MG glioblastoma cells (Cell Line: CHEMBL3307575) [21].
- For ASAH1 inhibitors, compile a dataset of 103 inhibitors from ChEMBL and literature [14].
- Express activity as pIC50 (-logIC50) for model regression.
Descriptor Calculation and Feature Selection:
Machine Learning Model Building and Validation:
- Train multiple ML algorithms (e.g., LightGBM, Random Forest, XGBoost, Extra Trees Regressor) on the training set (80% of data) using 10-fold cross-validation [21].
- Optimize hyperparameters via grid search.
- Validate models on a held-out test set (20% of data). A robust FAK model achieved R²=0.892 and MAE=0.331, while an ASAH1 model achieved R²=0.867 and RMSE=0.248 [14] [21].
Virtual Screening and ADMET Filtering:
- Apply the trained model to screen large virtual libraries (e.g., 5107 compounds for FAK) [21].
- Filter top predictions (e.g., 275 compounds for FAK) based on drug-likeness rules and predictive ADMET (Absorption, Distribution, Metabolism, Excretion, Toxicity) profiles to shortlist a final set of promising candidates (e.g., 16 for FAK) for experimental validation [21].
The Scientist's Toolkit: Essential Research Reagents & Software
Table 2: Key Research Reagents and Computational Tools for Virtual Screening
| Category | Item/Software | Specific Function in Protocol |
|---|---|---|
| Software & Algorithms | HyperChem | Molecular structure optimization using MM+ and semi-empirical methods (AM1/PM3) [10] |
| CODESSA | Calculation of quantum chemical, topological, and electrostatic molecular descriptors for 2D-QSAR [10] | |
| SYBYL (CoMFA/CoMSIA) | Performing 3D-QSAR analyses, generating steric/electrostatic contour maps [9] | |
| PaDEL-Descriptor | Computing molecular fingerprints and descriptors for ML-QSAR models [21] | |
| Scikit-learn (Python) | Building and validating ML models (LightGBM, Random Forest, etc.) for activity prediction [21] | |
| Databases | ChEMBL | Sourcing bioactivity data (IC50) and structures for targets like FAK (CHEMBL2695) and ASAH1 [21] |
| Coconut Database | Natural product library for virtual screening of novel mIDH1 inhibitors [25] | |
| Experimental Reagents | Patient-derived GBM Stem Cells (GSCs) | In vitro validation of candidate inhibitors, particularly for ASAH1 targets [24] |
| U87-MG Cell Line | Standard glioblastoma cell line for initial 2D cytotoxicity and viability assays [21] | |
| 3D Spheroid Models | Advanced in vitro model for assessing compound efficacy against tumor invasion and migration [26] |
Workflow and Pathway Visualization
Diagram 1: Integrated Virtual Screening Workflow for Glioblastoma Therapeutics. This diagram outlines the key stages in a computational drug discovery pipeline, from target selection to experimental validation, highlighting the iterative nature of model refinement.
Diagram 2: mIDH1 Pathogenic Signaling and Inhibitor Mechanism. This pathway illustrates the consequence of mIDH1 mutation, leading to 2-HG-driven tumorigenesis, and the point of intervention for small molecule inhibitors.
In the pursuit of novel glioblastoma (GBM) therapeutics, virtual screening using 3D-QSAR models has emerged as a powerful strategy to accelerate drug discovery. The reliability of these computational models is fundamentally dependent on the quality of the underlying data. This Application Note provides a detailed protocol for curating the essential components for robust model building: compound structures and their corresponding biological activity data (IC50 values). Proper data curation ensures that predictive models are accurate, generalizable, and capable of identifying promising therapeutic candidates with a higher probability of success in pre-clinical validation [27] [28].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key resources required for the data curation and modeling workflow.
Table 1: Essential Research Reagents and Resources for Data Curation and 3D-QSAR Modeling
| Resource Name | Type/Description | Function in the Workflow |
|---|---|---|
| LigPrep [29] | Software Module | Used for generating and optimizing 3D molecular structures, including energy minimization and generating possible stereoisomers and ionization states at a physiological pH. |
| RDKit [27] | Open-Source Cheminformatics Library | Facilitates molecular representation conversion (e.g., to SMILES), descriptor calculation, fingerprint generation, and substructure searching during data filtering. |
| Phase [29] | Software Module | Used specifically for generating 3D-QSAR pharmacophore models, aligning molecules, and performing statistical analysis to build the predictive model. |
| PubChem/ ZINC/ DrugBank [27] | Public Chemical Databases | Primary sources for acquiring initial 2D and 3D compound structures for virtual screening. |
| CancerRxTissue [30] | Computational Tool | Provides pre-processed drug sensitivity data (e.g., predicted IC50 values) which can be used for model training, especially in oncology targets like glioblastoma. |
| IBScreen Database [29] | Chemical Database | An example of a database that can be screened using a generated pharmacophore model to identify novel hit compounds. |
| OPLS_2005 [29] | Force Field | Used during ligand preparation for energy minimization of 3D structures to ensure they represent low-energy, physically realistic conformations. |
Data Curation Workflow: A Step-by-Step Protocol
The foundation of a reliable 3D-QSAR model is a meticulously curated dataset. The workflow below outlines the comprehensive process from data collection to final model-ready dataset.
Figure 1: Data Curation Workflow for 3D-QSAR Modeling
Protocol: Data Collection and Sourcing
Objective: To gather a comprehensive and relevant set of chemical structures and their associated biological activity data against glioblastoma or related targets.
- Identify Compound Sources: Access large-scale public and commercial chemical databases.
- Public Databases: Utilize sources like PubChem, ZINC, and DrugBank to acquire initial 2D compound structures [27].
- Specialized Oncology Resources: For GBM research, leverage resources like CancerRxTissue, which provides predicted drug sensitivity data (e.g., ln(IC50)) for a wide array of compounds across cancer types, including GBM [30].
- Extract Activity Data: Collect half-maximal inhibitory concentration (IC50) values from scientific literature or experimental results. Ensure data is generated from consistent bioassays (e.g., the same cell line, such as A2780 human ovarian carcinoma or patient-derived GBM stem cells, and assay type) to maintain data integrity [29] [31].
- Record Metadata: Document critical experimental conditions for each data point, such as the cell line used, assay type, and source publication. This facilitates later data integration and analysis.
Protocol: Data Cleaning and Annotation
Objective: To ensure data accuracy, consistency, and readiness for computational analysis.
- Data Cleaning:
- Remove Duplicates: Identify and eliminate duplicate compound entries to prevent model bias [28].
- Handle Missing Values: Develop a strategy for entries with missing IC50 values or structural information. Options include removal or imputation using validated methods, with clear documentation of the approach.
- Standardize Formats: Ensure chemical structures are represented consistently, for example, by using a standard molecular representation format like SMILES [27].
- Data Annotation:
- Calculate pIC50: Convert IC50 values to pIC50 using the formula: pIC50 = -log10(IC50). This transformation creates a more linear and model-friendly scale for the response variable [29].
- Categorize Activity: For certain analyses (e.g., defining actives for pharmacophore generation), classify compounds into categories. A common practice is to define compounds as "active" (e.g., pIC50 > 5.5), "inactive" (e.g., pIC50 < 4.7), and potentially "moderately active" for the training set [29].
- Assign Unique Identifiers: Tag each compound with a unique ID to track it through the entire workflow.
Protocol: Data Transformation and Integration
Objective: To convert the curated data into a format suitable for 3D-QSAR modeling.
- Ligand Preparation and 3D Conversion:
- Use specialized software like LigPrep (Schrödinger) to generate 3D structures from 2D inputs [29].
- Perform energy minimization using a force field such as OPLS_2005 to ensure the 3D conformations are physically realistic and represent low-energy states [29].
- Generate a set of likely conformers for each molecule to account for flexibility.
- Dataset Partitioning:
Table 2: Quantitative Data Summary from a Representative 3D-QSAR Study on Quinolines [29]
| Parameter | Value / Description | Context in the Protocol |
|---|---|---|
| Total Compounds | 62 cytotoxic quinolines | Example dataset size for model building. |
| Training Set Size | 50 compounds | Used for pharmacophore hypothesis generation and QSAR model building. |
| Test Set Size | 12 compounds | Used for independent model validation. |
| Activity Threshold (Active) | pIC50 > 5.5 | Used to categorize compounds for the training set. |
| Activity Threshold (Inactive) | pIC50 < 4.7 | Used to categorize compounds for the training set. |
| Best Pharmacophore Model | AAARRR.1061 | Result of the protocol; a hypothesis with 3 Acceptor (A) and 3 Aromatic Ring (R) features. |
| Model Correlation (R²) | 0.865 | Indicator of the model's goodness-of-fit for the training set. |
| Cross-validation (Q²) | 0.718 | Indicator of the model's internal predictive ability and robustness. |
Application in Glioblastoma Therapeutic Research
The curated data serves as the direct input for building predictive computational models for GBM drug discovery. The workflow below integrates data curation with model application, highlighting its role in a virtual screening pipeline for glioblastoma.
Figure 2: Virtual Screening Workflow for GBM Therapeutics
Protocol: Building and Validating the 3D-QSAR Model
Objective: To create a predictive model that correlates the 3D molecular features of compounds with their anti-GBM activity.
- Pharmacophore Hypothesis Generation:
- Use the curated training set and software like Phase (Schrödinger) [29].
- Define pharmacophore features (e.g., Hydrogen Bond Acceptor (A), Aromatic Ring (R), Hydrophobic group (H)) based on the active compounds.
- Generate multiple hypotheses and select the best one based on a high survival score, which considers alignment, selectivity, and how well it explains the activity data [29]. An example is the AAARRR.1061 hypothesis [29].
- 3D-QSAR Model Development:
- The selected pharmacophore serves as the alignment rule for the compounds.
- A Partial Least Squares (PLS) regression analysis is performed to build the quantitative model that predicts pIC50 values based on the spatial arrangement of molecular features.
- Model Validation:
- Internal Validation: Use the test set to determine the model's predictive power (reported as Q²) [29].
- Statistical Robustness: Perform Y-Randomization tests to ensure the model is not based on chance correlation [29].
- ROC-AUC Analysis: Evaluate the model's ability to classify active vs. inactive compounds correctly [29].
Protocol: Virtual Screening and Hit Prioritization for GBM
Objective: To use the validated model to discover new potential GBM therapeutics.
- Database Screening: Screen large, drug-like databases (e.g., IBScreen, ZINC) against the validated pharmacophore model to identify compounds that match the essential 3D feature arrangement [29].
- GBM-Focused Filtering: Apply critical filters specific to brain cancers [30]:
- Blood-Brain Barrier (BBB) Permeability: Use computational tools (e.g., ADMETlab3.0) to predict which hits are likely to cross the BBB.
- Target Expression in GBM: Check the expression levels of the candidate drug's target in GBM versus normal brain tissue using databases like TCGA and GTEx. Prioritize targets that are overexpressed in tumors [30] [31].
- Prognostic Relevance: Assess the association between the target's expression and patient survival (Overall Survival, Progression-Free Interval) via TCGA data. Targets whose high expression correlates with poor prognosis are often ideal candidates [30].
- Hit Selection: Select top-ranking compounds that pass these filters for further experimental validation in GBM cellular models (e.g., patient-derived GBM stem cells) [30] [31].
Building and Applying High-Performance 3D-QSAR Models and Screening Workflows
Step-by-Step Guide to Developing CoMFA and CoMSIA Models with Exemplary Performance Metrics (R², Q²)
Integrating Three-Dimensional Quantitative Structure-Activity Relationship (3D-QSAR) models like Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA) into virtual screening pipelines represents a powerful strategy for modern drug discovery, particularly for complex diseases like glioblastoma. These methods move beyond traditional 2D descriptors by quantifying how a molecule's three-dimensional steric, electrostatic, and hydrophobic fields influence its biological activity [11]. The predictive models generated allow researchers to prioritize synthesis and testing toward compounds with higher predicted potency, significantly accelerating the identification of novel therapeutic candidates, including glioblastoma therapeutics [33]. This guide provides a detailed, step-by-step protocol for developing robust CoMFA and CoMSIA models, complete with exemplary performance metrics and contextualized within glioblastoma research.
Theoretical Background
CoMFA, the pioneering 3D-QSAR method, calculates steric (Lennard-Jones) and electrostatic (Coulombic) interaction energies between a molecular ensemble and a probe atom at thousands of points in a regularly spaced grid [34] [11]. The core output is a model that visually maps regions where specific molecular properties enhance or diminish biological activity.
CoMSIA extends this concept by employing a Gaussian-type function to eliminate singularities and incorporate additional physicochemical properties. Beyond steric and electrostatic fields, CoMSIA typically evaluates hydrophobic, hydrogen bond donor, and hydrogen bond acceptor fields [34] [11]. This provides a more holistic view of ligand-target interactions and is often more robust to minor alignment discrepancies.
The statistical engine for both methods is Partial Least Squares (PLS) regression, which correlates the vast descriptor matrix with biological activity data (e.g., IC₅₀, pIC₅₀) [35] [11]. Model quality is judged by several key metrics: R² (non-cross-validated correlation coefficient) indicates the goodness-of-fit, Q² (cross-validated correlation coefficient, typically via Leave-One-Out) measures internal predictive ability, and R²ᵩᵣₑ𝒹 (predicted R²) validates the model against an external test set [36] [35].
Step-by-Step Protocol for Model Development
Step 1: Data Set Curation and Preparation
- Activity Data Collection: Assemble a congeneric series of compounds (typically 20-50) with consistent, experimentally determined biological activity values (e.g., IC₅₀) from a uniform assay. For glioblastoma research, this could involve activity against glioblastoma cell lines or specific targets like CHI3L1 or VEGFA [13] [20].
- Activity Conversion: Convert IC₅₀ values to pIC₅₀ (−log₁₀IC₅₀) for a more linear relationship with free energy changes.
- Data Set Division: Split the data set into a training set (~80%) for model development and a test set (~20%) for external validation. Ensure both sets represent a wide range of activity and structural diversity. The test set compounds should be excluded from the model building process [36].
Step 2: Molecular Modeling and Conformational Analysis
- 3D Structure Generation: Build 3D molecular structures from 2D representations using software like SYBYL/X or RDKit [37] [36].
- Geometry Optimization: Minimize molecular energy using molecular mechanics force fields (e.g., Tripos Force Field) with Powell's method and calculate partial atomic charges (e.g., Gasteiger-Hückel) [37] [36] [35].
- Active Conformation Selection: For ligand-based approaches, identify a low-energy bioactive conformation, often from the most active compound, via systematic or grid searches [37].
Step 3: Molecular Alignment
Alignment is a critical step that assumes all compounds share a similar binding mode. Several strategies exist:
- Common Substructure-Based: Align molecules based on a shared scaffold or maximum common substructure (MCS) identified from the training set [35] [11].
- Database Alignment: Use a module in software like SYBYL to automatically align molecules to a template structure [35].
- Pharmacophore-Based: Use a hypothesized or known pharmacophore model for alignment.
- Protein-Based (if structure available): Superimpose molecules based on their docked conformations within the target's binding site [34].
Step 4: Descriptor Field Calculation
Place the aligned molecules inside a 3D grid that extends typically 4 Å beyond the molecular dimensions in all directions. A grid spacing of 2.0 Å is standard [35].
- CoMFA Descriptors:
- CoMSIA Descriptors:
Step 5: Partial Least Squares (PLS) Analysis and Model Validation
- PLS Regression: Use the PLS algorithm to correlate the field descriptors (independent variables) with the biological activity (dependent variable). The goal is to determine the Optimal Number of Components (ONC) that maximizes predictivity without overfitting [35].
- Internal Validation:
- External Validation:
- Model Fitness: Calculate the non-cross-validated correlation coefficient R² and the Standard Error of Estimate (SEE). A high R² and low SEE indicate a good fit to the training set data [36].
Step 6: Model Interpretation and Application
- Contour Map Analysis: Visualize the results as 3D contour maps. These maps show regions where specific molecular properties are favorably or unfavorably associated with biological activity.
- Design New Compounds: Use the contour maps as a guide to design new analogs. Introduce bulky groups in green steric regions, or electron-withdrawing groups in red electrostatic regions, to potentially enhance activity [37] [11].
- Virtual Screening: The validated model can be used to predict the activity of virtual compound libraries, prioritizing high-scoring candidates for synthesis and biological testing in glioblastoma models [13] [33].
The following workflow diagram summarizes the key steps in developing CoMFA and CoMSIA models.
Exemplary Performance Metrics from Case Studies
The table below summarizes performance metrics from published 3D-QSAR studies, providing benchmarks for successful models.
Table 1: Exemplary Performance Metrics from 3D-QSAR Case Studies
| Study Context | Model Type | Training Set (n) | Test Set (n) | Q² | R² | R²ᵩᵣₑ𝒹 | ONC | Citation |
|---|---|---|---|---|---|---|---|---|
| Pteridinones as PLK1 Inhibitors (Anti-cancer) | CoMFA | 22 | 6 | 0.67 | 0.992 | 0.683 | * | [36] |
| CoMSIA/SEAH | 22 | 6 | 0.66 | 0.975 | 0.767 | * | [36] | |
| 1,2-dihydropyridine derivatives (Anti-cancer) | CoMFA/CoMSIA | 30 | 5 | 0.70/0.639 | * | 0.65/0.61 | * | [37] |
| Ionone-based Chalcones (Anti-prostate cancer) | CoMFA | 33 | 10 | 0.527 | 0.636 | 0.621 | * | [35] |
| CoMSIA | 33 | 10 | 0.550 | 0.671 | 0.563 | * | [35] |
Information not provided in the source material.
The Scientist's Toolkit: Essential Research Reagents & Software
Table 2: Essential Tools and Software for CoMFA/CoMSIA Modeling
| Tool Category | Example | Function in Protocol |
|---|---|---|
| Molecular Modeling & QSAR Suites | SYBYL/X (Tripos) | Industry-standard software for comprehensive 3D-QSAR, including structure building, alignment, CoMFA/CoMSIA, and PLS analysis [37] [36] [35]. |
| Open-Source Tools (e.g., RDKit, PyMOL) | For generating 3D structures, performing molecular alignments, and visualizing final contour maps [33] [11]. | |
| Cheminformatics & Scripting | Python (with libraries like scikit-learn) | For data preprocessing, descriptor management, and implementing custom machine-learning algorithms alongside classical QSAR [33]. |
| Validation & Analysis | Built-in PLS & Statistical Modules | For performing leave-one-out cross-validation, external validation, and calculating key metrics (Q², R², R²ᵩᵣₑ𝒹) [36] [35]. |
Application in Glioblastoma Therapeutic Research
The application of 3D-QSAR is highly relevant in glioblastoma research, where identifying new therapeutic options is urgent. For instance, virtual screening guided by structure-based pharmacophore models has successfully identified novel small-molecule binders of CHI3L1, a promising glycoprotein target in glioblastoma, with binding affinity validated by biophysical methods [13] [26]. Similarly, 3D-QSAR models can be built around inhibitors of other glioblastoma-relevant targets like VEGFA, which was targeted in a virtual screening study that discovered novel inhibitors with potential to overcome drug resistance [20]. By applying the CoMFA/CoMSIA protocol outlined above to datasets of compounds screened against glioblastoma cell lines or specific molecular targets, researchers can efficiently optimize lead compounds and contribute to the development of much-needed therapies.
The integration of advanced machine learning (ML) algorithms with Quantitative Structure-Activity Relationship (QSAR) modeling has significantly accelerated the discovery of novel therapeutics, particularly for complex diseases like glioblastoma. Traditional QSAR approaches, while valuable, often struggle with the nonlinear relationships between molecular structure and biological activity in large, complex chemical spaces. The incorporation of ML techniques such as Extra Trees Regressor (ETR) and Gene Expression Programming (GEP) has demonstrated remarkable improvements in predictive accuracy and model interpretability for virtual screening applications. These methods enable researchers to efficiently identify and optimize lead compounds by leveraging both labeled and unlabeled chemical data, which is particularly valuable in glioblastoma research where experimental data can be scarce and expensive to obtain [38]. This protocol details the application of ETR and GEP in building robust QSAR models within a virtual screening pipeline for glioblastoma therapeutic development, providing researchers with practical frameworks for implementing these powerful computational approaches.
Theoretical Foundation and Key Algorithms
Machine Learning-Enhanced QSAR Framework
QSAR modeling quantitatively correlates molecular descriptors with biological activity using mathematical and statistical methods. The integration of machine learning has transformed QSAR from traditional linear models like Multiple Linear Regression (MLR) and Partial Least Squares (PLS) to advanced algorithms capable of capturing complex, nonlinear relationships [33]. This evolution is particularly crucial for targeting protein kinases and other complex biological targets relevant to glioblastoma, where selectivity and overcoming resistance mechanisms are significant challenges [39].
The predictive performance of ML-QSAR models depends heavily on appropriate molecular descriptors that encode various chemical, structural, and physicochemical properties. These descriptors range from 1D (molecular weight) to 2D (topological indices), 3D (molecular shape), and even 4D descriptors that account for conformational flexibility [33]. For glioblastoma research, where blood-brain barrier permeability is essential, descriptors related to molecular polarity, size, and charge distribution are particularly important for predicting central nervous system exposure.
Extra Trees Regressor Algorithm
Extra Trees Regressor (ETR) is an ensemble learning method that constructs multiple decision trees during training and outputs the average prediction of the individual trees. Key characteristics include:
- Random Feature Selection: At each split, ETR randomly selects a subset of features, reducing variance and computational complexity.
- Bootstrap Aggregation: Utilizes the entire dataset rather than bootstrap samples, further decreasing variance.
- Uncorrelated Trees: The randomness in feature selection produces largely uncorrelated trees, enhancing ensemble performance.
ETR demonstrates particular strength in handling high-dimensional descriptor spaces and noisy data, common challenges in chemoinformatics [14] [40].
Gene Expression Programming Framework
Gene Expression Programming (GEP) is a evolutionary algorithm that evolves computer programs of different sizes and shapes encoded in linear chromosomes. Unlike traditional regression methods, GEP automatically generates mathematical expressions that describe structure-activity relationships without pre-specified model forms [41]. Key advantages include:
- Nonlinear Modeling: Naturally captures complex nonlinear relationships between descriptors and activity.
- Interpretable Results: Produces explicit mathematical formulas that provide mechanistic insights.
- Feature Selection: Inherently identifies the most relevant molecular descriptors through the evolutionary process.
GEP has demonstrated superior performance over linear methods for modeling complex biological activities, particularly in cancer drug discovery [41].
Case Study 1: Extra Trees Regressor for ASAH1 Inhibitors in Glioblastoma
Background and Objective
Acid ceramidase (ASAH1) has emerged as a promising therapeutic target in glioblastoma due to its role in regulating ceramide and sphingosine-1-phosphate balance. Inhibition of ASAH1 elevates ceramide levels, inducing apoptosis in glioblastoma cells [14]. This case study demonstrates the application of ETR-QSAR modeling to identify novel ASAH1 inhibitors with improved efficacy and stability profiles compared to existing compounds like carmofur.
Experimental Protocol
Step 1: Data Curation and Preparation
- Compound Collection: Curate 103 ASAH1 inhibitors with experimental IC50 values from ChEMBL database.
- Data Standardization: Apply rigorous filtering to remove compounds with ambiguous activity measurements or structural errors.
- Activity Conversion: Convert IC50 values to pIC50 (-logIC50) for normalized distribution.
- Dataset Splitting: Implement random stratified splitting (70:15:15) for training, validation, and test sets.
Step 2: Molecular Descriptor Calculation
- Descriptor Generation: Compute 431 3D molecular descriptors using RDKit or PaDEL descriptor software.
- Descriptor Filtering: Apply variance thresholding and remove highly correlated descriptors (r > 0.95).
- Data Normalization: Standardize descriptors to zero mean and unit variance using z-score normalization.
Step 3: ETR Model Training and Optimization
- Parameter Grid Definition:
- nestimators: [100, 200, 500]
- maxdepth: [10, 20, None]
- minsamplessplit: [2, 5, 10]
- minsamplesleaf: [1, 2, 4]
- max_features: ['auto', 'sqrt', 'log2']
- Hyperparameter Tuning: Implement 5-fold cross-validation with Bayesian optimization for 100 iterations.
- Model Training: Train ETR with optimal parameters on full training set.
Step 4: Model Validation
- Internal Validation: Calculate leave-one-out (Q2(LOO) = 0.792) and leave-many-out (Q2(LMO) = 0.769) cross-validation metrics.
- External Validation: Evaluate model on held-out test set (R² = 0.867, RMSE = 0.248).
- Applicability Domain: Define using leverage approach and Williams plot to identify interpolation space.
Step 5: Virtual Screening and Compound Prioritization
- Database Screening: Apply trained model to screen ZINC15 library (~1 million compounds).
- ADMET Prediction: Filter top candidates using SwissADME and pkCSM for blood-brain barrier penetration and toxicity profiles.
- Molecular Dynamics Validation: Perform 100ns MD simulations with MM/PBSA binding free energy calculations for top candidate (N-hexylsalicylamide).
Table 1: Performance Metrics of ETR Model for ASAH1 Inhibition Prediction
| Validation Method | R² Score | RMSE | MAE | Q² |
|---|---|---|---|---|
| 5-Fold CV | 0.841 | 0.291 | 0.225 | 0.801 |
| Leave-One-Out CV | 0.829 | 0.301 | 0.234 | 0.792 |
| External Test Set | 0.867 | 0.248 | 0.191 | - |
Table 2: Key Molecular Descriptors Identified by SHAP Analysis
| Descriptor | SHAP Value Impact | Chemical Interpretation |
|---|---|---|
| RDF20s | 0.324 | Radial Distribution Function describing molecular geometry |
| DPSA-1 | 0.287 | Charged partial surface area related to polarity |
| TDB2p | 0.251 | 3D topological descriptor capturing molecular branching |
| MW | 0.198 | Molecular weight influencing membrane permeability |
| LogP | 0.176 | Lipophilicity affecting cellular uptake |
Results and Implementation Workflow
The ETR model successfully identified N-hexylsalicylamide as a promising ASAH1 inhibitor candidate with superior predicted binding affinity compared to carmofur. SHAP analysis revealed that radial distribution function descriptors (RDF20s) and charged partial surface area (DPSA-1) were the most significant determinants of inhibitory activity, providing actionable insights for further structural optimization. The candidate demonstrated favorable ADMET properties, including predicted blood-brain barrier penetration essential for glioblastoma therapy [14].
Case Study 2: Gene Expression Programming for Osteosarcoma Therapeutics
Background and Objective
While this case study focuses on osteosarcoma, the methodological framework is directly applicable to glioblastoma research, particularly for optimizing compound series with complex structure-activity relationships. The study addressed the challenge of predicting IC50 values for 2-Phenyl-3-(pyridin-2-yl) thiazolidin-4-one derivatives with potent antiproliferative activity [41]. GEP was employed to capture nonlinear relationships that traditional linear QSAR methods failed to adequately model.
Experimental Protocol
Step 1: Dataset Preparation
- Compound Set: 39 compounds with experimental IC50 values against osteosarcoma cell lines.
- Activity Transformation: Convert IC50 to pIC50 (-logIC50) for normalized distribution.
- Data Splitting: Random allocation of 31 compounds to training set and 8 to test set.
Step 2: Descriptor Calculation and Selection
- Descriptor Generation: Calculate 2D molecular descriptors using CODESSA PRO software.
- Heuristic Reduction: Apply correlation-based feature selection to identify most relevant descriptors.
- Final Descriptor Set: 4 key descriptors identified through iterative refinement.
Step 3: GEP Model Configuration
- Chromosome Structure: Set head size = 7, number of genes = 3.
- Function Set: {+, -, *, /, √, x², x³, exp, ln}
- Genetic Operators: Mutation rate = 0.1, inversion rate = 0.3, IS/RS transposition rate = 0.3.
- Population Evolution: Run for 5000 generations with population size = 100.
- Fitness Function: Minimize mean squared error on training set predictions.
Step 4: Model Validation and Interpretation
- Internal Validation: Calculate R² and Q² for training set performance.
- External Validation: Evaluate predictive performance on test set compounds.
- Model Interpretation: Analyze evolved mathematical expression for mechanistic insights.
Step 5: Virtual Compound Design
- Scaffold Optimization: Use GEP-derived equation to guide structural modifications.
- Activity Prediction: Apply model to newly designed analogs for activity prioritization.
- Synthetic Planning: Select top candidates for synthesis based on predicted potency and synthetic accessibility.
Table 3: Performance Comparison of GEP vs. Linear QSAR Models
| Model Type | Training R² | Training Q² | Test R² | Test RMSE |
|---|---|---|---|---|
| Linear QSAR | 0.603 | 0.482 | 0.554 | 0.307 |
| GEP Model | 0.839 | 0.760 | 0.801 | 0.157 |
Table 4: Key Descriptors in GEP Osteosarcoma Model
| Descriptor | Relative Importance | Role in Bioactivity |
|---|---|---|
| HOMO-LUMO Gap | 0.381 | Electronic properties influencing target interaction |
| Molecular Polarizability | 0.295 | Membrane permeability and binding affinity |
| Topological Complexity | 0.227 | Molecular shape complementarity with target |
| Hydrophobic Surface Area | 0.197 | Solubility and cellular uptake characteristics |
Results and Implementation Workflow
The GEP approach significantly outperformed traditional linear QSAR, achieving R² values of 0.839 and 0.760 for training and test sets respectively, compared to 0.603 and 0.554 for the linear model [41]. The evolved mathematical expression provided interpretable insights into the nonlinear relationships between molecular descriptors and antiproliferative activity, enabling rational design of novel analogs with predicted enhanced potency. This methodology demonstrates particular value for optimizing lead series in glioblastoma drug discovery where complex structure-activity relationships often challenge traditional QSAR approaches.
Table 5: Key Research Reagent Solutions for ML-QSAR Implementation
| Resource Category | Specific Tools/Software | Application Function | Access Information |
|---|---|---|---|
| Chemical Databases | ChEMBL, PubChem | Source of bioactive compounds and experimental IC50 values | Publicly available |
| Descriptor Calculation | RDKit, PaDEL, DRAGON | Generation of molecular descriptors from compound structures | Open-source and commercial |
| Machine Learning Libraries | scikit-learn, XGBoost | Implementation of ETR, GEP, and other ML algorithms | Open-source |
| Model Interpretation | SHAP, LIME | Explainable AI for feature importance analysis | Open-source |
| Molecular Modeling | GROMACS, AMBER | Molecular dynamics simulations and binding free energy calculations | Academic licensing available |
| ADMET Prediction | SwissADME, pkCSM | Prediction of absorption, distribution, metabolism, excretion, and toxicity | Web-based and open-source |
| Cloud Platforms | Google Colab, AWS | Computational resources for intensive ML-QSAR calculations | Commercial with free tiers |
Concluding Remarks and Future Perspectives
The integration of machine learning algorithms like Extra Trees Regressor and Gene Expression Programming with QSAR modeling represents a transformative advancement in virtual screening for glioblastoma therapeutics. The case studies presented demonstrate that these methods significantly enhance predictive accuracy and provide interpretable insights that guide rational drug design. ETR excels in handling high-dimensional descriptor spaces and identifying complex feature interactions, while GEP automatically discovers nonlinear structure-activity relationships through evolutionary computation.
Future developments in ML-QSAR will likely focus on semi-supervised approaches that leverage both labeled and unlabeled data [38], multi-task learning for polypharmacology prediction, and integration with deep learning architectures for enhanced feature representation. As these methodologies continue to evolve, they will play an increasingly vital role in accelerating the discovery of effective glioblastoma therapies, ultimately contributing to improved outcomes for this devastating disease.
Leveraging Contour Maps and Key Descriptors for Rational Compound Design and Scaffold Hopping
Glioblastoma (GBM) remains one of the most aggressive primary brain malignancies with a dismal prognosis, necessitating the discovery of novel therapeutic agents [26] [42]. In this context, virtual screening using three-dimensional quantitative structure-activity relationship (3D-QSAR) models has emerged as a powerful strategy for accelerating drug discovery. These computational approaches are particularly valuable for designing blood-brain barrier (BBB)-permeant compounds and overcoming treatment resistance through multi-targeting strategies [42]. The integration of contour map analysis with key molecular descriptors provides a rational framework for compound optimization and scaffold hopping—the strategic replacement of core molecular structures while preserving biological activity [9] [43]. This application note details protocols for leveraging these computational techniques specifically for glioblastoma therapeutic research, enabling researchers to efficiently identify and optimize novel drug candidates with improved efficacy and pharmacokinetic properties.
Computational Methodologies and Key Descriptors
3D-QSAR Model Development
The foundation of rational compound design lies in robust 3D-QSAR models, particularly Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA). These methods establish correlations between molecular fields and biological activity through the following process:
Molecular Alignment and Field Calculation: Proper alignment of training set molecules is critical. In a recent study on isocitrate dehydrogenase 1 (IDH1) inhibitors, 47 compounds with pyridin-2-one backbones were aligned to establish a common orientation for comparative analysis [9]. The CoMFA model demonstrated excellent statistical validity (R² = 0.980, Q² = 0.765), while the CoMSIA model showed even higher predictive capability (R² = 0.997, Q² = 0.770) [9].
Contour Map Interpretation: CoMFA steric and electrostatic field maps provide visual guidance for molecular optimization. Green contours indicate regions where bulky substituents enhance activity, while yellow contours signify areas where steric bulk decreases activity. Similarly, blue contours represent regions where positive charge improves activity, and red contours indicate areas where negative charge is favorable [9].
Model Validation: Rigorous validation using test sets and applicability domain assessment ensures model reliability for virtual screening applications [42].
Molecular Descriptors for Virtual Screening
Beyond 3D fields, key molecular descriptors enable high-throughput screening of chemical databases:
Shape-Based Descriptors: The Volumetric Aligned Molecular Shapes (VAMS) approach encodes molecular shapes as voxelized volumes aligned to a canonical coordinate system, allowing rapid shape similarity comparisons using the Shape Tanimoto metric [44]. This method can screen millions of compounds in fractions of seconds while maintaining competitive enrichment performance compared to alignment-based methods like ROCS [44].
Orbital Energy Descriptors: For specific target classes, specialized descriptors significantly enhance screening efficiency. In discovering fluorescence materials with inverted singlet-triplet gaps, researchers developed two key descriptors (K~S~ and O~D~) based on exchange integral and molecular orbital energy, achieving a 90% screening success rate while reducing computational costs by 13-fold compared to post-Hartree-Fock calculations [45].
AI-Driven Representations: Modern approaches utilize graph neural networks and language models to learn continuous molecular embeddings that capture complex structure-activity relationships beyond traditional descriptors [43].
Table 1: Key Molecular Descriptors for Virtual Screening in Glioblastoma Research
| Descriptor Category | Specific Descriptors | Application in Glioblastoma Research | Performance Metrics |
|---|---|---|---|
| 3D Field-Based | CoMFA steric/electrostatic fields, CoMSIA similarity indices | IDH1 mutant inhibitor optimization [9] | Q² = 0.765-0.770, R² = 0.980-0.997 [9] |
| Shape-Based | Shape Tanimoto, VAMS voxel representations | Scaffold hopping for CDK6 inhibitors [46] | Millions of shapes screened in <1 second [44] |
| Orbital-Based | K~S~ (exchange integral), O~D~ (orbital energy difference) | Discovery of materials with inverted singlet-triplet gaps [45] | 90% success rate, 13x faster computation [45] |
| AI-Derived | Graph embeddings, transformer-based features | Multi-targeting approach for EGFR/PI3Kp110β inhibition [42] | Identification of 27 hit molecules from large libraries [42] |
Experimental Protocols
Comprehensive Virtual Screening Workflow
Protocol 1: 3D-QSAR Model Development with Contour Map Analysis
Purpose: To develop predictive 3D-QSAR models for glioblastoma-relevant targets and interpret contour maps for rational compound design.
Materials:
- Software: SYBYL, Open3DALIGN, KNIME with RDKit nodes [9] [42]
- Training Set: 30-50 compounds with known biological activity against target (e.g., IDH1 mutants, EGFR, PI3Kp110β) [9]
- Hardware: Workstation with sufficient memory for molecular field calculations
Procedure:
- Data Curation and Preparation
Molecular Alignment
- Identify and extract the common molecular framework
- Align all molecules using atom-based or field-based methods
- Verify alignment quality through visual inspection and RMSD values
Field Calculation and Model Generation
- Calculate steric and electrostatic fields using CoMFA protocol
- Generate similarity indices fields using CoMSIA with standard probes
- Perform Partial Least Squares (PLS) regression analysis
- Validate model using leave-one-out cross-validation and test set prediction
Contour Map Analysis
- Generate steric and electrostatic contour maps at default contribution levels
- Interpret green (favorable steric bulk) and yellow (unfavorable steric) regions
- Analyze blue (positive charge favorable) and red (negative charge favorable) regions
- Use maps to guide structural modifications for improved potency
Troubleshooting Tip: Poor model statistics (Q² < 0.5) often indicate inadequate molecular alignment or insufficient structural diversity in the training set. Revisit alignment strategy or expand training set diversity.
Protocol 2: Scaffold Hopping Using Shape-Based Descriptors
Purpose: To identify novel molecular scaffolds with similar shape and pharmacophore features to known active compounds but improved properties.
Materials:
- Software: OpenEye ROCS, VAMS implementation, Schrödinger Suite [44] [46]
- Query Compound: Known active compound with confirmed binding mode
- Screening Database: e.Molecules, ZINC, or in-house corporate library [46]
Procedure:
- Query Generation
- Extract co-crystallized ligand from protein structure or use known active compound
- Generate low-energy conformation(s) for shape reference
- Define pharmacophore features if using colored shape screening
Shape-Based Screening
- Implement VAMS screening using voxelized molecular shapes aligned to inertial moments [44]
- Set Shape Tanimoto threshold (typically >0.7) for hit identification
- Alternatively, use ROCS with ComboTanimoto scoring (Shape + Color) [46]
- Screen database of millions of compounds using efficient data structures
Hit Analysis and Selection
- Analyze top-ranking compounds for structural diversity
- Apply ADMET filters, particularly BBB penetration for glioblastoma applications [42]
- Verify synthetic accessibility and chemical stability
- Select 20-50 diverse candidates for further evaluation
Experimental Validation
Troubleshooting Tip: If shape-based screening yields too few hits, increase the shape similarity threshold or incorporate partial shape matching. For glioblastoma targets, prioritize compounds with predicted BBB penetration early in the screening cascade.
Applications in Glioblastoma Therapeutics
Case Studies and Research Applications
Table 2: Successful Applications of Virtual Screening in Glioblastoma Drug Discovery
| Target | Screening Approach | Key Descriptors/Features | Outcome | Reference |
|---|---|---|---|---|
| CHI3L1 | Pharmacophore-based virtual screening | 3D pharmacophore model, K~d~ prediction | Identification of compound G28 with validated activity in GBM spheroids [26] | [13] [26] |
| IDH1 mutant | 3D-QSAR with scaffold hopping | CoMFA/CoMSIA fields, molecular alignment | Novel inhibitors with pIC~50~ values up to 7.46 [9] | [9] |
| CDK6 | Shape-based virtual screening (ROCS) | ShapeTanimoto, ColorTanimoto, TanimotoCombo | Identification of Mol_370 with stable binding in MD simulations [46] | [46] |
| EGFR/PI3Kp110β | Multi-target QSAR models | Atom Pair Fingerprints, BBB permeation prediction | 27 hit molecules with dual inhibition and BBB penetration [42] | [42] |
Multi-Targeting Strategies for Overcoming Resistance
Glioblastoma treatment resistance often emerges through compensatory pathway activation. Integrated virtual screening approaches addressing multiple targets simultaneously show promise:
Dual EGFR/PI3Kp110β Inhibition: Using automated QSAR models and structure-based screening, researchers identified compounds with dual inhibitory activity, potentially overcoming compensatory signaling in glioblastoma [42].
Blood-Brain Barrier Penetration Prediction: Integration of BBB permeation models (logBB prediction) with activity models ensures identified hits can reach their CNS targets [42].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Virtual Screening in Glioblastoma Research
| Tool/Category | Specific Software/Resource | Function | Application Example |
|---|---|---|---|
| Molecular Modeling | SYBYL, Schrödinger Maestro | 3D-QSAR model development, molecular docking | CoMFA/CoMSIA model building for IDH1 inhibitors [9] |
| Shape Screening | OpenEye ROCS, VAMS | Shape-based virtual screening | Identification of CDK6 inhibitors using ROCS [46] |
| Cheminformatics | KNIME with RDKit, Open3DALIGN | Molecular descriptor calculation, data preprocessing | Automated QSAR model building for EGFR/PI3Kp110β inhibitors [42] |
| Compound Libraries | e.Molecules, ZINC, ChEMBL | Sources of screening compounds | Ligand-based virtual screening of e.Molecules database [46] |
| ADMET Prediction | QikProp, admetSAR, FP-ADMET | Prediction of BBB penetration, toxicity, pharmacokinetics | BBB permeation prediction for glioblastoma drug candidates [42] |
| Validation Software | GROMACS, AMBER | Molecular dynamics simulations | Validation of CDK6 inhibitor binding stability [46] |
Virtual screening (VS) has become a cornerstone of modern drug discovery, enabling the rapid and cost-effective identification of hit candidates from immense chemical libraries. Within oncology, this approach is particularly valuable for addressing aggressive cancers with high unmet medical need, such as glioblastoma multiforme (GBM). GBM presents unique therapeutic challenges, including tumour heterogeneity, rapid progression, and the protective obstacle of the blood-brain barrier (BBB) [47]. This Application Note details a structured VS protocol, framed within a broader thesis on utilizing 3D-QSAR models for GBM therapeutics, that successfully identified small-molecule inhibitors of Chitinase-3-like protein 1 (CHI3L1), a glycoprotein implicated in GBM progression and immune evasion [48]. We provide a detailed account of the workflow, from library preparation to experimental validation, including all critical quantitative data and reusable methodologies.
Virtual Screening Workflow & Quantitative Outcomes
The successful identification of CHI3L1 inhibitors was achieved through a structured, multi-stage virtual screening protocol applied to a library of over 4.4 million compounds [48]. The process leveraged a structure-based 3D pharmacophore model to efficiently prioritize candidates for experimental testing. The table below summarizes the key quantitative outcomes from each stage of this process.
Table 1: Summary of the Virtual Screening Workflow and Results
| Screening Stage | Description | Input Library Size | Output Candidates | Key Criteria / Results |
|---|---|---|---|---|
| 1. Library Preparation | Curating and preparing a diverse small-molecule library | ~4.4 million compounds | N/A | Compound libraries from public/commercial sources [48] |
| 2. Structure-Based 3D Pharmacophore Screening | Applying a 3D pharmacophore model based on the target protein structure | ~4.4 million compounds | 35 candidates | Model targeting the CHI3L1 binding site [48] |
| 3. Experimental Binding Validation | Validating binding affinity via Microscale Thermophoresis (MST) | 35 candidates | 2 confirmed hits | Dose-dependent CHI3L1 interaction; Kd of 6.8 µM (Compound 8) and 22 µM (Compound 39) [48] |
| 4. Functional Validation in GBM Spheroids | Assessing efficacy in a 3D disease model | 2 hits (Compound 8) | 1 lead compound | Reduced spheroid viability; attenuated phospho-STAT3 levels [48] |
This workflow demonstrates the powerful funneling capacity of VS, distilling millions of possibilities into a manageable number of high-quality leads for resource-intensive experimental work.
Detailed Experimental Protocols
Protocol A: Structure-Based 3D Pharmacophore Screening
This protocol outlines the steps for creating and applying a 3D pharmacophore model to screen a large compound library.
1. Target Selection and Preparation:
- Obtain the 3D crystallographic structure of the target protein (e.g., CHI3L1) from a protein data bank.
- Using molecular visualization software (e.g., UCSF Chimera), prepare the protein structure by adding hydrogen atoms, assigning correct protonation states to residues, and removing crystallographic water molecules, unless structurally relevant.
2. Pharmacophore Model Generation:
- Analyze the binding site to identify critical features that facilitate ligand binding, such as hydrogen bond donors/acceptors, hydrophobic regions, and aromatic rings.
- Using drug discovery software (e.g., MOE, Schrödinger), generate a 3D pharmacophore model that spatially defines these essential features based on the native ligand or the binding site geometry itself [48].
3. Compound Library Preparation:
- Convert the library of compounds from 2D structural representations (e.g., SDF files) into 3D conformers.
- Perform energy minimization on each conformer to ensure geometrical stability.
4. Virtual Screening Execution:
- Screen the entire prepared compound library against the generated pharmacophore model.
- The software will score and rank compounds based on their fit to the pharmacophore features. Select the top-ranked compounds (e.g., 35 in the cited study) for further evaluation [48].
Protocol B: Experimental Binding Validation via Microscale Thermophoresis (MST)
This protocol describes the use of MST to confirm and quantify the binding interaction between the hit compounds and the target protein.
1. Protein and Compound Labeling:
- Purify the target protein.
- Fluorescently label the protein using a commercially available dye kit according to the manufacturer's instructions. Alternatively, compounds can be labeled if protein labeling is not feasible.
2. Sample Preparation:
- Prepare a constant, low concentration of the labeled protein.
- Serially dilute the unlabeled test compound to create a range of concentrations (typically from nanomolar to high micromolar).
- Mix a constant volume of the labeled protein with each compound dilution. Include a control with protein and no compound.
3. MST Measurement:
- Load the samples into premium coated capillaries.
- Place the capillaries into the MST instrument.
- The instrument uses an infrared laser to create a microscopic temperature gradient, and the movement of molecules (thermophoresis) in this gradient is monitored via fluorescence. Binding events alter this movement.
4. Data Analysis:
- The instrument's software calculates the normalized fluorescence (Fnorm) for each compound concentration.
- Plot Fnorm against the compound concentration and fit the data to a binding model to determine the dissociation constant (Kd), as was done to determine the Kd of 6.8 µM for Compound 8 [48].
Visualizing the Workflow and Biological Pathway
The following diagrams, generated with Graphviz and adhering to the specified color and contrast guidelines, illustrate the logical flow of the virtual screening protocol and the biological pathway targeted by the identified hits.
Virtual Screening Funnel
Targeted CHI3L1 Signaling in GBM
This diagram outlines the key pathological role of CHI3L1 in Glioblastoma, which was targeted in the virtual screening study [48].
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key reagents, software, and instrumentation required to execute the virtual screening and validation protocols described in this note.
Table 2: Essential Research Reagents and Solutions for Virtual Screening and Validation
| Category / Item | Specific Examples / Specifications | Function in the Workflow |
|---|---|---|
| Compound Libraries | NCI Diversity Set, ZINC database, In-house curated libraries | Source of small molecules for screening; provides chemical diversity [49]. |
| Structural Data | Protein Data Bank (PDB) ID for target protein (e.g., CHI3L1) | Provides the 3D atomic coordinates necessary for structure-based pharmacophore modeling [48]. |
| Molecular Modeling Software | MOE (Molecular Operating Environment), Schrödinger Suite, OpenEye Toolkits | Used for protein preparation, pharmacophore model generation, compound library preparation, and virtual screening execution [48]. |
| Target Protein | Recombinant Human CHI3L1 protein, >95% purity | Required for experimental validation of binding affinity using biophysical techniques like MST [48]. |
| Validation Instrumentation | Monolith X Series (MST), Biacore Series (SPR) | Instruments used to quantitatively measure the binding affinity (Kd) between the hit compound and the target protein [48]. |
| Cell-Based Assay Systems | 3D GBM Spheroid Models (e.g., U87, U251 cells) | Physiologically relevant in vitro models for functional validation of hit compounds, assessing viability and pathway modulation (e.g., p-STAT3 levels) [48]. |
Overcoming Computational Hurdles: Model Robustness, Overfitting, and BBB Penetration
In the pursuit of novel glioblastoma (GBM) therapeutics, 3D-QSAR modeling serves as a cornerstone of virtual screening campaigns, enabling the prediction of compound activity based on structural and physicochemical properties. The high complexity and aggressive nature of GBM, coupled with the protective obstacle of the blood-brain barrier (BBB), make efficient computational screening particularly critical [47]. However, the predictive utility of any QSAR model is entirely contingent upon its robustness and generalizability. Overfitting occurs when a model learns not only the underlying relationship in the training data but also its noise and random fluctuations, leading to poor performance on new, unseen data. This application note outlines definitive, actionable strategies to mitigate overfitting and rigorously validate the predictive power of 3D-QSAR models within the context of GBM drug discovery.
Data Preparation and Curation
The foundation of a reliable QSAR model is a high-quality, well-curated dataset. Inadequate data preparation is a primary source of error and a key contributor to models that fail to generalize.
Protocol: Dataset Curation and Preprocessing
- Dataset Collection: Compile a dataset of chemical structures and their associated biological activities (e.g., IC₅₀, Ki) from reliable sources such as ChEMBL, BindingDB, or relevant scientific literature. For GBM, ensure activities are measured in relevant models (e.g., GBM cell lines, 3D spheroid models) [50] [51].
- Data Cleaning and Standardization:
- Remove duplicate, ambiguous, or erroneous entries.
- Standardize chemical structures using software like Standardizer or MolVS: remove salts, normalize tautomers, and handle stereochemistry consistently [51].
- Convert all biological activities to a common unit and scale (e.g., pIC₅₀ = -log₁₀(IC₅₀)).
- Chemical Space Analysis and Splitting: Partition the cleaned dataset into training, validation, and external test sets. Use structure-based methods like the Kennard-Stone algorithm to ensure each set is representative of the overall chemical space. The external test set must be reserved exclusively for final model assessment and must not be used in any model building or tuning steps [52].
Model Building and Overfitting Mitigation
During the model building phase, the choice of algorithm and feature selection are critical levers for controlling model complexity.
Protocol: Feature Selection and Model Training
- Descriptor Calculation and Pre-filtering: Calculate a comprehensive set of 3D molecular descriptors using software such as RDKit, Dragon, or PaDEL-Descriptor. Pre-filter descriptors to remove those with low variance or high pairwise correlation (e.g., |r| > 0.95) [52].
- Robust Feature Selection: Apply feature selection methods to identify the most relevant descriptors.
- Embedded Methods: Utilize algorithms like LASSO regression or Random Forests, which perform feature selection as part of the model training process. These are often preferred for their efficiency and stability [52].
- Wrapper Methods: Use genetic algorithms or sequential feature selection to evaluate different descriptor subsets based on model performance, though these are computationally intensive.
- Algorithm Selection with Cross-Validation: Choose modeling algorithms appropriate for your data size and complexity. Internal cross-validation on the training set is non-negotiable for tuning hyperparameters and preventing overfitting.
- Linear Models: Multiple Linear Regression (MLR), Partial Least Squares (PLS). PLS is particularly useful for handling descriptor multicollinearity [52].
- Non-Linear Models: Support Vector Machines (SVM) or Random Forests. While powerful, they require more data and careful validation to ensure they are learning the signal and not the noise [52]. Train the model using the selected features and optimized hyperparameters on the entire training set.
Table 1: Common QSAR Algorithms and Their Characteristics
| Algorithm | Type | Advantages | Overfitting Risk & Mitigation |
|---|---|---|---|
| Multiple Linear Regression (MLR) | Linear | Highly interpretable, simple | High risk with many descriptors; use strong feature selection. |
| Partial Least Squares (PLS) | Linear | Handles multicollinearity well | Lower risk; complexity controlled by the number of components. |
| Random Forest (RF) | Non-linear | Captures complex relationships, robust to noise | Moderate risk; controlled by tree depth and number of trees. |
| Support Vector Machine (SVM) | Non-linear | Effective in high-dimensional spaces | High risk; mitigated via cross-validation of regularization parameter. |
Comprehensive Model Validation
Relying on a single metric, particularly from the training data, is a common pitfall. A multi-faceted validation strategy is required to confidently assess predictive power [53].
Protocol: A Tiered Validation Strategy
- Internal Validation: Perform k-fold cross-validation (e.g., 5-fold or 10-fold) on the training set. Leave-One-Out (LOO) CV can be used for very small datasets. This provides an initial estimate of model robustness [52].
- External Validation: This is the most critical step for evaluating predictive power. Apply the final model, built exclusively on the training set, to the completely held-out external test set [53] [52].
- Statistical Analysis of External Validation: Calculate the following metrics for the external test set predictions [53]:
- Coefficient of Determination (r²): Measures the proportion of variance explained. An r² > 0.6 is often considered a threshold, but it is not sufficient alone [53].
- Root Mean Square Error (RMSE): Quantifies the average prediction error.
- Metrics for Regression Through Origin: Calculate r₀² and r'₀². The condition that r₀² ≈ r'₀² ≈ r² indicates a model without systematic bias [53].
Table 2: Key Statistical Parameters for External Validation of QSAR Models
| Parameter | Formula/Description | Interpretation and Acceptance Threshold |
|---|---|---|
| Coefficient of Determination (r²) | ( r^2 = 1 - \frac{\sum (y{obs} - y{pred})^2}{\sum (y{obs} - \bar{y}{obs})^2} ) | > 0.6 is a common threshold, but not sufficient alone [53]. |
| Root Mean Square Error (RMSE) | ( RMSE = \sqrt{\frac{\sum (y{obs} - y{pred})^2}{n}} ) | Lower values indicate better predictive accuracy. No universal threshold; should be considered in the context of the activity range. |
| r₀² (w/o intercept) | ( r0^2 = 1 - \frac{\sum (y{obs} - k \cdot y{pred})^2}{\sum (y{obs} - \bar{y}_{obs})^2} ) | Should be close to r². A significant difference suggests bias. |
| r'₀² (w/o intercept) | ( r0'^2 = 1 - \frac{\sum (y{pred} - k' \cdot y{obs})^2}{\sum (y{pred} - \bar{y}_{pred})^2} ) | Should be close to r² and r₀². The condition ( r0^2 \approx r0'^2 ) is critical [53]. |
Implementation Workflow for a GBM Case Study
The following workflow integrates the protocols above into a coherent strategy for a GBM-focused virtual screening project, such as discovering CHI3L1 inhibitors [50].
Validating a 3D-QSAR Model for GBM
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Software and Tools for Robust QSAR Modeling
| Category | Tool/Software | Specific Function in QSAR |
|---|---|---|
| Cheminformatics & Descriptor Calculation | RDKit, Dragon, PaDEL-Descriptor | Calculates molecular descriptors from 2D/3D structures for model development [52] [51]. |
| Conformer Generation | OMEGA, ConfGen, RDKit (ETKDG) | Generates representative 3D conformations essential for 3D-QSAR and pharmacophore modeling [51]. |
| Data Standardization | Standardizer, MolVS | Standardizes molecular structures (e.g., removes salts, normalizes tautomers) to ensure data consistency [51]. |
| Modeling & Validation | Scikit-learn, Orange, WEKA | Provides algorithms for machine learning, feature selection, and cross-validation. |
| Structure-Based Design | Flare, Maestro | Visualizes and analyzes protein-ligand interactions; aids in rationalizing QSAR results and structure-based filtering [51]. |
The strategies outlined herein provide a rigorous framework for developing reliable 3D-QSAR models. In the high-stakes field of glioblastoma therapeutic research, where computational models guide experimental efforts, adhering to these protocols of data curation, model validation, and practical application is paramount for translating virtual hits into tangible therapeutic leads.
Optimizing Molecular Alignment and Conformer Selection for Meaningful 3D-QSAR Results
Within the critical field of glioblastoma (GBM) therapeutics research, virtual screening strategies employing three-dimensional quantitative structure-activity relationship (3D-QSAR) models have emerged as powerful tools for identifying and optimizing novel chemotherapeutic agents [10] [47]. The aggressive nature of GBM and the protective obstacle of the blood-brain barrier (BBB) necessitate the discovery of highly effective and targeted drugs [47]. 3D-QSAR accelerates this process by predicting binding affinity based on the three-dimensional descriptors of aligned ligand molecules [54]. The predictive power and reliability of these models are profoundly dependent on two foundational pre-processing steps: molecular alignment and conformer selection [55]. Incorrect alignment or inappropriate conformer choice introduces noise that obscures the true structure-activity relationship, leading to models with poor predictive capability and unreliable guidance for drug design [56]. This Application Note provides detailed, actionable protocols for optimizing these crucial steps, framed within the context of a broader thesis on virtual screening for glioblastoma therapeutics.
Experimental Protocols for Robust 3D-QSAR
Molecular Alignment Strategies
Molecular alignment establishes a common reference frame for comparing the 3D structural fields of different molecules. The following protocols detail two common and effective alignment methods.
Distill Alignment Technique
This method is suitable for datasets with a common, rigid scaffold and is implemented in software suites like SYBYL [57].
- Template Selection: Identify and select the most active compound in your dataset as the template for alignment. For instance, in a study on phenylindole derivatives, compound 5n was used as the template due to its superior activity [57].
- Structure Sketching and Optimization:
- Sketch the 2D structure of all compounds using a module like the Sketch module in SYBYL [57].
- Optimize the 3D geometry of each molecule. Use a standard force field (e.g., Tripos molecular mechanics force field) and assign atomic charges (e.g., Gasteiger-Hückel charges) [57].
- Employ a conjugate gradient algorithm for energy minimization until a convergence criterion is reached (e.g., a gradient of 0.01 kcal/mol [57]).
- Alignment Execution: Use the distill alignment command, specifying the pre-optimized most active compound as the template. The software will automatically superimpose the remaining dataset molecules onto this template [57].
Flexible Ligand Alignment
This method is advantageous for datasets with significant structural diversity, as it accounts for conformational flexibility during the alignment process [55].
- Ligand Preparation: Generate accurate 3D structures for all ligands using a tool like the LigPrep module in the Maestro suite. This step includes energy minimization and the generation of possible states at a defined pH (e.g., 7.0 ± 2.0) [58] [55].
- Alignment Setup: Within the molecular alignment tool of your software (e.g., Maestro's "flexible ligand alignment" option), input the prepared 3D structures [55].
- Parameter Execution: Run the alignment procedure. The software will explore conformational space and align molecules based on shared pharmacophoric features or molecular similarity, without relying on a single rigid scaffold.
Conformer Generation and Selection
The goal of conformer selection is to identify the bioactive conformation—the 3D shape a molecule adopts when bound to its target.
- Conformer Generation:
- On-the-fly Generation: During pharmacophore modeling or alignment, software can generate conformers dynamically. Use the "best conformer generation" option, typically with a default maximum of 255 conformers per molecule and an energy threshold of 10 kcal/mol above the global minimum [59]. This ensures a diverse yet energetically reasonable set of conformations.
- Pre-computed Generation: For more control, generate a conformational ensemble for each molecule beforehand using a dedicated protocol (e.g., the "conformation protocol" in Discovery Studio). This ensemble is stored in a database for subsequent alignment and model building [59].
- Selection of the Bioactive Conformer:
- The most reliable approach is to use a co-crystallized ligand structure from a protein-ligand complex (e.g., from the Protein Data Bank) as a template for alignment and conformer selection [58]. For example, the ligand HOU from PDB ID 7DY7 has been used as a reference for aligning potential PD-L1 inhibitors [58].
- In the absence of experimental data, the conformer of the most active compound in the series, often derived from molecular docking studies, is used as the template for the rest of the dataset [60] [57].
Workflow Visualization
The following diagram illustrates the integrated workflow for molecular alignment and conformer selection, highlighting the critical decision points described in the protocols.
Diagram 1: Integrated workflow for molecular alignment and conformer selection prior to 3D-QSAR model building. Critical decision points and standard parameters are highlighted.
Quantitative Parameters and Model Validation
Successful application of the above protocols is gauged by the statistical quality of the resulting 3D-QSAR model. The table below summarizes key validation parameters from recent studies that employed rigorous alignment and conformer selection.
Table 1: Statistical Parameters from Validated 3D-QSAR Models
| Study Focus | Model Type | R² (Fit) | Q² (LOO CV) | R²Pred (Test Set) | Alignment Method / Template |
|---|---|---|---|---|---|
| Phenylindole Derivatives (Anti-cancer) [57] | CoMSIA/SEHDA | 0.967 | 0.814 | 0.722 | Distill / Most active compound (5n) |
| mIDH1 Inhibitors [9] | CoMFA | 0.980 | 0.765 | - | Common scaffold alignment |
| mIDH1 Inhibitors [9] | CoMSIA | 0.997 | 0.770 | - | Common scaffold alignment |
| 6-Hydroxybenzothiazole-2-carboxamides (MAO-B Inhibitors) [56] | COMSIA | 0.915 | 0.569 | - | Not Specified |
| Dihydropteridone Derivatives (Anti-glioma) [10] | CoMSIA | 0.928 | 0.628 | - | Not Specified |
Abbreviations: R²: Coefficient of determination; Q²: Leave-One-Out cross-validated correlation coefficient; R²Pred: Predictive R² for an external test set; LOO CV: Leave-One-Out Cross-Validation.
A high R² value indicates a good fit to the training set data, while a high Q² value (typically >0.5) is a primary indicator of the model's internal predictive ability [9] [57]. The external predictive power, represented by R²Pred, is the ultimate test of a model's utility in virtual screening [57]. The excellent statistical values reported in studies that used careful alignment protocols underscore the importance of these initial steps [9] [57].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Software and Tools for Molecular Alignment and 3D-QSAR
| Tool / Reagent | Function | Application Note |
|---|---|---|
| SYByl-X | Comprehensive molecular modeling suite. | Used for sketching structures, molecular optimization with the Tripos force field, and performing Distill alignment [56] [57]. |
| Schrödinger Suite (Maestro) | Integrated platform for drug discovery. | Used for LigPrep for 3D structure preparation and energy minimization, and for flexible ligand alignment [58] [55]. |
| Discovery Studio | Environment for biomolecular modeling. | Used for pharmacophore modeling, conformer generation protocols, and visualization of docking results [59] [57]. |
| ChemDraw/ChemBioDraw | Chemical structure drawing. | Used for the initial 2D sketching of molecular structures prior to 3D optimization [10] [59]. |
| OpenEye's 3D-QSAR | Specialized tool for building predictive 3D-QSAR models. | Uses descriptors based on 3D shape and electrostatics (ROCS, EON) to create a consensus model for binding affinity prediction [54]. |
| GROMACS | Package for molecular dynamics simulations. | Used to validate the stability of the binding pose of a designed compound through 100 ns simulations, providing final confirmation of the model's utility [55]. |
The path to a predictive and scientifically meaningful 3D-QSAR model in glioblastoma research is paved during the initial stages of molecular preparation. As demonstrated, a deliberate choice between distill and flexible alignment strategies, coupled with a rigorous protocol for conformer generation and selection using energetically reasonable thresholds, is non-negotiable. The resulting high-quality models, characterized by strong Q² and R²Pred values, provide a reliable virtual screening tool. This enables the efficient identification of novel, potent, and selective therapeutic candidates, such as dihydropteridone and phenylindole derivatives, offering a promising strategy to address the critical unmet need in glioblastoma therapy [10] [57]. By adhering to these detailed application notes, researchers can robustly integrate 3D-QSAR into their drug discovery pipeline, accelerating the development of life-saving treatments.
The blood-brain barrier (BBB) presents a major obstacle in developing effective therapeutics for central nervous system (CNS) diseases, particularly glioblastoma (GBM). This highly selective barrier, composed of endothelial cells with tight junctions, restricts nearly 98% of small molecule drugs and almost all large-molecule drugs from entering the brain [61] [62]. For GBM, the most aggressive and lethal primary brain tumor, the BBB significantly contributes to treatment failure by preventing chemotherapeutic agents from reaching therapeutic concentrations at the tumor site [47]. The imperative to address this challenge early in the drug discovery pipeline has catalyzed the development of sophisticated computational prediction models that can rapidly and accurately assess a compound's potential to cross the BBB before committing to expensive and time-consuming experimental work.
Integrating BBB permeability predictions during the initial virtual screening phases represents a paradigm shift in neuro-therapeutic development. Traditional experimental methods for determining BBB permeability, such as in vivo rodent models (logBB measurements) and in vitro Transwell models, are time-consuming, expensive, and ethically challenging [63] [61]. Computational approaches, particularly Quantitative Structure-Activity Relationship (QSAR) models and machine learning (ML) algorithms, now offer viable alternatives that can process thousands of compounds rapidly, significantly accelerating the early stages of drug discovery while reducing reliance on animal testing [63] [64] [62]. When combined with 3D-QSAR models targeting specific GBM therapeutic targets, these tools create a powerful framework for identifying promising drug candidates with both potent anti-tumor activity and favorable brain penetration properties.
Current BBB Permeability Prediction Models
The landscape of BBB permeability prediction has evolved from simple rule-based systems to complex artificial intelligence (AI) and ML models that demonstrate remarkable predictive accuracy. Early models primarily relied on lipophilicity (logP) and molecular weight as key determinants of BBB penetration [62]. While these physicochemical properties remain important, modern models incorporate a much broader array of molecular descriptors and leverage increasingly sophisticated algorithms to capture the complex nonlinear relationships governing BBB permeation.
Table 1: Overview of Contemporary BBB Permeability Prediction Models
| Model Type | Key Features/Descriptors | Example Performance | Representative Tools/Datasets |
|---|---|---|---|
| Traditional ML | Pre-calculated 1D/2D descriptors (e.g., logP, MW, TPSA, structural fingerprints) [61] | Accuracy: 82-93% [62] | Random Forest, SVM, LightGBM [62] |
| Graph Neural Networks (GNNs) | Learns directly from molecular graph structure [61] | AUC: ~0.97 [62] | Molecular Net BBBP, TDC bbbp_martins [61] |
| 3D-QSAR Approaches | 3D molecular fields, steric/electrostatic properties [64] | R²: ~0.75 [64] | CORAL software [64] |
| Encoder-Based Models | Uses SMILES strings as input [61] | Underperforms vs. other methods [61] | BERT-based architectures [61] |
Modern ML models achieve impressive predictive performance, with some ensemble methods reaching up to 95% accuracy in classifying compounds as BBB permeable (BBB+) or impermeable (BBB-) [62]. The development of these models has been facilitated by the creation of large, curated datasets such as the MoleculeNet BBBP (2,052 compounds), TDC bbbp_martins (2,030 compounds), and B3DB (7,807 compounds) [61]. These resources provide standardized benchmarks for model training and validation, though they often exhibit a bias toward BBB-permeable compounds, which must be considered when interpreting model performance [61].
Integration with 3D-QSAR Virtual Screening for Glioblastoma
The integration of BBB permeability prediction with 3D-QSAR virtual screening creates a powerful multi-stage filtering system for identifying promising GBM therapeutic candidates. This approach simultaneously optimizes for target affinity and brain penetrability, two critical determinants of in vivo efficacy. In the context of GBM, 3D-QSAR models have been successfully developed for various molecular targets, including PLK1 inhibitors (dihydropteridone derivatives) and mutant isocitrate dehydrogenase 1 (mIDH1) inhibitors, demonstrating the utility of this approach for specific glioma targets [9] [10].
The workflow begins with building robust 3D-QSAR models using comparative molecular field analysis (CoMFA) and comparative molecular similarity index analysis (CoMSIA). These methods establish quantitative relationships between the three-dimensional molecular structures of known inhibitors and their biological activities against specific GBM targets. For instance, studies on mIDH1 inhibitors have yielded 3D-QSAR models with excellent statistical parameters (CoMFA: R² = 0.980, Q² = 0.765; CoMSIA: R² = 0.997, Q² = 0.770), indicating strong predictive capability for designing novel compounds with improved potency [9]. Similarly, 3D-QSAR models for dihydropteridone derivatives demonstrated exemplary fit with Q² = 0.628 and R² = 0.928 [10].
Once developed and validated, these 3D-QSAR models can screen virtual compound libraries to identify candidates with predicted high activity against the target. The top-ranking compounds then undergo BBB permeability assessment using dedicated prediction models. This sequential approach ensures that only compounds with both desirable pharmacological activity and brain penetration potential advance to experimental validation, optimizing resource allocation and increasing the likelihood of success in later development stages.
Diagram 1: Integrated virtual screening workflow combining 3D-QSAR for target activity and ML models for BBB permeability prediction.
Experimental Protocols and Methodologies
Protocol 1: Developing a 3D-QSAR Model for Target Activity Prediction
This protocol outlines the key steps for constructing a predictive 3D-QSAR model targeting glioblastoma-relevant proteins, adapted from recent studies on PLK1 and mIDH1 inhibitors [9] [10].
Step 1: Data Set Curation and Preparation
- Collect a series of compounds (typically 30-50) with known experimental activity (e.g., IC₅₀) against the target of interest.
- Divide compounds into training (≈70-80%) and test sets (≈20-30%) using rational selection to ensure structural and activity diversity.
- Sketch 2D molecular structures using ChemDraw and perform geometry optimization. Initial optimization uses molecular mechanics (MM+ force field) followed by semi-empirical methods (AM1 or PM3) until the root mean square gradient reaches 0.01 [10].
Step 2: Molecular Alignment and Conformer Generation
- Identify and extract the common molecular scaffold shared by all compounds.
- Align all molecules to this common scaffold using field-fit or atom-based alignment techniques to ensure meaningful comparison of molecular fields [9].
- Generate representative low-energy conformers for each compound.
Step 3: 3D-QSAR Model Construction and Validation
- Perform CoMFA and CoMSIA analyses using the aligned molecules.
- Calculate steric, electrostatic, hydrophobic, and hydrogen-bonding fields around the molecules.
- Use partial least squares (PLS) regression to build the QSAR model correlating molecular fields with biological activity.
- Validate model robustness using leave-one-out cross-validation (Q²) and external prediction on the test set (R²ₚᵣₑd) [9] [10].
Protocol 2: Implementing BBB Permeability Prediction in Screening Cascades
This protocol describes how to integrate BBB permeability predictions into a virtual screening workflow using available tools and datasets.
Step 1: Model Selection and Implementation
- Select appropriate BBB prediction models based on performance metrics and applicability domain.
- Prefer ensemble models that combine multiple algorithms (e.g., Random Forest, XGBoost, SVM) for improved accuracy [62].
- Implement models using available software or web servers (e.g., LightBBB, EnsembleBBB).
Step 2: Compound Preparation and Descriptor Calculation
- Prepare compounds by converting to standardized SMILES format.
- Calculate relevant molecular descriptors known to influence BBB permeability, including:
- Lipophilicity (logP): Critical for passive diffusion [63] [64].
- Molecular Weight (MW): Lower MW (<500 Da) generally favors permeability [61].
- Polar Surface Area (TPSA): Lower TPSA (<60-70 Ų) correlates with better BBB penetration [63] [61].
- Hydrogen Bond Donors/Acceptors: Fewer HBD (<5) and HBA (<10) improve permeability [61].
Step 3: Prediction and Interpretation
- Input prepared compounds and calculated descriptors into the selected BBB model.
- Classify compounds as BBB+ (permeable) or BBB- (impermeable) based on established thresholds.
- For regression models, use predicted logBB values (log[brain]/[blood]) > -1.0 as indicative of good brain penetration [64] [62].
- Apply results to prioritize compounds from 3D-QSAR screening for further analysis.
Table 2: Key Computational Tools and Resources for Integrated Screening
| Resource Category | Specific Tools/Databases | Primary Function | Access Information |
|---|---|---|---|
| BBB-Specific Datasets | MoleculeNet BBBP, TDC bbbp_martins, B3DB [61] | Model training and benchmarking | Publicly available |
| General Compound Databases | ZINC, ChEMBL, PubChem [61] | Source of virtual compounds for screening | Publicly available |
| Molecular Modeling Software | Schrodinger Maestro, CORAL, HyperChem [10] [64] [65] | Structure preparation, QSAR model building | Commercial/Academic licenses |
| Descriptor Calculation | CODESSA, RDKit, PaDEL-Descriptor [10] [61] | Computation of molecular descriptors | Open source and commercial |
| BBB Prediction Tools | LightBBB, EnsembleBBB [62] | specialized BBB permeability prediction | Publicly available/web servers |
Successful implementation of the integrated screening approach requires careful consideration of several technical aspects. Dataset quality and applicability domain are critical - models trained primarily on CNS-active compounds may not generalize well to diverse chemical libraries [61]. Model interpretability remains challenging for complex deep learning models like GNNs, though traditional QSAR and ML models often provide more transparent decision-making processes [61]. Additionally, researchers should consider multi-parameter optimization to balance BBB permeability with other drug-like properties, as excessive focus on a single parameter can compromise overall compound viability.
The integration of BBB permeability predictions with 3D-QSAR virtual screening represents a significant advancement in the rational design of glioblastoma therapeutics. This synergistic approach enables researchers to simultaneously optimize for target potency and brain penetrability from the earliest stages of drug discovery, potentially reducing late-stage attrition due to poor pharmacokinetic properties. The availability of robust computational models, large curated datasets, and user-friendly tools has made this integrated strategy increasingly accessible to research teams without extensive computational expertise.
Future directions in this field point toward even more sophisticated multi-scale modeling approaches. The integration of BBB-on-a-chip microphysiological systems with computational models promises to generate highly relevant training data that better captures the complexity of the human BBB [47]. Generative AI models are emerging as powerful tools for de novo design of brain-penetrant compounds with desired target activity, potentially discovering novel chemical space beyond existing compound libraries [61] [47]. Additionally, the development of models that can predict site-specific BBB permeability in GBM, accounting for regional disruption of the barrier, could further enhance the translational relevance of these computational approaches [47]. As these technologies mature, the vision of rapidly identifying effective, brain-penetrant GBM therapeutics through integrated computational screening moves closer to reality.
Analyzing SHAP and Ablation Studies to Identify Critical Molecular Descriptors for Optimization
In the pursuit of effective glioblastoma therapeutics, virtual screening using 3D-QSAR models has emerged as a pivotal strategy for efficiently identifying and optimizing lead compounds. The integration of advanced explainable artificial intelligence (XAI) techniques, particularly SHapley Additive exPlanations (SHAP), alongside rigorous ablation studies, provides a powerful framework for deconstructing model predictions and identifying the critical molecular descriptors that govern biological activity. This protocol details the application of these analytical methods within the context of 3D-QSAR-driven virtual screening, enabling researchers to prioritize molecular features for the optimization of anti-glioblastoma agents. By systematically identifying and validating these key descriptors, the drug development process can be significantly accelerated, leading to compounds with improved potency and selectivity.
Background and Principles
The Role of Molecular Descriptors in 3D-QSAR for Glioblastoma
Quantitative Structure-Activity Relationship (QSAR) models, particularly three-dimensional (3D-QSAR) approaches like Comparative Molecular Field Analysis (CoMSIA), correlate the spatial and electronic features of compounds with their biological activity against specific targets. In glioblastoma research, these models are crucial for understanding the structural determinants of anti-tumor efficacy. For instance, studies on dihydropteridone derivatives as PLK1 inhibitors have successfully utilized 3D-QSAR to validate anticancer activity, with models demonstrating excellent predictive power (exemplified by Q² = 0.628 and R² = 0.928) [10]. The minimal exchange energy for a C-N bond (MECN) was identified as a crucial 2D molecular descriptor in such models, which, when combined with 3D hydrophobic field information, guided the design of novel compounds with enhanced activity [10].
Explainable AI and Ablation Studies in Computational Drug Discovery
As machine learning (ML) models become more complex, interpreting their decision-making processes is essential for building trust and extracting scientifically meaningful insights. SHAP is a game theory-based approach that assigns each feature an importance value for a particular prediction, explaining the output of any ML model [66]. Ablation studies, conversely, systematically remove or alter components of a model (e.g., specific input features, architectural layers) to quantify their contribution to overall performance [67]. Together, they form a complementary toolkit for model interpretation: SHAP explains "why" a model made a certain prediction, while ablation studies prove "how much" a specific component matters.
Computational Protocols
Protocol 1: SHAP Analysis for Interpreting Virtual Screening Models
This protocol describes the application of SHAP to interpret machine learning models used in virtual screening, identifying the molecular descriptors that most significantly influence predictions of binding affinity or activity.
- Step 1: Model Training. Train a machine learning model for activity prediction. This can be a model predicting pIC₅₀ values or approximating molecular docking scores to accelerate screening [68] [67]. Utilize a diverse set of molecular descriptors and fingerprints as input features.
- Step 2: SHAP Value Calculation. For the trained model, compute SHAP values using a suitable method (e.g., TreeSHAP for tree-based models, KernelSHAP for model-agnostic applications). This quantifies the marginal contribution of each molecular descriptor to the prediction for every compound in the dataset.
- Step 3: Global Interpretation. Generate a global feature importance plot by taking the mean absolute SHAP value for each feature across the entire dataset. This ranks molecular descriptors by their overall impact on the model's output. As demonstrated in glioma research, SHAP filtering can then be applied to eliminate features with consistently low importance, retaining only the most predictive ones for the final model [66].
- Step 4: Local Interpretation. Analyze individual compound predictions using force plots or waterfall plots. This reveals how specific molecular descriptors (e.g., a particular hydrophobic field contour or electronic property) combine to yield a high or low predicted activity for a single molecule, providing concrete optimization guidance [66].
Protocol 2: Ablation Studies for Validating Model Components
This protocol outlines the design of ablation studies to empirically validate the importance of specific molecular descriptors or model architectural choices identified as critical through SHAP analysis.
- Step 1: Define the Baseline Model. Establish a high-performing baseline model, such as a hybrid neural network (e.g., 1D-CNN + LSTM + DNN) or a 3D-QSAR model, using the full set of features or the complete architecture [67].
- Step 2: Design Ablation Experiments. Systematically create simplified models by removing specific components. Key experiments include:
- Feature Ablation: Remove the top molecular descriptors identified by SHAP analysis from the input set.
- Descriptor Category Ablation: Remove entire categories of descriptors (e.g., all topological, all electrostatic) to assess their collective contribution.
- Architectural Ablation: Modify the model's architecture to test the necessity of specific components, such as using only a 1D-CNN without an LSTM module [67].
- Step 3: Evaluate and Compare Performance. Retrain and evaluate each ablated model on a held-out test set. Monitor key performance metrics such as validation loss, accuracy, R², Q², and mean squared error.
- Step 4: Quantify Component Criticality. The drop in performance between the baseline model and an ablated model quantifies the importance of the removed component. A significant performance decrease confirms the critical nature of the ablated features or architecture.
Table 1: Example Results from an Ablation Study on a Hybrid Neural Network for Drug Sensitivity Prediction [67]
| Model Architecture | Validation Loss | Validation Accuracy | Conclusion |
|---|---|---|---|
| 1D-CNN only | 0.088 | 0.792 | Baseline performance, lowest metrics |
| 1D-CNN + LSTM | 0.059 | 0.815 | LSTM module captures important sequential patterns |
| 1D-CNN + DNN | 0.048 | 0.942 | DNN significantly enhances feature learning |
| 1D-CNN + LSTM + DNN (Full) | 0.042 | 0.979 | Combined architecture is critical for optimal performance |
Integrated Workflow: From Virtual Screening to Lead Optimization
The following diagram illustrates the synergistic integration of 3D-QSAR, SHAP analysis, and ablation studies into a cohesive workflow for identifying and validating critical molecular descriptors.
Diagram 1: Integrated descriptor identification and validation workflow.
Research Reagent Solutions
The following table catalogues essential computational tools and data resources for implementing the described protocols.
Table 2: Key Research Reagent Solutions for SHAP and Ablation Analysis
| Category | Item / Software | Function / Description | Example Use Case |
|---|---|---|---|
| Explainable AI (XAI) | SHAP (SHapley Additive exPlanations) | Explains the output of any machine learning model by quantifying feature importance [66]. | Interpreting a random forest model predicting PLK1 inhibition. |
| Molecular Descriptors | CODESSA | Computes a comprehensive set of molecular descriptors (quantum chemical, topological, geometrical) [10]. | Generating input features for a 2D/3D-QSAR model of dihydropteridone derivatives. |
| 3D-QSAR Modeling | CoMSIA (Comparative Molecular Similarity Indices Analysis) | 3D-QSAR method that evaluates steric, electrostatic, hydrophobic, and hydrogen bond donor/acceptor fields [10]. | Mapping the hydrophobic field critical for glioblastoma cell line (U-87) activity [10] [69]. |
| Docking & Scoring | Smina | Molecular docking software used for virtual screening and generating docking scores for training ML models [68]. | Rapidly assessing binding affinity of designed compounds for CDK6, a glioblastoma target [46]. |
| Feature Selection | Metaheuristic Algorithms (HHO, mGTO, ZOA) | Optimization algorithms that select informative feature subsets from high-dimensional data [66]. | Pre-filtering radiomics and molecular descriptors before SHAP analysis in glioma studies. |
| Activity Data | ChEMBL Database | Public repository of bioactive molecules with drug-like properties and associated bioactivities [68]. | Sourcing IC₅₀ and Kᵢ data for monoamine oxidase inhibitors or other relevant targets. |
Case Study Analysis
Application in Dihydropteridone Derivative Optimization
A study on dihydropteridone-based PLK1 inhibitors for glioblastoma exemplifies the process. A 3D-QSAR-CoMSIA model was developed, revealing that hydrophobic interactions were a major determinant of anticancer activity. Concurrently, a 2D-QSAR analysis identified the "Min exchange energy for a C-N bond" (MECN) as a significant descriptor [10]. While not using SHAP explicitly, this identification of a key 2D descriptor is analogous to the output of a SHAP analysis. An ablation study could be designed by removing the MECN descriptor or the hydrophobic field information from the model and observing a significant drop in predictive power (e.g., R² and Q²), thereby validating their criticality. The integration of these insights led to the design of compound 21E.153, which exhibited outstanding predicted antitumor properties and docking capabilities [10].
Application in Deep Learning Model Development
The ResisenseNet model, developed for predicting drug sensitivity, provides a clear example of a comprehensive ablation study [67]. Researchers systematically tested different architectural components to quantify their contribution to model performance. As shown in Table 1, the sequential addition of LSTM and DNN modules to a 1D-CNN base progressively and significantly improved validation accuracy and reduced loss, proving that the hybrid architecture was essential for capturing the complex relationships between molecular descriptors, transcription factors, and drug sensitivity.
The integration of SHAP analysis and ablation studies provides a robust, evidence-based methodology for moving beyond "black box" predictions in virtual screening. By systematically identifying and validating the critical molecular descriptors that drive anticancer activity, as demonstrated in glioblastoma therapeutic research, computational chemists and drug developers can make informed decisions. This approach focuses optimization efforts on the most impactful structural features, thereby de-risking the drug discovery pipeline and accelerating the development of novel, effective therapeutics for challenging diseases like glioblastoma.
From In-Silico Hits to Validated Leads: Docking, ADMET, and Dynamics
Molecular docking has become an indispensable tool in modern computational drug discovery, serving as a powerful structure-based approach for predicting how a small molecule ligand interacts with a target protein at the atomic level [70]. This methodology allows researchers to characterize the behavior of small molecules in the binding site of target proteins and elucidate fundamental biochemical processes [70]. In the context of glioblastoma (GBM) therapeutics research—the most common and highly aggressive fast-growing brain tumor with a tragically short survival rate—molecular docking provides crucial insights for overcoming treatment challenges posed by the tumor's invasive nature, genetic heterogeneity, and the brain's unique protective barriers [71]. The docking process fundamentally involves two basic steps: prediction of the ligand conformation, position, and orientation within protein binding sites (referred to as pose generation), and assessment of the binding affinity through computational scoring [70]. These capabilities make docking particularly valuable for virtual screening workflows, where it helps prioritize promising candidates from large chemical libraries for further experimental validation.
Theoretical Framework of Molecular Docking
Fundamental Principles and Sampling Algorithms
The theoretical foundation of molecular docking originates from early ligand-receptor binding mechanisms, beginning with Fischer's lock-and-key theory, which proposed that ligands fit into receptors with rigid complementarity [70]. This was later refined by Koshland's induced-fit theory, which states that the active site of the protein continually reshapes through interactions with ligands, suggesting both ligands and receptors should be treated as flexible during docking simulations [70]. Various sampling algorithms have been developed to address the computational challenge of exploring the vast conformational space of ligand-receptor interactions:
- Matching algorithms utilize shape-based approaches to map ligands into protein active sites using pharmacophore features and distance matrices, offering high-speed screening suitable for virtual screening [70].
- Incremental construction methods divide ligands into fragments, dock an anchor fragment first, then rebuild the complete ligand incrementally, effectively handling ligand flexibility [70].
- Stochastic methods including Monte Carlo algorithms and Genetic Algorithms introduce random modifications to ligand conformations, employing energy-based selection criteria to evolve toward optimal binding poses [70].
Scoring Functions and Binding Affinity Prediction
Scoring functions represent the computational engine for evaluating and ranking ligand poses in molecular docking. These mathematical functions approximate the binding free energy of protein-ligand complexes by evaluating various interaction terms:
- Force field-based scoring calculates energy terms using molecular mechanics force fields, including van der Waals interactions, electrostatic contributions, and bond deformation penalties.
- Empirical scoring utilizes weighted energy terms derived from regression analysis of experimental binding data, often including hydrophobic contact surfaces, hydrogen bonding, and rotatable bond penalties.
- Knowledge-based scoring employs statistical potentials derived from structural databases of protein-ligand complexes, based on the frequency of atomic contact pairs observed in known structures.
Advanced approaches like negative image-based rescoring (R-NiB) have demonstrated improved docking performance by comparing the shape and electrostatic potential of docking poses to a negative image of the protein's binding cavity, effectively filtering active compounds from inactive decoys [72].
Molecular Docking Application in Glioblastoma Research
Targeting Glioblastoma Transmembrane Receptors and Extracellular Ligands
In glioblastoma research, molecular docking has proven invaluable for investigating interactions between GBM cell surface proteins and extracellular ligands within the tumor microenvironment. A 2025 study systematically screened ten transmembrane protein receptors and their extracellular ligands implicated in GBM cancer cell progression [71]. Computational analysis revealed that fibronectin (PDB ID: 3VI4) demonstrated strong interactions with the majority of GBM surface receptors, identifying it as a crucial node in the network of protein-protein interactions driving tumor development [71]. Molecular docking studies between FDA-approved GBM drugs and fibronectin demonstrated the strongest binding interaction with Irinotecan, followed by Etoposide and Vincristine, suggesting these compounds may effectively disrupt fibronectin-receptor interactions that promote GBM tumor progression [71].
Table 1: Molecular Docking Analysis of GBM-Approved Drugs with Fibronectin
| Drug Compound | Binding Interaction Strength | Therapeutic Implications |
|---|---|---|
| Irinotecan | Strongest interaction | Effectively disrupts fibronectin-receptor interactions |
| Etoposide | Strong interaction | Potential to inhibit GBM cell proliferation and invasion |
| Vincristine | Strong interaction | Promising for targeting fibronectin in GBM microenvironment |
Investigating Temozolomide Interactions with Secretory Proteins
Molecular docking has also illuminated potential mechanisms for overcoming temozolomide (TMZ) resistance in GBM treatment. A 2022 study investigated TMZ interactions with nine brain-enriched secretory proteins involved in gliomagenesis [73]. Automated docking using AutoDock 4.2 revealed encouraging binding affinity of TMZ with all targeted proteins, with the strongest interaction and lowest binding energies observed with GDF1 (-9.87 Kcal/mol) and SLIT1 (-9.95 Kcal/mol), followed by NPTX1, CREG2, and SERPINI1 [73]. Subsequent molecular dynamics simulations demonstrated that TMZ-protein complexes exhibited favorable stability and flexibility, suggesting TMZ may target these putative proteins implicated in GBM pathogenesis and treatment resistance [73].
Table 2: Binding Affinity of Temozolomide with GBM-Related Secretory Proteins
| Protein Target | Binding Energy (Kcal/mol) | Hydrogen Bonds | Key Interacting Residues |
|---|---|---|---|
| SLIT1 | -9.95 | None | ASP742, VAL745, ALA739 |
| GDF1 | -9.87 | LEU147, THR74 | VAL194, PRO192, LEU149 |
| NPTX1 | -8.92 | ASN380, LEU394 | ALA427, CYS397, ALA401 |
| CREG2 | -8.73 | None | LEU130, LEU195, CYS215 |
| SERPINI1 | -8.06 | LEU257, ILE238 | ARG259 |
Docking for Novel Inhibitor Design Against Emerging Targets
Recent studies have identified granulocyte colony-stimulating factor (GCSF) as a differentially expressed protein in GBM patient samples, with significantly elevated levels in biopsy specimens of malignant glioblastoma associated with tumor progression [74]. Computational docking analysis of the bacteriocin peptide Nisin against GCSF demonstrated promising binding interactions, which were subsequently validated through in vitro cytotoxic activity assays using human glioblastoma cell line SF-767, showing dose-dependent growth inhibition [74]. This integrated computational-experimental approach highlights how molecular docking can guide the identification and validation of novel therapeutic candidates for GBM treatment.
Experimental Protocols and Methodologies
Standard Molecular Docking Protocol for Glioblastoma Targets
A typical molecular docking workflow for GBM therapeutic development involves sequential steps from target preparation to pose analysis:
Target Protein Preparation
- Retrieve three-dimensional protein structures from the Protein Data Bank (PDB), selecting structures based on high resolution and completeness [71].
- Prepare structures using molecular modeling suites (e.g., Discovery Studio) to remove water molecules, heteroatoms, and add polar hydrogens [71].
- Define the active site region based on experimental data or through cavity detection algorithms like GRID, POCKET, or PASS for blind docking scenarios [70].
Ligand Preparation
- Sketch or retrieve ligand structures from chemical databases (e.g., ChemDraw) and perform geometry optimization using molecular mechanics (MM+) followed by semi-empirical methods (AM1 or PM3) [10].
- Generate multiple conformations to ensure adequate sampling of flexible torsion angles and ring systems.
Docking Execution
- Employ docking software (e.g., AutoDock, HADDOCK) with appropriate sampling algorithms based on system flexibility requirements [71] [73].
- For rigid receptor docking, utilize incremental construction or genetic algorithms; for flexible receptor docking, consider Monte Carlo or molecular dynamics approaches [70].
- Conduct multiple docking runs to ensure reproducibility of results.
Pose Analysis and Validation
- Cluster resulting poses based on root-mean-square deviation (RMSD) to identify representative binding modes.
- Analyze interaction patterns including hydrogen bonds, hydrophobic contacts, pi-stacking, and electrostatic interactions.
- Validate docking protocols by redocking known crystallographic ligands and calculating RMSD between experimental and predicted poses.
Advanced Techniques: Negative Image-Based Optimization
For challenging virtual screening applications, advanced techniques like Brute Force Negative Image-Based Optimization (BR-NiB) can significantly enhance docking performance [72]. This methodology optimizes cavity-based negative images through iterative atom removal and benchmarking:
- Generate initial negative image model of the binding cavity using software like PANTHER [72].
- Perform greedy search optimization by systematically removing cavity atoms and evaluating enrichment metrics (e.g., BR20, AUC) after each removal [72].
- Continue iterative optimization until enrichment metrics no longer improve, typically requiring 10-20 generations [72].
- Apply optimized models to rescore docking poses using shape/electrostatic potential complementarity via algorithms like SHAEP [72].
This approach has demonstrated substantial improvements in early enrichment factors (over 20-fold in some cases) compared to standard docking, particularly for targets like neuraminidase and retinoid X receptor alpha [72].
Research Reagent Solutions for Docking Studies
Table 3: Essential Research Reagents and Computational Tools for Molecular Docking
| Reagent/Software | Type | Primary Function | Application in GBM Research |
|---|---|---|---|
| AutoDock 4.2 | Software | Molecular docking simulation | TMZ interaction studies with secretory proteins [73] |
| HADDOCK Server | Software | Biomolecular docking | GBM surface receptor-ligand interactions [71] |
| Discovery Studio | Software | Structure preparation and analysis | Protein optimization and water molecule removal [71] |
| SHAEP | Algorithm | Shape/electrostatic similarity | Negative image-based rescoring [72] |
| PANTHER | Software | Cavity detection and filling | Generation of negative image models [72] |
| PDB Structures | Data Resource | Experimental protein structures | Source of 3D coordinates for docking targets [71] |
Integration with Virtual Screening Workflows
Molecular docking serves as a critical component in integrated virtual screening pipelines for glioblastoma drug discovery. Quantitative Structure-Activity Relationship (QSAR) models, particularly 3D-QSAR approaches like Comparative Molecular Similarity Index Analysis (CoMSIA), can significantly enhance docking workflows [10]. The typical integrated approach involves:
- Developing 2D and 3D-QSAR models using known active compounds to identify critical structural features and activity trends [10].
- Utilizing pharmacophore models based on QSAR results for initial virtual screening of compound libraries [65].
- Applying molecular docking to evaluate binding modes and affinity of prioritized compounds against target protein structures [65].
- Validating top-ranked compounds through molecular dynamics simulations to assess complex stability and interaction persistence [65].
This integrated methodology was successfully applied in the design of dihydropteridone derivatives as novel PLK1 inhibitors for GBM treatment, where 3D-QSAR models guided the optimization of molecular descriptors like "Min exchange energy for a C-N bond" (MECN), leading to compound 21E.153 with outstanding antitumor properties and docking capabilities [10].
Validation Strategies and Best Practices
Methodological Validation Approaches
Robust validation of molecular docking protocols is essential for generating reliable results in GBM therapeutic development:
Pose Reproduction Validation
- Redock known crystallographic ligands to calculate RMSD between experimental and predicted poses.
- Accept protocols that reproduce native poses with RMSD values ≤2.0 Å.
Virtual Screening Validation
- Use benchmark datasets like Directory of Useful Decoys (DUD-E) containing active compounds and matched decoys [72].
- Evaluate enrichment factors, area under the ROC curve (AUC), and early enrichment metrics (BEDROC).
- Compare performance against established docking benchmarks to assess relative improvement.
Experimental Correlation
- Where possible, correlate computational predictions with experimental binding assays (e.g., IC50, Ki values).
- Validate predicted binding mechanisms through site-directed mutagenesis of key interacting residues.
Molecular Dynamics Validation
Following molecular docking, molecular dynamics (MD) simulations provide critical validation of binding pose stability and complex behavior:
- Perform MD simulations using packages like GROMACS or AMBER to assess conformational stability of protein-ligand complexes [73].
- Analyze root-mean-square deviation (RMSD) of protein backbone and ligand heavy atoms to evaluate structural stability.
- Calculate root-mean-square fluctuation (RMSF) to identify regions of structural flexibility impacted by ligand binding.
- Employ specialized MD approaches like CABS-flex for efficient evaluation of protein-ligand complex flexibility [73].
- Use binding free energy calculations (MM/PBSA, MM/GBSA) to complement docking scores and improve affinity predictions.
Molecular docking represents a cornerstone methodology in the structure-based drug discovery pipeline for glioblastoma therapeutics, providing atomic-level insights into protein-ligand interactions that drive therapeutic efficacy. When properly validated and integrated with complementary computational approaches like 3D-QSAR, pharmacophore modeling, and molecular dynamics simulations, docking significantly accelerates the identification and optimization of novel GBM therapeutic candidates. The continuing development of advanced docking algorithms—particularly those addressing full receptor flexibility and offering improved scoring functions—promises to further enhance our ability to target the complex molecular machinery driving glioblastoma pathogenesis. As these computational methodologies evolve, they will play an increasingly vital role in overcoming the therapeutic challenges presented by this devastating disease.
Molecular Docking Validation Workflow
The high failure rate of drug candidates in oncology, with up to 50% of failures attributed to undesirable ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties, underscores the critical importance of comprehensive ADMET profiling in early drug discovery stages [75]. For glioblastoma (GBM) therapeutics, this challenge is particularly acute due to the blood-brain barrier (BBB), which severely limits drug distribution to tumor sites, and the high molecular heterogeneity of these tumors which causes variable drug responses [76] [77]. The integration of computational approaches, particularly virtual screening using 3D-QSAR models, with robust ADMET assessment creates a powerful framework for identifying promising glioblastoma therapeutic candidates with optimal pharmacokinetic and safety profiles before advancing to costly clinical trials [69].
This protocol details comprehensive methodologies for ADMET profiling specifically contextualized within glioblastoma therapeutic development, where computational models must account for the unique challenges of brain tumor targeting. We present standardized experimental workflows, quantitative benchmarking data, and practical tools that research teams can implement to enhance their virtual screening pipelines for identifying glioblastoma therapeutics with higher clinical translation potential.
Computational ADMET Prediction Platforms and Protocols
Table: Computational Platforms for ADMET Prediction in Glioblastoma Drug Discovery
| Platform/Tool Name | Primary Function | Key Features | Applicability to Glioblastoma |
|---|---|---|---|
| ChemMORT | Multi-parameter ADMET optimization | Inverse QSAR design; Particle swarm optimization; Manages 9 ADMET endpoints | Optimizes BBB penetration and reduces neurotoxicity [75] |
| PharmaBench | ADMET benchmark dataset | 52,482 entries; 11 ADMET properties; LLM-curated experimental conditions | Training models for CNS drug property prediction [78] |
| Machine Learning Models [79] | FAK inhibitor activity prediction | LightGBM, Random Forest algorithms; R² = 0.892 for FAK inhibition | Targets glioblastoma invasion pathways [79] |
| 3D-QSAR Models [69] | Flavonoid activity prediction | R² = 0.91; Q² = 0.82; Molecular field analysis | Bcl-2 family protein inhibition for glioblastoma [69] |
| Deep-PK/DeepTox [80] | PK and toxicity prediction | Graph-based descriptors; Multitask learning | Manages neuro-specific toxicity endpoints [80] |
Protocol: Implementation of Computational ADMET Screening
Objective: To integrate computational ADMET prediction early in the virtual screening workflow for glioblastoma therapeutic candidates, enabling prioritization of compounds with optimal CNS pharmacokinetic profiles.
Materials and Software Requirements:
- ChemMORT platform (available at: https://cadd.nscc-tj.cn/deploy/chemmort/) [75]
- PharmaBench dataset for model training and validation [78]
- Molecular docking software (e.g., AutoDock, GOLD)
- 3D-QSAR modeling environment
- Python 3.7+ with scikit-learn, RDKit, and Deep Learning libraries [79]
Methodology:
Compound Library Preparation
3D-QSAR Model Development
- Align molecular structures using field-based or common scaffold approaches
- Calculate molecular interaction fields using appropriate probes
- Apply partial least squares (PLS) regression for model building
- Validate model using leave-one-out and external test sets
- For flavonoids targeting Bcl-2 proteins, benchmark against reported model (R² = 0.91, Q² = 0.82) [69]
ADMET Endpoint Prediction
- Implement nine ADMET prediction models within ChemMORT covering:
- Distribution: logD7.4, BBB penetration (logBB)
- Metabolism: CYP450 interactions
- Toxicity: hERG, hepatotoxicity, AMES mutagenicity [75]
- Utilize XGBoost algorithm with 512-dimensional molecular vectors
- Apply customized scoring scheme for glioblastoma-specific priorities
- Implement nine ADMET prediction models within ChemMORT covering:
Multi-parameter Optimization
- Apply particle swarm optimization (PSO) to navigate chemical space
- Set constraints to maintain target potency (e.g., FAK inhibition pIC50 > 7.0) [79]
- Prioritize compounds with balanced ADMET profile and predicted glioblastoma activity
Experimental Validation of ADMET Properties
Table: Experimental ADMET Assessment for Curcumin Derivatives in Glioblastoma Models
| Compound | IC50 (µg/mL) SF268 Cells | Selectivity Index | BBB Penetration Prediction | Metabolic Stability | Toxicity Profile |
|---|---|---|---|---|---|
| Curcumin | 6.30 | 2.5 | Low | Rapid metabolism | Low cytotoxicity [76] |
| Compound 2 | 0.59-3.97 | 3-20 | Moderate | Improved | Favorable [76] |
| Compound 4 | 0.59-3.97 | 3-20 | High | Significantly improved | Minimal toxicity [76] |
| Compound 6 | 0.59-3.97 | 3-20 | High | Significantly improved | Minimal toxicity [76] |
Protocol: In Vitro ADMET Assessment for Glioblastoma Therapeutics
Objective: To experimentally validate key ADMET properties for lead compounds identified through virtual screening against glioblastoma models.
Materials and Reagents:
- SF268 glioblastoma cell line (ATCC CRL-1712)
- Vero cells (ATCC CCL-81) for selectivity assessment
- Caco-2 cell line (ATTC HTB-37) for permeability studies
- Transwell plates (0.4 μm pore size, 12-well)
- HBSS (Hanks' Balanced Salt Solution)
- MTT reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide)
- Rhodamine 123 for mitochondrial membrane potential assessment
- BAX antibody for apoptosis mechanism studies [76]
Blood-Brain Barrier Penetration Assessment:
Caco-2 Permeability Assay
- Culture Caco-2 cells on Transwell membranes for 21 days until full differentiation
- Confirm monolayer integrity by measuring TEER (>400 Ω·cm²)
- Prepare compound solutions (10 μM) in HBSS buffer (pH 7.4)
- Apply donor solution to apical chamber (for A-B transport) or basolateral chamber (for B-A transport)
- Sample from receiver chambers at 30, 60, 90, and 120 minutes
- Analyze compound concentration using HPLC-MS/MS
- Calculate apparent permeability (Papp) using formula: Papp = (dQ/dt) / (A × C0)
- Interpret results: Papp > 10×10⁻⁶ cm/s indicates high BBB penetration potential
MDCK Cell Permeability Assay
- Culture MDCK cells on Transwell membranes for 5-7 days
- Follow similar protocol as Caco-2 assay with reduced incubation time
- Include reference compounds (e.g., propranolol for high permeability, atenolol for low permeability)
Metabolic Stability Assessment:
- Liver Microsome Incubation
- Prepare incubation mixture: 0.5 mg/mL liver microsomes, 1 mM NADPH, test compound (1 μM) in phosphate buffer
- Incubate at 37°C with shaking
- Aliquot at 0, 5, 15, 30, and 60 minutes
- Quench reaction with ice-cold acetonitrile
- Analyze parent compound remaining by LC-MS/MS
- Calculate half-life (t₁/₂) and intrinsic clearance (CLint)
Cytotoxicity and Selectivity Assessment:
- MTT Cytotoxicity Assay
- Seed SF268 glioblastoma cells and Vero normal cells in 96-well plates (5,000 cells/well)
- After 24 hours, treat with test compounds at concentrations ranging from 0.1-100 μg/mL
- Incubate for 72 hours at 37°C, 5% CO₂
- Add MTT solution (0.5 mg/mL) and incubate for 4 hours
- Dissolve formazan crystals with DMSO
- Measure absorbance at 570 nm with reference at 630 nm
- Calculate IC50 values using nonlinear regression
- Determine Selectivity Index (SI) = IC50 Vero cells / IC50 SF268 cells [76]
Mechanism of Action Studies:
Microtubule Depolymerization Assay
- Treat SF268 cells with test compounds at IC50 concentration for 24 hours
- Fix cells with 4% paraformaldehyde, permeabilize with 0.1% Triton X-100
- Stain with anti-α-tubulin antibody and DAPI
- Visualize using confocal microscopy
- Quantify microtubule organization and density
Mitochondrial Membrane Potential (ΔΨm) Assessment
- Load compound-treated cells with Rhodamine 123 (10 μM) for 30 minutes
- Analyze fluorescence intensity by flow cytometry
- Collapse in ΔΨm indicated by decreased fluorescence
BAX Activation Assay
- Perform immunofluorescence staining with anti-BAX antibody
- Assess BAX translocation to mitochondria
- Counterstain with mitochondrial marker
Integration of ADMET Profiling in Glioblastoma Therapeutic Development
Research Reagent Solutions for ADMET Profiling
| Reagent/Cell Line | Application | Key Features | Provider/Reference |
|---|---|---|---|
| SF268 Glioblastoma Cells | Cytotoxicity assessment | Stable cell line derived from CNS tumors | ATCC CRL-1712 [76] |
| Caco-2 Cell Line | Intestinal permeability/BBB model | Differentiates into enterocyte-like monolayers | ATCC HTB-37 [78] |
| U-87 MG Glioblastoma | 3D spheroid models, efficacy testing | Represents glioblastoma invasiveness | CHEMBL3307575 [79] [69] |
| Human Liver Microsomes | Metabolic stability studies | Phase I metabolism evaluation | Commercial vendors (e.g., Corning) |
| Transwell Plates | Permeability assays | 0.4 μm pore size for cell culture | Corning, Costar |
| MTT Reagent | Cell viability assessment | Tetrazolium reduction assay | Sigma-Aldrich [76] |
Case Study: ADMET Optimization of Curcumin Derivatives for Glioblastoma
The development of curcumin derivatives exemplifies the successful application of comprehensive ADMET profiling in glioblastoma therapeutics. Curcumin itself demonstrates promising bioactivity against SF268 glioblastoma cells (IC50: 6.3 µg/mL) but suffers from poor water solubility, rapid metabolism, and low BBB penetration [76]. Through strategic structural modifications, particularly to the hydroxyl groups on the aromatic rings, researchers developed derivatives with significantly improved properties:
Structural Optimization Strategy:
- Protection of phenolic hydroxyl groups to enhance metabolic stability
- Modification of β-diketone moiety to improve chemical stability
- Incorporation of substituents to enhance BBB penetration
Results:
- Derivatives 2-4, 6, and 11 demonstrated 10-fold improved potency (IC50: 0.59-3.97 µg/mL) compared to curcumin
- Significantly enhanced selectivity indices (SI: 3-20) compared to curcumin (SI: 2.5)
- Compound 4, with fully protected aromatic domains, emerged as the lead candidate with optimal ADMET profile for in vivo validation [76]
Mechanistic Insights:
- Lead compounds effectively destabilized microtubules in glioblastoma cells
- Induced mitochondrial membrane potential collapse
- Activated BAX-mediated apoptosis pathways
- Demonstrated favorable in silico ADMET predictions for CNS targeting
Protocol: PK/PD Modeling for Glioblastoma Therapeutic Optimization
Objective: To integrate ADMET data into pharmacokinetic-pharmacodynamic (PK/PD) models that predict drug efficacy in glioblastoma tumors.
Methodology:
Pharmacokinetic Modeling
- Develop multi-compartmental PK models incorporating BBB transport
- Parameterize models using in vitro ADMET data (permeability, metabolic clearance)
- Incorporate tumor compartment with enhanced permeability and retention (EPR) effect
Pharmacodynamic Modeling
- Implement tumor growth inhibition (TGI) models linked to drug exposure
- Incorporate heterogeneous drug distribution within glioblastoma tumors
- Account for resistance mechanisms specific to glioblastoma stem cells
Translational Projection
- Scale preclinical PK parameters to human equivalents using allometric scaling
- Predict human efficacious dose based on target exposure from PD models
- Optimize dosing regimens to maintain therapeutic concentrations in brain tumor tissue [77]
Application Example:
- A PK/PD model for temozolomide personalized dosing significantly reduced tumor size and toxicity compared to standard protocols [77]
- Models addressing glioblastoma heterogeneity can predict variable drug distribution and responses that standard analyses might miss
Comprehensive ADMET profiling, when integrated with virtual screening approaches such as 3D-QSAR modeling, provides an essential framework for advancing glioblastoma therapeutics with optimal pharmacokinetic properties and minimal toxicity. The protocols and platforms detailed in this application note enable research teams to systematically evaluate and optimize critical ADMET parameters early in the drug discovery process, with particular emphasis on the unique challenges presented by glioblastoma treatment. Through the implementation of these standardized methodologies, researchers can significantly improve the probability of clinical success for novel glioblastoma therapeutics by ensuring favorable pharmacokinetics and low toxicity profiles before advancing to costly clinical development stages.
Assessing Binding Stability and Free Energy with Molecular Dynamics (MD) Simulations
Molecular Dynamics (MD) simulations have become an indispensable computational tool in modern drug discovery, providing critical insights into the dynamic interactions between therapeutic compounds and their biological targets. In the context of glioblastoma (GBM), one of the most aggressive and treatment-resistant brain tumors, MD simulations enable researchers to move beyond static structural snapshots to understand the temporal evolution and stability of ligand-target complexes. This application note details protocols for employing MD simulations to assess binding stability and calculate free energy within a virtual screening pipeline for glioblastoma therapeutics, integrating with 3D-QSAR models to prioritize compounds with the highest potential for therapeutic efficacy.
The complex molecular profile of GBM necessitates multi-target therapeutic approaches. Recent studies have validated the utility of MD simulations for investigating potential GBM treatments, including polyphenol-based therapeutics [81], small-molecule CHI3L1 inhibitors [13], and novel FAK inhibitors [21]. These simulations provide quantitative metrics, such as binding free energies and complex stability parameters, that are essential for rational drug design and optimization against challenging targets like GRP78-CRIPTO [82] and VEGFA [20].
Key Quantitative Data from Recent Glioblastoma Studies
Table 1: Summary of Binding Free Energy and Stability Data from Recent Glioblastoma Studies
| Study Focus | Compound/Target | Binding Free Energy (kcal/mol) | Key Stability Metrics | Experimental Validation (IC50) |
|---|---|---|---|---|
| Polyphenol-based Therapeutics [81] | Mangiferin (5IKT complex) | -32.0 ± 4.4 | Most stable complex; Reduced conformational variability | 4.65 µM |
| Morin | Not specified | Favorable binding stability | 9.43 µM | |
| GRP78-CRIPTO Interaction [82] | Region 4 Complex | -126.26 | Highest stability among four regions | Not specified |
| Region 3 Complex | -81.92 | Stable interaction | Not specified | |
| Region 2 Complex | -59.78 | Stable interaction | Not specified | |
| Region 1 Complex | -15.07 | Stable interaction | Not specified | |
| FAK Inhibitors [21] | Machine learning-identified compounds | Not specified | Stable binding validated through MD | Predicted active from 275 candidates |
| VEGFA Inhibitors [20] | G868-0191 | Not specified | Most stable inhibitor in MD simulations | Not specified |
Table 2: Molecular Docking Affinities for Promising Glioblastoma Compounds
| Compound | Target PDB | Docking Affinity (kcal/mol) | Reference |
|---|---|---|---|
| Mangiferin | 6ESM | -11.0 | [81] |
| Mangiferin | 5UGC | -8.2 | [81] |
| Mangiferin | 5UFW | -7.5 | [81] |
| Mangiferin | 5IKT | -9.1 | [81] |
| CHI3L1 Inhibitors | Compound 8 | Kd: 6.8 µM (MST) | [13] |
| CHI3L1 Inhibitors | Compound 39 | Kd: 22 µM (MST) | [13] |
Computational Protocols and Methodologies
Comprehensive MD Simulation Protocol for Binding Stability Assessment
System Preparation:
- Obtain the initial protein-ligand complex from molecular docking studies (e.g., Autodock Vina, Glide)
- Solvate the complex in an appropriate water model (TIP3P is commonly used) in a triclinic box
- Add ions (Na+, Cl-) to neutralize system charge and achieve physiological salt concentration (0.15 M)
- Ensure a minimum distance of 1.0 nm between the protein and box edges
Energy Minimization:
- Perform steepest descent minimization for 5,000 steps or until maximum force < 1000 kJ/mol/nm
- Apply position restraints on protein heavy atoms during initial minimization (force constant: 1000 kJ/mol/nm²)
- Conduct subsequent minimization without restraints until convergence
System Equilibration:
- NVT ensemble equilibration for 100 ps with modified Berendsen thermostat (coupling constant: 0.1 ps) at 300 K
- NPT ensemble equilibration for 100 ps with Parrinello-Rahman barostat (coupling constant: 2.0 ps) at 1 bar
- Maintain position restraints on protein heavy atoms during equilibration phases
Production MD Simulation:
- Run unrestrained production simulation for 100-200 ns (longer for complex systems)
- Use a 2-fs time step with LINCS constraints on all bonds
- Employ Particle Mesh Ewald (PME) method for long-range electrostatics
- Save coordinates every 10 ps for subsequent analysis
Binding Free Energy Calculation Using MM-GBSA/PBSA
Trajectory Preparation:
- Remove water molecules and ions from the trajectory
- Ensure consistent numbering of atoms across frames
- Superpose trajectories to remove rotational and translational motions
MM-GBSA/PBSA Calculation:
- Extract evenly spaced frames from the stable simulation period (e.g., every 100 ps)
- Calculate the binding free energy using the following equation: ΔGbind = Gcomplex - (Gprotein + Gligand) Where G for each component is calculated as: G = Egas + Gsolv - TS Egas = Eint + Eele + Evdw Gsolv = GGB/PB + G_SA
Entropy Estimation:
- Use normal mode analysis or quasi-harmonic approximation
- Calculate conformational entropy from positional fluctuations
- Note: Entropy calculations are computationally demanding and often omitted for high-throughput screening
Advanced Analysis Techniques
Root Mean Square Deviation (RMSD):
- Calculate backbone RMSD to assess overall protein stability
- Calculate ligand RMSD to evaluate binding pose stability
- Systems with RMSD < 2-3 Å typically indicate stable complexes
Root Mean Square Fluctuation (RMSF):
- Analyze residual fluctuations to identify flexible regions
- Correlate binding site flexibility with ligand affinity
Principal Component Analysis (PCA):
- Identify essential dynamics and collective motions
- Project trajectories onto principal components to visualize conformational sampling
Hydrogen Bond Analysis:
- Monitor persistent hydrogen bonds between ligand and protein
- Identify key residues contributing to binding stability
Interaction Energy Decomposition:
- Per-residue decomposition to identify hot spot residues
- Electrostatic and van der Waals contributions analysis
Integration with Virtual Screening Workflows
The integration of MD simulations into virtual screening workflows for glioblastoma therapeutics provides a powerful multi-stage filtering approach. As demonstrated in recent studies, this integrated framework begins with large compound libraries that undergo initial virtual screening, followed by 3D-QSAR prediction to estimate activity against specific GBM targets [21]. Promising compounds then proceed to molecular docking to generate initial binding poses, which serve as starting points for detailed MD simulations. The MD phase assesses temporal stability and refines binding modes, while subsequent MM-GBSA/PBSA calculations provide quantitative binding free energy estimates [81] [82]. This comprehensive computational pipeline efficiently narrows thousands of initial compounds to a manageable number of high-priority candidates for experimental validation.
Signaling Pathways in Glioblastoma and Computational Assessment
MD simulations play a crucial role in investigating therapeutic interventions in key glioblastoma signaling pathways. The GRP78-CRIPTO complex activates multiple oncogenic pathways, including MAPK/AKT signaling, Src/PI3K/AKT, and Smad2/3 pathways, which drive tumor proliferation, plasticity, and therapy resistance [82]. Similarly, focal adhesion kinase (FAK) regulates essential processes in GBM progression, including epithelial-mesenchymal transition, angiogenesis, cell migration, and invasion [21]. Other critical targets validated through computational approaches include CHI3L1, which promotes STAT3 signaling and mesenchymal transition [13], and VEGFA, a key regulator of angiogenesis [20]. MD simulations enable researchers to assess how potential therapeutics disrupt these pathways by quantifying binding stability to specific targets and predicting the structural consequences of inhibition.
Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for MD Simulations
| Category | Specific Tools/Reagents | Function/Application | Reference |
|---|---|---|---|
| MD Simulation Software | AMBER, GROMACS, NAMD | Molecular dynamics simulation engines | [81] [82] |
| Analysis Tools | AmberTools, VMD, MDAnalysis | Trajectory analysis and visualization | [81] |
| Docking Software | AutoDock Vina, Glide, HADDOCK | Protein-ligand and protein-protein docking | [13] [82] |
| Free Energy Methods | MM-GBSA, MM-PBSA | Binding free energy calculation | [81] [82] |
| Quantum Chemistry | Density Functional Theory (DFT) | Electronic property analysis | [81] |
| Data Sources | CHEMBL, Protein Data Bank | Compound and protein structure databases | [21] |
| Machine Learning | Scikit-learn, LightGBM, Random Forest | Predictive modeling of compound activity | [21] |
Troubleshooting and Optimization Guidelines
Common Issues and Solutions:
High System Instability: If the simulation crashes due to high energy, extend the equilibration phases and ensure proper minimization before production runs. Check for atomic clashes in the initial structure.
Poor Ligand Binding Pose Stability: If the ligand drifts significantly from the initial docking pose during simulation, consider longer simulation times (200+ ns) or re-evaluate the docking pose. Implement positional restraints on protein backbone atoms during initial equilibration.
Inaccurate Solvation Effects: Ensure sufficient water molecules surround the protein-ligand complex. Use explicit solvent models rather than implicit for more accurate representation of solvation effects.
Convergence Issues in Free Energy Calculations: Use multiple, independent simulations to assess convergence. Ensure sampling is sufficient by extending simulation time or using enhanced sampling techniques.
Optimization Strategies:
- Implement accelerated sampling methods (GaMD, aMD) for improved conformational sampling
- Use multi-trajectory approach for MM-GBSA calculations to reduce statistical error
- Employ hybrid QM/MM methods for systems requiring electronic structure accuracy
- Leverage machine learning potentials to extend timescales accessible to simulations
The integration of MD simulations for assessing binding stability and free energy represents a cornerstone of modern computational approaches to glioblastoma therapeutic development. The protocols outlined in this application note provide researchers with robust methodologies for evaluating candidate compounds within virtual screening pipelines. As demonstrated in recent studies, these approaches have successfully identified promising therapeutics including polyphenol-based compounds [81], CHI3L1 inhibitors [13], and FAK inhibitors [21] with validated activity against GBM models.
Future developments in this field will likely focus on enhanced sampling techniques to access longer timescales, more accurate force fields for improved predictive capability, and tighter integration with machine learning approaches for rapid screening of ultra-large compound libraries. The continued refinement of these computational protocols will accelerate the discovery of effective therapeutics against this devastating disease.
Glioblastoma (GBM) remains the most aggressive and lethal primary brain tumor in adults, characterized by a median survival of only 12-18 months despite intensive treatment protocols [1]. The current standard of care involves maximal surgical resection followed by radiation therapy and temozolomide chemotherapy, but treatment efficacy is severely limited by therapeutic resistance, tumor heterogeneity, and the formidable blood-brain barrier (BBB) [83] [1]. The molecular landscape of GBM is characterized by key oncogenic drivers including epidermal growth factor receptor (EGFR) amplification, platelet-derived growth factor receptor (PDGFR) alterations, and dysregulation of the PI3K/AKT/mTOR pathway, which collectively promote tumorigenesis, invasion, and therapeutic resistance [1]. Molecular classification has further refined GBM into subtypes—proneural, neural, classical, and mesenchymal—each with distinct genetic features and clinical behaviors [1].
Against this challenging backdrop, targeted inhibitor therapies have emerged as promising avenues for intervention. This analysis provides a comprehensive benchmarking of established clinical compounds against novel investigational inhibitors, with particular focus on their application within virtual screening frameworks using 3D-QSAR models for glioblastoma therapeutics research. The integration of computational approaches with experimental validation offers transformative potential for accelerating drug discovery in this critically underserved area of oncology [46] [9].
Established Clinical Compounds: Mechanisms and Limitations
Table 1: Benchmarking Established Clinical Inhibitors in Glioblastoma
| Therapeutic Agent | Primary Target | Mechanism of Action | Clinical Status | Key Limitations |
|---|---|---|---|---|
| Temozolomide | DNA | Alkylating agent causing DNA methylation | Standard of care | Resistance via MGMT expression; limited BBB penetration |
| Vorasidenib | IDH1/2 mutant enzymes | Inhibits mutant IDH1/2, reduces 2-HG production | FDA-approved for IDH-mutant astrocytoma | Restricted to IDH-mutant tumors only |
| ONC201 (Dordaviprone) | H3 K27M-mutant gliomas | First-in-class therapy for H3 K27M alterations | FDA-approved for H3 K27M-mutant gliomas | Limited to specific genetic subtype |
| Ivosidenib (AG-120) | mIDH1 | Inhibits mutant IDH1 enzyme | FDA-approved for AML; investigational for GBM | Reported resistance mechanisms |
| Safusidenib | mIDH1 | Precision targeting of IDH1-mutated glioma | Clinical trials | Specific to IDH1 mutations only |
Established clinical compounds face significant challenges in glioblastoma treatment. Temozolomide, while the standard of care, demonstrates limited efficacy due to the development of resistance mechanisms mediated by O6-methylguanine-DNA methyltransferase (MGMT) expression and insufficient penetration across the blood-brain barrier [84] [83]. Targeted agents such as vorasidenib and safusidenib, while mechanistically innovative, are restricted to specific molecular subsets of GBM patients harboring IDH1 mutations, which represent only a fraction of the overall GBM population [83] [1]. Similarly, ONC201 represents a breakthrough for H3 K27M-mutant gliomas but has no demonstrated efficacy in other molecular subtypes [83].
The limitations of established compounds extend beyond target specificity to include pervasive challenges with intratumoral heterogeneity, compensatory signaling pathway activation, and the immunosuppressive tumor microenvironment that characterizes GBM [1]. Furthermore, the successful delivery of therapeutic agents to intracranial tumors remains a fundamental obstacle, as the blood-brain barrier effectively excludes most systematically administered compounds, contributing to the high failure rate of neuro-oncology clinical trials [85]. These collective limitations underscore the critical need for novel inhibitor development and more effective drug screening methodologies.
Emerging Novel Inhibitors: Pipeline and Preclinical Assessment
Table 2: Promising Novel Inhibitors in Glioblastoma Pipeline
| Therapeutic Agent | Novel Target/Mechanism | Development Stage | Key Advantage | Research Evidence |
|---|---|---|---|---|
| MT-125 | Non-muscle myosin IIA/IIB inhibitor | Phase I (FDA-cleared) | Quadruple mechanism: enhances chemo/radio-sensitivity, blocks invasion | Preclinical: prolonged survival in GBM models [86] |
| TNG456 | Targets MTAP-deficient tumors | Phase I/II | Specifically targets MTAP loss, common in GBM | Clinical trials enrolling solid tumors with MTAP loss [8] |
| BMX-001 | Redox-active metalloporphyrin | Phase III | Dual action: augments tumor killing, protects normal tissue | In development with BioMimetix [87] |
| Enzastaurin (DB102) | PKCβ, PI3K, and AKT pathway inhibitor | Phase III (biomarker-guided) | Oral administration; biomarker-driven patient selection | Denovo BioPharma; orphan drug designation [87] |
| Abemaciclib | CDK4/6 inhibitor | Phase II | Investigated for newly diagnosed grade 3 meningioma | Clinical trial: NCT06173014 [8] |
| Mol_370 (CDK6 inhibitor) | Selective CDK6 inhibition | Computational discovery | Enhanced selectivity over CDK1/2; potential BBB penetration | Molecular docking & dynamics [46] |
The glioblastoma therapeutic pipeline contains numerous promising novel inhibitors with diverse mechanisms of action. MT-125 represents a particularly innovative approach, targeting non-muscle myosin IIA and IIB motors in glioblastoma cells. This experimental medication employs a quadruple mechanism: sensitizing previously resistant malignant cells to radiation, creating multinucleated cells that cannot separate and are marked for cell death, blocking cellular invasion capacity, and delivering powerful synergistic responses when combined with kinase inhibitors [86]. In animal studies, MT-125 combined with kinase inhibitors created "long periods of a disease-free state that we haven't seen in these mouse models before" according to neuro-oncologist Steven Rosenfeld [86].
Other notable candidates include TNG456, which specifically targets tumors with MTAP loss—a common occurrence in glioblastoma—currently in Phase I/II clinical trials [8]. BMX-001 represents a novel class of redox-active small molecules that simultaneously augment tumor killing by radiation therapy while protecting normal tissue from radiation-induced injury [87]. Enzastaurin inhibits PKCβ, PI3K, and AKT pathways and is being investigated in a biomarker-guided Phase III trial for newly diagnosed GBM [87].
Computational approaches have identified additional promising candidates such as Mol_370, a selective CDK6 inhibitor discovered through integrated computational methods. This pyrimidine-based compound demonstrated substantial stability in density functional theory analysis and effective binding to CDK6 through hydrophobic interactions and hydrogen bonds in molecular dynamics simulations [46].
Virtual Screening and 3D-QSAR Models in Inhibitor Development
Computational Framework for Inhibitor Discovery
The development of novel glioblastoma inhibitors has been significantly accelerated by advances in virtual screening and 3D quantitative structure-activity relationship (3D-QSAR) modeling. These computational approaches enable rapid identification and optimization of therapeutic candidates before resource-intensive synthesis and experimental validation. For glioblastoma specifically, these methods must account for the unique requirement of blood-brain barrier penetration, adding an additional dimension to compound evaluation [46].
A recent study applied 3D-QSAR modeling to isocitrate dehydrogenase 1 (IDH1) mutants, developing both Comparative Molecular Field Analysis (CoMFA, R² = 0.980, Q² = 0.765) and Comparative Molecular Similarity Index Analysis (CoMSIA, R² = 0.997, Q² = 0.770) models with notably decent predictive ability [9]. These models were used to design novel structures through scaffold hopping, with compounds C3, C6, and C9 showing higher predicted pIC50 values in the 3D-QSAR model. Molecular dynamics simulations further identified potent mIDH1 inhibitors, with compound C2 exhibiting the highest binding free energy with IDH1 at -93.25 ± 5.20 kcal/mol [9].
For CDK6 inhibitors, integrated computational approaches have identified promising pyrimidine-based compounds. Ligand-based virtual screening using the vROCS tool identified Mol370 as a lead candidate with close similarity to co-crystallized ligands. Molecular docking revealed interactions at the CDK6 inhibitor-binding site via typical chemical interactions, such as hydrophobic interactions and hydrogen bonds, while MD simulations confirmed Mol370's compatibility with structural and functional requirements for effective CDK6 inhibition [46].
Experimental Protocols for Computational Screening
Protocol 1: Molecular Docking for CDK6 Inhibitor Screening
This protocol outlines the procedure for virtual screening of CDK6 inhibitors using molecular docking approaches, based on methodology from Nature Scientific Reports [46].
- Step 1: Protein Preparation: Retrieve CDK6 crystal structure (PDB ID: 6OQL) from Protein Data Bank. Prepare the protein using Schrödinger's Protein Preparation Wizard to assign correct bond orders, add hydrogens, detect disulfide bonds, and fix structural irregularities without altering protein geometry.
- Step 2: Receptor Grid Generation: Generate a three-dimensional receptor grid using the receptor grid generation interface in Maestro gliding program. Center the grid on active site residues with x-, y-, and z-axes coordinates at 21.84, 37.55, and -9.73 respectively.
- Step 3: Ligand-Based Virtual Screening (LBVS): Perform LBVS using the vROCS tool for rapid overlay of chemical structures. Create a query model using the co-crystallized ligand N1A (CCL) within the 6OQL binding pocket as a template. Screen against significant molecule collections from e.Molecules database using ShapeTanimoto, ColorTanimoto, and TanimotoCombo metrics.
- Step 4: Ligand Preparation: Prepare top 500 lead ligands using Schrödinger Suite Maestro 12.5 LigPrep. Determine chirality from 3D structure and obtain geometry-optimized structures using OPLS3 at pH 7.0 ± 2.0.
- Step 5: Molecular Docking Protocol: Perform docking using Maestro 12.5 Glide tool with extra precision (XP) mode. Implement flexible ligand sampling without relying solely on refining. Re-dock co-crystallized ligand to validate binding affinity before docking ligand library.
- Step 6: Structural Interaction Fingerprinting (SIFt) Analysis: Convert three-dimensional structural binding characteristics of ligand-protein complexes to binary digit interaction fingerprints using SIFt approach. Generate interaction fingerprints for top 50 docking complexes to identify key interaction features including H-bond acceptors, H-bond donors, and hydrophobic features.
Protocol 2: 3D-QSAR Model Development for IDH1 Inhibitors
This protocol describes the creation of 3D-QSAR models for IDH1 inhibitor optimization, based on research published in the International Journal of Molecular Sciences [9].
- Step 1: Dataset Curation: Collect 47 compounds with pyridin-2-one common backbone and associated inhibition activities. Divide into training set (38 compounds) and test set (9 compounds). The dataset should include compounds with IC50 values ranging from high activity (0.035 μM) to low activity (4.200 μM).
- Step 2: Molecular Alignment: Align all compounds based on their common skeleton structure. Ensure proper structural alignment for comparative analysis.
- Step 3: CoMFA Model Development: Develop Comparative Molecular Field Analysis (CoMFA) model using steric and electrostatic field parameters. Optimize model to achieve R² = 0.980 and Q² = 0.765 for predictive capability.
- Step 4: CoMSIA Model Development: Develop Comparative Molecular Similarity Index Analysis (CoMSIA) model incorporating steric, electrostatic, hydrophobic, hydrogen bond donor, and hydrogen bond acceptor fields. Target R² = 0.997 and Q² = 0.770 for robust predictive performance.
- Step 5: Scaffold Hopping and Novel Compound Design: Apply scaffold hopping techniques to design novel structures based on 3D-QSAR model predictions. Select compounds with higher predicted pIC50 values for further investigation.
- Step 6: Molecular Dynamics Validation: Perform molecular dynamics simulations to validate binding interactions, stability, and binding free energy. Analyze parameters including free energy landscape, radius of gyration, solvent accessible surface area, and polar surface area.
Signaling Pathways and Experimental Workflows
Clinical Translation: From Computational Prediction to Therapeutic Application
Advanced Clinical Trial Designs for Accelerated Evaluation
The transition from computational prediction to clinical application requires innovative trial designs that can efficiently evaluate therapeutic efficacy. Phase 0 and window-of-opportunity trials have emerged as valuable approaches for assessing novel glioblastoma inhibitors, particularly for evaluating blood-brain barrier penetration and target engagement [85].
These trials feature short treatment durations (typically a few days to weeks) implemented during the interval between diagnosis and standard treatment, ideally within a four-week timeframe. Primary endpoints focus on molecular or functional imaging parameters as surrogate markers of treatment efficacy, including decreased phosphorylation of targeted kinase receptors, modulation of cell cycle regulators, or metabolic alterations detected via 18F-FDG-PET imaging [85].
The critical distinction between phase 0 and window-of-opportunity trials lies in dosing strategy: traditional phase 0 trials utilize non-therapeutic microdoses, while window-of-opportunity trials employ therapeutic doses for brief durations to ensure adequate BBB penetrance and meaningful assessment of pharmacodynamic effects [85]. This approach allows for early elimination of ineffective therapies and promotes efficient drug development, potentially reducing the average duration from phase II to phase III trials, which currently stands at 7.2 years for GBM with over 91% of phase III trials proving unsuccessful [85].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Glioblastoma Inhibitor Development
| Category | Specific Tools/Platforms | Research Application | Key Features |
|---|---|---|---|
| Molecular Docking Software | Maestro (Schrödinger), AutoDock, Glide | Protein-ligand interaction prediction | XP precision mode; flexible ligand sampling; grid-based docking |
| 3D-QSAR Modeling | CoMFA, CoMSIA | Quantitative structure-activity relationship modeling | Steric/electrostatic field analysis; predictive activity modeling |
| Virtual Screening | vROCS, eMolecules database | Ligand-based compound screening | ShapeTanimoto, ColorTanimoto metrics; rapid overlay of structures |
| Molecular Dynamics | GROMACS, AMBER, Desmond | Binding stability and dynamics analysis | Free energy landscape; radius of gyration; binding free energy |
| ADMET Prediction | ADMET Predictor, SwissADME | Absorption, distribution, metabolism, excretion, toxicity | BBB penetration prediction; toxicity risk assessment |
| Structural Biology | Protein Data Bank (PDB) | Target protein structure retrieval | X-ray crystallography structures (e.g., CDK6: 6OQL) |
| Clinical Trial Platforms | ClinicalTrials.gov, NBTS Clinical Trial Finder | Trial identification and design | Comprehensive database of active neuro-oncology trials |
The comparative analysis of novel inhibitors against established clinical compounds reveals a dynamic landscape in glioblastoma therapeutics. Established compounds face significant limitations including restricted target populations, resistance mechanisms, and inadequate blood-brain barrier penetration. Novel inhibitors such as MT-125, TNG456, and computationally discovered compounds like Mol_370 offer promising alternative mechanisms and improved targeting capabilities.
The integration of virtual screening approaches with 3D-QSAR modeling represents a transformative paradigm for accelerating glioblastoma drug discovery. These computational methods enable more efficient identification and optimization of therapeutic candidates with improved likelihood of clinical success. Furthermore, advanced clinical trial designs including phase 0 and window-of-opportunity studies provide frameworks for more efficient translation of computational predictions to clinical applications.
Future directions should emphasize the integration of multi-omics data, enhanced BBB penetration prediction in silico models, and patient-derived tumor models that better recapitulate the immunosuppressive glioblastoma microenvironment. As these technologies converge, they offer the potential to significantly improve the dismal prognosis associated with glioblastoma through more targeted, effective therapeutic interventions.
Conclusion
The integration of 3D-QSAR-based virtual screening with machine learning and multi-stage validation represents a transformative approach in glioblastoma drug discovery. This methodology has proven effective in identifying and optimizing novel, potent inhibitors against critical targets such as PLK1, mIDH1, and FAK. The future of this field lies in refining these computational models with larger, more diverse datasets, improving the prediction of blood-brain barrier penetration, and fostering closer integration with experimental wet-lab studies. By systematically addressing the challenges of model robustness and lead compound optimization, these computational strategies offer a powerful and efficient path toward developing the next generation of targeted, effective glioblastoma therapeutics, ultimately improving patient outcomes.
References
- 1. Glioblastoma at the crossroads: current understanding and ... [https://www.nature.com/articles/s41392-025-02299-4]
- 2. Mechanisms of Resistance and Current Treatment Options for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10093719/]
- 3. Frontiers in glioblastoma therapy: Novel therapeutics ... [https://www.sciencedirect.com/science/article/abs/pii/S2773044125001330]
- 4. Targeting drug resistance in glioblastoma (Review) [https://www.spandidos-publications.com/10.3892/ijo.2024.5668]
- 5. Molecular Mechanisms of Drug Resistance in Glioblastoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232134/]
- 6. Breaking barriers for glioblastoma with a path to enhanced ... [https://www.nature.com/articles/s41467-023-41694-9]
- 7. Is the blood–brain barrier really disrupted in all glioblastomas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5777482/]
- 8. New Brain Tumor Clinical Trials: November 2024 – June ... [https://braintumor.org/news/new-brain-tumor-clinical-trials-november-2024-june-2025%EF%BF%BC/]
- 9. 3D-QSAR, Scaffold Hopping, Virtual Screening, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11242256/]
- 10. Exploration of 2D and 3D-QSAR analysis and docking studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10501407/]
- 11. Beginner's Guide to 3D-QSAR in Drug Design [https://neovarsity.org/blogs/beginners-guide-3d-qsar-drug-design]
- 12. 3D-QSAR : Principles and Methods [https://drugdesign.org/chapters/3d-qsar/]
- 13. Virtual Screening-Guided Discovery of Small-Molecule ... [https://pubmed.ncbi.nlm.nih.gov/41257003/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=06GkjNH4AH1NAvh0oy91COFblb7W8KaKLyYB8XAQFrh&fc=None&ff=20251119173212&v=2.18.0.post22+67771e2]
- 14. An innovative machine learning-based QSAR approach for ... [https://pubmed.ncbi.nlm.nih.gov/40682750/]
- 15. 3D-QSAR, Scaffold Hopping, Virtual Screening, and ... [https://www.mdpi.com/1422-0067/25/13/7434]
- 16. Derivation of Highly Predictive 3D-QSAR Models for hERG ... [https://www.mdpi.com/1424-8247/16/11/1509]
- 17. Prioritization of new molecule design using QSAR models - 2D [https://cresset-group.com/discovery/specific/prioritization-new-molecule-design-qsar-models/]
- 18. Robust and predictive 3D-QSAR models for ... - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2024/ra/d4ra05342g]
- 19. Alignment-independent technique for 3D QSAR analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4833814/]
- 20. Identification of potential therapeutic targets and ... [https://www.sciencedirect.com/science/article/pii/S3050475925000922]
- 21. Combined machine learning models, docking analysis ... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-024-01316-x]
- 22. Recent advances of IDH1 mutant inhibitor in cancer therapy [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.982424/full]
- 23. Drug Combinations Targeting FAK and MEK Overcomes ... [https://pubmed.ncbi.nlm.nih.gov/40430842/]
- 24. Acid ceramidase and its inhibitors: a de novo drug target and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5762539/]
- 25. Machine learning-based QSAR and structure-based virtual ... [https://pubmed.ncbi.nlm.nih.gov/40629220/]
- 26. CHI3L1-targeted small molecules as glioblastoma therapies [https://pubmed.ncbi.nlm.nih.gov/40663973/]
- 27. How Cheminformatics is Used in Drug Discovery in 2025? [https://neovarsity.org/blogs/how-cheminformatics-is-used-in-drug-discovery]
- 28. Data Curation in Machine Learning: Ultimate Guide 2024 [https://atlan.com/data-curation-in-machine-learning/]
- 29. 3D-QSAR-Based Pharmacophore Modeling, Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8410400/]
- 30. Integrated Workflow for Drug Repurposing in Glioblastoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191016/]
- 31. Generation and validation of a novel multitarget small ... [https://www.nature.com/articles/s41419-025-07569-1]
- 32. 3D-QSAR-Based Pharmacophore Modeling, Virtual ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2022.909111/full]
- 33. AI-Integrated QSAR Modeling for Enhanced Drug Discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525248/]
- 34. 3D-QSAR CoMFA/CoMSIA models based on theoretical ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523409003080]
- 35. CoMFA, CoMSIA, HQSAR and Molecular Docking Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4852576/]
- 36. 3D-QSAR Studies, Molecular Docking, Molecular Dynamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9865323/]
- 37. CoMFA and CoMSIA Studies of 1,2-dihydropyridine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4980841/]
- 38. Semi-supervised regression trees with application to QSAR ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417420303936]
- 39. Tracking protein kinase targeting advances: integrating QSAR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11980485/]
- 40. From Molecular Descriptors to Predictive Potency - Sciety [https://sciety.org/articles/activity/10.21203/rs.3.rs-7472281/v1?utm_source=sciety_labs_article_page]
- 41. A novel non-linear approach for establishing a QSAR model of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10565811/]
- 42. Multi-Targeting Approach in Glioblastoma Using Computer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9317902/]
- 43. Recent advances in molecular representation methods and ... [https://www.nature.com/articles/s44386-025-00017-2]
- 44. Shape-Based Virtual Screening with Volumetric Aligned ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4140985/]
- 45. Molecular descriptors for high-throughput virtual screening ... [https://www.nature.com/articles/s41524-025-01792-2]
- 46. Identification and evaluation of pyrimidine based CDK6 ... [https://www.nature.com/articles/s41598-025-10744-1]
- 47. Advances in bridging computational and clinical outcomes ... [https://www.sciencedirect.com/science/article/pii/S2949829525001044]
- 48. -Guided Discovery of Small-Molecule... Virtual Screening [https://pubmed.ncbi.nlm.nih.gov/41257003/]
- 49. Antiviral Compounds Discovered by Virtual Screening of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2782732/]
- 50. Virtual Screening-Guided Discovery of Small Molecule ... [https://pubmed.ncbi.nlm.nih.gov/40766683/]
- 51. The Light and Dark Sides of Virtual Screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC6470506/]
- 52. A Beginner's Guide to QSAR Modeling in Cheminformatics ... [https://neovarsity.org/blogs/cheminformatics-qsar-beginner-guides]
- 53. Comparison of various methods for validity evaluation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9396839/]
- 54. 3D-QSAR - Lead Optimization in Orion [https://www.eyesopen.com/3d-qsar]
- 55. Computational approaches: atom-based 3D-QSAR, molecular ... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-024-01357-2]
- 56. 3D-QSAR, design, molecular docking and dynamics ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1545791/full]
- 57. Insights from 3D-QSAR, molecular docking, and dynamics for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0326245]
- 58. Computational identification and evaluation of novel PD-L1 ... [https://www.nature.com/articles/s41598-025-01232-7]
- 59. Integrating ligand and structure-based discovery ... [https://japsonline.com/abstract.php?article_id=4367&sts=2]
- 60. Simulation, 3D-QSAR, molecular docking and ... [https://www.sciencedirect.com/science/article/pii/S1570180825000077]
- 61. Blood brain barrier permeability prediction with artificial ... [https://link.springer.com/article/10.1007/s44163-025-00494-4]
- 62. A Review of Blood Brain Barrier Permeability Prediction Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949286/]
- 63. Development of QSAR models to predict blood-brain barrier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9633177/]
- 64. QSAR model for blood-brain barrier permeation [https://www.sciencedirect.com/science/article/abs/pii/S105687191730014X]
- 65. Pharmacophore-based virtual screening, 3D QSAR ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482523009460]
- 66. GlioSurvQNet: A DuelContextAttn DQN Framework for ... [https://www.mdpi.com/2075-4418/15/18/2304]
- 67. ResisenseNet hybrid neural network model for predicting ... [https://www.nature.com/articles/s41598-024-71076-0]
- 68. Machine learning accelerates pharmacophore-based ... [https://www.nature.com/articles/s41598-024-58122-7]
- 69. 3D-QSAR, molecular docking, molecular dynamics, and ... [https://pubmed.ncbi.nlm.nih.gov/34791695/]
- 70. Molecular Docking: A powerful approach for structure-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3151162/]
- 71. Molecular Docking and Simulation Analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563906/]
- 72. Optimization of Cavity-Based Negative Images to Boost ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8889583/]
- 73. Molecular Docking and Molecular Dynamics Studies Reveal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9653723/]
- 74. Potential diagnostic and drug target markers in glioblastoma [https://www.nature.com/articles/s41598-024-57752-1]
- 75. ChemMORT: an automatic ADMET optimization platform using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10883642/]
- 76. Insights into the Structural Patterns in Human Glioblastoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389136/]
- 77. Role of Pharmacokinetic/ Pharmacodynamic Modeling and ... [https://esmed.org/MRA/mra/article/view/6147]
- 78. PharmaBench: Enhancing ADMET benchmarks with large ... [https://www.nature.com/articles/s41597-024-03793-0]
- 79. Combined machine learning models, docking analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11490052/]
- 80. Revolutionizing pharmacology: AI-powered approaches in ... [https://www.sciencedirect.com/science/article/pii/S259009862500020X]
- 81. Polyphenol-based therapeutics for glioblastoma : validation from... [https://pubmed.ncbi.nlm.nih.gov/41074968/]
- 82. In silico prediction of GRP78-CRIPTO binding sites to improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075867/]
- 83. 7 Brain Cancer Treatment Drugs: Latest Medications and ... [https://int.livhospital.com/7-brain-cancer-treatment-drugs-latest-medications-and-therapies-in-2025/]
- 84. Glioblastoma Treatment Drugs Market Size 2025 to 2035 [https://www.futuremarketinsights.com/reports/glioblastoma-treatment-drugs-market]
- 85. Glioma drug development benefits from emerging phase 0 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465642/]
- 86. Scientists Wipe Out Aggressive Brain Cancer Tumors by ... [https://wertheim.scripps.ufl.edu/2025/07/01/scientists-wipe-out-aggressive-brain-cancer-tumors-by-targeting-cellular-motors/]
- 87. Glioblastoma Pipeline Drugs Report 2025: Promising Drugs, [https://www.openpr.com/news/4202719/glioblastoma-pipeline-drugs-report-2025-promising-drugs]